Professional Documents
Culture Documents
ContentServer Asp
ContentServer Asp
Uploaded by
CoralonCopyright:
Available Formats
You might also like
- VP - PSV SEA VEGA REV.0 (New Logo) r2Document4 pagesVP - PSV SEA VEGA REV.0 (New Logo) r2Sugiman LayantoNo ratings yet
- Mcq. SurgeryDocument132 pagesMcq. Surgeryمنتظر اللاميNo ratings yet
- Impulsivity 7Document3 pagesImpulsivity 7Joe Hodge100% (1)
- Jurnal Diagnostik ADocument8 pagesJurnal Diagnostik AImtina AhdaNo ratings yet
- Gyaneshwar Tonk-Anatomical and Functional EvaluationDocument11 pagesGyaneshwar Tonk-Anatomical and Functional EvaluationchinmayghaisasNo ratings yet
- Accepted Manuscript: Injury, Int. J. Care InjuredDocument16 pagesAccepted Manuscript: Injury, Int. J. Care InjuredDwi AryanataNo ratings yet
- Paper 4. Study of Intra-Articular Distal End Radius EJMCMDocument9 pagesPaper 4. Study of Intra-Articular Distal End Radius EJMCMNaveen SathyanNo ratings yet
- 223654-Article Text-546414-1-10-20220403Document6 pages223654-Article Text-546414-1-10-20220403Christopher Freddy Bermeo RiveraNo ratings yet
- Mcrae 2015Document8 pagesMcrae 2015Ananth BalakrishnanNo ratings yet
- Surgical Treatment of Chronic Elbow Dislocation Allowing For Early Range of Motion: Operative Technique and Clinical ResultsDocument8 pagesSurgical Treatment of Chronic Elbow Dislocation Allowing For Early Range of Motion: Operative Technique and Clinical ResultsLuis Carlos HernandezNo ratings yet
- Functional Outcome After The Conservative Management of A Fracture of The Distal HumerusDocument7 pagesFunctional Outcome After The Conservative Management of A Fracture of The Distal HumerusnireguiNo ratings yet
- Clearing The Cervical Spine of Adult Victims of TraumaDocument7 pagesClearing The Cervical Spine of Adult Victims of TraumaVince AzevoucheNo ratings yet
- Clinicoradiological and Functional Outcomes of Lisfranc Injuries Managed by Different Treatment Modalities in A Tertiary Care CentreDocument7 pagesClinicoradiological and Functional Outcomes of Lisfranc Injuries Managed by Different Treatment Modalities in A Tertiary Care CentreIJAR JOURNALNo ratings yet
- 08 Can We Safely Apply The Ottawa Ankle Rules To ChildrenDocument3 pages08 Can We Safely Apply The Ottawa Ankle Rules To ChildrenAlejandro Godoy SaidNo ratings yet
- 1547 5654 Article p80Document12 pages1547 5654 Article p80wilsonwqaNo ratings yet
- Semiconstrained Total Elbow Arthroplasty-1Document6 pagesSemiconstrained Total Elbow Arthroplasty-1Ευαγγελια ΚιμπαρηNo ratings yet
- Trauma Clinical Guideline 2017Document7 pagesTrauma Clinical Guideline 2017Paolo ContrerasNo ratings yet
- Modi Ed Percutaneous Kirschner Wire With Mutual Linking Technique in Proximal Humeral Fracture: A Technique Note and Preliminary ResultsDocument14 pagesModi Ed Percutaneous Kirschner Wire With Mutual Linking Technique in Proximal Humeral Fracture: A Technique Note and Preliminary ResultsRahul ReddyNo ratings yet
- 2023 JOT Radiological and Long Term Functional Outcomes of Displaced Distal Clavicle FracturesDocument7 pages2023 JOT Radiological and Long Term Functional Outcomes of Displaced Distal Clavicle FracturesjcmarecauxlNo ratings yet
- Closed Intra - Articular Fractures of The Distal End of Humerus Surgically Treated by Trans - Olecranon Approach Using The Chevron OsteotomyDocument4 pagesClosed Intra - Articular Fractures of The Distal End of Humerus Surgically Treated by Trans - Olecranon Approach Using The Chevron OsteotomyIJAR JOURNALNo ratings yet
- Circumferential Casting of Distal Radius PDFDocument5 pagesCircumferential Casting of Distal Radius PDFRajiv TanwarNo ratings yet
- Principles of Critical Care MedicineDocument4 pagesPrinciples of Critical Care MedicineKarthik SNo ratings yet
- Vol29 - No2 - 59 - 63Document5 pagesVol29 - No2 - 59 - 63Kagiso Gigfreak Urban RoccoNo ratings yet
- Journal ReadingDocument7 pagesJournal ReadingTommy HardiantoNo ratings yet
- Poster PapersDocument262 pagesPoster PapersLeonardo RodríguezNo ratings yet
- PLDD&MicrodiscectomyLeiden NL 2015Document9 pagesPLDD&MicrodiscectomyLeiden NL 2015YAŞAR TÜRKNo ratings yet
- A Randomized Controlled Trial of Nonoperative Treatment Versus Open Reduction and Internal Fixation For Stable, Displaced, Partial Articular Fractures of The Radial Head: The RAMBO TrialDocument5 pagesA Randomized Controlled Trial of Nonoperative Treatment Versus Open Reduction and Internal Fixation For Stable, Displaced, Partial Articular Fractures of The Radial Head: The RAMBO TrialAndi Urviana AsrahNo ratings yet
- The Effect of Ulnar Styloid Fractures On Patient-Reported Outcomes After Surgically Treated Distal Radial FracturesDocument7 pagesThe Effect of Ulnar Styloid Fractures On Patient-Reported Outcomes After Surgically Treated Distal Radial FracturesOpsonin PharmaNo ratings yet
- Sipola. Detection and Quantification of Rotator Cuff Tears With Ultrasonography and Magnetic Resonance Imaging - A ProsDocument9 pagesSipola. Detection and Quantification of Rotator Cuff Tears With Ultrasonography and Magnetic Resonance Imaging - A Prossteven saputraNo ratings yet
- American Journal of Emergency MedicineDocument5 pagesAmerican Journal of Emergency MedicineMaria teresa salinas merelloNo ratings yet
- 10 1016@j Jse 2019 10 013Document12 pages10 1016@j Jse 2019 10 013Gustavo BECERRA PERDOMONo ratings yet
- 16 Van Leerdam Et Al J Hand Surg Eur Vol. 2017 Jun 42 5 501 506 AAMDocument13 pages16 Van Leerdam Et Al J Hand Surg Eur Vol. 2017 Jun 42 5 501 506 AAMChristopher Freddy Bermeo RiveraNo ratings yet
