Professional Documents
Culture Documents
Letters To The Editor: Posture Technique
Letters To The Editor: Posture Technique
Uploaded by
Muizzudin AzzaCopyright:
Available Formats
You might also like
- Complete Denture Evaluation DCNADocument17 pagesComplete Denture Evaluation DCNAAravind Krishnan80% (15)
- 2017-Craniofacial DistractionDocument234 pages2017-Craniofacial DistractionMarisol Gallego DuqueNo ratings yet
- Detailed Case History in C - DDocument54 pagesDetailed Case History in C - Dvahini niharika100% (8)
- Diagnostic Criteria Examination Form PDFDocument2 pagesDiagnostic Criteria Examination Form PDFNor Nadia Zakaria50% (2)
- Head & Neck Part 2Document29 pagesHead & Neck Part 2_str8cashhomie100% (1)
- The Arthritis Cure: The Medical Miracle That Can Halt, Reverse, And May Even Cure OsteoarthritisFrom EverandThe Arthritis Cure: The Medical Miracle That Can Halt, Reverse, And May Even Cure OsteoarthritisNo ratings yet
- Section 007 Articulators IDocument17 pagesSection 007 Articulators IAllen SharonNo ratings yet
- Complications of ExodontiaDocument33 pagesComplications of ExodontiaSunil Tiwari100% (1)
- Anatomi Dan Fisiologi TMJ Serta Pergerakan MandibulaDocument28 pagesAnatomi Dan Fisiologi TMJ Serta Pergerakan MandibulaAyu AnggayantiNo ratings yet
- Determinants of OcclusionDocument67 pagesDeterminants of Occlusiondrsmriti100% (4)
- Log of Literature DhiiDocument10 pagesLog of Literature Dhiiapi-733637938No ratings yet
- 0022 3913 (65) 90060 0Document14 pages0022 3913 (65) 90060 0barrera2001No ratings yet
- BioesteticaDocument8 pagesBioesteticasuareztepperNo ratings yet
- Increasing Occlusal Vertical Dimension - Why When and HowDocument6 pagesIncreasing Occlusal Vertical Dimension - Why When and HowLow Junfay MarkNo ratings yet
- Study Guide - Treatment of Edentulous PatientsDocument107 pagesStudy Guide - Treatment of Edentulous PatientsTosca Mavourneen100% (1)
- Problem in Complete Denture Treatment and Postinsertion DentureDocument35 pagesProblem in Complete Denture Treatment and Postinsertion DentureSorabh JainNo ratings yet
- Color Coding Second DraftDocument8 pagesColor Coding Second Draftapi-271242958No ratings yet
- Introduction To Orthotropics HandbookDocument15 pagesIntroduction To Orthotropics HandbookVio Prico100% (1)
- Why-When-How - To Increase Ovd PDFDocument6 pagesWhy-When-How - To Increase Ovd PDFFaheemuddin MuhammadNo ratings yet
- Limb Lengthening SurgeryDocument12 pagesLimb Lengthening Surgerypav20021No ratings yet
- Priyanka Arien Dr.Document5 pagesPriyanka Arien Dr.barcimNo ratings yet
- Ebpp Julie WalkerDocument6 pagesEbpp Julie Walkerapi-240603006No ratings yet
- Adult OrthodonticsDocument70 pagesAdult OrthodonticsTruppti SononeNo ratings yet
- 1retention and RelapseDocument12 pages1retention and RelapseTara TeraNo ratings yet
- Clubfoot ThesisDocument7 pagesClubfoot ThesisCollegePaperGhostWriterAkron100% (2)
- High Angle Cases-ManagementDocument11 pagesHigh Angle Cases-ManagementAmir IqbalNo ratings yet
- The Inverted Orthotic Technique: A Process of Foot Stabilization for Pronated FeetFrom EverandThe Inverted Orthotic Technique: A Process of Foot Stabilization for Pronated FeetNo ratings yet
- The Journey From The Past To The FutureDocument2 pagesThe Journey From The Past To The FutureplsssssNo ratings yet
- NotesDocument639 pagesNotesAmar Bhochhibhoya100% (1)
- Document 20220530145543Document15 pagesDocument 20220530145543Omar GadNo ratings yet
- Sit Stand BookDocument11 pagesSit Stand BookAditya Widya Pranata100% (1)
- Ergonomics Solutions in Dental PracticeDocument6 pagesErgonomics Solutions in Dental Practicecursoenao10No ratings yet
- Thesis OsteopathyDocument6 pagesThesis Osteopathygbv8rcfq100% (1)
- Dental Clinics of North America Sleep Medicine in Dentistry Xi XiiiDocument3 pagesDental Clinics of North America Sleep Medicine in Dentistry Xi XiiiKranti PrajapatiNo ratings yet
- Final File 5d79d83f30ce45.26319674Document6 pagesFinal File 5d79d83f30ce45.26319674Maulida Dara HarjantiNo ratings yet
- Posturodontics in Dentistry A Review PDFDocument4 pagesPosturodontics in Dentistry A Review PDFChaithra ShreeNo ratings yet
- Ear StaplingDocument4 pagesEar StaplingtennebNo ratings yet
- Total Hip Replacement: An Evidence-Based Approach Your Guide From Pre-op Through RecoveryFrom EverandTotal Hip Replacement: An Evidence-Based Approach Your Guide From Pre-op Through RecoveryRating: 5 out of 5 stars5/5 (1)
- One Step Ahead of Osteoarthritis: Stay Flexible and Keep MovingFrom EverandOne Step Ahead of Osteoarthritis: Stay Flexible and Keep MovingNo ratings yet
