Professional Documents
Culture Documents
Shared Nationwide Interoperability Roadmap PDF
Shared Nationwide Interoperability Roadmap PDF
Uploaded by
iggybauOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Shared Nationwide Interoperability Roadmap PDF
Shared Nationwide Interoperability Roadmap PDF
Uploaded by
iggybauCopyright:
Available Formats
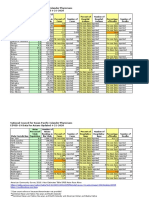
Shared Nationwide Interoperability Roadmap: The Journey to Better Health and Care
The nation relies on Health IT to securely, efficiently and effectively share electronic health information with patient
consent to achieve better care, smarter spending and healthier people. Interoperability will transform our health system
from a static one to a learning health system that improves individual, community and population health.
Where
We Are
94%
78%
of non-federal acute
care hospitals use a
certified EHR to
collect electronic
data about patients.1
1 in 3
of office-based
physicians use an
EHR system to
collect electronic
patient data.1
Number of consumers
burdened with providing their
own health information when
seeking care for a medical
problem (such as a test
result or medical history).2
62%
In 2013, more than six in
ten hospitals electronically
exchanged health
information with providers
outside of their system.3
STATE LINE
Most states have different laws and regulations making it
difficult to share health information across state lines.
The typical primary
care physician has to
coordinate care with
Taking a leisurely
Only half of hospitals can
electronically search for
critical health information
from outside sources
(such as in an emergency
or office visit).5
physicians
working in 117 practices.7
IN
By the end of 2017
The majority of individuals
and providers can send,
receive, find, and use a common
set of clinical information.
Where We
Are Going
for evidence to go from
research to practice.4
51%
229
other
The number of providers a typical Medicare
beneficiary sees annually.6
17 years
SPEED BUMPS TO INTEROPERABILITY
YEARS
Health information
is not sufficiently
standardized
Aligning
payment
incentives
Misinterpretation
and differences in
existing privacy laws
DETERMINANTS OF HEALTH
80%-90%
of office-based
providers
electronically
share patient information
with other providers.9
1 in 8
the number of Americans
in 2013 who tracked a
health metric like blood
pressure or weight using
some form of technology.8
of health determinants are NOT
related to health care.
Diet and
Exercise
Social
Lack
of
trust
14%
Environmental
Health
Care System
Economic
IN
YEARS
By the end of 2020
Connecting an expanded set of users and data sources through the use
of #mHealth and #wearables. Advances in the sharing and use of
patient-generated health data leads to consumer empowerment,
person-centered care, active individual health management and
greater information sharing with the public health community.
DRAMATICALLY REDUCE THE
TIME IT TAKES FOR EVIDENCE
FROM RESEARCH TO BECOME
COMMON PRACTICE
Healthier
People
By the end of 2024
IN
10
(thus better evidence-based diagnosis,
treatment and personalized medicine)
YEARS
Smarter
Spending
CO
N
Research Rd
Sources:
1. ONC Report to Congress, October 2014
http://www.healthit.gov/sites/default/files/rtc_adoption_and_exchange9302014.pdf
LEARNING
HEALTH
SYSTEM
2. http://www.healthit.gov/sites/default/files/consumeraccessdatabrief_9_10_14.pdf
3. http://healthit.gov/sites/default/files/oncdatabrief17_hieamonghospitals.pdf
4. Balas, E.A., Boren, S.A., Yearbook of Medical Informatics, 2000
5. http://dashboard.healthit.gov/quickstats/pages/FIG-Hospital-Electronic-Query-Capability.php
6. Pham HH, Schrag D, O'Malley AS, Wu B, Bach PB. Care patterns in Medicare and their implications for pay for
performance. N Engl J Med2007;356:1130-1139. http://www.nejm.org/doi/full/10.1056/NEJMsa063979
7. Pham HH, OMalley AS, Bach PB, Saiontz-Martinez C, Schrag D. Primary care physicians links to other physicians
through Medicare patients: the scope of care coordination. Ann Intern Med. 2009; 150:236-42
8. Pew Research Center. Tracking for Health. January 2013. Accessed from:
http://www.pewinternet.org/files/old-media//Files/Reports/2013/PIP_TrackingforHealth%20with%20appendix.pdf
9. Health affairs, August Issue; first author: Furukawa M
Public Health Pl
E
CL
Better
Care
EARNING
L
S
U
O
U
CY
IT N
A Learning Health System
reduces the time from evidence
to practice. This enables
ubiquitous connectivity, improves
population health and helps
researchers analyze data from a
variety of sources.
