Professional Documents
Culture Documents
Towards An Anti-Fibrotic Therapy For Scleroderma: Targeting Myofibroblast Differentiation and Recruitment
Towards An Anti-Fibrotic Therapy For Scleroderma: Targeting Myofibroblast Differentiation and Recruitment
Uploaded by
Mati AjaCopyright:
Available Formats
You might also like
- Ricardo v. Lloyd, Robert Y. Osamura, Gunter Kloppel, Juan Rosai - WHO Classification of Tumours of Endocrine Organs-IARC (2019)Document283 pagesRicardo v. Lloyd, Robert Y. Osamura, Gunter Kloppel, Juan Rosai - WHO Classification of Tumours of Endocrine Organs-IARC (2019)leartaNo ratings yet
- Test Bank For Essentials of Genetics 10th Edition William S KlugDocument9 pagesTest Bank For Essentials of Genetics 10th Edition William S KlugBarbara Hinkle100% (41)
- Essentials of Physical Anthropology 3rd Edition Clark Test BankDocument10 pagesEssentials of Physical Anthropology 3rd Edition Clark Test BankTravisChristensenfteir100% (15)
- GAPIT ManualDocument50 pagesGAPIT ManualNina MigueisNo ratings yet
- Biochemistry Extracellular MatrixDocument5 pagesBiochemistry Extracellular MatrixbrianhelbigNo ratings yet
- J Biocel 2006 11 005Document6 pagesJ Biocel 2006 11 005randomaeiou7273No ratings yet
- Macrophage Colony-Stimulating Factor and Cancer A ReviewDocument10 pagesMacrophage Colony-Stimulating Factor and Cancer A ReviewCristian Gutiérrez VeraNo ratings yet
- Anisa Zahra (190101030090) Final TLDocument34 pagesAnisa Zahra (190101030090) Final TLanisa zahraNo ratings yet
- My Elo PoiesisDocument6 pagesMy Elo PoiesisjonasNo ratings yet
- WRR 12952Document14 pagesWRR 12952randomaeiou7273No ratings yet
- Bmri2018 4578373Document13 pagesBmri2018 4578373dfkm5mjn7vNo ratings yet
- Involvement of Actin and Actin-Binding Proteins in CarcinogenesisDocument20 pagesInvolvement of Actin and Actin-Binding Proteins in CarcinogenesisVeronica JanethNo ratings yet
- Ai Apb#240055Document20 pagesAi Apb#240055Anonymous UJFK2jk5gNo ratings yet
- TGF B & Bone RemodelingDocument14 pagesTGF B & Bone RemodelingAzzahra zainunnisaNo ratings yet
- TGF-β Mediated SMAD Signaling NotesDocument5 pagesTGF-β Mediated SMAD Signaling Noteskim.yeuNo ratings yet
- Fimmu 03 00130Document18 pagesFimmu 03 00130Isabella1237No ratings yet
- Birkedal 1993Document11 pagesBirkedal 1993Héllen LacerdaNo ratings yet
- Hemopoiesis1Document17 pagesHemopoiesis1Octafiani Trikartika DarimanNo ratings yet
- Microenvironmental Regulation by Fibrillin-1: 1 January 2012 - Volume 8 - Issue 1 - E1002425Document16 pagesMicroenvironmental Regulation by Fibrillin-1: 1 January 2012 - Volume 8 - Issue 1 - E1002425Edin HamzicNo ratings yet
- Ulkus KorneaDocument23 pagesUlkus KorneaAurelia SuryaniNo ratings yet
- Platlate DisorderDocument76 pagesPlatlate DisordertoyyibNo ratings yet
- Ijmm 25 4 593 PDFDocument8 pagesIjmm 25 4 593 PDFNickNo ratings yet
- ACVR1R206H Extends Inflammatory Responses in Human Induced Pluripote 2021 BoDocument17 pagesACVR1R206H Extends Inflammatory Responses in Human Induced Pluripote 2021 BodianaNo ratings yet
- Effects of Collagen IV On Neuroblastoma Cell Matrix-Related FunctionsDocument9 pagesEffects of Collagen IV On Neuroblastoma Cell Matrix-Related FunctionsdjackapNo ratings yet
- Revisión 4Document12 pagesRevisión 4Natalia TorresNo ratings yet
- Metabolic Features of Multiple Myeloma: Molecular SciencesDocument19 pagesMetabolic Features of Multiple Myeloma: Molecular SciencesFirindaSoniyaNo ratings yet
- Angio GenesisDocument8 pagesAngio GenesisSamarTharwatNo ratings yet
- Phosphatidylinositol 3 - Kinase Signalling Supports Cell Height in Established Epithelial MonolayersDocument11 pagesPhosphatidylinositol 3 - Kinase Signalling Supports Cell Height in Established Epithelial MonolayersMohammed Elias AlamNo ratings yet
- Chhabra & Weeraratna 2023Document30 pagesChhabra & Weeraratna 2023Javiera FerradaNo ratings yet
- MegarariocitosDocument7 pagesMegarariocitosMartin GamboaNo ratings yet
- TransDocument2 pagesTransnazarovmuhammad1131No ratings yet
- The Mast Cell in Wound Healing (Pages 303-313)Document12 pagesThe Mast Cell in Wound Healing (Pages 303-313)jenNo ratings yet
- Cell Death 2011Document15 pagesCell Death 2011Paula Contreras MezaNo ratings yet
- NIH Public Access: Author ManuscriptDocument15 pagesNIH Public Access: Author ManuscriptarthoclaseNo ratings yet
- Quinderé Et Al 2015 PDFDocument9 pagesQuinderé Et Al 2015 PDFLuizaNo ratings yet
- Basic Concepts of Hematology (Hemostasis)Document53 pagesBasic Concepts of Hematology (Hemostasis)Hendra SshNo ratings yet
- Liver Fibrosis: ReviewDocument8 pagesLiver Fibrosis: ReviewmichaelNo ratings yet
- Physiological Functions of LMP2 B1i in The Female Reproductive SystemDocument4 pagesPhysiological Functions of LMP2 B1i in The Female Reproductive SystemEditor IJTSRDNo ratings yet
- Cell Stress, Inflammatory Responses and Cell Death: SynopsisDocument29 pagesCell Stress, Inflammatory Responses and Cell Death: SynopsisSasa PuiuNo ratings yet
- Clinical Flow Cytometry - Emerging ApplicationsDocument215 pagesClinical Flow Cytometry - Emerging ApplicationsDaoud IssaNo ratings yet
- JANA 2012 Curcumin As Anti-Endometriotic Agent Implication of MMP-3 and IntrinsicDocument8 pagesJANA 2012 Curcumin As Anti-Endometriotic Agent Implication of MMP-3 and IntrinsicCristiane HermesNo ratings yet
- tmp204 TMPDocument14 pagestmp204 TMPFrontiersNo ratings yet
- Megakaryocyte Development and Platelet Production: ReviewDocument14 pagesMegakaryocyte Development and Platelet Production: ReviewHikmanurulNo ratings yet
- SAJB 71 4 12 CDocument9 pagesSAJB 71 4 12 Cfarah azizahNo ratings yet
- The Regulation of Aging - Does Autophagy Underlie Longevity - PMCDocument15 pagesThe Regulation of Aging - Does Autophagy Underlie Longevity - PMCParth RanaNo ratings yet
- 02 Yeast Cell Architecture and FunctionDocument14 pages02 Yeast Cell Architecture and FunctionHugo SchmidtNo ratings yet
- Endocytic Deficiency Induced by ITSN-1s Knockdown Alters The Smad2/3-Erk1/2 Signaling Balance Downstream of Alk5Document14 pagesEndocytic Deficiency Induced by ITSN-1s Knockdown Alters The Smad2/3-Erk1/2 Signaling Balance Downstream of Alk5Sergeat18BNo ratings yet
- ArticleDocument14 pagesArticleOusmane KoneNo ratings yet
- Laminin TherapyDocument5 pagesLaminin TherapyCristian JimenezNo ratings yet
- Discuss The Role of Positive and Negative Regulators in HaemopoiesisDocument3 pagesDiscuss The Role of Positive and Negative Regulators in HaemopoiesisAlison HinesNo ratings yet
- The Effect of Hypoxia On Mesenchymal Stem Cell Biology: PharmaceuticalDocument9 pagesThe Effect of Hypoxia On Mesenchymal Stem Cell Biology: PharmaceuticalYolan TiaraNo ratings yet
- WithanolidoA Interfiere MicrofibrasDocument13 pagesWithanolidoA Interfiere MicrofibrascumbredinNo ratings yet
- KDM5B MacrophageDocument14 pagesKDM5B MacrophageMaurício DallowayNo ratings yet
