Professional Documents
Culture Documents
Intravenous Dexmedetomidine and Butorphanol Prolongs Bupivacaine Sensory Analgesia in Lower Abdominal Surgeries.
Intravenous Dexmedetomidine and Butorphanol Prolongs Bupivacaine Sensory Analgesia in Lower Abdominal Surgeries.
Original Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Intravenous Dexmedetomidine and Butorphanol Prolongs Bupivacaine Sensory Analgesia in Lower Abdominal Surgeries.
Intravenous Dexmedetomidine and Butorphanol Prolongs Bupivacaine Sensory Analgesia in Lower Abdominal Surgeries.
Copyright:
Available Formats
IOSR Journal of Dental and Medical Sciences (IOSR-JDMS)
e-ISSN: 2279-0853, p-ISSN: 2279-0861.Volume 14, Issue 2 Ver. IV (Feb. 2015), PP 74-78
www.iosrjournals.org
Intravenous Dexmedetomidine and Butorphanol Prolongs
Bupivacaine Sensory Analgesia in Lower Abdominal Surgeries.
Vandna Bharti MD*, Shefali Gautam MD*, Prasanta Das MD, DM*#,
Ajay Kumar ChaudharyMD**, Jaishree BograMD***
(*Senior Resident, **Associate Professorand ***Professor and Head)
Department of Anesthesiology, King Georges Medical University, Lucknow, Uttarpradesh, India.
#All India Institute of Medical Sciences, New Delhi
Abstract:
Background:To compare the effects of intra-thecal bupivacaine alone, with dexmedetomidine and butorphanol
administered by intravenous route as adjuvant to intra-thecal bupivacaine separately.
Methods:The randomized, double blind comparative study was conducted in 60 patientsbelonging to ASA
grade I or II, aged 18-55 years admitted for lower abdominal surgeries under spinal anesthesia. The patients
were randomly divided into 3 groups (n=20). All patients were administered 15mg of 0.5% bupivacaine for
spinal anesthesia. Group(B) was given spinal anesthesia alone. Group(B+D) was given DXM(1g/kg) IV,
group(B+B) was givenbutorphanol(20g/kg) IVas an adjuvant to intra-thecal bupivacaine.
Results:The mean time to reachmaximum sensory level was highest in Group(B) and least in (B+D).Total
duration of analgesia was almost similar in DXM and butorphanol group and least in the control group. No. of
rescue analgesic required was significantly lower in DXM group than the rest of the groups. VAS score was
highest in the control group(B) while it was almost similar in DXM and butorphanol group.
Conclusion: IV dexmedetomidine and butorphanol can prolong the duration of sensory block, time to first
analgesic request associated with spinal anesthesia and provide better postoperative analgesia than the group
in which no intravenous adjuvants are used.
Keywords:spinal anesthesia, dexmedetomidine, butorphanol, bupivacaine.
I.
Introduction
Because of the technical challenges of readily identifying the epidural space and the toxicity associated
with the large doses of local anesthetics needed for epidural anesthesia, spinal anesthesiais still dominant form
of neuraxial anesthesia.[1] Role of intrathecal DEX and butorphanol in prolonging the spinal analgesia and
anesthesia had been very well studied separately. This study was conducted to compare the effects of intrathecal
bupivacaine alone, with DXM and butorphanol when administered by intravenous route as adjunct to intrathecal
bupivacaine.
II.
Material And Methods
After getting approval from Institutional Ethical Committee, the current randomized, double blind,
prospective, comparative study was conducted in 60 patients, aged 18-55 of years belonging to ASA grade I or
II,scheduled for lower abdominal surgery under spinal anesthesia. An informed consent was taken from all the
patients and/or attendants.Patientsrefusals for consent,having contraindication to neuraxial blockade or allergy
to study drugs were excluded from the study.A computer-generated randomization list was used to assigned
patients into the three groups. The intravenous drug formula was prepared by an anesthetist doctor and was
passed on to the doctor who performed the spinal analgesia who was blinded as to which group the patient was
allocated.
Group(B): spinal anesthesia with hyperbaric bupivacaine15mg (3ml of 0.5%)+intravenous infusion of 100 ml
of NS over 10 min. This served as control group.
Group(B+D): spinal anesthesia with hyperbaric bupivacaine 15mg (3ml of 0.5%)+DXM 1g/kg infused
intravenously in 100 ml of NS over 10 min.
Group(B+B):spinal anesthesia with hyperbaric bupivacaine 15mg (3ml of 0.5%)+ butorphanol 20g/kg infused
intravenously in 100 ml of NS over 10 min.
DOI: 10.9790/0853-14247478
www.iosrjournals.org
74 | Page
Intravenous dexmedetomidine and butorphanol prolongs bupivacaine sensory analgesia in
All patients were pre-medicated, a night before surgery with ranitidine 150 mg and alprazolam 0.25mg orally. In
the operation theatre, standard monitoring was attached and all patients were preloaded with 10ml/kg of Ringer
Lactate.
