Professional Documents
Culture Documents
Histology of Larynx, Trachea, Bronchus - Dea Natalia - 130110110190 - E3/Respi
Histology of Larynx, Trachea, Bronchus - Dea Natalia - 130110110190 - E3/Respi
Uploaded by
Marshel BudiarsaCopyright:
Available Formats
You might also like
- Syllabus of BSC Nursing, Kathmandu UniversityDocument191 pagesSyllabus of BSC Nursing, Kathmandu UniversityKamal Raj Chapagain94% (18)
- Burton's Microbiology For The Health Sciences: Section VIII. Major Infectious Diseases of HumansDocument29 pagesBurton's Microbiology For The Health Sciences: Section VIII. Major Infectious Diseases of HumansCarmela Laraya Alayon25% (4)
- Sistem Pernapasan JunqueiraDocument33 pagesSistem Pernapasan JunqueiraFiya AfivaNo ratings yet
- Color Atlas and Text of Histology (6th Ed) (Gnv64)Document3 pagesColor Atlas and Text of Histology (6th Ed) (Gnv64)abdeljelileNo ratings yet
- The Respiratory System PP First - Stage 2021Document27 pagesThe Respiratory System PP First - Stage 2021HHHNo ratings yet
- Anatomy and Physiology of Respiratory SystemDocument4 pagesAnatomy and Physiology of Respiratory Systembilliam123No ratings yet
- Canine Study CircleDocument16 pagesCanine Study CircleMahesh KambleNo ratings yet
- (Histologi) Sistem Respirasi - Dr. SusiantiDocument51 pages(Histologi) Sistem Respirasi - Dr. SusiantiulfamarianaNo ratings yet
- 2nd Lec of Respiratory Histology by DR RoomiDocument39 pages2nd Lec of Respiratory Histology by DR RoomiMudassar Roomi100% (1)
- Ma Nurfaizah Ma04200026 Respiratory System April 2020Document3 pagesMa Nurfaizah Ma04200026 Respiratory System April 2020Nur Faizah Binti Jamail MANo ratings yet
- Animal CellDocument64 pagesAnimal CellFrance Dorothy SamortinNo ratings yet
- Respiratory System PDFDocument29 pagesRespiratory System PDFAgzar RidhoNo ratings yet
- Respiratory System - Lecture NoteDocument15 pagesRespiratory System - Lecture NoteZahina AmrinNo ratings yet
- Histo - Respiratory System - TheoryDocument12 pagesHisto - Respiratory System - Theoryمحمد العراقيNo ratings yet
- Lec 5 HistologyDocument25 pagesLec 5 Histologyأ. علي محمدNo ratings yet
- Histology The Respiratory System: Prof. Dr. Sabah N. AlwachiDocument15 pagesHistology The Respiratory System: Prof. Dr. Sabah N. AlwachilaithjnbNo ratings yet
- Respiratory System 2Document8 pagesRespiratory System 2Shawn Gaurav JhaNo ratings yet
- Anatomic and Physiologic OverviewDocument8 pagesAnatomic and Physiologic OverviewJoseph King MacaranasNo ratings yet
- Histology of Respiratory System: Dr. Mirna Muis, SP - Rad Dept. of Histology Faculty of Medicine, Hasanuddin UnivDocument31 pagesHistology of Respiratory System: Dr. Mirna Muis, SP - Rad Dept. of Histology Faculty of Medicine, Hasanuddin UnivNor Izhharuddin ZainyNo ratings yet
- Respiratory System by Dr. Vincent-JrDocument48 pagesRespiratory System by Dr. Vincent-JrEmma OsabohienNo ratings yet
- AICE Bio Notes Pages 186-190: Gas ExchangeDocument2 pagesAICE Bio Notes Pages 186-190: Gas ExchangeSanzida HossainNo ratings yet
- Respiratory System: A) The Conducting Portion, Which Consists of The Nasal CavitiesDocument7 pagesRespiratory System: A) The Conducting Portion, Which Consists of The Nasal CavitiesSalmah Alimah FitriNo ratings yet
- 1st Lecture of Respiratory Histology by DR RoomiDocument24 pages1st Lecture of Respiratory Histology by DR RoomiMudassar Roomi100% (1)
- Anatomy and Physiology of Respiratory SystemDocument5 pagesAnatomy and Physiology of Respiratory SystemNesra de PeraltaNo ratings yet
- SasuntqiDocument55 pagesSasuntqiNika MtsituriNo ratings yet
- Lec:2 Respiratory System DR - HudaDocument4 pagesLec:2 Respiratory System DR - HudaLina AyadNo ratings yet
