Professional Documents
Culture Documents
11 Epidemiologicalbbbbbb PDF
11 Epidemiologicalbbbbbb PDF
Uploaded by
Nur KholifahOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
11 Epidemiologicalbbbbbb PDF
11 Epidemiologicalbbbbbb PDF
Uploaded by
Nur KholifahCopyright:
Available Formats
Chang et al.
BMC Infectious Diseases 2011, 11:352
http://www.biomedcentral.com/1471-2334/11/352
RESEARCH ARTICLE
Open Access
Epidemiological characteristics of varicella from
2000 to 2008 and the impact of nationwide
immunization in Taiwan
Luan-Yin Chang1*, Li-Min Huang1, I-Shou Chang2 and Fang-Yu Tsai2
Abstract
Background: Varicella has an important impact on public health. Starting in 2004 in Taiwan, nationwide free
varicella vaccinations were given to 1-year-old children.
Methods: Our study investigated the epidemiological characteristics of varicella from 2000 to 2008, and assessed
the change of varicella epidemiology after the mass varicella immunization. ICD-9-CM codes related to varicella or
chickenpox (052, 052.1, 052.2, 052.7, 052.8, 052.9) were analyzed for all young people under 20 years of age
through the National Health Insurance database of Taiwan from 2000 to 2008.
Results: Case numbers of varicella or chickenpox significantly declined after the nationwide immunization in 2004.
Winter, particularly January, was the epidemic season of varicella. We found a significant post-vaccination decrease
in incidence among preschool children, especially 3 to 6 year-old children the peak incidence was 66 per
thousand for 4 and 5 year-old children before the nationwide immunization (2000 to 2003), and the peak
incidence was 23 per thousand for 6 year-old children in 2008 (p < 0.001). Varicella-related hospitalization also
significantly decreased in children younger than 6 years after the nationwide immunization.
Conclusion: The varicella annual incidence and varicella-related hospitalization markedly declined in preschool
children after nationwide varicella immunization in 2004.
Keywords: varicella, chickenpox, epidemiology, incidence, vaccine, prevention
Background
Varicella is the primary disease caused by the varicellazoster virus. It is a common and highly contagious disease and has a significant health impact on children.
Although the clinical course of varicella is usually mild
and self-limiting, varicella does cause complications and
mortality resulting in financial expense [1-3]. Chickenpox
or varicella now has been considered one of the most
common vaccine-preventable diseases in many countries
[4-7].
In Taiwan, some areas including Taipei City, Taichung
City and Taichung County gave the public free varicella
vaccinations for 1-2 year-old children before 2004. Taipei
City started the free varicella vaccination from 1998 and
* Correspondence: lychang@ntu.edu.tw
1
Department of Pediatrics, National Taiwan University Hospital, College of
Medicine, National Taiwan University, Taipei, Taiwan
Full list of author information is available at the end of the article
Taichung City and Taichung County from 1999. Other
areas did not provide free varicella vaccination, but people could receive varicella vaccination at their own
expense before 2004. Since 2004, free mass varicella
immunization has been given to all one year-old children
throughout Taiwan.
Since the implementation of National Health Insurance
(NHI) in 1995, there has been a healthcare database in
Taiwan. Taiwan has a population of 22.9 million people
and the land area of 36188 Km2. Its population density is
633/Km2. Taiwans NHI covered most of the health care
costs for 98% of its population in 2006 [8]; the remaining
2% of it population are living in the foreign countries or in
families with monthly household incomes less than 1000
US dollars. Taiwans NHI database includes health care
data collected from over 95% of the hospitals in Taiwan
for more than 96% of the population receiving health care.
We evaluated the disease burden and epidemiological
2011 Chang et al; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons
Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in
any medium, provided the original work is properly cited.
Chang et al. BMC Infectious Diseases 2011, 11:352
http://www.biomedcentral.com/1471-2334/11/352
characteristics of varicella by using the NHI database to
find out the age-specific incidences, seasonal distribution
and varicella-related hospitalization from 2000 to 2008
the period covering pre- and post-public free vaccination
so we could compare the epidemiological characteristics
of varicella before and after the mass immunization.
Methods
Vaccination
The administration of a live attenuated varicella vaccine
was licensed in Taiwan in 1997. Both Merck and GlaxoSmithKline, pharmaceutical companies, provided the varicella vaccines in Taiwan. In 2004 the varicella vaccine
was incorporated into Taiwans national immunization
program, and all 1-year-old children could receive the
varicella vaccine for free. The varicella coverage rate for
1-year-old children was 94% for the 2003 birth cohort,
95% for the 2004 cohort, and 97% for the 2005, 2006, and
2007 birth cohorts according to Taiwans National
Immunization Information System which was developed
in the early 1990s [9]. When a child received a vaccine,
his or her vaccination would not only be recorded in a
childs vaccination handbook but would also be reported
to the National Immunization Information System.