- Kit and C Kit Mutations in MastocytosisDocument7 pagesKit and C Kit Mutations in Mastocytosisvcox4460No ratings yet
- Stemcells 2007-0416Document12 pagesStemcells 2007-0416Ikke OppgaveNo ratings yet
- Methods For Measuring Autophagy in Mice. Manon Moulis and Cécile VindisDocument14 pagesMethods For Measuring Autophagy in Mice. Manon Moulis and Cécile VindisAzael Torales CardeñaNo ratings yet
- Fibroblast-initiationTumor Rev2019Document30 pagesFibroblast-initiationTumor Rev2019Banchob SripaNo ratings yet
- Ijms 24 01571 v2Document15 pagesIjms 24 01571 v2BOURICHENo ratings yet
- ApoptosisDocument16 pagesApoptosisonur ateşNo ratings yet
- 2014-Echeverria C-Endotoxin-induced endothelial fibrosis is dependent on the expression of TGF-β1 and TGF-β2Document9 pages2014-Echeverria C-Endotoxin-induced endothelial fibrosis is dependent on the expression of TGF-β1 and TGF-β2Pablo Tapia BatallaNo ratings yet
- 7.kuliah Dasar Molekuler Kanker Part 2Document29 pages7.kuliah Dasar Molekuler Kanker Part 2eleldev100% (1)
- Peripheral Blood Leukocy 2008 Veterinary Clinics of North America Equine PRDocument21 pagesPeripheral Blood Leukocy 2008 Veterinary Clinics of North America Equine PRCristina ArribasNo ratings yet
- The Genetic Basis of Haematological CancersFrom EverandThe Genetic Basis of Haematological CancersSabrina TosiNo ratings yet
- Tissue Engineering and Regeneration in Dentistry: Current StrategiesFrom EverandTissue Engineering and Regeneration in Dentistry: Current StrategiesRachel J. WaddingtonNo ratings yet
- Accessories Package Price List: Items Basic Aero Aero Plus A Aero Plus BDocument1 pageAccessories Package Price List: Items Basic Aero Aero Plus A Aero Plus BMati AjaNo ratings yet
- Cde 0006 0119Document5 pagesCde 0006 0119Mati AjaNo ratings yet
- Localized Scleroderma: Clinical Spectrum and Therapeutic UpdateDocument12 pagesLocalized Scleroderma: Clinical Spectrum and Therapeutic UpdateMati AjaNo ratings yet
- Table 3 PrintDocument1 pageTable 3 PrintMati AjaNo ratings yet
- BIO 423L EXERCISE 2 Creating and Using Taxonomic Keys PDFDocument6 pagesBIO 423L EXERCISE 2 Creating and Using Taxonomic Keys PDFclairosusNo ratings yet
- Langman's Medical Embryology - CoverDocument11 pagesLangman's Medical Embryology - CoverAriesta Wijaya PutraNo ratings yet
- 2009 - Statistical Methods in Environmental EpidemiologyDocument449 pages2009 - Statistical Methods in Environmental EpidemiologyDaniela Sánchez AcostaNo ratings yet
- ADBT 1 Overview of BiotechnologyDocument42 pagesADBT 1 Overview of BiotechnologyMaham AdnanNo ratings yet
- Annexure - XVI - IIVR Annual Report English 2017-18 PDFDocument221 pagesAnnexure - XVI - IIVR Annual Report English 2017-18 PDFVishwambhara Dasa100% (1)
- PG M.sc. Zoology 35022 ImmunologyDocument241 pagesPG M.sc. Zoology 35022 ImmunologyJo FighizNo ratings yet
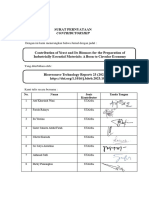
- 6.6. Contribution of Yeast and Its Biomass For The Preparation of Industrially - CSDocument16 pages6.6. Contribution of Yeast and Its Biomass For The Preparation of Industrially - CSFarida RahayuNo ratings yet
- BiologyDocument31 pagesBiologyPrinceton University Press100% (2)
- Answer Sheet - Module 6Document6 pagesAnswer Sheet - Module 6sjhdjshakjNo ratings yet
- Notes Biological Molecules 3Document8 pagesNotes Biological Molecules 3abdul rehmanNo ratings yet
- Igenomix UK Sample Requirements UKDocument2 pagesIgenomix UK Sample Requirements UKdrumerNo ratings yet
- STS Activity-18 Research-ActivityDocument2 pagesSTS Activity-18 Research-ActivityEvan Caringal SabioNo ratings yet
- Biomedical Science Coursework HelpDocument7 pagesBiomedical Science Coursework Helpdrrzjaifg100% (2)
- Role of Metal Ions in Dopamine Oxidation (1) (Autorecovered)Document19 pagesRole of Metal Ions in Dopamine Oxidation (1) (Autorecovered)intresting videoNo ratings yet
- Drug Resistance Pharmacology Lecture Lecture Series 2019Document23 pagesDrug Resistance Pharmacology Lecture Lecture Series 2019temitopeNo ratings yet
- Sample Paper Bs Bioinformatics and BiotechnologyDocument4 pagesSample Paper Bs Bioinformatics and BiotechnologySaad Hassan KheraNo ratings yet
- Protein SynthesisDocument24 pagesProtein SynthesisCOMPUTER ZONENo ratings yet
- Sepideh RQsDocument6 pagesSepideh RQsCésar HelenoNo ratings yet
- Bio 07 K1 (Perak)Document21 pagesBio 07 K1 (Perak)Ferguson TehNo ratings yet
- Chapter 6 The ABO Blood Group SystemDocument35 pagesChapter 6 The ABO Blood Group SystempartikNo ratings yet
- Cabrera Et Al. 2008 Araceae PhylogeneticsDocument13 pagesCabrera Et Al. 2008 Araceae PhylogeneticsGerardo A. SalazarNo ratings yet
- Le Syndrome de Bardet Biedl Endocrino 2008Document9 pagesLe Syndrome de Bardet Biedl Endocrino 2008Talala tililiNo ratings yet
- A New Theory Emerges Is Cancer A Fungus (Here Is The Evidence) - Humans Are Free (Humans Are Free) (Z-Library)Document10 pagesA New Theory Emerges Is Cancer A Fungus (Here Is The Evidence) - Humans Are Free (Humans Are Free) (Z-Library)sarapmaria97No ratings yet
- Assignment Chapter Covered Sexual Reproduction in Flowering Plants, Human Reproduction (Prepare These Lesson For Periodic Test-1)Document7 pagesAssignment Chapter Covered Sexual Reproduction in Flowering Plants, Human Reproduction (Prepare These Lesson For Periodic Test-1)PROPER GAMING MOBILENo ratings yet
- Biochem Task 9 BocalanbethinnaDocument4 pagesBiochem Task 9 BocalanbethinnaANA MARIA BETHINNA BOCALANNo ratings yet
- Abcam MOM IgG1,2a, 3 Linker Ordering InfoDocument2 pagesAbcam MOM IgG1,2a, 3 Linker Ordering InfoqinggaoiNo ratings yet
Towards An Anti-Fibrotic Therapy For Scleroderma: Targeting Myofibroblast Differentiation and Recruitment
Towards An Anti-Fibrotic Therapy For Scleroderma: Targeting Myofibroblast Differentiation and Recruitment
Uploaded by
Mati AjaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Towards An Anti-Fibrotic Therapy For Scleroderma: Targeting Myofibroblast Differentiation and Recruitment
Towards An Anti-Fibrotic Therapy For Scleroderma: Targeting Myofibroblast Differentiation and Recruitment
Uploaded by
Mati AjaCopyright:
Available Formats
Leask Fibrogenesis & Tissue Repair 2010, 3:8
http://www.fibrogenesis.com/content/3/1/8
Open Access
SHORT REVIEW
Towards an anti-fibrotic therapy for scleroderma:
targeting myofibroblast differentiation and
recruitment
Short review
Andrew Leask
Abstract
Background: In response to normal tissue injury, fibroblasts migrate into the wound where they synthesize and
remodel new extracellular matrix. The fibroblast responsible for this process is called the myofibroblast, which
expresses the highly contractile protein -smooth muscle actin (-SMA). In normal tissue repair, the myofibroblast
disappears. Conversely, abnormal myofibroblast persistence is a key feature of fibrotic dieases, including scleroderma
(systemic sclerosis, SSc). Myofibroblasts can be derived from differentiation of local resident fibroblasts or by
recruitment of microvascular pericytes.
