Professional Documents
Culture Documents
Tuberculosis: WHO Global Tuberculosis Report 2014
Tuberculosis: WHO Global Tuberculosis Report 2014
Uploaded by
blueicelandOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Tuberculosis: WHO Global Tuberculosis Report 2014
Tuberculosis: WHO Global Tuberculosis Report 2014
Uploaded by
blueicelandCopyright:
Available Formats
TUBERCULOSIS
WHO Global Tuberculosis
Report 2014
37 million lives saved
45% decline
Fragile progress in MDR-TB
between 2000 and 2013 through
effective diagnosis and treatment
in TB mortality rate and 41%
decline in TB prevalence since 1990
diagnosis and treatment but widening
gaps in treatment coverage could
compromise gains
TB SITUATION AND ACCESS TO CARE
EXTERNAL
Tuberculosis
(TB) FINANCING
is contagious IS
andCRITICAL
airborne. ItTO
ranks as the
second
of death from a single infectious
FILLleading
GAPS cause
AND ACCELERATE
agent,
after the human immunodeficiency virus (HIV).
PROGRESS
TB BURDEN
9 million people fell ill with TB in 2013, including 1.1 million
cases among people living with HIV.
In 2013, 1.5 million people died from TB, including 360 000
among people who were HIV-positive.
510 000 women died from TB in 2013, including 180 000
among women who were HIV-positive. Of the overall TB
deaths among HIV-positive people, 50% were among women.
TB is one of the top killers of women of reproductive age.
An estimated 550 000 children became ill with TB and
80 000 children who were HIV-negative died of TB in 2013.
The TB mortality rate has decreased 45% since 1990.
TB CARE
Access to TB care has expanded substantially since the
start of this millennium. Between 2000 and 2013, 37 million
lives were saved through effective diagnosis and treatment.
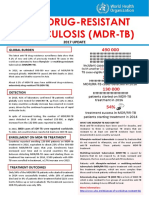
MULTIDRUG-RESISTANT TB
Globally in 2013, an estimated 480 000 people developed
multidrug-resistant TB (MDR-TB) and there were an
estimated 210 000 deaths from MDR-TB.
The number of people diagnosed with MDR-TB tripled
between 2009 and 2013, and reached 136 000 worldwide. This
was equivalent to 45% of the estimated MDR-TB cases among
notified TB patients. Progress in the detection of drug-resistant
TB has been facilitated by the use of new rapid diagnostics.
A total of 97 000 patients were started on MDR-TB treatment in
2013, a three-fold increase compared with 2009. However, 39
000 patients were on waiting lists, and the gap between
diagnosis and treatment widened between 2012 and 2013 in
several countries.
Extensively drug-resistant TB (XDR-TB) has been reported
by 100 countries in 2013. On average, an estimated 9% of
people with MDR-TB have XDR-TB.
NEW DIAGNOSTICS
Xpert MTB/RIF, a rapid molecular diagnostic test, is being
rapidly adopted by countries to detect TB and rifampicinresistant TB. By end June 2014, 3 269 testing machines and
7.5 million test cartridges had been procured by 108 of the
145 countries eligible for concessional prices.
In 2013, 5.7 million newly diagnosed cases were notified to
national TB programmes. Therefore about 3 million people
with TB were missed, either because they were not
diagnosed or because they were diagnosed but not reported.
More than 50 companies are involved in the development of
TB diagnostics.
TB/HIV CO-INFECTION
In 2013, 48% of TB patients globally had a documented HIV
test result. In the African region that has the highest TB/HIV
burden, three out of four TB patients knew their HIV status.
There are 10 new or re-purposed anti-TB drugs in late
phases of clinical development. In the last two years, two new
drugs have been approved for the treatment of MDR-TB under
specific conditions: bedaquiline and delamanid.
Globally, 70% of the TB patients known to be living with HIV
in 2013 were started on antiretroviral therapy (ART).
There are currently 15 vaccine candidates in clinical trials.
In 2013, 5.5 million people enrolled in HIV care were
screened for TB, up from 4.1 million in 2012.
Of the people newly enrolled in HIV care in 2013, 0.6 million
were provided with isoniazid preventive therapy.
