Professional Documents
Culture Documents
Acute Myocardial Infarction
Acute Myocardial Infarction
Uploaded by
Listya NormalitaCopyright:
Available Formats
You might also like
- Case Study Acute Myocardial InfarctionDocument11 pagesCase Study Acute Myocardial InfarctionChristine Elaine Batusin Ilagan91% (23)
- Case Study-Congestive Heart FailureDocument71 pagesCase Study-Congestive Heart FailureKentTangcalagan92% (13)
- Acute Myocardial InfarctionDocument35 pagesAcute Myocardial Infarctionvirnzrobz80% (10)
- Myocardial Infarction Case StudyDocument19 pagesMyocardial Infarction Case Studyapi-312992151No ratings yet
- Surgical Case Study: CranioplastyDocument50 pagesSurgical Case Study: Cranioplastyrhia casinillo100% (8)
- Vascular Surgery MCQsDocument66 pagesVascular Surgery MCQsmohammadeid100% (7)
- Acute Coronary Syndrome - CSDocument91 pagesAcute Coronary Syndrome - CSMASII89% (9)
- Acute Myocardial Infarction - CSDocument49 pagesAcute Myocardial Infarction - CSMASII94% (17)
- Acute Coronary Syndrome - A Case StudyDocument11 pagesAcute Coronary Syndrome - A Case StudyRocel Devilles100% (2)
- Case Study NSTEMIDocument26 pagesCase Study NSTEMIHomework Ping100% (1)
- Acute Myocardial InfarctionDocument20 pagesAcute Myocardial InfarctionDavid Christian CalmaNo ratings yet
- Acute Coronary SyndromeDocument13 pagesAcute Coronary Syndromelavs17100% (1)
- Case Study of A Patient With Ischemic CardiomyopathyDocument33 pagesCase Study of A Patient With Ischemic Cardiomyopathyromeo rivera80% (5)
- Pathophysiology of Myocardial InfarctionDocument2 pagesPathophysiology of Myocardial Infarctionkobe_andre15100% (28)
- Case Study Heart Attack PDFDocument30 pagesCase Study Heart Attack PDFtkgoon634950% (2)
- Congestive Heart FailureDocument18 pagesCongestive Heart FailureAisha Rashed100% (1)
- Case Study (ACS)Document12 pagesCase Study (ACS)Kristel Joy Cabarrubias Acena100% (1)
- Myocardial InfarctionDocument20 pagesMyocardial Infarctionshmily_0810100% (2)
- Myocardial InfarctionDocument21 pagesMyocardial Infarctionanon_516349434No ratings yet
- Pathophysiology Worksheet MIDocument2 pagesPathophysiology Worksheet MIpjbedelNo ratings yet
- 2 Myocardial Infarction Nursing Care Management and Study GuideDocument13 pages2 Myocardial Infarction Nursing Care Management and Study GuideQuijano Gpokskie100% (2)
- Myocardial InfarctionDocument21 pagesMyocardial InfarctionasdnofalNo ratings yet
- Micu Case Study d1Document28 pagesMicu Case Study d1jmarc_2180% (5)
- CASE-STUDY Myocardial InfarctionDocument77 pagesCASE-STUDY Myocardial Infarctionjuodie100% (1)
- Group-1b Myocardial InfarctionDocument39 pagesGroup-1b Myocardial InfarctionJean ReyesNo ratings yet
- CHF Case StudyDocument38 pagesCHF Case StudyMelissa David100% (1)
- Case Study Trauma and Emergency Nursing NRSG 467-SHOCKDocument21 pagesCase Study Trauma and Emergency Nursing NRSG 467-SHOCKErickNabiswa100% (2)
- Myocardial InfarctionDocument16 pagesMyocardial InfarctionCay Sevilla100% (4)
- Cardiac TamponadeDocument3 pagesCardiac Tamponadescremo_xtreme100% (2)
- Myocardial InfarctionDocument45 pagesMyocardial InfarctionGopal SinghNo ratings yet
- Non-St Segment Elevation Myocardial Infarction (Nstemi)Document24 pagesNon-St Segment Elevation Myocardial Infarction (Nstemi)MHIEMHOINo ratings yet
- Modified CaseDocument22 pagesModified CaseAli HawamdeNo ratings yet
- Pathophysiology of Myocardial InfarctionDocument4 pagesPathophysiology of Myocardial InfarctionYhr YhNo ratings yet
- Acute Coronary SyndromeDocument43 pagesAcute Coronary SyndromeMsOrange96% (27)
- Hypovolemic Shock 09Document58 pagesHypovolemic Shock 09Joanne Bernadette Aguilar100% (2)
- CvaDocument170 pagesCvaApril Jumawan ManzanoNo ratings yet
- Myocardial InfarctDocument4 pagesMyocardial InfarctDanelle Harrison, RN100% (1)
- Post Op Cabg CareDocument31 pagesPost Op Cabg CareYeria Rayanti100% (1)
- Aortic Aneurysm - FinalDocument67 pagesAortic Aneurysm - FinalJonathan DiazNo ratings yet
- PneumoniaDocument71 pagesPneumoniafrancis00090100% (1)
- Pulmonary EmbolismDocument5 pagesPulmonary EmbolismNica Duco100% (2)
- PT EducationDocument4 pagesPT Educationapi-248017509No ratings yet
- Cabg 130102113345 Phpapp01Document29 pagesCabg 130102113345 Phpapp01md.dascalescu2486No ratings yet
- HypertensionDocument8 pagesHypertensiongilma100% (3)
- Congestive Heart Failure PathophysiologyDocument16 pagesCongestive Heart Failure PathophysiologyDale LaurenteNo ratings yet
- Case Study On Subacute Subdural HematomaDocument33 pagesCase Study On Subacute Subdural Hematomajarelle bondoc100% (15)
- Acute Myocardial InfarctionDocument17 pagesAcute Myocardial InfarctionRuqowiyah TanjungNo ratings yet
- Myocardial InfarctionDocument18 pagesMyocardial InfarctionYanna Habib-MangotaraNo ratings yet
- "Acute Coronary Syndrome Non ST Elevation Myocardial Infarction, Hypertensive Cardiovascular Disease, Diabetes Mellitus Type 2, and Community Acquired Pneumonia" IntroDocument6 pages"Acute Coronary Syndrome Non ST Elevation Myocardial Infarction, Hypertensive Cardiovascular Disease, Diabetes Mellitus Type 2, and Community Acquired Pneumonia" IntroCarl Elexer Cuyugan AnoNo ratings yet
- Myocardial Infarction: Disscused With Head Supervisor: DR - Yassmeen Ahmed of Pathology Department:prof - Dr.Manal El-NemrDocument23 pagesMyocardial Infarction: Disscused With Head Supervisor: DR - Yassmeen Ahmed of Pathology Department:prof - Dr.Manal El-NemrOmar ShazlyNo ratings yet
- CARDIO (PBL3) - Mohamad Arbian Karim - FMUI20Document10 pagesCARDIO (PBL3) - Mohamad Arbian Karim - FMUI20Mohamad Arbian KarimNo ratings yet
- Prevalence and Risk Factors: HypertensionDocument2 pagesPrevalence and Risk Factors: HypertensionKhristine Anne FabayNo ratings yet
- Myocardial InfarctionDocument18 pagesMyocardial InfarctionMarc Lorenz DucusinNo ratings yet
- General Nursing Science 1 2020 PDFDocument95 pagesGeneral Nursing Science 1 2020 PDFRicardo DomingosNo ratings yet
- Cardiovasculer DiseasesDocument84 pagesCardiovasculer DiseasesrashrikantNo ratings yet
- Disorders of Cardiac FunctionDocument60 pagesDisorders of Cardiac FunctionSaif AliNo ratings yet
- Myocardial Infarction AssignmentDocument23 pagesMyocardial Infarction AssignmentPums100% (6)
- Ischaemic Cardiogenic ShockDocument4 pagesIschaemic Cardiogenic ShocksuckeydluffyNo ratings yet
- Myocardial InfarctionDocument20 pagesMyocardial Infarction* mokhtar !!50% (2)
- NCP Myocard Infarction Group 8Document12 pagesNCP Myocard Infarction Group 8nadyaNo ratings yet
- Mi PDFDocument10 pagesMi PDFReyan AbidinNo ratings yet
