Professional Documents
Culture Documents
14 CTN Celebi
14 CTN Celebi
Uploaded by
chr0m3b4tm4nCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
14 CTN Celebi
14 CTN Celebi
Uploaded by
chr0m3b4tm4nCopyright:
Available Formats
Kardiologia Polska
2010; 68, 8: 935937
Copyright Via Medica
ISSN 00229032
Chorzy trudni nietypowi/Case report
Inappropriate sinus tachycardia
successful treatment with ivabradine
Nieadekwatna tachykardia zatokowa skuteczna terapia iwabradyn
Ozlem Ozcan Celebi, Alper Canbay, Savas Celebi, Sinan Aydogdu, Erdem Diker
Department of Cardiology, Ankara Numune Education and Research Hospital, Ankara, Turkey
Abstract
Inappropriate sinus tachycardia (IST) is characterised by an exaggerated increase of heart rate in response to normal physiologic demands. Therapeutic options including medical and radiofrequency ablation interventions are still under debate.
Ivabradine inhibits spontaneous pacemaker activity of the sinus node by selectively blocking If channels of pacemaker cells.
Here we present a case of a patient with IST, who was successfully treated with ivabradine after various ineffective therapeutic approaches.
Key words: inappropriate sinus tachycardia, ivabradine, sinus node blocking
Kardiol Pol 2010; 68, 8: 935937
CASE REPORT
A 16 year-old female was addmitted to hospital due to tachycardia lasting for a few years. She was complaining of palpitations with minimal exercise during daily activities. Her physical examination was only remarkable for regular tachycardia
with a heart rate (HR) of 160 bpm. A 12-lead surface electrocardiogram (ECG) showed tachycardia. Secondary causes of
sinus tachycardia was excluded. A 24-hour ECG Holter monitoring revealed that basal HR was between 90 bpm and
180 bpm during daily activities. Heart rate inappropriately
increased from 100 bpm to 160 bpm at the first stage of treadmill exercise test. The p wave axis and morphology was
similar to that in sinus rhythm. All of these findings were suggestive of inappropriate sinus tachycardia (IST). Accordingly,
cardiac electrophysiological study was performed. No other
tachycardia was induced by programmed atrial and ventricular
stimulation. In order to confirm the diagnosis of IST 1 mg/min
isoproterenol infusion was administrated and thereafter HR
increased from 90 bpm to 140 bpm. Heart rate response to
isoproterenol was brisk. Metoprolol 50 mg daily with a target
dose of 200 mg daily was started thereafter. Despite metoprolol at maximal dose, she was still complaining of tachy-
cardia. Repetitive ECG Holter monitoring showed that basal HR was 105 bpm and increased to maximum 164 bpm
during daily activities. Because of resistant tachycardia, she
underwent sinus node area modification by radiofrequency
(RF) ablation. After the procedure HR decreased to 80 bpm
and increased to maximum 110 bpm with isoproterenol administration without palpitation. Hovever, she was readmitted to hospital suffering from the same symptoms two months after ablation, which raised concerns about recurrent IST.
Subsequent ECG Holter monitoring and treadmill exercise
test confirmed the recurrence of IST (Table 1). Since the symptoms were refractory to both metoprolol and RF ablation, we
decided to add verapamil at a target dose of 240 mg daily.
However, she was still symptomatic and experienced palpitation. Moreover, hypotension impeded additional verapamil use.
At that point ivabradine was added to medical therapy with
a dose of 5 mg bid and HR slowed down. The ivabradine
dose was increased to 7.5 mg bid. One month later, 24-hour
ECG Holter monitoring was reperformed and showed that
basal HR was 58 bpm and increased to maximal 120 bpm
during daily activities (Table 2). She was free from symptoms,
howewer, a phosphenes occured after ivabradine. Since it
Address for correspondence:
Ozlem Ozcan Celebi, MD, 381.sokak Idareciler Sitesi B-Blok No: 13 igdem, Ankara, Turkey, tel: +903125084776, fax: +903123110115,
e-mail: drozlemoz@mynet.com
Received: 26.11.2009
Accepted: 16.12.2009
www.kardiologiapolska.viamedica.pl
936
Ozlem Ozcan Celebi et al.
