Professional Documents
Culture Documents
Generalized Calcinosis Cutis Associated With Probable Leptospirosis in A Dog (Pages 401-406)
Generalized Calcinosis Cutis Associated With Probable Leptospirosis in A Dog (Pages 401-406)
Uploaded by
jenOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Generalized Calcinosis Cutis Associated With Probable Leptospirosis in A Dog (Pages 401-406)
Generalized Calcinosis Cutis Associated With Probable Leptospirosis in A Dog (Pages 401-406)
Uploaded by
jenCopyright:
Available Formats
Veterinary Dermatology 2005, 16, 401 406
Case report
Blackwell Publishing, Ltd.
Generalized calcinosis cutis associated with
probable leptospirosis in a dog
JOHN S. MUNDAY*, DAVID J. BERGEN and WENDI D. ROE*
*New Zealand Veterinary Pathology Ltd. and Department of Pathobiology, Institute of Veterinary and Animal
Biological Sciences, Massey University, Palmerston North, Northern Waikato Veterinary Services, Huntly,
New Zealand
(Received 28 February 2005; accepted 19 July 2005)
Abstract A 6.5-year-old male German Shepherd acutely developed renal and hepatic disease. Serology revealed
high concentrations of antibodies against Leptospira copenhageni, and a presumptive diagnosis of leptospirosis
was made. The dog was successfully treated with antibiotics and supportive care over a 12-day period. Sixty-two
days after the initial presentation, alopecia predominantly involving the dorsum and perineal areas developed.
The skin lesions expanded over a 20-day period. Histology revealed generalized calcinosis cutis with follicular
atrophy. An injection of 0.01 mg kg1 dexamethasone suppressed serum cortisol concentrations. No treatment
was given and lesions resolved over the following 30 days. This is the third case of generalized calcinosis cutis that
has developed in an adult dog after severe systemic disease. Both previous cases developed calcinosis cutis in
association with blastomycosis. To the authors knowledge, this is the first report of generalized calcinosis cutis
in an adult dog in association with a presumptive bacterial infection.
IN TRO D U C T ION
C A S E R E P O RT
Calcinosis cutis is the deposition of calcium salts
within the skin.1 It can be subclassified depending on
the distribution and the cause of the calcium deposition.2 Localized calcinosis cutis is present at a single
site, whereas lesions of generalized calcinosis cutis are
widespread and multiple.3 Calcinosis cutis can develop
as a result of four different processes.4,5 Dystrophic
calcinosis cutis is the calcification of altered skin.3
Serum calcium and phosphorus concentrations are
normal.3 Metastatic calcinosis cutis is the calcification
of normal skin as a result of increased serum calcium
and/or phosphorus concentrations.3 Idiopathic calcinosis
cutis develops within undamaged skin without abnormal
serum calcium or phosphorus concentrations.3 Finally,
iatrogenic calcinosis cutis is caused by exposure to
calcium-containing substances.6,7 This case report
describes a dog that developed generalized calcinosis
cutis approximately 2 months after severe systemic
disease. The calcinosis cutis subsequently resolved
without treatment.
A 6.5-year-old male German Shepherd presented to a
veterinary clinic with a 2-day history of lethargy and
anorexia. Clinical examination revealed marked icterus,
and initial differential diagnoses included haemolytic
anaemia, liver damage and bile duct blockage. Blood
samples were taken and serum chemistry analysis revealed
increased alanine aminotransferase and alkaline phosphatase concentrations (Table 1), consistent with hepatic
necrosis and cholestasis. Blood urea nitrogen (BUN)
and creatinine concentrations were also increased, suggesting concurrent kidney disease. Urinalysis revealed
a specific gravity of 1.019, 2+ protein, 4+ blood and 3+
bilirubin. Leptospirosis was suspected because of the
evidence of acute liver and kidney damage. The dog had
not received vaccination against this disease. The dog
was treated with subcutaneous 40 mg kg1 procaine
penicillin q 12 h (Bovicillin, Bomac Laboratories Ltd,
Manukau City, New Zealand) and intravenous lactated
Ringers solution (2.5 mL kg1 h1). The following day,
serology revealed a titre of 1/400 against Leptospira
copenhageni. Although a definitive diagnosis is not
possible using a single antibody titre, the high level of
antibodies detected in this dog, combined with the
acute hepatic and kidney disease, strongly suggested a
diagnosis of acute leptospirosis.
On the third day of treatment, the dog started vomiting and developed diarrhoea that contained mucous and
blood. Enrofloxacin 5 mg kg1 q 12 h (Baytril, Bayer
Correspondence: J. S. Munday, Department of Pathobiology, Institute
of Veterinary and Animal Biological Sciences, Massey University,
Private Bag 11 222, Palmerston North, New Zealand. Tel.:
006463569099; Fax: 006463505636; E-mail: jmunday@massey.ac.nz
2005 European Society of Veterinary Dermatology
401
402
J S Munday, D J Bergen and W D Roe
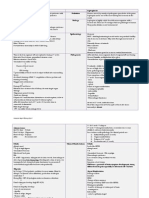
Table 1. Haematological and biochemical data from a 6.5-year-old, male German Shepherd that developed generalized calcinosis cutis shortly
after recovering from severe system disease. RBC, red blood cells. Reference ranges were provided by the diagnostic laboratory that performed
the analyses
RBC ( 1012 L1)
Segmented neutrophils ( 109 L1)
Lymphocytes ( 109 L1)
Monocytes ( 109 L1)
Alkaline phosphatase (ALP) (IU L1)
Alanine aminotransferase (ALT) (IU L1)
Bilirubin (mol L1)
Albumin (g L1)
Urea (mmol L1)
Creatinine (mol L1)
Phosphorus (mmol L1)
Calcium (mmol L1)
Adjusted calcium (mmol L1)23
Calciumphosphorus index
0 day
3 days
7 days
12 days
69 days
6.5
15.5
1.7
1.9
676
332
270
31
40.3
655
3.73
2.58
2.68
10
6.0
35.8
0.9
7.0
621
220
457
32
37.8
324
2.43
2.56
2.63
6.4
6.6
27.6
0.7
5.0
1023
202
249
6.1
13.9
2.9
1.9
810
162
97
31
215
15.9
131
5.0
8.1
2.2
0.4
35
51
6
32
10.1
101
1.85
2.1
2.17
4.0
NZ Ltd, Auckland, New Zealand) was given subcutaneously to prevent secondary infection of the damaged
gastrointestinal mucosa by gram-negative bacteria.