Spinal anesthesia was given using aseptic techniques in the sitting position at L4-L5 interspace via
midline approach using 25-G Quincke needle with3 ml of 0.5% hyperbaric bupivacaine. Patient was thenlaid in
supine position and operation table was kept flat with pillow under the head. Immediately after resuming supine
position, patients in Group(B) received IV infusion of 100 ml NS, Group(B+D) received IV infusion of DXM
diluted in 100 ml NS and Group(B+B) received butorphanol diluted in 100 ml NS. Infusion was given over
15mins in all the groups.
Heart rate, non-invasive arterial blood pressure and SpO2 were recorded in all three groups
preoperatively, intraoperatively and during shifting. Hypotension has been defined as systolic blood pressure
<90 mmHg or >30% decrease in baseline values and was treated with fluids boluses and injection
mephentermine 6mg IV. Tachycardia has been defined as heart rate >100/min and bradycardia has been defined
as heart rate <60/min and was treated with injection atropine 0.6 mg IV.
Sensory block was assessed by response to pin prick in mid-clavicular line bilaterally using a 20-G
hypodermic needle every two minutesinterval until the maximal level of sensory anesthesia is achieved and at 5
min interval thereafter. The time to reach the maximum level of sensory block and time for regression of two
segments in the maximum block height was noted.
The time for first analgesic requirement postoperatively or the time when the patient perceived pain for
the first time following spinal anesthesia was noted. Pain was assessed using VAS (visual analogue scale)
hourly for 24 hours.Duration of analgesia was defined as time from administration of subarachnoid block until
the first complaint of pain (VAS 4). Total number of rescue analgesia given was noted for 24 hours. Rescue
analgesia was given with paracetamol 10 mg/kg IV. Complications such as hypotension, bradycardia, nausea,
vomiting, shivering, and headache were noted and treated accordingly. An anesthesiologist, who was blinded to
the study drug used, documented all the parameters.
Statistical Analysis
Continuous data were summarized as MeanSD while discrete (categorical) in %. The outcome
measures(pulse rate, systolic BP, diastolic BP, SpO2, sedation score and VAS score) of three groups over the
periods(time) were compared by repeated measures two factor (Groups x Periods) analysis of variance
(ANOVA).Groups were also compared by one way ANOVA followed by Tukeys post hoc test. The
categorical variables were compared by chi-square (2) test. A two-sided (=2) p<0.05 was considered
statistically significant. All analyses were performed on SPSS 16.
III.
Results
The basic characteristics viz. age, gender, weight, height and ASA grade of the groups at admission
were found to be similar [Table 1]. Thus these variables did not affect the outcome of the study.The mean
baseline values of PR, SBP, DBP, RR and SpO2were recorded.The summary of sensory blockade and two
segment regression time is depicted in Table 2. Comparing the proportion of sensory blockade level and mean
time between the three groups ANOVA revealed significantly different sensory blockade level
(F=4.537,p=0.015) and time (p<0.05), respectively among the groups. Further, Tukey test was not significantly
differed (p>0.05) within group except B vs. B+D (p<0.01). Two segment regression time was 131.6551.38
min. in group (B), 211.0058.66 min. in group(B+D) and 181.6030.61min. In group(B+B), there was
significant difference (F=13.753, p<0.001). Further, Tukeytest also revealed significant (p<0.01) difference
within groups except (B+D) vs. (B+B) group which did not significantly differ (p=0.04).
Pain and analgesic usage summary (MeanSD) of three groups are depicted in Table 3.The pain
levels(VAS score) over 24 hrs. was 2.6 0.197 in group(B), 1.46 0.58 in group(B+D) and 1.38 0.54 in
group(B+B), there was significant difference (F=42.203,p<0.001)). Patients receiving DEX and butorphanol had
lower VAS (p=0.854) at all observed time compared to control group.1st Time requirement of analgesic was
193.7072.86 in group (B), 306.5057.70 in group (B+D) and 288.0076.20 in group(B+B), there was
significant difference (p<0.001). Further, Tukey test also revealed significant (p<0.05) difference within groups
except (B+D) vs. (B+B) group, which do not differed significantly (p=0.678).Use of analgesic was maximum in
group receiving only bupivacaine and similar in group(B+D) and (B+B) (p=0.09).
The frequency distributions of complications among three groups are summarized in Table 4/Fig. 1.
The complications such as hypotension, bradycardia, nausea and shivering were present in all three groups. The
intraoperative systolic blood pressure, diastolic blood pressure and heart rate for the study groups are presented
in Fig. 2, 3 & 4. Hypotension and shivering were higher in (B) group while bradycardia and nausea was higher
in (B+D) group. Comparing the proportion of each complication between the three groups, 2 test revealed
DOI: 10.9790/0853-14247478
www.iosrjournals.org
75 | Page
Intravenous dexmedetomidine and butorphanol prolongs bupivacaine sensory analgesia in
similar (p>0.05) proportion of complications among the groups except shivering, which was found significantly
(p 0.001) higher in (B) group as compared to both (B+D) and (B+B) groups.
IV.
