Professional Documents
Culture Documents
A National Study of Challenges To Electronic Health
A National Study of Challenges To Electronic Health
Uploaded by
Keri Gobin SamarooOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
A National Study of Challenges To Electronic Health
A National Study of Challenges To Electronic Health
Uploaded by
Keri Gobin SamarooCopyright:
Available Formats
BRIEF REPORT
A National Study of Challenges to Electronic Health
Record Adoption and Meaningful Use
Dawn Heisey-Grove, MPH, Lisa-Nicole Danehy, MHS, Michelle Consolazio, MPA,
Kimberly Lynch, MPH, and Farzad Mostashari, MD, ScM
Background: Adoption and implementation of electronic health
records (EHRs) has not been without challenges as it infuses
technology into what has been a historically manual process of
recording patient information. In an effort to identify these challenges, the Office of the National Coordinator for Health Information Technology leveraged the Regional Extension Center
population of over 140,000 providers to develop a structured way to
track challenges to EHR adoption and Meaningful Use (MU).
Objectives: This report summarizes challenges to EHR adoption and
MU based on nationwide data supplied by 55 Regional Extension
Centers reporting over 19,000 issues representing over 43,000 unique
health care providers. Practices were grouped on the basis of their
place in the lifecycle of EHR adoption and MU achievement.
Results: Provider engagement and administrative issues were
among the more common issues reported across all cohorts. The
most challenging MU measure was the clinical summaries measure,
but MU Measure challenges varied by practice setting.
Conclusions: EHR adoption and MU challenges are unique to
practice setting and stage of the adoption process.
Key Words: electronic health record, Meaningful Use, health care
reform, health information technology
(Med Care 2014;52: 144148)
he 2009 Health Information Technology for Economic
and Clinical Health Act established the Meaningful Use
(MU) electronic health record (EHR) Incentive Program for
eligible providers and hospitals to adopt and meaningfully
use EHRs.1 MU was intentionally staged to enable all health
From the Department of Health and Human Services, Office of the Secretary, Office of the National Coordinator for Health IT, Washington, DC.
The authors declare no conflict of interest.
Reprints: Dawn Heisey-Grove, MPH, Department of Health and Human
Services, Office of the Secretary, Office of the National Coordinator for
Health IT, 330 C St, SW, Suite 1100, Washington, DC 20201. E-mail:
dawn.heisey-grove@hhs.gov.
Supplemental Digital Content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF
versions of this article on the journals Website, www.lww-medical
care.com.
Copyright r 2013 by Lippincott Williams & Wilkins
ISSN: 0025-7079/14/5202-0144
144 | www.lww-medicalcare.com
care providers to progress utilizing a series of foundational
standards into more sophisticated standards. The ultimate
goal of MU is better patient care and improved population
health at a lower cost.2
There is a strong trend toward EHR adoption among
health care providers. A 2012 study by the National Center
for Health Statistics3 estimates approximately 72% of providers are using an EHR, up from 2009 estimates of 48%.4 In
2011, nearly half (47%) of physicians not currently using an
EHR expressed intent to adopt, or had already purchased, an
EHR in the next year.5 In addition, 65% of providers have
registered with the Centers for Medicare and Medicaid
Services (CMS) EHR Incentive Program and 35% have
already been paid.3
The CMS EHR incentive payments often help to decrease the financial burden that impacts providers and hospitals in adopting this new technology. Research shows
larger practices are substantially more likely to adopt than
small practices, which may face greater challenges in
adopting and meaningfully using EHRs.5 The Office of the
National Coordinator for Health Information Technologys
(ONC) Regional Extension Centers (RECs) are tasked to
help these primary care providers, focusing on assisting organizations including small practices, community health
centers, and practices that serve underserved populations.6
RECs success in helping providers achieve MU was demonstrated in a 2012 Government Accountability Office
study,7 which found that REC-enrolled providers are 2.3
times more likely to get paid for MU through CMS EHR
incentive program. One way the RECs provide assistance to
their providers is by identifying challenges to EHR adoption
and MU, and developing targeted solutions to those challenges. Using a nationwide sample of 140,000 REC-enrolled
providers, we examine challenges to EHR adoption and MU
through descriptive analyses.