Clinical problem addressed: Controlling myofibroblast differentiation and persistence is crucial for developing antifibrotic therapies targeting SSc.
Basic science advances: Insights have been recently generated into how the proteins transforming growth factor
(TGF), endothelin-1 (ET-1), connective tissue growth factor (CCN2/CTGF) and platelet derived growth factor (PDGF)
contribute to myofibroblast differentiation and pericyte recruitment in general and to the persistent myofibroblast
phenotype of lesional SSc fibroblast, specifically.
Relevance to clinical care: This minireview summarizes recent findings pertinent to the origin of myofibroblasts in
SSc and how this knowledge might be used to control the fibrosis in this disease.
Conclusions: TGF, ET-1, CCN2 and PDGF are likely to cooperate in driving tissue repair and fibrogenic responses in
fibroblasts. TGF, ET-1 and CCN2 appear to contribute to myofibroblast differentiation; PDGF appears to be involved
with pericyte recruitment. Thus, different therapeutic strategies may exist for targeting the multisystem fibrotic
disorder SSc.
Introduction
When connective tissue is damaged, fibroblasts migrate
into the wound and begin to produce and remodel extracellular matrix (ECM) [1]. These events involve a specific
sort of fibroblast termed the myofibroblast, a cell type
which expresses the highly contractile protein -smooth
muscle actin (-SMA) [1]. The -SMA protein is organized into stress fibres which are connected to the ECM
through specialized so-called 'supermature' FAs. As a
result, these -SMA stress fibers can contract and exert
mechanical tension on the ECM causing it to be reorga* Correspondence: andrew.leask@schulich.uwo.ca
1
Division of Oral Biology, Department of Dentistry, Schulich School of
Medicine and Dentistry University of Western Ontario, Dental Sciences
Building, London ON N6A 5C1 Canada
nized into functional connective tissue. Myofibroblast
persistence is believed to be responsible for fibrotic diseases including scleroderma (SSc; Figure 1) [1,2].
Myofibroblasts have multiple origins, possibly appearing, for example, by differentiation of local, resident
fibroblasts in response to proteins or by the migration of
microvascular pericytes into the lesional area [1] (Figure
1). Understanding how myofibroblasts may originate may
be useful in understanding how to combat the fibrosis
observed in SSc, and this is the subject of this minireview.
Transforming growth factor- (TGF-)
Extensive reviews on TGF signalling and the contribution of this pathway to experimentally-induced fibrosis
have been published elsewhere (for example, see [3]).
Full list of author information is available at the end of the article
2010 Leask; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any
medium, provided the original work is properly cited.
Leask Fibrogenesis & Tissue Repair 2010, 3:8
http://www.fibrogenesis.com/content/3/1/8
Page 2 of 5
PERICYTE
RECRUITMENT
PDGF
microvasculature
Myofibroblasts
(-SMA, collagen
production;
ECM contraction)
FIBROBLAST
DIFFERENTIATION
TGF,ET-1, CCN2
Resident fibroblasts
Figure 1 Model of myofibroblast origin in skin lesions of scleroderma patients. Transforming growth factor , endothelin-1 and
CCN2 can enhance differentiation of resident fibroblasts to myofibroblasts; platelet derived growth factor promotes pericyte recruitment.
Briefly, there are three TGF isoforms, TGF1, TGF2
and TGF3. These are initially generated as latent precursors from which active TGF is liberated by proteolysis,
enabling it to bind to a heteromeric receptor complex
consisting of one TGF type I [termed activin linked
kinase 5 (ALK5) in the case of fibroblasts] and one TGF
type II receptor. ALK5 phosphorylates Smad2 and 3,
which can then bind Smad4, translocates into the nucleus
and activate transcription. The ALK5/Smad pathway is
generally responsible for TGF signalling in fibroblasts.
In normal fibroblasts, ALK5 appears to mediate the fibrogenic activity of TGF [4]. Recombinant TGF is fibrogenic in both in vitro and in vivo models of fibrogenesis,
acting through ALK5/Smad3 [3]. The contribution of this
canonical TGF pathway on the persistent fibrotic phenotype of lesional SSc fibroblasts has been evaluated.
Targeting ALK5, using small molecule inhibitors,
reverses some aspects of lesional dermal scleroderma
fibroblasts but, critically, does not reduce -SMA or
CCN2 protein expression or -SMA stress fibre formation in this cell type [2,5,6]. These results are consistent
with data showing that Smad3 is not involved with CCN2
overexpression in SSc fibroblasts [7]. These observations
exist in spite of the fact that there is a trend towards
heightened Smad3 phosphorylation and nuclear localization in SSc fibroblasts compared to their healthy counterparts [8].
An interesting series of recent experiments have suggested the possibility that heightened activity of Smad1
may contribute to the pathogenesis of SSc [9]. This phenomenon appears to arise due to an alteration in the ratio
of the levels of the TGF type I receptor to the TGF type
II receptor. In SSc fibroblasts, there is an elevation in the
amount of the TGF type I receptor which may contribute to the overexpression of type I collagen in these cells
[10]. Overexpression of ALK5 caused an increase in collagen production by fibroblasts [10,11]. This up-regulation
of collagen does not appear to involve the kinase activity
of ALK5 or Smad2/3 activation but experiments using
mutant TGF receptors and siRNAs show that this phe-
nonomenon appears to be mediated by ALK1/Smad1 and
ERK1/2 pathways [9]. Overall, these data suggest that
canonical ALK5/Smad signalling is likely to contribute to
but not be the fundamental basis of the persistent fibrotic
phenotype of lesional SSc fibroblasts and suggest that
blocking non-canonical TGF pathways may be a better
alternative in combating the persistent fibrotic phenotype
in SSc [12,13].