Discussion
Dexmedetomidine (DXM) is a highly selective 2-adrenoceptor agonist. Small doses of DXM used in
combination with bupivacaine in humans for spinal anesthesia has been shown to produce a shorter onset and a
prolongation in the duration of sensory block with preserved hemodynamic stability and lack of
sedation.[2]DXM has been used for premedication and as an adjunct to general anesthesia. [3],[4],[5]Butorphanol
tartrate is a synthetic opioid partial agonist analgesic. Most of the observed behavioral, pharmacological, and
therapeutic effects appear due to its lower efficacy agonist actions at opioid receptors. Abboud et al. have
reported that epidural butorphanol cause dose dependent increase in duration of analgesia for relief of post
cesarean pain.[6]There have been studies which observed the effects of various intravenous anesthetic agents on
the characterstics of subarachnoid block produced by hyperbaric or isobaric bupivacaine.In one comparative
study theintravenous midazolam and DXM have been shown to increase the duration and height of sensory
block.[7]In few recent studies DXM has been studied separately as intravenous adjunct to intrathecal
bupivacainebut there is no study for intravenous butorphanol as an adjunct to intrathecalbupivacaine. It has been
mostly used for post-operative analgesia; its intraoperative role has been studied in our study. Our study not
only compared the role of intravenousDXM and butorphanol in lower abdominal surgeries, it also gave us an
idea about their individual performance separately.Alpha 2 receptors are found in the peripheral and central
nervous systems, platelets, and many other organs, including the liver, pancreas, kidney, and eye. Stimulation of
the receptors in the brain and spinal cord inhibits neuronal firing, causing hypotension, bradycardia, sedation,
and analgesia.The analgesic effect primarily results from the inhibition of locus ceruleus at the brain stem. In
addition, dexmedetomidine infusion may result in increased activation of alpha-2 receptors at the spinal cord
resulting in inhibition of nociceptive impulse transmission. Intravenous DXM alone have been shown to
increase the duration of sensory and motor block of isobaric bupivacaine.[8,9,10] The dose of DXM used to
prolong the effect of intrathecal bupivacaine varies between 0.25 g/kg to 1 g/kg. Although, 0.25 g/kg of
intravenous DXM has been found effective in exaggerating the effects of intrathecal bupivacine, we used single
bolus of DXM(1g/kg) as it is recommended loading dose.[11]In most of the studies, DXM infusion used as a
loading dose followed by an infusion has been found to prolong the duration of analgesia and motor blockade.
Butorphanol, 20-40g/kg i.v. was comparable or preferable to fentanyl 1-2 g/kg i.v. as a supplement to
balanced anesthesia in most studies.[12]Butorphanol is used in the treatment of moderate to severe pain
associated with as orthopedic issues, burns, renal colic, and surgical. Groups receiving butorphanol as a part of
balanced anesthesia were reported to be satisfied with their anesthetic experience, require less post-operative
analgesiaand also reported postoperative drowsiness and sedation.[13]Due to the extensive hepatic metabolism of
butorphanol, oral bioavailability is approximately 5 to 17%. Peak plasma concentrations of 1.5 ng/mL
butorphanol occur almost immediately after a single 1mg i.v. administration.
Apparent plasma half-lives of butorphanol were between 6 and 10 hours.[14]Intrathecal butorphanol
potentiates bupivacaine-induced sensory spinal block and reduces the analgesic requirement in the early postoperative period without prolonging motor block recovery time.[15]In our study, in all the three groups, the mean
time to reach maximum sensory level was highest in control group followed by butorphanol group and DXM
group with the least. Thus it is evident that both adjuncts were efficacious in decreasing onset of sensory
blockade with DXM more effective. In our study, VAS score was significantly different among all groups. It
was highest in the control group than the DXM and butorphanol group. Studies have showed that i.v DXM can
prolong time to first analgesic request associated with spinal anesthesia. [16] In butorphanol also the time for
requirement of first analgesia was prolonged compared to control group. Similarly, epidural, intravenous, or
intramuscular butorphanol can prolong analgesia of other agents and reduce opioid-induced nausea and pruritus.
The analgesic effect of butorphanol is influenced by the route of administration. Onset of analgesia is
within a few minutes for intravenous administration and within 15 minutes for intramuscular injection. [17] Both
showed almost similar time for requirement of first analgesia. No. of rescue analgesia was significantly lowered
in DXM and butorphanol than the control group.DXM also provides intense analgesia during the postoperative
period. In one study, by Venn RM et al, the postoperative analgesic requirements were reduced by 50% in
cardiac patients and the need for rescue midazolam for sedation was diminished by 80%. [18]In our study as we
used loading of 1microgm/kg DXM only and found more prolonged two segment regression time
(211.0058.6min) than the study using continuous infusion.[10] Thus, we found that both the drugs significantly
delay sensory emergence.
V.
Conclusion
Overall DXM is equipotent to butorphanol in prolongation of sensory analgesia and provide better post
operative analgesia than the group in which no intravenous adjuvant is used.