- Treatment of Bronchiectactasis by DR Bashir Ahmed Dar Associate Professor Medicine Sopore KashmirDocument132 pagesTreatment of Bronchiectactasis by DR Bashir Ahmed Dar Associate Professor Medicine Sopore KashmirProf Dr Bashir Ahmed Dar Chinki Pora Sopore KashmirNo ratings yet
- Respiratory SystemDocument15 pagesRespiratory SystemJovelou MihangosNo ratings yet
- The Respiratory SystemDocument5 pagesThe Respiratory SystemAllen BurdowskiNo ratings yet
- Histology of LungsDocument30 pagesHistology of LungsShahir21No ratings yet
- Respiratory System LECDocument5 pagesRespiratory System LECMax DelvalleNo ratings yet
- Anatomy and Physiology of The Respiratory SystemDocument5 pagesAnatomy and Physiology of The Respiratory SystemLek Bassig ReyesNo ratings yet
- Nasal CavitiesDocument14 pagesNasal CavitiesaikaNo ratings yet
- Histology of Lung FinalDocument23 pagesHistology of Lung FinalBishal PaulNo ratings yet
- Respiratory SystemDocument25 pagesRespiratory Systemada.codreanuNo ratings yet
- Respritory System Part2Document30 pagesRespritory System Part2Deniz asmazNo ratings yet
- Respiratory Epithelium: Human Histology Lecture Chapter 17 Ï The Respiratory SystemDocument16 pagesRespiratory Epithelium: Human Histology Lecture Chapter 17 Ï The Respiratory SystemEvandie OngNo ratings yet
- Handout Respiratory System 2022 2023Document3 pagesHandout Respiratory System 2022 2023reece sayamNo ratings yet
- Anatomy and Histology of The Normal Lung and AirwaysDocument20 pagesAnatomy and Histology of The Normal Lung and AirwaysFahd Abdullah Al-refaiNo ratings yet
- Respiratoy System HistologyDocument32 pagesRespiratoy System HistologyNaveed AkhterNo ratings yet
- Pulmo Management Week 1Document160 pagesPulmo Management Week 1Dharlyn MungcalNo ratings yet
- 3-5-2023 Anatomy of Human Respiratory SystemDocument7 pages3-5-2023 Anatomy of Human Respiratory Systemأ. علي محمدNo ratings yet
- A & P RespiratoryDocument18 pagesA & P Respiratoryamirul haakimNo ratings yet
- The Respirator Y System: Mungcal, Dharlynette RTRPDocument158 pagesThe Respirator Y System: Mungcal, Dharlynette RTRPDharlyn MungcalNo ratings yet
- Anatomy & Physiology of Respiratory SystemDocument12 pagesAnatomy & Physiology of Respiratory SystemDgjj CompuiterNo ratings yet
- Gas Exchange Text Book Based Revision NoteDocument6 pagesGas Exchange Text Book Based Revision NoteJamesNo ratings yet
- Rts k3 Rts1k3Document55 pagesRts k3 Rts1k3felixNo ratings yet
- Learning Objective: Respiratory SystemDocument4 pagesLearning Objective: Respiratory SystemReham QueNo ratings yet
- Respiratory SystemDocument6 pagesRespiratory SystemQK CLARONo ratings yet
- Histology of Trachea and Extrapulmonary Bronchi: By: Dr.M.Irfan Ashraf MBBS, MCPS, FcpsDocument14 pagesHistology of Trachea and Extrapulmonary Bronchi: By: Dr.M.Irfan Ashraf MBBS, MCPS, FcpsDr-Arsalan ZahidNo ratings yet
- The Respiratory SystemDocument5 pagesThe Respiratory SystemdeepmazumderNo ratings yet
- Diagnostic Examination of Pulmonary TuberculosisDocument5 pagesDiagnostic Examination of Pulmonary TuberculosisMark BerbanoNo ratings yet
- Sist RespDocument4 pagesSist RespTania MendozaNo ratings yet
- Histology of Respiratory SystemDocument6 pagesHistology of Respiratory SystemEzyan Syamin100% (2)
- Anatomy of The Respiratory SystemDocument8 pagesAnatomy of The Respiratory SystemAsher Eby VargeeseNo ratings yet
- Histologyoftracheaandlung 160315034320Document65 pagesHistologyoftracheaandlung 160315034320MUBEEN SHAIKHNo ratings yet
- RespiratoryDocument30 pagesRespiratoryamieNo ratings yet
- PAin and Oxygenation HandoutsPRELIMSDocument7 pagesPAin and Oxygenation HandoutsPRELIMSJhoanna de ChavezNo ratings yet