- JCO - Interviews Dr. Bjorn U. ZaDocument18 pagesJCO - Interviews Dr. Bjorn U. ZaAhmad KhalifaNo ratings yet
- Of Fice Procedures For The Oral and Maxillofacial Surgeon: PrefaceDocument2 pagesOf Fice Procedures For The Oral and Maxillofacial Surgeon: PrefacedrescobedocomfNo ratings yet
- Practical Points in Making Complete Dentures Suction Effective and FunctionalDocument46 pagesPractical Points in Making Complete Dentures Suction Effective and FunctionalCostin SilviuNo ratings yet
- Practice Station Explain Osteoporosis1Document6 pagesPractice Station Explain Osteoporosis1Wenbin GuoNo ratings yet
- 2Document4 pages2Anonymous hWVtGzmZNo ratings yet
- The Young Professions Australia Roundtable 2003 Achieving A Sustainable Future A Dental PerspectiveDocument7 pagesThe Young Professions Australia Roundtable 2003 Achieving A Sustainable Future A Dental PerspectiveAhmed GendiaNo ratings yet
- Sassouni AnalisisDocument2 pagesSassouni Analisisナスティオン ファジャルNo ratings yet
- Occlusal Dysesthesia or Phantom BiteDocument14 pagesOcclusal Dysesthesia or Phantom BitebryanabauerNo ratings yet
- Nutrition and The Teeth For Patients Receiving Radiotherapy To The Head and NeckDocument19 pagesNutrition and The Teeth For Patients Receiving Radiotherapy To The Head and NeckFadhlan Indra SNo ratings yet
- Ass A I Gnment For Data AnalysisDocument10 pagesAss A I Gnment For Data AnalysisFaisol NipunNo ratings yet
- Asynchronous Activity: What Does Good Posture Look Like?Document10 pagesAsynchronous Activity: What Does Good Posture Look Like?Claire Julianne CapatiNo ratings yet
- ErgonomicsDocument4 pagesErgonomicsSubhashini RajshekarNo ratings yet
- Orthodontic Treatment Planning: Problem List To Specific PlanDocument49 pagesOrthodontic Treatment Planning: Problem List To Specific PlanYusra AqeelNo ratings yet
- 1009cei Ortho WebDocument12 pages1009cei Ortho WebAshraf ShehataNo ratings yet
- Whiplash Injury Recovery Booklet - 2nd Edition PDFDocument21 pagesWhiplash Injury Recovery Booklet - 2nd Edition PDFshivani04No ratings yet
- Thesis Statement For Oral HygieneDocument5 pagesThesis Statement For Oral HygienePaySomeoneToWriteAPaperForMeFargo100% (1)
- The Effect of Obesity On The Outcome of Total Knee Arthroplasties in Arthritic PatientsDocument20 pagesThe Effect of Obesity On The Outcome of Total Knee Arthroplasties in Arthritic Patientsapi-379927920No ratings yet
- Cerebral Palsy Research PaperDocument7 pagesCerebral Palsy Research Paperapi-663723303No ratings yet
- Retention and Relapse 3Document13 pagesRetention and Relapse 3Tara TeraNo ratings yet
- A Study To Assess The Effectiveness of Hot and Cold Application On Arthritic Pain and Mobility Status Among Clients With Osteoarthritis in Selected Hospitals at Kolar District.Document31 pagesA Study To Assess The Effectiveness of Hot and Cold Application On Arthritic Pain and Mobility Status Among Clients With Osteoarthritis in Selected Hospitals at Kolar District.Lambert Winston67% (6)
- Reduce Dental AnxietyDocument10 pagesReduce Dental AnxietySung Soon ChangNo ratings yet
- Jaw Surgery: Everything You Need To KnowDocument24 pagesJaw Surgery: Everything You Need To KnowAdrian Stan100% (1)
- OM TherapyDocument8 pagesOM TherapyGiePramaNo ratings yet
- Orthopaedics PunchDocument6 pagesOrthopaedics PunchHicham GawishNo ratings yet
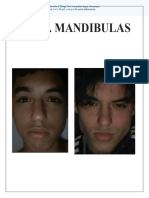
- Mr. Mandibulas: Subscribe To Deepl Pro To Translate Larger Documents. Visit For More InformationDocument87 pagesMr. Mandibulas: Subscribe To Deepl Pro To Translate Larger Documents. Visit For More Informationav495600No ratings yet
- A Parents Guide To Treatment For Development Dysplasia of The HipDocument16 pagesA Parents Guide To Treatment For Development Dysplasia of The HipSunny Gabriels100% (1)
- The Effectiveness of Using Two Stay Two Stray and Numbered Head Together in Teaching Writing Narrative TextDocument1 pageThe Effectiveness of Using Two Stay Two Stray and Numbered Head Together in Teaching Writing Narrative TextMuizzudin AzzaNo ratings yet
- Nursing Department Program Faculty of Nursing and Health University of Muhammadiyah SemarangDocument1 pageNursing Department Program Faculty of Nursing and Health University of Muhammadiyah SemarangMuizzudin AzzaNo ratings yet
- Chewing MasticationDocument6 pagesChewing MasticationMuizzudin AzzaNo ratings yet
- Reinforcement Technique and Variable y in This Study Is Students' Learning Motivation. DataDocument1 pageReinforcement Technique and Variable y in This Study Is Students' Learning Motivation. DataMuizzudin AzzaNo ratings yet