Metoclopramide (Metaclopramide injection, Pharmacia
(Perth) Pty Ltd, Bently, Australia) was administered
intravenously at a dose of 0.33 mg kg1 q 12 h to reduce
vomiting. An additional blood sample was taken. The
following day, haematemesis was observed and intravenous 0.66 mL kg1 q 12 h ranitidine (Zantac injectable,
GlaxoSmithKline, Parma, Italy) was administered.
Seven days after initial presentation, the vomiting
stopped and the antibiotic was changed to 20 mg kg1
q 12 h oral amoxicillin/clavulanate (Augmentin,
GlaxoSmithKline, Auckland, New Zealand). The antibiotic was changed at this time to avoid repeated
subcutaneous injections. Additional blood tests revealed
liver enzyme activities and bilirubin concentrations that
were similar to those measured at first presentation.
Serum BUN and creatinine concentrations were lower
than at initial presentation, but still increased above
reference ranges. The dogs clinical attitude gradually
improved over the following 4 days at which time intravenous therapy was discontinued. Blood taken 12 days
after initial presentation suggested reduced hepatocyte
necrosis and cholestasis as well as improved renal
function. The dog was discharged the following day on
oral doxycycline 3.3 mg kg1 q 24 h (Vibravet, Pfizer,
Auckland, New Zealand). A 14-day course of oral
doxycycline is recommended to eliminate the renal
carrier phase of leptospirosis.8
Sixty-two days after the disease onset, a small focus of
partial alopecia was observed on the dorsal surface of
the head. This area slowly expanded over the next week.
At this time, the lesion was 12 5 mm, well demarcated
and almost completely alopecic. Additionally, multiple,
roughly circular up to 10 cm in diameter, poorly demarcated areas of partial alopecia were visible on the dorsolumbar region and perineum extending down the caudal
aspect of the hind legs. The affected areas were not reddened or painful, and the owners had not noticed the dog
excessively scratching. Skin scrapings and tapings were
unremarkable. A blood sample did not reveal evidence
Reference ranges
5.58.5
311.5
1.04.8
0.21.4
0185
075
06
2644
2.610.2
45135
1.03.0
2.23.0
2.23.0
of liver or kidney disease. Trichography revealed a
predominance of telogen bulbs within hairs plucked
from the affected areas. Telogen effluvium was suspected
and no treatment was given. The dog was re-examined
7 days later (76 days after disease onset). The areas of
partial alopecia had enlarged and involved approximately 40% of the dorsum and perineum. The alopecic
areas appeared as multiple poorly defined patches that
measured up to 15 cm in diameter. Affected skin was
observed to be irregularly thickened but did not appear
darkened or reddened. Occasional 12-mm white papules
were visible within affected areas. Multiple skin biopsies
were taken and fixed in 10% buffered formalin solution.
Skin biopsies from affected skin on the head, shoulder,
dorsal thorax, lateral thorax and perineum were
examined histologically. Mineralization was visible within
all samples but was most marked within samples from
the head and perineum, of intermediate severity within
samples from the shoulder, and only identifiable using
von Kossa-stained sections within samples from the
dorsal and lateral thorax. Calcification of the external
follicular root sheath was visible multifocally throughout all the samples. Mineralization was also visible
within the deep dermis in samples from the head and
perineum and the superficial dermis within samples
from the shoulder. The deep dermal mineralization
appeared as up to 1-mm diameter foci of refractile
darkly speckled material (Fig. 1). The material stained
black using von Kossa stain, confirming calcification
(Fig. 2). The foci of deep dermal calcification were
surrounded by fibrosis and moderate numbers of
macrophages. Osseous metaplasia was visible within some
larger foci of calcification. Superficial dermal linear
calcification appeared as narrow horizontal refractile
basophilic bands interpreted as mineralized dermal
fibres. Follicles within sections from the head, perineum
and shoulders were smaller with follicular plugging
and trichilemmal keratinization. Anagen hair follicles
were not visible within samples from the head and
perineum, and few anagen follicles were visible within
biopsy samples from other locations. Dermal blood
vessels throughout the sections appeared within normal
2005 European Society of Veterinary Dermatology, Veterinary Dermatology, 16, 401 406
Canine calcinosis cutis due to Leptospirosis
403
hair loss was first noted and 124 days after initial
disease development), the owners reported complete
hair regrowth. No additional clinical disease has been
observed in this dog 9 months after resolution of the
skin lesions.
D IS C U S S IO N
Figure 1. Skin biopsy from the perineum of a 6.5-year-old male
German Shepherd. The asterisk indicates focal dermal calcification.
The calcification is surrounded by moderate fibrosis and
granulomatous inflammation. H&E bar = 110 m.
Figure 2. Skin biopsy from the perineum of a 6.5-year-old male
German Shepherd dog. The arrowheads indicate dermal
calcification. The asterisk indicates a hair follicle.
von Kossa stain bar = 140 m.
histological limits and no evidence of blood vessel
mineralization was observed. Clinically normal skin was
not biopsied, and it could not be determined whether
calcification was also present in unaffected skin.
The generalized calcinosis cutis and follicular atrophy
were considered suggestive of hyperadrenocorticism.
A low-dose dexamethasone suppression test was performed by administering 0.01 mg kg1 IV dexamethasone
(Dexadresson-V, Intervet Ltd., Auckland, New Zealand)
followed by serum cortisol measurement 4 and 8 h later.