- 50 The Gas Exchange SystemDocument5 pages50 The Gas Exchange SystemSarahNo ratings yet
- The Design of The Respiratory SystemDocument21 pagesThe Design of The Respiratory Systemvonneivan26No ratings yet
- The Respiratory SystemDocument16 pagesThe Respiratory SystemAirene Mae Lamputi SupilarNo ratings yet
- Senin Selasa Rabu Kamis Jummat Sabtu Pagi: Sari Ibrahim Garid Yohanes Dina Sari Vinod Tika Joyce VinodDocument4 pagesSenin Selasa Rabu Kamis Jummat Sabtu Pagi: Sari Ibrahim Garid Yohanes Dina Sari Vinod Tika Joyce VinodMarshel BudiarsaNo ratings yet
- LI10. E3 RespiDocument4 pagesLI10. E3 RespiMarshel BudiarsaNo ratings yet
- Natalia - 130110110190 - E3/Respi: Classification and Prevention of Pneumonia - DeaDocument1 pageNatalia - 130110110190 - E3/Respi: Classification and Prevention of Pneumonia - DeaMarshel BudiarsaNo ratings yet
- Natalia - 130110110190 - E3/Respi: Nutritional Supplement and Its Role For Tuberculosis Patients - DeaDocument2 pagesNatalia - 130110110190 - E3/Respi: Nutritional Supplement and Its Role For Tuberculosis Patients - DeaMarshel BudiarsaNo ratings yet
- Natalia - 130110110190 - E3/Respi: Chronic Obstructive Pulmonary Disease (COPD) - DeaDocument5 pagesNatalia - 130110110190 - E3/Respi: Chronic Obstructive Pulmonary Disease (COPD) - DeaMarshel BudiarsaNo ratings yet
- LI1. E3 RespDocument1 pageLI1. E3 RespMarshel BudiarsaNo ratings yet
- Retraction: Intercostal and Epigastric - Dea Natalia - 130110110190 - E3/RespiDocument2 pagesRetraction: Intercostal and Epigastric - Dea Natalia - 130110110190 - E3/RespiMarshel BudiarsaNo ratings yet
- Normal Flora of URT GAS-GBS Microbiology Diagnostic + Culture Procedure - DeaDocument5 pagesNormal Flora of URT GAS-GBS Microbiology Diagnostic + Culture Procedure - DeaMarshel BudiarsaNo ratings yet
- Disease Outbreak 2013Document60 pagesDisease Outbreak 2013Marshel BudiarsaNo ratings yet
- Iron SupplementationDocument3 pagesIron SupplementationMarshel BudiarsaNo ratings yet
- Lab Activity Repro 3 RpsDocument5 pagesLab Activity Repro 3 RpsMarshel BudiarsaNo ratings yet
- Role of IT in MedicineDocument10 pagesRole of IT in MedicineMarshel BudiarsaNo ratings yet
- Respiratory Failure PDFDocument5 pagesRespiratory Failure PDFOxana Turcu100% (1)
- Alterations in OxygenationDocument104 pagesAlterations in OxygenationMelchor Felipe Salvosa100% (1)
- Machine Learning Algorithms Utilizing Functional Respiratory Imaging May Predict COPD ExacerbationsDocument9 pagesMachine Learning Algorithms Utilizing Functional Respiratory Imaging May Predict COPD ExacerbationsFaraz KhanNo ratings yet
- Ca of The Respiratory System NCM 112 Cell Ab Final TopicsDocument95 pagesCa of The Respiratory System NCM 112 Cell Ab Final TopicsA. Lizette PabloNo ratings yet
- Respiratory Insufficiency & Other Clinical ConditionsDocument16 pagesRespiratory Insufficiency & Other Clinical ConditionsnirilibNo ratings yet
- CHAPTER - 6 LIFE PROCESSES CLASS XTH 2020-2021Document20 pagesCHAPTER - 6 LIFE PROCESSES CLASS XTH 2020-2021FACTOPEDIANo ratings yet
- Disturbances in OxygenationDocument10 pagesDisturbances in OxygenationjenrylNo ratings yet
- Unit 4. The Human BodyDocument28 pagesUnit 4. The Human BodyBeatriz Collado LogrosánNo ratings yet
- CpapDocument33 pagesCpapAtikah Putri AtmojoNo ratings yet
- Bronchi 0Document52 pagesBronchi 0Jennifer DixonNo ratings yet
- Pre-Op Preparation and Assessment of Pediatric PatientsDocument62 pagesPre-Op Preparation and Assessment of Pediatric PatientsBedahanakugmNo ratings yet
- RespiratoryDocument4 pagesRespiratoryHaliana IzatiNo ratings yet
- Respiratory DisordersDocument17 pagesRespiratory DisordersBrandi Worley100% (2)
