Professional Documents
Culture Documents
Addison Disease, Penyakit Addison
Addison Disease, Penyakit Addison
Uploaded by
KertiasihwayanOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Addison Disease, Penyakit Addison
Addison Disease, Penyakit Addison
Uploaded by
KertiasihwayanCopyright:
Available Formats
1
CHAPTER I
INTRODUCTION
1.1. Background
Addisons disease is a rare autoimmune dissease,1,2,3 that occurs when
the adrenal glands do not produce enough of their hormones. 1 Most of the
cases in Addisons disease is caused by autoimmune disease (about 80% of
total cases),
1,3,4,5
less common causes include granulomatous disease (eg
sarcoidosis, tuberculosis), haematological malignancies, metastatic malignant
disease, infiltrative metabolic disease (eg amyloidosis), congenital adrenal
hyperplasia, abdominal radiation and the abrupt cessation of long-term steroid
therapy.4 Those cases lead to destruction or disfunction of entire adrenal
cortex.1,3
Addisons disease has insidious onset (e.g. malaise, anorexia, diarrhea,
weight loss, joint, and back pain)2,6,4 as the chronic primary adrenal
insuffiency and acute manifestations, in the form of Addisonian crisis (e.g.
orthostatic hypotension, fever, and hypoglycemia)6,4, that can be fatal if not
properly recognized and treated,1,2 however, incidence of such causes of
deaths is not known.1
Further
investigations,
including
anti-adrenal
antibodies
and
radiologicalimaging of the adrenal glands, are required to determine the
underlying
cause. Treatment
involves
the
lifelong replacement of
glucocorticoid and mineralocorticoid.6,4,7
Thomas Addison is the first person that describe this disease at 1855, 3,8,5
in his classic paper, On the Constitutional and Local Effects of Disease of the
Supra-Renal Capsules.8
CHAPTER II
CONTENT
2.1. Etiology and Pathogenesis of Addison Disease
The etiopathogenesis of primary adrenocortical insufficiency has changed
over time. Prior to 1920, tuberculosis was the major cause of adrenocortical
insufficiency. Since 1950, autoimmune adrenalitis with adrenal atrophy has
accounted for about 80% of cases. It is associated with a high incidence of other
immunologic and autoimmune endocrine disorders. Primary adrenocortical
insufficiency, or Addison disease, is rare, with a reported prevalence of 35 to 140
per million population.9
2.1.1. Autoimmune Adrenocortical Insufficiency
Autoimmune Addison disease is frequently accompanied by other
immune disorders. There are two different syndromes in which autoimmune
adrenal insufficiency may occur. The best characterized one is known as
autoimmune
polyendocrinopathy-candidiasis-ectodermal
dystrophy
syndrome (APCED), or autoimmune polyglandular syndrome type 1 (APS1). This is an autosomal recessive disorder that usually presents in childhood
and is accompanied by hypoparathyroidism, adrenal failure, and
mucocutaneous candidiasis. APS-1 results in most cases from a mutation of
the autoimmune regulator gene (AIRE), which is located on chromosome
21q22.3. Autoantibodies against the cholesterol side chain cleavage enzyme
(P450scc, CYP11A1) and others have been described in patients with this
disorder.9
The more common presentation of autoimmune adrenocortical
insufficiency is associated with HLA-related disorders including type 1
diabetes mellitus and autoimmune thyroid disease. Other less common
related disorders include alopecia areata, vitiligo, primary hypogonadism,
pernicious anemia, and celiac disease. This disorder is often referred to as
APS type 2. The genetic susceptibility to this disorder is linked to HLADR3 or DR4 (or both). These patients have antiadrenal cytoplasmic
antibodies that may be important in the pathogenesis of this disorder and
autoantibodies against 21-hydroxylase (p450C21, CYP21A2)9,10,
2.1.2. Infection
Tuberculosis and fungal infections are associated with enlarged
adrenals that may show calcifications. Of note, the azole antifungal agents,
such as ketoconazole, inhibit adrenal cytochrome P450 steroidogenic
enzymes that are essential for cortisol biosynthesis. Thus, azole antifungal
treatment, especially with ketoconazole, in patients with marginal
adrenocortical reserve due to fungal disease may precipitate adrenal crisis.10
HIV/AIDS has been associated with pathologic involvement of the
adrenal gland. Primary adrenal insufficiency in AIDS is usually caused by
opportunistic infections such as fungal infection, cytomegalovirus, and
mycobacterium avium complex. Adrenocortical insufficiency usually occurs
as a late manifestation in AIDS patients with very low CD4 counts.10,11
2.2. Pathophysiology of Addison Disease
Addisons disease only affects the cortex portion of the adrenal glands; it
causes deficiency of hormone that is produced there, including mineralocorticoid
(aldosterone), glucocorticoid (cortisol), and adrenal androgen.