RESEARCH AND DEVELOPMENT
FINANCING FOR TB CARE AND CONTROL
2013
and
2015
to US$for
8 billion
per year to the
US$Between
8 billion
per
year
is up
needed
a full response
is needed
in low- and
middle-income
countries, with
a
global
TB epidemic
in lowand middle-income
countries
by
funding
of up to US$
year. per year. The
2015,
with gap
a funding
gap 3ofbillion
US$ per
2 billion
amount excludes resources required for research and develInternational
funding
is especially
critical
opment,
which aredonor
estimated
at about
US$ 2 billion
pertoyear.
sustain recent gains and make further progress in
WHO Global Tuberculosis Report 2014
Supplement
DRUG-RESISTANT TUBERCULOSIS
SURVEILLANCE & RESPONSE
ANTI-TB DRUG RESISTANCE SURVEILLANCE
This special supplement to the Global Tuberculosis Report
2014 marks the 20th anniversary of the Global Project on AntiTuberculosis Drug Resistance Surveillance and the TB
Supranational Reference Laboratory Network.
It is the oldest and largest project on surveillance of antimicrobial drug resistance (AMR) worldwide.
There is impressive progress in surveillance coverage. By
2014, data on drug resistance were available for 144 countries,
which collectively have 95% of the worlds population and TB
cases. This is a major increase compared with 19941999
when data were available for only 35 countries with 20% of the
worlds population and 16% of the global TB burden.
By 2013, data on trends in drug resistance were available for
96 countries. Analysis of trends focused on the period
20082013 suggests that globally, the proportion of new cases
with MDR-TB was 3.5% in 2013. This has not changed compared with recent years.
As a pathfinder with two decades of experience to draw upon,
the Global Project on Anti-Tuberculosis Drug Resistance
Surveillance is a model for scaling up AMR surveillance for
other infectious diseases.
MDR-TB POLICY AND RESPONSE
EXTERNAL
IS over
CRITICAL
Surveillance
of TBFINANCING
drug resistance
the last TO
two decades
GAPSand
AND
ACCELERATE
hasFILL
informed
guided
the response to the MDR-TB
epidemic.
WHO has been issuing guidance on MDR-TB
PROGRESS
prevention, diagnosis and care since 1996.
There is progress in the MDR-TB response: 136 000 cases of
MDR-TB were detected in 2013, up from 52 825 cases
detected in 2009. The number of MDR-TB cases enrolled on
treatment went up from 30 500 in 2009 to 97 000 in 2013.
Key challenges in the MDR-TB response include: growing
gaps between numbers detected and numbers started on
treatment; poor treatment outcomes due to health system
weaknesses; lack of effective regimens; and insufficient
funding including for research. These barriers must be urgently
addressed.
Two new drugs for the treatment of MDR-TB have been
approved over 2013-2014. Further, novel drug regimens for
shortened treatment of drug-susceptible and/or drug-resistant
TB, including new or re-purposed drugs, are under
investigation.
Five priority actions from prevention to cure are needed to
address the MDR-TB epidemic.These are outlined below:
Five priority actions to address the global MDR-TB crisis
PREVENT THE DEVELOPMENT OF DRUG RESISTANCE THROUGH
HIGH QUALITY TREATMENT OF DRUG-SUSCEPTIBLE TB
Prevent MDR-TB as a first priority.
EXPAND RAPID TESTING AND DETECTION OF DRUGRESISTANT TB CASES
Scale up rapid testing and detection of all MDR-TB cases.
PROVIDE IMMEDIATE ACCESS TO EFFECTIVE TREATMENT AND
PROPER CARE
Ensure prompt access to appropriate MDR-TB care, including adequate supplies of quality drugs and
scaled-up country capacity to deliver services.
PREVENT TRANSMISSION THROUGH INFECTION CONTROL
Implement appropriate TB infection control measures to minimize the risk of disease transmission.
This remains one of the most neglected components of TB prevention and care.
$$$
INCREASE POLITICAL COMMITMENT WITH FINANCING
Underpin and sustain the MDR-TB response through high level political commitment, strong
leadership across multiple governmental sectors, ever-broadening partnerships, and financing for
care and research.
The WHO Global TB Programme together with WHO regional and country offices: develops policies, strategies and standards; supports the efforts of WHO Member States; measures progress
towards TB targets and assesses national programme performance, financing and impact; promotes research; and facilitates partnerships, advocacy and communication.