Data collection
Taiwans National Health Insurance (NHI) covered most
of the health care costs for 98% of its population. Taiwans NHI database includes health care data collected
from over 95% of the hospitals in Taiwan for more than
98% of the population receiving health care. From this
database, hospitalization and outpatient healthcare
records were collected from 2000 to 2008, and International Classifications of Diseases, Ninth Revision, Clinical
Modification (ICD-9-CM) codes related to varicella or
chickenpox were analyzed for all the population. The
age-specific annual incidence and hospitalization rate
were calculated. For calculating the annual populationbased incidence, the annual incidence was calculated by
dividing the number of varicella-related diseases by the
population, which was obtained from Department of Statistics, Ministry of the Interior, Taiwan from 2000 to
2008 [10].
Definitions
ICD-9-CM codes for chickenpox or varicella include the
following: 052 chickenpox; 052.0 post-varicella encephalitis,
post-chickenpox encephalitis; 052.1 varicella (hemorrhagic)
pneumonitis; 052.7 with other specified complications;
052.8 with unspecified complication; 052.9 varicella without mention of complication.
For complications, we define varicella or chickenpox
patients to have complications in cases where the
patients had both ICD-9-CM codes for varicella or
Page 2 of 7
chickenpox (052 and the other related codes) and also
ICD-9-CM codes for varicella-related complications
which include the following: central nervous system
including 320 meningitis, 322 cerebellitis, 323 encephalitis, 348 encephalopathy, 351 facial palsy, 331.81 Reyes
syndrome, 780.3 febrile convulsion/seizure; skin and soft
tissue including 680-686 cellulites and abscess, 035 erysipela, 728 pyomyositis and necrotizing fasciitis, 373 &
376.01 blepharitis, 034 & 041 scarlet fever and streptococcal or staphylococcal infection; skeletal system including 711 arthritis, 730-733 osteomyelitis; lower respiratory
tract infection including 480-487 pneumonia, 510-519
pneumonitis, 466 & 490 bronchitis; hematological system- 287 thrombocytopenia, 283 & 285 anemia, 288 neutropenia; 038 & 790 & 995.91-995.92 for sepsis and
bacteremia; 040-041 for other bacterial infection; 422
cardiomyopathy, 425 myocarditis; 070.5 & 070.9 & 573
for hepatitis.
Statistics
In univariate analysis, categorical variables were compared with chi-square or Fishers exact test; continuous
variables were analyzed with Students t test. The difference of annual incidence among various age groups, the
difference of annual incidences in different years, and
the difference in seasonal distribution were measured
with appropriate c2 test. A p value of < 0.05 was considered to be statistically significant. All statistical analyses
were performed with SAS software, version 9.0.
Results
Number of cases before and after the mass immunization
The monthly distribution of case numbers from 2000 to
2008 is demonstrated in Figure 1. Case numbers markedly declined after the mass immunization in 2004, the
highest monthly number was 23460 in January 2000,
and the lowest was 2016 in September 2008. The peak
of varicella usually occurred during winter, especially in
January.
Age distribution
Overall age-specific case numbers and the cumulative
percentage of varicella in children from 2000 to 2008 are
shown in Figure 2, those of 2000 in Figure 3, and those
of 2008 in Figure 4. Children younger than 10 years old
represented 89% of all the cases and the peak age was 3
to 6 years from 2000 to 2008 (Figure 2). However, the
age distribution changed significantly after the mass
immunization (p < 0.001): 73% of varicella cases were
children less than 6 years of age in 2000 (before the mass
immunization, Figure 3) but only 24% of the cases were
children younger than 6 years of age in 2008 (4 years
after the mass immunization, Figure 4). In comparison
with age-specific case numbers of 2000 (Figure 3), those
Chang et al. BMC Infectious Diseases 2011, 11:352
http://www.biomedcentral.com/1471-2334/11/352
Page 3 of 7
Case Number
Mass immunization
2000
2001
2002
2003
2004
2005
2006
2007
7
10
7
10
10
7
10
7
10
10
7
10
7
10
10
2008
Figure 1 Monthly distribution of varicella case number from 2000 to 2008.
Age-specific annual incidence
Figure 5 demonstrates the age-specific annual incidence of
varicella before and after the nationwide immunization. In
160000
100%
140000
90%
80%
Case number
120000
70%
100000
Case number
80000
Cumulative percentage
60000
60%
50%
40%
30%
40000
20%
20000
10%
0%
0
10 11 12 13 14 15 16 17 18 19
Age
Figure 2 Age-specific case number and cumulative percentage of varicella in children from 2000 to 2008.
