Professional Documents
Culture Documents
Phacomorphic Glaucoma: Case and Review: Joseph Sowka, O.D
Phacomorphic Glaucoma: Case and Review: Joseph Sowka, O.D
Uploaded by
Dian Rahma RidwansyahOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Phacomorphic Glaucoma: Case and Review: Joseph Sowka, O.D
Phacomorphic Glaucoma: Case and Review: Joseph Sowka, O.D
Uploaded by
Dian Rahma RidwansyahCopyright:
Available Formats
Optometry (2006) 77, 586-589
Phacomorphic glaucoma: Case and review
Joseph Sowka, O.D.
Nova Southeastern University, College of Optometry, Ft. Lauderdale, Florida.
KEYWORDS
Phacomorphic
glaucoma;
Phacolysis;
Lens-induced
glaucoma;
Argon laser peripheral
iridoplasty
Abstract Phacomorphic glaucoma is a lens-induced secondary angle closure glaucoma that may occur
as a result of mature cataract formation. A patient with markedly asymmetric cataract and anterior
chamber depth was referred after the development of significant eye pain and elevated intraocular
pressure that did not respond to topical antiglaucoma medications. The presence of an asymmetric
mature lens, angle closure, and intraocular pressure elevation in the affected eye led to the diagnosis of
phacomorphic glaucoma. Because the patient was systemically ill, physically frail, and had poor vision
in the affected eye since birth, secondary to strabismic amblyopia, initial therapy was medically directed
toward pain management. Cycloplegia, corticosteroids, and aqueous suppressants successfully ameliorated the patients intraocular pressure and adequately controlled pain. However, progression to
phacolysis and subsequent failure of pain management necessitated referral for lens extraction. The
diagnosis and mechanism of phacomorphic glaucoma is discussed along with a review of current
treatment modalities.
Optometry 2006;77:586-589
Intraocular pressure elevation can be induced by the
crystalline lens through several mechanisms and represents
a significant cause of secondary glaucoma.1-3 Although
lens-induced glaucomas tend to be more common in developing countries where citizens have less access to surgical
care,1-3 they can and do occur in developed nations when
individuals, for a variety of reasons, allow cataracts to fully
mature and progress to hypermaturity. Phacomorphic glaucoma is a known cause of secondary angle closure glaucoma, the clinical appearance of which must be recognized
to institute appropriate management.
Case report
A 48-year-old black woman with cerebral palsy, sickle cell
disease, and arthritis was referred urgently for a glaucoma
Corresponding author: Joseph Sowka, O.D., Nova Southeastern University, College of Optometry, 3200 South University Drive, Ft. Lauderdale, Florida 33328.
E-mail: jsowka@nova.edu
consultation owing to elevated intraocular pressure (IOP)
and ocular pain in the left eye (O.S.) that had not responded
to topical glaucoma therapy. She presented to the referring
optometrists office with a painful left eye. Her left eye had
been moderately painful for approximately 3 months prior,
but the intensity of the pain had increased over the last
several days. Because the patient was unable to maintain
fixation in the biomicroscope, intraocular pressure evaluation at that time was performed with a Tono-Pen (Mentor,
Santa Barbara, California), with resultant readings of 19
mmHg in the right eye (O.D.) and 39 mmHg O.S. Gonioscopy reportedly had been attempted but was unsuccessful
because of the patients lack of cooperation. A dilated
fundus examination found angioid streaks in the right eye
without any evidence of sickle cell retinopathy. Funduscopic views of the left eye were unattainable because of a
dense cataract.
The referring optometrist initially used apraclonidine
0.5% in the office to reduce the intraocular pressure, without
success. The patient was prescribed travoprost 0.004% every evening O.S. When seen for follow-up 7 days later, her
intraocular pressure measured 45 mmHg O.S. (by Tono-
1529-1839/06/$ -see front matter 2006 American Optometric Association. All rights reserved.
doi:10.1016/j.optm.2006.08.013
Joseph Sowka
Issue Highlight
Pen), and travoprost was deemed ineffective. The patient
was then prescribed pilocarpine 2% 3 times a day and
brimonidine 0.2% twice a day O.S. and referred for evaluation and management.
On presentation for consultation 7 days later, the patient
reported that her left eye was still painful with no reduction
in pain with the use of the medications. Her medical history
was significant for sickle cell disease, mild cerebral palsy,
and osteoarthritis. She was using Bextra (valdecoxib; G.D.