World Health Organization 2014
You might also like
- Schalms Veterinary Hematology 7Th Edition Marjory B Brooks All ChapterDocument67 pagesSchalms Veterinary Hematology 7Th Edition Marjory B Brooks All Chapterefrain.blair179100% (13)
- Electronic Prescriptions For Controlled SubstancesDocument335 pagesElectronic Prescriptions For Controlled SubstancesJames Lindon100% (1)
- Lone WolfDocument286 pagesLone WolfAmoo Mayowa IsraelNo ratings yet
- Soc 621 Final PaperDocument16 pagesSoc 621 Final Paperapi-478028340No ratings yet
- Multi Drug ResistenDocument2 pagesMulti Drug ResistenNurul W.ANo ratings yet
- MDR TB FactsheetDocument2 pagesMDR TB FactsheetfaradillaNo ratings yet
- Tuberculosis: Key FactsDocument5 pagesTuberculosis: Key FactsIdris IkhsanNo ratings yet
- Contemporary Data On TB Epidemiology by Nwokotubo Beulah 2Document26 pagesContemporary Data On TB Epidemiology by Nwokotubo Beulah 2Beulah AlexNo ratings yet
- Mutidrug Resistant TuberculosisDocument2 pagesMutidrug Resistant Tuberculosistummalapalli venkateswara raoNo ratings yet
- Global Fact Sheet 2012 TBDocument2 pagesGlobal Fact Sheet 2012 TBbellamajNo ratings yet
- Gtbr2016 Executive SummaryDocument5 pagesGtbr2016 Executive SummaryihsansiregarNo ratings yet
- gtbr2016 Executive Summary PDFDocument5 pagesgtbr2016 Executive Summary PDFfandyNo ratings yet
- Epidemiology of Tuberculosis - UpToDateDocument33 pagesEpidemiology of Tuberculosis - UpToDateCentro de salud El quincheNo ratings yet
- TheUnion DR TB GuideDocument2 pagesTheUnion DR TB GuideDhani KurniawanNo ratings yet
- New Developments in Tuberculosis Diagnosis and TreatmentDocument15 pagesNew Developments in Tuberculosis Diagnosis and TreatmentannewidiatmoNo ratings yet
- Multidrug-Resistant Tuberculosis (MDR-TB) Is Defined As TB That Is Resistant To BothDocument4 pagesMultidrug-Resistant Tuberculosis (MDR-TB) Is Defined As TB That Is Resistant To Bothsanny_sundariNo ratings yet
- The War On TBDocument5 pagesThe War On TBSuresh KakkarNo ratings yet
- Surveillance Evaluation Report of Tuberculosis in District Bhawalpur-2018 by DR Ammara TahirDocument22 pagesSurveillance Evaluation Report of Tuberculosis in District Bhawalpur-2018 by DR Ammara TahirSantosh WadhwaniNo ratings yet
- TUBERCULOSISDocument4 pagesTUBERCULOSISLâm NguyễnNo ratings yet
- Health Related Millennium Development Goals Part IDocument24 pagesHealth Related Millennium Development Goals Part IGudegna GemechuNo ratings yet
- TuberculosisDocument6 pagesTuberculosisANGELINE CHRYSTABELNo ratings yet
- Multidrug-Resistant Tuberculosis (MDR-TB) : 2012 UpdateDocument2 pagesMultidrug-Resistant Tuberculosis (MDR-TB) : 2012 UpdateRobert MontgomeryNo ratings yet
- What Is Multidrug-Resistant Tuberculosis (MDR-TB) and How Do We Control It?Document2 pagesWhat Is Multidrug-Resistant Tuberculosis (MDR-TB) and How Do We Control It?Dvica SarahNo ratings yet
- The Global Tuberculosis EpidemicDocument2 pagesThe Global Tuberculosis EpidemicAkshaya KuganNo ratings yet
- Shibani Chapter IDocument9 pagesShibani Chapter IShibani KiskuNo ratings yet
- Recent Developments in The Diagnosis and Management of TuberculosisDocument8 pagesRecent Developments in The Diagnosis and Management of TuberculosisRhahahaNo ratings yet
- BY Dr. Tahmina AzharDocument71 pagesBY Dr. Tahmina Azharscribdnotes123No ratings yet
- TB Dots Program 11Document28 pagesTB Dots Program 11Mark SamonteNo ratings yet
- Mjhid 6 1 E2014070Document8 pagesMjhid 6 1 E2014070Khoiril AnwarNo ratings yet
- Tuberculosis: Infection and TransmissionDocument7 pagesTuberculosis: Infection and TransmissionMonica AgapitoNo ratings yet