- Lca TestDocument5 pagesLca Testkaren.heredia257No ratings yet
- To Evaluate The Functional Outcome of Volar Plating in Distal End Radius FracturesDocument11 pagesTo Evaluate The Functional Outcome of Volar Plating in Distal End Radius FracturesIJAR JOURNALNo ratings yet
- PDR Rsik Factors For RedisplacementDocument6 pagesPDR Rsik Factors For RedisplacementCleff FlowersNo ratings yet
- Definingnoptimal Calcar Screw Positioning in Proximal Humerus Fracture FixationDocument7 pagesDefiningnoptimal Calcar Screw Positioning in Proximal Humerus Fracture FixationAJ CésarNo ratings yet
- 4 03000605221103974Document13 pages4 03000605221103974Teuku FadhliNo ratings yet
- Jurnal Fraktur Humerus DistalDocument5 pagesJurnal Fraktur Humerus DistalthisisangieNo ratings yet
- Seguimiento A 5 Años PTGH ReversaDocument7 pagesSeguimiento A 5 Años PTGH Reversamarcelogascon.oNo ratings yet
- Primary Total Shoulder Arthroplasty Performed Entirely Thru The Rotator Interval - Technique and Minimum Two-Year OutcomesDocument10 pagesPrimary Total Shoulder Arthroplasty Performed Entirely Thru The Rotator Interval - Technique and Minimum Two-Year OutcomesmotohumeresNo ratings yet
- Tan2012 PDFDocument10 pagesTan2012 PDFdebyanditaNo ratings yet
- 1 s2.0 S0303846708002114 MainDocument5 pages1 s2.0 S0303846708002114 MainFNo ratings yet
- Lumbal Spinal Stenosis ODI ScoreDocument10 pagesLumbal Spinal Stenosis ODI ScoreTusan SidhartaNo ratings yet
- 17.PLDD Vs Surgery RCTDocument9 pages17.PLDD Vs Surgery RCTBeata SviantickaNo ratings yet
- Percutaneaus Kirschner-Wire Fixation For Displaced Distal Forearm Fractures in ChildrenDocument5 pagesPercutaneaus Kirschner-Wire Fixation For Displaced Distal Forearm Fractures in ChildrennaluphmickeyNo ratings yet
- Open FractureDocument16 pagesOpen FractureMazvita Maz MatipiraNo ratings yet
- Cervical Spine Clearance 2009Document7 pagesCervical Spine Clearance 2009Abdulelah Al.luhaybiNo ratings yet
- Bryan MorreyDocument5 pagesBryan MorreyokisutartoNo ratings yet
- Two Casting Methods Compared in Patients With Colles' Fracture: A Pragmatic, Randomized Controlled TrialDocument12 pagesTwo Casting Methods Compared in Patients With Colles' Fracture: A Pragmatic, Randomized Controlled TrialTeja Laksana NukanaNo ratings yet
- The Clinical Outcome After Extra-Articular Colles Fractures With Simultaneous Moderate Scapholunate DissociationDocument5 pagesThe Clinical Outcome After Extra-Articular Colles Fractures With Simultaneous Moderate Scapholunate DissociationYina Marcela Quintero OrtegaNo ratings yet
- Paper Section 3 Draft1Document11 pagesPaper Section 3 Draft1api-568855135No ratings yet
- Abstracts - Final Off Print BJNDocument57 pagesAbstracts - Final Off Print BJNZieshNo ratings yet
- Open Reduction and Internal Fixation ORIF of ComplDocument6 pagesOpen Reduction and Internal Fixation ORIF of ComplAnnisa AnggrainiNo ratings yet
- Ditkofsky 2015Document28 pagesDitkofsky 2015Allython Jureth Peña ReyesNo ratings yet
- Cast Immobilisation With and Without Immobilisation of The Thumbfor Non-Displaced Scaphoid FracturesDocument7 pagesCast Immobilisation With and Without Immobilisation of The Thumbfor Non-Displaced Scaphoid FracturesmonkeyzergNo ratings yet
- HTTPS://WWW Mendeley Com/reference-Manager/readerDocument6 pagesHTTPS://WWW Mendeley Com/reference-Manager/readerIJAR JOURNALNo ratings yet
- Long Term Outcome of Isolated DiaphysealDocument5 pagesLong Term Outcome of Isolated DiaphysealVIDevAryanNo ratings yet
- Preoperative Close Reduction of Cervical Fracture DislocationsDocument8 pagesPreoperative Close Reduction of Cervical Fracture DislocationsIJAR JOURNALNo ratings yet
- Use of Surgical Augmented Intelligence Maps Can ReDocument11 pagesUse of Surgical Augmented Intelligence Maps Can Resebasags19No ratings yet
- A Randomized Controlled Trial of Endovascular Aneurysm Repair Versus Open Surgery For Abdominal Aortic Aneurysms in Low - To Moderate-Risk PatientsDocument8 pagesA Randomized Controlled Trial of Endovascular Aneurysm Repair Versus Open Surgery For Abdominal Aortic Aneurysms in Low - To Moderate-Risk Patientsvfd08051996No ratings yet
- Distal Femur Fractures Fixation by Locking Compression Plate-Assessment of Outcome by Rasmussens Functional Knee ScoreDocument7 pagesDistal Femur Fractures Fixation by Locking Compression Plate-Assessment of Outcome by Rasmussens Functional Knee ScoreIJAR JOURNALNo ratings yet
- Hip Dislocation Are Hip Precautions Necessary in Anterior ApproachesDocument6 pagesHip Dislocation Are Hip Precautions Necessary in Anterior Approaches阿欧有怪兽No ratings yet
- Target Volume Delineation for Pediatric CancersFrom EverandTarget Volume Delineation for Pediatric CancersStephanie A. TerezakisNo ratings yet
- ScopeDocument3 pagesScopeGalano, Hana MarieNo ratings yet
- Reading b2 c1Document4 pagesReading b2 c1Karenza ThomasNo ratings yet
- Company Profile Kalgen Innolab Innobiogram - 2022Document12 pagesCompany Profile Kalgen Innolab Innobiogram - 2022asmadi arrumNo ratings yet
- The English Opening: Grandmaster Repertoire 3Document10 pagesThe English Opening: Grandmaster Repertoire 3lietotajs71No ratings yet
- Building Construction Company ProfileDocument62 pagesBuilding Construction Company ProfileFadhlan Dwi Gusti WarmanNo ratings yet
- Design Princples For Wood Burning Cook StovesDocument20 pagesDesign Princples For Wood Burning Cook Stoveshana temesegenNo ratings yet
