Professional Documents
Culture Documents
9 PDF
9 PDF
Uploaded by
jeka222Copyright:
Available Formats
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5820)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (845)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (898)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (349)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Medical Medium Life-Changing Foods: Save Yourself and The Ones You Love With The Hidden Healing Powers of Fruits & Vegetables - Anthony WilliamDocument5 pagesMedical Medium Life-Changing Foods: Save Yourself and The Ones You Love With The Hidden Healing Powers of Fruits & Vegetables - Anthony Williamwecatane12% (17)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Ern Baxter - Thy Kingdom ComeDocument20 pagesErn Baxter - Thy Kingdom ComeAussiedler77100% (1)
- Beadwork - November 2015 PDFDocument84 pagesBeadwork - November 2015 PDFIoan Cristian Popescu100% (24)
- Kantar Worldpanel 5 Key FMCG Trends in Vietnam 2023 ENDocument25 pagesKantar Worldpanel 5 Key FMCG Trends in Vietnam 2023 ENbrianNo ratings yet
- eCTD Guidance v4 0-20160422-FinalDocument62 pageseCTD Guidance v4 0-20160422-FinalvinayNo ratings yet
- 2012 01 30 BAM PresentationDocument19 pages2012 01 30 BAM PresentationJoão GomesNo ratings yet
- Acccob3 k36 Business Case Group 3 1Document13 pagesAcccob3 k36 Business Case Group 3 1Aaron HuangNo ratings yet
- The Cotton Industry in The Philippines: ' Country StatementDocument8 pagesThe Cotton Industry in The Philippines: ' Country StatementJocelle AlcantaraNo ratings yet
- DOPO - Productivity Meets PrecisionDocument4 pagesDOPO - Productivity Meets PrecisionRamakrishna MamidiNo ratings yet
- Solution Manual For Illustrated Anatomy of The Head and Neck 5th by FehrenbachDocument8 pagesSolution Manual For Illustrated Anatomy of The Head and Neck 5th by FehrenbachxewazixNo ratings yet
- Dce Brochure EnglishDocument2 pagesDce Brochure EnglishDamian RampersadNo ratings yet
- Prinsipal Kode Produk Nama ProdukDocument40 pagesPrinsipal Kode Produk Nama ProdukjihanvrpNo ratings yet
- 10 Deflection-Castigliano TheoremDocument40 pages10 Deflection-Castigliano TheoremGhaffar Laghari100% (1)
- Makerere Research FormatDocument7 pagesMakerere Research FormatMurice ElaguNo ratings yet
- Viscosity-1 Viscometer-2 Relation Between Viscosity &temperature-3 Vogel Equation-4 Programming ofDocument71 pagesViscosity-1 Viscometer-2 Relation Between Viscosity &temperature-3 Vogel Equation-4 Programming ofDr_M_SolimanNo ratings yet
- AP300Document2 pagesAP300Wislan LopesNo ratings yet
- ASTER Night-Time Thermal Infrared Data: Interpreting Subsurface Features From High Resolution DataDocument4 pagesASTER Night-Time Thermal Infrared Data: Interpreting Subsurface Features From High Resolution DataRoman Ignacio Escobar PizarroNo ratings yet
- The Pacific War 1941-45: Empire of The SunDocument56 pagesThe Pacific War 1941-45: Empire of The SunIvánNo ratings yet
- P e - First-Quarter-Exams 1st-SemDocument7 pagesP e - First-Quarter-Exams 1st-SemJieann BalicocoNo ratings yet
- I Sing of Arms and of A Man Medial Epicondylosis and The Sexual Division of Labour in Prehistoric EuropeDocument8 pagesI Sing of Arms and of A Man Medial Epicondylosis and The Sexual Division of Labour in Prehistoric EuropeFelipe ÁngelNo ratings yet
- Soal UAS 2023 KELAS 9Document5 pagesSoal UAS 2023 KELAS 9MASDALYLA TINENDUNGNo ratings yet
- Practical 06:-Write A Program in C To Translate 2D and 3D ObjectDocument5 pagesPractical 06:-Write A Program in C To Translate 2D and 3D ObjectKhan.aliNo ratings yet
- 12-Efka - FA 4644 PDFDocument2 pages12-Efka - FA 4644 PDFAniket PatelNo ratings yet
- WSET Systematic Approack To Tasting Wine & Spirits - XLSX - WINEDocument1 pageWSET Systematic Approack To Tasting Wine & Spirits - XLSX - WINEIl MulinaioNo ratings yet
- List NotesDocument27 pagesList NotesMohit MauryaNo ratings yet
- He Was The Secret Blacksmith Who Made Divine Weapons For Common PlayersDocument14 pagesHe Was The Secret Blacksmith Who Made Divine Weapons For Common PlayersisraqreqNo ratings yet
- Transfer Pricing of Tivo and Airbag Division: RequiredDocument7 pagesTransfer Pricing of Tivo and Airbag Division: RequiredajithsubramanianNo ratings yet
- Paste Copy FTTXDocument8 pagesPaste Copy FTTXfttxjpr JaipurNo ratings yet
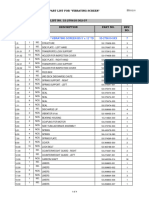
- 0 1 NO. Ga. of Vibrating Screen Bs 5' X 12' TD 53-270610-5XX 7Document4 pages0 1 NO. Ga. of Vibrating Screen Bs 5' X 12' TD 53-270610-5XX 7Benjamin MurphyNo ratings yet
- Interpreting Fits and Tolerances:: - by William B MoringDocument14 pagesInterpreting Fits and Tolerances:: - by William B Moringwillmors31No ratings yet
9 PDF
9 PDF
Uploaded by
jeka222Original Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
9 PDF
9 PDF
Uploaded by
jeka222Copyright:
Available Formats
Egypt. J. Histol. Vol. 33, No. 4, Dec.
, 2010: 709 - 721
(ISSN: 1110 - 0559)
Original Article
Histological and Immunohistochemical Study on Rat Spleen in
Experimentally Induced Liver Cirrhosis
Dina M. Radwan, Hanan A. Amin and Ashraf M. F. Kamel
Histology Department, Faculty of Medicine, Cairo University
ABSTRACT
Introduction: The present study aimed to examine the histological changes in the spleen of rats with liver cirrhosis,
and to determine the immunohistochemical expression of endothelial nitric oxide synthase (e-NOS), and its upstream
effectors; tumor necrosis factor (TNF-) and vascular endothelial growth factor (VEGF).