2.2.1. Mineralocorticoid (Aldosterone)
Aldosterone has function mainly to maintain electrolyte balance by
increasing natrium and chloride reabsorption and also increasing kalium
secretion in renal tubules epithelium. Deficiency of aldosterone causes
hyponatremia that followed by hyperkalemia in extracellular fluid
significantly. Decreasing extracellular fluid total volume leads to low
plasma volume and hypotension. Shock will present when cardiac output
decreases. In severe hyperkalemic condition (60-100% above normal),
cardiac contraction weakness and arrhythmia can be clearly seen.12
Aldosterone also stimulates hydrogen secretion that will be changed
with natrium in renal. Increasing hydrogen concentration in extracellular
fluid can cause mild acidosis. Another function of aldosterone is increasing
natrium absorption in intestine, mainly in colon. Failure of this function will
be followed by failure of kalium, another anion, and water absorption; the
patient will suffers from diarrhea and so will presents sign of dehydration.12
2.2.2. Glucocorticoid (Cortisol)
Cortisol plays a role in carbohydrate, protein, and lipid metabolism. In
carbohydrate metabolism, cortisol stimulates gluconeogenesis in the liver by
increasing enzymes that is needed to this process and transporting amino
acid from extrahepatic tissue. It also reduces cellular glucose usage by
unknown mechanism. In protein metabolism, cortisol increases level of
liver protein and plasma protein by suppressing amino acid mobilization
into extrahepatic tissue. It reduces protein synthesize, but protein catabolism
continues inside the cell, so tissue protein deposit will decrease. In lipid
metabolism, cortisol helps in increasing fatty acid mobilization from
adipose tissue. So, suppression of many metabolism functions will be
happened in Addisons disease, results in fatigue and weakness.12
In the correlation of metabolism, patient with Addisons disease may
presents with hypoglycemic, weight loss, and muscle weakness. Decreasing
cortisol secretion reduces blood glucose, thus will cause hypoglycemic. Low
blood glucose triggers insulin secretion to drop. Beside its function in
glucose uptake, insulin can also stimulates triglyceride storage, so the
patient will experienced weight loss. Muscle weakness is resulted from lack
of ATP because of low glucose. Cortisol is one of orexigenic substance or
appetite stimulant; it correlates with complain of loss of appetite from
patient with Addisons disease.12,13
Cortisol is important in managing the body to react with stress,
including trauma, inflammation, infection, surgery, emotional, etc. In
cortisol deficiency, the patient with extreme stressful events may present
with severe illnesses. Cortisol is also found to stimulates erythrocyte
production by unknown mechanism; the patient will show anemia signs in
Addisons disease.13
When Adrenocorticotropin Hormone (ACTH) was secreted from
anterior hypophysis gland, another hormone that has same chemical
characteristics, such as Melanocyte Stimulating Hormone (MSH), will also
be secreted too because those hormones have same precursor. In normal
condition, MSH did not give significant effect on human body because it
was secreted only in small amount. If ACTH is rapidly secreted because of
low level plasma cortisol, secretion of MSH will be increased too. This
condition
leads
to
overstimulation
of
melanin
formation
or
hyperpigmentation in skin and mucous membrane.12,14,15
2.2.3. Adrenal Androgen
Besides mineralocorticoid and glucocorticoid, adrenal cortex also
secretes sex hormone--adrenal androgen, which has same effects with
testosterone. Because it secreted in small amount, deficiency in this
hormone did not produce significant features. Women may have loss of
androgen-stimulated hair, such as pubic and axillary hair, and irregular or
absent menstrual periods. Men do not have hair loss because male androgen
is produced primarily in testes.12,13,16
2.3. Clinical Presentation of Addison Disease
Addison disease presents insidiously with nonspecic symptoms that easily
can be mistaken for other more prevalent conditions. For example, its common
symptoms, chronic fatigue, malaise, and anorexia may mimic a depressive illness.
