Professional Documents
Culture Documents
Time Course of Elevations in Plasma Olprinone Concentration During Pediatric Cardiac Surgery
Time Course of Elevations in Plasma Olprinone Concentration During Pediatric Cardiac Surgery
Uploaded by
Fika Khulma SofiaCopyright:
Available Formats
You might also like
- ATLS Practice Test 3 Answers & ExplanationsDocument10 pagesATLS Practice Test 3 Answers & ExplanationsCarl Sars50% (2)
- Five Level TriageDocument2 pagesFive Level TriageHarold Haze Cortez100% (4)
- AHA-PALS 2010: Pediatric Chain of SurvivalDocument10 pagesAHA-PALS 2010: Pediatric Chain of SurvivalIsabel CastilloNo ratings yet
- Dubin ECG Reference SheetsDocument13 pagesDubin ECG Reference SheetsEllie100% (1)
- 1 s2.0 S1110184913000639 MainDocument8 pages1 s2.0 S1110184913000639 MainRolando Juan Dávila SalcedoNo ratings yet
- 1 s2.0 S1110184913000639 MainDocument8 pages1 s2.0 S1110184913000639 MainRolando Juan Dávila SalcedoNo ratings yet
- Evaluation of Propofol Anesthesia in Morbidly Obese Children and AdolescentsDocument9 pagesEvaluation of Propofol Anesthesia in Morbidly Obese Children and AdolescentsDebi SumarliNo ratings yet
- ClonidineDocument4 pagesClonidineDR RAVI ANANDNo ratings yet
- J Neurol Neurosurg Psychiatry 1981 Young 323 8Document7 pagesJ Neurol Neurosurg Psychiatry 1981 Young 323 8Ian BoydNo ratings yet
- Vent AvisDocument9 pagesVent AvisArini NurlelaNo ratings yet
- Downloaded File-195Document6 pagesDownloaded File-195Abdul RachmanNo ratings yet
- Vranish 2016Document7 pagesVranish 2016Jenifer de OliveiraNo ratings yet
- Ağrısız Gastroskopi Sırasında Anestezi Indüksiyonunda Bireyselleştirilmiş Optimal Hedef Konsantrasyonu Hesaplamak Için Bir Gösterge Olarak Kirpik Refleksini Kullanmanın Uygulanabilirliğini Araştırmak.Document4 pagesAğrısız Gastroskopi Sırasında Anestezi Indüksiyonunda Bireyselleştirilmiş Optimal Hedef Konsantrasyonu Hesaplamak Için Bir Gösterge Olarak Kirpik Refleksini Kullanmanın Uygulanabilirliğini Araştırmak.Ali ÖzdemirNo ratings yet
- Articulo 3Document6 pagesArticulo 3Raul Soto FigueroaNo ratings yet
- Farmacology Del Paro CardiacoDocument14 pagesFarmacology Del Paro CardiacoNicoSwtifNo ratings yet
- Thrombolysis With Alteplase 3 To 4.5 Hours After Acute Ischemic StrokeDocument4 pagesThrombolysis With Alteplase 3 To 4.5 Hours After Acute Ischemic StrokeSalma Asri NovaNo ratings yet
- 17TOHJDocument4 pages17TOHJAriffa DiazNo ratings yet
- Jurnal GenerghjfgjyjhvjhgjfjdjmhfjmDocument5 pagesJurnal GenerghjfgjyjhvjhgjfjdjmhfjmH'Cham AchmadNo ratings yet
- Kang 2018Document20 pagesKang 2018Elisabeth EstellaNo ratings yet
- Pulmonary Pharmacology & TherapeuticsDocument5 pagesPulmonary Pharmacology & TherapeuticsClaudia SofroniaNo ratings yet
- 2010 BR J Anaesth Propofol PK Obese CortinezDocument9 pages2010 BR J Anaesth Propofol PK Obese CortinezmiguelzapienNo ratings yet
- New Evidence in Home Mechanical Ventilation: Thematic Poster Session Hall 2-4 - 12:50-14:40Document5 pagesNew Evidence in Home Mechanical Ventilation: Thematic Poster Session Hall 2-4 - 12:50-14:40Shirley CoelhoNo ratings yet
- Efficacy of Hyperventilation, Blood Pressure Elevation, and Metabolic Suppression Therapy in Controlling Intracranial Pressure After Head InjuryDocument9 pagesEfficacy of Hyperventilation, Blood Pressure Elevation, and Metabolic Suppression Therapy in Controlling Intracranial Pressure After Head InjuryAik NoeraNo ratings yet
- Conversion To Everolimus in Maintenance Patients-Current Clinical StrategiesDocument6 pagesConversion To Everolimus in Maintenance Patients-Current Clinical StrategieshassanNo ratings yet
- Jurnal AnestesiDocument8 pagesJurnal AnestesiapriiiiiiilllNo ratings yet
- Jimbo 2017Document15 pagesJimbo 2017Sahily MoralesNo ratings yet
- The Analgesic Efficacy of Tramadol As A Pre-Emptive Analgesic in Pediatric Appendectomy Patients PDFDocument6 pagesThe Analgesic Efficacy of Tramadol As A Pre-Emptive Analgesic in Pediatric Appendectomy Patients PDFUmmu Qonitah AfnidawatiNo ratings yet
- The Use of Sildenafil in Persistent Pulmonary Hypertension of The Newborn PDFDocument6 pagesThe Use of Sildenafil in Persistent Pulmonary Hypertension of The Newborn PDFmaciasdrNo ratings yet
- Overview of Total Intravenous Anesthesia in ChildrenDocument12 pagesOverview of Total Intravenous Anesthesia in ChildrenJosibel OcantoNo ratings yet
- Tatalaksana PJBDocument5 pagesTatalaksana PJBmayaNo ratings yet
- Efek Clon & Magnes PDFDocument5 pagesEfek Clon & Magnes PDFDisi Muhaymin RNo ratings yet
- Phenylephrine For Blood Pressure Control in Elective Cesarean Section: Therapeutic Versus Prophylactic DosesDocument8 pagesPhenylephrine For Blood Pressure Control in Elective Cesarean Section: Therapeutic Versus Prophylactic DosesPalwasha MalikNo ratings yet
- Yilmaz 2018Document18 pagesYilmaz 2018Hassler Barrios AcostaNo ratings yet
- KJAEDocument7 pagesKJAEM Wahyu UtomoNo ratings yet
- Ob 7Document22 pagesOb 7William OmarNo ratings yet
- Clinical StudyDocument7 pagesClinical StudyJonathan MarkNo ratings yet
- Comparison of Ondansetron, Cyclizine and Prochlorperazine For PONV Prophylaxis in Laparoscopic CholecystectomyDocument5 pagesComparison of Ondansetron, Cyclizine and Prochlorperazine For PONV Prophylaxis in Laparoscopic CholecystectomynikimahhNo ratings yet
- En V60n4a06Document5 pagesEn V60n4a06Palwasha MalikNo ratings yet
- 1 s2.0 S2531043718301107 MainDocument8 pages1 s2.0 S2531043718301107 MainCraniolyne RefianNo ratings yet