- Community Acquired Pneumonia, A Case StudyDocument26 pagesCommunity Acquired Pneumonia, A Case StudyMenggay SanDiego57% (7)
- Imaging of The Respiratory SystemDocument105 pagesImaging of The Respiratory SystemMizrab Nadeem100% (1)
- BurnsDocument9 pagesBurnsVincentus BinNo ratings yet
- Mechanical Ventilation Made Easy - 2009Document484 pagesMechanical Ventilation Made Easy - 2009Dan Bobeica75% (4)
- Nursing Care Plan For A Person With Croup Nursing DiagnosisDocument2 pagesNursing Care Plan For A Person With Croup Nursing DiagnosisMonica Rivera100% (1)
- Anatomy of The Respiratory SystemDocument4 pagesAnatomy of The Respiratory SystemMayden Grace GayatgayNo ratings yet
- OxygenationDocument24 pagesOxygenationJohn Anthony de GùzmanNo ratings yet
- Demo LPDocument3 pagesDemo LPNikki Anne BerlanasNo ratings yet
- Cardiovascular and Respiratory SystemDocument44 pagesCardiovascular and Respiratory SystemKlaudette Collin PaynorNo ratings yet
- Unit 2 Biology and Geology 3rd ESODocument64 pagesUnit 2 Biology and Geology 3rd ESOPaulaNo ratings yet
- Nursing Diagnosis For AsthmaDocument6 pagesNursing Diagnosis For AsthmaTINAIDA33% (3)
- Nursing Care PlansDocument3 pagesNursing Care PlansfanvicfayNo ratings yet
- Lung Sounds 3Document1 pageLung Sounds 3Kyle LatayanNo ratings yet
- Evers SafetyBook V3Document160 pagesEvers SafetyBook V3Gudruman EdisonNo ratings yet
- Every Cell in Your Body Needs Oxygen To LiveDocument12 pagesEvery Cell in Your Body Needs Oxygen To LiveSeraphim CamposNo ratings yet
Histology of Larynx, Trachea, Bronchus - Dea Natalia - 130110110190 - E3/Respi
Histology of Larynx, Trachea, Bronchus - Dea Natalia - 130110110190 - E3/Respi
Uploaded by
Marshel BudiarsaOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Histology of Larynx, Trachea, Bronchus - Dea Natalia - 130110110190 - E3/Respi
Histology of Larynx, Trachea, Bronchus - Dea Natalia - 130110110190 - E3/Respi
Uploaded by
Marshel BudiarsaCopyright:
Available Formats
Histology of Larynx, Trachea, Bronchus_Dea Natalia_130110110190_E3/Respi
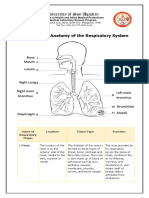
LARYNX
The larynx is a short passageway for air between the pharynx and trachea. Its wall contains skeletal
muscles and pieces of cartilage, all of which make the larynx specialized for sound production. The
lining of the larynx superior to the vocal folds is nonkeratinized stratified squamous epithelium. The
lining of the larynx inferior to the vocal folds is pseudostratified ciliated columnar epithelium
consisting of ciliated columnar cells, goblet cells, and basal cells. The mucus produced by the goblet
cells helps trap dust not removed in the upper passages. The cilia in the upper respiratory tract move
mucus and trapped particles down toward the pharynx; the cilia in the lower respiratory tract move
them up toward the pharynx.
The low-power micrograph shows the upper laryngeal
vestibule (LV), which is surrounded by seromucous glands
(G). The lateral walls of this region bulge as a pair of broad
folds, the vestibular folds (VF). These also contain
seromucous glands and areolar tissue with MALT, often with
lymphoid nodules (L) and are largely covered by respiratory
epithelium, with regions near the epiglottis having stratified
squamous epithelium. Below each large vestibular fold is a
narrow space or ventricle (V), below which is another pair of
lateral folds, the vocal folds or cords (VC). These are covered
by stratified squamous epithelium and project more sharply
into the lumen, defining the rim of the opening into the
larynx itself. Each contains a large striated vocalis muscle
(VM) and nearer the surface a small ligament, which is cut transversely and therefore difficult to see
here.