Materials and Methods: Twenty male adult albino rats were divided into two equal groups. The first was control.
In the second group, liver cirrhosis was induced by intraperitoneal (ip) injection of thioacetamide 200 mg/kg twice
weekly for 12 weeks. Splenic index (spleen weight / body weight) was determined and the spleens of rats which
developed liver cirrhosis were subjected to the following stains: hematoxylin and eosin (H & E), silver impregnation,
and immunostaining with specific antibodies for e-NOS, TNF- and VEGF. Quantitative assessments were carried out
using image analyzer with statistical analysis of the results.
Results: Splenic sections of cirrhotic rats showed in addition to congestion of venous sinuses, significant increase in
reticular fibers in capsule and trabeculae as well as throughout the red pulp. The percentages of red pulp and fibrous
trabeculae areas were significantly higher in cirrhotic rats, while the percentage of the white pulp areas was significantly
smaller. Immunohistochemical staining of both e-NOS and TNF- in spleen sections of group II rats were significantly
lower than control, while VEGF immunostaining was significantly higher.
Conclusion: Splenomegaly in liver cirrhosis was not only congestive but there was also significant increase of reticular
fibers, red pulp area and angiogenesis. Moreover, nitric oxide (NO) reduction resulting from suppression of e-NOS and
TNF- seen in this study contributed to the increased volume of the spleen.
Key Words: cirrhosis; thioacetamide; spleen; e-NOS;
TNF, VEGF; silver impregnation.
Corresponding author: Ashraf M F Kamel
Tel.: 0111765111
E-mail: ashrafkamel@cu.edu.eg
INTRODUCTION
Splenomegaly is often detected in patients with liver
cirrhosis and portal hypertension with a prevalence of
60-65%1,2. Splenic congestion due to portal hypertension
has been reported to play a part in this increase in spleen
size3. However, splenomegaly in cirrhosis cannot be
considered as a mere consequence in the rise in portal vein
pressure (PVP). Such congestion cannot be considered as
the only cause of the enlarged spleen in liver cirrhosis,
since no relationship was found between the spleen size
and PVP4-7 or the degree of oesophageal varices8.
that have been implicated as potential mediators of
portal hypertension. Among them, nitric oxide (NO)
has received the greatest attention13. NO is a potent
vasodilator and there are three isoforms of NO synthese
(NOS): Inducible NOS (iNOS), endothelial NOS
(e-NOS) and neuronal NOS (nNOS)14,15. The respective
roles of iNOS and e-NOS, in intrahepatic vasoregulation
have been well studied in cirrhotic liver13.
After liver transplantation, only a slight decrease in
spleen size is detected despite the dramatic decrease in
portal vein pressure probably due to a recovery of the
congestive component only9-12. This confirmed that in
cirrhosis splenic hemodynamics is characterized both
by congestion and tissue hyperplasia, the later probably
being at least partially, irreversible3.
Alterations in eNOS-derived NO synthesis in the
intrahepatic microcirculation and in the splanchnic
and systemic vasculature are strikingly opposite. Liver
cirrhosis is associated with endothelial dysfunction
and deficiency of endothelial NO release resulting in
enhanced vasoconstriction, increased intrinsic vascular
tone16. In contrast, splanchnic and systemic vasculature
exhibit endothelial NO overproduction and arterial
vasodilation leading to hyperdynamic circulation17-23.
Recently in liver cirrhosis, it has been shown that
the spleen is a source of several vasoactive substances
This alteration of e-NOS activity has been
reported to be mediated by abnormalities in TNF-
63 (1228-2010)
709
Dina M. Radwan et al.
and VEGF expression via the Akt signaling pathway
in portal hypertension24-27. To our knowledge, e-NOS
immunohistochemical expression in the enlarged spleen
of liver cirrhosis has not been reported.
B. Tumor Necrosis Factor (TNF , Neo Markers,
Lab Vision Corporation).
C. Vascular Endothelial Growth Factor (VEGF, Neo
Markers, Lab Vision Corporation).
aim of the study
The immunohistochemical staining was done
following the avidin -biotin- peroxidase complex
(ABC) method. Diaminobenzidine (DAB) served as
the chromogen. The slides were counterstained with
hematoxylin. Negative control sections were prepared
by adding phosphate buffer solution instead of the
corresponding primary antibody with all other steps
taken in the same fashion31.
The aim of the present study was to investigate
the
histological
changes
and
examine
the
immunohistochemical expression of e-NOS, TNF- and
VEGF in the spleen of rats with liver cirrhosis.
MATERIALS AND METHODS
The study was conducted at the Animal House of
Kasr Al Aini School of Medicine in accordance with the
guidelines for the care and use of laboratory animals.
Quantitative Morphometric Study:
Images were processed and analysed using computerbased image analysis software (Leica QWin 500;
Imaging Systems, Cambridge UK) with to measure the
area percent of the following:
It included twenty adult male albino rats (180-200
grams). Animals were housed with free access to food
and water. They were randomly allocated to two equal
groups:
A. Red pulp.
B. White pulp.
C. Red pulp/white pulp (RP/WP) index calculated from
the values of both pulps32.
D. Fibrous trabeculae.
E. Reticular fibers.
F. Endothelial nitric oxide synthase immunoreactivity.
G. Tumor Necrosis Factor immunoreactivity.
H. Vascular
Endothelial
Growth
Factor
immunoreactivity.
Group I (Control Group): Received saline
(intraperitoneal injection) twice weekly for 12 weeks and
served as control.
Group II (Cirrhosis Group): Liver cirrhosis
was induced by intraperitoneal (i.p.) injection of
Thioacetamide (TAA) (200 mg/kg body weight) twice a
week for 12 weeks28.
Thioacetamide powder was purchased from Sigma
Chemical Company St. Louis, Mo., USA and dissolved
in 0.9% saline.
Ten randomly selected low power fields from each
slide were analysed and expressed as a mean area percent
of total area.
All rats were sacrificed after 12 weeks under
isoflurane anaesthesia and body weights were recorded.
Liver and spleen were excised.
Statistical Analysis:
Computer software package SPSS 15.0 was used
in the analysis. For quantitative variables, mean
(as a measure of central tendency), standard deviation
(as a measure of variability) were presented.
