Professional Documents
Culture Documents
Condyloma Acuminatum: Some Aspects: Arūnas Rimkevičius, Alina Pūrienė, Mindaugas Gaigalas
Condyloma Acuminatum: Some Aspects: Arūnas Rimkevičius, Alina Pūrienė, Mindaugas Gaigalas
Uploaded by
faizawidiOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Condyloma Acuminatum: Some Aspects: Arūnas Rimkevičius, Alina Pūrienė, Mindaugas Gaigalas
Condyloma Acuminatum: Some Aspects: Arūnas Rimkevičius, Alina Pūrienė, Mindaugas Gaigalas
Uploaded by
faizawidiCopyright:
Available Formats
ACTA MEDICA LITUANICA. 2011. Vol. 18. No. 2. P.
4346
Lietuvos moksl akademija, 2011
Condyloma acuminatum: some aspects
ArnasRimkeviius,
AlinaPrien,
MindaugasGaigalas
Condyloma acuminatum is a rare human papilloma virus (HPV) related to oral lesion. The purpose of the article is to present a 42-year-old patient with condyloma
acuminatum and to review references on the subject-related etiological, pathological,
diagnostic and treatment aspects.
Keywords: condyloma acuminatum, oral mucosa, papilloma virus, HIV
Institute of Odontology,
Faculty of Medicine,
Vilnius University,
Vilnius, Lithuania
INTRODUCTION
Condyloma acuminatum is a verrucous or papillary growth
infectious lesion that is characteristically located in the
anogenital region but may also involve the oral mucosa
(1). Oral lesions are ordinarily located on the mucosa of
the gingiva, cheeks, lips and hard palate or at the site of the
contact / traumatic event on non-keratinized tissues (2).
The prevalence rate seems to be similar in men and women,
and the frequency of clinically apparent cases has been recorded at 1% in the sexually active population. It has been
etiologically related to human papilloma virus (HPV) subtypes 6 and 11, sometimes 16 and 18 (3, 4). Nearly 70 different strains of the virus exist, and 8 types are known to
cause pre-cancerous or cancerous changes (9). At present,
it is impossible to tell from a biopsy specimen which specific type of the virus was diagnosed in the patient, but the
biopsy is expected at least to show the presence or absence
of any pre-cancerous or cancerous changes. The maturation
of various subtypes of HPV within oral and genital mucosal
cells is essentially the same. Keratinized cells act as a virus
host, with replication linked to the process of keratinization. An increasing frequency of this lesion has been noted
in HIV-infected patients. The disease can be transmitted
sexually and characteristically grows as a group of numerous pink nodules (5, 6). There are certain strains of the virus
Correspondence to: Alina Prien, algiris Clinic, Vilnius
University Hospital, algirio 117, LT-08217 Vilnius, Lithuania.
E-mail:alina.puriene@mf.vu.lt
that are not necessarily transmitted sexually, i.e. they may
be contracted by merely getting the virus on ones hands.
Oral lesions can occur without the accompanying anogenital disease. The exact incubation time is unknown but has
been indicated to range from 3 weeks to 8 months by most
researchers in the area (8).
In some instances, condyloma acuminatum may resemble focal epithelial hyperplasia. The differential diagnosis
should also include condylomas from verruca vulgaris,
multiple squamous papillomas and oral mucosal lesions of
Cowdens (multiple hamartoma) syndrome (7).
Multiple medical treatments are available to remove
condyloma acuminatum; the main strategy is to eliminate
as many of the visible lesions as possible until the host immune system can control viral replication. Surgical excision
may be performed by cryosurgery, scalpel, electro desiccation, or laser ablation; however, not a single medical treatment technique can be referred to as in all instances preferable in respect of others. Patients should be informed that
after treatment the virus may endure and lesion reoccurrences are possible. The first case study of oral condyloma
was reported in 1967 by Knapp and Uohara (9).