DOI: 10.9790/0853-14247478
www.iosrjournals.org
76 | Page
Intravenous dexmedetomidine and butorphanol prolongs bupivacaine sensory analgesia in
References
[1].
[2].
[3].
[4].
[5].
[6].
[7].
[8].
[9].
[10].
[11].
[12].
[13].
[14].
[15].
[16].
[17].
[18].
Corning, JL (1888). "A Further Contribution On Local Medication Of The Spinal Cord, With Cases". New York Medical Record:
2913.
Kanazi GE, Aouad MT, Jabbour-Khoury SI. Effect Of Low-Dose Dexmedetomidine Or Clonidine On The Characteristics Of
Bupivacaine Spinal Block. ActaAnaesthesiol Scand. 2006; 50:222-7.
Aantaa RE, Kanto JH, Scheinin M, Kallio AM, Scheinin H: DexmedetomidinePremedication For Minor Gynecologic Surgery.
AnesthAnalg; 1990, 70(4):407-13.
Bhrer M, Mappes A, Lauber R, Stanski DR, Maitre PO: Dexmedetomidine Decreases Thiopental Dose Requirement And Alters
Distribution Pharmacokinetics. Anesthesiology; 1994, 80:1216-27.
Scheinin B, Lindgren L, Randell T, Scheinin H, Scheinin M. DexmedetomidineAttenuates Sympathoadrenal Responses To Tracheal
Intubation And Reduces The Need For Thiopentone And Preoperative Fentanyl. Br J Anaesth; 1992, 68:126 -31.
Abboud TK, Moore M, Zhu J, Murakawa K, Minehart M, Longhitano M. Et Al. Epidural Butorphanol Or Morphine For The Relief
Of Post- Caesarean Section Pain: VentilatoryResponses To Carbon Dioxide-AnesthAnalg1987;66:887-93.
Kaya FN, Yavascaoglu B, Turker G, Yildirim A, Gurbet A, Mogol EB, Et Al. Intravenous Dexmedetomidine, But Not Midazolam,
Prolongs Bupivacaine Spinal Anesthesia. Can J Anaesth. 2010 Jan; 57(1):39-45.
Al-Mustafa MM, Badran IZ, Abu-Ali HM, Al-Barazangi BA, Massad IM, Al-Ghanem SM:Intravenous Dexmedetomidine Prolongs
Bupivacaine Spinal Analgesia. Middle East J Anesthesiol.2009 Jun; 20(2):225-31.
Hong JY, Kim WO, Yoon Y, Choi Y, Kim SH, Kil HK. Effects Of Intravenous Dexmedetomidine On Low-Dose Bupivacaine
Spinal Anesthesia In Elderly Patients.ActaAnaesthesiol Scand. 2012 Mar; 56(3):382-7.
Harsoor SS, Rani DD, Yalamuru B, Sudheesh K, Nethra SS. Effect Of Supplementation Of Low Dose Intravenous
Dexmedetomidine On Characteristics Of Spinal Anesthesia With Hyperbaric Bupivacaine. Indian J Anaesth2013; 57:265-9.
Jung SH, Lee SK, Lim KJ, Park EY, Kang MH, Lee JMEt Al : The Effects Of Single-Dose Intravenous Dexmedetomidine On
Hyperbaric Bupivacaine Spinal Anesthesia.JAnesth. 2013 Jun; 27(3):380-4.
Abbott Labaratories. Precedex. Dexmedetomidine Hydrochloride Injection Prescribing Information. Abbott Labaratories, USA,
2000.
Ranga Chari VR, Goyal AA, Singh V. A Study Of Addition Of Inj.ButorphanolTo Hyperbaric Inj.BupivacaineGiven Intrathecally
To Patients Undergoing Lower Segment Caesarean Section: A Randomized, Controlled Trial. Med J DY PatilUniv2013; 6:156-60.
Abdallah FW, Abrishami A, Brull R. The Facilitatory Effects Of Intravenous Dexmedetomidine On The Duration Of Spinal
Anesthesia: A Systematic Review And Meta-Analysis. AnesthAnalg. 2013 Jul; 117(1):271-8.
Gear, RW; Miaskowski C, Gordon NC, Paul SM, Heller PH, Levine JD (November 1999). "The Kappa Opioid Nalbuphine
Produces Gender- And Dose-Dependent Analgesia And Antianalgesia In Patients With Postoperative Pain". Pain83 (2): 33945.
Abdallah FW, Abrishami A, Brull R. The Facilitatory Effects Of Intravenous Dexmedetomidine On The Duration Of Spinal
Anesthesia: A Systematic Review And Meta-Analysis. AnesthAnalg. 2013 Jul;117(1):271-8.
Gear, RW; Miaskowski C, Gordon NC, Paul SM, Heller PH, Levine JD (November 1999). "The Kappa Opioid Nalbuphine
Produces Gender- And Dose-Dependent Analgesia And Antianalgesia In Patients With Postoperative Pain". Pain83 (2): 33945.