TRACHEA
The layers of the tracheal wall, from deep to superficial, are the:
1. mucosa
epithelial layer of pseudo-stratified ciliated columnar epithelium consists of ciliated columnar
cells and goblet cells that reach the luminal surface, plus basal cells that do not; it provides the
same protection against dust as the membrane lining the nasal cavity and larynx
underlying layer of lamina propria that contains elastic and reticular fibers
2. submucosa
consists of areolar connective tissue that contains seromucous glands and their ducts
3. hyaline cartilage
the 1620 incomplete, horizontal rings of hyaline cartilage resemble the letter C, are stacked one
above another, and are connected together by dense connective tissue
the open part of each C-shaped cartilage ring faces posteriorly toward the esophagus and is
spanned by a fibromuscular membrane. Within this membrane are transverse smooth muscle
fibers, called the trachealis muscle, and elastic connective tissue that allow the diameter of the
trachea to change subtly during inhalation and exhalation, which is important in maintaining
efficient airflow; the solid C-shaped cartilage rings provide a semirigid support so that the
tracheal wall does not collapse inward (especially during inhalation) and obstruct the air
passageway
4. adventitia
consists of areolar connective tissue that joins the trachea to surrounding tissues
Histology of Larynx, Trachea, Bronchus_Dea Natalia_130110110190_E3/Respi
wall of the trachea is lined by typical respiratory epithelium (E)
underlain by connective tissue (CT) and seromucous glands (G) in
the lamina propria. The submucosa contains C-shaped rings of
hyaline cartilage (C) covered by perichondrium (P). The watery
mucous fluid produced by goblet cells and by the glands forms a
layer that permits the ciliary movement to propel foreign particles
continuously out of the respiratory system in the mucociliary
escalator. The openings in the cartilage rings are on the posterior
surface, against the esophagus, and contain smooth muscle and
elastic tissue. These allow distention of the tracheal lumen when
large pieces of food pass through the esophagus. The trachealis
muscle in the opening of the C also contracts during the cough
reflex to narrow the tracheal lumen and produce stronger
expulsion of air and dislodged mucus in the air passages
BRONCHUS
as the branching becomes more extensive in the bronchial tree, several structural changes may be
noted.
1. the mucous membrane in the bronchial tree changes from pseudostratified ciliated columnar
epithelium in the primary bronchi, secondary bronchi, and tertiary bronchi to ciliated simple
columnar epithelium with some goblet cells in larger bronchioles, to mostly ciliated simple cuboidal
epithelium with no goblet cells in smaller bronchioles, to mostly nonciliated simple cuboidal
epithelium in terminal bronchioles. (In regions where simple nonciliated cuboidal epithelium is
present, inhaled particles are removed by macrophages.)
2. plates of cartilage gradually replace the incomplete rings of cartilage in primary bronchi and finally
disappear in the distal bronchioles.
3. as the amount of cartilage decreases, the amount of smooth muscle increases. Smooth muscle
encircles the lumen in spiral bands. Because there is no supporting cartilage, however, muscle
spasms can close off the airways. This is what happens during an asthma attack, which can be a
life-threatening situation.
In a cross-section of a large bronchus the lining of
respiratory epithelium (E) and the mucosa are folded due
to contraction of its smooth muscle (SM). At this stage in
the bronchial tree, the wall is also surrounded by many
pieces of hyaline cartilage (C) and contains many
seromucous glands (G) in the submucosa which drain into
the lumen. In the connective tissue surrounding the bronchi
can be seen arteries and veins (V), which are also
branching as smaller and smaller vessels in the approach
to the respiratory bronchioles. All bronchi are surrounded
by distinctive lung tissue (LT) showing the many empty
spaces of pulmonary alveoli.
(a): A higher power view of the bronchus shows the epithelium (E) of mainly pseudostratified ciliated
columnar cells with a few goblet cells. The lamina propria (LP) contains the distinct layer of smooth