- Telecare Collaborative Management of Chronic Pain in Primary 222Document13 pagesTelecare Collaborative Management of Chronic Pain in Primary 222Listya NormalitaNo ratings yet
- Scabies Diagnosis and ManagementDocument5 pagesScabies Diagnosis and ManagementAbdul Rauf ZakariaNo ratings yet
- Dermatitis Herpetiformis: Timo L. Reunala, MDDocument9 pagesDermatitis Herpetiformis: Timo L. Reunala, MDListya NormalitaNo ratings yet
- 3 LOed-bedah Islam 33 - 41Document13 pages3 LOed-bedah Islam 33 - 41Listya NormalitaNo ratings yet
- Cover 24 Chap 1Document1 pageCover 24 Chap 1Listya NormalitaNo ratings yet
- Glaucoma American Journal of OphtalmologyDocument7 pagesGlaucoma American Journal of OphtalmologyListya NormalitaNo ratings yet
- Fisiologi BatukDocument25 pagesFisiologi BatukListya NormalitaNo ratings yet
- Fisiologi BatukDocument25 pagesFisiologi BatukListya NormalitaNo ratings yet
- 24th Block-Trauma & Emergencies: Kegawatan Gastrointestinal Kegawatdaruratan ObsginDocument2 pages24th Block-Trauma & Emergencies: Kegawatan Gastrointestinal Kegawatdaruratan ObsginListya NormalitaNo ratings yet
- Krisis AdrenalDocument18 pagesKrisis AdrenalListya NormalitaNo ratings yet
- Abnormal Labor-ModifiedDocument8 pagesAbnormal Labor-ModifiedListya NormalitaNo ratings yet
- Airway & Breathing Manaj DR BambangDocument50 pagesAirway & Breathing Manaj DR BambangListya NormalitaNo ratings yet
- Antiplatelet, Thrombolitik, Antikoagulan, Vasodilator Referat VaskularDocument23 pagesAntiplatelet, Thrombolitik, Antikoagulan, Vasodilator Referat Vaskularmonyet65No ratings yet
- Scientific Discussion: 1/20 EMEA 2004Document20 pagesScientific Discussion: 1/20 EMEA 2004Donny Rahman KhalikNo ratings yet
- Hemofarm Vademekum Engleska Verzija Za 2013Document143 pagesHemofarm Vademekum Engleska Verzija Za 2013Svet MedicineNo ratings yet
- Naturales CapsiumDocument8 pagesNaturales CapsiummaryNo ratings yet
- Blood Drugs Used For AneamiasDocument7 pagesBlood Drugs Used For AneamiasMaha KhanNo ratings yet
- Dha July 2NDDocument11 pagesDha July 2NDAryan KhanNo ratings yet
- Anticoagulant and Antiplatelet Medications and Dental Procedures ADADocument8 pagesAnticoagulant and Antiplatelet Medications and Dental Procedures ADADeeNo ratings yet
- Anticoagulant Powerpoint PresentationsDocument60 pagesAnticoagulant Powerpoint PresentationsREETHUNo ratings yet
- Complications in Dentoalveolar Surgery PDFDocument37 pagesComplications in Dentoalveolar Surgery PDFmirfanulhaqNo ratings yet
- Practice Guidelines For Acute Care Nurse Practitioners E Book 2Nd Edition PDF Full Chapter PDFDocument53 pagesPractice Guidelines For Acute Care Nurse Practitioners E Book 2Nd Edition PDF Full Chapter PDFpitsonmoedi100% (6)
- Antiplatelet Antikoagulan FibrinolitikDocument15 pagesAntiplatelet Antikoagulan FibrinolitikChimul Lavigne 'L'No ratings yet
- Kaplan Powerpoint Pharm Review Usmle Step 1-: - Flash Cards by Cueflash PDFDocument6 pagesKaplan Powerpoint Pharm Review Usmle Step 1-: - Flash Cards by Cueflash PDFAnonymous OAmXUJFRRR100% (1)
- Lecture 6 Pharma DR N AlhasaniDocument9 pagesLecture 6 Pharma DR N Alhasanialialahmedy24No ratings yet
- Anticoagulatns, Antiplatelets, Fibrinolytics, AntifibrinolyticsDocument2 pagesAnticoagulatns, Antiplatelets, Fibrinolytics, AntifibrinolyticsArvinth Guna SegaranNo ratings yet
- Lacunar Stroke Guide - Causes, Symptoms and Treatment OptionsDocument6 pagesLacunar Stroke Guide - Causes, Symptoms and Treatment OptionsRismanto TorsioNo ratings yet
- Cerebro Vascular DiseasesDocument45 pagesCerebro Vascular DiseasesonyotzNo ratings yet
- Pharmacology Review Drugs That Alter Blood Coagulation PDFDocument6 pagesPharmacology Review Drugs That Alter Blood Coagulation PDFyouyayuNo ratings yet
- Overall Strategy For Treatment of Critical Limb IschemiaDocument83 pagesOverall Strategy For Treatment of Critical Limb IschemiaamurachNo ratings yet
- Dipake 2Document19 pagesDipake 2AriWahyuNo ratings yet
- Abciximab Package InsertDocument22 pagesAbciximab Package InsertbiomedjobhuntNo ratings yet
- Materi - Antiplatelet Pada ACSDocument18 pagesMateri - Antiplatelet Pada ACSTuhfatul UlyaNo ratings yet
- Anticoagulants Preoperative InstructionsDocument3 pagesAnticoagulants Preoperative InstructionsDevaki VisvalingamNo ratings yet
- Transient Ischemic Attacks: Rodney W. Smith, MDDocument58 pagesTransient Ischemic Attacks: Rodney W. Smith, MDNatalija TomićNo ratings yet
- Anticoagulation Guidelines JMDocument32 pagesAnticoagulation Guidelines JMMichael HuntNo ratings yet
- Blood Pharmacology by Dr. Mayur Sayta M 910444Document21 pagesBlood Pharmacology by Dr. Mayur Sayta M 910444funzz100% (1)
- ASRA Guidelines Regional Anaesthesia in Anticoagulated PatientDocument10 pagesASRA Guidelines Regional Anaesthesia in Anticoagulated PatientRizg AlamriNo ratings yet
- Antiplatelet DrugsDocument15 pagesAntiplatelet Drugsngan321100% (1)
- Fibrinolytics, Anti Fibrinolytics and Anti Platelets: Dr. B.K.Bezbaruah Professor Pharmacology Gauhati Medical CollegeDocument46 pagesFibrinolytics, Anti Fibrinolytics and Anti Platelets: Dr. B.K.Bezbaruah Professor Pharmacology Gauhati Medical CollegeBidyut BanerjeeNo ratings yet
- Acute Coronary Syndrome & The PLATO Trial: Ticagrelor vs. ClopidogrelDocument42 pagesAcute Coronary Syndrome & The PLATO Trial: Ticagrelor vs. ClopidogrelDedeSumantraNo ratings yet
Acute Myocardial Infarction
Acute Myocardial Infarction
Uploaded by
Listya NormalitaOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Acute Myocardial Infarction
Acute Myocardial Infarction
Uploaded by
Listya NormalitaCopyright:
Available Formats
Critical care nursing cardiac imad thultheen
Acute Myocardial Infarction
Lecture Description
This Lecture is designed to give an overview of the care and management of
the patient who has suffered an acute myocardial infraction (MI). Focus will
be placed on the pathophysiologic changes that occur during an acute MI as
well as differentiating the different types of myocardial infarction (based on
location). The prevalence, risk factors, signs/symptoms and diagnosis of an
acute MI will also be presented. Potential complications associated with an
acute MI (including cardiogenic shock) as well as medical/pharmaceutical
interventions will be presented. Nursing care and management with NANDA
nursing diagnoses to include defining characteristics, nursing interventions
and patient/family education will also be presented. Appropriate cardiac
rehabilitation interventions will be the final focus of this course.
