Professional Documents
Culture Documents
Econ - Burden Parkinson
Econ - Burden Parkinson
Uploaded by
jpavlovaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Econ - Burden Parkinson
Econ - Burden Parkinson
Uploaded by
jpavlovaCopyright:
Available Formats
Dodel
17/12/08
09:52
Page 11
Economic Burden
The Economic Burden of Parkinsons Disease
a report by
R i c h a r d D o d e l , J e n s - P e t e r R e e s e , M o n i k a B a l z e r and W o l f g a n g H O e r t e l
Abstract
Objective
estimated average of 7,600. Total costs per patient increase with
To evaluate costs and health-related quality of life (HRQoL) in
increased H&Y disease stage, from average cost of 3,400 for
patients with Parkinsons disease (PD) in Europe.
H&Y stage 1 to 15,000 for H&Y stage 5. EQ-5D index score
decreased with increasing disease severity: 0.66 and 0.48 for H&Y
Study Design and Methods
stages 1/2 and 3/4, respectively. Differences in household income
Costs and HRQoL were evaluated in patients with idiopathic PD
also had a distinct relationship with HRQoL score: 0.54 and 0.75
recruited from outpatient departments for movement disorders in
for income <750 and income >1,500, respectively. In terms of
Germany. The generic EQ-5D instrument was used to assess
clinical factors, patients with dementia (0.40 versus 0.61),
HRQoL. Clinical data Hoehn and Yahr (H&Y) stage, Unified
depression (0.57 versus 0.63), pain (0.49 versus 0.62) and
Parkinsons Disease Rating Scale (UPDRS) III and motor and non-
constipation (0.43 versus 0.76) showed the largest differences in
motor symptoms were assessed in detail. Drug costs over the
HRQoL compared with the average.
previous three months were assessed using a questionnaire. PD
medication costs were stratified by H&Y stages. Bivariate
Conclusion
correlations were calculated of the EQ-5D index score and
The results show that PD places a major burden on the individual, the
sociodemographic and clinical outcomes. Statistical significance
family and society. Costs associated with PD increase substantially
was proved by means of t-tests and Kruskall-Wallis tests.
with disease progression, and the majority of costs originate from
outside the formal healthcare system. Owing to the scarcity of
Results
epidemiological and health economic data, cost calculations are
Direct costs per patient range from 2,500 to 13,000, with an
conservative and probably underestimate the true burden of PD.
The economic burden of Parkinsons disease (PD) has become a
into direct medical (e.g. drug costs) and direct non-medical costs (e.g.
very important health topic. From the perspective of a typical
cost of care). Indirect costs are those caused by the disease, and
neurologist, health economics can appear quite dry; however, it is a
usually relate to the patients employment status. Intangible costs are
growing topic in most modern healthcare systems, so doctors should
the hardest to quantify and measure, as suitable instruments are
have at least a minimal understanding of how health economic
lacking. Traditionally, in health economic evaluations only the direct
information is derived.
and indirect costs are included, but there can be a huge difference in
the calculation simply by including or excluding one category of costs.
Starting in Australia in 1993 with the establishment of the Economics
Subcommittee of the Pharmaceutical Benefits Advisory Committee
The gold standard of health economic evaluations is comparative
(PBAC), various authorities worldwide have been set up to analyse the
analysis. There are four different kinds: cost minimisation analysis,
cost-effectiveness of drugs and other medical products. Examples are the
costbenefit analysis, cost-effectiveness analysis and costutility
German Institute for Quality and Efficiency in Health Care (IQWIG),
analysis.1 The first two are rarely used in medicine; the last two are the
established in 2004, and the National Institute for Health and Clinical
most common. The cost-effectiveness analysis compares a monetary
Excellence (NICE), established in 1999 in the UK.
amount with a measurable clinical effect, such as change in blood
pressure, weight, etc., and the result is presented in these units, for
Calculating the Costs
example per mmHg or per kg. The costutility analysis compares the
Costs, according to health economic theory, are categorised as direct,
monetary differences of two interventions with non-monetary outcome,
indirect or intangible1 (see Table 1). Direct costs are those that are
with a typical result being per quality-adjusted life year (QALY) gained
incurred as a direct result of treating the patient and can be divided
or per disability-adjusted life year (DALY) gained, with QALYs being
the most commonly used aggregate. However, there is a large debate as
Corresponding author:
Richard Dodel
PhilippsUniversity Marburg, Germany
E: dodel@med.uni-marburg.de
TOUCH BRIEFINGS 2008
to what could be the best outcome measure for utility analyses.2 Noncomparative studies include the cost-analysis study, where only the
cost of the outcome is considered. If only the burden of the illness is
taken into account, the analysis is called cost of illness analysis.