muscle (SM) surrounding the entire bronchus. The submucosa is the site of the supporting cartilage
(C) and the adventitia includes blood vessels (V) and nerves (N). Lung tissue (LT) directly surrounds
the adventitia of bronchi.
Histology of Larynx, Trachea, Bronchus_Dea Natalia_130110110190_E3/Respi
(b): This micrograph shows
the epithelium of a smaller
bronchus, in which the
epithelium is primarily of
columnar cells with cilia
(arrows), with fewer goblet
cells. The lamina propria has
both smooth muscle (SM) and
small serous glands
You might also like
- Syllabus of BSC Nursing, Kathmandu UniversityDocument191 pagesSyllabus of BSC Nursing, Kathmandu UniversityKamal Raj Chapagain94% (18)
- Burton's Microbiology For The Health Sciences: Section VIII. Major Infectious Diseases of HumansDocument29 pagesBurton's Microbiology For The Health Sciences: Section VIII. Major Infectious Diseases of HumansCarmela Laraya Alayon25% (4)
- Sistem Pernapasan JunqueiraDocument33 pagesSistem Pernapasan JunqueiraFiya AfivaNo ratings yet
- Color Atlas and Text of Histology (6th Ed) (Gnv64)Document3 pagesColor Atlas and Text of Histology (6th Ed) (Gnv64)abdeljelileNo ratings yet
- The Respiratory System PP First - Stage 2021Document27 pagesThe Respiratory System PP First - Stage 2021HHHNo ratings yet
- Anatomy and Physiology of Respiratory SystemDocument4 pagesAnatomy and Physiology of Respiratory Systembilliam123No ratings yet
- Canine Study CircleDocument16 pagesCanine Study CircleMahesh KambleNo ratings yet
- (Histologi) Sistem Respirasi - Dr. SusiantiDocument51 pages(Histologi) Sistem Respirasi - Dr. SusiantiulfamarianaNo ratings yet
- 2nd Lec of Respiratory Histology by DR RoomiDocument39 pages2nd Lec of Respiratory Histology by DR RoomiMudassar Roomi100% (1)
- Ma Nurfaizah Ma04200026 Respiratory System April 2020Document3 pagesMa Nurfaizah Ma04200026 Respiratory System April 2020Nur Faizah Binti Jamail MANo ratings yet
- Animal CellDocument64 pagesAnimal CellFrance Dorothy SamortinNo ratings yet
- Respiratory System PDFDocument29 pagesRespiratory System PDFAgzar RidhoNo ratings yet
- Respiratory System - Lecture NoteDocument15 pagesRespiratory System - Lecture NoteZahina AmrinNo ratings yet
- Histo - Respiratory System - TheoryDocument12 pagesHisto - Respiratory System - Theoryمحمد العراقيNo ratings yet
- Lec 5 HistologyDocument25 pagesLec 5 Histologyأ. علي محمدNo ratings yet
- Histology The Respiratory System: Prof. Dr. Sabah N. AlwachiDocument15 pagesHistology The Respiratory System: Prof. Dr. Sabah N. AlwachilaithjnbNo ratings yet
- Respiratory System 2Document8 pagesRespiratory System 2Shawn Gaurav JhaNo ratings yet
- Anatomic and Physiologic OverviewDocument8 pagesAnatomic and Physiologic OverviewJoseph King MacaranasNo ratings yet
- Histology of Respiratory System: Dr. Mirna Muis, SP - Rad Dept. of Histology Faculty of Medicine, Hasanuddin UnivDocument31 pagesHistology of Respiratory System: Dr. Mirna Muis, SP - Rad Dept. of Histology Faculty of Medicine, Hasanuddin UnivNor Izhharuddin ZainyNo ratings yet
- Respiratory System by Dr. Vincent-JrDocument48 pagesRespiratory System by Dr. Vincent-JrEmma OsabohienNo ratings yet
- AICE Bio Notes Pages 186-190: Gas ExchangeDocument2 pagesAICE Bio Notes Pages 186-190: Gas ExchangeSanzida HossainNo ratings yet
- Respiratory System: A) The Conducting Portion, Which Consists of The Nasal CavitiesDocument7 pagesRespiratory System: A) The Conducting Portion, Which Consists of The Nasal CavitiesSalmah Alimah FitriNo ratings yet
- 1st Lecture of Respiratory Histology by DR RoomiDocument24 pages1st Lecture of Respiratory Histology by DR RoomiMudassar Roomi100% (1)
- Anatomy and Physiology of Respiratory SystemDocument5 pagesAnatomy and Physiology of Respiratory SystemNesra de PeraltaNo ratings yet
- SasuntqiDocument55 pagesSasuntqiNika MtsituriNo ratings yet
- Lec:2 Respiratory System DR - HudaDocument4 pagesLec:2 Respiratory System DR - HudaLina AyadNo ratings yet
- Treatment of Bronchiectactasis by DR Bashir Ahmed Dar Associate Professor Medicine Sopore KashmirDocument132 pagesTreatment of Bronchiectactasis by DR Bashir Ahmed Dar Associate Professor Medicine Sopore KashmirProf Dr Bashir Ahmed Dar Chinki Pora Sopore KashmirNo ratings yet