Venn RM, Bradshaw CJ, Spencer R, Brealey D, Caudwell E, Naughton C, Vedio A, Singer M, Feneck R, Treacher D, Willatts SM,
Grounds RM. Preliminary UK Experience Of Dexmedetomidine, A Novel Agent For Postoperative Sedation In The Intensive Care
Unit. Anesthesia. 1999;54:113642.
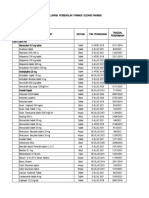
Table 1: Basic characteristics of three groups.
Table 2: Summary of sensory blockade and two segment regression time.
Sensory Blockade
Levels:
T4
T6
T7
T8
T10
Time (min)
Two
segment
regression time
(min)
Group (B)
(n=20)
Group (B+D)
(n=20)
Group (B+B)
(n=20)
3
6
1
3
7
8.253.45
1
10
0
9
0
6.101.65
1
11
1
7
0
6.501.64
131.6551.38
211.0058.66
181.6030.61
P
Value
p<0.05
p<0.05
p<0.001
Table 3:Pain and analgesic usage summary (MeanSD) ofthreegroups.
Group
(B)
VAS Score
1st Time requirement of
Analgesic (min)
Rescue Analgesia (no.)
DOI: 10.9790/0853-14247478
Group
(B+D)
Group
(B+B)
P Value
2.60.197
1.460.58
1.380.54
p<0.001
193.7072.86
3.81.20
306.5057.70
2.40.88
288.0076.20
2.551.15
p<0.001
p<0.001
www.iosrjournals.org
77 | Page
Intravenous dexmedetomidine and butorphanol prolongs bupivacaine sensory analgesia in
Table 4: Frequency distribution of complications of three groups.
Complications
Hypotension
Bradycardia
Nausea
Vomiting
Shivering
(B)
(n=20)
3 (15.0%)
4 (20.0%)
2 (20.0%)
0 (0.0%)
6 (30.0%)
(B+D) (n=20)
1 (5.0%)
8 (40.0%)
4 (20.0%)
0 (0.0%)
1 (5.0%)
(B+B) (n=20)
1 (5.0%)
3 (15.0%)
1 (5.0%)
0 (0.0%)
2 (10.0%)
PValue
0.129
0.372
0.585
0.200
0.001
Fig.1: Frequency distribution of Complicationsamong three groups.
Fig.2: Mean SBP of three groups over the periods.
Fig.3: Mean DBP of three groups over the periods.
Fig.4: Comparative pulse rate of three groups.
DOI: 10.9790/0853-14247478
www.iosrjournals.org
78 | Page
You might also like
- Dope Test For Driving LicenseDocument1 pageDope Test For Driving LicenseArif Hagan100% (4)
- NarcanDocument1 pageNarcanKatie McPeekNo ratings yet
- Applied Biopharmaceutics & Pharmacokinetics, 5th EditionDocument1 pageApplied Biopharmaceutics & Pharmacokinetics, 5th Editionbencleese14% (7)
- PTCB Exam 1Document20 pagesPTCB Exam 1Amber Chen80% (5)
- REGULATORYDocument19 pagesREGULATORYsrishty100% (1)
- The Effects of Dexmedetomidine Added To Spinal Bupivacaine For Lower Limb SurgeryDocument4 pagesThe Effects of Dexmedetomidine Added To Spinal Bupivacaine For Lower Limb SurgeryInternational Organization of Scientific Research (IOSR)No ratings yet
- Journal Homepage: - : IntroductionDocument5 pagesJournal Homepage: - : IntroductionIJAR JOURNALNo ratings yet
- Anesth Essays ResDocument8 pagesAnesth Essays ResFi NoNo ratings yet
- Ijhs 8383+12635 12654Document20 pagesIjhs 8383+12635 12654Muhammad Daniala SyuhadaNo ratings yet
- Does Intravenous Low Dose Dexmedetomidine Supplementation Has Beneficial Effects On Spinal Anaesthesia?Document4 pagesDoes Intravenous Low Dose Dexmedetomidine Supplementation Has Beneficial Effects On Spinal Anaesthesia?MOHAMMED IQBALNo ratings yet
- 11 LdpopDocument5 pages11 LdpopBaru Chandrasekhar RaoNo ratings yet
- DR Surekha S Chavan, DR Stephan Jebaraj & DR Priya ChavreDocument10 pagesDR Surekha S Chavan, DR Stephan Jebaraj & DR Priya ChavreTJPRC PublicationsNo ratings yet
- Comparison of Analgesic Effects of Intravenous Nalbuphine and Pentazocine in Patients Posted For Short-Duration Surgeries A Prospective Randomized Double-Blinded StudyDocument4 pagesComparison of Analgesic Effects of Intravenous Nalbuphine and Pentazocine in Patients Posted For Short-Duration Surgeries A Prospective Randomized Double-Blinded StudyMuhammad AtifNo ratings yet
- Comparison of Hyperbaric Levobupivacaine/ Bupivacaine For Ceserean SectionDocument6 pagesComparison of Hyperbaric Levobupivacaine/ Bupivacaine For Ceserean SectionIJAR JOURNALNo ratings yet
- Journal Reading AnestesiDocument4 pagesJournal Reading AnestesiVania RNo ratings yet
- DR Sourab Bokil ThesisDocument8 pagesDR Sourab Bokil ThesisPurushotham N PuruNo ratings yet