METHODS
RECs capture provider information in the ONCs
Customer Relationship Management (CRM) tool, a Webbased technology hosted by Salesforce.com. In response to
REC requests to have tools to better track and trend data
regarding challenges to EHR adoption and MU achievement,
ONC staff customized the existing database to include a
component that tracks these challenges.
The ONC CRM captures data at the parent organization, or practice level, with information on each site under
Medical Care
Volume 52, Number 2, February 2014
Medical Care
Volume 52, Number 2, February 2014
the practice (ie, a practice may be 1 site or may have multiple
sites under it). Within each site, information on each provider is captured. Information on EHR adoption and MU
challenges are captured at this level: sites may report single
or multiple challenges. The data reported by RECs includes
a description of the problem faced by the practice site. The
challenge section also captures when the problem is resolved
and when the site is on track to meeting its MU goal.
Initially, information was entered by REC staff using
several rudimentary challenge categories, with most of the
detail regarding the challenge captured in the description
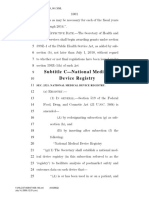
fields. After 2 months of this, 4 primary challenge classifications were established: Practice Issues, Vendor Issues,
Attestation Process Issues, and Meaningful Use measurespecific issues (Fig. 1). For measure-specific issues, multiple
MU measures can be reported within a single challenge report. An On Track classification was also added to indicate
when a site is not experiencing any challenges. ONC staff
reviewed and reclassified all challenge reports submitted
before that point. After the update, REC staff selected primary and secondary categories for each challenge issue
themselves.
ONC REC grant milestones were used to determine the
stage of EHR adoption and implementation at the time each
challenge issue was created. Milestone 1 indicates the site is
enrolled with an REC; a site that has not progressed beyond
this milestone is placed in cohort 1 (not yet live on an EHR).
Milestone 2 indicates all providers at the site are live on an
EHR with e-prescribing and quality-reporting capabilities
tested. Sites at Milestone 2 when the challenge issue was
Practice
Issues
Vendor
Issues
Workflow adoption
Upgrade
Provider engagement
Delays in implementation /
installation
Certification
Training
Reports slow / not available
Vendor selection
Training / support materials
inadequate/not available
Administrative
Lack of vendor support
Financial
Staffing
Technical
Inaccurate reports
and/or data
Challenges to EHR Adoption and Meaningful Use
created are placed in cohort 2 (EHR implementation). If a
site had multiple challenge issues reported through its lifecycle, it could be assigned to different cohorts depending on
when each issue was created.
This analysis is based on challenge reports created
between January 1 and December 31, 2012. Provider impact
for each challenge was calculated by using the number of
providers associated with the site in the CRM. Unless specifically stated, results presented below are only the reported
challenges, and do not include the On Track reports.
Analysis was completed using SAS software, version 9.2 of
the SAS System for Windows.
RESULTS
In 2012, there were 19,209 challenges and on track issues entered in the ONC CRM, representing 14,424 unique
sites (Table 1). Twenty-two percent of sites have multiple issues reported. Thirty percent of all participating REC providers
(n = 143,012) have either an on track or challenge issue reported. Over a third of all sites are reported as on track
toward EHR adoption and MU achievement (n = 5584).