- Diosana, Jezelle B. PSY 1Y2-5Document3 pagesDiosana, Jezelle B. PSY 1Y2-5JoshuaNo ratings yet
- 1201 Sanchez Padilla High Prevalence of Multidrug Resistant Tuberculosis Swaziland 2009 2010 Emerging Infectious Diseases 18 1Document9 pages1201 Sanchez Padilla High Prevalence of Multidrug Resistant Tuberculosis Swaziland 2009 2010 Emerging Infectious Diseases 18 1dewi ayu wulandariNo ratings yet
- Diagnosis & Treatment of Tuberculosis in HIV Co-Infected PatientsDocument16 pagesDiagnosis & Treatment of Tuberculosis in HIV Co-Infected PatientsdevisilalahiNo ratings yet
- Vol 42 No 13-EnglishDocument4 pagesVol 42 No 13-EnglishVijayakanth VijayakumarNo ratings yet
- MDG 6combat Hivaids, Malaria and Other DiseasesDocument8 pagesMDG 6combat Hivaids, Malaria and Other DiseasesLea Jean Lobrigo OleaNo ratings yet
- Research 1Document22 pagesResearch 1Biplov RoyNo ratings yet
- Baluchestan ProvinceDocument9 pagesBaluchestan ProvinceVincentius Michael WilliantoNo ratings yet
- Annotated Reading On Public Health Issues: GlobalDocument6 pagesAnnotated Reading On Public Health Issues: GlobalMarianette Ginulos CainongNo ratings yet
- PBH101 Assignment 05Document6 pagesPBH101 Assignment 05Siam AhmedNo ratings yet
- TB DR MohabbatDocument27 pagesTB DR Mohabbatdr_hammadNo ratings yet
- NIH Public Access: Treatment As Prevention-Where Next?Document15 pagesNIH Public Access: Treatment As Prevention-Where Next?Leon L GayaNo ratings yet
- TB HIV Research Proposal HarishDocument23 pagesTB HIV Research Proposal HarishLekha Bahadur Gurung100% (4)
- MDG Final EcodevDocument6 pagesMDG Final EcodevKing RenivaNo ratings yet
- MDR Somalia EID March 2013Document3 pagesMDR Somalia EID March 2013hirsi200518No ratings yet
- Drug Resistance TBDocument27 pagesDrug Resistance TBpriyanka bhowmikNo ratings yet
- Prevalence of Rifampicin Resistance Tuberculosis and Associated Factors Among Presumptive TB or MDRDocument3 pagesPrevalence of Rifampicin Resistance Tuberculosis and Associated Factors Among Presumptive TB or MDRTigray OutlookNo ratings yet
- The WHO Strategy For TB Control and EliminationDocument12 pagesThe WHO Strategy For TB Control and EliminationAdel HamadaNo ratings yet
- Burden of Tuberculosis - Combating Drug Resistance: EditorialDocument3 pagesBurden of Tuberculosis - Combating Drug Resistance: EditorialmominamalikNo ratings yet
- Research On Prevalence of TB FinalDocument9 pagesResearch On Prevalence of TB FinalBontuNo ratings yet
- Articulo 5Document15 pagesArticulo 5kevinNo ratings yet
- WHO Bulletin 2005Document10 pagesWHO Bulletin 2005ajh2675No ratings yet
- Publications - Through The CNS Lens - WHO Global TB Report 2012Document16 pagesPublications - Through The CNS Lens - WHO Global TB Report 2012bobbyramakantNo ratings yet
- We Are Intechopen, The World'S Leading Publisher of Open Access Books Built by Scientists, For ScientistsDocument17 pagesWe Are Intechopen, The World'S Leading Publisher of Open Access Books Built by Scientists, For ScientistsIoana AntonesiNo ratings yet
- Neumo8 Lecturas TBC SeminarioDocument15 pagesNeumo8 Lecturas TBC SeminarioMercedes Johanny Ortiz ChinguelNo ratings yet
- TB Burden Qatar: (CITATION Abu18 /L 1033)Document10 pagesTB Burden Qatar: (CITATION Abu18 /L 1033)Ahmad HashmiNo ratings yet
- MDR-TB Treatment As Prevention: The Projected Population-Level Impact of Expanded Treatment For Multidrug-Resistant TuberculosisDocument16 pagesMDR-TB Treatment As Prevention: The Projected Population-Level Impact of Expanded Treatment For Multidrug-Resistant TuberculosisSorina ElenaNo ratings yet