Serum cortisol concentrations were markedly reduced
throughout the 8-h time period, suggesting that an
adrenal or pituitary neoplasm was not the cause of the
skin lesions. A thyroid hormone assay was within
normal limits. As no cause of the skin lesions could
be determined, no treatment was given. Approximately
3 days later, hair loss ceased and hair regrowth was
observed 15 days later. Thirty days later (62 days after
Calcinosis cutis can be categorized both on the distribution and the cause of the lesions. Dystrophic calcinosis
cutis occurs as a result of alterations within the skin
that promote calcification without concurrent changes
in serum calcium or phosphorus concentrations.5
Generalized dystrophic calcinosis cutis is most commonly
observed in veterinary medicine in dogs with hyperadrenocorticism.3 Approximately 40% of cushingoid
dogs develop calcinosis cutis, and it is thought that excess
cortisol alters the structure of proteins within collagen
and elastin fibres, predisposing them to calcification.3
Generalized calcinosis cutis has been reported in farmed
chinchillas in association with adrenocortical hyperplasia.9 The animals were suggested to have excessive
endogenous glucocorticoid production as a result of
chronic stress. 9 Calcinosis cutis does not develop
secondary to hyperadrenocorticism in other animal
species or humans.3,5 Generalized dystrophic calcinosis
cutis occasionally develops in dogs as a result of diabetes
mellitus.3 In humans, generalized dystrophic calcinosis
cutis is observed most commonly as a result of dermatomyositis, systemic lupus erythematosus, systemic
sclerosis and calcinosis Raynaud esophageal sclerodactyly telangiectasia syndrome.5 Localized dystrophic
calcinosis cutis in animals and humans most commonly
develops secondary to degeneration of a neoplasm (especially pilomatricoma or lipoma) or follicular cyst.3,5 It
also rarely occurs as a result of trauma or an inflammatory
process.3,5
Metastatic calcification is defined as the calcification
of normal tissues caused by raised serum calcium and/
or phosphorus concentration.5 Alterations in extracellular calcium or phosphorus concentrations disrupt
intracellular calcium regulation, resulting in tissue
mineralization.5 The product of serum calcium and
phosphorus concentrations is referred to as the calcium
phosphorus index. In dogs, a high calciumphosphorus
index most commonly causes calcification of the
kidneys, gastric mucosa, lungs, systemic arteries and
pulmonary veins.10 These tissues are thought to be
predisposed to calcification as they secrete acid and
thus have an internal alkaline compartment.11 As the
skin does not have an alkaline environment, it is
usually spared and metastatic calcinosis cutis is rare in
dogs and cats.3 Lesions of metastatic calcinosis cutis in
animals are usually confined to the foot pads;3,1214
however, the formation of discrete nodular calcifying
masses close to the scapula of a dog15 and on the chin
of a cat14 has also been reported. Reduction of the
calciumphosphorus index can result in lesion resolution.12,14 Metastatic calcinosis cutis is a rare complication
2005 European Society of Veterinary Dermatology, Veterinary Dermatology, 16, 401406
404
J S Munday, D J Bergen and W D Roe
of hypercalcaemia and hyperphosphataemia in people.16
Calciphylaxis is a specific subset of metastatic calcinosis
cutis that has been reported in people.5 This occurs in
approximately 1% of human patients with end-stage
renal disease and is characterized by calcification of
superficial dermal blood vessels and subsequent dermal
infarction and necrosis.5,17 Although the pathogenesis
is poorly understood, most cases develop because of a
combination of increased calciumphosphorus index
and a challenging agent that can be as diverse as
subcutaneous injections, coagulopathies, human immunodeficiency virus infection, Crohns disease or corticosteroid therapy.17
Idiopathic calcinosis cutis occurs without identifiable
tissue alterations or abnormal serum calcium or
phosphorus concentrations.3,5 Localized idiopathic
calcinosis cutis (also called calcinosis circumscripta
and tumoral calcinosis) occurs frequently in dogs and
horses18 and rarely in cats3 and Mongolian gerbils.19
Generalized idiopathic calcinosis cutis has been
observed in puppies after systemic illness.1 It has also
been reported to develop, and then spontaneously
resolve by 1 year of age, in healthy puppies.3 Two dogs
were reported to develop generalized idiopathic calcinosis cutis in association with systemic blastomycosis.4
A third dog with blastomycosis was reported to develop
localized lesions.4 Generalized idiopathic mineralization
of the basement membrane zone of the hair follicle
occurs as a senile change in miniature poodles.20
Iatrogenic calcinosis cutis has been reported as a
consequence of subcutaneous injection of calciumcontaining solutions in a dog21 and a cat.7 Additionally,
calcinosis cutis was observed after a dog contacted a
calcium chloride-containing landscaping product.6 In
humans, iatrogenic calcinosis cutis has been reported
after extravasation of intravenous calcium solutions
and after the use of calcium-containing solutions during
electromyography or electroencephalography.22
The initial disease in this dog was considered to be
leptospirosis as a result of the high antibody titre,
suggestive clinical signs and the lack of vaccination.
However, identification of bacteria using dark-field
microscopy examination of urine, urine culture or tissue
biopsies is necessary to confirm this diagnosis.8 Because
of intermittent shedding of small numbers of bacteria,
both urine examination and culture have poor sensitivity.8 In addition, the initiation of antimicrobial therapy
prior to the serology findings would have further reduced
the sensitivity of subsequent urine culture in this case.
Leptospira interrogans serovar copenhageni is a common
cause of canine leptospirosis in New Zealand. This
serovar is closely related to Leptospira interrogans
serovar icterohemorrhagica, and the two serovars are
serologically and clinically indistinguishable (J. CollinsEmerson, pers. comm.). Infected dogs, as in the presently
described case, become bacteraemic and typically show
evidence of both kidney and liver disease.23
Although the precise pathogenesis of the generalized
calcinosis cutis in this dog is uncertain, three mechanisms
are considered most likely. First, hyperphosphataemia
as a result of reduced kidney function may have resulted
in metastatic calcinosis cutis. Uraemia (indicative of
reduced kidney function) was present in this dog until day
12, and the calciumphosphorus index was, respectively,
10 and 6.4 on day 0 and day 3 after disease presentation.
Metastatic calcification has been reported to develop
at calciumphosphorus indices above 5.7.4 However,
previously reported lesions of metastatic calcification
in dogs were restricted either to the foot pads3 or periarticular soft tissues15 rather than the generalized
lesions observed in this present case.