Likewise, unintentional weight loss, nausea, vomiting, and vague abdominal pain
may be confused with symptoms of a gastrointestinal or eating disorder.
Symptoms
of
postural
hypotension
(syncope,
postural
dizziness)
and
hypoglycemia are late manifestations of the disease. Pigmentation of skin and
mucous membranes, when present, is a cardinal sign of Addison disease.17
Several biochemical abnormalities may provide a clue to the diagnosis of
Addison disease. In a patient with unexplained hyponatremia, adrenal
insufciency must be excluded before making the diagnosis of syndrome of
inappropriate antidiuretic hormone secretion. Likewise, in a patient with
unexplained hyperkalemia, Addison disease must be considered as a possibility
before treating the patient with insulin and dextrose infusion. Some patients with
Addison disease show a raised serum thyrotropin level at presentation. The
diagnosis of Addison disease must be considered in a hypothyroid patient whose
symptoms worsen after starting thyroxine.18
Furthermore, unexplained recurrent hypoglycemic episodes in a patient with
type 1 diabetes should also raise a suspicion of Addison disease. About half of
patients with Addison disease present acutely with adrenal crises. This is a lifethreatening emergency characterized by severe dehydration and circulatory shock.
Many patients also have nausea, vomiting, and abdominal pain, which may lead to
a misdiagnosis of an acute abdomen. Acute adrenal crisis is usually precipitated
by infection or other forms of severe physiological stress.19
2.4. Diagnosis of Addison Disease
2.4.1. Anamnesis and Physical Examination
Patient with Addisons disease usually comes with non-specific
complains, such as Loss of appetite and weight, nausea, vomiting or diarrhea,
muscle weakness, fatigue, lightheadedness, chronic-worsening fatigue, salt
cravings, dehydration, abdominal pain, irregular or no menstrual periods in
women, mood swings, mental confusion or loss of consciousness. Low blood
pressure (hypotension), Increased pigmentation of the skin, particularly
around scars and bony areas, loss of pubic and axillary hair in women.
2.4.2. Laboratory Result
In the early phase of gradual adrenal destruction, there may be no
demonstrable abnormalities in the routine laboratory parameters. In more
advanced stage of adrenal destruction, serum sodium, chloride, and
bicarbonate levels are reduced, and the serum potassium level is elevated. The
hyponatremia is due both to loss sodium into the urine. This extravascular
sodium loss depletes extracellular fluid volume and accentuates hypotension.
Elevated plasma vasopressin and angiotensin II levels may contribute to the
hyponatremia. Hyperkalemia is due to a combination of aldosterone
deficiency, impaired glomerular filtration, and acidosis. Basal level of cortisol
and aldosterone are subnormal and fail to increase following ACTH
administration. There may be a normocytic anemia, a relative lymphocytosis,
and a moderate eosinophilia.
The diagnosis of adrenal insufficiency should be made only with ACTH
stimulation testing to assess adrenal reserve capacity for steroid production.