In addition to the ALK5/Smad pathway, TGF activates
additional signalling pathways including: ras/MEK/ERK,
which requires the heparan sulphate-containing proteoglycan (HSPG) syndecan 4; p38, which requires the
HSPG betaglycan and JNK which requires focal adhesion
kinase (FAK) and TGF activated kinase 1 (TAK1)
[2,14,15]. These pathways appear to modify gene expression in a promoter-selective fashion. For example, FAK,
JNK and TAK1 are required for myofibroblast differentiation and -SMA expression [14,15]. Whereas extra cellular signal-regulated kinase (ERK) is required for CCN2
and collagen type I expression [16,17], p38 appears to be
not involved with the fibrogenic activity of TGF [4].
Constitutive TAK1 and JNK activation independent of
ALK5 is seen in SSc fibroblasts [14,18]; thus, it is likely
that signalling pathways are abnormally activated in SSc
fibroblasts in a fashion independent of the canonical
TGF pathway. It is likely that targeting FAK, JNK or
TAK1 may be beneficial in alleviating the persistent SSc
phenotype of dermal fibroblasts.
Endothelin-1 (ET-1)
There are 3 isoforms of endothelin, namely ET-1, ET-2,
and ET-3 [12]. ET-1, the significant isoform in humans, is
normally produced by a variety of cell types including
endothelial cells, epithelial cells, bone marrow mast cells,
macrophages, polymorphonuclear leukocytes, cardiomyocytes, and fibroblasts [12]. Initially, ET-1 is produced
in the form of a 212-amino acid precursor (prepro-ET-1)
which is enzymatically cleaved to form a biologically
active 21-amino acid peptide [12]. ET-1 can then bind its
two receptors (ETA and ETB) [12].
ET-1 induces ECM production in fibroblasts through
the ETA and ETB receptors and MEK/ERK, whereas ET-1
induces myofibroblast formation, migration and ECM
contraction through ETA and Akt/rac [19,20] (Figure 1).
TGF induces ET-1 through JNK, and ET-1 is a downstream mediator of at least some of fibrotic responses of
fibroblasts to TGF [18,21]. Constitutive ET signalling,
operating through TAK1/JNK-dependent and ALK5independent mechanisms, is responsible for the persistent myofibroblast phenotype of SSc lung fibroblasts [18].
Consistent with the notion that ET-1 contributes to fibrosis in the lung, ET receptor antagonism alleviates bleomycin-induced lung fibrosis and TGF-induced skin
fibrogenesis in vivo [22,23]. However, the effect of ET
Leask Fibrogenesis & Tissue Repair 2010, 3:8
http://www.fibrogenesis.com/content/3/1/8
inhibition on SSc dermal fibroblasts has not yet been
tested. TGF appears to also cooperate with ET-1 to promote myofibroblast differentiation [24]. The ET receptor
antagonist bosentan may also be effective at reducing
skin fibrosis in patients with SSc [25]. These results suggest that endothelin receptor antagonism might be considered as an appropriate therapy for the fibrosis in SSc,
possibly in combination with anti-TGF regimens.
CCN2
CCN2, a member of the CCN family of matricellular proteins, is an excellent surrogate marker for the severity of
fibrosis in SSc [26]. CCN2 signals through a variety of
integrins and HSPGs or trkA and promotes cell adhesion
and enhances adhesive signaling in response to extracellular ligands [27]. CCN2 is induced by both TGF and
ET-1 and is considered to be a downstream mediator of
these proteins [12]. The CCN2 promoter appears to possess independent TGF and ET-1 response elements
[16,20] and thus may be a common downstream mediator
of the fibrotic effects of these proteins, and thus may represent a more attractive target than either protein alone.
CCN2 acts as a cofactor with TGF to induce fibrogenesis but is not considered to be a potent fibrogenic agent
on its own [28,29] (Figure 1). However, a recent study
revealed chronic overexpression of CCN2 can lead to a
fibrotic phenotype [30]. CCN2 is not required for all of
the activities of TGF actions but appears to be required
for TGF to maximally induce certain mRNAs including
type I collagen and -SMA and for TGF to promote cell
adhesion to ECM [31] (Figure 1). CCN2 also can activate
ERK by a syndecan 4-dependent mechanism [32]. A
CCN2 response element exists in the COL1A2 promoter;
blocking CCN2 action using an anti-CCN2 antibody or
siRNA reduces some effects of bleomycin-induced lung
fibrosis [33]. Overall, the available data suggest that targeting CCN2 may be useful in combating fibrosis in SSc.
Platelet derived growth factor (PDGF)
The PDGF family includes PDGF-AA, PDGF-AB, PDGFBB, PDGF-CC and PDGF-DD. These bind two different
PDGF receptors, and [34]. PDGF causes neutrophils,
macrophages, fibroblasts and smooth muscle cells to proliferate and migrate into the wound site [34]. In vitro,
PGDF stimulates fibroblasts to contract collagen matrices
and differentiate into myofibroblasts [35].
Studies have revealed that PDGF levels are elevated in
the bronchial lavage fluid of SSc patients, as well as elevated levels of the PDGF receptors on SSc fibroblasts
[36-38]. Moreover, one study has been reported showing
that autoantibodies stimulating the PDGF receptor may
be a hallmark of SSc [39].
Mice treated with PDGF receptor- inhibitor imatinib
mesylate, a tyrosine kinase inhibitor exhibit delayed cuta-
Page 3 of 5
neous wound closure, diminished numbers of myofibroblast numbers and reduced collagen type I expression
[40]. Imatinib mesylate did not prevent the myofibroblast
differentiation in vitro but inhibited fibroblast proliferation and migration and appeared to principally act by
blocking pericyte recruitment [40] (Figure 1). As a subset
(~30%) of myofibroblasts in cutaneous mouse wounds
are NG2-positive pericytes, this phenomenon is likely to
lead to the reduction myofibroblasts in the wound [41].
Intriguingly, however, the majority (~70%) of myofibroblasts in bleomycin-induced skin fibrosis are derived
from pericytes [42]. Tyrosine kinase inhibitors analogous
to imatinib mesylate blocked bleomycin-induced dermal
fibrosis in mice [43]. It is also interesting to note that imatinib mesylate also blocks the ability of TGF to activate
Smad 1 and the transcription factor egr-1 via c-abl,
emphasizing the potential of signalling crosstalk between
PDGF and non-canonical TGF signalling and further
suggesting that this inhibitor may also work by blocking
non-canonical TGF signalling [44,45]. Given that pericytes contribute to myofibroblast activation in SSc [46],
these results collectively suggest that perhaps targeting
PDGF/c-abl might be of benefit in SSc through its ability
to block pericyte recruitment. As such, anti-PDGF drugs
may represent a different sort of approach to alleviating
SSc than blocking growth factor differentiation of resident fibroblasts, which may be of lesser importance than
pericyte recruitment in generating a source of myofibroblasts in fibrosis.
Future Prospects and Conclusions
TGF, ET-1, CCN2 and PDGF are likely to cooperate in
driving tissue repair and fibrogenic responses in lesional
SSc fibroblasts. However, these proteins seem to be
responsible, for somewhat differing activities suggesting
that combination therapies may be appropriate for SSc.
Abbreviations
-SMA: -smooth muscle actin; CTGF: connective tissue growth factor; ECM:
extracellular matrix; ERK: extracellular signal-regulated kinase-1; ET: endothelin;
FAK: focal adhesion kinase; HSPG: heparan sulphate-containing proteoglycan;
PDGF: platelet derived growth factor; SSc: systemic sclerosis; TGF: transforming growth factor ; TAK: TGF activated kinase 1
Competing interests
The author declares that they have no competing interests.