Cumulative percentage
2000 to 2003 (before the nationwide immunization), the
peak incidence was in 4 and 5-year-old children with
annual incidence of 66 per thousand while in 2008, the
peak incidence occurred in 6-year-old children with
annual incidence of 23 per thousand (p < 0.01). After the
nationwide immunization in 2004, the annual incidence
significantly decreased among children younger than 7
of 2008 were significantly lower (Figure 4) (p < 0.01). In
2008, school children had more varicella cases than the
kindergarteners.
Chang et al. BMC Infectious Diseases 2011, 11:352
http://www.biomedcentral.com/1471-2334/11/352
Page 4 of 7
100%
30000
90%
20000
15000
80%
Cumulative percenatge
Case number
25000
70%
Case number
60%
Cumulative percentage
50%
40%
10000
30%
20%
5000
10%
0
0%
0 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19
Age
Figure 3 Age-specific case number and cumulative percentage of varicella in children in 2000, before the nationwide immunization.
30000
100%
Case number
80%
70%
20000
60%
15000
Case Number
50%
Cumulative Percentage
40%
10000
30%
20%
5000
Cumulative percentage
90%
25000
10%
0%
0 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19
Figure 4 Age-specific case number and cumulative percentage of varicella in children in 2008, 4 years after the nationwide
immunization.
Annual incidence per thousand
Chang et al. BMC Infectious Diseases 2011, 11:352
http://www.biomedcentral.com/1471-2334/11/352
Page 5 of 7
70
60
50
40
30
20
10
0
0
10 11 12 13 14 15 16 17 18 19
Age
Figure 5 Age-specific annual incidence of varicella before (2000-2003) and after the nationwide immunization (2004, 2005, 2006, 2007
and 2008).
years of age. In 2008, the annual incidence (6.8 per thousand) of infants who could not receive the varicella vaccine
was even higher than that (3.2 to 5.9 per thousand) of 1 to
4-year-old children. Children beyond 7 years had similar
annual incidence before and after the mass immunization.
Age-specific varicella-related hospitalization incidence
The proportion of the number of varicella-related hospitalization to the number of overall varicella cases was
the highest in infants and declined with age in children.
Figure 6 shows that the annual incidence of varicellarelated hospitalization was the highest in infants. In
comparison with the annual incidence of 2000 to 2003
(before the nationwide immunization), the annual incidence of hospitalization significantly declined in children
younger than 6 years of age from 2004 to 2008 (p <
0.01). From 2000 to 2008, the annual incidence of preschool children decreased obviously with the year.
Complications
Among the 21829 hospitalized cases, 561 (2.57%) had
central nervous system complications, 2721 (12.47%)
had skin or soft tissue infections, 4740 (21.71%) had
lower respiratory tract infections, 493 (2.26%) had hematological complications, 281 (1.29%) had septicemia or
bacteremia, and 721 (3.30%) had hepatitis.
Twelve children died and Table 1 lists the demography and complications of the 12 fatal varicella cases.
Five of them had underlying diseases including 2 with
acute lymphoblastic leukemia, 1 with severe combined
immunodeficiency, 1 with enzymopathy, and 1 with pulmonary vascular anomaly. Most of them had complications of septicemia, skin or soft tissue infections, or
encephalitis, and 1 had Reye syndrome.
Discussion
Nationwide varicella immunization has resulted in a
marked reduction of varicella incidence and varicellarelated hospitalization in children younger than 6 years
of age in Taiwan. The impact of mass varicella immunization has so far made it possible for most preschool children to be free of varicella and varicella-related
hospitalization in Taiwan. However, children beyond 7
years of age had similar annual incidence before and after
the mass immunization.
As Figure 3 shows the age distribution before the mass
immunization in 2000, the peak age of varicella was 3 to 6
years, which was also the age group of kindergarteners.
Kindergarteners might have more exposure to varicella
and also their hand hygiene and sanitation levels are generally not as high as adults or older school childrens, who
may in turn lead to more varicella cases in kindergarteners
without mass immunization (Figure 3). However, after the
mass immunization, we observed more varicella cases in
the school children than those in 3 to 4-year-old kindergarteners (Figure 4), who were supposed to have received
the free varicella vaccine at 1 year of age. Therefore, mass
immunization has changed the age distribution of varicella
cases significantly and the peak age has subsequently
moved to older children without previous immunization.
Chang et al. BMC Infectious Diseases 2011, 11:352
http://www.biomedcentral.com/1471-2334/11/352
Page 6 of 7
Annual incidence per thousand
0.9
0.8
0.7
0.6
0.5
0.4
0.3
0.2
0.1
0
0
9 10 11 12 13 14 15 16 17 18 19
Age
Figure 6 Age-specific annual incidence of varicella-related hospitalization before (2000-2003) and after the nationwide immunization
(2004, 2005, 2006, 2007 and 2008).
Similar results were also reported by Lian et al who found
that the greatest decrease in varicella incidence occurred
in children aged below 6 and the incidence of varicella
shifted to older age groups after implementation of the
one-dose varicella vaccination policy [11]. Lian et al also
found that the incidence in early launch areas was significantly lower than that in the other areas in Taiwan [11].
