Professional Documents
Culture Documents
Neurosurgical Image
Neurosurgical Image
Uploaded by
fraushaiCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Neurosurgical Image
Neurosurgical Image
Uploaded by
fraushaiCopyright:
Available Formats
British Journal of Neurosurgery, February 2015; 29(1): 5253
2014 The Neurosurgical Foundation
ISSN: 0268-8697 print / ISSN 1360-046X online
DOI: 10.3109/02688697.2014.954987
NEUROSURGICAL IMAGE
Deep cerebral venous thrombosis during pregnancy
Abdullah Hamid Feroze, Aditya Mantha & Omar Choudhri
Br J Neurosurg Downloaded from informahealthcare.com by Chinese University of Hong Kong on 04/10/15
For personal use only.
Department of Neurosurgery, Stanford University School of Medicine, Stanford, CA, USA
Introduction
injury to the thalamus, basal ganglia, and subcortical white
matter.1 However, with early diagnosis and appropriate management, excellent neurologic recovery remains possible.
The rarest form of cerebral venous thromboses, thrombosis of the deep venous system, is often fatal given potential
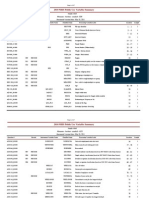
Fig. 1. Magnetic resonance (MR) imaging in deep cerebral venous thrombosis. (A) MR venography reconstruction demonstrating filling of only
the superficial cerebral venous system including the superior sagittal sinus and the transverse sigmoid sinus. There is no demonstration of the
deep venous system given thrombosis. (B) Axial gradient echo image demonstrating thrombosed internal cerebral veins (arrowheads) and the
straight sinus (arrow). (C) Axial T2 image showing increased signal in bilateral thalami and basal ganglia secondary to venous engorgement with
associated edema. (D) Coronal FLAIR image showing edema in bilateral thalami, caudate nuclei, and putamen secondary to deep cerebral venous
thrombosis.
Correspondence: Dr. Omar Choudhri, Department of Neurosurgery, Stanford University School of Medicine, Edwards Building R201, 300 Pasteur Drive,
Stanford, CA 94305, USA. Tel: 1 (610) 202-7144. Fax: 1 (650) 723-7813. E-mail: ochoudhri@stanford.edu
Received for publication 3 March 2014; accepted 4 August 2014
52
Cerebral venous thrombosis during pregnancy
Br J Neurosurg Downloaded from informahealthcare.com by Chinese University of Hong Kong on 04/10/15
For personal use only.
Case history
A 27-year-old pregnant woman at 10-week gestation presented with a 3-day history of headaches, vomiting, and
altered mental status, alert and oriented only to name and
location upon admission. Examination demonstrated 3/5
strength bilaterally in the lower extremities with the corresponding hyperactive (3) patellar and Achilles reflexes.
Imaging demonstrated significant edema of the bilateral
basal ganglia and thalami in addition to engorgement of the
central veins (Fig. 1).
Given concern for cerebral venous thrombosis involving the straight sinus in the setting of pregnancy-induced
hypercoagulability, the patient was initiated on a heparin
drip. Electroencephalography demonstrated no evidence
of epileptiform activity. She was stabilized with 3% normal
saline prior to transitioning to low molecular weight heparin, and ultimately discharged without evidence of residual
neurologic deficits.
Discussion
In contrast to dural venous sinus thromboses, pathology of
the deep cerebral vasculature is often associated with faster
progression to profound deficits and poorer prognosis, particularly when the internal cerebral veins are involved.2,3
Associated signs and symptoms are typically nonspecific.4
Thalami are usually bilaterally edematous with potential
superimposed venous infarction, but may also present in a
unilateral or asymmetric fashion.3 Anticoagulation is considered the treatment of choice, even in the presence of
53
hemorrhage.5 Albeit rare, full neurologic recovery is possible,
as documented herein.6
Twenty to thirty percentage of cerebral venous thromboses remain idiopathic in nature.4 In our case, hypercoagulability workup was negative for antiphospholipid antibody,
Factor V Leiden, prothrombin 20210A, and antithrombin
III syndromes. Levels of activated protein C resistance and
Protein S levels were elevated but were difficult to interpret
in the setting of pregnancy.
Declarations of interest: The authors report no declarations of interest. The authors alone are responsible for the
content and writing of the paper.