11
16/12/08
17:04
Page 12
Economic Burden
calculation of an opportunity cost in economics: it looks at the overall
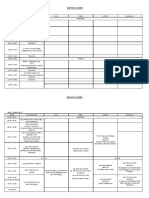
Table 1: Health Economics Distinction
impact of taking a particular decision versus making an alternative
Direct
Medical
Ambulatory/inpatient care
Diagnostics
Therapy
Care
Indirect
Unemployment
Part-time work
Early retirement
Intangible
Dependency
Psychological effects
Pain
choice. It is such a powerful tool that many agencies are adopting it:
IQWIG in Germany, for instance, has stated that decision analysis is
one of its preferred tools for determining cost-effectiveness.
The Macro View
The European Brain Council (EBC) published a study on brain disorders
and their epidemiology in 2005.3 There are around 466 million people
Figure 1: Cost Breakdown for Brain Disease
in Europe, 127 million (27%) of whom have brain disorders (both
neurological and general mental health). If those with co-morbidities
are excluded, that still leaves 104 million people (22%), roughly half of
whom (51.2 million people; 11%) have a neurological condition. The
number with PD is estimated to be around 1.1 million (0.2%).4
The number of patients with PD differs across the various countries. As
of 2004, The Netherlands had the highest percentage of brain
disorders, with around 36% of the population suffering from either a
neurological or a mental disorder (17 and 19%, respectively); Spain
had the lowest at around 19% (10 and 9%, respectively). The reason
for these discrepancies is not known.
In terms of the annual cost of treatment, Germany had the highest
Hospitalisation
Drugs
Outpatient care
expenses for brain disorders, at nearly 1,400 per person in
Social services
Informal care
Other direct costs
2004; Estonia spent the least, at barely 200 per person. There is
Sick leave
Early retirement
Premature death
also a clear correlation with gross domestic product (GDP) in the
Source: Adapted from Andlin-Sobocki et al., 2005.3
different countries.
Where Is the Money Spent?
The public view in most countries is that the main medical expense is
Figure 2: Cost per Patient of Brain Disorders in Europe
doctors salaries, with drug costs second. However, in actual fact 33%
of the total cost associated with a brain disorder is caused by sick leave
40,000
from work (see Figure 1). Early retirement adds a further 7% and
35,000
premature death an additional 7%. Therefore, nearly half of the total
30,000
cost is not directly under the control of neurologists.
25,000
According to the EBC data for 2004, annual spend in Europe on PD
20,000
was 10.7 billion, consisting of 4.6 billion on healthcare costs and
15,000
6.1 billion on direct non-medical costs. This is more than 12% of the
10,000
total spend on neurological diseases in Europe, which was 83.9
Migraine
Anxiety disorders
Addiction
Trauma
Affective disorders
Epilepsy
Parkinsons
Disease
Psychotic disorders
costs, in the case of the latter because they assumed a population over
Dementia
Stroke
billion.3 These data do not include either the intangible or the indirect
Multiple sclerosis
5,000
Tumour
Cost per patient ( 2004)
Dodel
Source: Adapted from Andlin-Sobocki et al., 2005.3
With migraine, for example, indirect
There are also different ways to gather data. It is possible to gather
costs dwarf direct costs by 17:1, a fact
them as field research, for example performing a clinical study
rarely mentioned in public debates.