Challenge issue reporting mirrors REC enrollment in most
states (Fig. 2). Eighty-nine percent of RECs (supplementary
table, Supplemental Digital Content 1, http://links.lww.com/
MLR/A617, showing challenge issues reported by REC and
REC enrollment numbers) reported at least 1 challenge or on
track issue (maximum = 2212, minimum = 2). The median
number of challenges and on track issues entered by RECs was
Attestation
MU
Process
Issues
Measures
Calculating patient
volume
Core CQMs
Medicaid program not
up yet
Alternate Core CQMs
Medicaid technical/
administrative
Additional CQMs
Medicare technical/
administrative
Each of the Core /
Menu Set measure
FIGURE 1. Regional Extension Center EHR Adoption and Meaningful Use achievement challenge issue categories. EHR indicates
electronic health record.
r
2013 Lippincott Williams & Wilkins
www.lww-medicalcare.com |
145
Medical Care
Heisey-Grove et al
Volume 52, Number 2, February 2014
TABLE 1. REC Population Representation in Challenge Reports
With Challenge
Reports
With On
Track Reports
Unique Count With an
On Track or Challenge
Issue Report
Total REC
Population
29,618
16,456
43,019
143,012
9842
55
5584
44
14,424
55
67,900
62
No. REC participating
providers
No. REC sites
No. RECs
Data on Meaningful Use Measure Challenges as reported by ONC Regional Extension Centers (RECs) in 2012. Challenge issues and on track reports are recorded at the site
level. Each site may have multiple challenges reported.
234, and the mean was 349. Unless otherwise indicated, data
presented below do not include on track reports.
A higher percentage of challenge and on track issues
were assigned to sites in cohort 2 (implementation stage)
(58%; n = 11,103). However, sites not live on an EHR (cohort 1, n = 8106) were 20% more likely to have a challenge
report than an on track report, compared with sites in the
implementation cohort (P<0.001).
Although some challenge categories were more prevalent in one cohort than another, several issues appear in the
top ranks for both. Provider engagement was the top challenge for sites not yet live on an EHR and third most common challenge for the EHR implementation cohort.
Administrative practice issues were ranked second and third
for cohorts 2 and 1, respectively. Selecting an EHR was the
second most frequently reported issue for the not yet live
cohort, whereas challenges with MU Measures is the most
commonly reported category for the EHR adoption
cohort. Table 2 provides a list of the secondary categories
Number of Reported Challenges
1-50
51-100
with the number of providers impacted and ranking for each
cohort.
Problems meeting specific Stage 1 MU measures account
for 14% of the challenge reports (n = 1668), impacting 5928
providers (Table 3). The top 5 most frequently reported MU
Measure challenges are shown in Table 3. The MU measure that
is most frequently reported as a challenge for REC-enrolled
providers is the Clinical Summary measure, with 1951 providers
reported as experiencing problems meeting this measure. The
Stage 1 core measure for drug-drug and drug-allergy interaction
checks had the fewest number of providers impacted (n = 68).
Further examination of the data by practice setting
offers insight into the different types of challenges posed by
the varying organization types (Table 3).
Solo and small private practices, defined as practices
with <10 primary care providers, are the largest practice
setting type working with RECs, comprising 36% of total
REC providers served.11 RECs report the biggest MU challenges are the Security Risk Analysis (SRA) and recording
101-250
251-500
500-1,000
>1,000
FIGURE 2. Regional Extension Center EHR Adoption and MU achievement challenges reported in 2012 by practice state. EHR
indicates electronic health record; MU, Meaningful Use.