The disease is sexually transmitted; therefore, the risk
of acquiring HPV is primarily dependent on several factors
related to sexual activity. These factors include the number
of sexual partners, frequency of sexual intercourse, and the
presence of genital warts on sexual partners. In most studies, cigarette smoking is a risk factor after controlling for
sexual behaviour (7). Latex condoms offer some, but not
complete, protection in the transmission of HPV. The most
44
ArnasRimkeviius, AlinaPrien, MindaugasGaigalas
A 42-year-old male applied to the algiris Clinic of Vilnius
University Hospital. The patient complained of a group of
growing lesions on the anterior part of his tongue. Lesions
had been first noticed almost two years ago and never treated.
No other symptoms were identified. Quite characteristically,
oral examination revealed on the tongue and buccal mucosas a group of multiple oral asymptomatic nodules, pink to
red in colour, with thin feet, less broad-based, soft texture
reminiscent of cauliflower, variably sized, up to 23cm on
the patients tongue. Three lesions were located at the contact/traumatic side of the tongue (Figs.1 and 2). The diag-
nostics of such oral lesions was based on the clinical evaluation, followed by cytology which was further confirmed by
biopsy. Such oral lesions may be an oral manifestation of HIV
infection, thus additional laboratory diagnostics for HIV infection and other sexually transmitted diseases were requested. The tests for other diseases were negative, so the lesions
were surgically removed by excisional biopsy under local
anesthesia and sutured with Vicryl 50 sutures. The histopathological examination of the oral lesion, performed by the
National Center of Pathology, revealed an exophytic papillary
squamous proliferation, hyperplastic epithelium irregularly
thickened by acanthosis and a concentration of parakeratosis, with identification of koilocytes (Fig.3), without evidence
of dysplastic changes. Koilocytes, a hallmark of condyloma
acuminatum and HPV infection-modified keratinocytes,
were found in the upper spinous and corneal layers.
After surgical treatment, the patient was informed
about possible recurrences which are common and presumably are related to the surrounding appearingly normal
tissue that may act as an infectious agent.
Fig.1. 42-year-old man with a group of nodules
up to 2 to 3 cm on the tongue
Fig.3. Photomicrograph (hematoxylin and eosin 200).
Koilocytic cells are visible in the epithelium
Fig.2. Lesions located at the contact/traumatic side
on the tongue and buccal mucosa
Fig.4. Patient after final healing
efficient prevention against condyloma acuminatum is provided by abstinence from sex or by the human papillomavirus vaccine (18).
The present report describes a 42-year-old man with
typical oral mucosa and histopathological features of oral
condyloma acuminatum and no HIV infection.
CASE PRESENTATION
Condyloma acuminatum: some aspects
45
DISCUSSION
CONCLUSION
The understanding of human papilloma virus disease has
significantly improved over the last 20 years, however, leaving a number of key issues unaddressed and requiring
some further research, with a view to evaluating the factors
relevant for the progression and regression of the disease.
HPV is one of the DNA-containing viruses that replicate the
flat epithelial cell nuclei. The genome encodes six early open
reading frames (E1, E2, E4, E5, E6 and E7) and two late open
reading frames (L1, L2). The E genes encode proteins important in the regulatory function, and the L genes encode
for viral capsid proteins. This group of viruses can infect
many different sites, including the larynx, skin, mouth, eso
phagus, and the anogenital tract. HPV induces proliferative
changes, both benign and malignant, in the stratified squamous epithelium in the epidermis and mucous membranes.
Without spontaneous regression, the clinical appearance of
condyloma acuminatum is similar to focal epithelial hyperplasia, and the histological distinction between these two
conditions also presents difficulties (11). There are no universally accepted microscopic features that can be used to
separate these diseases reliably, without clinical view differences; the lesions may be classified reliably only by means
of DNA hybridization studies (11).
Recurrences are common for both diseases and perhaps
are related to the surrounding normal-appearing tissue that
may be harboring the infectious agent. The treatment for
these lesions is generally surgical excision by cryosurgery,
scalpel, electrodessication, or laser ablation with no evidence of any treatment advantage (18). Surgical excision is
the most popular method used by doctors, especially when
biopsy is indicated (appropriate indications have obtained
by means of biopsy).
Sexually active adults aged 1524 account for approximately one half of new HPV infections each year (12).