- The Role of Shoe Design in Ankle Sprain Rates Among Collegiate Basketball PlayersDocument4 pagesThe Role of Shoe Design in Ankle Sprain Rates Among Collegiate Basketball PlayersMuizzudin AzzaNo ratings yet
- David Renz Defense Federal Sentencing MemorandumDocument13 pagesDavid Renz Defense Federal Sentencing MemorandumAmanda JordanNo ratings yet
- Occlusion / Orthodontic Courses by Indian Dental AcademyDocument90 pagesOcclusion / Orthodontic Courses by Indian Dental Academyindian dental academyNo ratings yet
- TMJ AnatomyDocument39 pagesTMJ AnatomyPravallika ManneNo ratings yet
- TMJ ImanDocument46 pagesTMJ Imanimaniyas imanNo ratings yet
- Examination & Diagnosis of Edentulous Patients: Presented By: Dr. Jehan Dordi 1 Yr. MdsDocument159 pagesExamination & Diagnosis of Edentulous Patients: Presented By: Dr. Jehan Dordi 1 Yr. MdsAkanksha MahajanNo ratings yet
- Temporomandibular Joint: DR Bhaumik Thakkar MDS-Part 1. Dept. of Periodontology and ImplantologyDocument60 pagesTemporomandibular Joint: DR Bhaumik Thakkar MDS-Part 1. Dept. of Periodontology and ImplantologyJoseph Eduardo Villar CordovaNo ratings yet
- TrismusDocument9 pagesTrismusJoão de BarrosNo ratings yet
- Ginglymoarthrodial JointDocument5 pagesGinglymoarthrodial JointŽäíñäb ÄljaÑabìNo ratings yet
- Muscles of MasticationDocument27 pagesMuscles of MasticationNanditha Swaroop100% (3)
- Lips Together and Teeth Apart: John T. Mahoney, D.D.S. Family DentistryDocument6 pagesLips Together and Teeth Apart: John T. Mahoney, D.D.S. Family DentistryZoran KosecNo ratings yet
- Airway Centric TMJ Airway Centric TMJDocument13 pagesAirway Centric TMJ Airway Centric TMJBeatrix Rednik100% (1)
- Hinge Axis: Presenter B.Alekhya Iiyrpg Moderator Dr. KamalDocument80 pagesHinge Axis: Presenter B.Alekhya Iiyrpg Moderator Dr. Kamalbharathi krishnaNo ratings yet
- Functional Anatomy of Temporomandibular JointDocument44 pagesFunctional Anatomy of Temporomandibular JointRomzi Hanif0% (1)
- TMJ DisordersDocument20 pagesTMJ DisordersErisa BllakajNo ratings yet
- Muscles of MasticationDocument106 pagesMuscles of MasticationShivam SharmaNo ratings yet
- Ferula de MichiganDocument11 pagesFerula de MichiganFernando Espada SalgadoNo ratings yet
- Evaluation of Temporomandibular Joint Spaces and Condylar Position - A CBCT StudyDocument6 pagesEvaluation of Temporomandibular Joint Spaces and Condylar Position - A CBCT StudyDr Yamuna Rani100% (1)
- SATO Dental Asymmetry - TMDDocument5 pagesSATO Dental Asymmetry - TMDJorge Mori VelásquezNo ratings yet
- Icd-10 Codes For Orthodontics: Introduction - Kirt E. Simmons, DDS, PHDDocument10 pagesIcd-10 Codes For Orthodontics: Introduction - Kirt E. Simmons, DDS, PHDmsk adiwiryaNo ratings yet
- Trauma Q&ADocument8 pagesTrauma Q&ANoor MaxeemNo ratings yet
- ASDA Released Papers L-MDocument46 pagesASDA Released Papers L-MZuhair Waheed100% (2)
- Temporo-Mandibular Joint Complex Exercise SuggestionsDocument9 pagesTemporo-Mandibular Joint Complex Exercise SuggestionsClaudia LeperaNo ratings yet
- Oral Surgery FlashCardsDocument63 pagesOral Surgery FlashCardsMihika MahandwanNo ratings yet
Letters To The Editor: Posture Technique
Letters To The Editor: Posture Technique
Uploaded by
Muizzudin AzzaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Letters To The Editor: Posture Technique
Letters To The Editor: Posture Technique
Uploaded by
Muizzudin AzzaCopyright:
Available Formats
Letters to the Editor
LETTERS
Send your letters to the Editor,
British Dental Journal,
64 Wimpole Street,
London
W1G 8YS
E-mail bdj@bda.org
Priority will be given to letters less
than 500 words long.
Authors must sign the letter, which
may be edited for reasons of space.
POSTURE TECHNIQUE
Sir, I compliment A. Gandavani et al.
(BDJ 2007; 203: 601-605) for highlight
ing the importance of correct posture in
preventing back pain. I am concerned
about some aspects of the study.
For example Figures 3 and 4 are not
truly comparable. The student in Figure
3 on the BSS has the patients head at
the correct working height (as shown by
her upward-sloping forearms). However,
the one on the CS in Figure 4 has the
patients head far too low; his stool is
not high enough (so producing the 90
degree exion of knees and hips rightly
condemned in the article); his stool seat
slopes down backwards and the stool
back is tilted so far back as to make it
useless. Little wonder he is in such dis
torted posture.
Any one of these errors would produce
the kyphosis and slumping referred to in
the study. Combined in one dentist they
are a disaster.