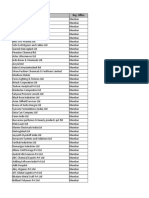
Table 1. 24-hour ECG monitoring before ivabradine shows increased heart rate during daily activities
INTERVAL
HEART RATE
TOTAL
VPB
RUNS
SVPB
SVPB
RUNS
VT
TOTAL
PAIRS
SVT
0:50
0:53
0:57
5832
0:58
131
5310
0:58
128
5215
0:58
92
152
5385
0:58
68
93
145
5370
0:57
67
112
174
6558
0:58
23:001
67
94
147
5202
0:54
0:002
62
91
127
4968
0:54
1:002
61
81
121
4618
0:56
2:002
63
74
93
4203
0:56
3:002
53
68
116
3885
0:56
4:002
54
63
104
3792
1:00
5:002
53
60
98
3555
0:59
6:002
51
61
109
3632
0:58
7:002
55
67
117
3903
0:57
8:002
57
67
114
3999
0:59
9:002
59
71
116
4280
0:59
10:002
59
75
128
4402
0: 58
STARTING
LO
MEAN
HI
BEATS
14:021
75
131
183
6680
15:001
66
99
166
5282
16:001
72
97
147
5674
17:001
69
100
154
18:001
65
91
19:001
63
89
20:001
67
21:001
22:001
VPB
TOTAL PAIRS
TIMES
PAUSES ANALYSED
11:002
61
100
166
5490
0: 54
12:002
72
117
171
6626
0:56
13:002
90
138
186
7080
0:50
14:002
128
184
200
1037
0:05
SUMMARY
51
89
200
121992
22:51
was tolerable and mild, we did not stop the medication. Phosphenes spontaneously disappeared and she improved symptomatically during six months of follow-up.
DISCUSSION
Inappropriate sinus tachycardia is charactarised by an exaggerated increase of HR in response to normal physiologic
demands [1]. Increased sympathetic tone and sympathetic
receptor sensitivity, blunted parasympathetic tone, and enhanced automaticity by virtue of regional autonomic neuropathy have been proposed to be underlying mechanisms [2].
Clinical features of IST may include palpitation, shortness of
breath, chest discomfort, dizziness and fatique [3]. Severe
symptoms sometimes may even prevent patients from daily
activities. Of note, important diagnostic challenge is to investigate other causes of sinus tachycardia before making a diagnosis of IST.
Medical management of IST usually includes beta-blockers and verapamil [4]. Sinus node modification using RF
ablation has been treatment modility of choice in patients
with drug refractory IST. However, sinus node modification
by catheter-based approach has high recurrence rate and
low success rate. A significant proportion of patients who
underwent RF ablation of sinus node area or received sinus
node blocking agents still suffer symptoms related to tachycardia.
Ivabradine blocks If channels of sinus node pacemaker
cells. Clinical trials have clearly documented the effectiveness of ivabradine for the treatment of chronic angina pectoris in the setting of contraindication or intolerance for beta-blockers [5, 6]. Blocking If channels of pacemaker cells allows HR reduction without affecting myocardial contractility,
relaxation and peripheral vascular resistance [7]. This feature
is crucial, as hypotensive response to other negative chronotrophic medications such as beta-blockers and verapamil may
limit thair widespread use as in our case. Therefore ivabradine, it has been recently suggested a new therapeutic step
before invasive sinus node modulation [4].
When ivabradine was administrated to our patient,
both the quality of life and symptoms improved. Howe-
www.kardiologiapolska.pl
937
Inappropriate sinus tachycardia: successful treatment with ivabradine
Table 2. 24-hour ECG monitoring after ivabradine shows slowered heart rate which is within normal limits at rest and during daily
activity
INTERVAL
HEART RATE
TOTAL
VPB
VPB
TOTAL PAIRS
RUNS
SVPB
SVPB
RUNS
VT
TOTAL
PAIRS
SVT
TIMES
STARTING
LO
MEAN
HI
BEATS
PAUSES ANALYSED
14:011
63
82
121
2682
0:32
15:001
49
69
104
4063
0:58
16:001
49
72
110
4275
0:58
17:001
49
67
97
4015
0:59
18:001
44
60
89
3619
0:59
19:001
43
55
85
3327
0:59
20:001
45
62
84
3718
0:59
21:001
48
61
82
3659
0:59
22:001
44
57
77
3415
0:59
23:001
45
59
85
3492
0:58
0:002
43
55
80
3259
0:59
1:002
39
48
71
2894
0:59
2:002
37
46
65
2760
0:59
3:002
42
52
78
3137
0:59
4:002
39
47
76
2854
0:59
5:002
36
47
79
2849
1:00
6:002
40
49
83
2351
0:47
7:002
38
45
80
2746
0:59
8:002
41
51
87
2891
0:56
9:002
45
65
101
3944
0:59
10:002
48
71
117
1298
0:18
SUMMARY
36
58
121
67248
19:25
ver, there is no established effective dose of ivabradine for
the treatment of IST. In our case, initial dose was 5 mg bid
but the effective decrease in HR and improvement of symptoms were achieved when the dose was increased to 7.5
mg bid.