- Revista Brasileira DE AnestesiologiaDocument9 pagesRevista Brasileira DE AnestesiologiayulianiNo ratings yet
- Undiagnosed Abdominal Paraganglioma: An Anaesthetic ChallengeDocument3 pagesUndiagnosed Abdominal Paraganglioma: An Anaesthetic ChallengeAde Gustina SiahaanNo ratings yet
- Critical Care CasesDocument7 pagesCritical Care CasesJude Micko Bunyi AlipitNo ratings yet
- Randomized Clinical Trial Investigating The Stress Response From Two Different Methods of Analgesia After Laparoscopic Colorectal SurgeryDocument7 pagesRandomized Clinical Trial Investigating The Stress Response From Two Different Methods of Analgesia After Laparoscopic Colorectal Surgeryvalerio.messinaNo ratings yet
- Inhaled Vasodilators As Salvage Therapy in ARDS Caused by H1N1 InfectionDocument5 pagesInhaled Vasodilators As Salvage Therapy in ARDS Caused by H1N1 InfectiondarmariantoNo ratings yet
- Research ArticleDocument7 pagesResearch Articlenaljnaby9No ratings yet
- Bauch-Atrial Natriuretic Peptide As A MarDocument6 pagesBauch-Atrial Natriuretic Peptide As A MarSzendeNo ratings yet
- SSRN Id3666867Document18 pagesSSRN Id3666867Douglas SantosNo ratings yet
- JurnalDocument6 pagesJurnalFitri Aesthetic centerNo ratings yet
- Paper Title: (16 Bold Blue Color)Document9 pagesPaper Title: (16 Bold Blue Color)Fauzi RusdiantoNo ratings yet
- Introduction: Intravenous Ibuprofen May Offer Advantages Over Ketorolac For Postoperative Pain ControlDocument6 pagesIntroduction: Intravenous Ibuprofen May Offer Advantages Over Ketorolac For Postoperative Pain ControlnadaNo ratings yet
- The Hemodynamic Effects of Propofol in Children With Congenital Heart DiseaseDocument6 pagesThe Hemodynamic Effects of Propofol in Children With Congenital Heart DiseaseAngelica Lucero OrtizNo ratings yet
- ARTIGO1Document9 pagesARTIGO1jtnylsonNo ratings yet
- Prompt Prediction of Fibrinogen Concentration During Cardiopulmonary BypassDocument8 pagesPrompt Prediction of Fibrinogen Concentration During Cardiopulmonary Bypassjuajimenez55No ratings yet
- Original Article: Ayesha Goyal, P. Shankaranarayan, P. GanapathiDocument6 pagesOriginal Article: Ayesha Goyal, P. Shankaranarayan, P. GanapathiAnonymous S0H8cqgnfiNo ratings yet
- Research ArticleDocument9 pagesResearch ArticleM RifkiNo ratings yet
- Research Article: Evaluation of Pre and Post Bronchodilator Pulmonary Function Test in Fifty Healthy VolunteersDocument8 pagesResearch Article: Evaluation of Pre and Post Bronchodilator Pulmonary Function Test in Fifty Healthy VolunteersEarthjournal PublisherNo ratings yet
- Guidelines Adult Advanced Life SupportDocument34 pagesGuidelines Adult Advanced Life SupportParvathy R NairNo ratings yet
- Variability of Residual Platelet Function Despite Clopidogrel Treatment in Patients With Peripheral Arterial Occlusive DiseaseDocument6 pagesVariability of Residual Platelet Function Despite Clopidogrel Treatment in Patients With Peripheral Arterial Occlusive DiseaseGono GenieNo ratings yet
- Universitas Indonesia: U. Weber, M. Krammel, S. Linke, T. Hamp, T. Stimpfl, B. Reiter, W. PlӧchlDocument8 pagesUniversitas Indonesia: U. Weber, M. Krammel, S. Linke, T. Hamp, T. Stimpfl, B. Reiter, W. PlӧchlgoldenNo ratings yet
- 1 s2.0 S0959804912009239 MainDocument10 pages1 s2.0 S0959804912009239 MainMarcel PopaNo ratings yet
- A Comparison of Hemodynamic Changes During Laryngoscopy and Endotracheal Intubation by Using Three Modalities of Anesthesia InductionDocument5 pagesA Comparison of Hemodynamic Changes During Laryngoscopy and Endotracheal Intubation by Using Three Modalities of Anesthesia Inductionammaa_No ratings yet
- Paper TemplateDocument10 pagesPaper Templatenur hidayatNo ratings yet
- 08 PDFDocument6 pages08 PDFintan kusumaningtyasNo ratings yet
- Essentials in Lung TransplantationFrom EverandEssentials in Lung TransplantationAllan R. GlanvilleNo ratings yet
- Morning Report Februari 2016: A 36-Year-Old-Man With Moderate Acute Asthma DD Acis DD CopdDocument14 pagesMorning Report Februari 2016: A 36-Year-Old-Man With Moderate Acute Asthma DD Acis DD CopdFika Khulma SofiaNo ratings yet
- InTech - Mechanisms in Erectile Function and Dysfunction An OverviewDocument21 pagesInTech - Mechanisms in Erectile Function and Dysfunction An OverviewFika Khulma SofiaNo ratings yet
- Interpreting D DimerDocument8 pagesInterpreting D DimerFika Khulma SofiaNo ratings yet
- Cardioplegia in Pediatric Cardiac Surgery: Do We Believe in Magic?Document12 pagesCardioplegia in Pediatric Cardiac Surgery: Do We Believe in Magic?Fika Khulma SofiaNo ratings yet
- Abstrak DR SariDocument2 pagesAbstrak DR SariFika Khulma SofiaNo ratings yet
- Venous Air Embolism During Anterior Lumbar Surgery: Case ReportDocument3 pagesVenous Air Embolism During Anterior Lumbar Surgery: Case ReportFika Khulma SofiaNo ratings yet
- Incidence of Venous Air Embolism During Craniectomy For Craniosynostosis RepairDocument4 pagesIncidence of Venous Air Embolism During Craniectomy For Craniosynostosis RepairFika Khulma SofiaNo ratings yet
- Physician. 2011 May 1 83 (9) :1078-1084Document4 pagesPhysician. 2011 May 1 83 (9) :1078-1084Fika Khulma SofiaNo ratings yet
- Practice Essentials: Essential Update: Chemotherapy Following Radiation May Improve Survival in Low-Grade GliomasDocument19 pagesPractice Essentials: Essential Update: Chemotherapy Following Radiation May Improve Survival in Low-Grade GliomasFika Khulma SofiaNo ratings yet