On the other hand I can guarantee
that if this students stool was raised to a
correct height and its seat tilted slightly
forward, this would produce the correct
knee and femur/trunk angles of more
than 90 degrees. The dental chair should
then be raised to place the patients
mouth at the correct height at the stu
dents mid-sternal level. Finally if the
stool back rest were brought forward
into rm contact with his lower back to
reciprocate his lumbar lordosis, his pos
ture would be as good as the student on
the BSS. No equipment will work if not
used correctly!
Excellent though this study is one
must also look at stools in a general
practice context.
In my experience there are some dis
advantages of the BSS:
BRITISH DENTAL JOURNAL VOLUME 204 NO. 4 FEB 23 2008
1. Sitting for long periods with the
thighs widely splayed seems to
put pressure on the hip joints.
I have met two dentists recently
who have had to cease using a
BSS due to hip pain
2. This thigh splay prevents the nurse
from sitting close enough to the
patient forcing her to lean over both
forwards and sideways (nurses also
have backs)
3. Some dental chairs do not go high
enough to put the mouth at a den
tists focal distance causing him or
her to overex
4. Nurses cannot sit high enough
when the dentist sits at the
height required by a BSS. Many
have to stand.
In conclusion even the most perfect
stool will not be totally effective if all
the other techniques needed to work in
perfect posture are not applied.
E. Paul
By email
Dr Amar Gandavani responds: We wish
to thank Dr Paul for his interest and
for his positive and helpful comments.
In response to his comment about g
ures: the students were initially trained
in properly adjusting and using their
respective seats (Bambach Seat [BS] and
Conventional Seat [CS]) with the correct
operating posture before the commence
ment of the study. The students using the
BS developed healthy posture, whereas
the students using the CS developed a
less ideal posture.
Regarding CS producing 90 degree
exion of the knees: Mandal (1984) has
clearly identied that using a CS keeps
the knees in 90 degree exion, the pelvis
2008 Nature Publishing Group
is tilted posteriorly, and the body is tilted
away from the work surface, which is
compensated by increasing the exion of
the lumbar spine (slumped sitting). This
posture was frequently observed in the
study and we consider this to be a prin
cipal contributory factor to the result
ant musculoskeletal problems reported
by the dental community in this and
previous studies.
Regarding Dr Pauls comment about the
positioning of the back rest: we consider
that the back rest may not be an impor
tant factor inuencing posture in this
study. In the observation of 21 dentists
across the West Midlands and around
200 students in the School of Dentistry
University of Birmingham, all using
a CS, none of them were actively using
their back rests while treating patients.
The BS used in this study does not have
a back rest; however, the design is such
that it promotes good posture.
In response to the comment about sit
ting with thighs widely splayed on the BS:
the BS allows the hips to fall into a sup
ported abducted position and the angle
adopted by each user will vary slightly,
but will be within the normal range of
movement. This position is encouraged
for increasing the blood supply to the
head of the femur and for maintaining
the length of the piriformis muscle. Sit
ting with slight abduction and external
rotation of the hips is a natural position
and seen as the position adopted by many
when sitting.
Finally in response to the comment
about seat height: we agree that seat
height is an important factor inuencing
the working posture. Dr Paul has sug
gested that the CS has to be high enough
for a dentist to put the mouth in his/her
focal distance. The BS, like conventional
169
LETTERS
seats, may readily be adjusted to the
correct height, but the dental chair also
needs to be adjusted relative to the den
tal seat height in order to obtain optimal
vision of the tooth being operated on.
This lack of sufcient raise may occur
in a minority of older chairs but was not
seen in this study.
We again thank Dr Paul for his com
ments regarding this article.
DOI: 10.1038/bdj.2008.110
of the FSAs 8 tips for eating well, and
so should be kept in mind by health professionals. If dental care professionals
remain in any doubt about what to say
to their patients in the surgery, Deliver
ing better oral health3 recommends that
everyone is advised to reduce the fre
quency and amount of sugary foods and
drinks consumed.
C. Stillman-Lowe
Independent Oral Health Promotion Adviser
SWEET NOTHINGS
1.
Sir, I must take issue with R. Cottrells
letter on sugar and health (BDJ 2007;
203: 560-561). He is incorrect to refer to
the review of evidence of effectiveness
of oral health promotion methods by
Professor Liz Kay for the Health Devel
opment Agency, which he then refer
ences to an article in the BDJ. The report,
published in 1997,1 was in fact commis
sioned by the Health Education Author
ity and was co-authored by Dr Elizabeth
Kay and Professor David Locker. Both Dr
Richard Watt and I wrote commentaries.
The exact statement that the book con
tains on sugar (in the executive sum
mary) runs as follows:
Attempts to control individuals con
sumption of sweet foods and drinks
are generally not satisfactorily evalu
ated. However, when such interventions
are directed towards individuals, they
appear to be of limited value.
The authors conclude that the most
cost-effective means of delivering u
oride to the population should be the
method of choice for promoting oral
health through caries reduction.
However, looking at the broader issue
of food and health today, the advice of
the Food Standards Agency (FSA) is to
cut down on sugar: 2
Most people in the UK are eating too
much sugar. We should all be trying to eat
fewer foods containing added sugar, such
as sweets, cakes and biscuits, and drink
ing fewer sugary soft and zzy drinks.
Having sugary foods and drinks too
often can cause tooth decay, especially
if you have them between meals. Many
foods that contain added sugar can also
be high in calories so cutting down could
help you control your weight.
Irrespective of whether this advice is
endorsed by the Sugar Bureau, it is part
170
2.
3.