References
1. Gladstone DJ, Silver FL, Willinsky RA , Tyndel FJ, Wennberg R. Deep
cerebral venous thrombosis: an illustrative case with reversible
diencephalic dysfunction. Can J Neurol Sci 2001;28:15962.
2. Haley EC Jr, Brashear HR, Barth JT, Cail WS, Kassell NF. Deep
cerebral venous thrombosis. Clinical, neuroradiological, and
neuropsychological correlates. Arch Neurol 1989;46:33740.
3. Herrmann KA , Sporer B, Yousry TA . Thrombosis of the internal
cerebral vein associated with transient unilateral thalamic edema:
a case report and review of the literature. AJNR Am J Neuroradiol
2004;25:13515.
4. Bousser MG, Chiras J, Bories J, Castaigne P. Cerebral venous
thrombosisa review of 38 cases. Stroke 1985;16:199213.
5. de Bruijn SF, Stam J. Randomized, placebo-controlled trial of
anticoagulant treatment with low-molecular-weight heparin for
cerebral sinus thrombosis. Stroke 1999;30:4848.
6. Hassan KM, Kumar D. Reversible diencephalic dysfunction
as presentation of deep cerebral venous thrombosis due to
hyperhomocysteinemia and protein S deficiency: Documentation
of a case. J Neurosci Rural Pract 2013;4:1936.
You might also like
- Cerebral Herniation Syndromes and Intracranial HypertensionFrom EverandCerebral Herniation Syndromes and Intracranial HypertensionMatthew KoenigNo ratings yet
- A Case Report of Hydrocephalus in A US Military RecruitDocument3 pagesA Case Report of Hydrocephalus in A US Military RecruitRomita PutriNo ratings yet
- The Dangers of PRESDocument5 pagesThe Dangers of PRESShahnaaz ShahNo ratings yet
- Bpa 12504Document31 pagesBpa 12504Sergeat18BNo ratings yet
- Neurohistiocytosis: Two Cases of A Rare DiseaseDocument8 pagesNeurohistiocytosis: Two Cases of A Rare DiseaseIJAR JOURNALNo ratings yet
- 5.V6 (1) 69 71Document3 pages5.V6 (1) 69 71王湘淇No ratings yet
- DISH With SCIDocument5 pagesDISH With SCICornerstone OrganizationNo ratings yet
- Adem LikeDocument4 pagesAdem LikeRodrigo AriasNo ratings yet
- Intracranial Hemorrhage With Cerebral Venous Sinus ThrombosisDocument2 pagesIntracranial Hemorrhage With Cerebral Venous Sinus ThrombosisNeurologia homicNo ratings yet
- Cerebellar Hemangioblastoma-A Rare EntityDocument10 pagesCerebellar Hemangioblastoma-A Rare EntityJay LeheriNo ratings yet
- Mycoplasma Pneumoniae. Ann Intern Med: Crisis Cerebelosas: ¿Se Puede Hablar de Ellas?Document2 pagesMycoplasma Pneumoniae. Ann Intern Med: Crisis Cerebelosas: ¿Se Puede Hablar de Ellas?Tamara GarcésNo ratings yet
- Steroid Pulse Therapy in Herpes Simplex Encephalitis: Neurosciences July 2013Document3 pagesSteroid Pulse Therapy in Herpes Simplex Encephalitis: Neurosciences July 2013Dwi KurniawanNo ratings yet
- Clinical Reasoning: A Young Man With Recurrent Paralysis, Revisable White Matter Lesions and Peripheral Neuropathy Word Count: 945Document13 pagesClinical Reasoning: A Young Man With Recurrent Paralysis, Revisable White Matter Lesions and Peripheral Neuropathy Word Count: 945aileenzhongNo ratings yet
- Posterior Reversible Encephalopathy Syndrome After Lumbar PunctureDocument2 pagesPosterior Reversible Encephalopathy Syndrome After Lumbar PunctureMedtext PublicationsNo ratings yet
- Maller2019 Neonatal Head Ultrasound Part 2Document12 pagesMaller2019 Neonatal Head Ultrasound Part 2Modou NianeNo ratings yet