Ivabradine is generally well tolerated and only few side
effects are known. The most common adverse event is reported to be visual symptoms due to inhibition of h-channels in
the eye [7]. Of note, visual symptoms are more likely to occur in a dose dependent fashion (increased by aproximately
14%, 18% and 29% with 5 mg, 7.5 mg and 10 mg of ivabradine respectively). Visual symptoms are usually mild and transient in nature. Besides, phosphenes are previously reported
to not be associated with withdrawal of the drug as in the
current case [8].
In conclusion, ivabradine seems to be clinically useful
for the treatment of IST and should be esperially considered
in patients with resistant symptoms.
References
1.
2.
3.
4.
5.
6.
7.
8.
Morill CA, Klein GJ, Thakur RK et al. Mechanism of inappropriate
sinus tachycardia. Role of sympthovagal balance. Circulation,
1994; 90: 873877.
Shen WK. How to manage patients with inappropriate sinus
tachycardia. Heart Rhythm, 2005; 2:10151019.
Leonelli F, Richey M, Beheiry S et al. Tridimensional mapping:
guided modification of sinus node. J Interven Card Electrophysiol, 1998; 9: 12141217.
Schulze V, Steiner S, Hennersdorf M et al. Ivabradine as an alternative therapeutic trial in the therapy of inappropriate sinus
tachycardia: a case report. Cardiology, 2008; 110: 206208.
Borer JS, Fox K, Jaillon P et al. Antianginal and antiischemic
effects of ivabradine, an If inhibitor, in stable angina. Circulation, 2003; 107: 817823.
Tardif JC, Ford I, Tendera M et al. Efficacy of ivabradine, a new
selective If inhibitor, compared with atenolol in patients with
chronic stable angina. Eur Heart J, 2005; 26: 25292536.
Savelieva I, Camm AJ. If inhibition with ivabradine: electrophysiological effects and safety. Drug Saf, 2008; 31: 95107.
Lpez-Bescs L, Filipova S, Martos R. Long-term safety and efficacy of ivabradine in patients with chronic stable angina. Cardiology, 2007; 108: 387396.
www.kardiologiapolska.pl
You might also like
- Mashaba FilesDocument1,268 pagesMashaba FilesGugu TeoNo ratings yet
- RAC Past PapersDocument6 pagesRAC Past PapersOlivia Merchant0% (2)
- Adverse Event Report CIOMS I FormDocument1 pageAdverse Event Report CIOMS I Formbouzina ibrahimNo ratings yet
- Sinupret patientInfoSheetDocument1 pageSinupret patientInfoSheetiisisiis100% (1)
- A Case of Atrial Tachycardia Treated With Ivabradine As Bridge To AblationDocument11 pagesA Case of Atrial Tachycardia Treated With Ivabradine As Bridge To Ablationdarlen bahriNo ratings yet
- Case 1 - Widuri - His Bundle Pacing in TAVBDocument17 pagesCase 1 - Widuri - His Bundle Pacing in TAVBW Wita SNo ratings yet
- Sample Case ScenarioDocument8 pagesSample Case ScenarioJan Crizza Dale R. FrancoNo ratings yet
- P ('t':'3', 'I':'669189663') D '' Var B Location Settimeout (Function ( If (Typeof Window - Iframe 'Undefined') ( B.href B.href ) ), 15000)Document45 pagesP ('t':'3', 'I':'669189663') D '' Var B Location Settimeout (Function ( If (Typeof Window - Iframe 'Undefined') ( B.href B.href ) ), 15000)Miranda Yudhi CyubidubiduuNo ratings yet
- Ivabradine Use in Heart Failure After Myocardial Infarction Can Help With The Titration of The Dose of ARB/ACEI or - Blockers: A Case ReportDocument4 pagesIvabradine Use in Heart Failure After Myocardial Infarction Can Help With The Titration of The Dose of ARB/ACEI or - Blockers: A Case ReportAzmia TabahNo ratings yet