146 | www.lww-medicalcare.com
2013 Lippincott Williams & Wilkins
Medical Care
Volume 52, Number 2, February 2014
Challenges to EHR Adoption and Meaningful Use
TABLE 2. Challenge Issues Reported by Regional Extension Centers in 2012 Adoption/Implementation Cohort
Primary Category
Practice issues
Practice issues
Practice issues
Vendor issues
Practice issues
Practice issues
MU measures
Practice issues
Practice issues
Vendor issues
Vendor issues
Attestation process
Vendor issues
Vendor issues
Attestation process
Attestation process
Vendor issues
Vendor issues
Attestation process
Vendor issues
Not Live With EHR
EHR Implementation
Secondary Category
Count
Rank
Count
Rank
Total
Provider engagement
Vendor selection
Administrative practice issues
Delays In implementation/installation
Practice workflow adoption
Financial (vendor fees, capital availability,
lack of or limited incentive eligibility)
MU measures
Practice staffing issues
Practice staff training
Other technical vendor issues
Vendor certification
Medicaid technical issues
Vendor reports and/or data are inaccurate
Vendor reports slow/not available
Problems calculating patient volume
Medicaid program not up yet
Vendor upgrade
Vendor lack of support
Medicare attestation issues
Vendor training/support materials insufficient
Total challenge issues
Total on track issues
1226
768
703
475
364
345
1
2
3
4
5
6
619
108
786
207
533
174
3
17
2
11
4
13
1845
876
1489
682
897
519
285
273
267
157
148
113
87
84
80
75
66
52
44
5
5617
2083
7
8
9
10
11
12
13
14
15
16
17
18
19
20
1383
154
334
198
33
442
247
279
143
241
127
66
215
9
6298
4261
1
14
6
12
19
5
8
7
15
9
16
18
10
20
1668
427
601
355
181
555
334
363
223
316
193
118
259
14
11915
6344
This table presents challenges to EHR adoption and Meaningful Use achievement, by adoption stage cohort, as reported by Regional Extension Centers in 2012. Shaded cells
indicate the top 5 reported challenge issues for either cohort. A total of 950 challenge issues (406 in the not yet live cohort; 544 in the EHR implementation cohort) did not include a
secondary category and are not listed in this table.
EHR indicates electronic health record.
patient smoking status. Providers in small private practices
require assistance along all steps of the SRA process, as they
usually do not have in-house IT, vendor or privacy and security expertise. Practice staff typically need education and
training on privacy and security compliance, how to perform
the SRA, and how to implement mitigation of issues identified in the SRA. Challenges in recording smoking status
within their EHR may be resolved through training of
practice staff, such as knowing where in the vendor product
to capture smoking status as structured data. For others,
challenges reside in modifying workflows to ensure that the
data are captured for all patients and may require more indepth practice coaching support.
Frequently reported among other underserved setting
types are problems associated with fully understanding and
achieving the summary care records measure. Challenges arise
in workflow redesign to facilitate the capture of appropriate
information and exchange of these data.
E-prescribing is often identified as a challenge for RECenrolled Federally Qualified Health Centers (FQHCs) and
Lookalikes (methods for identifying FQHCs described previously8). Among FQHCs, the issues may lie in the lack of an
interface with an internal pharmacy. These organizations may
also have financial problems in being able to afford a system to
electronically accept prescriptions. Alternately, some FQHCs
meet challenges in doing e-prescribing for medications their
patients may receive subsidies for.
The ability to meet the immunization reporting requirement is a commonly reported issue for the rural health
clinic setting type. Providers in this setting often indicate
r
2013 Lippincott Williams & Wilkins
they are waiting on either a vendor interface to facilitate
reporting or the local health department for testing. Identifying financial resources to pay for the interface or to facilitate reporting capabilities is also a common problem.
In both Critical Access Hospitals (CAHs) and rural
hospitals (RHs), staff are in need of additional education
related to the patient reminder measure. This education may
also help combat resistance encountered from providers in
making the necessary workflow changes.