Searle & Co., Skokie, Illinois) for pain associated with
sickle cell disease and osteoarthritis. The patient was frail
with limited mobility, for which she used a wheelchair. She
reported that she had a constant left eye turn since birth with
poor visual acuity in that eye, had no changes in vision in
either eye, and was most concerned about the pain in her left
eye.
Unaided visual acuity was 20/100 O.D., with refractive
improvement to 20/40 with a 3.00 spherical correction
and bare light perception O.S. The right pupil reacted to
light, whereas the left pupil was medically miotic. There
was a relative afferent pupil defect O.S. by reverse testing.
Confrontation visual field screening was full O.D. The
patient could not be screened in the left eye because of poor
vision. Ocular muscle testing found no restrictions in either
eye; however, there was a 45-prism diopter constant left
exotropia present at distance and near.
Biomicroscopic evaluation found a normal anterior segment O.D. with the exception of a mild nuclear sclerotic
cataract. The left eye showed normal adnexa and a fully
mature nuclear sclerotic cataract that was much denser than
that in the fellow eye. Funduscopic views through the left
cataract were not possible. The anterior chamber appeared
to be deep in the right eye and much shallower in the left
eye. Goldmann applanation tonometry was performed successfully. Intraocular pressures were 18 mmHg O.D. and 35
mmHg O.S. Gonioscopy found no angle structures in any
view in the left eye; however, there were areas of peripheral
anterior synechiae. There was no neovascularization of the
iris or angle. Gonioscopy was unsuccessful in the right eye
because of increasing lack of patient cooperation.
The patient had phacomorphic glaucoma diagnosed O.S.
based on the asymmetric maturity of the left cataract with
anterior chamber shallowing and angle closure. A deep
anterior chamber in the right eye as well as the presence of
myopia further supported a lens-induced mechanism of
angle closure. Previous use of apraclonidine, pilocarpine,
and travoprost had apparently not yielded any significant
success in either reducing the IOP, changing angle configuration, or ameliorating the patients discomfort. Because of
little visual potential in the left eye and pain being the
patients most significant concern, medical therapy was
instituted to address the discomfort. Pilocarpine and brimonidine were discontinued, and prednisolone acetate 1% 4
times a day, scopolamine 0.25% twice a day, and timolol
maleate 0.5% gel-forming solution every day in the morning O.S. were prescribed. The patient was reappointed for 1
587
week but told to call immediately if her pain did not
improve or if it worsened within the next several days.
The patient returned as scheduled and reported good
medical compliance. Her visual acuity was unchanged in
each eye. She now reported that her ocular pain had greatly
diminished and was now only occasional. She had no ocular
pain at the time of the visit. Intraocular pressures were 19
mmHg O.D. and 40 mmHg O.S. Her left pupil was pharmacologically dilated. The patient was instructed to continue the medications prescribed at the last visit as well as to
resume brimonidine bid O.S. The patient was reappointed
for 3 months with the instructions to return immediately
should there be any increase in pain or other changes.
At the 3 month follow-up, the patient reported good
medical compliance and no further instances of ocular pain.
Intraocular pressures by Goldman applanation were 16
mmHg O.D. and 25 mmHg O.S. There were no changes in
her biomicroscopic evaluation. Because there was no potential for improved functional vision O.S., and her pain was
well managed medically, she was deemed not to be a good
candidate for lens extraction. She continued all medications.
The patient was successfully followed up medically for
the next 7 months. However, at her most recent progress
evaluation, she reported that she had developed significant
pain again in her left eye as well as general photophobia.
The visual acuity was unchanged in the right eye but had
decreased to no light perception in the left eye. Additionally, the left cataract was visibly whiter on gross inspection.
Her family members had also noticed that her pupil seemed
whiter than in the past month.
Biomicroscopic evaluation found a hypermature, lytic
cataract O.S. with a moderate anterior chamber reaction.
Intraocular pressures were 18 mmHg O.D. and 38 mmHg
O.S. It was determined that the phacomorphic lens had now
become phacolytic. As a result, it was felt that medical
control would no longer be appropriate to manage the
patients pain and that the patient would now benefit from
medically necessary cataract extraction. Ultrasonography,
planned to ascertain if an intraocular process may have
contributed to the asymmetric cataract formation, was abandoned in favor of a surgical consultation for cataract extraction. The consulting surgeon agreed that lens removal was
medically necessary despite poor visual potential. At the
time of this writing, the patient is scheduled for cataract
extraction O.S (see Figure 1).