Kay E J, Locker D. Effectiveness of oral health
promotion: a review. London: Health Education
Authority, 1997.
http://www.eatwell.gov.uk/healthydiet/
eighttipssection/8tips/
Department of Health and the British Association
for the Study of Community Dentistry. Delivering
better oral health: an evidence-based toolkit for
prevention. London: Department of Health, 2007.
DOI: 10.1038/bdj.2008.111
TMJ DISLOCATION
Sir, we would like to report a case
of temporomandibular joint (TMJ)
dislocation which occurred during
administration of an inferior alveolar
nerve block.
A 28-year-old male patient was being
administered inferior alveolar nerve
block by his dentist for a class II lling
in the 36, when the patient felt a click
in the right TMJ, with associated pain
and inability to close his mouth. A diag
nosis of unilateral TMJ dislocation was
made, however, no attempt was made to
reduce the dislocation and the patient
was referred to the Accident and Emer
gency department.
The dislocation was spontaneous. The
patient did not have any previous his
tory of clicking, subluxation, trauma or
dislocation of the TMJ.
An orthopantogram was performed
(Fig. 1) and the patient was referred on
to the maxillofacial team. Clinical his
tory and examination was not sugges
tive of connective tissue disorders like
Ehler danlos or Marfans syndrome.
Fig. 1 Dislocated right condyle
2008 Nature Publishing Group
The patient was in considerable pain.
There was a palpable deformity and the
TMJ was low on the same side.
Two millilitres of local anaesthetic
was inltrated around the right TMJ
and the dislocation was reduced with
considerable effort using a combined
intraoral and extra oral technique. No
sedation was required. The patient was
advised not to open his mouth wide and
to support his jaw. He was subsequently
discharged with an analgesic prescrip
tion and warned about further risk
of dislocations.
Non-traumatic dislocations of the TMJ
occur most commonly while yawning,
eating, dental treatment, endoscopy1
and oral intubation.2 Most dental treat
ments require the patient to open his or
her mouth wide for a long period of time,
which makes it likely for the dislocation
to occur in the dental surgery. The risk
of dislocation can be minimised by ask
ing the patient to bite on a mouth prop
and ensuring adequate rest during pro
longed treatment.
In this particular patient, four hours
had elapsed since the dislocation dur
ing which time the patient had been in
a lot of discomfort. Spasm of the mas
seter and pterygoid muscles worsens as
time progresses, rendering reduction
difcult. In addition, complications of
reduction such as fracture of the con
dyle and the articular eminence are rare
if reduction is achieved early using the
correct techniques.
All the tools that are required to
reduce a non-traumatic dislocation
which occurs in the dental surgery are
within easy reach of a general dental
practitioners ie local anaesthetic, pano
rex and if necessary sedation. It is far
easier to relocate it immediately and the
morbidity is much reduced if the dislo
cation is reduced as soon as possible. If
needed, the patient may then be referred
on to a maxillofacial unit.
Reduction of dislocated TMJ is being
taught as a mandatory skill for phy
sicians working in the emergency
department. During dental school, the
theoretical management of TMJ disloca
tion is covered in the curriculum. How
ever, no attempt is made to train using
mannequins or simulators to teach prac
tical skills at reduction.
BRITISH DENTAL JOURNAL VOLUME 204 NO. 4 FEB 23 2008
We would like to emphasise the need
to include teaching practical techniques
in undergraduate dental education.
M. A. Nusrath, J. R. Adams, D. R. Farr,
D. G. Bryant
Middlesbrough
1.
2.
Mangi Q, Ridgway P F, Ibrahim Z, Evoy D.
Dislocation of the mandible. Surg Endosc 2004;
18: 554-556.
Ting J. Temporomandibular joint dislocation after
use of a laryngeal mask airway. Anaesthesia 2006;
61: 201.
DOI: 10.1038/bdj.2008.112
RIGA-FEDE DISEASE
Sir, we would like to report an unusual
case of sublingual and ventral tongue
ulceration, which was present for two
weeks, in a six-week-old female Cau
casian baby. The mother was concerned
about her babys intraoral discomfort
and difculty with feeding. Examination
revealed a distressed baby with a lower
right mandibular tooth of whitish colour
and shape resembling a primary incisor,
with grade II mobility. The tongue was
slightly raised at rest with an 8 x 10 mm
indurated and tender ulcer on the ven
tral surface/oor of the mouth extend
ing from the tip to the lingual fraenum
(Fig. 1). The medical history was clear.
As the tooth was the suspected cause of
the ulceration and pain it was extracted
and this was completed using topical
anaesthetic. On review ten days later,
examination revealed complete healing
of the ulcer and the extraction socket.
The baby appeared to be much more
content and the mother reported that her
baby was feeding normally.
Ulceration of the ventral surface of the
tongue in newborn babies or infants is
most commonly related to natal or neo
natal teeth, as illustrated in this case.1,2
We believe this particular type of ulcer
ation to be a case of Riga-Fede disease; 3
this was initially described by Riga in
1881 and Fede in 1890 4 and has been
reported since, but not widely in the
British literature. Typically, the benign
lesion begins as an ulcerated area on the
ventral surface of the tongue exposed
to repeated trauma from a natal tooth.2
It may progress to an enlarged brous
mass and has appearances that have
been described as those of a traumatic
BRITISH DENTAL JOURNAL VOLUME 204 NO. 4 FEB 23 2008
Fig. 1 Ulcer on the ventral surface/oor of
the mouth
ulcerative granuloma (with stromal
eosinophilia) 5 (Fig. 1). Such ulceration
can also be seen in infants with primary
teeth and a tongue thrusting habit and
in children with familial dysautonomia
(insensitivity to pain).6 Recognition of
these clinical signs may also be an indi
cator of neurological disorders.