HPV contributes to 90% of anal cancers and 40% of vulva,
vaginal, and penile cancers (13, 14). Squamous cell carcinoma of the oropharynx is associated with HPV in 50%
of cases. HPV-16 and HPV-18 subtypes can be recovered
in approximately 70% of squamous cell carcinomas of the
cervix (15, 16). A human papillomavirus (HPV) quadrivalent vaccine is now available for prevention of HPVassociated dysplasias and neoplasias, including cervical
cancer, genital warts (condyloma acuminatum), and precancerous genital lesions (18). Nevertheless, the relation
between these viruses and the pathogenic cancer in the
oral mucosa remains controversial, and there appears to
be more impact of HPV with other chemical and physical
carcinogens such as tobacco and alcohol. The importance
of multifactor aspects of mouth cancer and also the possibile of influence of the HPV and Epstein Barr virus should
be highlighted (17).
Oral condylomas are very rare, and a long-term postoperative follow-up is necessary to crosscheck the recurrences of
these lesions due to their prognosis. Patients who undergo
therapy for condyloma acuminatum should have a clinical
examination some 3 to 6 months after treatment, and regular yearly visits are recommended afterwards.
Received 20 April 2011
Accepted 26 May 2011
References
1. LeverWF, LeverG. Histopathology of the Skin. 5th ed.
Philadelphia: JB Lippincott. 1975: 352.
2. Ashiru JO, Ogunbanjo BO, Rotowa NA, AdeyemiDoro FA, Osoba AO. Intra-oral Condylomata acuminata. A case report. Br J Vener Dis. 1983; 59(5): 3256.
3. Oriel JD, Almeida JD. Demonstration of virus particles in human genital warts. Br J Vener Dis. 1970; 46:
3742.
4. Praetorius-ClavsenF. Rare oral viral disorders (molluscum contagiosum, localized keratoacanthoma, verrucae,
condyloma acuminatunt, and focal epithelial hyperplasia). Oral Surg. 1972; 34: 60418.
5. WrightRA, JudsonFN. Relative and seasonal incidences
of the sexually transmitted diseases: A two-year statistical review. Br J VenerDis. 1978; 54: 43340.
6. Chief Medical Officer of the Department of Health and
Social Security. Sexually transmitted diseases: extract
from the annual report for the year 1978. Br J Vener Dis.
1980; 56: 17881.
7. ReisHLB, Rabelo PC, SantanaMRF, FerreiraDC, FilhoAC. Oral squamous papilloma and condyloma acuminatum as manifestations of buccal-genital infection
by human papillomavirus. Ind J Sex Trans Dis. 2009;
30(1): 402.
8. HooryT, MonieA, GravittP, WuTC. Molecular epidemiology of human papillomavirus. J Formos Med Assoc. 2008; 107(3): 198217.
9. Knapp MJ, Uohara GI. Oral condyloma acuminatum.
Oral Surg. Oral Med. Oral Pathol. 1967; 23: 53845.
10. GarlickJA, TaichmanLB. Human papillomavirus infection of the oral mucosa. Am J Dermatopathol. 1991; 13:
38695.
11. Borborema-SantosCM, CastroMM, Santos PJ, Talhari
S, Astolfi-Filho S. Oral focal epithelial hyperplasia: report of five cases. Braz Dent J. 2006; 17: 7982.
12. WeinstockH, BermanS, CatesWJr. Sexually transmitted diseases among American youth: incidence and
prevalence estimates, 2000. Perspect Sex Reprod Health.
2004; 36(1): 610.
46
ArnasRimkeviius, AlinaPrien, MindaugasGaigalas
13. WattsDH, KoutskyLA, HolmesKKetal. Low risk of
perinatal transmission of human papillomavirus: results
from a prospective cohort study. Am J Obstet Gynecol.
1998; 178(2): 36573.
14. WelanderCE, HomesleyHD, SmilesKA. Intralesional
interferon alfa-2b for the treatment of genital warts. Am
J Obstet Gynecol. 1990; 162(2): 34854.