DISCUSSION
New challenges emerge as providers progress toward
MU, creating opportunities to preempt large-scale issues with
timely interventions. These interventions must take into account organizational and cultural dynamics, increasing the
need to identify multiple, often setting-specific, solutions. If
identified quickly and a timely response is provided, problems
may be halted before becoming widespread or impeding
progress. For example, initial rollout of the CMS registration
process initially posed challenges to many providers. RECs
collectively organized and addressed these by building tools
and processes that were proactively shared with providers,
ultimately leading to more timely attestation and payment.9 To
address the large number of challenge reports around the
Clinical Summaries MU measure, ONC and the RECs developed a variety of tools then tested in the field by RECs
(Supplemental Digital Content 2, http://links.lww.com/MLR/
A618, case study highlighting Clinical Summary measure
challenges and solutions development).10
www.lww-medicalcare.com |
147
Medical Care
Heisey-Grove et al
Volume 52, Number 2, February 2014
TABLE 3. Top 5 REC-reported Stage 1 Meaningful Use Measure Challenges by Practice Setting
Regional Extension
Center Overall
Top 5 Challenges
Small Private
Practice (r10
Providers)
Other
Underserved
Settings
Federally Qualied
Health Centers
and Lookalikes
Rural Health
Clinics
Critical Access
Hospitals and
Rural Hospitals
Clinical summary
(500/1951)
Clinical summary
(231/636)
Clinical summary
(106/664)
Security risk analysis
(33/112)
Clinical summary
(12/41)
Clinical summary
(33/188)
Security risk analysis
(263/822)
Security risk analysis
(163/394)
Patient reminders
(91/506)
Immunization (31/94)
Immunization
(8/13)
Medication reconciliation
(24/135)
Medication reconciliation
(187/822)
Immunization
(139/289)
Summary care record
(89/508)
eRx (28/102)
Smoking status
(8/13)
Summary care record
(24/145)
Summary care record
(171/756)
Electronic exchange
(116/288)
Medication reconciliation
(60/467)
Electronic exchange
(23/70)
Medication
reconciliation (7/17)
Patient reminders
(22/148)
Patient reminders
(166/753)
Smoking status
(96/228)
Educational resources
(60/342)
Clinical summary
(21/116)
Educational
resources (7/11)
Educational resources
(20/129)
Data on Meaningful Use (MU) measure challenges as reported by ONC Regional Extension Centers (RECs) in 2012. Values in parentheses represent the number of reports/
number of providers. The column on the far left reflects the top 5 MU measure challenges across all REC providers. The columns to the right of that include selected practice settings
within the REC-enrolled population, with the overall top 5 measures shaded when they reappear in the setting-specific columns. Small private practices are defined as having r10
primary care physicians in the practice. Other underserved settings are generally defined by RECs as other ambulatory settings that predominantly serve uninsured, underinsured, and
medically underserved populations.
Another example of evidence-based, proactive tool development is creation of a toolkit for CAHs and RHs. RECs
partnered with 2 EHR vendors that hold significant market
shares for health IT solutions dedicated to CAHs and RHs and
developed product-specific toolkits to provide an implementation path to MU. The task force developed the toolkits
after testing and collecting feedback from 11 CAHs and RHs
across 3 states.
RECs are working with 44% of all primary care providers in the United States.11 However, given the REC focus
on primary care providers, challenges reported here may
differ from those faced by other provider populations. In
addition, as not all RECs are using the CRM challenge reports to capture data, or are using the reporting system differently, all parts of the country may not be represented
equally. Despite these limitations, REC reports do represent
a significant portion of primary care providers and serve in
understanding challenges faced by some populations struggling with EHR adoption and MU achievement.
Challenges to EHR adoption, implementation, and MU
achievement are widely known, but this is the first nationwide assessment of these challenges. This work has identified and categorized those challenges so best practices, tools,
and resources can be developed and targeted to groups who
need the most assistance.
REFERENCES
1. American Recovery and Reinvestment Act of 2009, Pub. L. No. 111-5,
Pub. L. No. 111-5, div. A, tit. XIII, 123 Stat. 115, 226-279 and div. B,
tit. IV, 123 Stat. 115, 467-496 (2009). Available at: http://www.gpo.gov/
fdsys/pkg/BILLS-111hr1enr/pdf/BILLS-111hr1enr.pdf. Accessed December 6, 2012.
148 | www.lww-medicalcare.com
2. Medicare and Medicaid Programs; Electronic Health Record Incentive
Program; Final Rule. Fed. Reg. 75:144 (Jul. 28, 2010) p. 44314.
Available at: http://www.gpo.gov/fdsys/pkg/FR-2010-07-28/pdf/201017207.pdf.