- Unit 5. PHCDocument24 pagesUnit 5. PHCFenembar MekonnenNo ratings yet
- 1000 English Collocations EbookDocument128 pages1000 English Collocations EbookHerdeiro DicaprioNo ratings yet
- Pamphlet 21 (NCl3)Document210 pagesPamphlet 21 (NCl3)victorNo ratings yet
- Symbols: First LetterDocument2 pagesSymbols: First LetterFIDAH FYSALNo ratings yet
- The Following Is An Excerpt FromDocument12 pagesThe Following Is An Excerpt FromViktoria MolnarNo ratings yet
- Desoldering Tool: Designed For Lead FreeDocument2 pagesDesoldering Tool: Designed For Lead FreeMarco Antonio Ortiz RomeroNo ratings yet
- Suzumar Boat Engine PackagesDocument7 pagesSuzumar Boat Engine PackagesmarkoNo ratings yet
- PM Handbook (Full PDFDocument88 pagesPM Handbook (Full PDFGary LoNo ratings yet
- Hypogear 80W-90 - BP Australia Pty LTDDocument5 pagesHypogear 80W-90 - BP Australia Pty LTDBiju_PottayilNo ratings yet
- Process, People, and Conflict Management in OrganizationsDocument6 pagesProcess, People, and Conflict Management in OrganizationsMeldy IamNo ratings yet
- NIM: 2440007043 Nama: Ni Putu Young Yenyuo A Mata Kuliah: Accounting For Business Dosen: Herlin Tundjung SetijaningsihDocument5 pagesNIM: 2440007043 Nama: Ni Putu Young Yenyuo A Mata Kuliah: Accounting For Business Dosen: Herlin Tundjung SetijaningsihiyeNo ratings yet
- CED-PQP-5225-F01 Rev.0 Sieve AnalysisDocument4 pagesCED-PQP-5225-F01 Rev.0 Sieve AnalysisSslan seelanNo ratings yet
- Wallmat Supply Chain Analysis PDFDocument44 pagesWallmat Supply Chain Analysis PDFProsenjit RoyNo ratings yet
- NYJC Prelim 2006 P2Document12 pagesNYJC Prelim 2006 P2miiewNo ratings yet
- Topic 5 AC To AC ConverterDocument53 pagesTopic 5 AC To AC ConverterNorain ZakariaNo ratings yet
- PCB Design Techniques To Reduce EMIDocument21 pagesPCB Design Techniques To Reduce EMIelfrichNo ratings yet
- Hyva Oil Tank: Single Support Tank Double Support TankDocument4 pagesHyva Oil Tank: Single Support Tank Double Support TankPutera Bumi NusantaraNo ratings yet
- P I Iso TP M v13 enDocument6 pagesP I Iso TP M v13 enPedro SepúlvedaNo ratings yet
- Heridity: Table of SpecificationsDocument8 pagesHeridity: Table of SpecificationsJoseph GratilNo ratings yet
- Lec5 - Geotechnical Investigation Reports and Foundation Recommendations-Scope For Improvement-ExamplesDocument20 pagesLec5 - Geotechnical Investigation Reports and Foundation Recommendations-Scope For Improvement-ExamplesrohitNo ratings yet
- Demonizing Drugmakers: The Political Assault On The Pharmaceutical Industry, Cato Policy Analysis No. 475Document56 pagesDemonizing Drugmakers: The Political Assault On The Pharmaceutical Industry, Cato Policy Analysis No. 475Cato InstituteNo ratings yet
ContentServer Asp
ContentServer Asp
Uploaded by
CoralonOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
ContentServer Asp
ContentServer Asp
Uploaded by
CoralonCopyright:
Available Formats
Emergency Medicine Australasia (2009) 21, 298303
doi: 10.1111/j.1742-6723.2009.01200.x
ORIGINAL RESEARCH
Emergency department management of
Colles-type fractures: A prospective
cohort study
emm_1200
298..303
William Blakeney and Laurence Webber
Sir Charles Gairdner Hospital, Nedlands, Western Australia, Australia
Abstract
Objective:
To assess radiographic outcomes from ED reduction of Colles-type fractures.
Design:
Prospective cohort.
Setting:
One tertiary hospital in Western Australia.
Participants:
All patients (184) between ages 2185 years, presenting to ED with Colles-type fractures
between 1 April 2006 to 31 July 2008. Fractures were divided into two groups. Those with
15 dorsal angulation were classified as minimally displaced and those with >15 dorsal
angulation were classified as displaced.
Main outcome
measures:
Radiographic analysis of the dorsal angle on post-reduction and 6 week post-fracture
X-rays. A combined end-point of poor outcome, as defined by either poor radiological result
and/or progression to surgery.
Results:
In the group of patients with displaced fractures, 69 of 114 (61%) went on to have an
operation or a poor radiographic outcome versus 8 of 48 (17%) in the group with minimally
displaced fractures, an absolute difference of 44% (95% CI 3057%). Patients who had a
minimally displaced fracture with an adequate reduction went on to have a satisfactory
6 week X-ray in 37 of 43 cases (86%; 95% CI 7596%). Patients who had a displaced
fracture and an adequate reduction had a satisfactory 6 week X-ray in 42 of 86 cases (49%;
95% CI 3859%). Patients who had a displaced fracture and an inadequate reduction had
a satisfactory 6 week X-ray in only 3 of 22 cases (14%; 95% CI 028%).
Conclusion:
The study highlights the importance of the initial on arrival and post-reduction X-rays in
the ED. Displaced fractures are more likely to go onto poor outcome, as are inadequately
reduced fractures. Medical officers working in ED should be aware of the importance of
measuring the dorsal angle. They should be referring patients with >15 dorsal angulation
to orthopaedics early. Reduction should not be accepted until the dorsal angle has been
adequately corrected.
Key words:
Colles fracture/radiography, fracture fixation, fracture/radiography, radius prognosis, treatment outcome.
Correspondence:
Dr William Blakeney, 42/105 Colin Street, West Perth, WA 6005, Australia. Email: blakeney@gmail.com
William Blakeney, MB BS, Orthopaedic Surgery Registrar; Laurence Webber, MB BS, General Surgery Registrar.