- Imaging Features of Primary Breast SarcomaDocument8 pagesImaging Features of Primary Breast SarcomaFika Khulma SofiaNo ratings yet
- Vestibular Neutitis & Labyrinthitis PDFDocument6 pagesVestibular Neutitis & Labyrinthitis PDFFika Khulma SofiaNo ratings yet
- Ga Kebaca (Blabla)Document5 pagesGa Kebaca (Blabla)Fika Khulma SofiaNo ratings yet
- Jenis Pemeriksaan 4/5 6/5 7/5 Nilai Rujukan Satuan Hematologi Rutin 9.6 29 16.7Document2 pagesJenis Pemeriksaan 4/5 6/5 7/5 Nilai Rujukan Satuan Hematologi Rutin 9.6 29 16.7Fika Khulma SofiaNo ratings yet
- ORAL DIAG Q&A DentistryDocument46 pagesORAL DIAG Q&A DentistryTJ OberioNo ratings yet
- Necropsy Guide For Dogs Cats and Small Mammals - 2016 - McDonough - Appendix 4 Describing Gross LesionsDocument2 pagesNecropsy Guide For Dogs Cats and Small Mammals - 2016 - McDonough - Appendix 4 Describing Gross Lesionsimmanuel1111No ratings yet
- ShockDocument30 pagesShockvinnu kalyanNo ratings yet
- Blood Supply of The BrainDocument32 pagesBlood Supply of The BrainShimmering MoonNo ratings yet
- Iap CprdayDocument33 pagesIap CprdayRabi KumarNo ratings yet
- Cardiology SoalDocument9 pagesCardiology Soalanz_4191No ratings yet
- Parathyroid, HyperparathyroidismDocument4 pagesParathyroid, Hyperparathyroidismjamil aoudeNo ratings yet
- CVD Case StudyDocument23 pagesCVD Case StudyMsRhyxelle80% (5)
- Adrenergic NeurotransmittersDocument18 pagesAdrenergic Neurotransmittersparmarkeval1610No ratings yet
- TCHP Shock Series Part 2Document2 pagesTCHP Shock Series Part 2ikeernawatiNo ratings yet
- Osteoporosis & OsteomalaciaDocument29 pagesOsteoporosis & OsteomalaciaKeith OmwoyoNo ratings yet
- HipertenziaDocument2 pagesHipertenziaAfiya MohammedNo ratings yet
- Edmodo Quiz As Biology Topic 1 Cardiac Cycle1Document2 pagesEdmodo Quiz As Biology Topic 1 Cardiac Cycle1Arun NandhaNo ratings yet
- ALS Manual 2010.version 1Document84 pagesALS Manual 2010.version 1Elena How100% (1)
- NP 3. Compiled QuestionsDocument43 pagesNP 3. Compiled QuestionsAzurin JewelNo ratings yet
- Science TriviaDocument5 pagesScience TriviaasserenanoyagNo ratings yet
- Class 10 TransportationDocument5 pagesClass 10 TransportationKanishk KumarNo ratings yet
- Pedriatrics 6th YearDocument50 pagesPedriatrics 6th YearKimira GoundenNo ratings yet
- Pre Medical Evaluatiom Form PFT 1 PDFDocument2 pagesPre Medical Evaluatiom Form PFT 1 PDFAIEN WENDELEIH Q. CAPINPIN100% (2)
- SGOT (Aspartate Aminotransferase, AST, Glutamic Oxaloacetic Transaminase)Document9 pagesSGOT (Aspartate Aminotransferase, AST, Glutamic Oxaloacetic Transaminase)Reman A. AlingasaNo ratings yet
- Urinary SystemDocument6 pagesUrinary SystemKids JangNo ratings yet
- 心血管外科、胸外科专业术语 (名词) 汉英对照Document13 pages心血管外科、胸外科专业术语 (名词) 汉英对照Ted TsieNo ratings yet
- UntitledDocument48 pagesUntitledSamad MaqsoodNo ratings yet
- Introduction To Human Anatomy and PhysiologyDocument42 pagesIntroduction To Human Anatomy and PhysiologyDump Acc 2100% (1)
- Drug Study LCPDocument3 pagesDrug Study LCPalleen_viaNo ratings yet
- Ebook Textbook of Radiology and Imaging Vol 2 PDF Full Chapter PDFDocument54 pagesEbook Textbook of Radiology and Imaging Vol 2 PDF Full Chapter PDFdorothy.cook305100% (35)
Time Course of Elevations in Plasma Olprinone Concentration During Pediatric Cardiac Surgery
Time Course of Elevations in Plasma Olprinone Concentration During Pediatric Cardiac Surgery
Uploaded by
Fika Khulma SofiaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Time Course of Elevations in Plasma Olprinone Concentration During Pediatric Cardiac Surgery
Time Course of Elevations in Plasma Olprinone Concentration During Pediatric Cardiac Surgery
Uploaded by
Fika Khulma SofiaCopyright:
Available Formats
Open Journal of Anesthesiology, 2013, 3, 80-83
http://dx.doi.org/10.4236/ojanes.2013.32020 Published Online March 2013 (http://www.scirp.org/journal/ojanes)
Time Course of Elevations in Plasma Olprinone
Concentration during Pediatric Cardiac Surgery
Satoshi Kurokawa, Minoru Nomura
Department of Anesthesiology, Faculty of Medicine, Tokyo Womens Medical University, Tokyo, Japan.
Email: satokuro@sea.plala.or.jp
Received January 10th, 2013; revised February 15th, 2013; accepted March 2nd, 2013
ABSTRACT
Purpose: Little research has been reported to date on the usefulness of olprinone in pediatric cardiac surgery, and no
standard pediatric infusion protocol is currently established. Our study sought to confirm that the regimen described
herein rapidly achieves the requisite plasma olprinone concentrations. Methods: For the purposes of our study, we enrolled 13 patients: 7 biventricular repair candidates and 6 Fontan-type operation candidates. We administered a continuous infusion of olprinone to our study subjects at 0.3 g/kg/min with no loading dose starting approximately 30
minutes (min) before weaning from cardiopulmonary bypass (CPB). We performed blood sampling at 15, 30, 45, 60, 90,
and 120 min after the start of infusion and at the same elapsed intervals after separation from CPB. We measured
plasma olprinone concentrations using ultra-fast liquid chromatography. Results: We observed effective plasma olprinone concentrations (>20 ng/ml) at 30 min after weaning from CPB, or at 60 min after the start of infusion. Conclusion:
We conclude that continuous olprinone infusion at 0.3 g/kg/min without a loading dose initiated immediately after the
release of aortic cross-clamping or immediately after the completion of all surgical procedures quickly and reliably
achieves effective plasma concentrations.