Spleen Index: The spleen was weighed by an
electronic balance and the spleen index was calculated
according to the following formula:
Spleen index =spleen weight (g)/ body weight (g)29.
Independent Samples T-test was used to estimate
differences in quantitative variables between the
control and experimental group. It was considered to be
statistically significant if a P value was less <0.05
Spleen specimens were fixed in 10% buffered
formalin, embedded in paraffin, cut into 5 m serial
sections and subjected to the following stains:
RESULTS
1. Hematoxylin and Eosin (H & E) stain for histological
analysis.
2. Silver impregnation for detection of reticular fibers
fibers30.
3. Immunohistochemical staining using a primary anti
serum to:
I-Histological and Immunohistochemical Results:
The liver histology of the group II rats confirmed the
occurrence of liver cirrhosis with disorganization of the
normal lobular pattern accompanied by the formation
of well-defined pseudolobules (Fig. 1-a). Thick fibrous
connective tissue septa were seen bridging the portal
areas and frequently extending into the lobules (Fig. 1-b).
A. Endothelial nitric oxide synthase (e-NOS, Neo
Markers, Lab Vision Corporation).
710
Histological and Immunohistochemical Study on Rat Spleen in Experimentally Induced Liver Cirrhosis
H & E stained control spleen sections, consisted of
discrete lymphoid masses (white pulp) and embedded
in highly vascular matrix (red pulp). The white pulp
was subdivided into Peri-Arteriolar Lymphatic Sheath
(PALS), follicular and marginal zones. The PALS could be
identified as the dark region around the central arteriole.
Some lymph follicles exhibited germinal centers. The red
pulp was composed of meshwork of splenic cords and
several venous sinuses. Hemosiderinladen macrophages
were also present. Supporting trabeculae containing
smooth muscles were seen (Fig. 2). On the other hand,
examination of group II- sections, showed obvious
congestion of spleen tissues with markedly distended
venous sinuses. Thickening of splenic trabeculea was
also noted (Fig. 3).
The percentage of the areas occupied by the red pulp
was greater (P<0.05) in cirrhotic rats than in control rats
as was the case for both the fibrous trabeculae (P<0.005)
and the RP/WP index (P<0.005) (Table 2 Fig. 13).
Conversely, the percentage of the areas occupied by the
white pulp, was smaller in cirrhotic rats than in control
rats (P<0.005).
The area percent of silver stained reticular fibers was
greater (P<0.005) in cirrhotic rats than in control rats
(Table 3, Fig. 14-a).
The area percent of e-NOS immunoexpression
was significantly decreased (by 53%, P<0.005) in
cirrhotic rats compared with the area percent in control
rats (Table 3, Fig. 14-b). Similarly, the area percent of
TNF- immunostaining was significantly decreased
(by 45%, P<0.005) in cirrhotic rats than control rats
(Table 3, Fig. 14-c). In contrast, the area percent of VEGF
immunoreactivity was increased (by 30 %, P<0.005) in
cirrhotic rats than in control rats (Table3, Fig 14-d). Thus,
the increase in the area percent of VEGF immunostaining
in the cirrhotic rats was smaller than the decrease in the
area percent TNF- immunoreactivity.
Silver staining technique employed to demonstrate
the reticular architecture of the control spleen showed the
capsule and perivascular supporting tissue which provided
a framework ramifying throughout the section in the red
pulp. The reticular skeleton was almost absent in the
center of the white pulp nodules but was well developed
at their margins and around the central arteriole (Fig. 4).
With silver impregnation, an irregular fiber pattern was
visible in group II sections with increased reticular fibers
manifested as thickened capsule and trabeculae. Dense
meshwork was present throughout the red pulp (Fig. 5).
Table 1: Mean body weights, spleen weights and Spleen
weight / body weight indices of control and TAA treated rats:
Examination of e-NOS immunostained sections,
revealed that, red pulp had strong immunoreactivity
seen as brown cytoplasmic staining within sinus lining
endothelial cells with almost negatively stained white
pulp (Fig. 6). Compared to control sections, e-NOS
sections of group II showed weaker immunoractivity
within red pulp and in sinus lining cells. White pulp
exhibited negative reaction (Fig. 7).
Body
weight (g)
Spleen
weight (g)
Spleen weight
/ body weight
(%)
Control
(meanSD)
226.36.36
0.480.05
0.210.02
Cirrhosis
(meanSD)
1996*
1.260.05*
0.630.03*
* P<0.005 vs control rats which is highly statistically significant
Table 2: Area percent of white pulp, red pulp, index of red
pulp / white pulp and fibrous trabeculae of control and TAA
treated rats:
TNF- immunostained control sections showed
positive cytoplasmic reaction within mononuclear
cells in the red pulp with negatively stained white pulp
(Fig. 8). Decreased immunoreactivity was seen in group
II sections with almost similar distribution (Fig. 9).
Control
(meanSD)
Cirrhosis
(meanSD)
In VEGF-immunostained control sections, the positive
reaction was noted within red pulp only in endothelial
cells (Fig. 10). Examination of group II sections revealed
marked increase in immunoreactivity identified as brown
cytoplasmic staining within endothelial cells lining the
venous sinuses (Fig. 11).
White Pulp
Red Pulp
RP / WP
index
Fibrous
Trabeculae
21.463.67
71.444.44
3.450.85
7.111.70
11.052.13**
78.102.85*
7.381.82**
10.852.38**
* P<0.05 vs control rats which is statistically significant
** P<0.005 vs control rats which is highly statistically significant
Table 3: mean area percent of silver impregnation, e-NOS,
TNF- and VEGF in sections of rats of the control and TAA
treated groups:
II-Morphomertical and Statistical Results:
The body weights of cirrhotic rats were lower than
control rats (P<0.005) (Table 1, Fig. 12-a). On the other
hand, the spleen weights of cirrhotic rats were higher
than control rats (P<0.005) (Table 1), while the spleen
indices (Spleen weight / body weight) of cirrhotic
rats were higher than those of control rats (P<0.005)
(Table 1, Fig. 12-b).
Area %
Reticular
Fibers
Area %
e-NOS
Area %
TNF-
Area %
VEGF
Control
(meanSD)
30.378.58
12.234.08
16.834.05
8.171.21
Cirrhosis
(meanSD)
44.076.99*
5.741.51*
9.202.13*
11.822.96*
* P<0.005 vs their respective control rats which is highly statistically significant
711
Dina M. Radwan et al.