2009 The Authors
Journal compilation 2009 Australasian College for Emergency Medicine and Australasian Society for Emergency Medicine
Management of Colles-type fractures
Introduction
Patients with distal radius fractures frequently present
to ED for assessment and management.1,2 The most
common type of distal radius fracture is the Colles-type
fracture (distal radius fracture within 2.5 cm of the wrist
with dorsal angulation of the distal fragment). This type
of fracture usually occurs following a fall on an outstretched hand. It occurs in all ages and sexes, but
typically in middle-aged to elderly women.
It is common practice within Western Australia when
a patient presents to the ED with an uncomplicated
Colles-type fracture for that patient to be dealt with
entirely by ED medical officers and then to be referred
to orthopaedics fracture clinic to be seen in 12 weeks.
This practice reduces the patient burden on the orthopaedic team. If, however, there is any indication that the
patient is likely to have an adverse outcome from the
fracture, it would be beneficial to have that patient
identified at an early stage.
The largest study of distal radius fractures produced
several complex formulae to predict radiographic
outcome using up to six independent variables.3 Other
studies have also come up with many different variables
predictive of poor radiographic outcome.46 These
studies, however, all include the predictive value of the
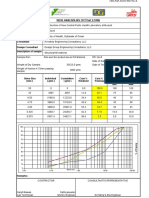
measurement of the dorsal angle. The dorsal angle (see
Fig. 1) is a quick and easy measurement to take from the
lateral X-ray of the wrist. In the often time-scarce setting
of a busy ED, it would be most valuable for the ED
medical officer to be armed with one simple predictor of
outcome, and therefore indicator for early orthopaedic
referral.
It has long been known that good anatomical reduction at follow up, evaluated by standard radiographic
criteria, equates with the best long-term functional
outcome.7,8 Studies have looked at many different
radiographic measurements for assessment of these
fractures.912 The measurement on follow-up X-rays that
is most closely associated with good functional outcome
is the dorsal angle. It is fair to hypothesize that the
initial dorsal angle on the ED X-rays might be associated with the dorsal angle at 6 week follow up. If this
proves to be the case, then the initial X-rays of the
fracture will give the treating doctor a good indication
of the likely outcome and potentially allow early identification of patients with certain fracture parameters
who might benefit from early orthopaedic referral and
consideration of intervention.
This prospective cohort study followed all patients
presenting to a tertiary hospital ED with a Colles-type
fracture requiring manipulation.
Method
Selection of study population
The patient cohort was selected from patients presenting to Sir Charles Gairdner Hospital (a tertiary hospital
in Perth, Western Australia). All patients upon discharge from the ED routinely receive one or more ICD
10 categorizations. The patients with the primary diagnostic codes S52.50 injury-+fractures/closed-+upper
limb-+radius-lower and/or S62.8 injury-+fractures/
closed-+upper limb-+wrist-wrist entered into the
hospitals Emergency Department Information System
(EDIS), were eligible for the study. The hospital unit
numbers of patients with these diagnostic codes were
flagged in the electronic radiology database automatically building a work list. This enabled us to capture all
patients presenting with a Colles-type fracture without
creating extra work for ED staff, and effectively provided an operator-blinded study.
Inclusion/exclusion criteria
Figure 1.
Measuring the dorsal angle.
Patients included in the final analysis group were aged
between 21 and 85 years with radiological evidence of a
Colles-type fracture (distal radius fracture within 2.5 cm
of the wrist with dorsal angulation of the distal fragment). Patients included must have had their fractures
manipulated. The decision to manipulate the fracture
was at the discretion of the treating ED medical officer.
2009 The Authors
Journal compilation 2009 Australasian College for Emergency Medicine and Australasian Society for Emergency Medicine
299
W Blakeney and L Webber
Patients with radiological evidence of intra-articular
fractures, open fractures or previous fracture malunion
were excluded from the study.
All fractures were immobilized in a standard plaster
of Paris back-slab after reduction.
Radiological evaluation
The radiographs of patients meeting these criteria were
de-identified and transferred to an image storage disc.
The degree of dorsal or volar tilt was measured (using a
vectorial goniometer) on the initial pre-reduction film,
the post-reduction film and the 6 week post-fracture
follow-up films.
For those patients who required further manipulation, if the initial post-reduction film was deemed
unsatisfactory, measurements were recorded from the
final post-reduction X-ray before discharge from the
ED.
All films were viewed using a high-resolution
monitor and IMPAX X-ray viewing software (identical
to that used by the staff in the ED). To determine the
degree of angulation, we first drew in the long axis of
the distal radius, then drew a line touching the most
distal points of the radial articular surface visible on
the lateral film. Second, we used an automated goniometric tool to measure the angle between these lines
and recorded positive values as dorsal displacement
and negative values as volar displacement (see
Fig. 1).
Fractures were divided into two groups. Those with
15 dorsal angulation were classified as minimally
displaced and those with >15 dorsal angulation were
classified as displaced.
Statistical methods
Comparison was made between the numbers achieving
the above outcomes in both minimally displaced and
displaced groups. We used Fishers exact test to determine whether the differences observed were significant.
Ancillary analyses
We separately placed the patients into two groups
based on adequate or inadequate reduction in the ED,
defined by the same reduction criteria as above, and
compared the final outcomes in these two groups.
Patients were then stratified by adequacy of reduction to see if the initial X-ray was still predictive of
outcome.
Blinding
All those involved in clinical care of patients were
blinded to the study.
X-rays were de-identified, thus blinding the investigators before measuring.
Sample size
We thought that a 25% difference in outcome between
the two arms would be important to detect. Assuming
that the minimally displaced group would have a good
outcome in 90% of cases, with a power of 0.9 and
significance level of 0.05, we would need 53 patients in
each arm.
Results
Reduction criteria
Post-reduction films that demonstrated dorsal angulation of <10 and volar angulation <20 were defined as
adequately reduced. Those films that demonstrated
dorsal angulation of 10 or volar angulation of 20
were deemed inadequately reduced.
Outcomes
1. Radiological result at 6 weeks as determined by the
above reduction criteria.
2. A combined end-point of poor outcome, as defined by
either poor radiological result and/or progression to
surgery.
300
Patient recruitment for the study occurred from 1 April
2006 to 31 July 2008. Of the cases identified by the
computer-tagging system, 184 were Colles-type fractures that fit the study inclusion and exclusion criteria.
The mean age of the sample was 58.2 years (SD 19.6),
of which 82.1% were female.
Of the 184 patients included in the study, 8 were
referred directly to orthopaedics. The flow chart (Fig. 2)
explains the flow of patients throughout the study.
Within the 176 fractures manipulated by ED staff, only
5 were re-manipulated when reduction was deemed
unsatisfactory. Fifty-five (31.2%) were classified as
minimally displaced (dorsal angulation (DA) 15) and
121 (68.8%) classified as displaced (DA >15).