15. FlaitzCM, HicksMJ. Molecular piracy: the viral link to
carcinogenesis. Oral Oncol. 1998; 34: 44853.
16. CheahPL, LooiLM. Biology and pathological associations of the human papillomaviruses: a review. Malays. J
Pathol. 1998; 20: 110.
17. HenleyDJ, SummerlinDJ, TomichCE. Condyloma acuminatum and condyloma-like lesions of the oral cavity:
a study of 11 cases with an intraductal component. Histopathology. 2004; 44(3): 21621.
18. ACOG Practice Bulletin. Clinical Management Guidelines for Obstetrician-Gynecologists. Human papillomavirus. Obstet Gynecol. 2005; 105(4): 90518.
19. BambaoC, Nofech-MozesS, ShierM. Giant condyloma
versus verrucous carcinoma: a case report. J Low Genit
Tract Dis. 2010; 14(3): 2303.
20. NucciV, TorchiaD, CappugiP. Condyloma acuminatum
of the tongue treated with photodynamic therapy. Clin
Infect Dis. 2009; 48(9): 13302.
21. dos Reis HLB, Rabelo PC, de Santana MRF, FerreiraDC,FilhoAC. Oral squamous papilloma and condyloma acuminatum as manifestations of buccal-genital
infection by human papillomavirus. IJSTD 2009; 30(1):
402.
22. FeriziM, GercariA, PajazitiL, BlytaY,KocinaA, ShkendijeD. Condyloma acuminata in child end laser therapy: a case report. Cases J. 2009; 2: 123.
23. Hicheri J. Giant condyloma (BuschkeLowenstein tumor). A case report. Acta Dermatovenerol Alp Panonica
Adriat. 2006; 15(4): 1813.
24. IshijiT. Condyloma acuminatum. Nippon Rinsho. 2007;
65(3): 38993.
25. NowickiMJ, BishopPR, SubramonyC. Diagnosis: Condyloma acuminatum. J Pediatr Gastroenterol Nutr. 2005;
40(3): 168.
26. Horewicz VV. Human papillomavirus-16 prevalence
in gingival tissue and its association with periodontal
destruction: a case-control study. J Periodontol. 2010; 4:
5628.
27. SyrjanenS. Human papillomavirus infections and oral
tumors. Med Microbiol Immunol. 2003; 3: 1238.
28. Ledesma-Montes C, Vega-Memije E, Garcs-Ortz M,
Cardiel-NievesM, Jurez-LunaC. Multifocal epithelial
hyperplasia. Report of nine cases. Med Oral Patol Oral
Cir Bucal. 2005; 10: 394401.
29. Segura-Saint-Gerons R, Toro-Rojas M, Ceballos-SalobreaA, Aparicio-SoriaJL, Fuentes-VaamondeH. Focal
30.
31.
32.
33.
epithelial hyperplasia. A rare disease in our area. Med
Oral Patol Oral Cir Bucal. 2005; 10: 12831.
Borborema-Santos CM, Castro MM, Santos PJ, TalhariS, Astolfi-FilhoS. Oral focal epithelial hyperplasia:
report of five cases. Braz Dent J. 2006; 17: 7982.
dosSantosPJ, BessaCF, deAguiarMC, doCarmoMA.
Cross-sectional study of oral mucosal conditions among
a central Amazonian Indian community, Brazil. J Oral
Pathol Med. 2004; 33(1): 712.
ClemonsRJ, Clemons-MillerA, JohnsonSM, WilliamsonSK, HornTD. Comparing therapy costs for physician treatment of warts. J Drugs Dermatol. 2003; 2(6):
64954.
JayasooriyaPR, AbeyratneS, RanasingheAW, Tilakaratne WM. Focal epithelial hyperplasia (Hecks disease):
report of two cases with PCR detection of human papillomavirus DNA. Oral Dis. 2004; 10(4): 2403.