Acknowledgements
AL is supported by the Canadian Institute of Health Research, the Ontario Thoracic Society and the Canadian Foundation for Innovation and is an Arthritis
Society (Scleroderma Society of Ontario) New Investigator.
Author Details
Division of Oral Biology, Department of Dentistry, Schulich School of Medicine
and Dentistry University of Western Ontario, Dental Sciences Building, London
ON N6A 5C1 Canada
Received: 3 December 2009 Accepted: 27 May 2010
Published: 27 May 2010
This
Fibrogenesis
2010
is
article
an
Leask;
Open
is&available
licensee
Tissue
Access
Repair
from:
BioMed
article
2010,
http://www.fibrogenesis.com/content/3/1/8
distributed
Central
3:8 Ltd.
under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Leask Fibrogenesis & Tissue Repair 2010, 3:8
http://www.fibrogenesis.com/content/3/1/8
References
1. Hinz B, Phan SH, Thannickal VJ, Galli A, Bochaton-Piallat ML, Gabbiani G:
The myofibroblast: one function, multiple origins. Am J Pathol 2007,
170:1807-1816.
2. Chen Y, Shiwen X, van Beek J, Kennedy L, McLeod M, Renzoni EA, BouGharios G, Wilcox-Adelman S, Goetinck PF, Eastwood M, Black CM,
Abraham DJ, Leask A: Matrix contraction by dermal fibroblasts requires
TGFbeta/ALK5, heparan sulfate containing proteoglycans and MEK/
ERK: Insights into pathological scarring in chronic fibrotic disease. Am
J Pathol 2005, 167:1699-1711.
3. Denton CP, Abraham DJ: Transforming growth factor-beta and
connective tissue growth factor: key cytokines in scleroderma
pathogenesis. Curr Opin Rheumatol 2001, 13:505-511.
4. Kapoun AM, Gaspar NJ, Wang Y, Damm D, Liu YW, O'young G, Quon D,
Lam A, Munson K, Tran TT, Ma JY, Murphy A, Dugar S, Chakravarty S,
Protter AA, Wen FQ, Liu X, Rennard SI, Higgins LS: Transforming growth
factor-beta receptor type 1 (TGFbetaRI) kinase activity but not p38
activation is required for TGFbetaRI-induced myofibroblast
differentiation and profibrotic gene expression. Mol Pharmacol 2006,
70:518-531.
5. Chen Y, Shi-wen X, Eastwood M, Black CM, Denton CP, Leask A, Abraham
DJ: Contribution of activin receptor-like kinase 5 (transforming growth
factor beta receptor type I) signaling to the fibrotic phenotype of
scleroderma fibroblasts. Arthritis Rheum 2006, 54:1309-1316.
6. Ishida W, Mori Y, Lakos G, Sun L, Shan F, Bowes S, Josiah S, Lee WC, Singh J,
Ling LE, Varga J: Intracellular TGF-beta receptor blockade abrogates
Smad-dependent fibroblast activation in vitro and in vivo. J Invest
Dermatol 2006, 126:1733-1744.
7. Holmes A, Abraham DJ, Sa S, Shiwen X, Black CM, Leask A: CTGF and
SMADs, maintenance of scleroderma phenotype is independent of
SMAD signaling. J Biol Chem 2001, 276:10594-10601.
8. Mori Y, Chen SJ, Varga J: Expression and regulation of intracellular SMAD
signaling in scleroderma skin fibroblasts. Arthritis Rheum 2003,
48:1964-1978.
9. Pannu J, Nakerakanti S, Smith E, ten Dijke P, Trojanowska M: Transforming
growth factor-beta receptor type I-dependent fibrogenic gene
program is mediated via activation of Smad1 and ERK1/2 pathways. J
Biol Chem 2007, 282:10405-10413.
10. Pannu J, Gore-Hyer E, Yamanaka M, Smith EA, Rubinchik S, Dong JY,
Jablonska S, Blaszczyk M, Trojanowska M: An increased transforming
growth factor beta receptor type I:type II ratio contributes to elevated
collagen protein synthesis that is resistant to inhibition via a kinasedeficient transforming growth factor beta receptor type II in
scleroderma. Arthritis Rheum 2004, 50:1566-1577.
11. Pannu J, Gardner H, Shearstone JR, Smith E, Trojanowska M: Increased
levels of transforming growth factor beta receptor type I and upregulation of matrix gene program: A model of scleroderma. Arthritis
Rheum 2006, 54:3011-3021.
12. Leask A: Targeting the TGF, endothelin-1 and CCN2 axis to combat
fibrosis in scleroderma. Cell Signal 2008, 20:1409-1414.
13. Trojanowska M: Noncanonical transforming growth factor beta
signaling in scleroderma fibrosis. Curr Opin Rheumatol 2009, 21:623-629.
14. Shi-wen X, Parapuram SK, Pala D, Chen Y, Carter D, Eastwood M, Abraham
DJ, Leask A: TGF induced -smooth muscle actin expression and
extracellular matrix contraction in fibroblasts requires TAK1. Arthritis
Rheum 2009, 60:234-241.
15. Thannickal VJ, Lee DY, White ES, Cui Z, Larios JM, Chacon R, Horowitz JC,
Day RM, Thomas PE: Myofibroblast differentiation by transforming
growth factor-beta1 is dependent on cell adhesion and integrin
signaling via focal adhesion kinase. J Biol Chem 2003, 278:12384-12389.
16. Leask A, Holmes A, Black CM, Abraham DJ: Connective tissue growth
factor gene regulation Requirements for its induction by transforming
growth factor-beta 2 in fibroblasts. J Biol Chem 2003, 278:13008-13015.
17. Li F, Zeng B, Chai Y, Cai P, Fan C, Cheng T: The linker region of Smad2
mediates TGF-beta-dependent ERK2-induced collagen synthesis.
Biochem Biophys Res Commun 2009, 386(2):289-293.
18. Shi-wen X, Rodrigues-Pascua F, Lamas S, Holmes A, Howat S, Pearson JD,
Dashwood MR, du Bois RM, Denton CP, Black CM, Abraham DJ, Leask A:
Constitutive ALK5-indepenent JNK activation contributes to
endothelin-1 over-expression in pulmonary fibrosis. Mol Cell Biol 2006,
26:5518-5527.
Page 4 of 5
19. Shi-Wen X, Chen Y, Denton CP, Eastwood M, Renzoni EA, Bou-Gharios G,
Pearson JD, Dashwood M, du Bois RM, Black CM, Leask A, Abraham DJ:
Endothelin-1 promotes myofibroblast induction through the ETA
receptor via a rac/phosphoinositide 3-kinase/Akt-dependent pathway
and is essential for the enhanced contractile phenotype of fibrotic
fibroblasts. Mol Biol Cel 2004, 15:2707-1279.
20. Xu SW, Howat SL, Renzoni EA, Holmes A, Pearson JD, Dashwood MR, BouGharios G, Denton CP, du Bois RM, Black CM, Leask A, Abraham DJ:
Endothelin-1 induces expression of matrix-associated genes in lung
fibroblasts through MEK/ERK. J Biol Chem 2004, 279:23098-23103.
21. Shi-wen X, Kennedy L, Renzoni E, du Bois R, Denton C, Black C, Abraham D,
Leask A: Endothelin-1 is a downstream mediator of TGF in fibroblasts.
Arthritis Rheum 2007, 56:4189-4194.