2009 The Authors
Journal compilation 2009 Australasian College for Emergency Medicine and Australasian Society for Emergency Medicine
Management of Colles-type fractures
Patients included in the study
N=184
Excluded (n= 8)
Referred directly to orthopaedics
Manipulated by ED staff (n=176)
Minimally displaced (n=55)
Displaced (n=121)
Allocation
Lost to follow up (n=7)
Lost to follow up (n= 7)
Underwent surgery before 6 week
follow up (n=4)
Underwent surgery before 6 week
follow up (n=29)
Follow up
Analysed (n= 44)
Analysed (n= 85)
6 week X-ray
Figure 2.
Patient flow.
Table 1.
Main outcomes
Minimally displaced
6 week follow-up X-ray (%)
Combined end-point (%)
P-value
Displaced
Good
Poor
Good
Poor
40 (91)
40 (83)
4 (9)
8 (17)
49 (58)
45 (40)
36 (42)
69 (61)
Of the patients who had 6 week follow-up X-rays,
40 of the 44 patients (90%) with minimally displaced on
arrival X-rays had satisfactory X-rays at 6 weeks, contrasted with 49 of 85 patients (58%) with displaced on
arrival X-rays. This represents an absolute difference of
33.3% (95% CI 2047%) (Table 1).
When using the combined end-point of patients who
went to theatre plus those with poor radiological
outcome, the two groups were further polarized. Forty
of the 48 patients (83%) in the minimally displaced
<0.001
<0.001
group now had a good outcome compared with 45 of 114
(39%) in the displaced group, an absolute difference of
44% (95% CI 3058%).
We evaluated the effect of reduction on 6 week X-ray
outcome in both minimally displaced and displaced
initial fractures. There is a significant difference in outcomes between the groups. Patients who had a minimally displaced fracture, with an adequate reduction
went on to have a satisfactory 6 week X-ray in 37 of
43 cases (86%; 95% CI 7696%). Patients who had a
2009 The Authors
Journal compilation 2009 Australasian College for Emergency Medicine and Australasian Society for Emergency Medicine
301
W Blakeney and L Webber
displaced fracture and an adequate reduction had a
satisfactory 6 week X-ray in 42 of 86 cases (49%; 95%
CI 3859%). Patients who had a displaced fracture and
an inadequate reduction had a satisfactory 6 week X-ray
in only 3 of 22 cases (14%; 95% CI 028%).
If we look only at the post-reduction X-ray and
compare this with the 6 week X-ray and combined
outcome (including patients who went to theatre), the
results were also significant. Seventy-nine of the 128
(61.7%) patients with adequate reduction had a good
outcome versus only 6 of the 25 with inadequate reduction (24%). Of the patients who had a 6 week X-ray,
83 of 111 (74.8%) with adequate reduction had a satisfactory appearance, whereas only 6 of the 18 (33%)
with inadequate reduction did (P < 0.001).
Within the minimally displaced group, 52 (95%) were
adequately reduced, compared with 97 (80%) in the
displaced group (P = 0.01). Alarmingly, 27 patients who
had inadequate reduction were discharged to orthopaedic follow up. Of the 55 patients in the minimally
displaced group, only 20 had a dorsal angle between
1015; that is, the other 35 would have satisfied the
criteria for adequacy of reduction before manipulation.
Discussion
Our results show that there is a significant difference in
outcomes between minimally displaced fractures and
displaced fractures. Of the patients with displaced fractures, 61% went on to have an operation and/or a poor
radiographic outcome versus 17% in the minimally displaced group, an absolute difference of 44% (95% CI
3058%). Removing the patients who went on to have
an operation, there was still a large difference. Ninety
point nine per cent of patients in the minimally displaced group had satisfactory radiographic outcome,
contrasted with 58% of patients in the displaced group,
an absolute difference of 33% (95% CI 2047%).
A minimally displaced fracture that is adequately
reduced will have a good outcome in 86% of cases (95%
CI 7697%). A displaced fracture with adequate reduction will have a good outcome in 49% of cases (95% CI
3859%). If, however, adequate reduction of a displaced
fracture is not achieved, a poor outcome is almost inevitable, with only 14% (95% CI 028%) having a satisfactory outcome.
The present study assumes that satisfactory 6 week
X-ray alignment equates with good functional outcome.
There have been many studies comparing follow-up
X-rays of Colles-type fractures with functional outcome
302
that support this. A 1951 study first noted that the
dorsal angle on the follow-up X-ray has the greatest
bearing on the eventual functional result.7 A study of
2000 Colles-type fractures in 1953 equated functional
loss with poor anatomical outcome.8 More recent studies
have all found a large dorsal angle, using the cut-off of
10, to be associated with poor functional outcome.912
There have also been studies that have failed to
demonstrate an association between good function and
radiographic outcome.13,14 These studies, however, have
been looking specifically at an elderly population. In an
elderly population, for numerous possible reasons, good
outcome is related to many other factors apart from
X-ray appearance. For this reason, we excluded anyone
over 85 years old. Our study populations demographics
compares favourably with the former studies in terms of
both mean age and sex proportions. We believe that it is
fair to conclude that the patients in our study with a
good radiographic result will go on to have good function. It would, however, be advantageous to follow up
the present study population with formal functional
assessment.
The results shows that minimally displaced fractures
are more likely to satisfy the reduction criteria. Many of
the minimally displaced fractures that were manipulated in ED, however, would have satisfied the criteria
for adequacy of reduction before manipulation. The
decision to manipulate was at the discretion of the treating ED medical officer, who presumably thought that a
better reduction was possible. Many post-reduction
X-rays were deemed acceptable by ED staff when in fact
they were not adequately reduced. Worryingly, only
five patients were re-manipulated in the ED whereas
27 were discharged to orthopaedic follow up without
having been adequately reduced. There were no guidelines for which fractures to manipulate and which to
accept. It has been demonstrated in a recent study that
many ED junior medical officers do not know how best
to assess displacement of Colles-type fractures.15 ED
registrars, residents and occasionally even interns were
the staff dealing with these fractures in the study. These
results stress the importance of either having guidelines
or simply educating ED junior medical officers on which
fractures to reduce, which reductions to accept and
which to refer.
The study highlights the importance of the initial on
arrival and post-reduction X-rays in the ED as predictors of outcome. Medical officers working in ED should
be aware of the importance of measuring the dorsal
angle. They should be referring patients with >15
dorsal angulation to orthopaedics early, as this group is
2009 The Authors
Journal compilation 2009 Australasian College for Emergency Medicine and Australasian Society for Emergency Medicine
Management of Colles-type fractures
5.