- Multidrug-Resistant Tuberculosis in Children: Evidence From Global SurveillanceDocument7 pagesMultidrug-Resistant Tuberculosis in Children: Evidence From Global SurveillanceAldy RinaldiNo ratings yet
- World Malaria Report 2013Document284 pagesWorld Malaria Report 2013Anonymous LjJZBb5dgC100% (1)
- 701 Full PDFDocument7 pages701 Full PDFMuhammad Tri Septo WibawaNo ratings yet
- Directly Observed TreatmentDocument9 pagesDirectly Observed TreatmentNovelia CarolinNo ratings yet
- Drug-Resistant TB: Deadly, Costly and in Need of A VaccineDocument6 pagesDrug-Resistant TB: Deadly, Costly and in Need of A VaccineSorina ElenaNo ratings yet
- TB and HIVDocument62 pagesTB and HIVNational Press FoundationNo ratings yet
- Tuberculosis-Reflection Paper HakdogDocument2 pagesTuberculosis-Reflection Paper Hakdogjoycamajalan2005No ratings yet
- G8010 2GR PREMIUM - Molykote - g8010Document2 pagesG8010 2GR PREMIUM - Molykote - g8010Dicky PratamaNo ratings yet
- Mt. Balagbag Reforest The Road - July 17, 2016Document6 pagesMt. Balagbag Reforest The Road - July 17, 2016ipo_dam4441No ratings yet
- FOMAR-QTN-2019-20-117 Kamat PDFDocument1 pageFOMAR-QTN-2019-20-117 Kamat PDFPriyesh KamatNo ratings yet
- Power Your Signal: Antenna SpecificationsDocument4 pagesPower Your Signal: Antenna SpecificationsДмитрийNo ratings yet
- Flow Control Valves: 1 DescriptionDocument6 pagesFlow Control Valves: 1 Descriptionnotitle91No ratings yet
- General Chemistry 2Document10 pagesGeneral Chemistry 2Aubrey GuilaranNo ratings yet
- ReferenceDocument5 pagesReferencenikhil moreNo ratings yet
- 1 - FLD-25 3D Printer Filament MachineDocument11 pages1 - FLD-25 3D Printer Filament MachineNitin PatilNo ratings yet
- Esquire Middle East - October 2016Document150 pagesEsquire Middle East - October 2016Anonymous Ow7wC7JIJNo ratings yet
- Hysteretic Relative Permeability EffectsDocument8 pagesHysteretic Relative Permeability Effectshfdshy12No ratings yet
- Fibertec 1023 Solution Brochure ENDocument2 pagesFibertec 1023 Solution Brochure ENrani hindiNo ratings yet
- Manufacturing Sector Hi Tech Aerospace Auto Industrial Medical Devices Chemicals & ProcessDocument9 pagesManufacturing Sector Hi Tech Aerospace Auto Industrial Medical Devices Chemicals & ProcessSambit RathNo ratings yet
- Cflga 2022Document9 pagesCflga 2022Hedjarah MulokNo ratings yet
- JHARKHAND-Mobile Health Unit ProposalDocument38 pagesJHARKHAND-Mobile Health Unit ProposalArun MudholNo ratings yet
- Bass Drum TechniqueDocument5 pagesBass Drum TechniqueRudy LievensNo ratings yet
- G.R. No. 198501 Kestrel Shipping Inc. v. MunarDocument12 pagesG.R. No. 198501 Kestrel Shipping Inc. v. MunarJa RuNo ratings yet
- College Adjustment Scale (CAS)Document7 pagesCollege Adjustment Scale (CAS)Bianca CarmenNo ratings yet
- TUGAS LAPORAN KIMED 3 MARET 2020 AnfaqDocument8 pagesTUGAS LAPORAN KIMED 3 MARET 2020 AnfaqMelati Ihza Safara PermataNo ratings yet
- GPM - Datasheet - NAE2092320 BenderDocument7 pagesGPM - Datasheet - NAE2092320 BenderAlexander MiltonNo ratings yet
- Bod and CodDocument66 pagesBod and CodKamlesh Kamlesh EtwaroNo ratings yet
- Lehx9590-02 Emcp II+Document4 pagesLehx9590-02 Emcp II+Jorge Luis Tanaka ConchaNo ratings yet
- 990-736 ABL80 FLEX Service ManualDocument409 pages990-736 ABL80 FLEX Service ManualIsmael MorinigoNo ratings yet
- Lysosome PresentationDocument5 pagesLysosome Presentationapi-241502402No ratings yet
- Zomato FindingsDocument24 pagesZomato FindingsNibu MathewNo ratings yet
- PT Level IIDocument161 pagesPT Level IIJerry100% (5)
- Sigmatherm™ 540 / PPG Hi-Temp™ 540: Product Data SheetDocument4 pagesSigmatherm™ 540 / PPG Hi-Temp™ 540: Product Data SheetSubodh KulkarniNo ratings yet