Lecture Objectives
Upon completion of this course the student will be able to:
Understand and define the pathophysiologic changes seen with an
acute MI
Differentiate the different types of MI based on location of
ischemia/infarct
Discuss the prevalence associated with an acute MI
State the risk factors associated with an acute MI
Critical care nursing cardiac imad thultheen
Explain the necessary assessment/tests to diagnose an acute MI
Discuss the potential complications associated with having an acute MI
Describe medical management for the patient who has suffered and
acute MI
List 3 appropriate nursing diagnoses for managing the patient with and
acute MI
Discuss the nursing interventions appropriate for caring for the patient
who has suffered and acute MI (alteration in cardiac output, pain,
anxiety and ineffective coping)
Explain the important aspects of patient education post MI
Describe the important aspects of cardiac rehabilitation
Defining Myocardial Infarction:
An acute MI occurs when myocardial cells have reached the threshold of
ischemia; which in turn cause the bodys myocardial cell repair mechanism to
first become overwhelmed and second to completely fail. When this
mechanism fails, myocardial tissue necrosis causing irreparable tissue/cell
death occurs.
The following are possible contributors to myocardial ischemia and ultimately
myocardial infarction (tissue necrosis and cell death):
Increased myocardial metabolic demand which include:
o
Extremes in physical exertion
Severe hypertension
Obstructive Cardiomyopathy
Severe aortic stenosis
Critical care nursing cardiac imad thultheen
o
Other cardiac valvular disorders
Low cardiac output states associated with a decrease in aortic
diastolic pressure
Decreased delivery of oxygen and nutrients to the myocardium (via the
coronary circulation).
An interruption in the delivery of oxygen and nutrients to the
myocardium from a thrombus (that usually attaches itself to plaque).
A high grade (usually > 75%) fixed coronary artery stenosis do to
atherosclerosis.
Pathophysiology:
The most frequent cause of an acute MI is a disruption in the vascular
endothelium that is associated with myocardial plaque (plaque occurs
over a period or years or decades). This combination causes the
development of an intra-coronary thrombus, which causes the coronary
artery affected to occlude. Within 20 to 40 minutes of an occlusion;
irreversible myocardial cell damage/death occurs.
The two primary characteristics of plaque development are (1) a
fibromuscular cap and (2) an underlying lipid rich core. Plaque erosion
is thought to occur when there is a release of collagen and proteases
(within the plaque) which results in thinning of the overlying
fibromuscular cap. The action/release of proteases within the plaque
combined with hemodynamic pressure applied to the arterial segment,
causes continued disruption of the endothelium which leads not only to
continued thinning of the fibromuscular cap, but to actual cap rupture
(causing plaque erosion and/or ulceration).
Critical care nursing cardiac imad thultheen
The overall loss of structural stability of the plaque usually occurs at the
junction between the fibromuscular cap and the vessel wall (which is
called the shoulder region). When this occurs, a thrombus develops
(due to the platelet-mediated activation of the coagulation cascade),
and partial or complete occlusion occurs causing an acute myocardial
infarction.
The severity of an acute MI depends on the level of occlusion in the
coronary artery, the length of time of the occlusion and the patients
own collateral circulation. Myocardial cell death first occurs in the
portion of the artery that is most distal to arterial blood flow and as the
occlusion increases the damage spreads from the myocardium to the
endocardium and eventually to the epicardium. After cell death has
reached the epicardium, the tissue/cell death then moves laterally to
the areas of collateral perfusion.
Critical care nursing cardiac imad thultheen
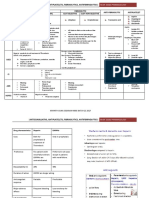
Different Types of Acute MI (Based on Location):
The location of an acute MI is dependant on the coronary artery that has been
affected and what portion of the heart that artery feeds. The following table
describes the affected artery, a description of the major areas and structures
that supply blood to the area and the primary infarction area.
Coronary Artery
Area and Structures
Primary Area of
Right Coronary
Supplied
1. SA and AV nodes.
Infarction
1. Inferior wall MI (leads II,
Artery
2. Bundle of HIS.
III and AVF).
3. Right atrium/ventricle.
2. Inferoposterior wall MI.
4. Left ventricle (inferior and
3. Right ventricular MI.
diaphragmatic regions).
5. Septum (1/3rd).
6. Posterior/Inferior portion of
Left Coronary Artery
the Left bundle branch.
1. The major portion of the left
Left ventricular MI.
ventricular region of the heart.
Left Anterior
1. Anterior wall of the left
1. Anterior wall MI (Leads
Descending Artery
ventricle.
V1 through V6).
2. Anterior two thirds of the
2. Septal MI.
septum.
3. Anterolateral wall MI.
3. Bundle of HIS.
4. Inferoapical wall MI.
4. Right bundle branch.
5. Apex (region) MI.
5. Anterosuperior portion of the
left bundle branch.
6. Posteroinferior portion of the
left bundle branch.
Critical care nursing cardiac imad thultheen
Left Circumflex
1. SA and AV nodes.
1. Lateral wall MI (leads I
Artery
2. Inferior and diaphragmatic
aV1, V5 and V6).
surface of the left ventricle.
2. Inferolateral wall MI.
3. Lateral wall of the left
3. Posterior wall MI (leads
ventricle.
V1 and V2).
4. Left atrium.
4. Inferoposterior wall MI.
5. Posteroinferior portion of the
left bundle branch.
Note: An ST-segment elevation myocardial infarction (STEMI) can occur
when there is a complete blockage of any artery(s). This type of MI is
characterized by an upward shift in a portion of the ST segment (seen on
EKG). With this type of myocardial infarction, quick interventions to reopen
the occluded vessel or vessels are imperative. The longer the myocardium
goes without oxygenated blood, the greater the damage.
Prevalence:
Myocardial infarction is the leading cause of death in the United States
and is the most common cause of death in the industrial world as well.
The good news is that the survival rate for patients who seek medical
treatment for an acute MI is up to 90% to 95%. This improvement in
survival is thought to be related to improved EMS responses and
treatment strategies.
With approximately 50% of all acute MIs in the United States
occurring to people under the age of 65; this disease is no longer
thought to be a disease for the elderly (as the baby boomers age, this
Critical care nursing cardiac imad thultheen
percentage is thought to again switch back to show more people over
the age of 65 with acute MIs).
The actual incident of suffering an acute MI depends on the number of
pre-disposing factors for atherosclerosis.
Risk Factors/Causes:
There are six primary risk factors for developing atherosclerosis/coronary
artery disease and acute myocardial infarction. The presence of any risk factor
is thought to double the relative risk for developing atherosclerosis/coronary
artery disease and acute myocardial infarction.
These risk factors include:
High Blood Cholesterol (Hyperlipidemia) An elevated total
cholesterol level is major component of atherosclerotic plaque build up
which causes the development of an acute MI.
Diabetes Mellitus Patients with DM have a substantially greater risk
of developing atherosclerotic vascular disease at an accelerated rate.
This acceleration occurs regardless of whether the patient has insulin
dependant or non insulin dependant diabetes.
Hypertension High blood pressure (squeezing of arteries and veins)
has consistently been associated with an increased risk of developing
an acute MI (both systolic and diastolic elevations).
Smoking Tobacco contains certain components that are known to
damage vessel walls. The bodys response to this damage elicits the
formation of atherosclerosis thereby increasing the risk of an acute MI.
Critical care nursing cardiac imad thultheen
Male Gendered The incidence of developing an acute MI is greater for
men than women however; with age this risk narrows.
Family History A family history of premature coronary disease
increases and individuals risk of developing atherosclerosis and acute
MI. Family history includes both genetic components and learned
behaviors (i.e. smoking and high fat diets).
Diagnosis:
Diagnosing an acute MI can either be a very straight forward process or it can
be a difficult process. The straight forward diagnosis usually couples the
patients risk factors with the presentation of current symptoms (and past
medical history). Once a diagnosis of acute MI is suspected, the following
confirmatory tests should be ordered:
Electrocardiogram (ECG) Based on electrical changes in the coronary
system during an acute MI; an ECG is the first test that should be run.
Laboratory Tests Because heart cells have specific enzymes and proteins
that are released when cell death occurs, drawing blood levels to check for the
presence and degree of these enzymes will assist in diagnosing an acute MI.
The following provides a description of the major enzymes that are thought to
assist with the diagnosis of an acute MI.
Creatine Kinase (CK or CPK) Released from damaged muscle, CK is
an enzyme found in the heart, skeletal muscle and brain. It consists of 3
isoenzymes; mm (found in skeletal muscle, MB (found in cardiac
muscle) and BB (found in brain tissue). Damage to any of these tissues
Critical care nursing cardiac imad thultheen
causes the release of CK into the blood stream and hence an elevated
level.