Privacy Blvd
Connecting an expanded set of data sources
and care settings, over time, such as:
Human Services
Schools
Prisons
Emergency responders
Home and Community
Nursing homes
Laboratory and
ancillary
Specialists
To learn more about interoperability,
visit www.healthit.gov/interoperability.
You might also like
- HCM 340 7-2Document11 pagesHCM 340 7-2Robin McFaddenNo ratings yet
- Benefits of Iclinicsys in The Rural Health Unit of Lupi, Camarines SurDocument5 pagesBenefits of Iclinicsys in The Rural Health Unit of Lupi, Camarines Surattyleoimperial100% (1)
- Final Economics Project Report 1Document56 pagesFinal Economics Project Report 1vikrant4us77% (13)
- Clinical Data Management, IInd EditionDocument18 pagesClinical Data Management, IInd EditionThomas Eipe100% (1)
- Review of Related LiteratureDocument6 pagesReview of Related LiteratureSkyla FiestaNo ratings yet
- NURSING INFORMATICS Community Health ApplicationsDocument6 pagesNURSING INFORMATICS Community Health ApplicationsThirdy Aquino100% (2)
- Information Technology and Community HealthDocument9 pagesInformation Technology and Community HealthAngel Joy CATALAN (SHS)100% (3)
- Pharma R&D Annual Review 2019: PharmaprojectsDocument32 pagesPharma R&D Annual Review 2019: PharmaprojectsraviNo ratings yet
- Pharma - Prescription Writing PDFDocument3 pagesPharma - Prescription Writing PDFVon Javier GamateroNo ratings yet
- Hca 353 Proposal UpdatedDocument18 pagesHca 353 Proposal Updatedapi-490705060No ratings yet
- Management of MedicationsDocument12 pagesManagement of Medicationsnayan4uNo ratings yet
- Tizon, R. - Assignment in NCM 112Document4 pagesTizon, R. - Assignment in NCM 112Royce Vincent TizonNo ratings yet
- Tihp It 012610Document7 pagesTihp It 012610api-258667648No ratings yet
- Tizon, R. - Assignment in NCM 112Document4 pagesTizon, R. - Assignment in NCM 112Royce Vincent TizonNo ratings yet
- Information SystemDocument6 pagesInformation SystemFaisal NiaziNo ratings yet
- According To JMIR PublicationsDocument3 pagesAccording To JMIR PublicationsJanine KhoNo ratings yet
- Bibek (CIS)Document3 pagesBibek (CIS)Bibek Ale MagarNo ratings yet
- Health Care Outlook For 2019: Five Trends That Could Impact Health Plans, Hospitals, and PatientsDocument5 pagesHealth Care Outlook For 2019: Five Trends That Could Impact Health Plans, Hospitals, and PatientsGracie Sugatan PlacinoNo ratings yet
- Text 2Document9 pagesText 2Alvin Josh CalingayanNo ratings yet
- CHN 7 & 8 - E-LearningDocument66 pagesCHN 7 & 8 - E-LearningCristina AdolfoNo ratings yet
- Decision Science Project - Prashant NairDocument11 pagesDecision Science Project - Prashant Nairprakhar jainNo ratings yet
- Health and Digital LiteracyDocument7 pagesHealth and Digital Literacywafula stanNo ratings yet
- Key Issues As Wearable Digital Health Technologies Enter Clinical CareDocument16 pagesKey Issues As Wearable Digital Health Technologies Enter Clinical CareJeya Seelan B PositiveNo ratings yet
- Summarissed Trends in Mobile ApsDocument4 pagesSummarissed Trends in Mobile ApsthomasNo ratings yet
- Module 14Document5 pagesModule 14camille nina jane navarroNo ratings yet
- Health InformationDocument30 pagesHealth InformationifelakojaofinNo ratings yet
- Knowledge and Attitude of Health Workers in State Hospitals, Towards Information TechnologyDocument49 pagesKnowledge and Attitude of Health Workers in State Hospitals, Towards Information TechnologyTajudeen AdegbenroNo ratings yet
- Healthcare Unwired HRI PWCDocument40 pagesHealthcare Unwired HRI PWCKarl HessNo ratings yet