including economic variables in the protocol. This is usually done in a
phase II or III trial. Alternatively, there is a naturalistic design, for
example as part of a post-marketing study, or the Delphi method,
where a certain number of specialists convene to determine a
consensus on the costs involved. The other way to gather data is
65 years of age and thus already in retirement. This is a critical
through desk-based research. The meta-analysis is a common way to
omission: with migraine, for example, indirect costs dwarf direct costs
pool and analyse published data, but in recent years decision analysis
by 17:1, a fact rarely mentioned in public debates. Nevertheless,
has become the most popular tool. It employs a similar process to the
according to current data the cost per patient of treating PD is close to
12
EUROPEAN NEUROLOGICAL REVIEW VOLUME 3 ISSUE 2 2008 SUPPLEMENT: III INTERNATIONAL FORUM ON ADVANCED PARKINSONS DISEASE
Dodel
16/12/08
17:04
Page 13
The Economic Burden of Parkinsons Disease
the median value of the cost of all brain disorders, where brain
tumours cost society the most and migraines the least (see Figure 2).
Figure 3: Composition of Annual Costs of Treating
Parkinsons Disease in Germany
In order to evaluate the cost and the health-related quality of life
(HRQoL) of patients with PD in Europe, we undertook a study in seven
European countries: Austria, Czech Republic, Italy, Germany, Portugal,
Russia and the UK. Drug costs over the previous three months were
assessed with a questionnaire. The generic EQ-5D instrument was
used to assess HRQoL, while clinical data Hoehn and Yahr (H&Y)
In Germany, treatment for patients
with dyskinesias, at 10,760 per
year, was roughly double that for
patients without.
Direct cost
Drugs
Patients
Indirect costs
Cost RV and PV
NB: RV and PV are special German retirement and care insurance payments.
Source: Adapted from Spottke et al., 2005.6
stage, Unified Parkinsons Disease Rating Scale (UPDRS) III and motor
Figure 4: Distribution of Parkinsons Disease Drug Costs
and non-motor symptoms were retrieved from the EuroPa database.5
The results from this study are currently being analysed and will be
published soon.
The Micro View
The results presented here are derived from a health economics study
that took place in Germany in 20042006, although the results are
assumed to be representative of those found in other major European
countries. The study examined 145 PD patients with an average age of
67 years in different H&Y stages and with a range of UPDRS scores
over three years.6 The researchers used a range of questionnaires in
order to fully understand the HRQoL of all of the participants, as well
as other emotional aspects. Treatment was provided by different
groups from university level through peripheral level down to the
Dopamine agonists
L-Dopa
Antiepileptics
Benzodiazepines
Opioids
Sleep medication
Pain
Iron
Others
community level.7
Results were total annual costs of 20,860 per PD patient. This
consisted of 3,720 in direct costs (excluding medications) and 3,840
in drug costs, accounting for slightly more than one-third of the total
Source: Adapted from Spottke et al., 2005.6
(see Figure 3). The indirect costs are quite high at 6,360 of the total
cost, or slightly less than one-third.
who specialised in PD. The findings of the study show that the average
reimbursement received by these neurologists was 42 per patient
Within direct costs, hospital costs were found to be the largest
over the three months. This ranged from 22.00 for a newly
contributor at 1,420 (38%). All other costs, including for the office-
diagnosed patient at an early stage of PD to 45.78 for an advanced,
based physician, diagnostics, physiotherapy, inpatient rehabilitation,
H&Y 5 patient. These do not appear to be unreasonable amounts.
transportation and walking aids, are less than 1,000 each, and thus
do not represent excessive spending where savings can be made. Of
Costs as Disease Progresses
the drug costs of 3,840, 65% is accounted for by dopamine agonists
During the course of PD costs do change. When analysing the costs by
(see Figure 4). Therefore, high-dose dopaminergic therapies
H&Y stage, several trends become apparent. Indirect costs remain
particularly those including more than one dopamine agonist will
pretty stable over the course of the disease (with an anomalous minor
significantly add to the overall cost.
blip for H&Y 4), but the costs of health insurance and care
(represented
by
PV
and
RV
[Pflegeversicherung
and
One of the claims in Germany is that office-based physicians are too
Rentenversicherung, respectively; these are special German retirement
expensive. In order to properly assess this claim, we undertook an
and care insurance payments] and direct costs) in the advanced
additional three-month study in Berlin of 12 office-based neurologists
disease stages increase disproportionately (see Figure 5).