Treatment of Riga-Fede disease has
varied from excision of the lesion, to
smoothening of the sharp incisal edges
or rounding of the sharp edges of the
tooth with composite increments, the
latter being where mild to moderate
ulceration occurs.4 Where the ulceration
is large and interfering with feeding,
removal of the tooth can be benecial,
as in this case.
D. Jariwala, R. M. Graham, T. Lewis
By email
1.
2.
3.
4.
5.
6.
Goho C. Neonatal sublingual traumatic ulceration
(Riga-Fede disease): reports of cases. J Dent Child
1996; 63: 362-364.
Hedge R J. Sublingual traumatic ulceration due to
neonatal teeth. J Indian Soc Pedod Prev Dent 2005;
23: 51-52.
Baghdadi Z D. Riga-Fede disease: report of
a case and review. J Clin Pediatr Dent 2001;
25: 209-213.
Slayton R. Treatment alternatives for sublingual
traumatic ulceration (Riga-Fede disease). Pediatr
Dent 2000; 22: 413-414.
Elzay R P. Traumatic ulcerative granuloma with
stromal eosinophilia (Riga-Fede disease and
traumatic eosinophilic granuloma). Oral Surg Oral
Med Oral Pathol 1983; 55: 497-506.
Rakocz M, Frand M, Brand N. Familial dysatonomia
with Riga-Fedes disease: report of case. ASDC
J Dent Child 1987; 54: 57-59.
DOI: 10.1038/bdj.2008.113
2008 Nature Publishing Group
You might also like
- Complete Denture Evaluation DCNADocument17 pagesComplete Denture Evaluation DCNAAravind Krishnan80% (15)
- 2017-Craniofacial DistractionDocument234 pages2017-Craniofacial DistractionMarisol Gallego DuqueNo ratings yet
- Detailed Case History in C - DDocument54 pagesDetailed Case History in C - Dvahini niharika100% (8)
- Diagnostic Criteria Examination Form PDFDocument2 pagesDiagnostic Criteria Examination Form PDFNor Nadia Zakaria50% (2)
- Head & Neck Part 2Document29 pagesHead & Neck Part 2_str8cashhomie100% (1)
- The Arthritis Cure: The Medical Miracle That Can Halt, Reverse, And May Even Cure OsteoarthritisFrom EverandThe Arthritis Cure: The Medical Miracle That Can Halt, Reverse, And May Even Cure OsteoarthritisNo ratings yet
- Section 007 Articulators IDocument17 pagesSection 007 Articulators IAllen SharonNo ratings yet
- Complications of ExodontiaDocument33 pagesComplications of ExodontiaSunil Tiwari100% (1)
- Anatomi Dan Fisiologi TMJ Serta Pergerakan MandibulaDocument28 pagesAnatomi Dan Fisiologi TMJ Serta Pergerakan MandibulaAyu AnggayantiNo ratings yet
- Determinants of OcclusionDocument67 pagesDeterminants of Occlusiondrsmriti100% (4)
- Log of Literature DhiiDocument10 pagesLog of Literature Dhiiapi-733637938No ratings yet
- 0022 3913 (65) 90060 0Document14 pages0022 3913 (65) 90060 0barrera2001No ratings yet
- BioesteticaDocument8 pagesBioesteticasuareztepperNo ratings yet
- Increasing Occlusal Vertical Dimension - Why When and HowDocument6 pagesIncreasing Occlusal Vertical Dimension - Why When and HowLow Junfay MarkNo ratings yet
- Study Guide - Treatment of Edentulous PatientsDocument107 pagesStudy Guide - Treatment of Edentulous PatientsTosca Mavourneen100% (1)
- Problem in Complete Denture Treatment and Postinsertion DentureDocument35 pagesProblem in Complete Denture Treatment and Postinsertion DentureSorabh JainNo ratings yet
- Color Coding Second DraftDocument8 pagesColor Coding Second Draftapi-271242958No ratings yet
- Introduction To Orthotropics HandbookDocument15 pagesIntroduction To Orthotropics HandbookVio Prico100% (1)
- Why-When-How - To Increase Ovd PDFDocument6 pagesWhy-When-How - To Increase Ovd PDFFaheemuddin MuhammadNo ratings yet
- Limb Lengthening SurgeryDocument12 pagesLimb Lengthening Surgerypav20021No ratings yet
- Priyanka Arien Dr.Document5 pagesPriyanka Arien Dr.barcimNo ratings yet
- Ebpp Julie WalkerDocument6 pagesEbpp Julie Walkerapi-240603006No ratings yet
- Adult OrthodonticsDocument70 pagesAdult OrthodonticsTruppti SononeNo ratings yet
- 1retention and RelapseDocument12 pages1retention and RelapseTara TeraNo ratings yet
- Clubfoot ThesisDocument7 pagesClubfoot ThesisCollegePaperGhostWriterAkron100% (2)
- High Angle Cases-ManagementDocument11 pagesHigh Angle Cases-ManagementAmir IqbalNo ratings yet
- The Inverted Orthotic Technique: A Process of Foot Stabilization for Pronated FeetFrom EverandThe Inverted Orthotic Technique: A Process of Foot Stabilization for Pronated FeetNo ratings yet
- The Journey From The Past To The FutureDocument2 pagesThe Journey From The Past To The FutureplsssssNo ratings yet
- NotesDocument639 pagesNotesAmar Bhochhibhoya100% (1)