CKMB After cardiac injury, CK and the isoenzyme MB are released
into the blood stream at a predictable rate. Within a 4 to 8 hour
window (post injury) the CKMB level rises above normal and within 12
to 24 hours this level elevates to approximately 5 to 15 times normal.
Within 2 to 3 days the CKMB returns to normal. Because the MB
isoenzyme is exclusive to cardiac muscle tissue, it is considered to be a
very definitive test for diagnosing an acute MI.
Troponin Troponin is a protein that helps regulate heart muscle
contraction and because it can be isolated in the blood, it is considered
to be a sensitive indicator of an acute MI. Troponin consists of 3
separate proteins which are Troponin I, Troponin T and Troponin C.
The function of each of these specific proteins is as follows:
o
Troponin I and T these levels are not normally found in the
blood stream so any detection of these protein in the blood
indicates the infarction or death of cardiac muscle/tissue.
Troponin C binds to calcium ions and is not used to determine
cell tissue/death.
Cardiac Enzyme Normal Values
Enzyme/Protein
Creatine Kinase
Total Creatinine Phosphokinase
Normal Value
50 80 U/L
30 - 200 U/L
(CPK)
CPK MB (Fraction)
CPK MB (Fraction with percent of
0 - 8.8 ng/ml
0-4%
total CPK).
CPK MB2 (Fraction)
Troponin 1
Troponin T
Less than 1 U/L
0 0.4 ng/ml
0 0.1 ng/ml
Critical care nursing cardiac imad thultheen
Echocardiogram An echocardiogram can assist with diagnosing which
portion of the heart has been damaged and which coronary arteries have been
affected. An echocardiogram can also help determine cardiac muscle
movement/contraction and cardiac wall abnormalities.
Potential Complications Associated with an Acute MI:
Dysrhythmias A dysrhythmia is the most common complication after an
acute MI. Dysrhythmias after an acute MI are caused by the formation of reentry circuits between the still healthy and necrotic myocardium. The
10
Critical care nursing cardiac imad thultheen
following table describes the percentage of time specific dysrhythmias occur
post acute MI.
Dysrhythmias
Percentage of time
Premature Ventricular
present post acute MI
90%
Contraction
Ventricular Fibrillation
Supraventricular (thought to
2% - 4%
< 10%
produce worse outcomes than
ventricular dysrhythmias)
Bradyarrhythmias (including
20% of patients with acute RV
AV block and sinus brady).
infarction
Embolic Complications The incidence of clinical significant systemic
embolism post acute MI is less than 2% (this percentage increases in patients
who have suffered and acute anterior wall MI). Mural thrombus formation is
however more prevalent post acute MI with numbers ranging in the 20%
range and increasing as high as 60% in patients with large anterior wall MIs
(development of emboli comes from myocardial wall motion deficits or atrial
fibrillation). The most common time post acute MI for the development of
embolism is within the first 10 days. Patients who suffer from the
complication of embolism are at risk of developing limb ischemia, renal
infarction, intestinal ischemia but the most common clinical presentation
after an embolic event is a stroke.
Pericarditis The incidence of early Pericarditis after and acute MI is
approximately 10% with inflammation developing within the first 24 to 96
hours after MI. Late Pericarditis occurs in 1% to 3% of post acute MI patients
11
Critical care nursing cardiac imad thultheen
between weeks 1 and 8 (after MI). The cause of Pericarditis after acute MI is
due to an inflammatory reaction that occurs secondary to the presence of
necrotic tissue (acute Pericarditis occurs most often in patients who have
suffered a transmural MI).
Cardiogenic Shock (secondary to acute MI) Simply stated; cardiogenic shock
occurs when the bodies needs for oxygen are not met for a prolonged period of
time. When this occurs; the body attempts to compensate for the decreased
oxygen supply by increasing heart rate, stroke volume and contractility.
Unfortunately as this continues, the workload of the heart becomes too much
and the result; total cardiac decompensation begins. When decompensation
begins the patient shows signs of shock, low blood pressure, increased or
decreased heart rate and decreased oxygen saturations. Other symptoms
mimic those that are seen with congestive heart failure and/or pulmonary
edema. This condition is critical and must be addressed emergently. In
addition to other medical and pharmaceutical therapies; patients in
cardiogenic shock are often helped with the addition of a balloon pump
(IABP). The major advantage of a balloon pump during cardiogenic shock is
the decrease in myocardial oxygen demand by decreasing myocardial
workload, and the increase in coronary artery perfusion.
Medical/Interventional Management:
PTCA A percutaneous transmural coronary angioplasty (PTCA) is an
effective revascularization procedure that is used to increase the diameter of
an artery that has been stenosed due to coronary artery disease. With the use
of fluoroscopy, a cardiologist can insert a catheter (through the femoral
12
Critical care nursing cardiac imad thultheen
artery) and guide it through the arterial circulation through the ascending
aorta and into the ostium of the right or left coronary artery. A balloon tipped
catheter is then passed into the area of blockage and inflated (no more than 30
to 129 seconds) which in turns helps to compress plaque against the lumina of
the artery. The balloon can also help to stretch the lumina itself which also
improves blood flow. Of note: when the balloon is inflated, there is an
occlusion of coronary blood supply, so patients often experience a degree of
chest pain during balloon inflation. The degree of chest pain experienced and
the difficulty in compression plaque may require that the physician inflate and
deflate the balloon several times during the procedure.
The following is a list of patients who are thought to be good candidates for
percutaneous transmural coronary angioplasty:
Patients with acute, chronic or unstable angina.
Patients with an acute MI or post acute MI.
Patients with angina post coronary artery bypass grafting (CABG).
Patients with single of double vessel disease.
Patients with at least 50% vessel stenosis.
Patients with a blockage that is concentric and located away from
bifurcations.
Patients who are thought to be good candidates for the survival of
emergency cardiac surgery (if there are procedural complications).
Note: PTCA is contraindicated in patients with left main coronary artery
disease (especially those who are thought to be poor surgical candidates).
13
Critical care nursing cardiac imad thultheen
Complications of PTCA include the following:
Acute coronary occlusion (requiring emergent surgical intervention).
Dissection of the artery.
Allergic reaction to contrast.
The development of bleeding or a hematoma at the femoral insertion
site (or retroperitoneal bleeding).
Decrease in circulation below the femoral insertion site (diminished or
absent pulses).
Vasovagal reaction (when sheath is removed).
The development of a pseudo aneurysm of the artery.
Re-stenosis or occlusion of the artery with in 6 months.
A blood clot breaking away and causing a stroke (or other embolic
event).
Contraindications for PTCA include:
A bleeding disorder (anti-coagulation should be stopped prior to
procedure).
Renal insufficiency
Severe uncontrolled hypertension
Severe peripheral vascular disease
Untreated active infections
Severe anemia
Uncorrected electrolyte imbalances
Endocarditis
PTCA (with stent placement) In addition to using angioplasty as an
intervention for compressing plaque and stretching the lumina of the artery;
14
Critical care nursing cardiac imad thultheen
the procedure can also be used to place a stent into the artery. A stent is a
small stainless steel tube that can be attached to the end of the balloon tipped
catheter and placed into the artery immediately after PTCA in an attempt to
more permanently prevent re-occlusion of the artery. For patients who have
undergone PTCA and suffered an arterial re-occlusion; the placement of a
stent is an alternative (benefit has been shown for patient who suffer renarrowing or re-occlusion).
Laser Angioplasty Laser angioplasty is a technique that can be used to open
coronary arteries that are blocked by plaque. With this procedure, the catheter
that is inserted has a small laser at the tip. When the catheter is in place; the
laser emits small pulsating beams of light that vaporize the plaque that is
blocking the artery. This procedure can be used alone or in conjunction with
balloon angioplasty.
Pharmaceutical Treatment Options:
Morphine Because catecholamines are released in response to the anxiety
and pain associated with suffering an acute MI (increasing the workload of the
heart), Morphine can be used. Morphine is also beneficial in reducing the
hemodynamic workload by increasing venous capacitance and reducing
systemic vascular resistance (therefore decreasing myocardial oxygen
demand).
Nitroglycerin Nitrates such as Nitroglycerin cause vasodilation of the vessels
and help to decrease cardiac oxygen demand, cardiac preload and afterload
while increasing cardiac output.