EUROPEAN NEUROLOGICAL REVIEW VOLUME 3 ISSUE 2 2008 SUPPLEMENT: III INTERNATIONAL FORUM ON ADVANCED PARKINSONS DISEASE
13
16/12/08
17:05
Page 14
Economic Burden
dementia, depression and hallucinations; and autonomic dysfunction,
Figure 5: Parkinsons Disease Costs by Disease Stage
such as loss of bladder control and gastrointestinal complications. In
Cost ( 2006)
50,000
45,000
Germany, treatment for patients with dyskinesias, at 10,760 per year,
40,000
was roughly double that for patients without. Similarly, motor fluctuations
35,000
caused treatment costs to rise to 11,040 from 6,040 at baseline.6
30,000
25,000
With dementia in PD,9 the odds ratio for nursing home placement is
20,000
2.5 times higher than for non-demented PD patients. Meanwhile,
15,000
psychosis in PD raised the odds ratio to 17 times higher than
10,000
baseline.10,11 This difference, measured using the MMSE score, is
5,000
consistent across age groups (see Figure 6). Furthermore, for
0
Average
II
III
IV
demented patients with low MMSE scores, inpatient stay is nearly
doubled on average, while rehabilitation costs are more than tripled.
Indirect costs
Costs to patients
Drugs
Direct costs
PV and RV costs
Interestingly, the result was that PD patients with dementia were no
more likely to visit their physician than those without dementia, but
drug costs were around one-third higher. Similarly, the cost to HRQoL,
Source: Adapted from Spottke et al., 2005.6
for both the patient and the care-giver, is higher when the PD patient
Figure 6: Mini-mental State Examination
Annual cost ()
Dodel
7,000
Parkinsons disease is an expensive
6,000
disorder, a fact that must be faced by
5,000
both the medical community and
4,000
patients to ensure that enough
3,000
funding is available for suitable and
2,000
innovative treatments.
1,000
0
<61
6169
MMSE >25
>69
MMSE <25
has dementia. Autonomic dysfunction does not appear to affect costs,
although quality of life is reduced.6
Summary and Conclusions
Source: Adapted from Spottke et al., 2005.6
PD is an expensive disorder, a fact that must be faced by both the medical
One aspect of PD care that was not covered in the study is the cost
community and patients to ensure that enough funding is available for
incurred when a patient has to leave home and enter institutional care.
suitable and innovative treatments. The indirect costs associated with
There are no data available anywhere that directly relate to these
Parkinsons disease are greater than the direct costs: roughly 50% of the
costs. However, there are data available for Alzheimers disease, which
latter are accounted for by the cost of the drugs themselves. However, as
is assumed to be at least comparable to PD. As with PD, the
a patient develops complications, costs increase.
therapeutic and drug costs for Alzheimers disease are quite low at
the beginning, but when patients reach a mini-mental state
These data largely come from the results of a study undertaken by the
examination (MMSE) state of less than 10, about 9095% of the total
EBC. Overall, the epidemiological and disease-specific data available in
is taken up by care costs.8
most European countries are insufficient for an accurate health economic
assessment. Without these data, the different healthcare systems will not
Costs by Disease Complication
be able to determine the best areas for investment for the different
As illustrated in the article by Jos Obeso, progressive PD brings with it
neurological disorders. It is imperative that more epidemiological and
new complications over time. These include: motor complications, such as
disease-specific data are gathered so that healthcare systems and
dyskinesias and motor fluctuations; psychiatric disorders, including
neurologists are not pushed away from the patient.
1. Meltzer MI, Introduction to health economics for physicians,
Lancet, 2001;358:9938.
2. Smith DM, Brown SL, Ubel PA, Are subjective well-being
measures any better than decision utility measures?, Health
Econ Policy Law, 2008;3(Pt 1):8591.
3. Andlin-Sobocki P, Jnsson B, Wittchen H-U, Olesen J, Costs
of Disorders of the Brain in Europe, Eur J Neurol, 2005;12
(Suppl. 1): iiiv.