- Respiratory SystemDocument15 pagesRespiratory SystemJovelou MihangosNo ratings yet
- The Respiratory SystemDocument5 pagesThe Respiratory SystemAllen BurdowskiNo ratings yet
- Histology of LungsDocument30 pagesHistology of LungsShahir21No ratings yet
- Respiratory System LECDocument5 pagesRespiratory System LECMax DelvalleNo ratings yet
- Anatomy and Physiology of The Respiratory SystemDocument5 pagesAnatomy and Physiology of The Respiratory SystemLek Bassig ReyesNo ratings yet
- Nasal CavitiesDocument14 pagesNasal CavitiesaikaNo ratings yet
- Histology of Lung FinalDocument23 pagesHistology of Lung FinalBishal PaulNo ratings yet
- Respiratory SystemDocument25 pagesRespiratory Systemada.codreanuNo ratings yet
- Respritory System Part2Document30 pagesRespritory System Part2Deniz asmazNo ratings yet
- Respiratory Epithelium: Human Histology Lecture Chapter 17 Ï The Respiratory SystemDocument16 pagesRespiratory Epithelium: Human Histology Lecture Chapter 17 Ï The Respiratory SystemEvandie OngNo ratings yet
- Handout Respiratory System 2022 2023Document3 pagesHandout Respiratory System 2022 2023reece sayamNo ratings yet
- Anatomy and Histology of The Normal Lung and AirwaysDocument20 pagesAnatomy and Histology of The Normal Lung and AirwaysFahd Abdullah Al-refaiNo ratings yet
- Respiratoy System HistologyDocument32 pagesRespiratoy System HistologyNaveed AkhterNo ratings yet
- Pulmo Management Week 1Document160 pagesPulmo Management Week 1Dharlyn MungcalNo ratings yet
- 3-5-2023 Anatomy of Human Respiratory SystemDocument7 pages3-5-2023 Anatomy of Human Respiratory Systemأ. علي محمدNo ratings yet
- A & P RespiratoryDocument18 pagesA & P Respiratoryamirul haakimNo ratings yet
- The Respirator Y System: Mungcal, Dharlynette RTRPDocument158 pagesThe Respirator Y System: Mungcal, Dharlynette RTRPDharlyn MungcalNo ratings yet
- Anatomy & Physiology of Respiratory SystemDocument12 pagesAnatomy & Physiology of Respiratory SystemDgjj CompuiterNo ratings yet
- Gas Exchange Text Book Based Revision NoteDocument6 pagesGas Exchange Text Book Based Revision NoteJamesNo ratings yet
- Rts k3 Rts1k3Document55 pagesRts k3 Rts1k3felixNo ratings yet
- Learning Objective: Respiratory SystemDocument4 pagesLearning Objective: Respiratory SystemReham QueNo ratings yet
- Respiratory SystemDocument6 pagesRespiratory SystemQK CLARONo ratings yet
- Histology of Trachea and Extrapulmonary Bronchi: By: Dr.M.Irfan Ashraf MBBS, MCPS, FcpsDocument14 pagesHistology of Trachea and Extrapulmonary Bronchi: By: Dr.M.Irfan Ashraf MBBS, MCPS, FcpsDr-Arsalan ZahidNo ratings yet
- The Respiratory SystemDocument5 pagesThe Respiratory SystemdeepmazumderNo ratings yet
- Diagnostic Examination of Pulmonary TuberculosisDocument5 pagesDiagnostic Examination of Pulmonary TuberculosisMark BerbanoNo ratings yet
- Sist RespDocument4 pagesSist RespTania MendozaNo ratings yet
- Histology of Respiratory SystemDocument6 pagesHistology of Respiratory SystemEzyan Syamin100% (2)
- Anatomy of The Respiratory SystemDocument8 pagesAnatomy of The Respiratory SystemAsher Eby VargeeseNo ratings yet
- Histologyoftracheaandlung 160315034320Document65 pagesHistologyoftracheaandlung 160315034320MUBEEN SHAIKHNo ratings yet
- RespiratoryDocument30 pagesRespiratoryamieNo ratings yet
- PAin and Oxygenation HandoutsPRELIMSDocument7 pagesPAin and Oxygenation HandoutsPRELIMSJhoanna de ChavezNo ratings yet
- 50 The Gas Exchange SystemDocument5 pages50 The Gas Exchange SystemSarahNo ratings yet
- The Design of The Respiratory SystemDocument21 pagesThe Design of The Respiratory Systemvonneivan26No ratings yet
- The Respiratory SystemDocument16 pagesThe Respiratory SystemAirene Mae Lamputi SupilarNo ratings yet
- Senin Selasa Rabu Kamis Jummat Sabtu Pagi: Sari Ibrahim Garid Yohanes Dina Sari Vinod Tika Joyce VinodDocument4 pagesSenin Selasa Rabu Kamis Jummat Sabtu Pagi: Sari Ibrahim Garid Yohanes Dina Sari Vinod Tika Joyce VinodMarshel BudiarsaNo ratings yet
- LI10. E3 RespiDocument4 pagesLI10. E3 RespiMarshel BudiarsaNo ratings yet
- Natalia - 130110110190 - E3/Respi: Classification and Prevention of Pneumonia - DeaDocument1 pageNatalia - 130110110190 - E3/Respi: Classification and Prevention of Pneumonia - DeaMarshel BudiarsaNo ratings yet