Fig. 1: Photomicrographs of a section of the liver of group II rats showing: Fig. 2-b: Hemosiderinladen macrophages (arrow head) are seen within
the red pulp (RP). Supporting trabeculae (T) containing smooth muscles
a- Disorganized lobular pattern with the formation of pseudolobules.
H & E x400
H & E x100 are also noted.
Fig. 1-b: Fibrous connective tissue septa (arrow) are noted bridging the Figure (3): Photomicrographs of splenic sections of group II showing:
portal areas and extending into the lobules. Masson trichrome stain x100 a- Marked congestion of red pulp (RP). Note the almost normal appearance
of the white pulp (WP) with central arteriole (CA).
H & E x200
Fig. 2: Photomicrographs of control splenic sections showing:
a- Lymphoid masses (white pulp) embedded in highly vascular matrix
(red pulp) [RP] with several venous sinuses (arrow head). The white
pulp has dark region around the central arteriole (CA) representing the Fig. 3-b: Markedly congested (C) and distended venous sinuses (arrow
peri-arteriolar lymphatic sheath (PALS). Germinal centers (GC) could be head) and thickened trabeculae (T).
H & E x 400
H & E x200
identified in some follicles.
712
Histological and Immunohistochemical Study on Rat Spleen in Experimentally Induced Liver Cirrhosis
Fig. 4: Photomicrographs of control splenic sections showing:
Fig. 5: Photomicrographs of splenic sections of group II showing:
a- Capsule (arrow head) and perivascular supporting trabeculae (arrow).
a-
Irregular fiber pattern and thickened capsule (arrowhead) and
Silver impregnation x40 trabeculae (arrow).
Silver impregnation x40
Fig. 4-b: Reticular skeleton is almost absent in the center of the white pulp
nodules (WP) but well developed at their margins.
Silver impregnation x100
Fig. 5-b: Marked thickening of trabeculae (arrow) containing blood
vessels
Silver impregnation x100
Fig 4-c: Reticular framework is ramifying throughout the red pulp [RP]
(arrow head).
Silver impregnation x400
Fig. 5-c: Dense reticular meshwork is present throughout the red pulp
(RP) (arrow head)
Silver impregnation x400
713
Dina M. Radwan et al.
Fig. 6: Photomicrographs of control splenic sections, showing:
a- Red pulp (RP) with strong immunoreactivity with almost negatively
stained white pulp (WP).
e-NOS immunostaining x200
Fig. 7- b: obvious decrease in positive staining within sinus lining cells
(boxed areas)
e-NOS immunostaining x400
Fig. 6- b: Brown cytoplasmic staining within sinus lining endothelial
cells (boxed areas) with thickened trabeculae (arrow).
e-NOS immunostaining x400
Fig. 8: Photomicrographs of control splenic sections showing:
a-
positive brown staining within red pulp (arrow) while white
pulp (WP) is negatively stained.
TNF- immunostaining x200
Fig. 7: Photomicrographs of splenic sections of group II showing:
a- decreased immunoreactivity within red pulp (RP) with negatively
stained white pulp (WP).
e-NOS immunostaining x200
Fig. 8- b: positive brown reaction within mononuclear cells (arrow)
TNF- immunostaining x400
present in the red pulp (RP).
714
Histological and Immunohistochemical Study on Rat Spleen in Experimentally Induced Liver Cirrhosis
Fig. 9: Photomicrographs of splenic sections of group II showing:
a- Decreased immunoreactivity within red pulp (RP) with negatively
stained white pulp (WP).
TNF- immunostaining x200
Fig. 10- b: positive brown reaction within endothelial cells lining venous
sinuses (arrow)
VEGF immunostaining x400
Fig. 11: Photomicrographs of splenic sections of group II showing:
a-
marked increase in immunoreactivity (arrow) within red pulp
Fig. 9- b: Obvious decrease in positive staining within mononuclear cells
(RP) with negatively stained white pulp (WP).
TNF- immunostaining x400
in the red pulp (RP).
VEGF immunostaining x200
Fig. 11- b: increased positive staining within endothelial cells lining
Fig. 10: Photomicrographs of control splenic sections showing:
positive brown staining (arrow) within the red pulp (RP) while venous sinuses (arrow) in the red pulp (RP).
a-
VEGF immunostaining x400
white pulp (WP) is negatively stained.
VEGF immunostaining x200
715
Dina M. Radwan et al.
Fig. 12-a: mean body weights of control and cirrhotic rats.
Fig. 14: Histograms comparing control and cirrhotic spleen sections as
regards: (a): mean area percent of silver stained reticular fibers.
Fig. 12-b: mean spleen indices (spleen weight / body weight) of control
and cirrhotic rats.
Fig. 14-b: mean area percent of e-NOS immunostaining,
Fig. 13: mean area percent occupied by the white pulp, red pulp and
fibrous trabeculae as well as the RP/WP index in spleen sections of both
cirrhotic and control rats.
Fig. 14-c: mean area percent of TNF- immunostaining,
716
Histological and Immunohistochemical Study on Rat Spleen in Experimentally Induced Liver Cirrhosis
This agreed with a previous study on spleens of 34
patients with advanced hepatosplenic schistosomiasis32.
However, other scientists found an increase
in the white pulp volume and thereby suggested a
possible immunologic involvement in the genesis of
splenomegaly37.
In our study the white pulp areas were found less
in cirrhotic rats than in control rats probably because it
was a percentage and not an absolute measurement and
perhaps the increase in red pulp and fibrous trabeculae
percentages was much more and masked any increase in
white pulp area that might have occurred.
Furthermore, the present results revealed significantly
increased VEGF immunoreactivity within endothelial
cells lining the venous sinuses in the spleen of cirrhotic rats.
Thus, angiogenesis and increased vascular permeability
may also be involved in the spleen enlargement. This
finding agreed with previous reports34,38,39.
Fig. 14-d: mean area percent of VEGF immunoreactivity.
DISCUSSION
Splenomegaly resulting from TAA-induced liver
cirrhosis was investigated in adult male albino rats. It
was found that animals in the cirrhotic group presented
a statistically significant smaller increase in BW than
control animals. The spleen indices of cirrhotic rats
were statistically higher than those of control rats. This
coincided with the results of a previous research33.