Our study additionally reported the seasonality, varicellarelated hospitalization and complications from 2000 to
2008 in Taiwan. Moreover, our data in this study is
nationwide rather than the selected sample size like that of
Lian et als study.
We found that the annual incidence of children beyond
7 years of age was similar before and after mass immunization. Its because most of the school children were not
allowed to receive the free varicella vaccine. Thus, the
varicella incidence of the school children did not change
significantly after the mass immunization in this study.
We suppose that the annual incidence of school children
may decrease several years later if the immunized children grow up to be 6 to 12 years old. However, we have
to follow up on the impact of mass immunization on
school children to prove the above assumption several
years later.
Table 1 Demography and complications of 12 fatal varicella cases
Year
Age
Sex
Underlying disease
Complications
2000
Nil
Encephalitis, septic shock
2000
Unspecified Enzymopathy
Pseudomonas septicemia
2000
Acute lymphoblastic leukemia
Septicemia
2001
Nil
Encephalitis, septicemia
2001
2002
6
3
F
F
Nil
Nil
Sudden death
Respiratory failure
2002
Acute lymphoblastic leukemia
Not mentioned
2003
Nil
Skin/soft tissue infections, streptococcal septicemia
2004
16
Nil
Skin/soft tissue infections, pneumonia, septicemia
2005
Nil
Reyes syndrome
2006
Severe combined immunodeficiency
Acute and subacute hepatic necrosis, gastrointestinal hemorrhage
2007
Pulmonary vascular anomaly
Hemoptysis, acute respiratory failure
Chang et al. BMC Infectious Diseases 2011, 11:352
http://www.biomedcentral.com/1471-2334/11/352
The infants had the highest annual incidence of varicella-related hospitalization both before and after the
mass immunization (Figure 6). Infants cannot receive
the varicella vaccine and they have a higher chance of
severe varicella and more complications [12], so their
varicella-related hospitalization was significantly higher
than the other children.
There were 12 cases of fatality, of which 5 of them
had underlying diseases. Children with underlying diseases such as acute leukemia are more susceptible to
getting severe varicella with complications and have a
significantly higher mortality rate [12]. Therefore, the
varicella vaccine may be administered to children with
acute lymphoblastic leukemia who are in remission, or,
high-titer anti-varicella-zoster virus immune globulin as
post-exposure prophylaxis is recommended for immunocompromised children and newborns that are
exposed maternally to varicella [12].
Currently, the varicella vaccine program consists of a
single-dose vaccination in Taiwan, as it is in Canada,
Korea and Australia [13]. However, both varicella outbreaks and breakthrough infections have occurred after
the single-dose varicella vaccine program was initiated
[14]. These might be related to a loss of immunity or to
primary vaccine failure. Although the reports are limited,
varicella vaccine effectiveness may be higher when two
doses are administered than when a single-dose is administered. In 2006, the United States changed its immunization policy by stipulating that 2 doses be administered,
once at 1 year of age and another administered between
the ages of 3 and 4 years old [15]. In Taiwan, boosters in
4-6 year-old children to reduce the breakthrough infection
or amend the primary vaccine failure may be considered if
further epidemiology reveals frequent outbreaks or breakthrough infections in kindergarteners.
The major limitation of this study is that we could not
verify the diagnoses because we could just analyze the
NHI database rather than detailed medical charts. However, at the very least the nationwide database can let us
outline the comprehensive picture of varicella epidemiology in Taiwan and sketch the impact of nationwide
immunization.
Conclusions
In conclusion, nationwide varicella immunization significantly decreased the varicella annual incidence and varicella-related hospitalization in preschool children in
Taiwan. The impact of the varicella vaccine on schoolchildren may be followed up on several years later.
Acknowledgements and Funding
This study is based in part on data from the National Health Insurance
Research Database provided by the Bureau of National Health Insurance,
Department of Health and managed by National Health Research Institutes.
Page 7 of 7
The interpretation and conclusions contained herein do not represent those
of the Bureau of National Health Insurance, Department of Health or
National Health Research Institutes. This research was supported by the
grants, NSC 100-2321-B-002 -012 from National Science Council and DOH
98-CD-1010 from Centers for Disease Control, Taiwan. The funding institutes
did not have any role in study design, data collection/analysis, the writing of
the manuscript and the decision to submit the manuscript for publication.
Author details
Department of Pediatrics, National Taiwan University Hospital, College of
Medicine, National Taiwan University, Taipei, Taiwan. 2National Institute of
Cancer Research and Division of Biostatistics and Bioinformatics, National
Health Research Institute, Miaoli, Taiwan.