Discussion
As the name implies, phacomorphic (phaco lens; morph
shape) glaucoma develops secondary to the shape of the
lens. Angle closureacute, subacute, or chronic can be
triggered by a mature or intumescent cataract and occurs in
eyes with previously open angles as well as in those with
narrow, occludable angles. This is encountered more often
in developing countries where health care is not easily
588
Figure 1
Optometry, Vol 77, No 12, December 2006
Phacolytic lens in another patient.
accessible, and patients present late, often waiting until the
cataract becomes mature. It is a common belief among these
patients that cataracts should not be removed until vision
drops to the level of hand movements or light perception.4
Typically, an advanced, intumescent cataract will be present
in the affected eye. Visual acuity is reduced, often to a level
of hand motion or worse.1,3 In addition, there will be a
shallow anterior chamber. In eyes with markedly asymmetric cataract formation, the depth of the anterior chambers
may be accordingly disparate, which can be very diagnostic.
On occasion, phacomorphic glaucoma will occur not because of mature cataract formation but because of
spherophakia in Weill-Marchesani syndrome.5-8 Pain is a
very common presenting accompanying symptom, being
present in 71% of cases in one report.1 Intraocular pressure is significantly elevated, often exceeding 30 to 40
mmHg.1,9
Thickening of the lens during cataractogenesis can result
in a relative pupil block, with resultant iris bomb and
subsequent angle closure glaucoma. This may occur commonly in patients with already shallow anterior chamber
angles, and cataractogenesis enhances the physiology of
angle closure. However, when angle closure occurs in
myopic eyes or in those patients manifesting a deep fellow
eye anterior chamber, then phacomorphic glaucoma is the
primary mechanism.1,4 Further, the swelling of the lens may
cause it to press on the iris and ciliary body forcing them
anteriorly and shallowing the anterior chamber. Thus, there
can be an acute angle closure attack without relative pupil
block as a mechanism, which may not respond to laser
peripheral iridotomy (LPI).
Medical therapy is often used initially in an attempt to
reverse the process and acutely lower the intraocular pressure. Beta-blockers, -2 adrenergic agonists, topical corticosteroids, topical or oral carbonic anhydrase inhibitors, and
oral hyperosmotic agents all may be systematically used.
However, the use of pilocarpine is somewhat controversial
because it has the effect of increasing axial lens thickness
and causing anterior lens movement, resulting in the anterior chamber becoming more shallow, worsening the condition.10,11 Superior IOP control and shortening the dura-
tion of the attack preoperatively is essential in improving
the final visual outcome.12
It has long been believed that surgical management of
patients with phacomorphic glaucoma tends to be associated
with complications and poor visual outcomes.1,13,14 Although complications can and do occur surgically, successful outcomes are not infrequent.3,12,15 However, surgical
therapy may not be indicated when visual potential is
known to be poor because of glaucomatous damage or other
pre-existing conditions.
In any case of phacomorphic glaucoma, especially those
with the presence of iris bomb indicating pupil block, LPI
remains a strong component of early management. In one
review of 10 patients undergoing LPI for phacomorphic
glaucoma, it was seen that the acute angle closure attack
was prevented successfully or reversed by the procedure in
all cases.4
Argon laser peripheral iridoplasty (ALPI) is rapidly becoming an accepted management of phacomorphic glaucoma.9,16-18 ALPI is a thermally induced iridoretraction
procedure designed to pull the iris from its apposition
against the cornea and trabecular meshwork.18
In one report involving 21 eyes of 21 patients having
ALPI as an initial step in the management of phacomorphic
glaucoma, it was seen that IOP was controlled successfully
in 81% of eyes, with a statistically significant decrease at 2
and 24 hours postoperatively. Elective cataract surgery was
performed in 16 of the 17 successful cases. In 12 patients
completing at least 12 months of follow-up, IOP was normal
without medications in 11 eyes, and only 1 patient required
antiglaucoma eye drops to control IOP. All patients maintained an open angle without further surgical intervention.
No complications directly attributable to ALPI were noted.
It was seen that ALPI was a safe and efficacious measure for
the initial management of phacomorphic glaucoma, obviating the need to operate in highly inflamed eyes in an
emergency setting.17
Tham et al.9 reported on 10 consecutive patients with
acute phacomorphic glaucoma receiving an immediate standard treatment consisting of atropine, timolol, and ALPI and
found that only 1 patient additionally required systemic
acetazolamide to control IOP. Ultimately, all eyes underwent cataract extraction without complications within 4
days after ALPI. There were no complications associated
with ALPI. The investigators concluded that ALPI is a safe
and effective first-line treatment for acute phacomorphic
angle closure, obviating the need for systemic IOP medications.