- NehaDocument20 pagesNehaRecorders RndNo ratings yet
- Community Health Nursing Also Called Public Health Nursing or Community NursingDocument2 pagesCommunity Health Nursing Also Called Public Health Nursing or Community NursingZanie CruzNo ratings yet
- Interoperability and Universal Health Care in The PhilippinesDocument4 pagesInteroperability and Universal Health Care in The PhilippinesRvbrRubaNo ratings yet
- Challenges in Law With Regard To Digital HealthcareDocument6 pagesChallenges in Law With Regard To Digital HealthcareAnna TomNo ratings yet
- National Digital Health MissionDocument3 pagesNational Digital Health MissionSrinivas JupalliNo ratings yet
- WHO - The Need For Strong Health Information Systems - Rationale For The HMN FrameworkDocument4 pagesWHO - The Need For Strong Health Information Systems - Rationale For The HMN FrameworkHarumNo ratings yet
- Healthcast The Customisation of Diagnosis Care and Cure-Pwc-2010 PDFDocument58 pagesHealthcast The Customisation of Diagnosis Care and Cure-Pwc-2010 PDFEhli HibreNo ratings yet
- Medical Informatics Activity No.1Document3 pagesMedical Informatics Activity No.1leomillmendiolaNo ratings yet
- Nick POLESTICO (MT 102 HIS LAB. PTSK.)Document4 pagesNick POLESTICO (MT 102 HIS LAB. PTSK.)Nick PolesticoNo ratings yet
- Nursing Informatics FinalsDocument7 pagesNursing Informatics FinalsAlyNo ratings yet
- Issues in International Health Policy: Electronic Health Records: An International Perspective On "Meaningful Use"Document18 pagesIssues in International Health Policy: Electronic Health Records: An International Perspective On "Meaningful Use"Sevi Cephy ONo ratings yet
- Allied Health Scenario (AHS)Document4 pagesAllied Health Scenario (AHS)Johnson JayNo ratings yet
- IT in HealthcareDocument44 pagesIT in HealthcaremarkdemonteverdeNo ratings yet
- 1ausing Information Systems To Improve Population Outcomes Concepts in Program Design and Development Structure SystemsDocument7 pages1ausing Information Systems To Improve Population Outcomes Concepts in Program Design and Development Structure Systemsapi-678571963No ratings yet
- Electronic Health Record SystemDocument7 pagesElectronic Health Record SystemmainuddinbhNo ratings yet
- Hit Research ProjectDocument20 pagesHit Research ProjectDavid JuarezNo ratings yet
- A Market Research On EhrDocument29 pagesA Market Research On EhrFranklin MalukiNo ratings yet
- Wjarr 2024 0478Document10 pagesWjarr 2024 0478punishermoviesNo ratings yet
- State Success Spurs National Innovation in Health Information Exchanges - Shared HealthDocument6 pagesState Success Spurs National Innovation in Health Information Exchanges - Shared Healthlisarx5No ratings yet
- Digital Transformation of Healthcare Industry Liquid Hub WhitepaperDocument14 pagesDigital Transformation of Healthcare Industry Liquid Hub WhitepaperNitin AmesurNo ratings yet
- Evolution of Health InformaticsDocument10 pagesEvolution of Health InformaticsMULUKENNo ratings yet
- Order ### 2672790Document11 pagesOrder ### 2672790Wallace Mandela Ong'ayoNo ratings yet
- What Is Nursing InformaticsDocument3 pagesWhat Is Nursing InformaticsRose JoyNo ratings yet
- Chn 2 Ict Finals Part1Document48 pagesChn 2 Ict Finals Part1clarenzsolivenNo ratings yet
- E GovernanceDocument21 pagesE GovernanceIshita chughNo ratings yet
- What Is The Critical Care Information System? What Comprises It and How Does It Work?Document2 pagesWhat Is The Critical Care Information System? What Comprises It and How Does It Work?FANER, ANGELINE N.No ratings yet