1
Authors contributions
LYC, LMH and ISC designed the study. LYC and FYT analyzed the data. LYC
wrote the paper. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Received: 9 June 2011 Accepted: 16 December 2011
Published: 16 December 2011
References
1. Carapetis JR, Russell DM, Curtis N: The burden and cost of hospitalised
varicella and zoster in Australian children. Vaccine 2004, 23:755-61.
2. Poulsen A, Cabral F, Nielsen J, Roth A, Lisse I, Aaby P: Growth, morbidity
and mortality after chickenpox infection in young children in GuineaBissau. J Infect 2005, 51:307-13.
3. Rivest P, Bedard L, Valiquette L, Mills E, Lebel MH, Lavoie G, et al: Severe
complications associated with varicella: Province of Quebec, April 1994
to March 1996. Can J Infect Dis 2001, 12:21-6.
4. Patrick D: Prevention strategies: experience of varicella vaccination
programmes. Herpes 2007, 14(Suppl 2):48-51.
5. Asano Y: Varicella vaccine: the Japanese experience. J Infect Dis 1996,
174(Suppl 3):S310-3.
6. Macartney KK, Beutels P, McIntyre P, Burgess MA: Varicella vaccination in
Australia. J Paediatr Child Health 2005, 41:544-52.
7. Getsios D, Caro JJ, Caro G, De Wals P, Law BJ, Robert Y, et al: Instituting a
routine varicella vaccination program in Canada: an economic
evaluation. Pediatr Infect Dis J 2002, 21:542-7.
8. Burea of National Health Insurance, Department of Health, Executive Yuan,
Taiwan ROC: Statistical annual reports., (Accessed at http://www.doh.gov.
tw/statistic/%A5%FE%A5%C1%B0%B7%ABO/95.htm).
9. Taiwan Center for Disease Control, Department of Health, Executive Yuan,
Taiwan: National Immunization Information System (NIIS).[http://www.cdc.
gov.tw/public/Data/7121816155271.doc].
10. Department of Statistics MotI, Taiwan: Population by Single Year of Age.
Department of Statistics, Taiwan;[http://www.moi.gov.tw/stat/index.asp].
11. Lian IB, Chien YZ, Hsu PS, Chao DY: The changing epidemiology of
varicella incidence after implementation of the one-dose varicella
vaccination policy. Vaccine 2011, 29(7):1448-54.
12. Myers MG, Seward JF, LaRussa FS: Varicella-zoster virus. Nelson Textbook of
Pediatrics , 18 2007.
13. Heininger U, Seward JF: Varicella. Lancet 2006, 368:1365-76.
14. Galil K, Lee B, Strine T, et al: Outbreak of varicella at a day-care center
despite vaccination. N Engl J Med 2002, 347(24):1909-15.
15. Marin M, Meissner HC, Seward JF: Varicella prevention in the United
States: a review of successes and challenges. Pediatrics 2008, 122:e744-51.
Pre-publication history
The pre-publication history for this paper can be accessed here:
http://www.biomedcentral.com/1471-2334/11/352/prepub
doi:10.1186/1471-2334-11-352
Cite this article as: Chang et al.: Epidemiological characteristics of
varicella from 2000 to 2008 and the impact of nationwide
immunization in Taiwan. BMC Infectious Diseases 2011 11:352.
You might also like
- 10 DOH ProgramsDocument28 pages10 DOH ProgramsDhonnalyn Amene Caballero100% (6)
- Analysis of The Rate of Infant Mortality From I Month To I YearDocument62 pagesAnalysis of The Rate of Infant Mortality From I Month To I YearChukwuma NdubuisiNo ratings yet
- Research Proposal On Prevalence of PneumoniaDocument26 pagesResearch Proposal On Prevalence of Pneumoniasolomon demissew62% (13)
- Critique PaperDocument2 pagesCritique PaperJeanne Kamille Evangelista Pinili100% (4)
- The Strategy Behind Taiwan's COVID-19 Immunization Program National Security and Global SolidarityDocument18 pagesThe Strategy Behind Taiwan's COVID-19 Immunization Program National Security and Global Solidarity林冠年No ratings yet
- Samuel CHAPTER 1 CorrectionDocument10 pagesSamuel CHAPTER 1 CorrectionNaomi AkinwumiNo ratings yet
- Civ 028Document9 pagesCiv 028Deah RisbaNo ratings yet
- The Effect of The COVID-19 Vaccine On Daily Cases and Deaths Based On Global Vaccine DataDocument12 pagesThe Effect of The COVID-19 Vaccine On Daily Cases and Deaths Based On Global Vaccine DataCorneliu PaschanuNo ratings yet