- J Neurol Neurosurg Psychiatry 2005 Vanopdenbosch 1017 8Document3 pagesJ Neurol Neurosurg Psychiatry 2005 Vanopdenbosch 1017 8afiwahyuNo ratings yet
- HydrancephalyDocument3 pagesHydrancephalyinammetNo ratings yet
- Eastern Equine Encephalitis: A Classical Case: Connecticut Medicine October 2014Document4 pagesEastern Equine Encephalitis: A Classical Case: Connecticut Medicine October 2014Chrislyn SanlaoNo ratings yet
- Ecr2013 C-2557Document33 pagesEcr2013 C-2557olaNo ratings yet
- Agenesia CerebeloDocument5 pagesAgenesia CerebeloDiretoria CientíficaNo ratings yet
- 07-11 Dipper StrokeDocument6 pages07-11 Dipper StrokeKelly Jasmin Meza CapchaNo ratings yet
- Neurology Clinical Cases PDFDocument219 pagesNeurology Clinical Cases PDFHandre PutraNo ratings yet
- مصدر بحث PDFDocument9 pagesمصدر بحث PDFMohammed AdilNo ratings yet
- Comment: Vs 1 7% of 261 Patients With Atrial TachyarrhythmiasDocument2 pagesComment: Vs 1 7% of 261 Patients With Atrial TachyarrhythmiasDewina Dyani Rosari IINo ratings yet
- Journal Pre-Proof: Journal of Chemical NeuroanatomyDocument48 pagesJournal Pre-Proof: Journal of Chemical NeuroanatomyandreiNo ratings yet
- Adult-Onset Subgaleal Hematoma Caused by Hair Pulling: A Rare OccurrenceDocument2 pagesAdult-Onset Subgaleal Hematoma Caused by Hair Pulling: A Rare OccurrenceAisyah MoslemzzNo ratings yet
- Cadasil Syndrome: A Case Report With A Literature ReviewDocument4 pagesCadasil Syndrome: A Case Report With A Literature ReviewAna Carolina RibasNo ratings yet
- J Clinph 2013 03 031Document7 pagesJ Clinph 2013 03 031Andres Rojas JerezNo ratings yet
- E110 FullDocument2 pagesE110 FullLuther ThengNo ratings yet
- 1 s2.0 S0031395503002153 MainDocument21 pages1 s2.0 S0031395503002153 Maindiego bustosNo ratings yet
- Ischemic Stroke in A 3-Year-Old Child Revealing Thrombosis of The Vertebrobasilar Territory, A Case ReportDocument5 pagesIschemic Stroke in A 3-Year-Old Child Revealing Thrombosis of The Vertebrobasilar Territory, A Case ReportIJAR JOURNALNo ratings yet
- Case Report Pons 1Document5 pagesCase Report Pons 1indanazulfaaNo ratings yet
- 0309 Case 2Document4 pages0309 Case 2willygopeNo ratings yet
- Posterior Reversible Encephalopathy Syndrome (Pres) in A Patient With Late Postpartum Eclampsia: Case ReportDocument4 pagesPosterior Reversible Encephalopathy Syndrome (Pres) in A Patient With Late Postpartum Eclampsia: Case ReportIJAR JOURNALNo ratings yet
- Misdiagnosis of Spontaneous Spinal Epidural Hematoma in A Parturient: A Case ReportDocument4 pagesMisdiagnosis of Spontaneous Spinal Epidural Hematoma in A Parturient: A Case ReportIJAR JOURNALNo ratings yet
- Intrasphenoidal Encephalocele: An Incidental Finding in Emergency DepartmentDocument3 pagesIntrasphenoidal Encephalocele: An Incidental Finding in Emergency DepartmentRinda AndreanditaNo ratings yet
- TRuncal AtaxiaDocument2 pagesTRuncal AtaxiavinhannyNo ratings yet
- Double-Outlet Left Ventricle and Vascular MalformationsDocument3 pagesDouble-Outlet Left Ventricle and Vascular MalformationsRaul UrietaNo ratings yet
- A 7-Year-Old Boy Dying of Acute Encephalopathy: Case History Autopsy FindingsDocument4 pagesA 7-Year-Old Boy Dying of Acute Encephalopathy: Case History Autopsy FindingswillygopeNo ratings yet
- Hereditary Hemorrhagic Telangiectasia (HHT)Document15 pagesHereditary Hemorrhagic Telangiectasia (HHT)MarshallNo ratings yet