- International Journal of Health Sciences and ResearchDocument7 pagesInternational Journal of Health Sciences and ResearchAritha HandricoNo ratings yet
- Artigo - Auricular AcupunctureDocument2 pagesArtigo - Auricular AcupunctureAry NogueiraNo ratings yet
- Analgesic Efficacy of Ultrasound-Guided Transversus Abdominis Plane Block in Patients Undergoing Laparoscopic AppendicectomyDocument9 pagesAnalgesic Efficacy of Ultrasound-Guided Transversus Abdominis Plane Block in Patients Undergoing Laparoscopic AppendicectomyIJAR JOURNALNo ratings yet
- Effectiveness of Fascia Iliaca Compartment Block For Post Operative Analgesia After Surgery For Femur Bone FractureDocument12 pagesEffectiveness of Fascia Iliaca Compartment Block For Post Operative Analgesia After Surgery For Femur Bone FractureIJAR JOURNALNo ratings yet
- 1 s2.0 S0007091217366175 MainDocument5 pages1 s2.0 S0007091217366175 MainMeutia LaksaniNo ratings yet
- Fentanyl Versus Tramadol As An Adjunct TDocument8 pagesFentanyl Versus Tramadol As An Adjunct TRabnawaz BanGashNo ratings yet
- Tramadol en NiñosDocument5 pagesTramadol en NiñosElias Vera RojasNo ratings yet
- HBO Femoral Head NecrosisDocument6 pagesHBO Femoral Head NecrosisMarica MonaNo ratings yet
- Original Research Article: Anurag Bijalwan, Pradeep Singhal, Syed AltamashDocument7 pagesOriginal Research Article: Anurag Bijalwan, Pradeep Singhal, Syed Altamashagus sukarnaNo ratings yet
- SivevskiDocument12 pagesSivevskiPalwasha MalikNo ratings yet
- Critical AppraisalDocument13 pagesCritical AppraisalRatna Widiyanti KNo ratings yet
- AnesDocument8 pagesAnesrachma30No ratings yet
- SynopsisDocument14 pagesSynopsisAqeel AhmadNo ratings yet
- Intrathecal Fentanyl Prolongs Sensory Bupivacaine Spinal BlockDocument5 pagesIntrathecal Fentanyl Prolongs Sensory Bupivacaine Spinal BlockRezza HaryNo ratings yet
- DR T. Suryasree, DR K. Indira Priya Darshini, DR PratikshaDocument9 pagesDR T. Suryasree, DR K. Indira Priya Darshini, DR PratikshaIOSRjournalNo ratings yet
- Rawal Medical JournalDocument8 pagesRawal Medical JournalBahRunNo ratings yet
- Asfr 2 QrqwasfcagsevDocument6 pagesAsfr 2 QrqwasfcagsevkennydimitraNo ratings yet
- Kumar S.Document4 pagesKumar S.Van DaoNo ratings yet
- Randomized Controlled Trial of The Effect of Depth of Anaesthesia On Postoperative PainDocument6 pagesRandomized Controlled Trial of The Effect of Depth of Anaesthesia On Postoperative PainIntan PurnamasariNo ratings yet
- 4services On DemandDocument9 pages4services On DemandDe WiNo ratings yet
- Complementary Therapies in Clinical Practice: SciencedirectDocument5 pagesComplementary Therapies in Clinical Practice: Sciencedirectbara muhammadNo ratings yet
- 2 Material and Methods 2.1 Patient Collective 2.1.1 Selection of Sample ScopeDocument46 pages2 Material and Methods 2.1 Patient Collective 2.1.1 Selection of Sample ScopeSystematic ReviewsNo ratings yet
- Dr. - Nataraj - EJCM 132 1888 1893 2023Document7 pagesDr. - Nataraj - EJCM 132 1888 1893 2023vithz kNo ratings yet
- Comparison of The Efficacy of Physical Therapy andDocument5 pagesComparison of The Efficacy of Physical Therapy andfi.afifah NurNo ratings yet
- PRM2017 1721460 PDFDocument6 pagesPRM2017 1721460 PDFmikoNo ratings yet
- Jurnal Bariyah 1Document6 pagesJurnal Bariyah 1Ratrika SariNo ratings yet
- Eledjam1991 Article BrachialPlexusBlockWithBupivac PDFDocument6 pagesEledjam1991 Article BrachialPlexusBlockWithBupivac PDFKalpanaNo ratings yet
- Intrathecal Fentanyl For Prevention of Shivering in Spinal Anesthesia in Cesarean SectionDocument5 pagesIntrathecal Fentanyl For Prevention of Shivering in Spinal Anesthesia in Cesarean SectionMuhammad Habibi NstNo ratings yet
- Xia 2018Document7 pagesXia 2018Jefferson891127No ratings yet
- Analgesic 3Document7 pagesAnalgesic 3Indra T BudiantoNo ratings yet
- Mode of Action of Cupping - Local Metabolism and Pain Thresholds in Neck Pain Patients and Healthy SubjectsDocument14 pagesMode of Action of Cupping - Local Metabolism and Pain Thresholds in Neck Pain Patients and Healthy Subjectsdwi putri ratehNo ratings yet