- Surveillance of Healthcare-Associated Infections in A Neonatal Intensive Care Unit in Italy During 2006 - 2010Document8 pagesSurveillance of Healthcare-Associated Infections in A Neonatal Intensive Care Unit in Italy During 2006 - 2010Refy Dwi Maltha PratiwiNo ratings yet
- Expanded Program On Immunization: Source: Weekly Epidemiological Record, WHO: No.46,2011,86.509-520)Document6 pagesExpanded Program On Immunization: Source: Weekly Epidemiological Record, WHO: No.46,2011,86.509-520)Abeer AguamNo ratings yet
- Expanded Program On Immunization: Source: Weekly Epidemiological Record, WHO: No.46,2011,86.509-520)Document6 pagesExpanded Program On Immunization: Source: Weekly Epidemiological Record, WHO: No.46,2011,86.509-520)Abeer AguamNo ratings yet
- 933-Article Text-3081-1-10-20221107Document5 pages933-Article Text-3081-1-10-20221107Andri Tri KuncoroNo ratings yet
- Guidelines For The Management of Suspected and Confirmed Bacterial Meningitis inDocument18 pagesGuidelines For The Management of Suspected and Confirmed Bacterial Meningitis inswr88kv5p2No ratings yet
- An Analysis of Taiwan's Vaccination Services and Applications For Vaccine Injury CompensationsDocument15 pagesAn Analysis of Taiwan's Vaccination Services and Applications For Vaccine Injury CompensationsAnonymous FNZ3uR2AHsNo ratings yet
- Persevere in The Dynamic COVID-Zero Strategy in China To Gain A Precious Time Window For The FutureDocument2 pagesPersevere in The Dynamic COVID-Zero Strategy in China To Gain A Precious Time Window For The FutureBillNo ratings yet
- Expanded Program On ImmunizationDocument6 pagesExpanded Program On ImmunizationAiza Oronce100% (1)
- Journal Article PDFDocument10 pagesJournal Article PDFAlyssa marieNo ratings yet
- Surveillance and Outbreak Investigation StudentDocument11 pagesSurveillance and Outbreak Investigation Studentnura meccaNo ratings yet
- Influenza Vaccination Among Infection Control Teams A EUCIC Surve - 2020 - VaccDocument5 pagesInfluenza Vaccination Among Infection Control Teams A EUCIC Surve - 2020 - VaccSavaNo ratings yet
- Department of Health - Expanded Program On Immunization - 2012-05-16Document7 pagesDepartment of Health - Expanded Program On Immunization - 2012-05-16MasterclassNo ratings yet
- The Rise of Imported Dengue Infections in Victoria, Australia, 2010-2016Document11 pagesThe Rise of Imported Dengue Infections in Victoria, Australia, 2010-2016Satriya WibawaNo ratings yet
- OpenSAFELY. Effectiveness of COVID-19 vaccination in children and adolescentsDocument29 pagesOpenSAFELY. Effectiveness of COVID-19 vaccination in children and adolescentsPABLO HONDUVILLANo ratings yet
- The Impact of Rotavirus Mass Vaccination On Hospitalization Rates, Nosocomial Rotavirus Gastroenteritis and Secondary Blood Stream InfectionsDocument10 pagesThe Impact of Rotavirus Mass Vaccination On Hospitalization Rates, Nosocomial Rotavirus Gastroenteritis and Secondary Blood Stream InfectionsKollar RolandNo ratings yet
- HHS Public Access: A Comparison of Post-Elimination Measles Epidemiology in The United States, 2009 2014 Versus 2001 2008Document20 pagesHHS Public Access: A Comparison of Post-Elimination Measles Epidemiology in The United States, 2009 2014 Versus 2001 2008Titania YuliskaNo ratings yet
- Meningitis in Children Under Five Year of Age.: DR Farrukh Iqbal Roll Number 06Document23 pagesMeningitis in Children Under Five Year of Age.: DR Farrukh Iqbal Roll Number 06dr_hammadNo ratings yet
- Vaccines 11 00306Document10 pagesVaccines 11 00306Mr SoehartoNo ratings yet
- SceirdDocument9 pagesSceirdGiaWay HsuNo ratings yet
- Zamora-Ledezma Et Al. - 2020 - Biomedical Science To Tackle The COVID-19 PandemicDocument48 pagesZamora-Ledezma Et Al. - 2020 - Biomedical Science To Tackle The COVID-19 PandemicEli Díaz de ZamoraNo ratings yet
- M1.U2 Measuring and Comparing Disease Frequency - StudentDocument6 pagesM1.U2 Measuring and Comparing Disease Frequency - StudentHusni MubarakNo ratings yet
- National HIV Action Plan 2017-2025: Tallinn 2017Document31 pagesNational HIV Action Plan 2017-2025: Tallinn 2017MeriAndaniSiahaanNo ratings yet