15
Critical care nursing cardiac imad thultheen
Aspirin Antiplatelet therapy (specifically aspirin) is now a standard therapy
for the treatment of angina and acute MI. The primary mechanism is believed
to be related to irreversible inhibition of the cyclooxygenase pathway of
platelets (blocking the formation of thromboxane A2 and thromboxane A2induced platelet aggregation). It is strongly recommended that all patients
who have suffered and acute MI be given a non-enteric coated aspirin (160mg
to 325mg) to chew and swallow as soon as possible.
Anticoagulants (ReoPro) ReoPro is a platelet glycoprotein II/b/IIIa receptor
inhibitor that has been proven to be effective for the management of any
coronary ischemic syndrome. It is starting during a PTCA procedure and in
most cases is used as an adjunct for stent placement. ReoPro is given as an IV
bolus of 0.25 mg/kg and followed by a continuous infusion rate of 10 mcg/min
for the following 12 hours. The use of ReoPro is thought to reduce platelet
aggregation by approximately 80%.
Anticoagulants (Ticlid) Ticlid is given in 250 mg doses BID and is also an
Antiplatelet agent. Unlike aspirin, Ticlid does not block cyclooxygenase but
instead interferes with the platelet activation mechanism that is mediated by
adenosine diphosphate (ADP) which in turn interferes with the fibrinogen
receptor glycoprotein IIb/IIIa. It takes approximately 2 weeks of therapy with
Ticlid before the full benefit is achieved.
Heparin Heparin is an anticoagulant that inhibits activated factors IS, S, SI
and XII (which are all involved in the conversion of Prothrombin to
16
Critical care nursing cardiac imad thultheen
thrombin). By inhibiting these activated factors, Heparin is thought to keep
the blood thinner and prevents clotting. This is turns allows for easier blood
travel through the vessels that are affected by narrowing and atherosclerosis.
Beta Blockers A beta blocker acts by blocking the B-adrenergic responses to
catecholamine stimulation. Beta blockers decrease heart rate, blood pressure,
contractility and myocardial oxygen demand. Being able to decrease the work
load of the heart assists with improving cardiac output and lessens the severity
of the damage caused by the acute MI. Beta blockers can actually interrupt an
evolving MI, limit the infarct size and decrease the risk of ventricular
arrhythmias by decreasing oxygen demand.
Calcium Channel Blockers Calcium channel blockers prohibit the entry of
calcium into smooth muscle. This assists with dilating coronary arteries and
veins which in turn provides an increase in overall cardiac blood flow. Calcium
channel blockers also decrease systemic blood pressure, total peripheral
resistance and cardiac afterload.
ACE inhibitors An Angiotensin converting enzyme; ACE inhibitors block to
the conversion of Angiotensin I to Angiotensin II (which is a potent
vasoconstrictor). The goal of and ACE inhibitor is to decrease blood pressure
and afterload without increasing heart rate or the workload of the heart.
tPA (Ateplase) tPA is a human protein that is manufactured by genetic
engineering. Tissue plasminogen activator is one of several drugs not
approved for use in certain patients who are suffering from and acute MI. tPA
17
Critical care nursing cardiac imad thultheen
is designed to dissolve the blood clots (in the arteries) that are responsible for
causing the majority of acute MIs. tPA is given in an initial 15 mg IV bolus
then 0.75 mg/kg (maximum of 50 mg) over 30 minutes. This is then followed
by 0.5 mg/kg (maximum 35 mg) over 60 minutes for a total of 100 mg over 90
minutes. Signs of reperfusion include pain relief; reperfusion arrhythmias
(accelerated idioventricular rhythm, ventricular ectopy and bradycardia).
Contraindications for the use of tPA:
Active internal bleeding
Intracranial neoplasm or recent brain surgery
Prolonged traumatic cardiopulmonary resuscitation
Allergy to streptokinase
Recent trauma or surgery (within the past 2 weeks)
Pregnancy
A history of hemorrhagic or non-hemorrhagic stroke
Dopamine Dopamine has both a and b-adrenergic effects (as well as
dopaminergic effects). At low doses (2-5 mcg/kg/min) it increases renal and
mesenteric blood flow. At moderate doses (5-10 mcg/kg/min) it has a positive
inotrope affect which increases blood pressure and cardiac output. At larger
doses (10-20 mcg/kg/min) it exhibits a pure alpha stimulation which causes
peripheral vasoconstriction with both increased systemic vascular resistance
(SVR) and afterload.
Dobutamine Dobutamine stimulates B-receptors of the heart and provide a
direct acting positive inotrope effect. Dobutamine increases stroke volume
18
Critical care nursing cardiac imad thultheen
and cardiac output by increasing cardiac contractility while decreasing SVR.
By increasing contractility and cardiac output; there is more oxygen rich blood
available for damaged tissue.
Nursing Care/Management and Patient Education (Based on
NANDA diagnosis):
Decreased Cardiac Output:
Definition Inadequate blood pumped by the heart to meet the metabolic
demands of the body.
Defining Characteristics:
Dysrhythmias (tachycardia, bradycardia, electrocardiographic
changes).
Altered Preload (jugular vein distention, fatigue, edema,
increased/decreased central venous pressure (CVP),
increased/decreased pulmonary artery wedge pressure (PAWP).
Altered Afterload (cool clammy skin, shortness of breath/dyspnea,
oliguria, prolonged capillary refill, decreased peripheral pulses)
Altered Contractility (crackles at the lung bases, cough,
orthopnea/nocturnal dyspnea, cardiac output less than 4 liters/min,
cardiac index less that 2.5 liters/min, decreased stroke volume,
decreased left ventricular stroke work index (LVSWI), S3 or S4 heart
sounds present).
Behavioral/Emotional (anxiety or restlessness).
Nursing Interventions:
19
Critical care nursing cardiac imad thultheen
Monitor for symptoms of heart failure/decreased cardiac output (VS,
heart sounds, and S3 gallop).
Observe for symptoms of cardiogenic shock (cool clammy skin,
hypotension, decreased peripheral pulses, and pulmonary congestion).
If shock present, monitor hemodynamic parameters for increased
PAWP and increased systemic vascular resistance.
Titrate inotropic and vasoactive medication within defined parameters
to maintain adequate contractility, pre/afterload and blood pressure.
For complaints of chest pain, medicate and note severity, location,
radiation, what were contributing factors (getting up, participating in
ADLs for example) and report findings.
Monitor intake and output (IV fluid, urine output, PO intake (fluid
overload increases the workload of the heart and decreased cardiac
output can cause a decrease in perfusion to the kidneys).
Note results of diagnostic imaging studies (EKG, radionuclide imaging,
and Dobutamine stress tests).
Watch laboratory data closely (ABGs, serial enzymes, electrolytes, Btype natriuretic peptide, serum creatinine).
Monitor oxygen saturation and provide O2 as ordered and necessary.
Monitor blood pressure/pulse before and after the administration of
cardiac medications.
HOB should be at 30 degrees to decrease the work of breathing and
decrease preload.
Provide a proper rest/activity balance to assure that cardiac output is
not compromised (gradually increase activity as condition warrants).
20
Critical care nursing cardiac imad thultheen
Order small sodium restricted diet (sodium restriction helps to avoid
fluid overload).
Monitor bowel function (a stool softener should be ordered to avoid
unnecessary pushing).
Provide a peaceful environment that minimizes stressors to promote
healing.
Weigh patient daily (same time each day, same equipment).
Assess for the presence of anxiety (keep environment free of
unnecessary stressors, educate patient to the rationale for interventions
and procedures).
Assess for the presence of depression (depression is common after and
acute MI and can result in increased mortality).
Refer patient to cardiac outpatient program and support groups. Assist
with organizing cardiac rehabilitation efforts post discharge.
Patient/Family Teaching:
Teach the patient the symptoms of heart failure and appropriate
actions to take.
Teach the importance of smoking cessation (patients who continue to
smoke increase their risk of a secondary MI by 50%).
Explain necessary restrictions (sodium restricted diet, guidelines for
fluid intake, avoidance of the valsalvo maneuver, pacing activity, work
simplification techniques).
Teach the patient regarding the importance of modifying other risk
factors such as diabetes and obesity.
21
Critical care nursing cardiac imad thultheen
Teach stress reduction exercises (controlled breathing, imagery, muscle
relaxation techniques).