It is important to distinguish phacomorphic from phacolytic glaucoma; the patient presented herein developed both
conditions. As noted, phacomorphic glaucoma is a closed
angle situation, whereas phacolytic glaucoma is predominately an open-angle condition. Phacolysis refers to the
dissolution of the hypermature crystalline lens. As a cataract
progresses to hypermaturity, the lens shrinks with loss of
high molecular weight (HMW) soluble proteins through an
intact lens capsule.19 This incites an immune-mediated
Joseph Sowka
Issue Highlight
cellular response, with the proteins being engulfed by macrophages, which congregate on the surface of the lens and
become trapped within the trabecular meshwork.19 When
the accumulation of macrophages and HMW-soluble proteins physically block and impede aqueous outflow through
the trabecular meshwork, a secondary pressure rise known
as phacolytic glaucoma is said to ensue.20
Conclusions
Although lens-induced glaucomas are not encountered commonly in populations that have ready access to cataract
surgery, they can easily occur in patients who allow cataracts to mature. Lens-induced glaucomas represent a significant percentage of secondary glaucomas.3 A mature cataract can induce angle closure and phacomorphic glaucoma,
whereas a hypermature cataract can induce phacolytic glaucoma. In some cases, such as the one presented here, more
than 1 lens-induced mechanism may occur in a patient.
Although cataract extraction typically is the definitive treatment for lens-induced glaucomas, there are steps that must
be taken in advance to address the acute nature of the
condition. Also, for a variety of reasons, some patients may
not be good surgical candidates, which may be the underlying reason that a cataract may not have been addressed
earlier and allowed to mature. Alternate chronic medical
therapies may then be more appropriate for that particular
patient situation.
The patient presented here was a poor surgical candidate
because of no potential visual improvement and frail health.
Because the pain was the most significant concern, medical
rather than surgical therapy was initially successfully instituted. However, the progression from phacomorphic to
phacolytic glaucoma with an inability to medically control
pain necessitated a change in therapeutic approach.
References
1. Pradhan D, Hennig A, Kumar J, et al. A prospective study of 413 cases
of lens-induced glaucoma in Nepal. Indian J Ophthalmol 2001;49(2):
103-7.
589
2. Rao SK, Padmanabhan P. Capsulorhexis in eyes with phacomorphic
glaucoma. J Cataract Refract Surg 1998;24(7):882-4.
3. Prajna NV, Ramakrishnan R, Krishnadas R, et al. Lens induced
glaucomasvisual results and risk factors for final visual acuity.
Indian J Ophthalmol 1996;44(3):149-55.
4. Tomey KF, al-Rajhi AA. Neodymium:YAG laser iridotomy in the
initial management of phacomorphic glaucoma. Ophthalmology 1992;
99(5):660-5.
5. Fujiwara H, Takigawa Y, Ueno S, et al. Histology of the lens in the
Weill-Marchesani syndrome. Br J Ophthalmol 1990;74(10):631-4.
6. Ritch R, Chang BM, Liebmann JM. Angle closure in younger patients.
Ophthalmology 2003;110(10):1880-9.
7. Harasymowycz P, Wilson R. Surgical treatment of advanced chronic
angle closure glaucoma in Weill-Marchesani syndrome. J Pediatr
Ophthalmol Strabismus 2004;41(5):295-9.
8. Barkana Y, Shihadeh W, Oliveira C, et al. Angle closure in highly
myopic eyes. Ophthalmology 2006;113(2):247-54.
9. Tham CC, Lai JS, Poon AS, et al. Immediate argon laser peripheral
iridoplasty (ALPI) as initial treatment for acute phacomorphic angleclosure (phacomorphic glaucoma) before cataract extraction: a preliminary study. Eye 2005;19(7):778-83.
10. Abramson DH, Franzen LA, Coleman DJ. Pilocarpine in the presbyope: demonstration of an effect on the anterior chamber and lens
thickness. Arch Ophthalmol 1973;89:100-2.
11. Gorin G. Angle closure glaucoma induced by miotics. Am J Ophthalmol 1966;62:1063-6.
12. Das JC, Chaudhuri Z, Bhomaj S, et al. Combined extracapsular
cataract extraction with Ahmed glaucoma valve implantation in phacomorphic glaucoma. Indian J Ophthalmol 2002;50(1):25-8.