ArnasRimkeviius, AlinaPrien, MindaugasGaigalas
SMAILIAGAL KONDILIOMA: ATVEJO
PRISTATYMAS
S antrauka
io straipsnio tikslas pateikti 42 met paciento klinikin atvej,
kai, ityrus burnos gleivins paeidimus klinikai ir histologikai,
buvo patvirtinta smailiagals kondiliomos diagnoz, taip pat apvelgti literatros duomenis smailiagals kondiliomos etiologijos,
patogenezs, diagnostikos ir gydymo klausimais.
Raktaodiai: smailiagal kondilioma, burnos gleivin, papilomos virusas, IV
You might also like
- LETAK HPV-Sanevax Hrvatska VerzijaDocument2 pagesLETAK HPV-Sanevax Hrvatska VerzijaNikola IvankovicNo ratings yet
- Papilloma Skuamosa: Laporan Kasus Dan Tinjauan PustakaDocument4 pagesPapilloma Skuamosa: Laporan Kasus Dan Tinjauan PustakarizkyayuarristaNo ratings yet
- Papi LomaDocument10 pagesPapi LomaIsai LVazquezNo ratings yet
- HPV InfectionDocument6 pagesHPV Infectionsrikantnairsemail8038No ratings yet
- Human Papilloma Virus Infections: David Tindle, BS, DDS, MS, FAGD, DABOM University of MichiganDocument20 pagesHuman Papilloma Virus Infections: David Tindle, BS, DDS, MS, FAGD, DABOM University of Michiganneustadt3noeNo ratings yet
- MainDocument4 pagesMainMardhiatiNo ratings yet
- Squamous Papilloma of The Tongue: A Case ReportDocument3 pagesSquamous Papilloma of The Tongue: A Case ReportAninda Wulan PradaniNo ratings yet
- Verruca Vulgaris in A Non-Immunocompromised Patient: Case ReportDocument4 pagesVerruca Vulgaris in A Non-Immunocompromised Patient: Case ReportBryan Eliezer SitumorangNo ratings yet
- Oral Squamous Papilloma in A Pediatric Patient A Case ReportDocument4 pagesOral Squamous Papilloma in A Pediatric Patient A Case Reportaulia lubisNo ratings yet
- Viruses and Oral Cancer. Is There A Link?: Lars Sand, Jamshid JalouliDocument8 pagesViruses and Oral Cancer. Is There A Link?: Lars Sand, Jamshid JalouliWJNo ratings yet
- Kondilomata AkuminataDocument6 pagesKondilomata AkuminataChristy BradyNo ratings yet
- Oral Warts.: DR Nwachukwu N. CDocument19 pagesOral Warts.: DR Nwachukwu N. Cenwachukwu_1No ratings yet
- Prevalence of HPV in Patients Affected by Oral Lichen Planus - A Prospective Study Using Two Different Chair-Side Sampling MethodsDocument7 pagesPrevalence of HPV in Patients Affected by Oral Lichen Planus - A Prospective Study Using Two Different Chair-Side Sampling MethodsKiarra Vashti NadiraNo ratings yet
- PemfigusDocument5 pagesPemfigusSherlyNo ratings yet
- Contact Dermatitis 2001Document6 pagesContact Dermatitis 2001GilankNo ratings yet
- Atypical TuberculosisDocument3 pagesAtypical TuberculosisWilda Khairani DalimuntheNo ratings yet
- NigerJClinPract21121674-5994143 163901Document4 pagesNigerJClinPract21121674-5994143 163901Adriana CardeñaNo ratings yet
- Oral Squamous Cell Carcinoma - Case ReportDocument4 pagesOral Squamous Cell Carcinoma - Case ReportIJAR JOURNALNo ratings yet
- Human Papillomavirus and Its Influence On Head and Neck Cancer PredispositionDocument7 pagesHuman Papillomavirus and Its Influence On Head and Neck Cancer PredispositionKathia Pinilla GuizadoNo ratings yet
- Journal Reading MataDocument15 pagesJournal Reading MataMichael Jayanto ParameanNo ratings yet