4. Olesen J, Baker MG, Freund T, et al., Consensus document
on European brain research, J Neurol Neurosurg Psychiatry,
2006;77(Suppl. 1):i149.
14
5. www.europarkinson.net/html/1/1_over/fs_1over.html
6. Spottke AE, Reuter M, Machat O, et al., Cost of illness and
its predictors for Parkinsons disease in Germany,
Pharmacoeconomics, 2005;23(8):81736.
7. Reuther M, Spottke EA, Klotsche J, et al., Assessing healthrelated quality of life in patients with Parkinsons disease in a
prospective longitudinal study, Parkinsonism Relat Disord,
2007;13(2):10814.
8. Hallauer JF, Schons M, Smala A, Berger K, Costs of medical
treatment of Alzheimer patients in Germany, Gesundh kon
Qual manag, 2000;5:739
9. Hely MA, Reid WG, Adena MA, et al., The Sydney multicenter
study of Parkinsons disease: the inevitability of dementia at
20 years, Mov Disord, 2008;23(6):83744.
10. Aarsland D, Larsen JP, Tandberg E, Laake K, Predictors of
nursing home placement in Parkinsons disease: a
population-based, prospective study, J Am Geriatr Soc,
2000;48(8):93842.
11. Goetz CG, Stebbins GT, Risk factors for nursing home
placement in advanced Parkinsons disease, Neurology,
1993;43(11):22279.
EUROPEAN NEUROLOGICAL REVIEW VOLUME 3 ISSUE 2 2008 SUPPLEMENT: III INTERNATIONAL FORUM ON ADVANCED PARKINSONS DISEASE
You might also like
- Fundamentals of EU Regulatory Affairs 9th EditionDocument681 pagesFundamentals of EU Regulatory Affairs 9th Editioncyrilaaron0406No ratings yet
- Econometrics PaperDocument24 pagesEconometrics PaperPam Ramos0% (1)
- Introduction To PeriodontologyDocument33 pagesIntroduction To PeriodontologyEmine Alaaddinoglu100% (1)
- (13142143 - Folia Medica) Pharmacoeconomics of Bronchial AsthmaDocument9 pages(13142143 - Folia Medica) Pharmacoeconomics of Bronchial AsthmaChristinaNo ratings yet
- The Economic Costs of Disease Related MalnutritionDocument6 pagesThe Economic Costs of Disease Related MalnutritionHusdup NarcisaNo ratings yet
- Euro J of Neurology - 2011 - Linde - The Cost of Headache Disorders in Europe The Eurolight ProjectDocument13 pagesEuro J of Neurology - 2011 - Linde - The Cost of Headache Disorders in Europe The Eurolight Projectnb2dw7y9btNo ratings yet
- NannsDocument9 pagesNannsal jaynNo ratings yet
- A Review of The Costs of ManagingDocument2 pagesA Review of The Costs of ManagingApsopela SandiveraNo ratings yet
- Comparing Hospitals and Health Prices and Volumes Across Countries: A New ApproachDocument22 pagesComparing Hospitals and Health Prices and Volumes Across Countries: A New ApproachAnonymous CgufQ4wiNo ratings yet
- Brettschneider (2014) A Systematic Review of Economic Evaluations of Treatments For Borderline Personality Disorder. PLoS One.Document12 pagesBrettschneider (2014) A Systematic Review of Economic Evaluations of Treatments For Borderline Personality Disorder. PLoS One.daniela opazoNo ratings yet
- Cki 116Document7 pagesCki 116Nurul pattyNo ratings yet
- Cost Heart FailureDocument5 pagesCost Heart FailureMinh Hai TranNo ratings yet
- Economics of Mental Well-Being - Predicting Healthcare Costs and Sickness Benefit TransfersDocument13 pagesEconomics of Mental Well-Being - Predicting Healthcare Costs and Sickness Benefit TransfersZiggi SantiniNo ratings yet
- Literature Review - FinalDocument10 pagesLiterature Review - FinaloscarNo ratings yet