13. Angra SK, Pradhan R, Garg SP. Cataract induced glaucomaan
insight into management. Indian J Ophthalmol 1991;39(3):97-101.
14. Lim TH, Tan DT, Fu ER. Advanced cataract in Singaporeits
prognosis and complications. Ann Acad Med Singapore 1993;22(6):
891-4.
15. McKibbin M, Gupta A, Atkins AD. Cataract extraction and intraocular
lens implantation in eyes with phacomorphic or phacolytic glaucoma.
J Cataract Refract Surg 1996 Jun;22(5):633-6.
16. Thyagarajan S. Immediate argon peripheral iridoplasty (ALPI) as
initial treatment phacomorphic glaucoma: a safe and cost-effective
treatment? Eye 2005 Dec 2; [Epub ahead of print].
17. Yip PP, Leung WY, Hon CY, et al. Argon laser peripheral iridoplasty
in the management of phacomorphic glaucoma. Ophthalmic Surg
Lasers Imaging 2005;36(4):286-91.
18. Leung CK, Chan WM, Ko CY, et al. Visualization of anterior chamber
angle dynamics using optical coherence tomography. Ophthalmology
2005;112(6):980-4.
19. Brown NP, Bron AJ. Lens disorders. A clinical manual of cataract
diagnosis. Oxford: Butterworth-Heinemann; 1996.
20. Shields MB. Glaucomas associated with disorders of the lens. In:
Shields MB, editor. Textbook of glaucoma. Baltimore: Williams &
Wilkins; 1992.
You might also like
- Appendicitis (Case Study)Document40 pagesAppendicitis (Case Study)Cherr Noll Sanchez100% (1)
- Nursing Research ReportDocument15 pagesNursing Research Reportapi-546467833No ratings yet
- Clinical Diagnosis and Management of Ocular Myasthenia GravisDocument11 pagesClinical Diagnosis and Management of Ocular Myasthenia GravisAinul NurrahmahNo ratings yet
- Dong KimberlyDocument7 pagesDong KimberlyalmaNo ratings yet
- 100255-Article Text-1482-2-10-20220311Document6 pages100255-Article Text-1482-2-10-20220311Fachry RahmanNo ratings yet
- Clinical CasesDocument49 pagesClinical Casesnorfitri hadeyNo ratings yet
- Medicine: Sumatriptan-Induced Angle-Closure GlaucomaDocument4 pagesMedicine: Sumatriptan-Induced Angle-Closure GlaucomanidaNo ratings yet
- A Rare Case of Terson Syndrome With Subarachnoid HemorrhageDocument12 pagesA Rare Case of Terson Syndrome With Subarachnoid HemorrhageNinaNo ratings yet
- Atypical Presentation of Optic Neuritis in Multiple Sclerosis - Dian ParamitasariDocument15 pagesAtypical Presentation of Optic Neuritis in Multiple Sclerosis - Dian ParamitasariGufront MustofaNo ratings yet
- Esferofauia Aislada y GlaucomaDocument3 pagesEsferofauia Aislada y GlaucomaManuel VasquezNo ratings yet
- Penatalaksanaan Glaukoma Sekunder Refrakter Pada Implantasi Lensa Intraokular Bilik Mata Depan - Pauline Meilisa SihiteDocument13 pagesPenatalaksanaan Glaukoma Sekunder Refrakter Pada Implantasi Lensa Intraokular Bilik Mata Depan - Pauline Meilisa SihiteZikra Herlius14No ratings yet
- Orbital Apex Syndrome Secondary To Herpes Zoster OphthalmicusDocument4 pagesOrbital Apex Syndrome Secondary To Herpes Zoster OphthalmicusYosiita KartinaaNo ratings yet
- Vogt Koyanagi Harada SyndromeDocument9 pagesVogt Koyanagi Harada SyndromeBianca PavelNo ratings yet
- Angle Recession GlaucomaDocument15 pagesAngle Recession GlaucomaDia Asri RusliNo ratings yet
- Downloadophthalmology Cases All Team PDF PDF Free - HTMLDocument23 pagesDownloadophthalmology Cases All Team PDF PDF Free - HTMLDương Yến TrânNo ratings yet
- Traumatic Hyphema: A Teaching Case Report: Priscilla Lenihan, OD Dorothy Hitchmoth, OD, FAAODocument9 pagesTraumatic Hyphema: A Teaching Case Report: Priscilla Lenihan, OD Dorothy Hitchmoth, OD, FAAOMarshaNo ratings yet