In brief, the best screening test is the cortisol response 60 min after 250 g of
cosyntropin given intramuscularly or intravenously. Cortisol level should
exceed 495 nmol/L (18 g/dL). If the response is abnormal, then primary and
secondary adrenal insufficiency can be distinguish by measuring aldosterone
levels from the same blood sample. Furthermore, in primary adrenal
insufficiency, plasma ACTH and associated peptides (-LPT) are elevated
because
of
loss
the
usual
cortisol-hypothalamic-pituitary
feedback
relationship.20
Antiadrenal antibodies are found in most cases of idiopathic Addisons
disease but in minority of those due to adrenal tuberculosis. Said to have very
high sensitivity, specificity, and predictive value for development of
adrenocortical failure in women with normal adrenal adrenocortical
function.21 In patients suspected of having an Addisonian crisis, health professionals
must begin treatment with injections of salt, glucose-containing fluids, and
glucocorticoid hormones immediately. Although a reliable diagnosis is not possible
during crisis treatment, measurement of blood ACTH and cortisol during the crisisbefore glucocorticoids are given-is enough to make a preliminary diagnosis. Low
blood sodium, low blood glucose, and high blood potassium are also usually present
at the time of an adrenal crisis. Once the crisis is controlled, an ACTH stimulation
test can be performed to obtain the specific diagnosis. 22
2.4.3. Imaging
In Addison disease from an autoimmune abnormality, the adrenal gland
is small at CT. A second cause of Addison disease is replacement of the
adrenal gland by either neoplasm, hemorrhage, or infection, the adrenal gland
is often enlarged. The adrenal masses caused by granulomatous disease or
hemorrhage may involute and subsequently calcify.23
2.5. Differential Diagnosis
2.5.1. Adrenal Crisis
Adrenal crisis is an acute adrenal insufficiency, which occurs if the level
of cortisol hormone is decreasing suddenly, and can lead to death if it doesnt
treat immediately. The difference of Addisons disease and adrenal crisis is
the symptoms. Symptoms in Addisons disease develop slowly, over months
to
years,
with
weakness,
fatigue,
anorexia,
weight
loss,
and
hyperpigmentation as the primary symptoms. In contrast, symptoms of
adrenal crisis occur acutely, can manifest with vomiting, abdominal pain, and
hypovolemic shock.24,25
2.5.2. Adrenal Hemorrhage
Adrenal hemorrhage is a relatively uncommon condition with a variable
and nonspecific presentation that may lead to acute adrenal crisis, shock, and
death unless it is recognized promptly and treated appropriately. It can result
from a variety of causes (traumatic as well as non traumatic), When
unilateral, it is often clinically silent. In contrast, bilateral adrenal hemorrhage
can lead to catastrophic adrenal insufficiency.26,27
2.5.3. C-17 Hydroxylase Deficiency
It is the rare variant of congenital adrenal hyperplasia. Patients with 17hydroxylase deficiency have alterations in their CYP17 gene, which encodes
the P450C17 enzyme, enzyme that found in the zona reticularis of the adrenal
cortex and plays a central role in steroidogenesis. Steroidogenesis is essential
for the production of cortisol and sex steroids. Thus, patient with 17hydroxylase deficiency have reduced secretion of cortisol, androgen, and
estrogen, with adrenal and gonadal steroidogenesis impairment.28,29
2.6. Treatment of Addison Disease
The primary goal of treatment is to overcome glucocorticoid and
mineralocorticoid deficiencies.30
2.6.1. Glucocorticoid Replacement
Hydrocortisone is most commonly used for glucocorticoid replacement.
Long-acting glucocorticoids, dexamethasone, and prednisolone have the
advantage of a once-daily dosing schedule but have the drawback of losing