Since tissue hypoxia was an important stimulus for
VEGF expression40, another possible mechanism for
splenomegaly would be the hypoxic status with splenic
congestion. However, further studies are needed to fully
elucidate it.
The main finding in the present study was splenic
congestion with markedly distended venous sinuses in
the spleens of cirrhotic rats.
Therefore, even by only considering the histological
data, splenomegaly in cirrhosis cannot be simply
classified as congestive, but should be defined as
congestive-hyperplastic.
In the present study, sections of group II showed
significantly weaker e-NOS immunoractivity within red
pulp and in sinus lining cells and negative immunostaining
in the white pulp. These findings were in agreement with
a report that showed e-NOS reduction in the spleen by
Western blot34.
It was long established that spleen enlargement in liver
cirrhosis was considered to be congestive splenomegaly34.
However, such congestion could not be considered as the
only cause of the enlarged spleen in liver cirrhosis, since
no relationship was found between the spleen size and
PVP 4-7,34 and since complete resolution of splenomegaly
had never been reported after liver transplantation9-12.
NO generated by e-NOS was settled to be an important
regulator of the microcirculation at the sinusoidal level
by being a vaso-relaxing agent41-43.
In the present study by silver impregnation, the
reticular fibers significantly increased in group II splenic
sections manifested by thickening of the capsule and
trabeculae with dense reticular meshwork throughout the
red pulp.
Additionally, NO was found to have antiproliferative
and antifibrogenic activities44-47. Therefore, insufficient
production of NO could contribute to increased portal
pressure not only by increasing vascular tone but also by
increasing the fiber formation. This concept may have
therapeutic implications in portal hypertension. Recently,
NO received most attention in gene therapy for the
treatment of portal hypertension targeting its regulatory
system48.
These results were in agreement with previous studies
which had demonstrated that splenomegaly exhibited not
only pooling of blood in the red pulp, but also increased
reticular fibers that later evolved into diffuse fibrosis35,36.
Additionally, it was observed that the percentage of
the areas occupied by the red pulp and fibrous trabeculae
were significantly higher in cirrhotic rats compared to
control rats, while the percentage of the areas occupied
by the white pulp, was significantly smaller.
Moreover, NO derived from e-NOS was found
to contribute to angiogenesis, in addition to VEGF,
however, the exact roles of each remained to be defined49.
717
Dina M. Radwan et al.
In the present study, the splenic TNF-
immunoexpression was significantly decreased in
cirrhotic rats.
10.
TNF- is considered a mediator of NO release via
the PI 3-kinase Akt signaling pathway50-54. Inhibition of
TNF- synthesis was found to decrease NO synthesis55-57.
Thus, the findings of the present study indicated that
the decreased TNF- may be a direct contributor to the
decreased NO release in the spleen of cirrhotic rats as
previously suggested34.
11.
CONCLUSION
12.
In conclusion, splenomegaly in liver cirrhosis was
not totally congestive, but also involved hyperplasia of
reticular fibers and red pulp, as well as angiogenesis
verified by high VEGF expression. Moreover, suppression
of e-NOS and TNF- decreased NO. Studying the
role of NO and the factors influencing its level in the
hemodynamics of the spleen in cases of liver cirrhosis
may lead to a new therapeutic potential in the future.
13.
14.
REFERENCES
15.
1.
2.
3.
4.
5.
6.
7.
8.
9.
Zhang J, Ling Y, Luo B, Tang L, Ryter SW, Stockard CR,
Grizzle WE and Fallon MB. (2003): Analysis of pulmonary
heme oxygenase-1 and nitric oxide synthase alterations in
experimental hepatopulmonary syndrome. Gastroenterology
Nov; 125(5):1441-1451.
Chen YC, Gines P, Yang J, Summer SN, Falk S, Russell
NS and Schrier RW. (2004): Increased vascular heme
oxygenase-1 expression contributes to arterial vasodilation
in experimental cirrhosis in rats. Hepatology Apr; 39(4):
1075-1087.
Bolognesi M, Merkel C, Sacerdoti D, Nava V and Gatta
A. (2002): Role of spleen enlargement in cirrhosis with portal
hypertension. Dig.Liver Dis. ; 34(2):144-150.
Witte CL, Witte MH, Renert W and Corrigan JJ,Jr. (1974):
Splenic circulatory dynamics in congestive splenomegaly.
Gastroenterology Sep; 67(3):498-505.
Rozenblit G, Del Guercio LR, Savino J, Cerabona T, Policastro
A and McPhee M. (1996): Splenic venous hypertension
presenting as variceal hemorrhage caused by portal hypertension.
J.Am.Coll.Surg. Jan; 182(1):63-68.
Merkel C, Gatta A, Arnaboldi L and Zuin R. (1985): Splenic
haemodynamics and portal hypertension in patients with liver
cirrhosis and spleen enlargement. Clin.Physiol. Dec; 5(6):
531-539.
Shah SH, Hayes PC, Allan PL, Nicoll J and Finlayson
ND. (1996): Measurement of spleen size and its relation to
hypersplenism and portal hemodynamics in portal hypertension
due to hepatic cirrhosis. Am.J.Gastroenterol. Dec; 91(12):
2580-2583.
Sheth SG, Amarapurkar DN, Chopra KB, Mani SA and Mehta
PJ. (1996): Evaluation of splenomegaly in portal hypertension.
J.Clin.Gastroenterol. Jan; 22(1):28-30.
Bolognesi M, Sacerdoti D, Bombonato G, Angeli P, Gerunda
16.
17.
18.
19.
20.
21.
22.
23.
24.
718
G, Merenda R, Volpin R, Iemmolo R and Gatta A. (1998):
Splenic impedance indices: A useful method to monitor patients
after liver transplantation? Hepatology Mar; 27(3):674-678.
Pozzato C, Marzano L, Botta A, Anania RM and Uslenghi
CM. (1998): Splenomegalia e ipersplenismo nei pazienti
cirrotici prima e dopo trapianto ortotopico del fegato.
[Splenomegaly and hypersplenism in cirrhotic patients before
and after orthotopic liver transplantation]. Radiol.Med.
(Torino) Apr; 95(4):349-352.