- Economic Burden of Vertigo A Systematic ReviewDocument14 pagesEconomic Burden of Vertigo A Systematic ReviewMartin Ramos AlvaradoNo ratings yet
- Best Buys SummaryDocument12 pagesBest Buys SummaryJASSNARRONo ratings yet
- Cardiac ServicesDocument22 pagesCardiac ServicesAnaid FourevaNo ratings yet
- WNL 0000000000009673 Full1Document20 pagesWNL 0000000000009673 Full1Veloz RedNo ratings yet
- Applying EconomicDocument12 pagesApplying EconomicnurNo ratings yet
- Interoduction CRPDocument8 pagesInteroduction CRPsalons.errands0hNo ratings yet
- NG9FullGuidanceAppendicesA-J 20150601 PDFDocument713 pagesNG9FullGuidanceAppendicesA-J 20150601 PDFJosué Espino RomeroNo ratings yet
- Unhealthy Diets ePDF v1Document114 pagesUnhealthy Diets ePDF v1aryan sharmaNo ratings yet
- Jurnal MigrainDocument7 pagesJurnal MigrainAnie NieNo ratings yet
- Cost of Illne HFDocument11 pagesCost of Illne HFJohan SalimNo ratings yet
- Arterial Hypertension in Poland in 2002: Review ArticleDocument6 pagesArterial Hypertension in Poland in 2002: Review ArticleTautu-Fronea OanaNo ratings yet
- The Impact of Headache in Europe: Principal Results of The Eurolight ProjectDocument11 pagesThe Impact of Headache in Europe: Principal Results of The Eurolight ProjectChristian LamplNo ratings yet
- Hearts and Minds -Сърца и умове-25 обобщава връзката между влошеното психично здраве и сърдечните заболяванияDocument137 pagesHearts and Minds -Сърца и умове-25 обобщава връзката между влошеното психично здраве и сърдечните заболяванияGeorgi IlievNo ratings yet
- The Year in Cardiology 2013: Cardiovascular Disease PreventionDocument6 pagesThe Year in Cardiology 2013: Cardiovascular Disease PreventionVincent LivandyNo ratings yet
- Social and Economic Costs and Health-Related Quality of Life in Stroke Survivors in The Canary Islands, SpainDocument9 pagesSocial and Economic Costs and Health-Related Quality of Life in Stroke Survivors in The Canary Islands, SpainDeudeu Durotun NafisahNo ratings yet
- Measuring Burden of Disease in Estonia To Support Public Health PolicyDocument7 pagesMeasuring Burden of Disease in Estonia To Support Public Health PolicysosoalsoukhniNo ratings yet
- The Economic Cost of Sleep DisordersDocument7 pagesThe Economic Cost of Sleep DisordersjamesteryNo ratings yet
- Eurpub ckr007 FullDocument5 pagesEurpub ckr007 FullEugenio MartinezNo ratings yet
- Management of Traumatic Brain Injury PatientsDocument14 pagesManagement of Traumatic Brain Injury Patientsyayaslaras96No ratings yet
- Chapter30 Economic Impact of DiabetesDocument12 pagesChapter30 Economic Impact of DiabetessimainsusNo ratings yet
- Supplement 399Document8 pagesSupplement 399cuvinhNo ratings yet
- EFNS Guideline 2010 Diagnosis and Management of ADDocument13 pagesEFNS Guideline 2010 Diagnosis and Management of ADDeni Andre AtmadinataNo ratings yet
- Cea Hipertensi 8Document7 pagesCea Hipertensi 8ani rahayuNo ratings yet
- Critical Thinking Assessment - CorrDocument7 pagesCritical Thinking Assessment - CorrMichael NdegwaNo ratings yet
- ECNP Press Release: The Size and Burden of Mental Disorders in Europe (09/2011)Document2 pagesECNP Press Release: The Size and Burden of Mental Disorders in Europe (09/2011)ElJay AremNo ratings yet
- Lancet Austerity and UE HealthDocument9 pagesLancet Austerity and UE HealthBen TotushekNo ratings yet