Hove LM, Solheim E, Skjeie R, Sorensen FK. Prediction of secondary displacement in Colles fracture. J. Hand Surg. 1994; 19B:
7316.
6.
Lafontaine M, Hardy D, Delince P. Stability assessment of distal
radius fractures. Injury 1989; 20: 20810.
Competing interests
7.
Gartland JJ, Werley CW. Evaluation of healed Colles fractures.
J. Bone Joint Surg. Am. 1951; 33: 895907.
None declared.
8.
Bacorn RW, Kurtzke JF. Colles fracture: a study of two thousand
cases from the New York state workmens compensation board.
J. Bone Joint Surg. Am. 1953; 35: 64358.
9.
Gliatis JD, Plessas SJ, Davis TRC. Outcome of distal radial fractures in young adults. J. Hand Surg. 2000; 25B: 53543.
more likely to have poor outcome. A good reduction is
still important though and should not be accepted if the
dorsal angle has not been adequately corrected.
Accepted 31 May 2009
10. McQueen M, Caspers J. Colles fracture: does the anatomical result
affect the final outcome? J. Bone Joint Surg. Br. 1988; 70: 64951.
References
1.
Sanders KM, Seeman E, Ugoni AM et al. Age- and genderspecific rate of fractures in Australia: a population based study.
Osteoporos. Int. 1999; 10: 2407.
2.
Thompson PW, Taylor J, Dawson A. The annual incidence and
seasonal variation of fractures of the distal radius in men and
women over 25 years in Dorset, UK. Injury 2004; 35: 4626.
3.
Mackenney PJ, McQueen MM, Elton R. Prediction of instability
in distal radial fractures. J. Bone Joint Surg. Am. 2006; 88: 1944
51.
4.
Jenkins NH. The unstable Colles fracture. J. Hand Surg. 1989;
14B: 14954.
11. Van Der Linden W, Ericson R. Colles fracture: how should its
displacement be measured and how should it be immobilised?
J. Bone Joint Surg. Am. 1981; 63: 12858.
12. Villar RN, Marsh D, Rushton N, Greatorex RA. Three years after
Colles fracture. J. Bone Joint Surg. Br. 1987; 69: 6358.
13. Anzarut A, Johnson JA, Rowe BH, Lambert RG, Blitz S, Majumdar SR. Radiologic and patient-reported functional outcomes in
an elderly cohort with conservatively treated distal radius fractures. J. Hand Surg. 2004; 29A: 11217.
14. Beumer A, McQueen MM. Fractures of the distal radius in lowdemand elderly patients. Acta Orthop. Scand. 2003; 74: 98100.
15. Batra S, McMutrie A, Batra M, Gul A, Kanvinde R. Distal radius
fracture management in the emergency departments in UK: are
we doing enough? Int. J. Clin. Pract. 2007; 61: 11316.
2009 The Authors
Journal compilation 2009 Australasian College for Emergency Medicine and Australasian Society for Emergency Medicine
303
You might also like
- VP - PSV SEA VEGA REV.0 (New Logo) r2Document4 pagesVP - PSV SEA VEGA REV.0 (New Logo) r2Sugiman LayantoNo ratings yet
- Mcq. SurgeryDocument132 pagesMcq. Surgeryمنتظر اللاميNo ratings yet
- Impulsivity 7Document3 pagesImpulsivity 7Joe Hodge100% (1)
- Jurnal Diagnostik ADocument8 pagesJurnal Diagnostik AImtina AhdaNo ratings yet
- Gyaneshwar Tonk-Anatomical and Functional EvaluationDocument11 pagesGyaneshwar Tonk-Anatomical and Functional EvaluationchinmayghaisasNo ratings yet
- Accepted Manuscript: Injury, Int. J. Care InjuredDocument16 pagesAccepted Manuscript: Injury, Int. J. Care InjuredDwi AryanataNo ratings yet
- Paper 4. Study of Intra-Articular Distal End Radius EJMCMDocument9 pagesPaper 4. Study of Intra-Articular Distal End Radius EJMCMNaveen SathyanNo ratings yet
- 223654-Article Text-546414-1-10-20220403Document6 pages223654-Article Text-546414-1-10-20220403Christopher Freddy Bermeo RiveraNo ratings yet
- Mcrae 2015Document8 pagesMcrae 2015Ananth BalakrishnanNo ratings yet
- Surgical Treatment of Chronic Elbow Dislocation Allowing For Early Range of Motion: Operative Technique and Clinical ResultsDocument8 pagesSurgical Treatment of Chronic Elbow Dislocation Allowing For Early Range of Motion: Operative Technique and Clinical ResultsLuis Carlos HernandezNo ratings yet
- Functional Outcome After The Conservative Management of A Fracture of The Distal HumerusDocument7 pagesFunctional Outcome After The Conservative Management of A Fracture of The Distal HumerusnireguiNo ratings yet
- Clearing The Cervical Spine of Adult Victims of TraumaDocument7 pagesClearing The Cervical Spine of Adult Victims of TraumaVince AzevoucheNo ratings yet
- Clinicoradiological and Functional Outcomes of Lisfranc Injuries Managed by Different Treatment Modalities in A Tertiary Care CentreDocument7 pagesClinicoradiological and Functional Outcomes of Lisfranc Injuries Managed by Different Treatment Modalities in A Tertiary Care CentreIJAR JOURNALNo ratings yet
- 08 Can We Safely Apply The Ottawa Ankle Rules To ChildrenDocument3 pages08 Can We Safely Apply The Ottawa Ankle Rules To ChildrenAlejandro Godoy SaidNo ratings yet
- 1547 5654 Article p80Document12 pages1547 5654 Article p80wilsonwqaNo ratings yet
- Semiconstrained Total Elbow Arthroplasty-1Document6 pagesSemiconstrained Total Elbow Arthroplasty-1Ευαγγελια ΚιμπαρηNo ratings yet
- Trauma Clinical Guideline 2017Document7 pagesTrauma Clinical Guideline 2017Paolo ContrerasNo ratings yet
- Modi Ed Percutaneous Kirschner Wire With Mutual Linking Technique in Proximal Humeral Fracture: A Technique Note and Preliminary ResultsDocument14 pagesModi Ed Percutaneous Kirschner Wire With Mutual Linking Technique in Proximal Humeral Fracture: A Technique Note and Preliminary ResultsRahul ReddyNo ratings yet