22. Park SH, Saleh D, Giaid A, Michel RP: Increased endothelin-1 in
bleomycin-induced pulmonary fibrosis and the effect of an endothelin
receptor antagonist. Am J Respir Crit Care Med 1997, 156:600-608.
23. Lagares D, Garca-Fernndez RA, Jimnez CL, Magn-Marchal N,
Busnadiego O, Lamas S, Rodrguez-Pascual F: Endothelin 1 contributes to
the effect of transforming growth factor beta1 on wound repair and
skin fibrosis. Arthritis Rheum 2010, 62:878-889.
24. Shephard P, Hinz B, Smola-Hess S, Meister JJ, Krieg T, Smola H: Dissecting
the roles of endothelin, TGF-beta and GM-CSF on myofibroblast
differentiation by keratinocytes. Thromb Haemost 2004, 92:262-274.
25. Kuhn A, Haust M, Ruland V, Weber R, Verde P, Felder G, Ohmann C, Gensch
K, Ruzicka T: Effect of bosentan on skin fibrosis in patients with systemic
sclerosis: a prospective, open-label, non-comparative trial.
Rheumatology (Oxford) 2010 in press.
26. Takehara K: Hypothesis: pathogenesis of systemic sclerosis. J Rheumatol
2003, 30:755-759.
27. Chen CC, Lau LF: Functions and mechanisms of action of CCN
matricellular proteins. Int J Biochem Cell Biol 2009, 41:771-783.
28. Mori T, Kawara S, Shinozaki M, Hayashi N, Kakinuma T, Igarashi A, Takigawa
M, Nakanishi T, Takehara K: Role and interaction of connective tissue
growth factor with transforming growth factor-beta in persistent
fibrosis: a mouse fibrosis model. J Cell Physiol 1999, 181:153-159.
29. Bonniaud P, Martin G, Margetts PJ, Ask K, Robertson J, Gauldie J, Kolb M:
Connective tissue growth factor is crucial to inducing a profibrotic
environment in 'fibrosis-resistant' BALB/c mouse lungs. Am J Respir Cell
Mol Biol 2004, 31:510-516.
30. Sonnylal S, Shi-Wen X, Leoni P, Naff K, Van Pelt C, Nakamura H, Leask A,
Abraham D, Bou-Gharios G, de Crombrugghe B: Selective expression of
connective tissue growth factor in fibroblasts in vivo promotes
systemic tissue fibrosis. Arthritis Rheum 2010, 62:1523-32.
31. Shi-wen X, Stanton L, Kennedy L, Pala D, Chen Y, Howat SL, Renzoni EA,
Carter DE, Bou-Gharios G, Stratton RJ, Pearson JD, Beier F, Lyons KM, Black
CM, Abraham DJ, Leask A: CCN2 is necessary for adhesive responses to
TGF1 in embryonic fibroblasts. J Biol Chem 2006, 281:10715-10726.
32. Kennedy L, Liu S, Shi-wen X, Carter D, Lyons K, Black CM, Abraham DJ,
Leask A: CCN2 is essential for fibroblast function. Expl Cell Res 2007,
313:952-964.
33. Ponticos M, Holmes AM, Shiwen X, Leoni Pl, Khan K, Rajkumar VS, Hoyles
RK, Bou-Gharios G, Black CM, Denton CP, Abraham DJ, Leask A, Lindahl GE:
Pivotal role of connective tissue growth factor in lung fibrosis: MAPKdependent transcriptional activation of type I collagen. Arthritis Rheum
2009, 60:2142-2155.
34. Bonner JC: Regulation of PDGF and its receptors in fibrotic diseases.
Cytokine Growth Factor Rev 2004, 15:255-273.
35. Rhee S, Grinnell F: P21-activated kinase 1: convergence point in PDGFand LPA-stimulated collagen matrix contraction by human fibroblasts.
J Cell Biol 2006, 172:423-432.
36. Ludwicka A, Ohba T, Trojanowska M, Yamakage A, Strange C, Smith EA,
Leroy EC, Sutherland S, Silver RM: Elevated levels of platelet derived
growth factor and transforming growth factor-beta 1 in
bronchoalveolar lavage fluid from patients with scleroderma. J
Rheumatol 1995, 22:1876-1883.
37. Klareskog L, Gustafsson R, Scheynius A, Hllgren R: Increased expression
of platelet-derived growth factor type B receptors in the skin of
patients with systemic sclerosis. Arthritis Rheum 1990, 33:1534-1541.
38. Zheng XY, Zhang JZ, Tu P, Ma SQ: Expression of platelet-derived growth
factor B-chain and platelet-derived growth factor beta-receptor in
fibroblasts of scleroderma. J Dermatol Sci 1998, 18:90-97.
Leask Fibrogenesis & Tissue Repair 2010, 3:8
http://www.fibrogenesis.com/content/3/1/8
39. Baroni SS, Santillo M, Bevilacqua F, Luchetti M, Spadoni T, Mancini M,
Fraticelli P, Sambo P, Funaro A, Kazlauskas A, Avvedimento EV, Gabrielli A:
Stimulatory autoantibodies to the PDGF receptor in systemic sclerosis.
N Engl J Med 2006, 354:2667-2676.
40. Rajkumar VS, Shiwen X, Bostrom M, Leoni P, Muddle J, Ivarsson M, Gerdin
B, Denton CP, Bou-Gharios G, Black CM, Abraham DJ: Platelet-derived
growth factor-beta receptor activation is essential for fibroblast and
pericyte recruitment during cutaneous wound healing. Am J Pathol
2006, 169:2254-2265.
41. Kapoor M, Liu S, Huh K, Parapuram S, Kennedy L, Leask A: Connective
tissue growth factor promoter activity in normal and wounded skin.
Fibrogenesis Tissue Repair 2008, 1:3.
42. Liu S, Taghavi R, Leask A: Connective tissue growth factor is induced in
bleomycin-induced skin scleroderma. J Cell Commun Signal 2010,
4:25-30.
43. Akhmetshina A, Dees C, Pileckyte M, Maurer B, Axmann R, Jngel A,
Zwerina J, Gay S, Schett G, Distler O, Distler JH: Dual inhibition of c-abl
and PDGF receptor signaling by dasatinib and nilotinib for the
treatment of dermal fibrosis. FASEB J 2008, 22:2214-2222.
44. Bhattacharyya S, Ishida W, Wu M, Wilkes M, Mori Y, Hinchcliff M, Leof E,
Varga J: A non-Smad mechanism of fibroblast activation by
transforming growth factor-beta via c-Abl and Egr-1: selective
modulation by imatinib mesylate. Oncogene 2009, 28:1285-1297.
45. Pannu J, Asano Y, Nakerakanti S, Smith E, Jablonska S, Blaszczyk M, ten
Dijke P, Trojanowska M: Smad1 pathway is activated in systemic
sclerosis fibroblasts and is targeted by imatinib mesylate. Arthritis
Rheum 2008, 58:2528-2537.