- Role of His and Ris in Improving Quality of PatientcareDocument10 pagesRole of His and Ris in Improving Quality of Patientcareمحمدعبدالخالق العلواني100% (1)
- Standard Electronic Health Record (EHR) Framework For Indian Healthcare SystemDocument24 pagesStandard Electronic Health Record (EHR) Framework For Indian Healthcare SystemAgus MutamakinNo ratings yet
- What Is EDocument4 pagesWhat Is ECake ManNo ratings yet
- Chapter 2 RRL (NEW UPDATE)Document7 pagesChapter 2 RRL (NEW UPDATE)kieferdoctor043No ratings yet
- Evelyn Hone College: School of Applied Health and SciencesDocument6 pagesEvelyn Hone College: School of Applied Health and SciencesDave0% (1)
- Iceland National Ehealth Strategies January 2016 FinalDocument8 pagesIceland National Ehealth Strategies January 2016 Finalalbert svanNo ratings yet
- A Study and Impact of Cyberchondria On The Indian PopulationDocument18 pagesA Study and Impact of Cyberchondria On The Indian PopulationRajesh DasNo ratings yet
- Defining MedicalHealth InformaticsDocument5 pagesDefining MedicalHealth InformaticsKamnenwNo ratings yet
- New Technologies Related To Public Health Electronic InformationDocument5 pagesNew Technologies Related To Public Health Electronic InformationRose Lyn Camarista VelascoNo ratings yet
- Divergent Canada MhealthcareDocument12 pagesDivergent Canada MhealthcareSteveEpsteinNo ratings yet
- Health informatics: Improving patient careFrom EverandHealth informatics: Improving patient careBCS, The Chartered Institute for ITRating: 3 out of 5 stars3/5 (1)
- Bostock v. Clayton County, Georgia DecisionDocument119 pagesBostock v. Clayton County, Georgia DecisionNational Content DeskNo ratings yet
- AAFP Letter To Domestic Policy Council 6-10-2020Document3 pagesAAFP Letter To Domestic Policy Council 6-10-2020iggybauNo ratings yet
- Boston Mayor Executive Order 6-12-2020Document3 pagesBoston Mayor Executive Order 6-12-2020iggybauNo ratings yet
- S 3609 Coronavirus Immigrant Families Protection ActDocument17 pagesS 3609 Coronavirus Immigrant Families Protection ActiggybauNo ratings yet
- HR 6437 Coronavirus Immigrant Families Protection AcfDocument16 pagesHR 6437 Coronavirus Immigrant Families Protection AcfiggybauNo ratings yet
- A Bill: in The House of RepresentativesDocument2 pagesA Bill: in The House of RepresentativesiggybauNo ratings yet
- HR 6763 COVID-19 Racial and Ethnic Disparities Task ForceDocument11 pagesHR 6763 COVID-19 Racial and Ethnic Disparities Task ForceiggybauNo ratings yet
- Doe v. Trump Preliminary Injunction Against Proclamation Requiring Private Health InsuranceDocument48 pagesDoe v. Trump Preliminary Injunction Against Proclamation Requiring Private Health InsuranceiggybauNo ratings yet
- S 3721 COVID-19 Racial and Ethnic Disparities Task ForceDocument11 pagesS 3721 COVID-19 Racial and Ethnic Disparities Task ForceiggybauNo ratings yet
- SF StayHome MultiLang Poster 8.5x11 032620Document1 pageSF StayHome MultiLang Poster 8.5x11 032620iggybauNo ratings yet
- Doe v. Trump Denial of All Writs Injunction Against April 2020 Presidential ProclamationDocument9 pagesDoe v. Trump Denial of All Writs Injunction Against April 2020 Presidential ProclamationiggybauNo ratings yet
- HR 6585 Equitable Data Collection COVID-19Document18 pagesHR 6585 Equitable Data Collection COVID-19iggybauNo ratings yet
- NCAPIP Recommendations For Culturally and Linguistically Appropriate Contact Tracing May 2020Document23 pagesNCAPIP Recommendations For Culturally and Linguistically Appropriate Contact Tracing May 2020iggybauNo ratings yet