The second possible cause of the calcinosis cutis in
this dog is dystrophic calcification as a result of alterations
in the dermis. As leptospirosis causes bacteraemia and
has been cultured from a skin lesion,24 it is possible that
bacteria deposited in the skin caused direct dermal
damage. However, this appears unlikely as other canine
dermatitides rarely result in calcification. Additionally,
bacterial damage to the dermal collagen is unlikely to
have been restricted to the dorsum of this dog. Alternatively, it is possible that increased release of adrenal
glucocorticoids caused by the stress of the disease could
have altered the dermal collagen. The follicular atrophy
visible histologically within samples taken from this dog
was consistent with hyperadrenocorticism. The dorsal
distribution of the calcinosis cutis visible in this dog was
also similar to the dorsal lesion distribution seen in cushingoid dogs.3 Chronic stress has been reported to cause
calcinosis cutis and follicular atrophy in chinchillas.9
However, most dogs that experience severe stress caused
by systemic illness do not subsequently develop calcinosis cutis.
Therefore, the third possible pathogenesis for the
development of the calcinosis cutis in this dog is a
combination of altered collagen (as a result of increased
endogenous glucocorticoids or direct bacterial dermal
damage) in the presence of an increased calcium
phosphorus index. Hypercalcaemia promotes dystrophic
calcification in people.11 Although hypercalcaemia did
not develop in this dog, it appears likely that increases in
serum phosphorus could likewise promote dystrophic
calcification. Interestingly, a similar mechanism may
have resulted in the generalized calcinosis cutis that
developed in two dogs in association with systemic
blastomycosis.4 In both dogs, a transiently increased
calcium-phosphorus index (presumably the result of
granulomatous inflammation) and prolonged severe
systemic disease were reported.4 Hyperphosphataemia
is a common incidental finding in young dogs.25 The
increased serum phosphorus concentrations may explain
why young dogs appear to develop generalized calcinosis
cutis after systemic illness more commonly than adult
animals. Idiopathic calcinosis cutis in healthy dogs
has been reported to resolve at 1 year of age. This may
coincide with the decline in serum phosphorus concentrations that occurs at this age.25
To the authors knowledge, this is the third adult dog
that has been reported to develop generalized calcinosis
cutis in association with systemic disease. Leptospirosis
was suspected as the cause of the systemic disease;
2005 European Society of Veterinary Dermatology, Veterinary Dermatology, 16, 401 406
Canine calcinosis cutis due to Leptospirosis
however, this was not definitively diagnosed. Regardless,
the observations in this case suggest that the stress
of severe systemic disease combined with impaired
renal function can result in generalized calcinosis cutis.
When the results of this case are considered along with
the previously reported dogs that developed generalized
calcinosis cutis after blastomycosis, it appears that
the calcinosis cutis spontaneously regresses once the
systemic illness is resolved.
REFEREN C E S
1. Gross TL, Ihrke PJ, Walder EJ. Veterinary Dermatopathology: a Macroscopic and Microscopic Evaluation
of Canine and Feline Skin Disease. St. Louis, Missouri:
Mosby Year Book, 1992: 223 8.
2. Ogretmen Z, Akay A, Bicakci C et al. Calcinosis cutis
universalis. Journal of the European Academy of
Dermatology and Venereology 2002; 16: 621 4.
3. Scott DW, Miller WH, Griffin CE. Muller and Kirks
Small Animal Dermatology, 6th edn. Philadelphia: W.B.
Saunders, 2001.
4. Gortel K, McKiernan BC, Johnson JK et al. Calcinosis
cutis associated with systemic blastomycosis in three dogs.
Journal of the American Animal Hospital Association
1999; 35: 36874.
5. Walsh JS, Fairley JA. Calcifying disorders of the skin.
Journal of the American Academy of Dermatology 1995;
33: 693706.
6. Schick MP, Schick RO, Richardson JA. Calcinosis
cutis secondary to percutaneous penetration of calcium
chloride in dogs. Journal of the American Veterinary
Medical Association 1987; 191: 20711.
7. Ruopp JL. Primary hypoparathyroidism in a cat complicated by suspect iatrogenic calcinosis cutis. Journal of the
American Animal Hospital Association 2001; 37: 3703.
8. Nelson RW, Couto CG. Small Animal Internal Medicine,
2nd edn. St. Louis: Mosby, Inc., 1998: 12739.
9. Tisljar M, Janic D, Grabarevic Z et al. Stress-induced
Cushings syndrome in fur-chewing chinchillas. Acta
Veterinaria Hungarica 2002; 50: 133 42.
10. Kruger JM, Osborne CA. Canine and feline hypercalcemic nephropathy. Part 1. Causes and consequences.
Compendium on Continuing Education for the Practicing Veterinarian 1994; 16: 1299316.
11. Kumar V, Abul KA, Fausto N. Cellular adaptations, cell
injury, and cell death. In: Kumar V, Abul KA, Fausto N
eds. Robins and Cotran Pathologic Basis of Disease, 7th
edn. Philadelphia: Elsevier Saunders, 2005: 3 46.
405
12. Komori S, Washizu M. Metastatic calcinosis circumscripta treated with an oral charcoal absorbent in a
dog. Journal of Veterinary Medical Science 2001; 63:
9136.
13. Jackson HA, Barber PJ. Resolution of metastatic
calcification in the paws of a cat with successful dietary
management of renal hyperparathyroidism. Journal of
Small Animal Practice 1998; 39: 4957.
14. Declercq J, Bhatti S. Calcinosis involving multiple
paws in a cat with chronic renal failure and in a cat
with hyperthyroidism. Veterinary Dermatology 2005; 16:
748.
15. Spotswood TC. Tumoral calcinosis in a dog with chronic
renal failure. Journal of the South African Veterinary
Association 2003; 74: 2932.
16. Tan HH, Cheong WK. Cutaneous gangrene secondary
to metastatic calcification in end stage renal failure a
case report. Singapore Medical Journal 1996; 37: 43840.
17. Hassaballa H, Luther MS, Bloom MK et al. Systemic
calciphylaxis in a patient with end-stage renal disease
and a normal parathyroid hormone level taking erythropoietin intramuscularly. Endocrine Practice 1999; 5: 46
50.
18. Roudebush P, Maslin WR, Cooper RC. Canine tumoral
calcinosis. Compendium on Continuing Education for
the Practicing Veterinarian 1988; 10: 11625.
19. Vincent AL, Ash LR. Further observations on spontaneous
neoplasms in the Mongolian gerbil, Meriones unguiculatus.