- e507d2a9-15d1-4ffe-96d4-dccb4188b121Document12 pagese507d2a9-15d1-4ffe-96d4-dccb4188b121Julio AltamiranoNo ratings yet
- 1878-Article Text-5104-1-10-20210310Document4 pages1878-Article Text-5104-1-10-20210310kiki 13No ratings yet
- DexamethasoneDocument8 pagesDexamethasoneTenzinNo ratings yet
- Anaesthesia - February 1994 - Ørntoft - A Comparison of Pre and Postoperative Tonsillar Infiltration With Bupivacaine OnDocument4 pagesAnaesthesia - February 1994 - Ørntoft - A Comparison of Pre and Postoperative Tonsillar Infiltration With Bupivacaine Onnagraj18kalyaniNo ratings yet
- Double-Blind Randomized Controlled Trial of Caudal Versus Intravenous S (+) - Ketamine For Supplementation in Caudal Analgesia in ChildrenDocument35 pagesDouble-Blind Randomized Controlled Trial of Caudal Versus Intravenous S (+) - Ketamine For Supplementation in Caudal Analgesia in ChildrennabilchyNo ratings yet
- Low Dose Levobupivacaıne 0.5% With Fentanyl in Spinal Anaesthesia For Transurethral Resection of Prostate SurgeryDocument6 pagesLow Dose Levobupivacaıne 0.5% With Fentanyl in Spinal Anaesthesia For Transurethral Resection of Prostate Surgeryblabarry1109No ratings yet
- Effect of Dexamethasone As An Adjuvant To Bupivacaine in Ultrasound Guided Interscalene Brachial Plexus Block in Upper Arm SurgeriesDocument16 pagesEffect of Dexamethasone As An Adjuvant To Bupivacaine in Ultrasound Guided Interscalene Brachial Plexus Block in Upper Arm SurgeriesIJAR JOURNALNo ratings yet
- IndianJAnaesth542116-1332734 034207Document5 pagesIndianJAnaesth542116-1332734 034207balab2311No ratings yet
- Chauan - Effects of Phenylephrine and Ephedrine inDocument15 pagesChauan - Effects of Phenylephrine and Ephedrine inFadil AhmadNo ratings yet
- Anesthesia & ClinicalDocument4 pagesAnesthesia & Clinicalreinhard fourayNo ratings yet
- The Effectiveness of Magnesium Sulphate Intravenous Bolus or Added As An Adjunct To Ropivacaine For Brachial Plexus Block in Upper Limb Orthopaedic SurgeriesDocument7 pagesThe Effectiveness of Magnesium Sulphate Intravenous Bolus or Added As An Adjunct To Ropivacaine For Brachial Plexus Block in Upper Limb Orthopaedic SurgeriesInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- IJISRT23JUN363Document7 pagesIJISRT23JUN363International Journal of Innovative Science and Research TechnologyNo ratings yet
- A Comparative Study of Intrathecal Plain Bupivacaine Versus Bupivacaine With Midazolam For Subarachnoid Block in Lower Abdominal and Lower Limb SurgeriesDocument4 pagesA Comparative Study of Intrathecal Plain Bupivacaine Versus Bupivacaine With Midazolam For Subarachnoid Block in Lower Abdominal and Lower Limb SurgeriesInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- JAnaesthClinPharmacol294459-335648 091924 PDFDocument6 pagesJAnaesthClinPharmacol294459-335648 091924 PDFaltaikhsannurNo ratings yet
- Levobupivacaine and Bupivacaine in Spinal Anesthesia For Transurethral Endoscopic SurgeryDocument7 pagesLevobupivacaine and Bupivacaine in Spinal Anesthesia For Transurethral Endoscopic SurgeryCassandraBussinkNo ratings yet
- Revista Brasileira DE AnestesiologiaDocument9 pagesRevista Brasileira DE AnestesiologiayulianiNo ratings yet
- Dexme IntratechalDocument5 pagesDexme IntratechalDianWindiAmaliaNo ratings yet
- Top Trials in Gastroenterology & HepatologyFrom EverandTop Trials in Gastroenterology & HepatologyRating: 4.5 out of 5 stars4.5/5 (7)
- Effects of Formative Assessment On Mathematics Test Anxiety and Performance of Senior Secondary School Students in Jos, NigeriaDocument10 pagesEffects of Formative Assessment On Mathematics Test Anxiety and Performance of Senior Secondary School Students in Jos, NigeriaInternational Organization of Scientific Research (IOSR)100% (1)
- Necessary Evils of Private Tuition: A Case StudyDocument6 pagesNecessary Evils of Private Tuition: A Case StudyInternational Organization of Scientific Research (IOSR)No ratings yet