the diurnal pattern, resulting in excess glucocorticoid levels overnight.30 In the
chronic cases, prednisone or prednisolone are preferably performed,
glucocorticoids with reduced mineralocorticoid effect and lower incidence of
myopathy than fluorinated glucocorticoids (e.g. dexamethasone).31
In Addison disease, standard replacement dose of hydrocortisone is 1525 mg a day, given in 2 or 3 divided doses (10 mg on waking, 5 mg at noon, 5
mg early evening). In practice, the dose of hydrocortisone is maintained on
the basis of clinical assessment, taking an account of patients wellbeing, and
presence of any signs of over-replacement (eg, hypertension, weight gain,
thin skin, easy bruising, and glucose intolerance) or under-replacement (eg,
weight loss and pigmentation).30
2.6.2. Mineralocorticoid Replacement
Fludrocortisone is the only available agent for mineralocorticoid
replacement. The usual starting dose is 100 gram a day. The dose is adjusted
(usually 50-200 gram a day) according to clinical response. Hypertension and
presence of ankle edema suggest over-replacement, while salt craving,
postural hypotension, and hyperkalemia are signs of under-replacement..30
2.6.3. Management of an Adrenal Crisis
An adrenal crisis is a life-threatening medical emergency that requires
urgent hospital admission for treatment with intravenous hydrocortisone and
crystalloid. Patients may need several liters of normal saline to maintain their
blood pressure. The recommended initial dose of hydrocortisone is 100 mg,
with subsequent doses of 100-200 mg over 24 hours divided into 3 or 4
doses.30
2.7. Complication of Addison Disease
10
Adrenal crisis is a medical emergency and must be treated immediately. 32 If it
is left untreated, it can lead to coma and death. Adrenal crisis can cause:
cardiac arrest: when the heart stops completely
stroke: when the blood supply to the brain is interrupted
hypovolemic shock: when severe blood and fluid loss means that
your heart cannot pump enough blood around your body
hypoxia: when the bodys tissues do not get enough oxygen
If any of organs or tissues, including brain, do not get enough oxygen, it can
cause permanent disability(an injury which impairs the physical and mental
ability of a person to perform normal work for the remainder of their life).33
11
CHAPTER III
CONCLUSION
Addisons disease is a rare autoimmune dissease, that occurs when the
adrenal glands do not produce enough of their hormones.1 Most of the cases in
Addisons disease is caused by autoimmune disease (about 80% of total cases),
less common causes include granulomatous disease (eg sarcoidosis, tuberculosis),
haematological malignancies, metastatic malignant disease, infiltrative metabolic
disease (eg amyloidosis), congenital adrenal hyperplasia, abdominal radiation and
the abrupt cessation of long-term steroid therapy. Those cases lead to destruction
or disfunction of entire adrenal cortex.
Deficiency of aldosterone causes hyponatremia, hyperkalemia, low plasma
volume, mild acidosis, and diarrhea. Deficiency of cortisol causes hypoglycemic,
weight loss, muscle weakness, loss of appetite, failure to react with stress, anemia,
and hyperpigmentation. Deficiency of adrenal androgen causes less significant
effects.
Treatment to decrease severity to the patient who are suffering from addison
disease including glucocorticoid replacement, mineralocorticoid replacement,
management of an adrenal crisis. Adrenal crisis is a medical emergency and must
be treated immediately. If it is left untreated, it can lead to coma and death.
Adrenal crisis can cause.
You might also like
- Simply Local Flaps.52Document1 pageSimply Local Flaps.52Steven GarcíaNo ratings yet