Laboratory Animal Science 1978; 28: 297300.
20. Seaman WJ, Chang SH. Dermal perifollicular mineralization of toy poodle bitches. Veterinary Pathology 1984;
21: 1223.
21. Schaer M, Ginn PE, Fox LE et al. Severe calcinosis cutis
associated with treatment of hypoparathyroidism in a dog.
Journal of the American Animal Hospital Association
2001; 37: 3649.
22. Kagen MH, Bansal MG, Grossman M. Calcinosis cutis
following the administration of intravenous calcium
therapy. Cutis 2000; 65: 1934.
23. Prescott JF, McEwen B, Taylor J et al. Resurgence of
leptospirosis in dogs in Ontario: recent findings.
Canadian Veterinary Journal 2002; 43: 95561.
24. Anderson JF, Miller DA, Post JE et al. Isolation of
Leptospira interrogans serovar grippotyphosa from the
skin of a dog. Journal of the American Veterinary
Medical Association 1993; 203: 15501.
25. Nelson RW, Turnwald GH, Willard MD. Endocrine,
metabolic, and lipid disorders. In: Willard MD, Tvedten
H, Turnwald GH eds. Small Animal Clinical Diagnosis
by Laboratory Methods, 3rd Edn. Philadelphia: W.B.
Saunders Company, 1999: 13671.
Rsum Un Berger allemand g de 6.5 ans a dvelopp soudainement une maladie hpatique et rnale. La
srologie a montr des taux levs danticorps dirigs contre Leptospira copenhageni et un diagnostic de
leptospirose a t fait. Le chien a t trait avec succs avec des antibiotiques et une ranimation pendant 21 jours.
62 jours aprs la premire consultation, une alopcie du dos et de la zone prianale est apparue. Les lsions se
sont tendues en 20 jours. Lhistologie a montr une calcinose gnralise avec atrophie folliculaire. Une injection
de 0.01 mg/kg de dexamthasone a frein les concentrations de cortisol. Aucun traitement na t administr et
les lsions ont disparu en 30 jours. Il sagit du troisime cas de calcinose cutane chez un chien adulte aprs une
maladie systmique svre. Les deux cas prcdents taient associs une blastomycose. Il sagit du premier cas
dcrit de calcinose cutane en association avec une infection bactrienne.
2005 European Society of Veterinary Dermatology, Veterinary Dermatology, 16, 401406
406
J S Munday, D J Bergen and W D Roe
Resumen Un perro pastor alemn de 6.5 aos de edad desarroll una enfermedad renal y heptica de forma
aguda. Mediante serologa se observaron altas concentraciones de anticuerpos frente a Leptospira copenhageni,
y dndose un diagnstico presuntivo de leptopirosis. El perro fue tratado con xito con antibiticos y cuidados
de mantenimiento durante 12 das. Sesenta y dos das tras la presentacin inicial observamos alopecia afectando
principalmente el dorso y perin. Las lesiones de la piel crecieron en tamao a lo largo de veinte das. El anlisis
histopatolgico revel calcinosis cutis generalizada con atrofia follicular. Una inyeccin de 0.01 mg/kg de
dexametasona neutraliz la concentracin de cortisol en suero. Sin otro tratamiento adicional las lesiones
curaron durante los siguientes 30 das. Este es el tercer caso de calcinosis cutis generalizada observado en un perro
adulto tras una severa enfermedad sistmica. Los casos previos desarrollaron calcinosis cutis asociada con
blastomicosis. Segn nuestras informaciones, este es el primer caso de calcinosis cutis generalizada en un perro
adulto asociada con una presunta infeccin bacteriana.
Zusammenfassung Ein 6.5 Jahre alter Deutscher Schferhund entwickelte eine akute Nieren- und Lebererkrankung. Serologisch wurde ein hoher Titer an Leptospira copenhageni Antikrpern nachgewiesen und die
Verdachtdiagnose einer Leptospirose gestellt. ber einen Zeitraum von 12 Tagen wurde der Hund mit
Antibiotika und untersttzender Therapie erfolgreich behandelt. Zweiundsechzig Tage nach der Erstprsentation entstand eine Alopezie, die in erster Linie den Rcken und die Perinealgegend betraf. ber einen Zeitraum
von 20 Tagen wurden diese Hautlsionen grer. Histologisch wurde eine generalisierte Calcinosis cutis mit
follikulrer Atrophie festgestellt. Eine Injektion von 0.01mg/kg Dexamethason unterdrckte die Kortisolkonzentration im Serum. Der Hund wurde nicht behandelt und die Vernderungen verschwanden innerhalb der
nchsten 30 Tage. Es handelt sich hierbei um den 3. Fall von generalisierter Calcinosis cutis, die bei einem adulten
Hund nach einer schweren systemischen Erkrankung entstand. Die beiden vorhergehenden Flle entwickelten
Calcinosis cutis im Zusammenhang mit einer Blastomykose. Soweit dem Autor bekannt, ist dies der erste
Fallbericht einer generalisierten Calcinosis cutis, die bei einem erwachsenen Hund im Zusammenhang mit einer
mutmalichen bakteriellen Infektion auftrat.