- 2023 JOT Radiological and Long Term Functional Outcomes of Displaced Distal Clavicle FracturesDocument7 pages2023 JOT Radiological and Long Term Functional Outcomes of Displaced Distal Clavicle FracturesjcmarecauxlNo ratings yet
- Closed Intra - Articular Fractures of The Distal End of Humerus Surgically Treated by Trans - Olecranon Approach Using The Chevron OsteotomyDocument4 pagesClosed Intra - Articular Fractures of The Distal End of Humerus Surgically Treated by Trans - Olecranon Approach Using The Chevron OsteotomyIJAR JOURNALNo ratings yet
- Circumferential Casting of Distal Radius PDFDocument5 pagesCircumferential Casting of Distal Radius PDFRajiv TanwarNo ratings yet
- Principles of Critical Care MedicineDocument4 pagesPrinciples of Critical Care MedicineKarthik SNo ratings yet
- Vol29 - No2 - 59 - 63Document5 pagesVol29 - No2 - 59 - 63Kagiso Gigfreak Urban RoccoNo ratings yet
- Journal ReadingDocument7 pagesJournal ReadingTommy HardiantoNo ratings yet
- Poster PapersDocument262 pagesPoster PapersLeonardo RodríguezNo ratings yet
- PLDD&MicrodiscectomyLeiden NL 2015Document9 pagesPLDD&MicrodiscectomyLeiden NL 2015YAŞAR TÜRKNo ratings yet
- A Randomized Controlled Trial of Nonoperative Treatment Versus Open Reduction and Internal Fixation For Stable, Displaced, Partial Articular Fractures of The Radial Head: The RAMBO TrialDocument5 pagesA Randomized Controlled Trial of Nonoperative Treatment Versus Open Reduction and Internal Fixation For Stable, Displaced, Partial Articular Fractures of The Radial Head: The RAMBO TrialAndi Urviana AsrahNo ratings yet
- The Effect of Ulnar Styloid Fractures On Patient-Reported Outcomes After Surgically Treated Distal Radial FracturesDocument7 pagesThe Effect of Ulnar Styloid Fractures On Patient-Reported Outcomes After Surgically Treated Distal Radial FracturesOpsonin PharmaNo ratings yet
- Sipola. Detection and Quantification of Rotator Cuff Tears With Ultrasonography and Magnetic Resonance Imaging - A ProsDocument9 pagesSipola. Detection and Quantification of Rotator Cuff Tears With Ultrasonography and Magnetic Resonance Imaging - A Prossteven saputraNo ratings yet
- American Journal of Emergency MedicineDocument5 pagesAmerican Journal of Emergency MedicineMaria teresa salinas merelloNo ratings yet
- 10 1016@j Jse 2019 10 013Document12 pages10 1016@j Jse 2019 10 013Gustavo BECERRA PERDOMONo ratings yet
- 16 Van Leerdam Et Al J Hand Surg Eur Vol. 2017 Jun 42 5 501 506 AAMDocument13 pages16 Van Leerdam Et Al J Hand Surg Eur Vol. 2017 Jun 42 5 501 506 AAMChristopher Freddy Bermeo RiveraNo ratings yet
- Lca TestDocument5 pagesLca Testkaren.heredia257No ratings yet
- To Evaluate The Functional Outcome of Volar Plating in Distal End Radius FracturesDocument11 pagesTo Evaluate The Functional Outcome of Volar Plating in Distal End Radius FracturesIJAR JOURNALNo ratings yet
- PDR Rsik Factors For RedisplacementDocument6 pagesPDR Rsik Factors For RedisplacementCleff FlowersNo ratings yet
- Definingnoptimal Calcar Screw Positioning in Proximal Humerus Fracture FixationDocument7 pagesDefiningnoptimal Calcar Screw Positioning in Proximal Humerus Fracture FixationAJ CésarNo ratings yet
- 4 03000605221103974Document13 pages4 03000605221103974Teuku FadhliNo ratings yet
- Jurnal Fraktur Humerus DistalDocument5 pagesJurnal Fraktur Humerus DistalthisisangieNo ratings yet
- Seguimiento A 5 Años PTGH ReversaDocument7 pagesSeguimiento A 5 Años PTGH Reversamarcelogascon.oNo ratings yet
- Primary Total Shoulder Arthroplasty Performed Entirely Thru The Rotator Interval - Technique and Minimum Two-Year OutcomesDocument10 pagesPrimary Total Shoulder Arthroplasty Performed Entirely Thru The Rotator Interval - Technique and Minimum Two-Year OutcomesmotohumeresNo ratings yet
- Tan2012 PDFDocument10 pagesTan2012 PDFdebyanditaNo ratings yet
- 1 s2.0 S0303846708002114 MainDocument5 pages1 s2.0 S0303846708002114 MainFNo ratings yet
- Lumbal Spinal Stenosis ODI ScoreDocument10 pagesLumbal Spinal Stenosis ODI ScoreTusan SidhartaNo ratings yet
- 17.PLDD Vs Surgery RCTDocument9 pages17.PLDD Vs Surgery RCTBeata SviantickaNo ratings yet
- Percutaneaus Kirschner-Wire Fixation For Displaced Distal Forearm Fractures in ChildrenDocument5 pagesPercutaneaus Kirschner-Wire Fixation For Displaced Distal Forearm Fractures in ChildrennaluphmickeyNo ratings yet
- Open FractureDocument16 pagesOpen FractureMazvita Maz MatipiraNo ratings yet
- Cervical Spine Clearance 2009Document7 pagesCervical Spine Clearance 2009Abdulelah Al.luhaybiNo ratings yet
- Bryan MorreyDocument5 pagesBryan MorreyokisutartoNo ratings yet
- Two Casting Methods Compared in Patients With Colles' Fracture: A Pragmatic, Randomized Controlled TrialDocument12 pagesTwo Casting Methods Compared in Patients With Colles' Fracture: A Pragmatic, Randomized Controlled TrialTeja Laksana NukanaNo ratings yet
- The Clinical Outcome After Extra-Articular Colles Fractures With Simultaneous Moderate Scapholunate DissociationDocument5 pagesThe Clinical Outcome After Extra-Articular Colles Fractures With Simultaneous Moderate Scapholunate DissociationYina Marcela Quintero OrtegaNo ratings yet
- Paper Section 3 Draft1Document11 pagesPaper Section 3 Draft1api-568855135No ratings yet
- Abstracts - Final Off Print BJNDocument57 pagesAbstracts - Final Off Print BJNZieshNo ratings yet