- Ch04oral MedicineDocument35 pagesCh04oral MedicineNaleena JosephNo ratings yet
- HPV FullpaperDocument11 pagesHPV Fullpapersamanta_argNo ratings yet
- Todentj 6 126Document5 pagesTodentj 6 126AngelicaNo ratings yet
- Current Aspects On Oral Squamous Cell Carcinoma: Anastasios K. MarkopoulosDocument5 pagesCurrent Aspects On Oral Squamous Cell Carcinoma: Anastasios K. MarkopoulosYeni PuspitasariNo ratings yet
- Articulo CientíficoDocument11 pagesArticulo CientíficoCarolina SalazarNo ratings yet
- Review ArticleDocument12 pagesReview ArticleThallita Rahma ZiharviardyNo ratings yet
- Background: Bowenoid Papulosis Seborrheic KeratosesDocument3 pagesBackground: Bowenoid Papulosis Seborrheic KeratosesdesyihalimNo ratings yet
- Jurnal OMDocument8 pagesJurnal OMSaraswita Gabriellah SaetikhoNo ratings yet
- Kaposi Sarcoma Virus (HHV8) InfectionsDocument13 pagesKaposi Sarcoma Virus (HHV8) InfectionsindahNo ratings yet
- Review - Update On Diagnosis and Management of Conjunctival PapillomaDocument17 pagesReview - Update On Diagnosis and Management of Conjunctival PapillomaGiovanna SoaresNo ratings yet
- Human Immunodeficiency Virus AND Acquired Immunodeficiency SyndromeDocument59 pagesHuman Immunodeficiency Virus AND Acquired Immunodeficiency SyndromeJose Joy IdicullaNo ratings yet
- Australian Dental Journal: Human Papillomavirus and Oral and Oropharyngeal Carcinoma: The EssentialsDocument8 pagesAustralian Dental Journal: Human Papillomavirus and Oral and Oropharyngeal Carcinoma: The EssentialsBagis Emre GulNo ratings yet
- Case Report Pemphigus Vulgaris As Oral Mucosal Ulcer Progressive To Skin LesionDocument5 pagesCase Report Pemphigus Vulgaris As Oral Mucosal Ulcer Progressive To Skin LesionAninda Wulan PradaniNo ratings yet
- Diţescu D Et Al 2021Document15 pagesDiţescu D Et Al 2021ayasofiavrNo ratings yet
- DX Dif Midline Destructive Disease 2014Document7 pagesDX Dif Midline Destructive Disease 2014MARIE SELENE RAMIREZ REVOLLARNo ratings yet
- Ncbi Sinonasal IPDocument5 pagesNcbi Sinonasal IPReza RahadianNo ratings yet
- Hand Foot and Mouth DiseaseDocument14 pagesHand Foot and Mouth DiseaseE=MC2No ratings yet
- Acute Herpetic Gingivostomatitis in Adults: A Review of 13 Cases, Including Diagnosis and ManagementDocument5 pagesAcute Herpetic Gingivostomatitis in Adults: A Review of 13 Cases, Including Diagnosis and ManagementAfaf MahmoudNo ratings yet
- Martha Gonzalez G 1819vxczlibnlborazpj Vphpia Etal 2019 Med OralDocument6 pagesMartha Gonzalez G 1819vxczlibnlborazpj Vphpia Etal 2019 Med OralGLORIA ISABEL VALDES CASTRONo ratings yet
- TB UlcerDocument4 pagesTB UlcerKelvin BulainNo ratings yet
- Medicina: Oral and Maxillo-Facial Manifestations of Systemic Diseases: An OverviewDocument22 pagesMedicina: Oral and Maxillo-Facial Manifestations of Systemic Diseases: An OverviewS FznsNo ratings yet
- At-A-Glance: Human Papillomavirus InfectionsDocument26 pagesAt-A-Glance: Human Papillomavirus Infectionsketty putriNo ratings yet
- Case Report 2 PDFDocument5 pagesCase Report 2 PDFSittiNurQomariahNo ratings yet
- 1.oral CavityDocument60 pages1.oral CavitySalma NajjarNo ratings yet
- Orofacial Viral Infections An UpdateDocument6 pagesOrofacial Viral Infections An UpdateAli RazaNo ratings yet