2005 European Society of Veterinary Dermatology, Veterinary Dermatology, 16, 401 406
You might also like
- FaR-RMS Protocol Version 2.0b - 06thdec2021Document187 pagesFaR-RMS Protocol Version 2.0b - 06thdec2021Alina CretuNo ratings yet
- Case Analysis Spina BifidaDocument11 pagesCase Analysis Spina BifidaErica Joy Algire VillalunaNo ratings yet
- Linear Organoid Nevus in A Dog (Pages 69-73)Document5 pagesLinear Organoid Nevus in A Dog (Pages 69-73)jenNo ratings yet
- Pioderma Articulo 2Document6 pagesPioderma Articulo 2Carla SancleNo ratings yet
- An Idiopathic Facial Dermatitis of Persian CatsDocument7 pagesAn Idiopathic Facial Dermatitis of Persian CatsjenNo ratings yet
- Kwashiorkor - ProQuest CentralDocument4 pagesKwashiorkor - ProQuest CentralDrbee10No ratings yet
- Chronic Splenic Torsion AdhesionsDocument5 pagesChronic Splenic Torsion AdhesionsDaniel CapuchoNo ratings yet
- Hyperoestrogenism and Mammary Adenosis Associated With A Metastatic Sertoli Cell Tumour in A Male Pekingese DogDocument5 pagesHyperoestrogenism and Mammary Adenosis Associated With A Metastatic Sertoli Cell Tumour in A Male Pekingese DogALAN RODRIGO ROJAS COVARRUBIASNo ratings yet
- Newmexico Investigation of A Cattle Mutilation in Which The Animal SurvivedDocument10 pagesNewmexico Investigation of A Cattle Mutilation in Which The Animal SurvivedLionel ElyansunNo ratings yet
- Canvetj00072 0045Document3 pagesCanvetj00072 0045D.S.M.No ratings yet
- Progressive Langerhans' Cell Histiocytosis in A Puppy (Pages 241-246)Document6 pagesProgressive Langerhans' Cell Histiocytosis in A Puppy (Pages 241-246)jenNo ratings yet
- PMC2480949Document8 pagesPMC2480949Nat C.No ratings yet
- Degeneration of Autonomic Nervous System in Feline Dysautonomia CaseDocument2 pagesDegeneration of Autonomic Nervous System in Feline Dysautonomia CaseBernadhete Gaudia SabiroseNo ratings yet
- Pyometra and Splenic Tumor in A Rescued Daschund Cross Bitch Positive With Ehrlichiosis and AnaplasmosisDocument8 pagesPyometra and Splenic Tumor in A Rescued Daschund Cross Bitch Positive With Ehrlichiosis and AnaplasmosisJohn AlzateNo ratings yet
- 10 1016@j Cvex 2020 01 005Document15 pages10 1016@j Cvex 2020 01 005Ophelia de VosNo ratings yet
- Acutehemorrhagicdiarrhea Syndromeindogs: Stefan Unterer,, Kathrin BuschDocument14 pagesAcutehemorrhagicdiarrhea Syndromeindogs: Stefan Unterer,, Kathrin BuschMaria HelenaNo ratings yet
- Severe Zinc Responsive Dermatosis in A Litter of Pharaoh Hounds Gregory A. Campbell, Dennis CrowDocument4 pagesSevere Zinc Responsive Dermatosis in A Litter of Pharaoh Hounds Gregory A. Campbell, Dennis CrowsafitriaNo ratings yet
- Role of Cryptosporidial Infection F. Osman and Ali SadiekDocument10 pagesRole of Cryptosporidial Infection F. Osman and Ali SadiekAli H. Sadiek أ.د. علي حسن صديق100% (4)
- Panniculitis and Concurrent Inflammatory Bowel Disease in A DogDocument4 pagesPanniculitis and Concurrent Inflammatory Bowel Disease in A DogRaiisa MtNo ratings yet
- OperationDocument4 pagesOperationTia KawairiIzhukaNo ratings yet
- ProstatitisDocument5 pagesProstatitisAz-zahra BudimanNo ratings yet
- Chronic Splenic Torsion in Two DogsDocument6 pagesChronic Splenic Torsion in Two DogsDaniel CapuchoNo ratings yet
- Https:journals Sagepub Com:doi:pdf:10 1354:vp 37-6-650Document3 pagesHttps:journals Sagepub Com:doi:pdf:10 1354:vp 37-6-650Lucas XavierNo ratings yet
- Malakoplakia of The Urinary Bladder in A Young French BulldogDocument6 pagesMalakoplakia of The Urinary Bladder in A Young French BulldogEmilia AmmariNo ratings yet
- J Vet Emergen Crit Care - 2008 - F Lix - Canine Leishmaniasis With Nephrotic Syndrome and Aortic and Caudal Vena CavaDocument6 pagesJ Vet Emergen Crit Care - 2008 - F Lix - Canine Leishmaniasis With Nephrotic Syndrome and Aortic and Caudal Vena CavadaniruizcasNo ratings yet
- Cap Polyposis in Children: Case Report and Literature ReviewDocument6 pagesCap Polyposis in Children: Case Report and Literature ReviewLuis ArrietaNo ratings yet
- Hypospadias and Megacolon in A Persian CatDocument3 pagesHypospadias and Megacolon in A Persian CatRizki FitriaNo ratings yet
- Cystic Endometrial Hyperplasia and Pyometra in Three Captive African Hunting Dogs (Lycaon Pictus)Document7 pagesCystic Endometrial Hyperplasia and Pyometra in Three Captive African Hunting Dogs (Lycaon Pictus)Intan Renita Yulianti DrumerNo ratings yet
- Case Report Generalized Dermatophytosis in Six Yorkshire Terrier DogsDocument7 pagesCase Report Generalized Dermatophytosis in Six Yorkshire Terrier DogsjenNo ratings yet
- A Prospective Study of The Clinical Findings, Treatment and Histopathology of 44 Cases of Pyotraumatic Dermatitis (Pages 369-376)Document8 pagesA Prospective Study of The Clinical Findings, Treatment and Histopathology of 44 Cases of Pyotraumatic Dermatitis (Pages 369-376)jenNo ratings yet
- Jurnal Balantidium Coli PDFDocument6 pagesJurnal Balantidium Coli PDFNika Dwi AmbarwatiNo ratings yet
- Methyl Mercury Mink Brain Ataxia DeathMercury and Mink 11. Experimental Methyl Mercury Intoxication G. Wobeser, N. 0. Nielsen and B. SchieferDocument12 pagesMethyl Mercury Mink Brain Ataxia DeathMercury and Mink 11. Experimental Methyl Mercury Intoxication G. Wobeser, N. 0. Nielsen and B. Schiefer23980hcasdjknNo ratings yet