- ACLS Class Packet PDFDocument9 pagesACLS Class Packet PDFImam GultomNo ratings yet
- Basinger Abraham - ConsultationDocument80 pagesBasinger Abraham - ConsultationVikas NairNo ratings yet
- Case Discussion 3Document7 pagesCase Discussion 3Siraj INo ratings yet
- Ischemic Heart Disease: Dr. Amin ShneifiDocument65 pagesIschemic Heart Disease: Dr. Amin Shneificarmitjulya228No ratings yet
- NstemiDocument6 pagesNstemishamaamo19No ratings yet
- Practice Exam 1Document103 pagesPractice Exam 1aayceeNo ratings yet
- 10 1016@j Amjcard 2015 01 455Document1 page10 1016@j Amjcard 2015 01 455Elis FatmayantiNo ratings yet
- Conrad Fischer MCQsDocument328 pagesConrad Fischer MCQsPopescu Tina100% (1)
- 15 Walters LLSA ArticlesDocument33 pages15 Walters LLSA ArticlesericNo ratings yet
- How To Stop Paroxysm of SVT and AF at Home and in HospitalDocument35 pagesHow To Stop Paroxysm of SVT and AF at Home and in HospitalOlga Goryacheva100% (1)
- Andi 26-30Document6 pagesAndi 26-30Andi HidayatNo ratings yet
- Queen's University Internal Medicine Simulation CourseDocument5 pagesQueen's University Internal Medicine Simulation CourseletonierNo ratings yet
- Reversal of Tachycardiomyopathy Due To Left Atrial Tachycardia by IvabradineDocument3 pagesReversal of Tachycardiomyopathy Due To Left Atrial Tachycardia by Ivabradinedarlen bahriNo ratings yet
- Spring 2014 NewsletterDocument5 pagesSpring 2014 Newsletterapi-236445988No ratings yet
- Case of The WeekDocument20 pagesCase of The WeekLady KweeNo ratings yet
- Anafilactic ShockDocument2 pagesAnafilactic ShockprayogarathaNo ratings yet
- LAPSUS LAKI-LAKI 52 TAHUN DENGAN TRANSIENT ST SEGMENT ELEVATION - Dr. Yusuf Haz CondengDocument47 pagesLAPSUS LAKI-LAKI 52 TAHUN DENGAN TRANSIENT ST SEGMENT ELEVATION - Dr. Yusuf Haz CondengIrham Khairi100% (1)
- AVJ Ablation Vs CardioversionDocument6 pagesAVJ Ablation Vs CardioversionAndy CordekNo ratings yet
- TurpDocument99 pagesTurpakanksha singhNo ratings yet
- Idiopathic Fascicular LV Tachycardia Case Report - Kadek Agus Putra - Edit 1Document8 pagesIdiopathic Fascicular LV Tachycardia Case Report - Kadek Agus Putra - Edit 1putra udayanaNo ratings yet
- Ccrep 2010 051Document4 pagesCcrep 2010 051prohormusicNo ratings yet
- Qara Syifa Fachrani - 2010221030 - Case Report Exercise-Induced Supraventricular Tachycardia in A 16-Year-Old Boy With Tricuspid RegurgitationDocument7 pagesQara Syifa Fachrani - 2010221030 - Case Report Exercise-Induced Supraventricular Tachycardia in A 16-Year-Old Boy With Tricuspid RegurgitationQara Syifa FNo ratings yet
- PracticeExam1 & 2Document160 pagesPracticeExam1 & 2Arash SamieiNo ratings yet
- Case Reports AbstractsDocument7 pagesCase Reports AbstractsNovie AstiniNo ratings yet
- Brugada SyndromeDocument10 pagesBrugada SyndromeRavikiran SuryanarayanamurthyNo ratings yet
- Neostigmina AH Niño 18 MesesDocument3 pagesNeostigmina AH Niño 18 MeseshmtorsNo ratings yet
- Case PresentationDocument47 pagesCase PresentationmwaniksNo ratings yet
- Laporan Jaga 11 Sep (English) KoreksiDocument30 pagesLaporan Jaga 11 Sep (English) KoreksiArick Frendi AndriyanNo ratings yet
- The CaseDocument33 pagesThe CasemarunxNo ratings yet
- CARDIOLOGY Notes by MeDocument33 pagesCARDIOLOGY Notes by MeJanie-Vi GorospeNo ratings yet
- Medically Compromised PaftientsDocument21 pagesMedically Compromised PaftientsLedjon KaciNo ratings yet
- Doctors OrderDocument9 pagesDoctors OrderReal TetisoraNo ratings yet