- Changes in Childhood Vaccination During The Coronavirus Disease 2 - 2021 - VacciDocument7 pagesChanges in Childhood Vaccination During The Coronavirus Disease 2 - 2021 - VacciProfessor BiologiaNo ratings yet
- Ca Covid 19 Delta VariantDocument42 pagesCa Covid 19 Delta VariantKristine Joy Vivero BillonesNo ratings yet
- 32Document10 pages32María Jesús Maass OleaNo ratings yet
- Impact of COVID19 On Routine Immunization: A Cross-Sectional Study in SenegalDocument6 pagesImpact of COVID19 On Routine Immunization: A Cross-Sectional Study in SenegalAjeng SuparwiNo ratings yet
- Article Covid-19 Children ReviewDocument12 pagesArticle Covid-19 Children ReviewAlexRázuri100% (1)
- Measles Study PDFDocument8 pagesMeasles Study PDFWebster The-TechGuy LunguNo ratings yet
- Effectiveness of Vaccination Against Varicella in Children Under 5 Years in Puglia Italy 2006 2012Document7 pagesEffectiveness of Vaccination Against Varicella in Children Under 5 Years in Puglia Italy 2006 2012NurulAlviFauzianaNo ratings yet
- Varicella in Pediatric Oncology Patients in The Post-Vaccine Era-Analysis of Routine Hospital Data From Bavaria (Germany), 2005-2011Document13 pagesVaricella in Pediatric Oncology Patients in The Post-Vaccine Era-Analysis of Routine Hospital Data From Bavaria (Germany), 2005-2011Hizam ZulfhiNo ratings yet
- Acute Flaccid Paralysis Field Manual: For Communicable Diseases Surveillance StaffDocument29 pagesAcute Flaccid Paralysis Field Manual: For Communicable Diseases Surveillance StaffAuliyaa RahmahNo ratings yet
- Dengue Net Flyer 2006Document1 pageDengue Net Flyer 2006Neha SameerNo ratings yet
- Telehealth For Global Emergencies: Implications For Coronavirus Disease 2019 (COVID-19)Document6 pagesTelehealth For Global Emergencies: Implications For Coronavirus Disease 2019 (COVID-19)Niki Pratiwi WijayaNo ratings yet
- Directly Observed Treatment Short-Course (DOTS) For Tuberculosis Control Program in Gambella Regional State, Ethiopia: Ten Years ExperienceDocument8 pagesDirectly Observed Treatment Short-Course (DOTS) For Tuberculosis Control Program in Gambella Regional State, Ethiopia: Ten Years ExperienceTammy Utami DewiNo ratings yet
- Out 123Document8 pagesOut 123Ilvita MayasariNo ratings yet
- Acceptance of A COVID-19 VacciDocument12 pagesAcceptance of A COVID-19 VacciahmadNo ratings yet
- MeningitisDocument62 pagesMeningitisDaniela Ramírez DavilaNo ratings yet
- The First Ever Confirmed Case of COVID-19 in Australia Was On January 25, 2020. The Patient Came From Wuhan and Flew To Melbourne On January 19Document6 pagesThe First Ever Confirmed Case of COVID-19 in Australia Was On January 25, 2020. The Patient Came From Wuhan and Flew To Melbourne On January 19Rastie CruzNo ratings yet
- Invasive Pneumococcal Disease - Canada - Ca 2000-2011Document12 pagesInvasive Pneumococcal Disease - Canada - Ca 2000-2011Regina EnggelineNo ratings yet
- Dept. Expanded Program On ImmunizationDocument6 pagesDept. Expanded Program On ImmunizationknotstmNo ratings yet
- 10 1016@j Jiac 2017 02 014Document12 pages10 1016@j Jiac 2017 02 014Achmad YunusNo ratings yet
- Asia Covid EstrategiasDocument10 pagesAsia Covid EstrategiasJonell SanchezNo ratings yet
- Safety Monitoring of COVID-19 Vaccines in Hong KongDocument19 pagesSafety Monitoring of COVID-19 Vaccines in Hong KongCarrie ChanNo ratings yet
- Covid 19Document16 pagesCovid 19Mazia MansoorNo ratings yet
- Outside The Window by David Naga (Essay)Document5 pagesOutside The Window by David Naga (Essay)David NagaNo ratings yet
- Cost-Effectiveness Evidence - A Case Study: How To Use This DocumentDocument3 pagesCost-Effectiveness Evidence - A Case Study: How To Use This DocumentPragnesh ChauhanNo ratings yet
- 1331907497-Montasseretal 2011BJMMR1038Document12 pages1331907497-Montasseretal 2011BJMMR1038puppyhandaNo ratings yet
- Expanded Program On ImmunizationDocument4 pagesExpanded Program On ImmunizationKrizle AdazaNo ratings yet
- Chapter OneDocument8 pagesChapter OneHOPENo ratings yet