- 10.1515@sjdv 2016 0005Document6 pages10.1515@sjdv 2016 0005Gaby D'LuneNo ratings yet
- Oral and Maxillofacial Surgery/fifth Year: The Natural History of Oral SCCDocument25 pagesOral and Maxillofacial Surgery/fifth Year: The Natural History of Oral SCCAbdullah Muhammed khaleel HassanNo ratings yet
- Ilovepdf MergedDocument22 pagesIlovepdf MergedSRO oONo ratings yet
- OMIC 311 Lecture 17 Human Papilloma, Herpes, Hepatits VirusDocument51 pagesOMIC 311 Lecture 17 Human Papilloma, Herpes, Hepatits VirusMaryam XANo ratings yet
- VerukaDocument4 pagesVerukaMuhajir BusraNo ratings yet
- Viral Involvement in The Pathogenesis and Clinical Features of Opthalmic Pterygium"Document14 pagesViral Involvement in The Pathogenesis and Clinical Features of Opthalmic Pterygium"Zahara FonnaNo ratings yet
- Oral Leishmaniasis Report of Two Cases 2020Document5 pagesOral Leishmaniasis Report of Two Cases 2020MARIE SELENE RAMIREZ REVOLLARNo ratings yet
- Oral Viral Infections Diagnosis and ManagementDocument13 pagesOral Viral Infections Diagnosis and ManagementhunarsandhuNo ratings yet
- Otolaryngologic Manifestations of HIV Infection: ReviewsDocument6 pagesOtolaryngologic Manifestations of HIV Infection: ReviewsSo NicNo ratings yet
- Blistering Disorders: Diagnosis and Treatment: S. W. Y, B A, N S, & A. R ADocument10 pagesBlistering Disorders: Diagnosis and Treatment: S. W. Y, B A, N S, & A. R ARashmi KumariNo ratings yet
- Hand, Foot and Mouth Disease in Children: A Clinico Epidemiological StudyDocument6 pagesHand, Foot and Mouth Disease in Children: A Clinico Epidemiological Studysamy22722No ratings yet
- CRM 2015Document7 pagesCRM 2015Kiran KumarNo ratings yet
- Papiloma TerbalikDocument6 pagesPapiloma TerbalikLasman RadjaNo ratings yet
- ART Mod. Grey y MariDocument6 pagesART Mod. Grey y MarigreynerNo ratings yet
- Clinically Relevant Mycoses: A Practical ApproachFrom EverandClinically Relevant Mycoses: A Practical ApproachElisabeth PresterlNo ratings yet
- Human Papillomavirus VaccineDocument18 pagesHuman Papillomavirus VaccineJarvis Guthrey BaldopeñaNo ratings yet
- HPV PowerpointDocument11 pagesHPV PowerpointharyatikennitaNo ratings yet
- List of Cervical Cancer Screening Centres in GhanaDocument15 pagesList of Cervical Cancer Screening Centres in Ghanamyjoyonline.comNo ratings yet
- Human Papilloma Virus Vaccine For Cervical Cancer PreventionDocument9 pagesHuman Papilloma Virus Vaccine For Cervical Cancer Preventionsayeef khanNo ratings yet
- Knowledge, Attitude & Practice On Human Papillomavirus Vaccination: A Cross-Sectional Study Among Healthcare ProvidersDocument9 pagesKnowledge, Attitude & Practice On Human Papillomavirus Vaccination: A Cross-Sectional Study Among Healthcare ProvidersHari PrasathNo ratings yet
- HPVDocument7 pagesHPVWillbourNo ratings yet
- Health Belief Model On The Determinants of Human Papilloma Virus Vaccination in Women of Reproductive Age in Surakarta, Central JavaDocument11 pagesHealth Belief Model On The Determinants of Human Papilloma Virus Vaccination in Women of Reproductive Age in Surakarta, Central Javaadilla kusumaNo ratings yet
- Lesi Prakanker CervixDocument50 pagesLesi Prakanker CervixjeihanalkhairNo ratings yet