3. Hsiao CJ, Hing E. Use and Characteristics of Electronic Health Record
Systems Among Office-Based Physician Practices: United States, 20012012. NCHS Data Brief, no. 111. Hyattsville, MD: National Center for
Health Statistics; 2012. http://www.cdc.gov/nchs/data/databriefs/db111.htm.
4. Hsiao CJ, Hing E, Socey TC, et al. Electronic Medical Record/
Electronic Health Record Systems Of Office-Based Physicians: United
States, 2009 and Preliminary 2010 State Estimates. Health E-Stats.
National Center for Health Statistics; 2010. http://www.cdc.gov/nchs/
data/hestat/emr_ehr_09/emr_ehr_09.htm.
5. Jamoom E, Beatty P, Bercovitz A, et al. Physician Adoption of Electronic
Health Record Systems: United States, 2011. NCHS Data Brief, no. 98.
Hyattsville, MD: National Center for Health Statistics 2012.
6. Maxson E, Jain S, Kendall M, et al. The Regional Extension Center
program: helping physicians meaningfully use health information
technology. Ann Intern Med. 2010;153:666670.
7. Government Accountability Office. Electronic Health Records: Number
and Characteristics of Providers Awarded Medicare Incentive Payments
for 2011, GAO-12-778R. Washington, DC: Government Accountability
Office; 2012. http://www.gao.gov/assets/600/593078.pdf.
8. Heisey-Grove D, Hawkins K, Jones E, et al. Supporting Health
Information Technology Adoption in Federally Qualified Health
Centers. ONC Data Brief, no. 8. Washington, DC: Office of the
National Coordinator for Health Information Technology; 2013.
9. Kissam SM, Banger AK, Dimitropoulos LL, et al. Barriers to
Meaningful Use in Medicaid: Analysis and recommendations. (Prepared by RTI International, under Contract No. HHSA290200710079T.)
AHRQ Publication No. 12-0062-EF. Rockville, MD: Agency for
Healthcare Research and Quality; 2012. http://healthit.ahrq.gov/Barrier
stoMeaningfulUseFinalReport.
10. Kessels RP. Patients memory for medical information. J R Soc Med.
2003;96:219222.
11. Lynch K, Kendall M, Shanks K, et al. The Health IT Regional Extension
Center Program: evolution and lessons for health care transformation.
Health Services Research. 2013. [In press].
2013 Lippincott Williams & Wilkins
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5822)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (852)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (898)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (349)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (403)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- CAHIMS Learning Plan: Preparing For Success in Healthcare Information and Management Systems: The CAHIMS Review GuideDocument6 pagesCAHIMS Learning Plan: Preparing For Success in Healthcare Information and Management Systems: The CAHIMS Review GuideZubeen ShahNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Electronic Prescriptions For Controlled SubstancesDocument335 pagesElectronic Prescriptions For Controlled SubstancesJames Lindon100% (1)
- Construct2 ManualDocument9 pagesConstruct2 ManualKeri Gobin SamarooNo ratings yet
- Canvas Student GuideDocument419 pagesCanvas Student GuideKeri Gobin SamarooNo ratings yet
- Solutions From EnderleDocument9 pagesSolutions From EnderleKeri Gobin SamarooNo ratings yet
- Turning Android Smartphones Into Professional Thermography CamerasDocument4 pagesTurning Android Smartphones Into Professional Thermography CamerasKeri Gobin SamarooNo ratings yet
- Bio Med Hipaa RileyD - 2Document1 pageBio Med Hipaa RileyD - 2Keri Gobin SamarooNo ratings yet