- Prognostic Factors and OutcomesDocument7 pagesPrognostic Factors and Outcomesyikeberabebaw123No ratings yet
- Long Covid RevDocument9 pagesLong Covid RevJorge Dávila GonzálezNo ratings yet
- Vaccine: SciencedirectDocument10 pagesVaccine: SciencedirectNenqx Inthandt C'bunqxzu TheaNo ratings yet
- Dr. Eaton DeclarationDocument47 pagesDr. Eaton DeclarationJonece DuniganNo ratings yet
- FundingModel TBAndHIVConceptNote Final Ethiopia Oct15 2014Document94 pagesFundingModel TBAndHIVConceptNote Final Ethiopia Oct15 2014tokumaNo ratings yet
- Beyond One Health: From Recognition to ResultsFrom EverandBeyond One Health: From Recognition to ResultsJohn A. HerrmannNo ratings yet
- Dog BiteDocument24 pagesDog BitekranthichokkakulaNo ratings yet
- Health Check Consent FormDocument4 pagesHealth Check Consent Formaxenic04No ratings yet
- Polio Eradication: Pulse Polio Programme: A.Prabhakaran M.SC (N), Tutor, VMACON, SalemDocument13 pagesPolio Eradication: Pulse Polio Programme: A.Prabhakaran M.SC (N), Tutor, VMACON, SalemPrabhakaran Aranganathan100% (3)
- Cough and Colds, Fever, Asthma Topical: Headache, Skin Diseases Diuretics Anti - FungalDocument7 pagesCough and Colds, Fever, Asthma Topical: Headache, Skin Diseases Diuretics Anti - FungalElpijong Mijares JugalbotNo ratings yet
- Standardized Health Messages Book (With Bookmarked Headings) PDFDocument350 pagesStandardized Health Messages Book (With Bookmarked Headings) PDFKyaw Zaw HeinNo ratings yet
- Tetanus 2014Document32 pagesTetanus 2014Vanya Tri WindisariNo ratings yet
- Splenectomy: DisclaimerDocument5 pagesSplenectomy: DisclaimerMimi FatinNo ratings yet
- Framework of National Cancer Control Program in IndonesiaDocument20 pagesFramework of National Cancer Control Program in IndonesiaIndonesian Journal of Cancer100% (3)
- Final Pmmvy (Faq) Bookelt PDFDocument18 pagesFinal Pmmvy (Faq) Bookelt PDFrajat jainNo ratings yet
- What Is Polio?: SymptomsDocument2 pagesWhat Is Polio?: SymptomsJP LandagoraNo ratings yet
- Bill Gates Bio & History: Who Is Bill Gates?Document12 pagesBill Gates Bio & History: Who Is Bill Gates?ChristCarrieMeNo ratings yet
- ABC's of Primary Health Care...Document24 pagesABC's of Primary Health Care...rhenier_ilado100% (7)
- "Expanded Program On Immunization": Angeles University FoundationDocument12 pages"Expanded Program On Immunization": Angeles University FoundationJaillah Reigne CuraNo ratings yet
- Acs Ca3 BookDocument69 pagesAcs Ca3 BookchrisNo ratings yet
- 085 The Crab Tales 29 April To 12 MayDocument20 pages085 The Crab Tales 29 April To 12 MayElizabeth KingNo ratings yet
- Landasan Teori Tetanus GeneralisataDocument22 pagesLandasan Teori Tetanus GeneralisataadityaNo ratings yet
- Anti Fungal Susceptibility TestingDocument13 pagesAnti Fungal Susceptibility TestingMohamed75% (4)
- Generic Risk Assessment New and Expectant MothersDocument10 pagesGeneric Risk Assessment New and Expectant MothersBga ArmyNo ratings yet
- Health INDICATORSDocument30 pagesHealth INDICATORSYeontan Kim100% (1)
- 06SMARTeZ Drug Stability Table Non USDocument2 pages06SMARTeZ Drug Stability Table Non USJessica Blaine BrumfieldNo ratings yet
- CDC Healthcare Personnel Vaccination RecommendationsDocument1 pageCDC Healthcare Personnel Vaccination RecommendationsdocktpNo ratings yet
- Moving Target Vaccines Thimerosol and AutismDocument25 pagesMoving Target Vaccines Thimerosol and AutismcirclestretchNo ratings yet
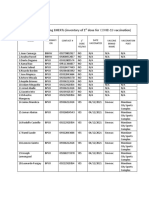
- Barangay Mantuyong Bherts (Inventory of 1 Dose For Covid-19 Vaccination)Document1 pageBarangay Mantuyong Bherts (Inventory of 1 Dose For Covid-19 Vaccination)Barangay CentroNo ratings yet
- Unit 10 Under My SkinDocument26 pagesUnit 10 Under My SkinYanz MuhamadNo ratings yet
- CPM17th RabiesDocument15 pagesCPM17th RabiesMae DoctoleroNo ratings yet
- Amniocentesis HindiDocument6 pagesAmniocentesis HindiRohit KumarNo ratings yet
- Surgical Prophylaxis: Prepared By: Gerard-IanDocument10 pagesSurgical Prophylaxis: Prepared By: Gerard-IanGerard-Ian de VeraNo ratings yet