Keywords: Olprinone; Phosphodiesterase-3 Inhibitor; Plasma Concentration; Pediatric Cardiac Surgery;
Weaning from Cardio-Pulmonary Bypass
1. Introduction
The effects of milrinone on hemodynamics and outcomes
in pediatric cardiac surgery have been extensively investigated. A large multi-center study in North America (the
PRIMACORP study) demonstrated high-dose milrinone
significantly reduced mortality or the incidence of low
cardiac output syndrome (LOS) after pediatric cardiac
surgery and that even low-dose milrinone likewise tended to reduce mortality or LOS development, although
low-dose results failed to reach statistically significant
levels [1]. Milrinone is now widely administered to patients with congenital heart disease.
Olprinone is a phosphodiesterase-3 (PDE-3) inhibitor
developed and commercially available in Japan since
1996. Several studies involving adults show olprinone
reduces SVR and increases CI significantly during or
after cardiac surgery, including coronary artery bypass
graft or valve surgery [2-5]. However, the manner of administration has differed from study to study, and no
standard protocol has been established. In contrast to
milrinone, little data on olprinone is available at this time,
data on use during pediatric cardiac surgery in particular.
Even optimal regimens for achieving effective blood
Copyright 2013 SciRes.
concentrations remain uncertain. Our study sought to
confirm that our infusion method rapidly achieves effective blood concentrations on weaning from CPB during
pediatric cardiac surgery.
2. Methods
2.1. Materials
After local ethics committee approval and informed parental consent, 13 pediatric patients enrolled in this study
underwent cardiac surgery under CPB at Tokyo Womens Medical University Hospital from March 2009 to
September 2009. Our policies call for administering
PDE-3 inhibitors in patients with congestive heart failure
or pulmonary hypertension preoperatively and in patients
regarded to be at high risk of LOS post-operatively. We
selected these 13 patients at random from candidates for
PDE-3 inhibitor administration by having the attending
anesthesiologist (a study member but not a study coordinator) draw a hidden card for each patient. These cards
were either blank or bore a red mark for olprinone infusion. If a blank card was drawn, the patient was given
milrinone. The group of 13 subjects administered olprinone included 7 candidates for biventricular repair and 6
OJAnes
81
Time Course of Elevations in Plasma Olprinone Concentration during Pediatric Cardiac Surgery
candidates for Fontan-type operation.
Table 1. Data on patient demographics.
Patients administered olprinone (n = 13)
2.2. Olprinone Infusion
We initiated olprinone infusion at 0.3 g/kg/min with no
loading dose immediately after the release of aortic
cross-clamping. In cases not involving aortic crossclamping, we began the infusion immediately after all
surgical procedures had been completed. The study rules
did not prevent the concurrent infusion of other cardiovascular active drugs (i.e., inotropes or vasodilators). The
selection and infusion doses of such agents were generally left to the discretion of the attending anesthesiologists.
2.3. Plasma Olprinone Concentrations
We sampled blood to measure plasma olprinone concentrations at 15, 30, 60, 90, and 120 minutes (min) after the
start of infusion and at the same elapsed intervals after
separation from CPB. We collected 2 ml of plasma of
each sample after centrifuging whole blood samples. We
then measured plasma olprinone concentrations using ultra-fast liquid chromatography (UFLC) with a spectrofluorometric detector (Shimadzu, Kyoto, Japan). We assessed excitation/emission at 335/400 nm. The UFLC
samples were prepared by extraction using ethyl acetate
with milrinone as the internal standard (IS). We separated olprinone with a Shim-pack XR-ODS column (3.0
mm i.d. 100 mm) with a mobile phase consisting of 10
mmol/liter phosphoric acid solution and acetonitrile
(88:12, v/v) adjusted to pH 7.0. The analysis was performed at a column temperature of 25C. Retention times
were 8.0 min for olprinone and 5.5 min for IS. The lowest limit of quantification was 5.0 ng/ml.
3. Results
3.1. Demographic Data for Study Subjects
Table 1 summarizes the demographic data for the study
subjects. Data are given as median with the range in parentheses.
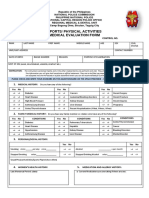
3.2. Elevated Plasma Olprinone Concentrations
We successfully measured plasma olprinone concentrations for all 13 patients. Figure 1 illustrates the changes
in plasma olprinone concentrations. The effective plasma
concentration (>20 ng/ml) was achieved from 30 min
after separation from CPB (Figure 1(a)). After dividing
the patients into three groups based on the time elapsed
from initiation of infusion to separation from CPB, we
found concentrations elevated above the effective concentration by 60 min after separation from CPB, even in
patients with times of less than 30 min (Figure 1(b)).
Copyright 2013 SciRes.
Age (mo)
21 (4 - 48)
Gender (M/F)
6/7
BW (kg)
12.0 (4.6 - 15.3)
Diagnosis
VSD with PH 3, CoA complex after PAB 1,
ASD with PS 1, TOF 2, SRV 3, TA 2, PPA 1
Operation
VSD closure 4, TOF correction 2, ASD
closure with RVOTR 1, BDG 2, TCPC 4
mo: months old. M: male. F: female. BW: body weight. VSD: ventricular
septal defect. PH: pulmonary hypertension. CoA: coarctation of aorta. PAB:
pulmonary artery banding. ASD: atrial septal defect. PS: pulmonary stenosis.
TOF: tetralogy of Fallot. SRV: single right ventricle. TA: tricuspid atresia,
PPA: pure pulmonary atresia. RVOTR: right ventricular outflow tract reconstruction. BDG: bidirectional Glenn anastomosis. TCPC: total cavopulmonary connection.
With respect to time after start of infusion, we achieved effective concentrations starting 60 min after infusion began (Figure 1(c)).
3.3. Side Effects
We observed no signs of hypotension or arrhythmia with
suspicious causal relationship to olprinone administration,
for the duration for which the patient was administered
olprinone.
4. Discussion
To the best of our knowledge, this study is the first to
demonstrate the time course of elevations in plasma olprinone concentration after the start of infusion at weaning from CPB in pediatric cardiac surgery cases. The
study results showed that our infusion protocol achieved
effective plasma concentrations quite rapidly, within 30
min after weaning from CPB.