- The Effect of Ivabradine On Functional Capacity in Patients With Chronic Obstructive Pulmonary DiseaseDocument4 pagesThe Effect of Ivabradine On Functional Capacity in Patients With Chronic Obstructive Pulmonary DiseaseArick Frendi AndriyanNo ratings yet
- MNI SAH ProtocolDocument10 pagesMNI SAH ProtocolAbo ZakariaNo ratings yet
- Topic 10 Internal Medicine Ali SaifDocument5 pagesTopic 10 Internal Medicine Ali SaifAnkit Kumar PatelNo ratings yet
- ARNI in Cardiovascular, Current UpdateDocument12 pagesARNI in Cardiovascular, Current Updatefazlur risyad laochiNo ratings yet
- Update in Stroke Management: David Lee Gordon, M.D., FAHADocument43 pagesUpdate in Stroke Management: David Lee Gordon, M.D., FAHAMuhidin AeNo ratings yet
- Hippokratia 18 185Document2 pagesHippokratia 18 185Antonio CerdaNo ratings yet
- Anaesthesia and Atrial FibrillationDocument15 pagesAnaesthesia and Atrial FibrillationNaresh Dhawan100% (1)
- ATRIAL FIBRILLATION Anil KRDocument41 pagesATRIAL FIBRILLATION Anil KRanil sahNo ratings yet
- SA VM Case Discussion - Cataract Surgery in A Patient With PacemakerDocument23 pagesSA VM Case Discussion - Cataract Surgery in A Patient With PacemakerVishnu ManglaNo ratings yet
- Ws Ahf - Intro Apicd 2017 - EditedDocument18 pagesWs Ahf - Intro Apicd 2017 - Editedvkhen88No ratings yet
- 1 SMDocument15 pages1 SMemmanuellagrace06No ratings yet
- Carvedilol and Nebivolol Improve Left Ventricular Systolic Functions in Patients With Non-Ischemic Heart FailureDocument6 pagesCarvedilol and Nebivolol Improve Left Ventricular Systolic Functions in Patients With Non-Ischemic Heart FailureBramantyo DwiputraNo ratings yet
- Atrial Fibrilation (AF) : Moh Gilang Fajriansyah Nohu (C11110285)Document38 pagesAtrial Fibrilation (AF) : Moh Gilang Fajriansyah Nohu (C11110285)GilankNo ratings yet
- Jaga Tengah - MedCon - 010321 - CAMDocument22 pagesJaga Tengah - MedCon - 010321 - CAMAdinda DianNo ratings yet
- Arrhythmia Induction in the EP LabFrom EverandArrhythmia Induction in the EP LabGabriel CismaruNo ratings yet
- Fast Facts: Optimización del tratamiento de las fluctuaciones motoras en la enfermedad de Parkinson: Adaptando el tratamiento al pacienteFrom EverandFast Facts: Optimización del tratamiento de las fluctuaciones motoras en la enfermedad de Parkinson: Adaptando el tratamiento al pacienteNo ratings yet
- Critical Care Medications: Vasopressors, Inotropes and Anti-Hypertensives Study Guide: Critical Care EssentialsFrom EverandCritical Care Medications: Vasopressors, Inotropes and Anti-Hypertensives Study Guide: Critical Care EssentialsNo ratings yet
- Pacemaker Syndrome, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandPacemaker Syndrome, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- New Text DocumentDocument1 pageNew Text Documentchr0m3b4tm4nNo ratings yet
- New Text DocumentDocument1 pageNew Text Documentchr0m3b4tm4nNo ratings yet
- TachalgoDocument1 pageTachalgochr0m3b4tm4nNo ratings yet
- Pi Catheter Ablation Ventricular TachycardiaDocument16 pagesPi Catheter Ablation Ventricular Tachycardiachr0m3b4tm4nNo ratings yet
- Ventricular Tachycardia: History Signs and Symptoms DifferentialDocument1 pageVentricular Tachycardia: History Signs and Symptoms Differentialchr0m3b4tm4nNo ratings yet
- Atrial Fibrillation: The Most Common ArrhythmiaDocument2 pagesAtrial Fibrillation: The Most Common Arrhythmiachr0m3b4tm4nNo ratings yet