- VSim Packet Edith JacobsenDocument18 pagesVSim Packet Edith JacobsenRachael Moore100% (1)
- Pahtophysiology of EsrdDocument5 pagesPahtophysiology of EsrdCarl JardelezaNo ratings yet
- Pernicious AnemiaDocument24 pagesPernicious AnemiaArthadian De PeraltaNo ratings yet
- Buerger DiseaseDocument3 pagesBuerger DiseaseElmer DizonNo ratings yet
- Critical Care Medicine PDFDocument153 pagesCritical Care Medicine PDFRadovanNo ratings yet
- HemaDocument15 pagesHemauzbekistan143No ratings yet
- Minggu 5 LP THALASSEMIADocument14 pagesMinggu 5 LP THALASSEMIAMuhammad PanduNo ratings yet
- Cholecystitis Litiasis EctomyDocument23 pagesCholecystitis Litiasis EctomyTimothy WilliamsNo ratings yet
- NCP CvaDocument4 pagesNCP CvaMariquita BuenafeNo ratings yet
- Pathophysiology of HyperthyroidismDocument4 pagesPathophysiology of HyperthyroidismKitty YuffieNo ratings yet
- Case Report Non-infection Unit Β-Major ThalassemiaDocument27 pagesCase Report Non-infection Unit Β-Major ThalassemiaimamkdNo ratings yet
- EndometriosisDocument6 pagesEndometriosissalamredNo ratings yet
- CTC 2.18 Open-Angle Glaucoma PDFDocument29 pagesCTC 2.18 Open-Angle Glaucoma PDFNorvim LascanoNo ratings yet
- Case Press FinalDocument32 pagesCase Press FinalmadsoleNo ratings yet
- Sample Case Presentation - Occult BacteremiaDocument51 pagesSample Case Presentation - Occult BacteremiaPrecious Gutierrez BagazinNo ratings yet
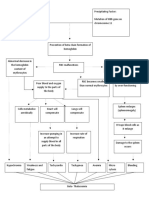
- Concept MapDocument2 pagesConcept Mapantherchio100% (2)
- Kawasaki DiseaseDocument7 pagesKawasaki DiseaseRitamariaNo ratings yet
- Diabetic Ketoacidosis: Albano, Bautista, Cimatu, Purificacion, SieteralesDocument84 pagesDiabetic Ketoacidosis: Albano, Bautista, Cimatu, Purificacion, SieteralesSyd BautistaNo ratings yet
- Obstructive Uropathy Secondary To Benign Prostatic HyperplasiaDocument74 pagesObstructive Uropathy Secondary To Benign Prostatic HyperplasiaGregory Litang100% (1)
- Beta ThalaDocument2 pagesBeta ThalaAngie LamoNo ratings yet
- Nontoxic Nodular GoiterDocument9 pagesNontoxic Nodular GoiterKayshey Christine ChuaNo ratings yet
- Lupus NephritisDocument15 pagesLupus NephritisVilza maharaniNo ratings yet
- NCP PlanningDecreased in Cardiac Output Related To Low Hemoglobin and Hematocrit CountDocument6 pagesNCP PlanningDecreased in Cardiac Output Related To Low Hemoglobin and Hematocrit CountMabelle SorianoNo ratings yet
- Hypertension in PregnancyDocument31 pagesHypertension in PregnancyradhabobbyNo ratings yet
- ThalassemiaDocument1 pageThalassemiaJobelle Fernandez-SantosNo ratings yet
- Post Cesarean Section DeliveryDocument5 pagesPost Cesarean Section Deliveryᒙᕧᖇᕦᙏᖻ ᗴᔛᓦᗩᖆᗩNo ratings yet
- Glasgow Coma ScaleDocument3 pagesGlasgow Coma Scaletoto11885No ratings yet
- Beta Thalassemia PathoDocument1 pageBeta Thalassemia PathoAngie LamoNo ratings yet
- Case Study OligoDocument7 pagesCase Study OligomutiaNo ratings yet
- Coma - Types, Causes, Treatments, PrognosisDocument3 pagesComa - Types, Causes, Treatments, PrognosisgcsNo ratings yet
- Post-Partum Hemorrhage Pathophysiology PaperDocument5 pagesPost-Partum Hemorrhage Pathophysiology Paperapi-399619969No ratings yet
- Small Bowel ObstructionDocument2 pagesSmall Bowel ObstructionSrividya PushpalaNo ratings yet
- Case Study Anemia-1Document6 pagesCase Study Anemia-1Melsya H UtamiNo ratings yet
- Case Pres A1-RhdDocument11 pagesCase Pres A1-RhdCharm TanyaNo ratings yet
- JDM Care PlanDocument5 pagesJDM Care PlangopscharanNo ratings yet
- Surgical Management For Cryptorchidism With Nursing ManagementsDocument4 pagesSurgical Management For Cryptorchidism With Nursing ManagementsAprille Claire MoralesNo ratings yet
- Case PresentationDocument50 pagesCase Presentationapi-19762967No ratings yet
- Case Study 1 (Muscular) - ALSDocument5 pagesCase Study 1 (Muscular) - ALSSamantha AquinoNo ratings yet