Assist the patient to understand the importance of incorporating
changes into his/her current lifestyle. Refer to cardiac rehabilitation for
assistance with coping and adjusting).
Teach to patient the actions and side affects of the cardiac medication
they will be taking. Stress the importance of keeping prescriptions filled
and the importance of taking medication as ordered. Also teach the
patient to call or seek medical assistance if they are experiencing
serious side affects.
Instruct the patient on the importance of getting a flu shot and
pneumovac vaccine (if not already provided during the hospital stay).
Instruct the patient on the importance of daily weight and how an
increase in weight can signal fluid gain (which may be a sign of pending
heart failure). Provide specific written material and a self care plan for
the patient to take home and use as a reference.
Consult dietician or assist the patient to understand the importance of
a low sodium restricted diet.
Expected Outcomes:
Effective pump effectiveness
Improved cardiac circulation
Improved cardiac tissue perfusion
Improved perfusion to the abdominal organs/periphery
Improved vital signs
Alteration in Comfort (Pain):
22
Critical care nursing cardiac imad thultheen
Definition:
A state in which an individual experiences an uncomfortable sensation in
response to noxious stimulus.
Defining Characteristics:
Verbalization of discomfort
Observed behavior indicative of discomfort
Restless/tense behavior
Avoidance
Malaise
Aching/stiffness
Unusual hunger or thirst
Reduced mobility
Nursing Interventions:
Assess patients need holistically (physical discomfort often coexists
with emotional and spiritual discomfort).
Assess the degree of pain the patient is experiencing using the same
type of pain scale each time (i.e. 1-10 scale or FLACC scale).
Assess and document the onset, duration, location, type,
contributing/relieving factors when assessing for pain.
Consult with the physician for the most effective medication to reduce
pain (Nitroglycerin, Morphine and Oxygen are most commonly used).
Position patient for maximum comfort.
Assure a proper rest/activity balance (group nursing activities and
when possible limit uncomfortable interventions).
23
Critical care nursing cardiac imad thultheen
Provide distraction (imagery for example).
Assure an adequate rest period is available for patients post pain
medication administration.
Provide a quiet environment for patient and family.
Patient/Family Teaching:
Teach patient techniques to use when uncomfortable.
Teach patient to call nurse immediately if chest pain occurs.
Educate patient to all prescribed medications and treatments.
Upon discharge; assure that the patient/family has a good
understanding of medications to be taken at home.
Explain the importance of keeping all medical appointments.
Educate patient to the importance of balancing activity with rest.
Expected Outcomes:
Comfort level and pain in control.
Able to scale pain appropriately.
Able to recognize signs and symptoms of chest pain and promptly call
for assistance.
Explains methods to decrease discomfort.
Displays increase activity without discomfort.
Appears calm and without undue anxiety or stress.
Anxiety:
Definition: A vague uneasy feeling of discomfort or dread accompanied by an
autonomic response. The source of this feeling is either known or unknown to
the individual, but causes a feeling of apprehension, or possible danger.
24
Critical care nursing cardiac imad thultheen
Anxiety is an alerting signal that warns of impending danger and enables the
individual to take measures to deal with the threat.
Defining Characteristics:
Diminished productivity
Scanning and vigilance
Poor eye contact
Restless behavior
Glancing about
Extraneous movement (repetitive movement, foot shuffling)
Expressed concern resulting from life changes
Insomnia
Fidgeting
Irritability
Regretful/helpless/worried
Quivering voice/trembling/hand tremors
Elevated pulse and blood pressure
Nursing Interventions:
Assess patient/family level of anxiety as well of knowledge of existence
and cause. Use presence, touch (with permission), verbalization and
environmental factors to assist in decreasing anxiety.
25
Critical care nursing cardiac imad thultheen
Provide distraction (music, magazines, TV).
Accept the patient/family defenses or explanations of anxiety (denial
after an acute MI is often present).
Do not try to argue or demean the patient/family for their feelings.
Allow and reinforce the patient/family members expressions of pain,
discomfort and/or threats to their well being.
Help the patient/family develop coping strategies that will decrease
anxiety. Encourage positive (but realistic) thinking regarding
outcomes.
Avoid excessive reassurance as this may cause the patient/family to
worry unnecessarily.
Intervene when possible to remove sources of stress.
Explain, Explain, Explain (all activities, procedures, tests, and goals).
Patient/Family Teaching:
Teach patient/family the symptoms of anxiety.
Explain equipment (especially if in the ICU) and the monitors in the
room. Reinforce that most equipment is to make the assessment of the
patient easier and not actually NECESSARY as part of the patient
treatment or therapy.
Help the patient/family to be able to define anxiety levels (from easily
tolerated to intolerable). Use a color or number code for easy
identification.
Teach the patient/family self help techniques to avoid or minimize
stress and anxiety.
26
Critical care nursing cardiac imad thultheen
Teach the patient/family the use of distracters to avoid or minimize
stress and anxiety.
Teach the patient/family relaxation and deep breathing exercises.
Teach the patient/family the correlation between balancing sleep,
nutrition, exercise and lifestyle to avoid anxiety.
Help the patient/family distinguish between anxiety and panic.
Teach the patient/family appropriate community support.
Provide social services consult if patient/family showing signs of severe
anxiety.
Encourage the patient/family to keep a note pad handy to jot down
questions or concerns that they may have.
Expected Patient Outcomes:
Identifies and verbalizes symptoms of anxiety.
Identifies and demonstrates methods to decrease anxiety.
Verbalizes absence or decrease in subjective distress.
Normal vital signs.
Reports sleeping better and denies insomnia (use language that a child
will understand for this assessment).
27
Demonstrates improved concentration.
Demonstrates return ability to problem solve.
Demonstrates some ability to reassure self.
Critical care nursing cardiac imad thultheen
Ineffective Coping (Individual or Family):
Definition:
The inability to form a valid appraisal of internal or external stressors,
inadequate choices of practiced responses and/or the inability to access or use
currently available sources.
Defining Characteristics:
Lack of goal direction behavior.
The inability to resolve problems.
Difficulty with remembering or organizing thoughts.
Sleep disturbance.
Abuse of chemical agents.
Decreased use of social support.
The use of coping mechanisms that actually impeded adaptive
behavior.
Poor concentration.
Verbalization of the inability to cope.
Change in usual communication patterns.
Risk taking.
Nursing Interventions:
Observe for causes of ineffective coping such as a poor self-concept, a
lack of problem solving skills or lack of support for example (denial or
fear of the post MI lifestyle changes is often the source of stress that
causes ineffective coping).
28
Critical care nursing cardiac imad thultheen
Observe for strengths such as the ability to relate the facts and
recognize the source of stress.
Assess the risk of possible self harm.
Help the patient/family set realistic goals while identifying personal
skills and knowledge.
Use empathetic communication and encourage the patient/family to
verbalize fears and concerns.
Encourage the patient/family to participate in his/her care (on all
levels).
Explain tests, procedures and all other aspects of care prior to delivery.
Provide both mental and physical activities that are within the patients
ability.
Discuss changes with the patient/family before making them (room
changes, increases in activity for example).
Use active listening techniques when the patient is describing feelings
of sadness, loss, guilt or anger.
Encourage the patient to describe previous life stressors and how
he/she coped with those stressors in the past.
Be supportive.
Use systematic desensitization when introducing new people, places,
test or procedures (fear of new things diminishes with repeated
exposure).
Refer for counseling as needed.
Patient/Family Education:
29
Teach patient/family coping techniques such as problem solving.
Critical care nursing cardiac imad thultheen
Have the patient/family describe the problem or cause of their inability
to cope.
List the advantages and disadvantages of the situation as well as
possible options.
Provide the patient/family with literature about situations (test
procedures for example) of the stressor (if the stressor is identifiable).
Teach relaxation techniques.
Provide information about community resources.
Expected Outcomes:
Improved coping abilities
Improved decision making
Improved Impulse self control
Improved information processing
Ability to effectively participate in care
Additional NANDA Nursing Diagnoses for Consideration:
Alteration in breathing pattern
Alteration in nutrition
Fluid volume overload
Alteration in mobility
Knowledge deficit
Cardiac Rehabilitation:
The goals of cardiac rehab are to provide a medically supervised program
(post discharge) that is aimed at improving the patients overall physical and
mental abilities while stabilizing, slowing or even reversing the progression of
30
Critical care nursing cardiac imad thultheen
cardiovascular disease. The following components are part of a good cardiac
rehabilitation program:
Proper counseling and support so the patient has a better
understanding of his/her disease process.