- A 19-Year-Old Man With Sickle Cell Disease Presenting With Spinal Infarction: A Case ReportDocument6 pagesA 19-Year-Old Man With Sickle Cell Disease Presenting With Spinal Infarction: A Case ReportJabber PaudacNo ratings yet
- 1 s2.0 S1878875018317406 PDFDocument10 pages1 s2.0 S1878875018317406 PDFeribu191No ratings yet
- Brmedj00111 0029aDocument1 pageBrmedj00111 0029aapi-289577018No ratings yet
- A Case Report of Posterior Reversible Encephalopathy Syndrome in A Patient Diagnosed With Emphysematous Necrotizing Biliary PancreatitisDocument5 pagesA Case Report of Posterior Reversible Encephalopathy Syndrome in A Patient Diagnosed With Emphysematous Necrotizing Biliary Pancreatitisbijnn journalNo ratings yet
- Art Acta - Neurol.belgicaDocument6 pagesArt Acta - Neurol.belgicaAna GabrielaNo ratings yet
- Prion BrainDocument2 pagesPrion BrainD SNo ratings yet
- Thalssemia & Spinal Cord Compression in PregnancyDocument1 pageThalssemia & Spinal Cord Compression in PregnancyThao NguyenNo ratings yet
- Brain 2014 Yu Brain Awu239Document5 pagesBrain 2014 Yu Brain Awu239Angeles RbNo ratings yet
- NCC Case StudyDocument4 pagesNCC Case StudyMasego MekgoeNo ratings yet
- Donovan 2006Document7 pagesDonovan 2006PGY 6No ratings yet
- 2011 BakirciogluDocument13 pages2011 BakirciogluMestrado EducacaoNo ratings yet
- Frontal Encephalocele - A Rare Case Report With Review of LiteratureDocument4 pagesFrontal Encephalocele - A Rare Case Report With Review of LiteratureAyu TrisyaNo ratings yet
- A Case of Deep Cerebral Venous Thrombosis Presenting Like Acute Necrotizing EncephalopathyDocument4 pagesA Case of Deep Cerebral Venous Thrombosis Presenting Like Acute Necrotizing EncephalopathySachin DangiNo ratings yet
- Central Venous Catheterization: To The EditorDocument3 pagesCentral Venous Catheterization: To The Editordrpiratheepan4274No ratings yet
- BH 010060 ENGDocument2 pagesBH 010060 ENGCarlosNo ratings yet
- Posterior Reversible Encephalopathy Syndrome Secondary To Acute Post-Streptococcal Glomerulonephritis in A 12-Year-Old GirlDocument2 pagesPosterior Reversible Encephalopathy Syndrome Secondary To Acute Post-Streptococcal Glomerulonephritis in A 12-Year-Old GirlwawaningNo ratings yet
- Journal of Medical Case ReportsDocument4 pagesJournal of Medical Case ReportsSri Wahyuni YkNo ratings yet
- Hyperintense Vessels On FLAIR: Hemodynamic Correlates and Response To ThrombolysisDocument5 pagesHyperintense Vessels On FLAIR: Hemodynamic Correlates and Response To ThrombolysisKumail KhandwalaNo ratings yet
- Lateralization in Autononic Dysfunction in Ischemic Stroke Involving The Insular CortexDocument5 pagesLateralization in Autononic Dysfunction in Ischemic Stroke Involving The Insular CortexAlbertochoNo ratings yet
- Neurovascular NeuropsychologyFrom EverandNeurovascular NeuropsychologyRonald M. LazarNo ratings yet
- Lucky Draw - List of Winners - 1st PhaseDocument1 pageLucky Draw - List of Winners - 1st PhasefraushaiNo ratings yet
- IntermediateCourse2014 Timetable 20150218 WebsiteDocument2 pagesIntermediateCourse2014 Timetable 20150218 WebsitefraushaiNo ratings yet
- Practice of Radiology in 2018Document130 pagesPractice of Radiology in 2018fraushaiNo ratings yet
- Spring Issue 2012Document22 pagesSpring Issue 2012fraushaiNo ratings yet
- Japanese Doctors Life SpanDocument5 pagesJapanese Doctors Life SpanfraushaiNo ratings yet