- Diagnosis Dan Tatalaksana Steroid Induced Glaucoma - Andivan Rahman PDFDocument11 pagesDiagnosis Dan Tatalaksana Steroid Induced Glaucoma - Andivan Rahman PDFMarini Yusufina LubisNo ratings yet
- Letters To The EditorDocument8 pagesLetters To The EditorGheavita Chandra DewiNo ratings yet
- Prospective Evaluation of Acupuncture As Treatment For GlaucomaDocument10 pagesProspective Evaluation of Acupuncture As Treatment For Glaucoma16.11Hz MusicNo ratings yet
- Penatalaksanaan Pasien Glaukoma Sudut Terbuka Dengan PemasanganintanmaulaDocument10 pagesPenatalaksanaan Pasien Glaukoma Sudut Terbuka Dengan PemasanganintanmaulaShela GranityaNo ratings yet
- The Chiropractic Care of An Infant Female With A Medical Diagnosis of Strabismus: A Case ReportDocument4 pagesThe Chiropractic Care of An Infant Female With A Medical Diagnosis of Strabismus: A Case ReportAndrea Parisio-FerraroNo ratings yet
- Ace SetiawanDocument11 pagesAce SetiawanGlaucoma UnhasNo ratings yet
- Jurnal StrabismusDocument3 pagesJurnal StrabismusBonita AsyigahNo ratings yet
- Diagnosis BandingDocument10 pagesDiagnosis BandingIntan Rahmi NasyaNo ratings yet
- Cogan-Reese Syndrome - A Rare Case of Unilateral GlaucomaDocument8 pagesCogan-Reese Syndrome - A Rare Case of Unilateral GlaucomaDr. Abhishek OnkarNo ratings yet
- Lapkas Glaukoma Pemasangan Implan GDD Lapkas Glaukoma (AutoRecovered)Document14 pagesLapkas Glaukoma Pemasangan Implan GDD Lapkas Glaukoma (AutoRecovered)Vincent RoorohNo ratings yet
- 86 Normal Low Tension Glaucoma PDFDocument4 pages86 Normal Low Tension Glaucoma PDFSherZalattha KuchikiElfNo ratings yet
- Ocular Myasthenia Gravis in Children A Case Report - Muhammad Arief MunandarDocument10 pagesOcular Myasthenia Gravis in Children A Case Report - Muhammad Arief Munandarirvan rahmanNo ratings yet
- 1 PBDocument4 pages1 PBRian YupitaNo ratings yet
- Adverse Drug Reaction FormDocument2 pagesAdverse Drug Reaction FormAhmad SaeedNo ratings yet
- Bilatteral Acute Angle Closure GlaucomaDocument17 pagesBilatteral Acute Angle Closure GlaucomaAhmed_Algihady_2987No ratings yet
- Case Report Urretz Zavalia SyndromeDocument6 pagesCase Report Urretz Zavalia SyndromeAi HidayatNo ratings yet
- Case ReportDocument7 pagesCase ReportJeel GaralaNo ratings yet
- A Review of Optic NeuritisDocument5 pagesA Review of Optic NeuritissatrianiNo ratings yet
- Questions and Answer Group 3 "Glaucoma" Nama: Gustin Ibrahim Umamah Kelas: A S1 FARMASI 2017 NIM: 821417021Document13 pagesQuestions and Answer Group 3 "Glaucoma" Nama: Gustin Ibrahim Umamah Kelas: A S1 FARMASI 2017 NIM: 821417021Afni YunitaNo ratings yet
- Opth 8 1351Document5 pagesOpth 8 1351Muhammad Halil GibranNo ratings yet
- Tatalaksana Dan Prognosis Severe Visual Impairment Pada Miopia Patologi - Nikho Melga ShalimDocument14 pagesTatalaksana Dan Prognosis Severe Visual Impairment Pada Miopia Patologi - Nikho Melga ShalimOt PtkNo ratings yet
- PDF StrabismusDocument1 pagePDF StrabismusirawadiputraNo ratings yet
- Association Between Hypertriglyceridemia and Open Angle Glaucoma: A Case ReportDocument3 pagesAssociation Between Hypertriglyceridemia and Open Angle Glaucoma: A Case Reportsyntacs skNo ratings yet
- Case IIM Tama NewDocument11 pagesCase IIM Tama NewAryati PutriNo ratings yet