The development of a patient specific exercise plan (even geriatric
patients with coronary disease/heart failure have been found to benefit
from exercise).
Dietary consultation to help educate the patient the importance of
following a low sodium, low fat diet. Diet planning/shopping should
also be a part of this education.
Education and support to modify risk factors such as cigarette smoking,
high blood pressure, diabetes, high cholesterol, physical inactivity and
obesity.
Teach the importance of limiting or avoiding alcohol intake (An average
of one to two drinks per day for men and one drink per day for
women. A drink is one 12 oz. beer, 4 oz. of wine, 1.5 oz. of 80-proof
spirits, or 1 oz. of 100-proof spirits.) This amount of alcohol is
considered to be drinking in moderation.
Vocational/social education in the attempt to return the patient to work
and normal activities.
Supplying information about physical limitations (excessive exercise,
sexual activity for example).
Education/counseling regarding prescription medication and the
importance of sticking to the routine as well as reporting side effects.
31
Emotional/spiritual support as needed.
Critical care nursing cardiac imad thultheen
Note: Long term success of the prevention of a secondary MI is dependant on
the patient having a good understanding of the role he/she plays after
discharge. Without compliance with all treatment and rehabilitation
interventions (in combination), patients is at great risk of having a second
MI.
32
You might also like
- Case Study Acute Myocardial InfarctionDocument11 pagesCase Study Acute Myocardial InfarctionChristine Elaine Batusin Ilagan91% (23)
- Case Study-Congestive Heart FailureDocument71 pagesCase Study-Congestive Heart FailureKentTangcalagan92% (13)
- Acute Myocardial InfarctionDocument35 pagesAcute Myocardial Infarctionvirnzrobz80% (10)
- Myocardial Infarction Case StudyDocument19 pagesMyocardial Infarction Case Studyapi-312992151No ratings yet
- Surgical Case Study: CranioplastyDocument50 pagesSurgical Case Study: Cranioplastyrhia casinillo100% (8)
- Vascular Surgery MCQsDocument66 pagesVascular Surgery MCQsmohammadeid100% (7)
- Acute Coronary Syndrome - CSDocument91 pagesAcute Coronary Syndrome - CSMASII89% (9)
- Acute Myocardial Infarction - CSDocument49 pagesAcute Myocardial Infarction - CSMASII94% (17)
- Acute Coronary Syndrome - A Case StudyDocument11 pagesAcute Coronary Syndrome - A Case StudyRocel Devilles100% (2)
- Case Study NSTEMIDocument26 pagesCase Study NSTEMIHomework Ping100% (1)
- Acute Myocardial InfarctionDocument20 pagesAcute Myocardial InfarctionDavid Christian CalmaNo ratings yet
- Acute Coronary SyndromeDocument13 pagesAcute Coronary Syndromelavs17100% (1)
- Case Study of A Patient With Ischemic CardiomyopathyDocument33 pagesCase Study of A Patient With Ischemic Cardiomyopathyromeo rivera80% (5)
- Pathophysiology of Myocardial InfarctionDocument2 pagesPathophysiology of Myocardial Infarctionkobe_andre15100% (28)
- Case Study Heart Attack PDFDocument30 pagesCase Study Heart Attack PDFtkgoon634950% (2)
- Congestive Heart FailureDocument18 pagesCongestive Heart FailureAisha Rashed100% (1)
- Case Study (ACS)Document12 pagesCase Study (ACS)Kristel Joy Cabarrubias Acena100% (1)
- Myocardial InfarctionDocument20 pagesMyocardial Infarctionshmily_0810100% (2)
- Myocardial InfarctionDocument21 pagesMyocardial Infarctionanon_516349434No ratings yet
- Pathophysiology Worksheet MIDocument2 pagesPathophysiology Worksheet MIpjbedelNo ratings yet
- 2 Myocardial Infarction Nursing Care Management and Study GuideDocument13 pages2 Myocardial Infarction Nursing Care Management and Study GuideQuijano Gpokskie100% (2)
- Myocardial InfarctionDocument21 pagesMyocardial InfarctionasdnofalNo ratings yet
- Micu Case Study d1Document28 pagesMicu Case Study d1jmarc_2180% (5)
- CASE-STUDY Myocardial InfarctionDocument77 pagesCASE-STUDY Myocardial Infarctionjuodie100% (1)
- Group-1b Myocardial InfarctionDocument39 pagesGroup-1b Myocardial InfarctionJean ReyesNo ratings yet
- CHF Case StudyDocument38 pagesCHF Case StudyMelissa David100% (1)
- Case Study Trauma and Emergency Nursing NRSG 467-SHOCKDocument21 pagesCase Study Trauma and Emergency Nursing NRSG 467-SHOCKErickNabiswa100% (2)
- Myocardial InfarctionDocument16 pagesMyocardial InfarctionCay Sevilla100% (4)
- Cardiac TamponadeDocument3 pagesCardiac Tamponadescremo_xtreme100% (2)
- Myocardial InfarctionDocument45 pagesMyocardial InfarctionGopal SinghNo ratings yet
- Non-St Segment Elevation Myocardial Infarction (Nstemi)Document24 pagesNon-St Segment Elevation Myocardial Infarction (Nstemi)MHIEMHOINo ratings yet
- Modified CaseDocument22 pagesModified CaseAli HawamdeNo ratings yet
- Pathophysiology of Myocardial InfarctionDocument4 pagesPathophysiology of Myocardial InfarctionYhr YhNo ratings yet
- Acute Coronary SyndromeDocument43 pagesAcute Coronary SyndromeMsOrange96% (27)
- Hypovolemic Shock 09Document58 pagesHypovolemic Shock 09Joanne Bernadette Aguilar100% (2)
- CvaDocument170 pagesCvaApril Jumawan ManzanoNo ratings yet
- Myocardial InfarctDocument4 pagesMyocardial InfarctDanelle Harrison, RN100% (1)
- Post Op Cabg CareDocument31 pagesPost Op Cabg CareYeria Rayanti100% (1)
- Aortic Aneurysm - FinalDocument67 pagesAortic Aneurysm - FinalJonathan DiazNo ratings yet
- PneumoniaDocument71 pagesPneumoniafrancis00090100% (1)
- Pulmonary EmbolismDocument5 pagesPulmonary EmbolismNica Duco100% (2)
- PT EducationDocument4 pagesPT Educationapi-248017509No ratings yet
- Cabg 130102113345 Phpapp01Document29 pagesCabg 130102113345 Phpapp01md.dascalescu2486No ratings yet
- HypertensionDocument8 pagesHypertensiongilma100% (3)
- Congestive Heart Failure PathophysiologyDocument16 pagesCongestive Heart Failure PathophysiologyDale LaurenteNo ratings yet
- Case Study On Subacute Subdural HematomaDocument33 pagesCase Study On Subacute Subdural Hematomajarelle bondoc100% (15)
- Acute Myocardial InfarctionDocument17 pagesAcute Myocardial InfarctionRuqowiyah TanjungNo ratings yet
- Myocardial InfarctionDocument18 pagesMyocardial InfarctionYanna Habib-MangotaraNo ratings yet
- "Acute Coronary Syndrome Non ST Elevation Myocardial Infarction, Hypertensive Cardiovascular Disease, Diabetes Mellitus Type 2, and Community Acquired Pneumonia" IntroDocument6 pages"Acute Coronary Syndrome Non ST Elevation Myocardial Infarction, Hypertensive Cardiovascular Disease, Diabetes Mellitus Type 2, and Community Acquired Pneumonia" IntroCarl Elexer Cuyugan AnoNo ratings yet