- GRP 20 Final Abscess Case StudyDocument14 pagesGRP 20 Final Abscess Case StudyBorja, Kimberly GraceNo ratings yet
- A Case Report On Multifetal PregnancyDocument5 pagesA Case Report On Multifetal PregnancyThreecee VelezNo ratings yet
- Jaundice NeonatalDocument26 pagesJaundice Neonatalhunk2662No ratings yet
- Assessment Nsg. Diagnosis Sci. Explanation Planning Intervention Rationale EvaluationDocument6 pagesAssessment Nsg. Diagnosis Sci. Explanation Planning Intervention Rationale EvaluationRoMarie AbainzaNo ratings yet
- Danger Signs of PregnancyDocument3 pagesDanger Signs of PregnancyNesly Khyrozz LorenzoNo ratings yet
- NCP GeDocument14 pagesNCP GeSuluhTriUtomoNo ratings yet
- Guada A. Dumapit RN, ManDocument18 pagesGuada A. Dumapit RN, ManAnne B. BuenvenidaNo ratings yet
- PathophysiologyDocument9 pagesPathophysiologySuzette PipoNo ratings yet
- Acute Cholecystitis SeminarDocument42 pagesAcute Cholecystitis SeminarNatnaelNo ratings yet
- Chest Pain.Document53 pagesChest Pain.Shimmering MoonNo ratings yet
- Live Preterm Baby Delivered NSDDocument13 pagesLive Preterm Baby Delivered NSDKristine Anne SorianoNo ratings yet
- Assignment On GCSDocument2 pagesAssignment On GCSPraty SawadenNo ratings yet
- Case (Acute Gastroenteritis) Group 4Document36 pagesCase (Acute Gastroenteritis) Group 4EljhayrosNo ratings yet
- Spontaneous AbortionDocument17 pagesSpontaneous Abortionanon_985338331No ratings yet
- Craniotomy or CraniectomyDocument14 pagesCraniotomy or CraniectomyEssaj Rosanat100% (2)
- Myasthenic Crisis Vs Cholinergic CrisisDocument1 pageMyasthenic Crisis Vs Cholinergic CrisisNicole VogelsbergNo ratings yet
- Acute Glomerulonephritis: Gordon Sara Sonnya Ayutthaya Novita Sari DewiDocument12 pagesAcute Glomerulonephritis: Gordon Sara Sonnya Ayutthaya Novita Sari DewiSara Sonnya Ayutthaya NapitupuluNo ratings yet
- Basilar Skull FractureDocument16 pagesBasilar Skull FractureRindahMDNo ratings yet
- Case Study On Toxic GoiterDocument5 pagesCase Study On Toxic GoiterRein EstradaNo ratings yet
- Model Nursing Care PlanDocument35 pagesModel Nursing Care PlanAnuchithra RadhakrishnanNo ratings yet
- Case Study Benign Tumors of The Uterus: MyomaDocument3 pagesCase Study Benign Tumors of The Uterus: MyomaToto RyanNo ratings yet
- Hirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandHirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Update On Prescribing in Pregnancy & Breastfeeding: DR Aman DurraniDocument42 pagesUpdate On Prescribing in Pregnancy & Breastfeeding: DR Aman DurraniKertiasihwayanNo ratings yet
- Binge Eating Disorder: Assessment and Treatment: Christina Wood Baker, PH.DDocument47 pagesBinge Eating Disorder: Assessment and Treatment: Christina Wood Baker, PH.DKertiasihwayanNo ratings yet
- CBT InsomniaDocument26 pagesCBT InsomniaKertiasihwayan100% (1)
- DR A.A.Ayu Meidiary, SPS: Department of Neurology, Sanglah General Hospital, Udayana University DenpasarDocument47 pagesDR A.A.Ayu Meidiary, SPS: Department of Neurology, Sanglah General Hospital, Udayana University DenpasarKertiasihwayanNo ratings yet
- NeuroimagingDocument47 pagesNeuroimagingKertiasihwayan100% (1)
- Vascular Dementia Alzheimer'S Dementia: A. LaksmidewiDocument46 pagesVascular Dementia Alzheimer'S Dementia: A. LaksmidewiKertiasihwayanNo ratings yet
- Febrile Seizure (Kejang Demam)Document25 pagesFebrile Seizure (Kejang Demam)KertiasihwayanNo ratings yet
- Anemia Defisiensi Asam FolatDocument15 pagesAnemia Defisiensi Asam FolatKertiasihwayanNo ratings yet
- Fibroadenoma PDFDocument2 pagesFibroadenoma PDFAthika Dwi Sofiana100% (1)
- Drug Provocation Test, Tes Provokasi ObatDocument12 pagesDrug Provocation Test, Tes Provokasi ObatKertiasihwayanNo ratings yet