Piscaglia F, Zironi G, Gaiani S, Mazziotti A, Cavallari A,
Gramantieri L, Valgimigli M and Bolondi L. (1999): Systemic
and splanchnic hemodynamic changes after liver transplantation
for cirrhosis: A long-term prospective study. Hepatology Jul;
30(1):58-64.
DArienzo A, Manguso F, Cimino L, Scaglione G, Celentano L,
Vicinanza G, Parrilli G and Mattera D. (1998): Could spleensize determine long-term thrombocytopenia following orthotopic
liver transplant even after reversal of portal hypertension?
Ital.J.Gastroenterol.Hepatol. Aug; 30(4):441-442.
Rockey D. (1997): The cellular pathogenesis of portal
hypertension: Stellate cell contractility, endothelin and nitric
oxide. Hepatology Jan; 25(1):2-5.
Wiest R and Groszmann RJ. (1999): Nitric oxide and portal
hypertension: Its role in the regulation of intrahepatic and
splanchnic vascular resistance. Semin.Liver Dis. ; 19(4):411-426.
Farzaneh Far R and Moore K. (2001): Nitric oxide and the
liver. Liver Jun; 21(3):161-174.
Wiest R and Groszmann RJ. (2002): The paradox of nitric
oxide in cirrhosis and portal hypertension: Too much, not enough.
Hepatology Feb; 35(2):478-491.
Cahill PA, Foster C, Redmond EM, Gingalewski C, Wu Y and
Sitzmann JV. (1995): Enhanced nitric oxide synthase activity in
portal hypertensive rabbits. Hepatology Aug; 22(2):598-606.
Cahill PA, Redmond EM, Hodges R, Zhang S and Sitzmann
JV. (1996): Increased endothelial nitric oxide synthase activity in
the hyperemic vessels of portal hypertensive rats. J.Hepatol. Sep;
25(3):370-378.
Martin PY, Xu DL, Niederberger M, Weigert A, Tsai P, St
John J, Gines P and Schrier RW. (1996): Upregulation of
endothelial constitutive NOS: A major role in the increased
NO production in cirrhotic rats. Am.J.Physiol. Mar; 270
(3 Pt 2):F494-F499.
Morales Ruiz M, Jimenez W, Perez Sala D, Ros J, Leivas
A, Lamas S, Rivera F and Arroyo V. (1996): Increased nitric
oxide synthase expression in arterial vessels of cirrhotic rats with
ascites. Hepatology Dec; 24(6):1481-1486.
Niederberger M, Gines P, Martin PY, Tsai P, Morris K,
McMurtry I and Schrier RW. (1996): Comparison of vascular
nitric oxide production and systemic hemodynamics in cirrhosis
versus prehepatic portal hypertension in rats. Hepatology Oct;
24(4):947-951.
Gadano AC, Sogni P, Yang S, Cailmail S, Moreau R, Nepveux
P, Couturier D and Lebrec D. (1997): Endothelial calciumcalmodulin dependent nitric oxide synthase in the in vitro
vascular hyporeactivity of portal hypertensive rats. J.Hepatol.
Mar; 26(3):678-686.
Liu H, Song D and Lee SS. (1999): Increased nitric oxide synthase
expression in aorta of cirrhotic rats. Life Sci. ; 64(19):1753-1759.
Kawanaka H, Jones MK, Szabo IL, Baatar D, Pai R, Tsugawa
Histological and Immunohistochemical Study on Rat Spleen in Experimentally Induced Liver Cirrhosis
25.
26.
27.
28.
29.
30.
31.
32.
33.
34.
35.
36.
37.
K, Sugimachi K, Sarfeh IJ and Tarnawski AS. (2002):
Activation of eNOS in rat portal hypertensive gastric mucosa
is mediated by TNF-alpha via the PI 3-kinase-Akt signaling
pathway. Hepatology Feb; 35(2):393-402.
Barsacchi R, Perrotta C, Bulotta S, Moncada S, Borgese N
and Clementi E. (2003): Activation of endothelial nitric-oxide
synthase by tumor necrosis factor-alpha: A novel pathway
involving sequential activation of neutral sphingomyelinase,
phosphatidylinositol-3 kinase and Akt. Mol.Pharmacol. Apr;
63(4):886-895.
Tazi KA, Moreau R, Herve P, Dauvergne A, Cazals Hatem
D, Bert F, Poirel O, Rabiller A and Lebrec D. (2005):
Norfloxacin reduces aortic NO synthases and proinflammatory
cytokine up-regulation in cirrhotic rats: Role of Akt signaling.
Gastroenterology Jul; 129(1):303-314.
Abraldes JG, Iwakiri Y, Loureiro Silva M, Haq O, Sessa WC
and Groszmann RJ. (2006): Mild increases in portal pressure
upregulate vascular endothelial growth factor and endothelial
nitric oxide synthase in the intestinal microcirculatory bed,
leading to a hyperdynamic state. Am.J.Physiol.Gastrointest.Liver
Physiol. May; 290(5):G980-G987.
Hori N, Okanoue T, Sawa Y, Mori T and Kashima K.
(1993): Hemodynamic characterization in experimental liver
cirrhosis induced by thioacetamide administration. Dig.Dis.Sci.
; 38(12):2195-2202.
Xia Z, Wang G, Wan C, Liu T, Wang S, Wang B and Cheng
R. (2010): Expression of NALP3 in the spleen of mice with
portal hypertension. J.Huazhong Univ.Sci.Technology Med.Sci.
; 30(2):170-172.
Puchtler H and Waldrop FW. (1978): Silver impregnation
methods for reticulum fibers and reticulin: A re-investigation
of their origins and specificity. Histochemistry Sep 15; 57(3):
177-187.
Bancroft JD and Cook HC. (1994):Immunohistochemistry.In:
Bancroft JD and Cook HC. Manual of histological techniques
and their diagnostic application.2nd ed.: Churchill Livingstone.
p.263-325
Freitas CR, Barbosa AA,Jr, Fernandes AL and Andrade ZA.
(1999): Pathology of the spleen in hepatosplenic schistosomiasis.
Morphometric evaluation and extracellular matrix changes. Mem.
Inst.Oswaldo Cruz Nov-Dec; 94(6):815-822.
Mendez Lopez M, Mendez M, Sanchez Patan F, Casado I,
Aller MA, Lopez L, Corcuera MT, Alonso MJ, Nava MP,
Arias J and Arias JL. (2007): Partial portal vein ligation plus
thioacetamide: A method to obtain a new model of cirrhosis and
chronic portal hypertension in the rat. J.Gastrointest.Surg. Feb;
11(2):187-194.