- Myocardial Infarction: Disscused With Head Supervisor: DR - Yassmeen Ahmed of Pathology Department:prof - Dr.Manal El-NemrDocument23 pagesMyocardial Infarction: Disscused With Head Supervisor: DR - Yassmeen Ahmed of Pathology Department:prof - Dr.Manal El-NemrOmar ShazlyNo ratings yet
- CARDIO (PBL3) - Mohamad Arbian Karim - FMUI20Document10 pagesCARDIO (PBL3) - Mohamad Arbian Karim - FMUI20Mohamad Arbian KarimNo ratings yet
- Prevalence and Risk Factors: HypertensionDocument2 pagesPrevalence and Risk Factors: HypertensionKhristine Anne FabayNo ratings yet
- Myocardial InfarctionDocument18 pagesMyocardial InfarctionMarc Lorenz DucusinNo ratings yet
- General Nursing Science 1 2020 PDFDocument95 pagesGeneral Nursing Science 1 2020 PDFRicardo DomingosNo ratings yet
- Cardiovasculer DiseasesDocument84 pagesCardiovasculer DiseasesrashrikantNo ratings yet
- Disorders of Cardiac FunctionDocument60 pagesDisorders of Cardiac FunctionSaif AliNo ratings yet
- Myocardial Infarction AssignmentDocument23 pagesMyocardial Infarction AssignmentPums100% (6)
- Ischaemic Cardiogenic ShockDocument4 pagesIschaemic Cardiogenic ShocksuckeydluffyNo ratings yet
- Myocardial InfarctionDocument20 pagesMyocardial Infarction* mokhtar !!50% (2)
- NCP Myocard Infarction Group 8Document12 pagesNCP Myocard Infarction Group 8nadyaNo ratings yet
- Mi PDFDocument10 pagesMi PDFReyan AbidinNo ratings yet
- Telecare Collaborative Management of Chronic Pain in Primary 222Document13 pagesTelecare Collaborative Management of Chronic Pain in Primary 222Listya NormalitaNo ratings yet
- Scabies Diagnosis and ManagementDocument5 pagesScabies Diagnosis and ManagementAbdul Rauf ZakariaNo ratings yet
- Dermatitis Herpetiformis: Timo L. Reunala, MDDocument9 pagesDermatitis Herpetiformis: Timo L. Reunala, MDListya NormalitaNo ratings yet
- 3 LOed-bedah Islam 33 - 41Document13 pages3 LOed-bedah Islam 33 - 41Listya NormalitaNo ratings yet
- Cover 24 Chap 1Document1 pageCover 24 Chap 1Listya NormalitaNo ratings yet
- Glaucoma American Journal of OphtalmologyDocument7 pagesGlaucoma American Journal of OphtalmologyListya NormalitaNo ratings yet
- Fisiologi BatukDocument25 pagesFisiologi BatukListya NormalitaNo ratings yet
- Fisiologi BatukDocument25 pagesFisiologi BatukListya NormalitaNo ratings yet
- 24th Block-Trauma & Emergencies: Kegawatan Gastrointestinal Kegawatdaruratan ObsginDocument2 pages24th Block-Trauma & Emergencies: Kegawatan Gastrointestinal Kegawatdaruratan ObsginListya NormalitaNo ratings yet
- Krisis AdrenalDocument18 pagesKrisis AdrenalListya NormalitaNo ratings yet
- Abnormal Labor-ModifiedDocument8 pagesAbnormal Labor-ModifiedListya NormalitaNo ratings yet
- Airway & Breathing Manaj DR BambangDocument50 pagesAirway & Breathing Manaj DR BambangListya NormalitaNo ratings yet
- Antiplatelet, Thrombolitik, Antikoagulan, Vasodilator Referat VaskularDocument23 pagesAntiplatelet, Thrombolitik, Antikoagulan, Vasodilator Referat Vaskularmonyet65No ratings yet
- Scientific Discussion: 1/20 EMEA 2004Document20 pagesScientific Discussion: 1/20 EMEA 2004Donny Rahman KhalikNo ratings yet
- Hemofarm Vademekum Engleska Verzija Za 2013Document143 pagesHemofarm Vademekum Engleska Verzija Za 2013Svet MedicineNo ratings yet
- Naturales CapsiumDocument8 pagesNaturales CapsiummaryNo ratings yet
- Blood Drugs Used For AneamiasDocument7 pagesBlood Drugs Used For AneamiasMaha KhanNo ratings yet
- Dha July 2NDDocument11 pagesDha July 2NDAryan KhanNo ratings yet
- Anticoagulant and Antiplatelet Medications and Dental Procedures ADADocument8 pagesAnticoagulant and Antiplatelet Medications and Dental Procedures ADADeeNo ratings yet
- Anticoagulant Powerpoint PresentationsDocument60 pagesAnticoagulant Powerpoint PresentationsREETHUNo ratings yet
- Complications in Dentoalveolar Surgery PDFDocument37 pagesComplications in Dentoalveolar Surgery PDFmirfanulhaqNo ratings yet
- Practice Guidelines For Acute Care Nurse Practitioners E Book 2Nd Edition PDF Full Chapter PDFDocument53 pagesPractice Guidelines For Acute Care Nurse Practitioners E Book 2Nd Edition PDF Full Chapter PDFpitsonmoedi100% (6)
- Antiplatelet Antikoagulan FibrinolitikDocument15 pagesAntiplatelet Antikoagulan FibrinolitikChimul Lavigne 'L'No ratings yet
- Kaplan Powerpoint Pharm Review Usmle Step 1-: - Flash Cards by Cueflash PDFDocument6 pagesKaplan Powerpoint Pharm Review Usmle Step 1-: - Flash Cards by Cueflash PDFAnonymous OAmXUJFRRR100% (1)
- Lecture 6 Pharma DR N AlhasaniDocument9 pagesLecture 6 Pharma DR N Alhasanialialahmedy24No ratings yet
- Anticoagulatns, Antiplatelets, Fibrinolytics, AntifibrinolyticsDocument2 pagesAnticoagulatns, Antiplatelets, Fibrinolytics, AntifibrinolyticsArvinth Guna SegaranNo ratings yet
- Lacunar Stroke Guide - Causes, Symptoms and Treatment OptionsDocument6 pagesLacunar Stroke Guide - Causes, Symptoms and Treatment OptionsRismanto TorsioNo ratings yet
- Cerebro Vascular DiseasesDocument45 pagesCerebro Vascular DiseasesonyotzNo ratings yet
- Pharmacology Review Drugs That Alter Blood Coagulation PDFDocument6 pagesPharmacology Review Drugs That Alter Blood Coagulation PDFyouyayuNo ratings yet
- Overall Strategy For Treatment of Critical Limb IschemiaDocument83 pagesOverall Strategy For Treatment of Critical Limb IschemiaamurachNo ratings yet
- Dipake 2Document19 pagesDipake 2AriWahyuNo ratings yet
- Abciximab Package InsertDocument22 pagesAbciximab Package InsertbiomedjobhuntNo ratings yet
- Materi - Antiplatelet Pada ACSDocument18 pagesMateri - Antiplatelet Pada ACSTuhfatul UlyaNo ratings yet
- Anticoagulants Preoperative InstructionsDocument3 pagesAnticoagulants Preoperative InstructionsDevaki VisvalingamNo ratings yet
- Transient Ischemic Attacks: Rodney W. Smith, MDDocument58 pagesTransient Ischemic Attacks: Rodney W. Smith, MDNatalija TomićNo ratings yet
- Anticoagulation Guidelines JMDocument32 pagesAnticoagulation Guidelines JMMichael HuntNo ratings yet
- Blood Pharmacology by Dr. Mayur Sayta M 910444Document21 pagesBlood Pharmacology by Dr. Mayur Sayta M 910444funzz100% (1)
- ASRA Guidelines Regional Anaesthesia in Anticoagulated PatientDocument10 pagesASRA Guidelines Regional Anaesthesia in Anticoagulated PatientRizg AlamriNo ratings yet
- Antiplatelet DrugsDocument15 pagesAntiplatelet Drugsngan321100% (1)
- Fibrinolytics, Anti Fibrinolytics and Anti Platelets: Dr. B.K.Bezbaruah Professor Pharmacology Gauhati Medical CollegeDocument46 pagesFibrinolytics, Anti Fibrinolytics and Anti Platelets: Dr. B.K.Bezbaruah Professor Pharmacology Gauhati Medical CollegeBidyut BanerjeeNo ratings yet
- Acute Coronary Syndrome & The PLATO Trial: Ticagrelor vs. ClopidogrelDocument42 pagesAcute Coronary Syndrome & The PLATO Trial: Ticagrelor vs. ClopidogrelDedeSumantraNo ratings yet