- Fish DiseaseDocument6 pagesFish Diseasemorrison musebeNo ratings yet
- 47 Pathology in PracticeDocument3 pages47 Pathology in PracticeCarlos Alberto Chaves VelasquezNo ratings yet
- Cuerpos de CohleDocument15 pagesCuerpos de CohleJoseNeiserCastilloArrascueNo ratings yet
- Foster 1997Document5 pagesFoster 1997mario256No ratings yet
- Cuy BeditoDocument15 pagesCuy BeditoLucero CarranzaNo ratings yet
- Hepatic Necrosis and Degenerative Myopathy Associated With Cassava Feeding in PigsDocument4 pagesHepatic Necrosis and Degenerative Myopathy Associated With Cassava Feeding in PigsLAURA DANIELA VERA BELTRANNo ratings yet
- Cricopharyngeal DysphagiaDocument8 pagesCricopharyngeal Dysphagiataner_soysurenNo ratings yet
- Laparoscopic Cryptorchidectomy in Dogs - Report of 15 Cases: Polish Journal of Veterinary Sciences February 2005Document5 pagesLaparoscopic Cryptorchidectomy in Dogs - Report of 15 Cases: Polish Journal of Veterinary Sciences February 2005giovanna.paschoaloto610No ratings yet
- Javma 237 3 299Document5 pagesJavma 237 3 299tcvhNo ratings yet
- Morphologic and Immunologic Characterization of A Canine Isthmus Mural Folliculitis Resembling Pseudopelade of Humans (Pages 17-24)Document8 pagesMorphologic and Immunologic Characterization of A Canine Isthmus Mural Folliculitis Resembling Pseudopelade of Humans (Pages 17-24)jenNo ratings yet
- Javma-Javma 20 04 0230Document3 pagesJavma-Javma 20 04 0230Fiorella YavarNo ratings yet
- Lead Intoxication in A Puppy - A Case Report: E. S, J. P - G, I. K, B. P, B. A, Z. Š - PDocument2 pagesLead Intoxication in A Puppy - A Case Report: E. S, J. P - G, I. K, B. P, B. A, Z. Š - PMauricio RíosNo ratings yet
- Progressive Lymphocytic Cholangitis in The Cat (Journal of Small Animal Practice, Vol. 25, Issue 5) (1984)Document12 pagesProgressive Lymphocytic Cholangitis in The Cat (Journal of Small Animal Practice, Vol. 25, Issue 5) (1984)Dalia ExtrapolisNo ratings yet
- HFRS Vs LeptospirosisDocument5 pagesHFRS Vs LeptospirosisSarah RepinNo ratings yet
- Lepromatous Leprosy in A Patient With B-Cell Lymphoma and Tubulointerstitial NephritisDocument4 pagesLepromatous Leprosy in A Patient With B-Cell Lymphoma and Tubulointerstitial NephritisDar LynnNo ratings yet
- Therapeutic Management of Canine Babesiosis Associated With Acute Renal FailureDocument4 pagesTherapeutic Management of Canine Babesiosis Associated With Acute Renal FailurekamalNo ratings yet
- LinfomaMott FullDocument6 pagesLinfomaMott FullVeterinariaUTNo ratings yet
- Thermographic Imaging in A Dog With Macroglossia From An Encircling, Strangulating Lingual Linear Foreign BodyDocument4 pagesThermographic Imaging in A Dog With Macroglossia From An Encircling, Strangulating Lingual Linear Foreign BodyFrancisco Luis Briseño MedinaNo ratings yet
- Q FeverDocument28 pagesQ FeverAbhinav VermaNo ratings yet
- Salmonella Enterica Serotype I 4, 5, 12:-: 1,2. This Is The First Report of Acute HepaticDocument12 pagesSalmonella Enterica Serotype I 4, 5, 12:-: 1,2. This Is The First Report of Acute HepaticOktavia firnandaNo ratings yet
- Systemic Lupus Erythematosus Discoid in Dog CanisDocument4 pagesSystemic Lupus Erythematosus Discoid in Dog CanisAlina BlondaNo ratings yet
- Carcinomas Celulas Transicionales FinalDocument25 pagesCarcinomas Celulas Transicionales FinalLeidy CriolloNo ratings yet
- Case StudiesDocument56 pagesCase StudiesMayra F. MontielNo ratings yet
- Ménétrier-Like Disease in A Pointer With Concurrent Granulomatous Gastritis, Helicobacteriosis and LeishmaniosisDocument8 pagesMénétrier-Like Disease in A Pointer With Concurrent Granulomatous Gastritis, Helicobacteriosis and LeishmaniosisVitor MolinaNo ratings yet
- January 24 2006 TIME: 1hour Instructions To Candidates: Answer All Questions Answer Each Question in A Separate BookletDocument9 pagesJanuary 24 2006 TIME: 1hour Instructions To Candidates: Answer All Questions Answer Each Question in A Separate BookletAto Kwamena Sagoe100% (1)
- Canine Sterile Steroid-Responsive Lymphadenitis in 49 Dogs - Ribas & OtrosDocument11 pagesCanine Sterile Steroid-Responsive Lymphadenitis in 49 Dogs - Ribas & OtrosJuanMartínezNo ratings yet
- EchinococcusDocument20 pagesEchinococcusJuan Fernando Calcina IsiqueNo ratings yet
- Liken PlanusDocument6 pagesLiken PlanusAmirahShalehaNo ratings yet
- Feline Plasma Cell Pododermatitis - A Study of 8 Cases (Pages 333-337) PDFDocument5 pagesFeline Plasma Cell Pododermatitis - A Study of 8 Cases (Pages 333-337) PDFjenNo ratings yet
- Effects of Dietary Flax Seed and Sunflower Seed Supplementation On Normal Canine Serum Polyunsaturated Fatty Acids and Skin and Hair PDFDocument7 pagesEffects of Dietary Flax Seed and Sunflower Seed Supplementation On Normal Canine Serum Polyunsaturated Fatty Acids and Skin and Hair PDFjenNo ratings yet
- Isolation of Microsporum Canis From The Hair Coat of Pet Dogs and Cats Belonging To Owners Diagnosed With M. Canis Tinea Corporis (Pages 327-331)Document5 pagesIsolation of Microsporum Canis From The Hair Coat of Pet Dogs and Cats Belonging To Owners Diagnosed With M. Canis Tinea Corporis (Pages 327-331)jenNo ratings yet