The infusion procedures used in other studies have
varied from study to study, and several of these studies
have measured and reported blood concentrations. In the
adults described in the studies reported to date, a loading
dose of 15 g/kg followed by continuous infusion at 0.1
g/kg/min achieved effective blood concentrations
within 5 min after weaning from CPB [3], while continuous infusion at 0.1 to 0.2 g/kg/min without a loading dose took 1.5 to 2 hours [5,6]. A study involving
children showed that a bolus injection of 50 g/kg produced elevations above the effective blood concentration
within 30 min after weaning from CPB [7]. Another
study confirmed levels above the effective blood concentration at 120 minutes after the initiation of continuous
infusion at 0.4 g/kg/min in ICU following pediatric cardiac surgery in all study subjects [8]. In two other studies
that did not measure plasma olprinone concentrations in
adult cardiac surgery cases, continuous infusion doses
OJAnes
82
Time Course of Elevations in Plasma Olprinone Concentration during Pediatric Cardiac Surgery
(a)
not seek to achieve effective blood concentrations of olprinone at or before the discontinuation of CPB; rather,
our goal was simply to achieve the effective concentration shortly after separation from CPB, generally within
60 min, thereby minimizing the risk of unwanted side
effects. Given these goals, we eschewed a loading dose
and high-dose infusions exceeding 0.3 g/ kg/min. Ultimately, our infusion procedurecontinuous infusion at
0.3 g/kg/min without a loading dose after aortic clamp
release or completion of the surgical procedureachieved effective blood concentrations within just 30 min
after weaning from CPB. Our data strongly supports the
notion that the infusion procedure applied in this study is
reasonable and adequate for rapidly achieving effective
blood concentrations.
Limitations
(b)
(c)
Figure 1. Time course of elevations in plasma olprinone
concentration. We observed effective plasma concentrations
(>20 ng/ml) starting 30 minutes (min) after separation from
CPB (Figure 1(a)). Even in patients for whom the time
elapsed from initiation of infusion to separation from CPB
was less than 30 min, concentrations reached or exceeded
the effective concentration at 60 min after separation from
CPB (Figure 1(b)). With respect to the time from initiation
of infusion, the effective concentration was achieved from
60 min after initiation of the infusion (Figure 1(c)).
ranged from 0.05 to 0.3 g/kg/min, whether or not a
loading dose was administered [2,9]. Both studies confirmed that olprinone infusion at 0.1 or 0.3 g/kg/min
achieved clinical hemodynamic stability: namely, significant tapering of concomitantly administered catecholamines [9] or significant increase in the cardiac index with
reduced systemic vascular resistance [2]. Although a
loading dose may assure effective blood concentrations
following discontinuation of CPB, it also poses certain
potential disadvantages, including the risk of BP depletion requiring noradrenaline administration [3]. We did
Copyright 2013 SciRes.
Our study is subject to several limitations. First, to our
knowledge, no study has been performed to date to determine the effective concentration of olprinone in children. Two earlier studies describing blood concentrations
of olprinone in children have simply extrapolated an effective concentration from those for adults. We applied
the same procedure in our study. Second, the sample size
was small, and the study subjects varied significantly in
several potentially important parameters, including age,
diagnosis, pathophysiology, and severity of illness. Moreover, the extent and duration of various surgical insults,
including time required for the surgical procedure, CPB
time, and aortic cross-clamping time, differed from case
to case. Some of these factors may affect the pharmacokinetics of olprinone. In the case of milrinone, Bailey
et al. report that whereas CPB did not significantly alter
the pharmacokinetics of milrinone in adults [10], certain
pharmacokinetic parameterscompartment volume and
clearance in the third compartment in particularexhibited wide inter-individual variations in children aged 3 to
22 months undergoing cardiac surgery [11]. Ramamoorthy et al. have shown that milrinone does not bind to
CPB circuits and that infants (<1 year) had small clearance compared to children (>1 year), despite similar distribution volumes [12]. Ideally, a study characterized by
a small sample size would control for such factors. Further studies of pharmacokinetics and the effects on circulation and oxygen delivery are needed to establish optimal olprinone infusion protocols.
In summary, the results of our study indicate our olprinone infusion procedurecontinuous infusion at 0.3
g/kg/minrapidly and reliably achieved effective plasma concentrations.
5. Acknowledgements
We wish to thank Professor Kazuyuki Ueno at the Niigata University of Pharmacy and Applied Life Sciences,
OJAnes
Time Course of Elevations in Plasma Olprinone Concentration during Pediatric Cardiac Surgery
tery Bypass Grafting (in Japanese with English Abstract), Masui (The Japanese Journal of Anesthesiology),
Vol. 55, No. 2, 2006, pp. 158-163.
Faculty of Pharmacy, for assistance with measurements
of olprinone plasma concentrations.
[7]
T. M. Hoffman, G. Wernovsky, A. M. Atz, T. J. Kulik, N.
D. P. Nelson, A. C. Chang, et al., Efficacy and Safety of
Milrinone in Preventing Low Cardiac Output Syndrome
in Infants and Children after Corrective Surgery for Congenital Heart Disease, Circulation, Vol. 107, No. 7,
2003, pp. 996-1002.
doi:10.1161/01.CIR.0000051365.81920.28
M. Itou, H. Okamoto, J. Suwa, T. Asou and S. Hoka, Application of a PDE-3 Inhibitor, Olprinone, for Fast Track
Pediatric Cardiac Surgery (in Japanese with English Abstract), Masui (The Japanese Journal of Anesthesiology),
Vol. 53, No. 3, 2004, pp. 258-263.
[8]
Y. Orime, M. Shiono, H. Hata, S. Yagi, S. Tsukamoto, S.
Kimura, et al., Post-Operative Effects of Olprinone after
Coronary Artery Bypass Grafting, Annals of Thoracic
and Cardiovascular Surgery, Vol. 4, No. 6, 1998, pp. 340346.
T. Iwasaki, Y. Toda, K. Shimizu, K. Suzuki, T. Kanazawa
and K. Morita, Hemodynamic Effects of Phosphodiesterase-3 Inhibitors, Olprinone and Milrinone after Open
Heart Surgery in Child of Congenital Heart Disease,
Anesthesia & Analgesia, Vol. 106, No. S1, 2008, pp. 1128.
[9]
K. Sha, M. Iwata, M. Mori, Y. Motozu, N. Yonemoto, K.
Kitaguchi, et al., Evaluation of the Different Doses of
Olprinone for Continuous Infusion after Cardiopulmonary
Bypass for Coronary Artery Bypass Surgery (in Japanese
with English Abstract), Masui (The Japanese Journal of
Anesthesiology), Vol. 52, No. 6, 2003, pp. 621-625.