Yamaguchi S, Kawanaka H, Yoshida D, Maehara Y and
Hashizume M. (2007): Splenic hemodynamics and decreased
endothelial nitric oxide synthase in the spleen of rats with liver
cirrhosis. Life Sci. May 8; 80(22):2036-2044.
Manenti A, Botticelli A, Gibertini G and Botticelli L. (1993):
Experimental congestive splenomegaly: Histological observations
in the rat. Pathologica Nov-Dec; 85(1100):721-724.
Ruehl Fehlert C, Hartmann E and Rinke M. (2008):
Reactive and proliferative changes of splenic reticulum
cells of rats investigated with special staining methods and
immunohistochemistry. Exp.Toxicol.Pathol. ; 59(5):281-290.
Re G, Casali AM, Cavalli D, Guida G, Cau R and Cavalli
38.
39.
40.
41.
42.
43.
44.
45.
46.
47.
48.
49.
50.
51.
52.
719
G. (1986): Histometric analysis of white pulp arterial vessels in
congestive splenomegaly. Appl.Pathol. ; 4(1-2):98-103.
Cavalli G, Re G and Casali AM. (1984): Red pulp arterial
terminals in congestive splenomegaly. A morphometric study.
Pathol.Res.Pract. Jul; 178(6):590-594.
Fernandez M, Vizzutti F, Garcia Pagan JC, Rodes J and Bosch
J. (2004): Anti-VEGF receptor-2 monoclonal antibody prevents
portal-systemic collateral vessel formation in portal hypertensive
mice. Gastroenterology ; 126(3):886-894.
Ferrara N, Gerber HP and LeCouter J. (2003): The biology of
VEGF and its receptors. Nat.Med. Jun; 9(6):669-676.
Moncada S, Palmer RM and Higgs EA. (1991): Nitric oxide:
Physiology, pathophysiology and pharmacology. Pharmacol.Rev.
Jun; 43(2):109-142.
Kawada N, Tran Thi TA, Klein H and Decker K. (1993): The
contraction of hepatic stellate (Ito) cells stimulated with vasoactive
substances. Possible involvement of endothelin 1 and nitric oxide
in the regulation of the sinusoidal tonus. Eur.J.Biochem. Apr 15;
213(2):815-823.
Rockey DC and Chung JJ. (1995): Inducible nitric oxide
synthase in rat hepatic lipocytes and the effect of nitric oxide on
lipocyte contractility. J.Clin.Invest. Mar; 95(3):1199-1206.
Garg UC and Hassid A. (1989): Nitric oxide-generating
vasodilators and 8-bromo-cyclic guanosine monophosphate
inhibit mitogenesis and proliferation of cultured rat vascular
smooth muscle cells. J.Clin.Invest. May; 83(5):1774-1777.
Radomski MW, Palmer RM and Moncada S. (1990): An
L-arginine/nitric oxide pathway present in human platelets
regulates
aggregation.
Proc.Natl.Acad.Sci.U.S.A.
Jul;
87(13):5193-5197.
Casini A, Ceni E, Salzano R, Biondi P, Parola M, Galli A,
Foschi M, Caligiuri A, Pinzani M and Surrenti C. (1997):
Neutrophil-derived superoxide anion induces lipid peroxidation
and stimulates collagen synthesis in human hepatic stellate cells:
Role of nitric oxide. Hepatology Feb; 25(2):361-367.
Failli P, DeFranco RM, Caligiuri A, Gentilini A, Romanelli
RG, Marra F, Batignani G, Guerra CT, Laffi G, Gentilini P
and Pinzani M. (2000): Nitrovasodilators inhibit platelet-derived
growth factor-induced proliferation and migration of activated
human hepatic stellate cells. Gastroenterology Aug; 119(2):
479-492.
Bansal MB and Friedman SL. (2005): Future Treatments:
Antifibrotic agents, nitric oxide donors and gene therapy in the
treatment of portal hypertension.In: Sanyal AJ and Shah VH.
Portal hypertension: Pathobiology, evaluation and treatment
(clinical gastroenterology).1st ed.: Humana Press. p.485-503
Shergill U, Das A, Langer D, Adluri R, Maulik N and Shah VH.
(2010): Inhibition of VEGF- and NO-dependent angiogenesis
does not impair liver regeneration. Am.J.Physiol.Regul.Integr.
Comp.Physiol. ; 298(5):R1279-R1287.
Kilbourn RG and Belloni P. (1990): Endothelial cell production
of nitrogen oxides in response to interferon gamma in combination
with tumor necrosis factor, interleukin-1 or endotoxin. J.Natl.
Cancer Inst. May 2; 82(9):772-776.
Diez Ruiz A, Tilz GP, Gutierrez Gea F, Gil Extremera B, Murr
C, Wachter H and Fuchs D. (1995): Neopterin and soluble
tumor necrosis factor receptor type I in alcohol-induced cirrhosis.
Hepatology Apr; 21(4):976-978.
Lopez Talavera JC, Merrill WW and Groszmann RJ.
Dina M. Radwan et al.
(1995): Tumor necrosis factor alpha: A major contributor to the
hyperdynamic circulation in prehepatic portal-hypertensive rats.
Gastroenterology Mar; 108(3):761-767.
53. Lee FY, Lu RH, Tsai YT, Lin HC, Hou MC, Li CP, Liao TM,
Lin LF, Wang SS and Lee SD. (1996): Plasma interleukin-6
levels in patients with cirrhosis. Relationship to endotoxemia,
tumor necrosis factor-alpha and hyperdynamic circulation.
Scand.J.Gastroenterol. May; 31(5):500-505.
54. Panes J, Perry MA, Anderson DC, Muzykantov VR, Carden
DL, Miyasaka M and Granger DN. (1996): Portal hypertension
enhances endotoxin-induced intercellular adhesion molecule 1
up-regulation in the rat. Gastroenterology Mar; 110(3):866-874.
55. Lopez Talavera JC, Cadelina G, Olchowski J, Merrill W and
Groszmann RJ. (1996): Thalidomide inhibits tumor necrosis
factor alpha, decreases nitric oxide synthesis and ameliorates the
hyperdynamic circulatory syndrome in portal-hypertensive rats.