- The Economic Burden of ObesityDocument13 pagesThe Economic Burden of ObesityNasir Ali100% (1)
- ResearchDocument75 pagesResearchArun AhirwarNo ratings yet
- 2018 Healthatglance Sum enDocument4 pages2018 Healthatglance Sum enLucian SalaNo ratings yet
- Drug-Related Admissions and Hospital-Acquired Adverse Drug Events in Germany: A Longitudinal Analysis From 2003 To 2007 of ICD-10-coded Routine DataDocument9 pagesDrug-Related Admissions and Hospital-Acquired Adverse Drug Events in Germany: A Longitudinal Analysis From 2003 To 2007 of ICD-10-coded Routine DataYuli CartrinaNo ratings yet
- 2011 in The Clinic - EPOCDocument16 pages2011 in The Clinic - EPOCKarla WevarNo ratings yet
- Esclerosis Tuberosa 3Document31 pagesEsclerosis Tuberosa 3Santiago CeliNo ratings yet
- Prevalence of Depression and Anxiety Among ParticiDocument10 pagesPrevalence of Depression and Anxiety Among ParticiAishah FarihaNo ratings yet
- tmpE2CA TMPDocument5 pagestmpE2CA TMPFrontiersNo ratings yet
- Elsevier Article PaperDocument24 pagesElsevier Article Paperjaveriazia97No ratings yet
- Chapter 2 Introduction To PharmacoeconomicsDocument35 pagesChapter 2 Introduction To Pharmacoeconomicshailu tasheNo ratings yet
- Fernandez - 2017 EspañaDocument30 pagesFernandez - 2017 EspañaJuan camiloNo ratings yet
- Anxiety and Depression in Patients With Chronic Obstructive Pulmonary Disease (COPD) - A ReviewDocument6 pagesAnxiety and Depression in Patients With Chronic Obstructive Pulmonary Disease (COPD) - A ReviewArja' WaasNo ratings yet
- PSY21 COST EFFECTIVENESS ANALYSIS OF EMICIZUMAB FOR THE TREATME - 2019 - Value IDocument1 pagePSY21 COST EFFECTIVENESS ANALYSIS OF EMICIZUMAB FOR THE TREATME - 2019 - Value IMichael John AguilarNo ratings yet
- Article 1575090034Document5 pagesArticle 1575090034FitriNo ratings yet
- An Analysis of Clinical Pharmacist Interventions at A Cze - 2022 - General HospiDocument2 pagesAn Analysis of Clinical Pharmacist Interventions at A Cze - 2022 - General Hospijingwen2002No ratings yet
- Podcast IIDocument49 pagesPodcast IINumeratorNo ratings yet
- Osteoarthritis Research Priorities: A Report From A EULAR Ad Hoc Expert CommitteeDocument4 pagesOsteoarthritis Research Priorities: A Report From A EULAR Ad Hoc Expert CommitteeAndriany FirdausNo ratings yet
- Excess Length of Stay and Economic Consequences of Adverse Events in Dutch Hospital PatientsDocument7 pagesExcess Length of Stay and Economic Consequences of Adverse Events in Dutch Hospital PatientsAlessandra Miranda PadillaNo ratings yet
- Direct Costs of Parkinson's Disease in Brazil: A Case StudyDocument8 pagesDirect Costs of Parkinson's Disease in Brazil: A Case StudyIJAERS JOURNALNo ratings yet
- The Economic Burden of Cardiovascular Disease and Hypertension in Low-And Middle-Income Countries: A Systematic ReviewDocument11 pagesThe Economic Burden of Cardiovascular Disease and Hypertension in Low-And Middle-Income Countries: A Systematic ReviewJordán MaulénNo ratings yet
- Essai Contrôlé Randomisé de La Maladie de ParkinsonDocument10 pagesEssai Contrôlé Randomisé de La Maladie de Parkinsonlorit1988No ratings yet
- Pbl-Gin Urine Test (Feme)Document11 pagesPbl-Gin Urine Test (Feme)KarthigaRamanNo ratings yet