- Cantlie and PVEDocument3 pagesCantlie and PVEfraushaiNo ratings yet
- SyncopeDocument3 pagesSyncopeanishdNo ratings yet
- Susunan Acara Seminar ANGINA 2019Document2 pagesSusunan Acara Seminar ANGINA 2019Mellia Wida MasitaNo ratings yet
- Second SightDocument2 pagesSecond SightMasbooksNo ratings yet
- RKUD2999Document34 pagesRKUD2999Nabila AzharNo ratings yet
- Biocompatibility of Dental MaterialsDocument51 pagesBiocompatibility of Dental MaterialsEsome Sharma100% (1)
- Vtne Study Strategies Zuku ReviewDocument33 pagesVtne Study Strategies Zuku ReviewEmmanuel Boulay100% (1)
- Maxillary Anesthesia - 2Document35 pagesMaxillary Anesthesia - 2Mohammed NabeelNo ratings yet
- Ayurveda Consultation SydneyDocument5 pagesAyurveda Consultation SydneyAnand Singh ContentNo ratings yet
- CHN 1st and 2nd Level 2nd SemDocument9 pagesCHN 1st and 2nd Level 2nd SemCharlaine Gripal SudlaNo ratings yet
- The Medical Mystery of Vincent Van GoghDocument21 pagesThe Medical Mystery of Vincent Van Goghapi-243780701No ratings yet
- Data ObatDocument17 pagesData ObatnooNo ratings yet
- Sandhi VataDocument72 pagesSandhi VataP V N R PrasadNo ratings yet
- CHN UltiDocument7 pagesCHN UltiZen AbzuNo ratings yet
- CIVIL SERVICE FORM 41 Medical CertificateDocument1 pageCIVIL SERVICE FORM 41 Medical CertificateElc Elc ElcNo ratings yet
- Rules of TransfusionDocument4 pagesRules of Transfusionapi-233414716100% (1)
- Psychiatry McqsDocument9 pagesPsychiatry McqsSagar Karia100% (4)
- National Tech Guidelines For IsdrDocument616 pagesNational Tech Guidelines For IsdrYahya H SakwaNo ratings yet
- Fluid and Electrolytes ImbalanceDocument49 pagesFluid and Electrolytes ImbalanceMohamed Na3eemNo ratings yet
- Đề 03Document4 pagesĐề 03teachingielts2023No ratings yet
- NCP For Deficient Fluid VolumeDocument2 pagesNCP For Deficient Fluid VolumeRedwing_Dc_854758% (12)
- 2010 NHIS Public Use Variable Summary: Filename - Section: Document Vers Ion DateDocument27 pages2010 NHIS Public Use Variable Summary: Filename - Section: Document Vers Ion DateJin SiclonNo ratings yet
- EpisiotomyDocument3 pagesEpisiotomyAlexandra Chiriac AntonNo ratings yet
- Session 5 Guide 31 Workplace Based AssessmentDocument21 pagesSession 5 Guide 31 Workplace Based AssessmentRiry AmbarsaryNo ratings yet
- Daftar Pustaka 4Document5 pagesDaftar Pustaka 4Devinta Nurul ErlanggaNo ratings yet
- Clinical Oral Implants Res - 2020 - Neckel - Influence of Implant Specific Radiation Doses On Peri Implant Hard and SoftDocument13 pagesClinical Oral Implants Res - 2020 - Neckel - Influence of Implant Specific Radiation Doses On Peri Implant Hard and SoftFelix SchweppeNo ratings yet
- TMF Reference Model v3.2.1 Release NotesDocument7 pagesTMF Reference Model v3.2.1 Release NotesKosomotoNo ratings yet
- JawetzDocument3 pagesJawetzAvissa Fadlika DausawatiNo ratings yet
- Running Head: Fast Tracks in The Emergency Department 1Document11 pagesRunning Head: Fast Tracks in The Emergency Department 1FikriNo ratings yet
- Oncology EmergencyDocument41 pagesOncology Emergencyomad pendaftaranPPDS100% (2)
- The Impact of An Online Educational Game On Breast Cancer Awareness Among University Female Students, Malaysia: A Pilot StudyDocument11 pagesThe Impact of An Online Educational Game On Breast Cancer Awareness Among University Female Students, Malaysia: A Pilot StudySteve GannabanNo ratings yet