- Document 20220530145543Document15 pagesDocument 20220530145543Omar GadNo ratings yet
- Sit Stand BookDocument11 pagesSit Stand BookAditya Widya Pranata100% (1)
- Ergonomics Solutions in Dental PracticeDocument6 pagesErgonomics Solutions in Dental Practicecursoenao10No ratings yet
- Thesis OsteopathyDocument6 pagesThesis Osteopathygbv8rcfq100% (1)
- Dental Clinics of North America Sleep Medicine in Dentistry Xi XiiiDocument3 pagesDental Clinics of North America Sleep Medicine in Dentistry Xi XiiiKranti PrajapatiNo ratings yet
- Final File 5d79d83f30ce45.26319674Document6 pagesFinal File 5d79d83f30ce45.26319674Maulida Dara HarjantiNo ratings yet
- Posturodontics in Dentistry A Review PDFDocument4 pagesPosturodontics in Dentistry A Review PDFChaithra ShreeNo ratings yet
- Ear StaplingDocument4 pagesEar StaplingtennebNo ratings yet
- Total Hip Replacement: An Evidence-Based Approach Your Guide From Pre-op Through RecoveryFrom EverandTotal Hip Replacement: An Evidence-Based Approach Your Guide From Pre-op Through RecoveryRating: 5 out of 5 stars5/5 (1)
- One Step Ahead of Osteoarthritis: Stay Flexible and Keep MovingFrom EverandOne Step Ahead of Osteoarthritis: Stay Flexible and Keep MovingNo ratings yet
- JCO - Interviews Dr. Bjorn U. ZaDocument18 pagesJCO - Interviews Dr. Bjorn U. ZaAhmad KhalifaNo ratings yet
- Of Fice Procedures For The Oral and Maxillofacial Surgeon: PrefaceDocument2 pagesOf Fice Procedures For The Oral and Maxillofacial Surgeon: PrefacedrescobedocomfNo ratings yet
- Practical Points in Making Complete Dentures Suction Effective and FunctionalDocument46 pagesPractical Points in Making Complete Dentures Suction Effective and FunctionalCostin SilviuNo ratings yet
- Practice Station Explain Osteoporosis1Document6 pagesPractice Station Explain Osteoporosis1Wenbin GuoNo ratings yet
- 2Document4 pages2Anonymous hWVtGzmZNo ratings yet
- The Young Professions Australia Roundtable 2003 Achieving A Sustainable Future A Dental PerspectiveDocument7 pagesThe Young Professions Australia Roundtable 2003 Achieving A Sustainable Future A Dental PerspectiveAhmed GendiaNo ratings yet
- Sassouni AnalisisDocument2 pagesSassouni Analisisナスティオン ファジャルNo ratings yet
- Occlusal Dysesthesia or Phantom BiteDocument14 pagesOcclusal Dysesthesia or Phantom BitebryanabauerNo ratings yet
- Nutrition and The Teeth For Patients Receiving Radiotherapy To The Head and NeckDocument19 pagesNutrition and The Teeth For Patients Receiving Radiotherapy To The Head and NeckFadhlan Indra SNo ratings yet
- Ass A I Gnment For Data AnalysisDocument10 pagesAss A I Gnment For Data AnalysisFaisol NipunNo ratings yet
- Asynchronous Activity: What Does Good Posture Look Like?Document10 pagesAsynchronous Activity: What Does Good Posture Look Like?Claire Julianne CapatiNo ratings yet
- ErgonomicsDocument4 pagesErgonomicsSubhashini RajshekarNo ratings yet
- Orthodontic Treatment Planning: Problem List To Specific PlanDocument49 pagesOrthodontic Treatment Planning: Problem List To Specific PlanYusra AqeelNo ratings yet
- 1009cei Ortho WebDocument12 pages1009cei Ortho WebAshraf ShehataNo ratings yet
- Whiplash Injury Recovery Booklet - 2nd Edition PDFDocument21 pagesWhiplash Injury Recovery Booklet - 2nd Edition PDFshivani04No ratings yet
- Thesis Statement For Oral HygieneDocument5 pagesThesis Statement For Oral HygienePaySomeoneToWriteAPaperForMeFargo100% (1)
- The Effect of Obesity On The Outcome of Total Knee Arthroplasties in Arthritic PatientsDocument20 pagesThe Effect of Obesity On The Outcome of Total Knee Arthroplasties in Arthritic Patientsapi-379927920No ratings yet
- Cerebral Palsy Research PaperDocument7 pagesCerebral Palsy Research Paperapi-663723303No ratings yet
- Retention and Relapse 3Document13 pagesRetention and Relapse 3Tara TeraNo ratings yet
- A Study To Assess The Effectiveness of Hot and Cold Application On Arthritic Pain and Mobility Status Among Clients With Osteoarthritis in Selected Hospitals at Kolar District.Document31 pagesA Study To Assess The Effectiveness of Hot and Cold Application On Arthritic Pain and Mobility Status Among Clients With Osteoarthritis in Selected Hospitals at Kolar District.Lambert Winston67% (6)
- Reduce Dental AnxietyDocument10 pagesReduce Dental AnxietySung Soon ChangNo ratings yet
- Jaw Surgery: Everything You Need To KnowDocument24 pagesJaw Surgery: Everything You Need To KnowAdrian Stan100% (1)
- OM TherapyDocument8 pagesOM TherapyGiePramaNo ratings yet