- Open Reduction and Internal Fixation ORIF of ComplDocument6 pagesOpen Reduction and Internal Fixation ORIF of ComplAnnisa AnggrainiNo ratings yet
- Ditkofsky 2015Document28 pagesDitkofsky 2015Allython Jureth Peña ReyesNo ratings yet
- Cast Immobilisation With and Without Immobilisation of The Thumbfor Non-Displaced Scaphoid FracturesDocument7 pagesCast Immobilisation With and Without Immobilisation of The Thumbfor Non-Displaced Scaphoid FracturesmonkeyzergNo ratings yet
- HTTPS://WWW Mendeley Com/reference-Manager/readerDocument6 pagesHTTPS://WWW Mendeley Com/reference-Manager/readerIJAR JOURNALNo ratings yet
- Long Term Outcome of Isolated DiaphysealDocument5 pagesLong Term Outcome of Isolated DiaphysealVIDevAryanNo ratings yet
- Preoperative Close Reduction of Cervical Fracture DislocationsDocument8 pagesPreoperative Close Reduction of Cervical Fracture DislocationsIJAR JOURNALNo ratings yet
- Use of Surgical Augmented Intelligence Maps Can ReDocument11 pagesUse of Surgical Augmented Intelligence Maps Can Resebasags19No ratings yet
- A Randomized Controlled Trial of Endovascular Aneurysm Repair Versus Open Surgery For Abdominal Aortic Aneurysms in Low - To Moderate-Risk PatientsDocument8 pagesA Randomized Controlled Trial of Endovascular Aneurysm Repair Versus Open Surgery For Abdominal Aortic Aneurysms in Low - To Moderate-Risk Patientsvfd08051996No ratings yet
- Distal Femur Fractures Fixation by Locking Compression Plate-Assessment of Outcome by Rasmussens Functional Knee ScoreDocument7 pagesDistal Femur Fractures Fixation by Locking Compression Plate-Assessment of Outcome by Rasmussens Functional Knee ScoreIJAR JOURNALNo ratings yet
- Hip Dislocation Are Hip Precautions Necessary in Anterior ApproachesDocument6 pagesHip Dislocation Are Hip Precautions Necessary in Anterior Approaches阿欧有怪兽No ratings yet
- Target Volume Delineation for Pediatric CancersFrom EverandTarget Volume Delineation for Pediatric CancersStephanie A. TerezakisNo ratings yet
- ScopeDocument3 pagesScopeGalano, Hana MarieNo ratings yet
- Reading b2 c1Document4 pagesReading b2 c1Karenza ThomasNo ratings yet
- Company Profile Kalgen Innolab Innobiogram - 2022Document12 pagesCompany Profile Kalgen Innolab Innobiogram - 2022asmadi arrumNo ratings yet
- The English Opening: Grandmaster Repertoire 3Document10 pagesThe English Opening: Grandmaster Repertoire 3lietotajs71No ratings yet
- Building Construction Company ProfileDocument62 pagesBuilding Construction Company ProfileFadhlan Dwi Gusti WarmanNo ratings yet
- Design Princples For Wood Burning Cook StovesDocument20 pagesDesign Princples For Wood Burning Cook Stoveshana temesegenNo ratings yet
- Unit 5. PHCDocument24 pagesUnit 5. PHCFenembar MekonnenNo ratings yet
- 1000 English Collocations EbookDocument128 pages1000 English Collocations EbookHerdeiro DicaprioNo ratings yet
- Pamphlet 21 (NCl3)Document210 pagesPamphlet 21 (NCl3)victorNo ratings yet
- Symbols: First LetterDocument2 pagesSymbols: First LetterFIDAH FYSALNo ratings yet
- The Following Is An Excerpt FromDocument12 pagesThe Following Is An Excerpt FromViktoria MolnarNo ratings yet
- Desoldering Tool: Designed For Lead FreeDocument2 pagesDesoldering Tool: Designed For Lead FreeMarco Antonio Ortiz RomeroNo ratings yet
- Suzumar Boat Engine PackagesDocument7 pagesSuzumar Boat Engine PackagesmarkoNo ratings yet
- PM Handbook (Full PDFDocument88 pagesPM Handbook (Full PDFGary LoNo ratings yet
- Hypogear 80W-90 - BP Australia Pty LTDDocument5 pagesHypogear 80W-90 - BP Australia Pty LTDBiju_PottayilNo ratings yet
- Process, People, and Conflict Management in OrganizationsDocument6 pagesProcess, People, and Conflict Management in OrganizationsMeldy IamNo ratings yet
- NIM: 2440007043 Nama: Ni Putu Young Yenyuo A Mata Kuliah: Accounting For Business Dosen: Herlin Tundjung SetijaningsihDocument5 pagesNIM: 2440007043 Nama: Ni Putu Young Yenyuo A Mata Kuliah: Accounting For Business Dosen: Herlin Tundjung SetijaningsihiyeNo ratings yet
- CED-PQP-5225-F01 Rev.0 Sieve AnalysisDocument4 pagesCED-PQP-5225-F01 Rev.0 Sieve AnalysisSslan seelanNo ratings yet
- Wallmat Supply Chain Analysis PDFDocument44 pagesWallmat Supply Chain Analysis PDFProsenjit RoyNo ratings yet
- NYJC Prelim 2006 P2Document12 pagesNYJC Prelim 2006 P2miiewNo ratings yet
- Topic 5 AC To AC ConverterDocument53 pagesTopic 5 AC To AC ConverterNorain ZakariaNo ratings yet
- PCB Design Techniques To Reduce EMIDocument21 pagesPCB Design Techniques To Reduce EMIelfrichNo ratings yet
- Hyva Oil Tank: Single Support Tank Double Support TankDocument4 pagesHyva Oil Tank: Single Support Tank Double Support TankPutera Bumi NusantaraNo ratings yet
- P I Iso TP M v13 enDocument6 pagesP I Iso TP M v13 enPedro SepúlvedaNo ratings yet
- Heridity: Table of SpecificationsDocument8 pagesHeridity: Table of SpecificationsJoseph GratilNo ratings yet
- Lec5 - Geotechnical Investigation Reports and Foundation Recommendations-Scope For Improvement-ExamplesDocument20 pagesLec5 - Geotechnical Investigation Reports and Foundation Recommendations-Scope For Improvement-ExamplesrohitNo ratings yet
- Demonizing Drugmakers: The Political Assault On The Pharmaceutical Industry, Cato Policy Analysis No. 475Document56 pagesDemonizing Drugmakers: The Political Assault On The Pharmaceutical Industry, Cato Policy Analysis No. 475Cato InstituteNo ratings yet