REFERENCES
[1]
[2]
[3]
[4]
[5]
[6]
83
T. Arai, Y. Takano, S. Muzukami and I. Sato, The Effect
of Olprinone Administered after Cardiopulmonary Bypass during Open Heart Surgery, Evaluated by Its Plasma
Concentrations and Hemodynamic Changes (in Japanese
with English Abstract), Masui (The Japanese Journal of
Anesthesiology), Vol. 48, No. 10, 1999, pp. 1083-1090.
T. Arai, Effects of Olprinone Hydrochroride after Coronary Artery Bypass Grafting (in Japanese with English Abstract), Masui (The Japanese Journal of Anesthesiology),
Vol. 53, No. 2, 2004, pp. 122-130.
M. Unoshima, H. Iwasaka, S. Hattori, T. Kitano and T.
Noguchi, Effects of Olprinone Hydrochloride on Hemodynamics and Respiratory Oxygenation in Patients after
Cardiac Surgery (in Japanese with English Abstract), Masui (The Japanese Journal of Anesthesiology), Vol. 46,
No. 8, 1997, pp. 1053-1058.
T. Arai, K. Kamishima, T. Terauchi, Y. Enomoto, M.
Shimazaki, H. Inoue, et al., Effects of Olprinone Hydrochroride in Patients Undergoing Off-Pump Coronary Ar-
Copyright 2013 SciRes.
[10] J. M. Bailey, J. H. Levy, M. Kikura, F. Szlam and C. C.
Hug Jr., Pharmacokinetics of Intravenous Milrinone in
Patients Undergoing Cardiac Surgery, Anesthesiology,
Vol. 81, No. 3, 1994, pp. 616-622.
doi:10.1097/00000542-199409000-00014
[11] J. M. Bailey, B. E. Miller, W. Lu, S. R. Tosone, K. R.
Kanter and V. K. Tam, The Pharmacokinetics of Milrinone in Pediatric Patients after Cardiac Surgery, Anesthesiology, Vol. 90, No. 4, 1999, pp. 1012-1018.
doi:10.1097/00000542-199904000-00014
[12] C. Ramamoorthy, G. D. Anderson, G. D. Williams and A.
M. Lynn, Pharmacokinetics and Side Effects of Milrinone in Infants and Children after Open Heart Surgery,
Anesthesia & Analgesia, Vol. 86, No. 2, 1998, pp. 283289. doi:10.1097/00000539-199802000-00011
OJAnes
You might also like
- ATLS Practice Test 3 Answers & ExplanationsDocument10 pagesATLS Practice Test 3 Answers & ExplanationsCarl Sars50% (2)
- Five Level TriageDocument2 pagesFive Level TriageHarold Haze Cortez100% (4)
- AHA-PALS 2010: Pediatric Chain of SurvivalDocument10 pagesAHA-PALS 2010: Pediatric Chain of SurvivalIsabel CastilloNo ratings yet
- Dubin ECG Reference SheetsDocument13 pagesDubin ECG Reference SheetsEllie100% (1)
- 1 s2.0 S1110184913000639 MainDocument8 pages1 s2.0 S1110184913000639 MainRolando Juan Dávila SalcedoNo ratings yet
- 1 s2.0 S1110184913000639 MainDocument8 pages1 s2.0 S1110184913000639 MainRolando Juan Dávila SalcedoNo ratings yet
- Evaluation of Propofol Anesthesia in Morbidly Obese Children and AdolescentsDocument9 pagesEvaluation of Propofol Anesthesia in Morbidly Obese Children and AdolescentsDebi SumarliNo ratings yet
- ClonidineDocument4 pagesClonidineDR RAVI ANANDNo ratings yet
- J Neurol Neurosurg Psychiatry 1981 Young 323 8Document7 pagesJ Neurol Neurosurg Psychiatry 1981 Young 323 8Ian BoydNo ratings yet
- Vent AvisDocument9 pagesVent AvisArini NurlelaNo ratings yet
- Downloaded File-195Document6 pagesDownloaded File-195Abdul RachmanNo ratings yet
- Vranish 2016Document7 pagesVranish 2016Jenifer de OliveiraNo ratings yet
- Ağrısız Gastroskopi Sırasında Anestezi Indüksiyonunda Bireyselleştirilmiş Optimal Hedef Konsantrasyonu Hesaplamak Için Bir Gösterge Olarak Kirpik Refleksini Kullanmanın Uygulanabilirliğini Araştırmak.Document4 pagesAğrısız Gastroskopi Sırasında Anestezi Indüksiyonunda Bireyselleştirilmiş Optimal Hedef Konsantrasyonu Hesaplamak Için Bir Gösterge Olarak Kirpik Refleksini Kullanmanın Uygulanabilirliğini Araştırmak.Ali ÖzdemirNo ratings yet
- Articulo 3Document6 pagesArticulo 3Raul Soto FigueroaNo ratings yet
- Farmacology Del Paro CardiacoDocument14 pagesFarmacology Del Paro CardiacoNicoSwtifNo ratings yet
- Thrombolysis With Alteplase 3 To 4.5 Hours After Acute Ischemic StrokeDocument4 pagesThrombolysis With Alteplase 3 To 4.5 Hours After Acute Ischemic StrokeSalma Asri NovaNo ratings yet
- 17TOHJDocument4 pages17TOHJAriffa DiazNo ratings yet
- Jurnal GenerghjfgjyjhvjhgjfjdjmhfjmDocument5 pagesJurnal GenerghjfgjyjhvjhgjfjdjmhfjmH'Cham AchmadNo ratings yet
- Kang 2018Document20 pagesKang 2018Elisabeth EstellaNo ratings yet
- Pulmonary Pharmacology & TherapeuticsDocument5 pagesPulmonary Pharmacology & TherapeuticsClaudia SofroniaNo ratings yet
- 2010 BR J Anaesth Propofol PK Obese CortinezDocument9 pages2010 BR J Anaesth Propofol PK Obese CortinezmiguelzapienNo ratings yet
- New Evidence in Home Mechanical Ventilation: Thematic Poster Session Hall 2-4 - 12:50-14:40Document5 pagesNew Evidence in Home Mechanical Ventilation: Thematic Poster Session Hall 2-4 - 12:50-14:40Shirley CoelhoNo ratings yet
- Efficacy of Hyperventilation, Blood Pressure Elevation, and Metabolic Suppression Therapy in Controlling Intracranial Pressure After Head InjuryDocument9 pagesEfficacy of Hyperventilation, Blood Pressure Elevation, and Metabolic Suppression Therapy in Controlling Intracranial Pressure After Head InjuryAik NoeraNo ratings yet
- Conversion To Everolimus in Maintenance Patients-Current Clinical StrategiesDocument6 pagesConversion To Everolimus in Maintenance Patients-Current Clinical StrategieshassanNo ratings yet
- Jurnal AnestesiDocument8 pagesJurnal AnestesiapriiiiiiilllNo ratings yet