- Virus Hepatitis Dan HPV (Human Papilloma Virus)Document15 pagesVirus Hepatitis Dan HPV (Human Papilloma Virus)TresaNo ratings yet
- Its A Simple Test Cervical Cancer Screening UrduDocument1 pageIts A Simple Test Cervical Cancer Screening UrduIqbal BaryarNo ratings yet
- Ver E-Hpv-R1Document2 pagesVer E-Hpv-R1api-309082881No ratings yet
- Bethesda SystemDocument186 pagesBethesda SystemJoyce Pardo FernandezNo ratings yet
- Available Online Through: ISSN 2321 - 6328Document4 pagesAvailable Online Through: ISSN 2321 - 6328Himanshu ThukralNo ratings yet
- Distribuţia Genotipurilor Virusului Papiloma Uman La Paciente Din Zona MoldoveiDocument5 pagesDistribuţia Genotipurilor Virusului Papiloma Uman La Paciente Din Zona MoldoveiZama VitalieNo ratings yet
- Adenoviridae & Papovaviridae: R. Lia K. Iswara, DR, MS, SPMK Dept. Microbiology FK UsuDocument16 pagesAdenoviridae & Papovaviridae: R. Lia K. Iswara, DR, MS, SPMK Dept. Microbiology FK UsuMuhammad AslamNo ratings yet
- Centro Universitario Siglo Xxi: Genital Human Papillomavirus InfectionDocument11 pagesCentro Universitario Siglo Xxi: Genital Human Papillomavirus InfectionDafne Polet Monroy SampalloNo ratings yet
- HPV: Infection, Prevention and Vaccination in India: Ritesh KumarDocument6 pagesHPV: Infection, Prevention and Vaccination in India: Ritesh Kumarsandeep raiNo ratings yet
- Health Matters Understanding HPV VaccinesDocument4 pagesHealth Matters Understanding HPV VaccinesFrancisca Camila ApablazaNo ratings yet
- Hubungan Tingkat Pengetahuan Kanker Serviks Dengan Minat Untuk Vaksinasi HPV Pada Mahasiswi Fakultas Kedokteran Universitas HKBP Nommensen MedanDocument4 pagesHubungan Tingkat Pengetahuan Kanker Serviks Dengan Minat Untuk Vaksinasi HPV Pada Mahasiswi Fakultas Kedokteran Universitas HKBP Nommensen Medanintan fairuzNo ratings yet
- Deteksi Dini Kanker Serviks UteriDocument80 pagesDeteksi Dini Kanker Serviks UteriJULINNo ratings yet
- Nejmcp 2108502Document9 pagesNejmcp 2108502Manuel GilNo ratings yet
- Jurnal Vaksin HPVDocument9 pagesJurnal Vaksin HPVlitaayuningdyahNo ratings yet
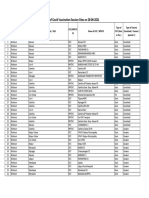
- List of Covid Vaccination Session Sites On 28-06-2021Document44 pagesList of Covid Vaccination Session Sites On 28-06-2021JitNo ratings yet
- Papovaviridae PowerpointDocument53 pagesPapovaviridae PowerpointMia Fernandez100% (3)
- Daftar Pustaka: Human Papillomavirus and HPV Vaccines: A ReviewDocument2 pagesDaftar Pustaka: Human Papillomavirus and HPV Vaccines: A Reviewdr.deyshieNo ratings yet
- Vaccination CentersDocument30 pagesVaccination CentersAnil Kumar NallaNo ratings yet
- All Vaccinees Are Requested To Bring Certificate of Dose-II From COWIN Portal Alongwith Registered Mobile Number Before Proceeding For VaccinationDocument7 pagesAll Vaccinees Are Requested To Bring Certificate of Dose-II From COWIN Portal Alongwith Registered Mobile Number Before Proceeding For VaccinationRakesh KumarNo ratings yet
- Id AssignmentDocument4 pagesId AssignmentAmutuhaire JudithNo ratings yet
- Vaccination Contre La Covid-19: Voici Le CalendrierDocument6 pagesVaccination Contre La Covid-19: Voici Le CalendrierDefimedia100% (1)