- Oestrogen Receptor Evaluation in Pomeranian Dogs With Hair Cycle Arrest (Alopecia X) On Melatonin Supplementation (Pages 252-258)Document7 pagesOestrogen Receptor Evaluation in Pomeranian Dogs With Hair Cycle Arrest (Alopecia X) On Melatonin Supplementation (Pages 252-258)jenNo ratings yet
- Patch Testing of Experimentally Sensitized Beagle Dogs - Development of A Model For Skin Lesions of Atopic Dermatitis (Pages 95-102)Document8 pagesPatch Testing of Experimentally Sensitized Beagle Dogs - Development of A Model For Skin Lesions of Atopic Dermatitis (Pages 95-102)jenNo ratings yet
- Mouse Epidermal Development - Effects of Retinoic Acid Exposure in Utero (Pages 36-44)Document9 pagesMouse Epidermal Development - Effects of Retinoic Acid Exposure in Utero (Pages 36-44)jenNo ratings yet
- The Impact of Body Site, Topical Melatonin and Brushing On Hair Regrowth After Clipping Normal Siberian Husky Dogs (Pages 45-50)Document6 pagesThe Impact of Body Site, Topical Melatonin and Brushing On Hair Regrowth After Clipping Normal Siberian Husky Dogs (Pages 45-50)jenNo ratings yet
- A Retrospective Study of Cutaneous Equine Sarcoidosis and Its Potential Infectious Aetiological Agents (Pages 51-62)Document12 pagesA Retrospective Study of Cutaneous Equine Sarcoidosis and Its Potential Infectious Aetiological Agents (Pages 51-62)jenNo ratings yet
- Immunolocalization of Aquaporin-5 Expression in Sweat Gland Cells From Normal and Anhidrotic Horses (Pages 17-23)Document7 pagesImmunolocalization of Aquaporin-5 Expression in Sweat Gland Cells From Normal and Anhidrotic Horses (Pages 17-23)jenNo ratings yet
- Diagnostic CentreDocument14 pagesDiagnostic CentreJonas AsiaNo ratings yet
- Case Discussion Day 2 - MatulaDocument1 pageCase Discussion Day 2 - MatulaTRISHA MATULANo ratings yet
- Rationaldruguse 150519185142 Lva1 App6892Document12 pagesRationaldruguse 150519185142 Lva1 App6892nikki_bamsNo ratings yet
- Chapter 12 Summary Abnormal Psychology An Integrative ApproachDocument12 pagesChapter 12 Summary Abnormal Psychology An Integrative ApproachDjane VillarinNo ratings yet
- FDA Executive Summary Dermal FillersDocument41 pagesFDA Executive Summary Dermal FillersAhmed Sad100% (1)
- Drug SupplyDocument441 pagesDrug SupplyJIBRIL ALINo ratings yet
- Dementia and Alzheimers Topic ReportingDocument9 pagesDementia and Alzheimers Topic ReportingROGEN KATE AZARCONNo ratings yet
- Vitamin K Deficiency in InfantsDocument20 pagesVitamin K Deficiency in InfantsAnne TjanNo ratings yet
- ReferensiDocument126 pagesReferensiFatchul ChoiriNo ratings yet
- Posterior Tibial Tendon DysfunctionDocument2 pagesPosterior Tibial Tendon Dysfunctionvisa12345No ratings yet
- Counseling in Menopausal Women How To Address The Benefits and Risks of Menopause Hormone Therapy A FIGO Position PaperDocument15 pagesCounseling in Menopausal Women How To Address The Benefits and Risks of Menopause Hormone Therapy A FIGO Position PapermurarosmNo ratings yet
- Peritoneal DialysisDocument17 pagesPeritoneal Dialysisellya theresiaNo ratings yet
- On Catatonia Seizures and BradycardiaDocument1 pageOn Catatonia Seizures and BradycardiaFlorin TudoseNo ratings yet
- Oncology EmergencyDocument41 pagesOncology Emergencyomad pendaftaranPPDS100% (2)
- Infection Control Program Flow ChartDocument1 pageInfection Control Program Flow ChartAnonymous ORleRrNo ratings yet
- SyncopeDocument3 pagesSyncopeanishdNo ratings yet
- Vtne Study Strategies Zuku ReviewDocument33 pagesVtne Study Strategies Zuku ReviewEmmanuel Boulay100% (1)
- Association Subungual Abscess and Pyogenic Granuloma Secondary To Docetaxel TherapyDocument2 pagesAssociation Subungual Abscess and Pyogenic Granuloma Secondary To Docetaxel TherapyasclepiuspdfsNo ratings yet
- Uetquwiuj 912083949Document4 pagesUetquwiuj 912083949TzvineZNo ratings yet
- Medicine For Consumers 1St Edition Full ChapterDocument41 pagesMedicine For Consumers 1St Edition Full Chapteredward.weisner630100% (22)
- Caalm Citizen Petition To FDADocument23 pagesCaalm Citizen Petition To FDAZerohedge JanitorNo ratings yet
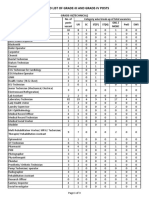
- Revised List of Grade-III Grade-IV Posts 0Document3 pagesRevised List of Grade-III Grade-IV Posts 0CLASHING ELECTRONo ratings yet
- Lecture 17 - Thyroid Disorders (Including Struma and CA Thyroid) - Dr. M. Robikhul Ikhsan, SP - PD-KEMD (2021)Document21 pagesLecture 17 - Thyroid Disorders (Including Struma and CA Thyroid) - Dr. M. Robikhul Ikhsan, SP - PD-KEMD (2021)Ivan AditamaNo ratings yet
- Investiture of Prof. Ebitimitula Nicholas Etebu As Honorary Fellow of The Nigerian Council of Physicians and Natural Medicine.Document2 pagesInvestiture of Prof. Ebitimitula Nicholas Etebu As Honorary Fellow of The Nigerian Council of Physicians and Natural Medicine.GILBERTNo ratings yet
- JurisprudenceDocument121 pagesJurisprudenceKate EvangelistaNo ratings yet
- 76962CT0010006-01 en USDocument98 pages76962CT0010006-01 en USKathy ApergisNo ratings yet
- Thromboelastogram (TEG) - LITFL - CCC Investigations PDFDocument13 pagesThromboelastogram (TEG) - LITFL - CCC Investigations PDFSiddharth Parmar100% (1)
- Susunan Acara Seminar ANGINA 2019Document2 pagesSusunan Acara Seminar ANGINA 2019Mellia Wida MasitaNo ratings yet