- Orthopaedics PunchDocument6 pagesOrthopaedics PunchHicham GawishNo ratings yet
- Mr. Mandibulas: Subscribe To Deepl Pro To Translate Larger Documents. Visit For More InformationDocument87 pagesMr. Mandibulas: Subscribe To Deepl Pro To Translate Larger Documents. Visit For More Informationav495600No ratings yet
- A Parents Guide To Treatment For Development Dysplasia of The HipDocument16 pagesA Parents Guide To Treatment For Development Dysplasia of The HipSunny Gabriels100% (1)
- The Effectiveness of Using Two Stay Two Stray and Numbered Head Together in Teaching Writing Narrative TextDocument1 pageThe Effectiveness of Using Two Stay Two Stray and Numbered Head Together in Teaching Writing Narrative TextMuizzudin AzzaNo ratings yet
- Nursing Department Program Faculty of Nursing and Health University of Muhammadiyah SemarangDocument1 pageNursing Department Program Faculty of Nursing and Health University of Muhammadiyah SemarangMuizzudin AzzaNo ratings yet
- Chewing MasticationDocument6 pagesChewing MasticationMuizzudin AzzaNo ratings yet
- Reinforcement Technique and Variable y in This Study Is Students' Learning Motivation. DataDocument1 pageReinforcement Technique and Variable y in This Study Is Students' Learning Motivation. DataMuizzudin AzzaNo ratings yet
- The Role of Shoe Design in Ankle Sprain Rates Among Collegiate Basketball PlayersDocument4 pagesThe Role of Shoe Design in Ankle Sprain Rates Among Collegiate Basketball PlayersMuizzudin AzzaNo ratings yet
- David Renz Defense Federal Sentencing MemorandumDocument13 pagesDavid Renz Defense Federal Sentencing MemorandumAmanda JordanNo ratings yet
- Occlusion / Orthodontic Courses by Indian Dental AcademyDocument90 pagesOcclusion / Orthodontic Courses by Indian Dental Academyindian dental academyNo ratings yet
- TMJ AnatomyDocument39 pagesTMJ AnatomyPravallika ManneNo ratings yet
- TMJ ImanDocument46 pagesTMJ Imanimaniyas imanNo ratings yet
- Examination & Diagnosis of Edentulous Patients: Presented By: Dr. Jehan Dordi 1 Yr. MdsDocument159 pagesExamination & Diagnosis of Edentulous Patients: Presented By: Dr. Jehan Dordi 1 Yr. MdsAkanksha MahajanNo ratings yet
- Temporomandibular Joint: DR Bhaumik Thakkar MDS-Part 1. Dept. of Periodontology and ImplantologyDocument60 pagesTemporomandibular Joint: DR Bhaumik Thakkar MDS-Part 1. Dept. of Periodontology and ImplantologyJoseph Eduardo Villar CordovaNo ratings yet
- TrismusDocument9 pagesTrismusJoão de BarrosNo ratings yet
- Ginglymoarthrodial JointDocument5 pagesGinglymoarthrodial JointŽäíñäb ÄljaÑabìNo ratings yet
- Muscles of MasticationDocument27 pagesMuscles of MasticationNanditha Swaroop100% (3)
- Lips Together and Teeth Apart: John T. Mahoney, D.D.S. Family DentistryDocument6 pagesLips Together and Teeth Apart: John T. Mahoney, D.D.S. Family DentistryZoran KosecNo ratings yet
- Airway Centric TMJ Airway Centric TMJDocument13 pagesAirway Centric TMJ Airway Centric TMJBeatrix Rednik100% (1)
- Hinge Axis: Presenter B.Alekhya Iiyrpg Moderator Dr. KamalDocument80 pagesHinge Axis: Presenter B.Alekhya Iiyrpg Moderator Dr. Kamalbharathi krishnaNo ratings yet
- Functional Anatomy of Temporomandibular JointDocument44 pagesFunctional Anatomy of Temporomandibular JointRomzi Hanif0% (1)
- TMJ DisordersDocument20 pagesTMJ DisordersErisa BllakajNo ratings yet
- Muscles of MasticationDocument106 pagesMuscles of MasticationShivam SharmaNo ratings yet
- Ferula de MichiganDocument11 pagesFerula de MichiganFernando Espada SalgadoNo ratings yet
- Evaluation of Temporomandibular Joint Spaces and Condylar Position - A CBCT StudyDocument6 pagesEvaluation of Temporomandibular Joint Spaces and Condylar Position - A CBCT StudyDr Yamuna Rani100% (1)
- SATO Dental Asymmetry - TMDDocument5 pagesSATO Dental Asymmetry - TMDJorge Mori VelásquezNo ratings yet
- Icd-10 Codes For Orthodontics: Introduction - Kirt E. Simmons, DDS, PHDDocument10 pagesIcd-10 Codes For Orthodontics: Introduction - Kirt E. Simmons, DDS, PHDmsk adiwiryaNo ratings yet
- Trauma Q&ADocument8 pagesTrauma Q&ANoor MaxeemNo ratings yet
- ASDA Released Papers L-MDocument46 pagesASDA Released Papers L-MZuhair Waheed100% (2)
- Temporo-Mandibular Joint Complex Exercise SuggestionsDocument9 pagesTemporo-Mandibular Joint Complex Exercise SuggestionsClaudia LeperaNo ratings yet
- Oral Surgery FlashCardsDocument63 pagesOral Surgery FlashCardsMihika MahandwanNo ratings yet