- Agri Portfolio-1Document37 pagesAgri Portfolio-1Keri Gobin Samaroo100% (1)
- Health Informatics Technology in Population Healthcare AnalyticsDocument54 pagesHealth Informatics Technology in Population Healthcare AnalyticsPradeep JoshiNo ratings yet
- Lesson 1 Overview of Health InformaticsDocument5 pagesLesson 1 Overview of Health InformaticsDOMILE, SAMANTHA RIANNENo ratings yet
- Nur 1211: Nursing InformaticsDocument29 pagesNur 1211: Nursing InformaticsAllyza EspirituNo ratings yet
- Opportunities and Challenges in An Evolving Market (KPMG)Document48 pagesOpportunities and Challenges in An Evolving Market (KPMG)vikalp123123No ratings yet
- Chapter 25 InformaticsDocument76 pagesChapter 25 InformaticsJa DimasNo ratings yet
- Federal Health IT Strategic Plan - 2020 - 2025Document50 pagesFederal Health IT Strategic Plan - 2020 - 2025CherylNo ratings yet
- Comments On Meaningful Use Stage 2Document4 pagesComments On Meaningful Use Stage 2vidmar polorioNo ratings yet
- Cphims Learning Plan 2020-1-3Document6 pagesCphims Learning Plan 2020-1-3PatriciaNo ratings yet
- Electronic Health Record (EHR) Certification ProgramDocument2 pagesElectronic Health Record (EHR) Certification ProgramONC for Health Information TechnologyNo ratings yet
- Senate Hearing, 111TH Congress - Departments of Labor, Health and Human Services, and Education, and Related Agencies Appropriations For Fiscal Year 2011Document655 pagesSenate Hearing, 111TH Congress - Departments of Labor, Health and Human Services, and Education, and Related Agencies Appropriations For Fiscal Year 2011Scribd Government DocsNo ratings yet
- 07 Health Data Standards Development Harmonization and Interoperability TRANSESDocument5 pages07 Health Data Standards Development Harmonization and Interoperability TRANSESElyza DionisioNo ratings yet
- CHAPTER 16 Nursing Informatics and Healthcare PolicyDocument9 pagesCHAPTER 16 Nursing Informatics and Healthcare PolicyAllyssa Leila Estrebillo OrbeNo ratings yet
- Nursing InformaticsDocument10 pagesNursing InformaticsNoisy KenNo ratings yet
- 1 10Document60 pages1 10Kaden MikaelNo ratings yet
- NCM 110 Module 1 Historical Perspectives of Nursing InformaticsDocument21 pagesNCM 110 Module 1 Historical Perspectives of Nursing InformaticsKi PieNo ratings yet
- Informatics PrelimDocument47 pagesInformatics PrelimtrishaNo ratings yet
- Ramos, Sioco Chapter 25 and 26Document59 pagesRamos, Sioco Chapter 25 and 26DOROTHY ANN SOMBILUNANo ratings yet
- Subtitle C-National Medical Device Registry: Ffective ATEDocument8 pagesSubtitle C-National Medical Device Registry: Ffective ATEVino DNo ratings yet
- EMR Vs EMRDocument6 pagesEMR Vs EMRisurukalharaNo ratings yet
- Nursing Informatics PrelimsDocument65 pagesNursing Informatics PrelimsANHIBEY, JEZREEL ACE S.No ratings yet
- Nursing InformaticsDocument102 pagesNursing InformaticsYumeko JabamiNo ratings yet
- Recent Research Papers in Medical ElectronicsDocument9 pagesRecent Research Papers in Medical Electronicsh040pass100% (1)
- Sas#1 MLS050Document11 pagesSas#1 MLS050Aubrey BrionesNo ratings yet
- Mls 050 NotesDocument24 pagesMls 050 NotesJulianneNo ratings yet
- 175671756RFPDocument72 pages175671756RFPOliverNo ratings yet
- Nursing Informatics Topic OutlineDocument23 pagesNursing Informatics Topic OutlineAngela Joy AmparadoNo ratings yet
- ISSUES IN INFORMATICS and NURSING INITIATIVESDocument16 pagesISSUES IN INFORMATICS and NURSING INITIATIVESFilamae Jayahr CadayNo ratings yet
- Nursing InformaticsDocument26 pagesNursing InformaticsMary Ann SacramentoNo ratings yet