- Jimbo 2017Document15 pagesJimbo 2017Sahily MoralesNo ratings yet
- The Analgesic Efficacy of Tramadol As A Pre-Emptive Analgesic in Pediatric Appendectomy Patients PDFDocument6 pagesThe Analgesic Efficacy of Tramadol As A Pre-Emptive Analgesic in Pediatric Appendectomy Patients PDFUmmu Qonitah AfnidawatiNo ratings yet
- The Use of Sildenafil in Persistent Pulmonary Hypertension of The Newborn PDFDocument6 pagesThe Use of Sildenafil in Persistent Pulmonary Hypertension of The Newborn PDFmaciasdrNo ratings yet
- Overview of Total Intravenous Anesthesia in ChildrenDocument12 pagesOverview of Total Intravenous Anesthesia in ChildrenJosibel OcantoNo ratings yet
- Tatalaksana PJBDocument5 pagesTatalaksana PJBmayaNo ratings yet
- Efek Clon & Magnes PDFDocument5 pagesEfek Clon & Magnes PDFDisi Muhaymin RNo ratings yet
- Phenylephrine For Blood Pressure Control in Elective Cesarean Section: Therapeutic Versus Prophylactic DosesDocument8 pagesPhenylephrine For Blood Pressure Control in Elective Cesarean Section: Therapeutic Versus Prophylactic DosesPalwasha MalikNo ratings yet
- Yilmaz 2018Document18 pagesYilmaz 2018Hassler Barrios AcostaNo ratings yet
- KJAEDocument7 pagesKJAEM Wahyu UtomoNo ratings yet
- Ob 7Document22 pagesOb 7William OmarNo ratings yet
- Clinical StudyDocument7 pagesClinical StudyJonathan MarkNo ratings yet
- Comparison of Ondansetron, Cyclizine and Prochlorperazine For PONV Prophylaxis in Laparoscopic CholecystectomyDocument5 pagesComparison of Ondansetron, Cyclizine and Prochlorperazine For PONV Prophylaxis in Laparoscopic CholecystectomynikimahhNo ratings yet
- En V60n4a06Document5 pagesEn V60n4a06Palwasha MalikNo ratings yet
- 1 s2.0 S2531043718301107 MainDocument8 pages1 s2.0 S2531043718301107 MainCraniolyne RefianNo ratings yet
- Revista Brasileira DE AnestesiologiaDocument9 pagesRevista Brasileira DE AnestesiologiayulianiNo ratings yet
- Undiagnosed Abdominal Paraganglioma: An Anaesthetic ChallengeDocument3 pagesUndiagnosed Abdominal Paraganglioma: An Anaesthetic ChallengeAde Gustina SiahaanNo ratings yet
- Critical Care CasesDocument7 pagesCritical Care CasesJude Micko Bunyi AlipitNo ratings yet
- Randomized Clinical Trial Investigating The Stress Response From Two Different Methods of Analgesia After Laparoscopic Colorectal SurgeryDocument7 pagesRandomized Clinical Trial Investigating The Stress Response From Two Different Methods of Analgesia After Laparoscopic Colorectal Surgeryvalerio.messinaNo ratings yet
- Inhaled Vasodilators As Salvage Therapy in ARDS Caused by H1N1 InfectionDocument5 pagesInhaled Vasodilators As Salvage Therapy in ARDS Caused by H1N1 InfectiondarmariantoNo ratings yet
- Research ArticleDocument7 pagesResearch Articlenaljnaby9No ratings yet
- Bauch-Atrial Natriuretic Peptide As A MarDocument6 pagesBauch-Atrial Natriuretic Peptide As A MarSzendeNo ratings yet
- SSRN Id3666867Document18 pagesSSRN Id3666867Douglas SantosNo ratings yet
- JurnalDocument6 pagesJurnalFitri Aesthetic centerNo ratings yet
- Paper Title: (16 Bold Blue Color)Document9 pagesPaper Title: (16 Bold Blue Color)Fauzi RusdiantoNo ratings yet
- Introduction: Intravenous Ibuprofen May Offer Advantages Over Ketorolac For Postoperative Pain ControlDocument6 pagesIntroduction: Intravenous Ibuprofen May Offer Advantages Over Ketorolac For Postoperative Pain ControlnadaNo ratings yet
- The Hemodynamic Effects of Propofol in Children With Congenital Heart DiseaseDocument6 pagesThe Hemodynamic Effects of Propofol in Children With Congenital Heart DiseaseAngelica Lucero OrtizNo ratings yet
- ARTIGO1Document9 pagesARTIGO1jtnylsonNo ratings yet
- Prompt Prediction of Fibrinogen Concentration During Cardiopulmonary BypassDocument8 pagesPrompt Prediction of Fibrinogen Concentration During Cardiopulmonary Bypassjuajimenez55No ratings yet
- Original Article: Ayesha Goyal, P. Shankaranarayan, P. GanapathiDocument6 pagesOriginal Article: Ayesha Goyal, P. Shankaranarayan, P. GanapathiAnonymous S0H8cqgnfiNo ratings yet
- Research ArticleDocument9 pagesResearch ArticleM RifkiNo ratings yet
- Research Article: Evaluation of Pre and Post Bronchodilator Pulmonary Function Test in Fifty Healthy VolunteersDocument8 pagesResearch Article: Evaluation of Pre and Post Bronchodilator Pulmonary Function Test in Fifty Healthy VolunteersEarthjournal PublisherNo ratings yet
- Guidelines Adult Advanced Life SupportDocument34 pagesGuidelines Adult Advanced Life SupportParvathy R NairNo ratings yet
- Variability of Residual Platelet Function Despite Clopidogrel Treatment in Patients With Peripheral Arterial Occlusive DiseaseDocument6 pagesVariability of Residual Platelet Function Despite Clopidogrel Treatment in Patients With Peripheral Arterial Occlusive DiseaseGono GenieNo ratings yet
- Universitas Indonesia: U. Weber, M. Krammel, S. Linke, T. Hamp, T. Stimpfl, B. Reiter, W. PlӧchlDocument8 pagesUniversitas Indonesia: U. Weber, M. Krammel, S. Linke, T. Hamp, T. Stimpfl, B. Reiter, W. PlӧchlgoldenNo ratings yet
- 1 s2.0 S0959804912009239 MainDocument10 pages1 s2.0 S0959804912009239 MainMarcel PopaNo ratings yet