- Case Presentation DengueDocument3 pagesCase Presentation DengueLindel Assley Turqueza100% (1)
- Nested and Swaddled Positioning Support in The Prone Position Facilitates Sleep and Heart Rate Stability in Very Low Birth Weight InfantsDocument4 pagesNested and Swaddled Positioning Support in The Prone Position Facilitates Sleep and Heart Rate Stability in Very Low Birth Weight InfantsRama AfandiNo ratings yet
- 4 6012518666061482070 PDFDocument347 pages4 6012518666061482070 PDFKhushboo Rana A Scientist100% (1)
- Case Report PresentationDocument41 pagesCase Report PresentationlukitaniningNo ratings yet
- Circulatory System Word FindDocument1 pageCirculatory System Word FindZac McGillNo ratings yet
- HB 6617 - Philippine HIV and AIDS Policy Act (Substitute Bill - Approved On SECOND READING)Document24 pagesHB 6617 - Philippine HIV and AIDS Policy Act (Substitute Bill - Approved On SECOND READING)Rappler100% (2)
- Preventing Hospital Infections Real World Problems Realistic Solutions 2Nd Edition Jennifer Meddings Download PDF ChapterDocument52 pagesPreventing Hospital Infections Real World Problems Realistic Solutions 2Nd Edition Jennifer Meddings Download PDF Chaptermary.schoonmaker770100% (11)
- Subjective and Objective DataDocument9 pagesSubjective and Objective DatagraceNo ratings yet
- Neuroendocrine TumorsDocument21 pagesNeuroendocrine TumorsAnonymous 8KN8IR1GTWNo ratings yet
- A New Treatment For Severe Burn and Post Traumatic Scars A Preliminary Report Treatment Strategies Dermatology Volume 2 Issue 2Document5 pagesA New Treatment For Severe Burn and Post Traumatic Scars A Preliminary Report Treatment Strategies Dermatology Volume 2 Issue 2TAZZ150002No ratings yet
- New Defmition Medicine: 'Neo-Islamic Medicine'Document2 pagesNew Defmition Medicine: 'Neo-Islamic Medicine'Meity ElvinaNo ratings yet
- 6th Semester 2nd BatchDocument20 pages6th Semester 2nd BatchKhushboo AliNo ratings yet
- Levels of Prevention (Leavell & Clark)Document10 pagesLevels of Prevention (Leavell & Clark)Ta RaNo ratings yet
- Salmonella Infections: (Salmonelloses)Document56 pagesSalmonella Infections: (Salmonelloses)andualemNo ratings yet
- Components of The CBCDocument8 pagesComponents of The CBCapi-236078478No ratings yet
- PCEP-PC Module 2 Slides and Key PointsDocument10 pagesPCEP-PC Module 2 Slides and Key PointsMan MedNo ratings yet
- Germany Health Benefits SummaryDocument6 pagesGermany Health Benefits Summarytracy leeNo ratings yet
- Peritoneal Dialysis Procedure: Amy Neufeldt, RN, BSCN, William J. Lawton, Md. July 2015 Mbingo Baptist HospitalDocument5 pagesPeritoneal Dialysis Procedure: Amy Neufeldt, RN, BSCN, William J. Lawton, Md. July 2015 Mbingo Baptist HospitalSapna thakurNo ratings yet
- Episode 221 Hy Trauma - mp3Document11 pagesEpisode 221 Hy Trauma - mp3sssddasfdsds dssfdNo ratings yet
- Essential List On 5th November 2022Document9 pagesEssential List On 5th November 2022AFI FARMANo ratings yet
- Check - List - Form - No - 2 - Registration of Imported - MedicinesDocument1 pageCheck - List - Form - No - 2 - Registration of Imported - Medicines박지원No ratings yet
- Exercise 2: Venipuncture Using Vacuum Collection System: ObjectivesDocument28 pagesExercise 2: Venipuncture Using Vacuum Collection System: ObjectivesFrieda CayabyabNo ratings yet
- Chorea Approach PDFDocument1 pageChorea Approach PDFdrsushmakNo ratings yet
- House MD Season 1 - Everybody LiesDocument2 pagesHouse MD Season 1 - Everybody LiesMelea Kristine RosalNo ratings yet
- 1912-Article Text-5592-1-10-20220729Document9 pages1912-Article Text-5592-1-10-20220729Xyaraz LarasaNo ratings yet
- Assessment Diagnosis Planning Nursing Intervention Rationale EvaluationDocument4 pagesAssessment Diagnosis Planning Nursing Intervention Rationale Evaluationcharles estradaNo ratings yet