- Health Facilities and Services Regulatory Bureau: Republic of The Philippines Department of HealthDocument3 pagesHealth Facilities and Services Regulatory Bureau: Republic of The Philippines Department of Healthal gulNo ratings yet
- SportsMedicine PDHPEDocument29 pagesSportsMedicine PDHPEKobeNo ratings yet
- Salbutamol AcidosisDocument3 pagesSalbutamol AcidosisAccounts OfficerNo ratings yet
- 4 6012518666061482070 PDFDocument347 pages4 6012518666061482070 PDFKhushboo Rana A Scientist100% (1)
- Bricks Intensive Reading - L2 - Word List BDocument16 pagesBricks Intensive Reading - L2 - Word List BNathaniel McleodNo ratings yet
- Hyperemesis GravidarumDocument16 pagesHyperemesis GravidarumArra MayNo ratings yet
- OTC and PRESCRIPTION DRUGS Ppt. (TANTICO)Document10 pagesOTC and PRESCRIPTION DRUGS Ppt. (TANTICO)Ladyfair TanticoNo ratings yet
- Check - List - Form - No - 2 - Registration of Imported - MedicinesDocument1 pageCheck - List - Form - No - 2 - Registration of Imported - Medicines박지원No ratings yet
- HOTEZ - 2014 - Vaccine Diplomacy Historical Perspective and Future DirectionsDocument7 pagesHOTEZ - 2014 - Vaccine Diplomacy Historical Perspective and Future DirectionsRodrigo Torres AlmeidaNo ratings yet
- Leiomyoma Types, Incidence and Clinical Presentation - A Study at A Tertiary Care HospitalDocument6 pagesLeiomyoma Types, Incidence and Clinical Presentation - A Study at A Tertiary Care HospitalIJAR JOURNALNo ratings yet
- Jadwal AcaraDocument2 pagesJadwal AcaraElok Faiqotul UmmaNo ratings yet
- Bioanalysis NotesDocument7 pagesBioanalysis NoteskeerthiNo ratings yet
- Sedation in Pediatric Dentistry: January 2019Document8 pagesSedation in Pediatric Dentistry: January 2019Ina Vetrila100% (1)
- Handbook of Otolaryngology Head - and - Neck - SurgeryDocument2 pagesHandbook of Otolaryngology Head - and - Neck - Surgeryyoela13No ratings yet
- Allergic Rhinitis History and Presentation PDFDocument6 pagesAllergic Rhinitis History and Presentation PDFJimena LopezNo ratings yet
- Modalities of Cancer TreatmentDocument65 pagesModalities of Cancer TreatmentBspharma 2E100% (1)
- A Lens To Understand Sanitation Workers and Their Health Status in IndiaDocument3 pagesA Lens To Understand Sanitation Workers and Their Health Status in IndiaRejesh BoseNo ratings yet
- Record Storage SafekeepingDocument3 pagesRecord Storage Safekeepingilog ndp100% (1)
- CBT For ADHD in Adults: Cognitive Behavioral Therapy For ADD SymptomsDocument6 pagesCBT For ADHD in Adults: Cognitive Behavioral Therapy For ADD Symptomsrico rubenNo ratings yet
- HAEMORRHAGE Seminar-IDocument25 pagesHAEMORRHAGE Seminar-ISimran Josan100% (1)
- Aida Mujakovic CVDocument5 pagesAida Mujakovic CVHaris AjkunićNo ratings yet
- SOAP Note Directions & AbbreviationsDocument4 pagesSOAP Note Directions & AbbreviationsTyler KingNo ratings yet
- ICICI Lombard - Andromeda DimpeshDocument3 pagesICICI Lombard - Andromeda DimpeshDimpesh AshiyaniNo ratings yet
- Case Presentation DengueDocument3 pagesCase Presentation DengueLindel Assley Turqueza100% (1)
- Vi Psa Pres Common Eye Conditions Aug10 3.08.29 PMDocument58 pagesVi Psa Pres Common Eye Conditions Aug10 3.08.29 PMSarthak KabiNo ratings yet
- What Is AphasiaDocument4 pagesWhat Is AphasiaValentina DubNo ratings yet
- Acute ScrotumDocument38 pagesAcute ScrotumShochibul KahfiNo ratings yet