- Penatalaksanaan Pasien Dengan Sudut Tertutup Primer - DegianaDocument13 pagesPenatalaksanaan Pasien Dengan Sudut Tertutup Primer - Degianacindy sweeteniaNo ratings yet
- Topiramate Induced GlaucomaDocument38 pagesTopiramate Induced GlaucomaArnob ShahriarNo ratings yet
- Ni Hms 419332Document10 pagesNi Hms 419332Monica Lauretta Sembiring IINo ratings yet
- American Journal of Emergency Medicine: Dietrich Jehle Mary Claire Lark, Clay O'BrienDocument3 pagesAmerican Journal of Emergency Medicine: Dietrich Jehle Mary Claire Lark, Clay O'BrienGufront MustofaNo ratings yet
- Neurosyphilis Masquerading As An Acute Adie's Tonic Pupil: Report of A CaseDocument6 pagesNeurosyphilis Masquerading As An Acute Adie's Tonic Pupil: Report of A CaseOlvaria MisfaNo ratings yet
- Catarta e HipoparatiroidismoDocument3 pagesCatarta e HipoparatiroidismoBernardo RomeroNo ratings yet
- Departemen Ilmu Kesehatan Mata Fakultas Kedokteran Universitas Padjadjaran Pusat Mata Nasional Rumah Sakit Mata Cicendo BandungDocument11 pagesDepartemen Ilmu Kesehatan Mata Fakultas Kedokteran Universitas Padjadjaran Pusat Mata Nasional Rumah Sakit Mata Cicendo BandungBambang RinandiNo ratings yet
- Tatalaksana Operatif Dan Pascaoperatif Pada Pasien Juvenile Open Angle Glaucoma JOAG - Andreas Lukita HalimDocument14 pagesTatalaksana Operatif Dan Pascaoperatif Pada Pasien Juvenile Open Angle Glaucoma JOAG - Andreas Lukita HalimINDRINo ratings yet
- EENT Weekly TestDocument8 pagesEENT Weekly Testrajivsingal248No ratings yet
- Mindanao Medical Foundation CollegeDocument4 pagesMindanao Medical Foundation Collegeleidysaves0821No ratings yet
- Laporan Kasus SACG Dan Katarak Kongenital Pada AniridiaDocument15 pagesLaporan Kasus SACG Dan Katarak Kongenital Pada AniridiaIntan EkarulitaNo ratings yet
- Asian Upper Eyelid Blepharoplasty Sebagai Tatalaksana Dermatokalasis - Adessa RachmaDocument11 pagesAsian Upper Eyelid Blepharoplasty Sebagai Tatalaksana Dermatokalasis - Adessa Rachmafadil ahmadi100% (1)
- Running Head: A Patient Who Has Glaucoma 1Document10 pagesRunning Head: A Patient Who Has Glaucoma 1Alonso LugoNo ratings yet
- Revisi Ke-3 Journal Glaucoma (Group 12)Document12 pagesRevisi Ke-3 Journal Glaucoma (Group 12)TaschiaNo ratings yet
- Diagnosis Dan Tatalaksana Pasien Dengan Insufisiensi Akomodasi - Sri Hudaya WidihasthaDocument13 pagesDiagnosis Dan Tatalaksana Pasien Dengan Insufisiensi Akomodasi - Sri Hudaya WidihasthamalaNo ratings yet
- Orbital Apex Syndrome With Encephalitis A Rare and Serious Complication of Herpes Zoster Opthalmicus - Ludwig Melino Tjokrovonco 2Document12 pagesOrbital Apex Syndrome With Encephalitis A Rare and Serious Complication of Herpes Zoster Opthalmicus - Ludwig Melino Tjokrovonco 2Handi KrisnaniNo ratings yet
- Grand Rounds Glaucoma NTGDocument37 pagesGrand Rounds Glaucoma NTGRon TongbaiNo ratings yet
- Soal TryoutDocument3 pagesSoal Tryouthanidya fazwatNo ratings yet
- A Case of Angle-Closure Glaucoma, Cataract, Nanophthalmos and Spherophakia in Oculo-Dento-Digital SyndromeDocument3 pagesA Case of Angle-Closure Glaucoma, Cataract, Nanophthalmos and Spherophakia in Oculo-Dento-Digital SyndromeSriana K. LaliyoNo ratings yet
- 100122-Article Text-1484-2-10-20220311Document11 pages100122-Article Text-1484-2-10-20220311muzakiNo ratings yet
- IJCRR Nov2020 Vol12 Issue22Document9 pagesIJCRR Nov2020 Vol12 Issue22Aravind KumarNo ratings yet
- ACT TherapyDocument7 pagesACT TherapyPrince AroraNo ratings yet