- CDC Covid-19 Report FormDocument2 pagesCDC Covid-19 Report FormiggybauNo ratings yet
- Covid-19 Data For Asians Updated 4-21-2020Document2 pagesCovid-19 Data For Asians Updated 4-21-2020iggybauNo ratings yet
- Exposing Corporate Profiteering From Immigration Detention and Enforcement September 2018Document16 pagesExposing Corporate Profiteering From Immigration Detention and Enforcement September 2018iggybauNo ratings yet
- MACRA Quality Payment Program Year 2 Final RuleDocument662 pagesMACRA Quality Payment Program Year 2 Final RuleiggybauNo ratings yet
- PNDFvol1ed7 2008Document315 pagesPNDFvol1ed7 2008Wilma de LeonNo ratings yet
- Export Prospect of Pharmaceuticals Sector in BangladeshDocument7 pagesExport Prospect of Pharmaceuticals Sector in BangladeshMarshal RichardNo ratings yet
- 05 Ich GCPDocument25 pages05 Ich GCPBhaskar Satya Sankar Balaji100% (1)
- 3700Document164 pages3700Đức LinhNo ratings yet
- Register, 2012Document233 pagesRegister, 2012Natalia Pika Ambrace0% (1)
- Clinical Research AssociateDocument3 pagesClinical Research Associateapi-79117686No ratings yet
- Medicine StandardsDocument58 pagesMedicine Standardsmd100% (2)
- Essay Topic 1 Healthcare in India @pdf4examsDocument9 pagesEssay Topic 1 Healthcare in India @pdf4examsAbhinav Ashok ChandelNo ratings yet
- Georgia Healthcare Group PLC-Annual Report (Apr-08-2020)Document188 pagesGeorgia Healthcare Group PLC-Annual Report (Apr-08-2020)Messina04No ratings yet
- Digital-Circulation-Report - NATHEALTHDocument36 pagesDigital-Circulation-Report - NATHEALTHadikabraNo ratings yet
- Corruption in Public Healthcare Sector of BangladeshDocument14 pagesCorruption in Public Healthcare Sector of BangladeshNaushin Fariha Jalal 1821146630No ratings yet
- Don Failla 45 MinutosDocument54 pagesDon Failla 45 MinutosEfrain M. Galvan DzNo ratings yet
- Reminder of Appropriate Prescribing and Dispensing 3-24-2020 684869 7Document1 pageReminder of Appropriate Prescribing and Dispensing 3-24-2020 684869 7Scott JohnsonNo ratings yet
- Processing and Submission of Drug Master FileDocument11 pagesProcessing and Submission of Drug Master FileNOORUDDIN100% (1)
- An Emperical Study On Consumer's Perception Towards Health Insurance in Gwalior District of Madhya PradeshDocument6 pagesAn Emperical Study On Consumer's Perception Towards Health Insurance in Gwalior District of Madhya PradeshPARTH PATELNo ratings yet
- 09 2021uganda National Survey Report 2019 2020Document387 pages09 2021uganda National Survey Report 2019 2020Boniface OkudaNo ratings yet
- Clincal Trial Phases FinalDocument59 pagesClincal Trial Phases FinalHemant MittalNo ratings yet
- Historical Overview of Pharmaceutical Industry and Drug Regulatory Affairs 2167 7689.S11 002Document11 pagesHistorical Overview of Pharmaceutical Industry and Drug Regulatory Affairs 2167 7689.S11 002Gopal KarvaNo ratings yet
- SanbeDocument13 pagesSanbeJar JarNo ratings yet
- A Review On Drug Approval in Regulated and Non-Regulated MarketsDocument5 pagesA Review On Drug Approval in Regulated and Non-Regulated MarketsJohannes SchufiNo ratings yet
- 1 SuDocument4 pages1 SuHoniel PagoboNo ratings yet
- Pharma ListDocument22 pagesPharma ListdialankitNo ratings yet
- SOP C117 PVG V1 1 07jan2014 PDFDocument18 pagesSOP C117 PVG V1 1 07jan2014 PDFweilinmdNo ratings yet
- Updated Changes - Unique Identification Framework 30 - August - 2022CLDocument63 pagesUpdated Changes - Unique Identification Framework 30 - August - 2022CLMich LadoNo ratings yet