- Comparison of Explosive Strength Between Football and Volley Ball Players of Jamboni BlockDocument2 pagesComparison of Explosive Strength Between Football and Volley Ball Players of Jamboni BlockInternational Organization of Scientific Research (IOSR)No ratings yet
- Youth Entrepreneurship: Opportunities and Challenges in IndiaDocument5 pagesYouth Entrepreneurship: Opportunities and Challenges in IndiaInternational Organization of Scientific Research (IOSR)100% (1)
- Factors Affecting Success of Construction ProjectDocument10 pagesFactors Affecting Success of Construction ProjectInternational Organization of Scientific Research (IOSR)No ratings yet
- Design and Analysis of Ladder Frame Chassis Considering Support at Contact Region of Leaf Spring and Chassis FrameDocument9 pagesDesign and Analysis of Ladder Frame Chassis Considering Support at Contact Region of Leaf Spring and Chassis FrameInternational Organization of Scientific Research (IOSR)No ratings yet
- Design and Analysis of An Automotive Front Bumper Beam For Low-Speed ImpactDocument11 pagesDesign and Analysis of An Automotive Front Bumper Beam For Low-Speed ImpactInternational Organization of Scientific Research (IOSR)No ratings yet
- Fatigue Analysis of A Piston Ring by Using Finite Element AnalysisDocument4 pagesFatigue Analysis of A Piston Ring by Using Finite Element AnalysisInternational Organization of Scientific Research (IOSR)No ratings yet
- Administrative Medical Assisting 8th Edition French Test BankDocument10 pagesAdministrative Medical Assisting 8th Edition French Test Bankcrystalolson09071990ynb100% (41)
- NubainDocument2 pagesNubainJose Luis HernandezNo ratings yet
- Opioid AnalgesicsDocument16 pagesOpioid AnalgesicsSanthosh Krishna RajanNo ratings yet
- Puskesmas: Sambungmacan 1 Kecamatan: Sambungmacan Kabupaten: SragenDocument605 pagesPuskesmas: Sambungmacan 1 Kecamatan: Sambungmacan Kabupaten: SragenRobed Nur CahyonoNo ratings yet
- Misoprostol: Pharmacokinetic Profiles, Effects On The Uterus and Side-EffectsDocument8 pagesMisoprostol: Pharmacokinetic Profiles, Effects On The Uterus and Side-EffectsFarrukh Ali KhanNo ratings yet
- Chapter 11 Multiple Dosage RegimenDocument35 pagesChapter 11 Multiple Dosage RegimenYuli Irvaransiah DIatun NIkmah100% (2)
- History of PharmacologyDocument26 pagesHistory of PharmacologyHollan Galicia100% (1)
- Tracey Jones (Desertation)Document63 pagesTracey Jones (Desertation)David Abdul KonnehNo ratings yet
- Diuretics Pharmacology 79 88Document6 pagesDiuretics Pharmacology 79 88Neha RoyNo ratings yet
- Day 2 QuizDocument2 pagesDay 2 QuizAngie MandeoyaNo ratings yet
- Formulary - 2014Document20 pagesFormulary - 2014vijay kumarNo ratings yet
- Miostat InjDocument4 pagesMiostat InjSri Wahyuni HandayaniNo ratings yet
- Oral Disintegrating Tablets A Future CompactionDocument10 pagesOral Disintegrating Tablets A Future CompactionArifin I. OputuNo ratings yet
- EpiPen CaseDocument5 pagesEpiPen CaseTanvi RastogiNo ratings yet
- Approved Drug Products Supl 2009Document141 pagesApproved Drug Products Supl 2009Mada madalinaNo ratings yet
- Scottish MDSDocument7 pagesScottish MDSQasim AkhtarNo ratings yet
- INDIA BUSINESS Product List 1Document41 pagesINDIA BUSINESS Product List 1Tanisha AgarwalNo ratings yet
- ph16 03 02 1016 MEDICINEDocument15 pagesph16 03 02 1016 MEDICINEAlaa DarwishNo ratings yet
- DesomorphineDocument8 pagesDesomorphineMarcNo ratings yet
- Ceftriazone (Rocephin)Document1 pageCeftriazone (Rocephin)Adrianne BazoNo ratings yet
- Estradiol TransdermalDocument8 pagesEstradiol TransdermalAditya Krishna MurthiNo ratings yet
- Notes On Drugs in Peptic Ulcer and Biliary Diseases 2021Document7 pagesNotes On Drugs in Peptic Ulcer and Biliary Diseases 2021CARMEL CHRISTY CHRISTOPHER -No ratings yet
- Trends in The Global Immuno-Oncology Landscape: From The Analyst'S CouchDocument2 pagesTrends in The Global Immuno-Oncology Landscape: From The Analyst'S CouchnagarajharishNo ratings yet
- A. Gudang Farmasi 2023 (Feni Dwi) UpdateDocument882 pagesA. Gudang Farmasi 2023 (Feni Dwi) UpdatehefikurniasariNo ratings yet
- Moh PaperDocument160 pagesMoh PaperManisanthosh Kumar100% (2)