Hepatology Jun; 23(6):1616-1621.
56. Ohta M, Tarnawski AS, Itani R, Pai R, Tomikawa M,
Sugimachi K and Sarfeh IJ. (1998): Tumor necrosis factor alpha
regulates nitric oxide synthase expression in portal hypertensive
gastric mucosa of rats. Hepatology ; 27(4):906-913.
57. Sztrymf B, Rabiller A, Nunes H, Savale L, Lebrec D, Le
Pape A, de Montpreville V, Mazmanian M, Humbert M and
Herv P. (2004): Prevention of hepatopulmonary syndrome
and hyperdynamic state by pentoxifylline in cirrhotic rats. Eur.
Respir.J. ; 23(5):752-758.
720
Histological and Immunohistochemical Study on Rat Spleen in Experimentally Induced Liver Cirrhosis
:
.
:
( ) .
: :
200/ 12 .
( / ) :
.
: (
)
.
.
.
:
.
.
.
721
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5820)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (845)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (898)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (349)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Medical Medium Life-Changing Foods: Save Yourself and The Ones You Love With The Hidden Healing Powers of Fruits & Vegetables - Anthony WilliamDocument5 pagesMedical Medium Life-Changing Foods: Save Yourself and The Ones You Love With The Hidden Healing Powers of Fruits & Vegetables - Anthony Williamwecatane12% (17)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Ern Baxter - Thy Kingdom ComeDocument20 pagesErn Baxter - Thy Kingdom ComeAussiedler77100% (1)
- Beadwork - November 2015 PDFDocument84 pagesBeadwork - November 2015 PDFIoan Cristian Popescu100% (24)
- Kantar Worldpanel 5 Key FMCG Trends in Vietnam 2023 ENDocument25 pagesKantar Worldpanel 5 Key FMCG Trends in Vietnam 2023 ENbrianNo ratings yet
- eCTD Guidance v4 0-20160422-FinalDocument62 pageseCTD Guidance v4 0-20160422-FinalvinayNo ratings yet
- 2012 01 30 BAM PresentationDocument19 pages2012 01 30 BAM PresentationJoão GomesNo ratings yet
- Acccob3 k36 Business Case Group 3 1Document13 pagesAcccob3 k36 Business Case Group 3 1Aaron HuangNo ratings yet
- The Cotton Industry in The Philippines: ' Country StatementDocument8 pagesThe Cotton Industry in The Philippines: ' Country StatementJocelle AlcantaraNo ratings yet
- DOPO - Productivity Meets PrecisionDocument4 pagesDOPO - Productivity Meets PrecisionRamakrishna MamidiNo ratings yet
- Solution Manual For Illustrated Anatomy of The Head and Neck 5th by FehrenbachDocument8 pagesSolution Manual For Illustrated Anatomy of The Head and Neck 5th by FehrenbachxewazixNo ratings yet
- Dce Brochure EnglishDocument2 pagesDce Brochure EnglishDamian RampersadNo ratings yet
- Prinsipal Kode Produk Nama ProdukDocument40 pagesPrinsipal Kode Produk Nama ProdukjihanvrpNo ratings yet
- 10 Deflection-Castigliano TheoremDocument40 pages10 Deflection-Castigliano TheoremGhaffar Laghari100% (1)
- Makerere Research FormatDocument7 pagesMakerere Research FormatMurice ElaguNo ratings yet
- Viscosity-1 Viscometer-2 Relation Between Viscosity &temperature-3 Vogel Equation-4 Programming ofDocument71 pagesViscosity-1 Viscometer-2 Relation Between Viscosity &temperature-3 Vogel Equation-4 Programming ofDr_M_SolimanNo ratings yet
- AP300Document2 pagesAP300Wislan LopesNo ratings yet
- ASTER Night-Time Thermal Infrared Data: Interpreting Subsurface Features From High Resolution DataDocument4 pagesASTER Night-Time Thermal Infrared Data: Interpreting Subsurface Features From High Resolution DataRoman Ignacio Escobar PizarroNo ratings yet
- The Pacific War 1941-45: Empire of The SunDocument56 pagesThe Pacific War 1941-45: Empire of The SunIvánNo ratings yet
- P e - First-Quarter-Exams 1st-SemDocument7 pagesP e - First-Quarter-Exams 1st-SemJieann BalicocoNo ratings yet
- I Sing of Arms and of A Man Medial Epicondylosis and The Sexual Division of Labour in Prehistoric EuropeDocument8 pagesI Sing of Arms and of A Man Medial Epicondylosis and The Sexual Division of Labour in Prehistoric EuropeFelipe ÁngelNo ratings yet
- Soal UAS 2023 KELAS 9Document5 pagesSoal UAS 2023 KELAS 9MASDALYLA TINENDUNGNo ratings yet
- Practical 06:-Write A Program in C To Translate 2D and 3D ObjectDocument5 pagesPractical 06:-Write A Program in C To Translate 2D and 3D ObjectKhan.aliNo ratings yet
- 12-Efka - FA 4644 PDFDocument2 pages12-Efka - FA 4644 PDFAniket PatelNo ratings yet
- WSET Systematic Approack To Tasting Wine & Spirits - XLSX - WINEDocument1 pageWSET Systematic Approack To Tasting Wine & Spirits - XLSX - WINEIl MulinaioNo ratings yet
- List NotesDocument27 pagesList NotesMohit MauryaNo ratings yet
- He Was The Secret Blacksmith Who Made Divine Weapons For Common PlayersDocument14 pagesHe Was The Secret Blacksmith Who Made Divine Weapons For Common PlayersisraqreqNo ratings yet
- Transfer Pricing of Tivo and Airbag Division: RequiredDocument7 pagesTransfer Pricing of Tivo and Airbag Division: RequiredajithsubramanianNo ratings yet
- Paste Copy FTTXDocument8 pagesPaste Copy FTTXfttxjpr JaipurNo ratings yet
- 0 1 NO. Ga. of Vibrating Screen Bs 5' X 12' TD 53-270610-5XX 7Document4 pages0 1 NO. Ga. of Vibrating Screen Bs 5' X 12' TD 53-270610-5XX 7Benjamin MurphyNo ratings yet
- Interpreting Fits and Tolerances:: - by William B MoringDocument14 pagesInterpreting Fits and Tolerances:: - by William B Moringwillmors31No ratings yet