- Natalia - 130110110190 - E3/Respi: Nutritional Supplement and Its Role For Tuberculosis Patients - DeaDocument2 pagesNatalia - 130110110190 - E3/Respi: Nutritional Supplement and Its Role For Tuberculosis Patients - DeaMarshel BudiarsaNo ratings yet
- Natalia - 130110110190 - E3/Respi: Chronic Obstructive Pulmonary Disease (COPD) - DeaDocument5 pagesNatalia - 130110110190 - E3/Respi: Chronic Obstructive Pulmonary Disease (COPD) - DeaMarshel BudiarsaNo ratings yet
- LI1. E3 RespDocument1 pageLI1. E3 RespMarshel BudiarsaNo ratings yet
- Retraction: Intercostal and Epigastric - Dea Natalia - 130110110190 - E3/RespiDocument2 pagesRetraction: Intercostal and Epigastric - Dea Natalia - 130110110190 - E3/RespiMarshel BudiarsaNo ratings yet
- Normal Flora of URT GAS-GBS Microbiology Diagnostic + Culture Procedure - DeaDocument5 pagesNormal Flora of URT GAS-GBS Microbiology Diagnostic + Culture Procedure - DeaMarshel BudiarsaNo ratings yet
- Disease Outbreak 2013Document60 pagesDisease Outbreak 2013Marshel BudiarsaNo ratings yet
- Iron SupplementationDocument3 pagesIron SupplementationMarshel BudiarsaNo ratings yet
- Lab Activity Repro 3 RpsDocument5 pagesLab Activity Repro 3 RpsMarshel BudiarsaNo ratings yet
- Role of IT in MedicineDocument10 pagesRole of IT in MedicineMarshel BudiarsaNo ratings yet
- Respiratory Failure PDFDocument5 pagesRespiratory Failure PDFOxana Turcu100% (1)
- Alterations in OxygenationDocument104 pagesAlterations in OxygenationMelchor Felipe Salvosa100% (1)
- Machine Learning Algorithms Utilizing Functional Respiratory Imaging May Predict COPD ExacerbationsDocument9 pagesMachine Learning Algorithms Utilizing Functional Respiratory Imaging May Predict COPD ExacerbationsFaraz KhanNo ratings yet
- Ca of The Respiratory System NCM 112 Cell Ab Final TopicsDocument95 pagesCa of The Respiratory System NCM 112 Cell Ab Final TopicsA. Lizette PabloNo ratings yet
- Respiratory Insufficiency & Other Clinical ConditionsDocument16 pagesRespiratory Insufficiency & Other Clinical ConditionsnirilibNo ratings yet
- CHAPTER - 6 LIFE PROCESSES CLASS XTH 2020-2021Document20 pagesCHAPTER - 6 LIFE PROCESSES CLASS XTH 2020-2021FACTOPEDIANo ratings yet
- Disturbances in OxygenationDocument10 pagesDisturbances in OxygenationjenrylNo ratings yet
- Unit 4. The Human BodyDocument28 pagesUnit 4. The Human BodyBeatriz Collado LogrosánNo ratings yet
- CpapDocument33 pagesCpapAtikah Putri AtmojoNo ratings yet
- Bronchi 0Document52 pagesBronchi 0Jennifer DixonNo ratings yet
- Pre-Op Preparation and Assessment of Pediatric PatientsDocument62 pagesPre-Op Preparation and Assessment of Pediatric PatientsBedahanakugmNo ratings yet
- RespiratoryDocument4 pagesRespiratoryHaliana IzatiNo ratings yet
- Respiratory DisordersDocument17 pagesRespiratory DisordersBrandi Worley100% (2)
- Community Acquired Pneumonia, A Case StudyDocument26 pagesCommunity Acquired Pneumonia, A Case StudyMenggay SanDiego57% (7)
- Imaging of The Respiratory SystemDocument105 pagesImaging of The Respiratory SystemMizrab Nadeem100% (1)
- BurnsDocument9 pagesBurnsVincentus BinNo ratings yet
- Mechanical Ventilation Made Easy - 2009Document484 pagesMechanical Ventilation Made Easy - 2009Dan Bobeica75% (4)
- Nursing Care Plan For A Person With Croup Nursing DiagnosisDocument2 pagesNursing Care Plan For A Person With Croup Nursing DiagnosisMonica Rivera100% (1)
- Anatomy of The Respiratory SystemDocument4 pagesAnatomy of The Respiratory SystemMayden Grace GayatgayNo ratings yet
- OxygenationDocument24 pagesOxygenationJohn Anthony de GùzmanNo ratings yet
- Demo LPDocument3 pagesDemo LPNikki Anne BerlanasNo ratings yet
- Cardiovascular and Respiratory SystemDocument44 pagesCardiovascular and Respiratory SystemKlaudette Collin PaynorNo ratings yet
- Unit 2 Biology and Geology 3rd ESODocument64 pagesUnit 2 Biology and Geology 3rd ESOPaulaNo ratings yet
- Nursing Diagnosis For AsthmaDocument6 pagesNursing Diagnosis For AsthmaTINAIDA33% (3)
- Nursing Care PlansDocument3 pagesNursing Care PlansfanvicfayNo ratings yet
- Lung Sounds 3Document1 pageLung Sounds 3Kyle LatayanNo ratings yet
- Evers SafetyBook V3Document160 pagesEvers SafetyBook V3Gudruman EdisonNo ratings yet
- Every Cell in Your Body Needs Oxygen To LiveDocument12 pagesEvery Cell in Your Body Needs Oxygen To LiveSeraphim CamposNo ratings yet