- A Comparison of Hemodynamic Changes During Laryngoscopy and Endotracheal Intubation by Using Three Modalities of Anesthesia InductionDocument5 pagesA Comparison of Hemodynamic Changes During Laryngoscopy and Endotracheal Intubation by Using Three Modalities of Anesthesia Inductionammaa_No ratings yet
- Paper TemplateDocument10 pagesPaper Templatenur hidayatNo ratings yet
- 08 PDFDocument6 pages08 PDFintan kusumaningtyasNo ratings yet
- Essentials in Lung TransplantationFrom EverandEssentials in Lung TransplantationAllan R. GlanvilleNo ratings yet
- Morning Report Februari 2016: A 36-Year-Old-Man With Moderate Acute Asthma DD Acis DD CopdDocument14 pagesMorning Report Februari 2016: A 36-Year-Old-Man With Moderate Acute Asthma DD Acis DD CopdFika Khulma SofiaNo ratings yet
- InTech - Mechanisms in Erectile Function and Dysfunction An OverviewDocument21 pagesInTech - Mechanisms in Erectile Function and Dysfunction An OverviewFika Khulma SofiaNo ratings yet
- Interpreting D DimerDocument8 pagesInterpreting D DimerFika Khulma SofiaNo ratings yet
- Cardioplegia in Pediatric Cardiac Surgery: Do We Believe in Magic?Document12 pagesCardioplegia in Pediatric Cardiac Surgery: Do We Believe in Magic?Fika Khulma SofiaNo ratings yet
- Abstrak DR SariDocument2 pagesAbstrak DR SariFika Khulma SofiaNo ratings yet
- Venous Air Embolism During Anterior Lumbar Surgery: Case ReportDocument3 pagesVenous Air Embolism During Anterior Lumbar Surgery: Case ReportFika Khulma SofiaNo ratings yet
- Incidence of Venous Air Embolism During Craniectomy For Craniosynostosis RepairDocument4 pagesIncidence of Venous Air Embolism During Craniectomy For Craniosynostosis RepairFika Khulma SofiaNo ratings yet
- Physician. 2011 May 1 83 (9) :1078-1084Document4 pagesPhysician. 2011 May 1 83 (9) :1078-1084Fika Khulma SofiaNo ratings yet
- Practice Essentials: Essential Update: Chemotherapy Following Radiation May Improve Survival in Low-Grade GliomasDocument19 pagesPractice Essentials: Essential Update: Chemotherapy Following Radiation May Improve Survival in Low-Grade GliomasFika Khulma SofiaNo ratings yet
- Imaging Features of Primary Breast SarcomaDocument8 pagesImaging Features of Primary Breast SarcomaFika Khulma SofiaNo ratings yet
- Vestibular Neutitis & Labyrinthitis PDFDocument6 pagesVestibular Neutitis & Labyrinthitis PDFFika Khulma SofiaNo ratings yet
- Ga Kebaca (Blabla)Document5 pagesGa Kebaca (Blabla)Fika Khulma SofiaNo ratings yet
- Jenis Pemeriksaan 4/5 6/5 7/5 Nilai Rujukan Satuan Hematologi Rutin 9.6 29 16.7Document2 pagesJenis Pemeriksaan 4/5 6/5 7/5 Nilai Rujukan Satuan Hematologi Rutin 9.6 29 16.7Fika Khulma SofiaNo ratings yet
- ORAL DIAG Q&A DentistryDocument46 pagesORAL DIAG Q&A DentistryTJ OberioNo ratings yet
- Necropsy Guide For Dogs Cats and Small Mammals - 2016 - McDonough - Appendix 4 Describing Gross LesionsDocument2 pagesNecropsy Guide For Dogs Cats and Small Mammals - 2016 - McDonough - Appendix 4 Describing Gross Lesionsimmanuel1111No ratings yet
- ShockDocument30 pagesShockvinnu kalyanNo ratings yet
- Blood Supply of The BrainDocument32 pagesBlood Supply of The BrainShimmering MoonNo ratings yet
- Iap CprdayDocument33 pagesIap CprdayRabi KumarNo ratings yet
- Cardiology SoalDocument9 pagesCardiology Soalanz_4191No ratings yet
- Parathyroid, HyperparathyroidismDocument4 pagesParathyroid, Hyperparathyroidismjamil aoudeNo ratings yet
- CVD Case StudyDocument23 pagesCVD Case StudyMsRhyxelle80% (5)
- Adrenergic NeurotransmittersDocument18 pagesAdrenergic Neurotransmittersparmarkeval1610No ratings yet
- TCHP Shock Series Part 2Document2 pagesTCHP Shock Series Part 2ikeernawatiNo ratings yet
- Osteoporosis & OsteomalaciaDocument29 pagesOsteoporosis & OsteomalaciaKeith OmwoyoNo ratings yet
- HipertenziaDocument2 pagesHipertenziaAfiya MohammedNo ratings yet
- Edmodo Quiz As Biology Topic 1 Cardiac Cycle1Document2 pagesEdmodo Quiz As Biology Topic 1 Cardiac Cycle1Arun NandhaNo ratings yet
- ALS Manual 2010.version 1Document84 pagesALS Manual 2010.version 1Elena How100% (1)
- NP 3. Compiled QuestionsDocument43 pagesNP 3. Compiled QuestionsAzurin JewelNo ratings yet
- Science TriviaDocument5 pagesScience TriviaasserenanoyagNo ratings yet
- Class 10 TransportationDocument5 pagesClass 10 TransportationKanishk KumarNo ratings yet
- Pedriatrics 6th YearDocument50 pagesPedriatrics 6th YearKimira GoundenNo ratings yet
- Pre Medical Evaluatiom Form PFT 1 PDFDocument2 pagesPre Medical Evaluatiom Form PFT 1 PDFAIEN WENDELEIH Q. CAPINPIN100% (2)
- SGOT (Aspartate Aminotransferase, AST, Glutamic Oxaloacetic Transaminase)Document9 pagesSGOT (Aspartate Aminotransferase, AST, Glutamic Oxaloacetic Transaminase)Reman A. AlingasaNo ratings yet
- Urinary SystemDocument6 pagesUrinary SystemKids JangNo ratings yet
- 心血管外科、胸外科专业术语 (名词) 汉英对照Document13 pages心血管外科、胸外科专业术语 (名词) 汉英对照Ted TsieNo ratings yet
- UntitledDocument48 pagesUntitledSamad MaqsoodNo ratings yet
- Introduction To Human Anatomy and PhysiologyDocument42 pagesIntroduction To Human Anatomy and PhysiologyDump Acc 2100% (1)
- Drug Study LCPDocument3 pagesDrug Study LCPalleen_viaNo ratings yet
- Ebook Textbook of Radiology and Imaging Vol 2 PDF Full Chapter PDFDocument54 pagesEbook Textbook of Radiology and Imaging Vol 2 PDF Full Chapter PDFdorothy.cook305100% (35)