- Temporary Policy For Preparation of Certain Alcohol-Based Hand Sanitizer Products During The Public Health Emergency (COVID-19)Document15 pagesTemporary Policy For Preparation of Certain Alcohol-Based Hand Sanitizer Products During The Public Health Emergency (COVID-19)herfuentesNo ratings yet
- Webmm - Ahrq.gov.2 SlideshowDocument28 pagesWebmm - Ahrq.gov.2 SlideshowAlien_42No ratings yet
- Hypoglycemia: Manage Well, Live WellDocument4 pagesHypoglycemia: Manage Well, Live WellHashim Mushtasin RezaNo ratings yet
- Pharmacological Review On Terminalia ChebulaDocument5 pagesPharmacological Review On Terminalia ChebulaSri Sakthi SumananNo ratings yet
- Quiz Pha313-2Document11 pagesQuiz Pha313-2hugersofiNo ratings yet
- Valproic Acid DrugstudyDocument2 pagesValproic Acid DrugstudyVince John SevillaNo ratings yet
- Assignment ACC205Document4 pagesAssignment ACC205GarimaNo ratings yet
- Cpm12th RabiesDocument15 pagesCpm12th RabiesKaren ArchesNo ratings yet
- Clinical Medications Worksheets: (Why Med Ordered) Contraindications/warnings/interactionsDocument3 pagesClinical Medications Worksheets: (Why Med Ordered) Contraindications/warnings/interactionsENo ratings yet
- GastrointestinaldrugsDocument30 pagesGastrointestinaldrugsmayaNo ratings yet
- Calcium CarbonateDocument102 pagesCalcium CarbonateSantiagoNo ratings yet
- ECDD 37th Report FINAL PrelayoutDocument45 pagesECDD 37th Report FINAL PrelayoutsppNo ratings yet
- Cialis Case Study1Document9 pagesCialis Case Study1Jeff Crawford100% (1)
- Topical and Transdermal Drug ProductsDocument14 pagesTopical and Transdermal Drug Productsczisu730% (1)
- Executive Director Research Development in Boston MA Resume Paul HallenbeckDocument5 pagesExecutive Director Research Development in Boston MA Resume Paul HallenbeckPaulHallenbeckNo ratings yet
- DR Reddy Lab - Leveraging CapabilitiesDocument13 pagesDR Reddy Lab - Leveraging CapabilitiesNirankar RoyalNo ratings yet
- Index Incl ExclDocument183 pagesIndex Incl Exclyakubpasha.mohdNo ratings yet
- Ibuprofen 5% Topical CreamDocument1 pageIbuprofen 5% Topical CreamSameed BashaNo ratings yet
- Imcops Price List From 01 - 11 - 2015 PDFDocument26 pagesImcops Price List From 01 - 11 - 2015 PDFGoutham PillaiNo ratings yet
- LCM and HCF (001-050)Document5 pagesLCM and HCF (001-050)Banwari Lal PrajapatNo ratings yet
- Maharashta and NCR ListDocument7 pagesMaharashta and NCR ListAnkita ShrivastavaNo ratings yet
- Evidence-Based Guideline: Clinical Evaluation and Treatment of Transverse MyelitisDocument8 pagesEvidence-Based Guideline: Clinical Evaluation and Treatment of Transverse MyelitisAnonymous V5l8nmcSxbNo ratings yet
- Biopharming and The Food System - Examining The Potential Benefits and Risksl - Aziz Elbehri - 2005Document8 pagesBiopharming and The Food System - Examining The Potential Benefits and Risksl - Aziz Elbehri - 2005NaveenNo ratings yet
- OPPI - EY Report - Unlocking The Potential of The Pharma Distribution ChannelDocument36 pagesOPPI - EY Report - Unlocking The Potential of The Pharma Distribution ChannelVivek JaiswalNo ratings yet
- Diva Tertia Almira (470320) - Analisis Ratio Kalbe Farma W4Document4 pagesDiva Tertia Almira (470320) - Analisis Ratio Kalbe Farma W4Diva Tertia AlmiraNo ratings yet
- Brochure Chynops PharmaDocument10 pagesBrochure Chynops PharmaMohamed DarwishNo ratings yet
- BEXIMCO Bus 101Document21 pagesBEXIMCO Bus 101Mahedi Azam PollobNo ratings yet