46. Rajkumar VS, Sundberg C, Abraham DJ, Rubin K, Black CM: Activation of
microvascular pericytes in autoimmune Raynaud's phenomenon and
systemic sclerosis. Arthritis Rheum 1999, 42:930-941.
doi: 10.1186/1755-1536-3-8
Cite this article as: Leask, Towards an anti-fibrotic therapy for scleroderma:
targeting myofibroblast differentiation and recruitment Fibrogenesis & Tissue
Repair 2010, 3:8
Page 5 of 5
You might also like
- Ricardo v. Lloyd, Robert Y. Osamura, Gunter Kloppel, Juan Rosai - WHO Classification of Tumours of Endocrine Organs-IARC (2019)Document283 pagesRicardo v. Lloyd, Robert Y. Osamura, Gunter Kloppel, Juan Rosai - WHO Classification of Tumours of Endocrine Organs-IARC (2019)leartaNo ratings yet
- Test Bank For Essentials of Genetics 10th Edition William S KlugDocument9 pagesTest Bank For Essentials of Genetics 10th Edition William S KlugBarbara Hinkle100% (41)
- Essentials of Physical Anthropology 3rd Edition Clark Test BankDocument10 pagesEssentials of Physical Anthropology 3rd Edition Clark Test BankTravisChristensenfteir100% (15)
- GAPIT ManualDocument50 pagesGAPIT ManualNina MigueisNo ratings yet
- Biochemistry Extracellular MatrixDocument5 pagesBiochemistry Extracellular MatrixbrianhelbigNo ratings yet
- J Biocel 2006 11 005Document6 pagesJ Biocel 2006 11 005randomaeiou7273No ratings yet
- Macrophage Colony-Stimulating Factor and Cancer A ReviewDocument10 pagesMacrophage Colony-Stimulating Factor and Cancer A ReviewCristian Gutiérrez VeraNo ratings yet
- Anisa Zahra (190101030090) Final TLDocument34 pagesAnisa Zahra (190101030090) Final TLanisa zahraNo ratings yet
- My Elo PoiesisDocument6 pagesMy Elo PoiesisjonasNo ratings yet
- WRR 12952Document14 pagesWRR 12952randomaeiou7273No ratings yet
- Bmri2018 4578373Document13 pagesBmri2018 4578373dfkm5mjn7vNo ratings yet
- Involvement of Actin and Actin-Binding Proteins in CarcinogenesisDocument20 pagesInvolvement of Actin and Actin-Binding Proteins in CarcinogenesisVeronica JanethNo ratings yet
- Ai Apb#240055Document20 pagesAi Apb#240055Anonymous UJFK2jk5gNo ratings yet
- TGF B & Bone RemodelingDocument14 pagesTGF B & Bone RemodelingAzzahra zainunnisaNo ratings yet
- TGF-β Mediated SMAD Signaling NotesDocument5 pagesTGF-β Mediated SMAD Signaling Noteskim.yeuNo ratings yet
- Fimmu 03 00130Document18 pagesFimmu 03 00130Isabella1237No ratings yet
- Birkedal 1993Document11 pagesBirkedal 1993Héllen LacerdaNo ratings yet
- Hemopoiesis1Document17 pagesHemopoiesis1Octafiani Trikartika DarimanNo ratings yet
- Microenvironmental Regulation by Fibrillin-1: 1 January 2012 - Volume 8 - Issue 1 - E1002425Document16 pagesMicroenvironmental Regulation by Fibrillin-1: 1 January 2012 - Volume 8 - Issue 1 - E1002425Edin HamzicNo ratings yet
- Ulkus KorneaDocument23 pagesUlkus KorneaAurelia SuryaniNo ratings yet
- Platlate DisorderDocument76 pagesPlatlate DisordertoyyibNo ratings yet
- Ijmm 25 4 593 PDFDocument8 pagesIjmm 25 4 593 PDFNickNo ratings yet
- ACVR1R206H Extends Inflammatory Responses in Human Induced Pluripote 2021 BoDocument17 pagesACVR1R206H Extends Inflammatory Responses in Human Induced Pluripote 2021 BodianaNo ratings yet
- Effects of Collagen IV On Neuroblastoma Cell Matrix-Related FunctionsDocument9 pagesEffects of Collagen IV On Neuroblastoma Cell Matrix-Related FunctionsdjackapNo ratings yet
- Revisión 4Document12 pagesRevisión 4Natalia TorresNo ratings yet
- Metabolic Features of Multiple Myeloma: Molecular SciencesDocument19 pagesMetabolic Features of Multiple Myeloma: Molecular SciencesFirindaSoniyaNo ratings yet
- Angio GenesisDocument8 pagesAngio GenesisSamarTharwatNo ratings yet
- Phosphatidylinositol 3 - Kinase Signalling Supports Cell Height in Established Epithelial MonolayersDocument11 pagesPhosphatidylinositol 3 - Kinase Signalling Supports Cell Height in Established Epithelial MonolayersMohammed Elias AlamNo ratings yet
- Chhabra & Weeraratna 2023Document30 pagesChhabra & Weeraratna 2023Javiera FerradaNo ratings yet
- MegarariocitosDocument7 pagesMegarariocitosMartin GamboaNo ratings yet
- TransDocument2 pagesTransnazarovmuhammad1131No ratings yet
- The Mast Cell in Wound Healing (Pages 303-313)Document12 pagesThe Mast Cell in Wound Healing (Pages 303-313)jenNo ratings yet
- Cell Death 2011Document15 pagesCell Death 2011Paula Contreras MezaNo ratings yet
- NIH Public Access: Author ManuscriptDocument15 pagesNIH Public Access: Author ManuscriptarthoclaseNo ratings yet
- Quinderé Et Al 2015 PDFDocument9 pagesQuinderé Et Al 2015 PDFLuizaNo ratings yet
- Basic Concepts of Hematology (Hemostasis)Document53 pagesBasic Concepts of Hematology (Hemostasis)Hendra SshNo ratings yet
- Liver Fibrosis: ReviewDocument8 pagesLiver Fibrosis: ReviewmichaelNo ratings yet
- Physiological Functions of LMP2 B1i in The Female Reproductive SystemDocument4 pagesPhysiological Functions of LMP2 B1i in The Female Reproductive SystemEditor IJTSRDNo ratings yet
- Cell Stress, Inflammatory Responses and Cell Death: SynopsisDocument29 pagesCell Stress, Inflammatory Responses and Cell Death: SynopsisSasa PuiuNo ratings yet
- Clinical Flow Cytometry - Emerging ApplicationsDocument215 pagesClinical Flow Cytometry - Emerging ApplicationsDaoud IssaNo ratings yet
- JANA 2012 Curcumin As Anti-Endometriotic Agent Implication of MMP-3 and IntrinsicDocument8 pagesJANA 2012 Curcumin As Anti-Endometriotic Agent Implication of MMP-3 and IntrinsicCristiane HermesNo ratings yet
- tmp204 TMPDocument14 pagestmp204 TMPFrontiersNo ratings yet
- Megakaryocyte Development and Platelet Production: ReviewDocument14 pagesMegakaryocyte Development and Platelet Production: ReviewHikmanurulNo ratings yet
- SAJB 71 4 12 CDocument9 pagesSAJB 71 4 12 Cfarah azizahNo ratings yet
- The Regulation of Aging - Does Autophagy Underlie Longevity - PMCDocument15 pagesThe Regulation of Aging - Does Autophagy Underlie Longevity - PMCParth RanaNo ratings yet
- 02 Yeast Cell Architecture and FunctionDocument14 pages02 Yeast Cell Architecture and FunctionHugo SchmidtNo ratings yet
- Endocytic Deficiency Induced by ITSN-1s Knockdown Alters The Smad2/3-Erk1/2 Signaling Balance Downstream of Alk5Document14 pagesEndocytic Deficiency Induced by ITSN-1s Knockdown Alters The Smad2/3-Erk1/2 Signaling Balance Downstream of Alk5Sergeat18BNo ratings yet