- Associated Persons: Bertram Welton Sippy Description: TreatmentDocument5 pagesAssociated Persons: Bertram Welton Sippy Description: Treatmentkill_noj_olarcNo ratings yet
- Shoma Morita - WikipediaDocument8 pagesShoma Morita - WikipediacamicrisNo ratings yet
- Magnesium in Women's Health and Gynecology: Shawna Tonick, Ozgul Muneyyirci-DelaleDocument9 pagesMagnesium in Women's Health and Gynecology: Shawna Tonick, Ozgul Muneyyirci-DelaleyoggsssNo ratings yet
- Attitudinize Psychotherapy NewDocument30 pagesAttitudinize Psychotherapy NewLeenah ÃskareeNo ratings yet
- Lauren Humphrey ResumeDocument2 pagesLauren Humphrey Resumeapi-242376719No ratings yet
- Penggunaan Ekstrak Buah Adas Dalam Mengurangi Dismenore Pada Remaja Putri Hermayanti, Gita Kostania, Siti YulaikahDocument8 pagesPenggunaan Ekstrak Buah Adas Dalam Mengurangi Dismenore Pada Remaja Putri Hermayanti, Gita Kostania, Siti YulaikahAnas TasiaNo ratings yet
- Maternal and Child Healthe Nursing MCQ 6Document18 pagesMaternal and Child Healthe Nursing MCQ 6shanika100% (2)
- Spine Oncology, An Issue of Orthopedic Clinics PDFDocument168 pagesSpine Oncology, An Issue of Orthopedic Clinics PDFThanh Le DangNo ratings yet
- Morning Report Tension Type HeadacheDocument12 pagesMorning Report Tension Type HeadacheLintan FarzNo ratings yet
- Nutrition Repaired)Document10 pagesNutrition Repaired)Brylle MirandaNo ratings yet
- Kanner 2016Document11 pagesKanner 2016Izara Maité Mondragón MorenoNo ratings yet
- Presentation 307w Correct One MeatballsDocument24 pagesPresentation 307w Correct One Meatballsapi-347761303No ratings yet
- Lecture 1 Historical Aspects of Surgery (Core)Document27 pagesLecture 1 Historical Aspects of Surgery (Core)Charwinth KankaNo ratings yet
- Kpop Body Challenge Diet FinalDocument5 pagesKpop Body Challenge Diet FinalJaneNo ratings yet
- Mcfadden S System o 00 Mac FDocument144 pagesMcfadden S System o 00 Mac FcgonzjamNo ratings yet
- Livro - Acido LáticoDocument670 pagesLivro - Acido LáticoLuciana CoelhoNo ratings yet
- Behavior TheoryDocument6 pagesBehavior Theoryapi-401555861No ratings yet
- Pharmacology of Thyroid Hormones and Anti Thyroid Drugs For Second Year Medicine StudentsDocument48 pagesPharmacology of Thyroid Hormones and Anti Thyroid Drugs For Second Year Medicine StudentsAmanuel MaruNo ratings yet
- Chocolate: Chocolate Is A Raw or Processed Food Produced From The Seed of The TropicalDocument7 pagesChocolate: Chocolate Is A Raw or Processed Food Produced From The Seed of The TropicalNyimas Irina SilvaniNo ratings yet
- Traumatic Brain Injury A Case Report: SCORE:40/50Document10 pagesTraumatic Brain Injury A Case Report: SCORE:40/50Allan CastroNo ratings yet
- Atm 04 08 160Document9 pagesAtm 04 08 160manalNo ratings yet
- Mechanical Ventilation SeminarDocument82 pagesMechanical Ventilation Seminarrajan kumar91% (22)
- Clearing Clutter With EFT BonusDocument10 pagesClearing Clutter With EFT BonusKristen Hammer75% (4)
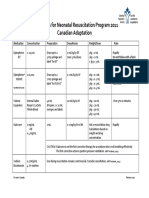
- Medications For Neonatal Resuscitation Program 2011 Canadian AdaptationDocument1 pageMedications For Neonatal Resuscitation Program 2011 Canadian AdaptationrubymayNo ratings yet
- The Vibration of Exceptional Health - Carol LookDocument5 pagesThe Vibration of Exceptional Health - Carol LookMichael CliftonNo ratings yet
- CipaDocument15 pagesCipaapi-247628136No ratings yet
- Yang Line Hani CD 10Document13 pagesYang Line Hani CD 10Janine NogueraNo ratings yet