- ArticleDocument14 pagesArticleOusmane KoneNo ratings yet
- Laminin TherapyDocument5 pagesLaminin TherapyCristian JimenezNo ratings yet
- Discuss The Role of Positive and Negative Regulators in HaemopoiesisDocument3 pagesDiscuss The Role of Positive and Negative Regulators in HaemopoiesisAlison HinesNo ratings yet
- The Effect of Hypoxia On Mesenchymal Stem Cell Biology: PharmaceuticalDocument9 pagesThe Effect of Hypoxia On Mesenchymal Stem Cell Biology: PharmaceuticalYolan TiaraNo ratings yet
- WithanolidoA Interfiere MicrofibrasDocument13 pagesWithanolidoA Interfiere MicrofibrascumbredinNo ratings yet
- KDM5B MacrophageDocument14 pagesKDM5B MacrophageMaurício DallowayNo ratings yet
- Kit and C Kit Mutations in MastocytosisDocument7 pagesKit and C Kit Mutations in Mastocytosisvcox4460No ratings yet
- Stemcells 2007-0416Document12 pagesStemcells 2007-0416Ikke OppgaveNo ratings yet
- Methods For Measuring Autophagy in Mice. Manon Moulis and Cécile VindisDocument14 pagesMethods For Measuring Autophagy in Mice. Manon Moulis and Cécile VindisAzael Torales CardeñaNo ratings yet
- Fibroblast-initiationTumor Rev2019Document30 pagesFibroblast-initiationTumor Rev2019Banchob SripaNo ratings yet
- Ijms 24 01571 v2Document15 pagesIjms 24 01571 v2BOURICHENo ratings yet
- ApoptosisDocument16 pagesApoptosisonur ateşNo ratings yet
- 2014-Echeverria C-Endotoxin-induced endothelial fibrosis is dependent on the expression of TGF-β1 and TGF-β2Document9 pages2014-Echeverria C-Endotoxin-induced endothelial fibrosis is dependent on the expression of TGF-β1 and TGF-β2Pablo Tapia BatallaNo ratings yet
- 7.kuliah Dasar Molekuler Kanker Part 2Document29 pages7.kuliah Dasar Molekuler Kanker Part 2eleldev100% (1)
- Peripheral Blood Leukocy 2008 Veterinary Clinics of North America Equine PRDocument21 pagesPeripheral Blood Leukocy 2008 Veterinary Clinics of North America Equine PRCristina ArribasNo ratings yet
- The Genetic Basis of Haematological CancersFrom EverandThe Genetic Basis of Haematological CancersSabrina TosiNo ratings yet
- Tissue Engineering and Regeneration in Dentistry: Current StrategiesFrom EverandTissue Engineering and Regeneration in Dentistry: Current StrategiesRachel J. WaddingtonNo ratings yet
- Accessories Package Price List: Items Basic Aero Aero Plus A Aero Plus BDocument1 pageAccessories Package Price List: Items Basic Aero Aero Plus A Aero Plus BMati AjaNo ratings yet
- Cde 0006 0119Document5 pagesCde 0006 0119Mati AjaNo ratings yet
- Localized Scleroderma: Clinical Spectrum and Therapeutic UpdateDocument12 pagesLocalized Scleroderma: Clinical Spectrum and Therapeutic UpdateMati AjaNo ratings yet
- Table 3 PrintDocument1 pageTable 3 PrintMati AjaNo ratings yet
- BIO 423L EXERCISE 2 Creating and Using Taxonomic Keys PDFDocument6 pagesBIO 423L EXERCISE 2 Creating and Using Taxonomic Keys PDFclairosusNo ratings yet
- Langman's Medical Embryology - CoverDocument11 pagesLangman's Medical Embryology - CoverAriesta Wijaya PutraNo ratings yet
- 2009 - Statistical Methods in Environmental EpidemiologyDocument449 pages2009 - Statistical Methods in Environmental EpidemiologyDaniela Sánchez AcostaNo ratings yet
- ADBT 1 Overview of BiotechnologyDocument42 pagesADBT 1 Overview of BiotechnologyMaham AdnanNo ratings yet
- Annexure - XVI - IIVR Annual Report English 2017-18 PDFDocument221 pagesAnnexure - XVI - IIVR Annual Report English 2017-18 PDFVishwambhara Dasa100% (1)
- PG M.sc. Zoology 35022 ImmunologyDocument241 pagesPG M.sc. Zoology 35022 ImmunologyJo FighizNo ratings yet
- 6.6. Contribution of Yeast and Its Biomass For The Preparation of Industrially - CSDocument16 pages6.6. Contribution of Yeast and Its Biomass For The Preparation of Industrially - CSFarida RahayuNo ratings yet
- BiologyDocument31 pagesBiologyPrinceton University Press100% (2)
- Answer Sheet - Module 6Document6 pagesAnswer Sheet - Module 6sjhdjshakjNo ratings yet
- Notes Biological Molecules 3Document8 pagesNotes Biological Molecules 3abdul rehmanNo ratings yet
- Igenomix UK Sample Requirements UKDocument2 pagesIgenomix UK Sample Requirements UKdrumerNo ratings yet
- STS Activity-18 Research-ActivityDocument2 pagesSTS Activity-18 Research-ActivityEvan Caringal SabioNo ratings yet
- Biomedical Science Coursework HelpDocument7 pagesBiomedical Science Coursework Helpdrrzjaifg100% (2)
- Role of Metal Ions in Dopamine Oxidation (1) (Autorecovered)Document19 pagesRole of Metal Ions in Dopamine Oxidation (1) (Autorecovered)intresting videoNo ratings yet
- Drug Resistance Pharmacology Lecture Lecture Series 2019Document23 pagesDrug Resistance Pharmacology Lecture Lecture Series 2019temitopeNo ratings yet
- Sample Paper Bs Bioinformatics and BiotechnologyDocument4 pagesSample Paper Bs Bioinformatics and BiotechnologySaad Hassan KheraNo ratings yet
- Protein SynthesisDocument24 pagesProtein SynthesisCOMPUTER ZONENo ratings yet
- Sepideh RQsDocument6 pagesSepideh RQsCésar HelenoNo ratings yet
- Bio 07 K1 (Perak)Document21 pagesBio 07 K1 (Perak)Ferguson TehNo ratings yet
- Chapter 6 The ABO Blood Group SystemDocument35 pagesChapter 6 The ABO Blood Group SystempartikNo ratings yet
- Cabrera Et Al. 2008 Araceae PhylogeneticsDocument13 pagesCabrera Et Al. 2008 Araceae PhylogeneticsGerardo A. SalazarNo ratings yet
- Le Syndrome de Bardet Biedl Endocrino 2008Document9 pagesLe Syndrome de Bardet Biedl Endocrino 2008Talala tililiNo ratings yet
- A New Theory Emerges Is Cancer A Fungus (Here Is The Evidence) - Humans Are Free (Humans Are Free) (Z-Library)Document10 pagesA New Theory Emerges Is Cancer A Fungus (Here Is The Evidence) - Humans Are Free (Humans Are Free) (Z-Library)sarapmaria97No ratings yet
- Assignment Chapter Covered Sexual Reproduction in Flowering Plants, Human Reproduction (Prepare These Lesson For Periodic Test-1)Document7 pagesAssignment Chapter Covered Sexual Reproduction in Flowering Plants, Human Reproduction (Prepare These Lesson For Periodic Test-1)PROPER GAMING MOBILENo ratings yet
- Biochem Task 9 BocalanbethinnaDocument4 pagesBiochem Task 9 BocalanbethinnaANA MARIA BETHINNA BOCALANNo ratings yet
- Abcam MOM IgG1,2a, 3 Linker Ordering InfoDocument2 pagesAbcam MOM IgG1,2a, 3 Linker Ordering InfoqinggaoiNo ratings yet