Professional Documents
Culture Documents
5
5
Uploaded by
rahmawati aliwarmanCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
5
5
Uploaded by
rahmawati aliwarmanCopyright:
Available Formats
Berents et al.
BMC Dermatology (2015) 15:7
DOI 10.1186/s12895-015-0027-9
RESEARCH ARTICLE
Open Access
Topical treatment with fresh human milk versus
emollient on atopic eczema spots in young
children: a small, randomized, split body,
controlled, blinded pilot study
Teresa Lvold Berents1,2*, Jrgen Rnnevig1,2, Elisabeth Syland3, Peter Gaustad1,4, Gro Nylander5
and Beate Fossum Lland5
Abstract
Background: Public health nurses report on effects of fresh human milk as treatment for conjunctivitis, rhinitis and
atopic eczema (AE), the latter being highly prevalent in early childhood. Emollients and topical corticosteroids are
first line treatment of AE. As many caregivers have steroid phobia, alternative treatment options for mild AE are of
interest. The aim of this small pilot study was to assess the potential effects and risks of applying fresh human milk
locally on eczema spots in children with AE.
Methods: This was a split body, controlled, randomized and physician blinded pilot study, of children with AE with
two similar contralateral eczema spots having a mother breastfeeding the child or a sibling. Fresh expressed milk
and emollient was applied on the intervention spot and emollient alone on the control area, three times a day for
four weeks. The severity and area of the eczema spots was evaluated weekly, and samples from milk and the spots
were analysed weekly with respect to bacterial colonisation.
Results: Of nine patients included, six completed the study. Mean age at inclusion was 18.5 months. The spots
examined were localized on the arms, legs or cheeks. The spots were similar in severity, but differed in area. In one
patient the eczema ceased after inclusion. In four patients both control and intervention areas increased during the
intervention. The relative change in eczema area compared to baseline showed less increase in the intervention
spots in two patients, whereas the opposite was observed in three. In four children Staphylococcus aureus was
found in their eczema once or more. In three of the 28 human milk samples, Staphylococcus aureus, alfa haemolytic
streptococci or coagulase negative staphylococci were detected. Staphylococcus aureus was found once both in
human milk and in the eczema spots, no clinical signs of infection were however observed. No secondary infection
due to milk application was detected.
Conclusion: In this small pilot study, no effect was found on eczema spots treated with topical application of fresh
human milk. (ClinicalTrials.gov Identifier, NCT02381028).
Keywords: Atopic eczema, Children, Human milk, Emollient, Topical treatment, Pilot study
* Correspondence: t.l.berents@medisin.uio.no
1
Institute of Clinical Medicine, University of Oslo, Oslo, Norway
2
Department of Dermatology, Oslo University Hospital, Oslo, Norway
Full list of author information is available at the end of the article
2015 Berents et al.; licensee BioMed Central. This is an Open Access article distributed under the terms of the Creative
Commons Attribution License (http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and
reproduction in any medium, provided the original work is properly credited. The Creative Commons Public Domain
Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article,
unless otherwise stated.
Berents et al. BMC Dermatology (2015) 15:7
Background
Atopic eczema (AE) is a common, chronic, pruritic,
relapsing skin disease which affects up to 20% of children
in the Nordic European countries [1]. AE is strongly
associated with other atopic disorders, such as allergic
rhinitis and asthma [2]. The pathogenesis is interplay
between barrier dysfunction, genetic, immunological,
environmental factors and colonization by Staphylococcus
aureus (S. aureus) [3].
The treatment algorithm in AE is based on treating
the barrier defect, the inflammation, the infection and
the pruritus [4]. First line treatment is treating the
barrier defect with optimal skin care by the use of
emollients and baths. If a clinical infection is present
in the eczema, local antiseptics may be utilized; for severe
cases systemic antibiotics are needed. The inflammation is
treated with topical steroid creams. Topical steroids have
been shown to be a well-tolerated treatment, but in spite
of this many caregivers have steroid phobia, mainly
because of the potential side effects [5]. A treatment
option in chronic eczema is topical calcineurin inhibitors;
these are however not to be used in children under two
years of age [4]. Alternatives without side effects for young
children are therefore of interest.
Human milk may represent a source with potential
treatment properties. Knowledge of the immunological
qualities of mammalian milk can be traced back to 1892,
when Paul Ehrlich demonstrated that newborn mice were
protected against the toxic effects of phytotoxins if they
were fed milk from an immunized mouse [6]. Today,
numerous studies have contributed to our present
knowledge of the short- and long-term effects of human
milk in the breastfed child [7]. Mammalian milk is species
specific. Human milk contains specialized immune
components, including factors with anti-microbial and
anti-inflammatory properties [8], which theoretically
could be responsible for an effect on eczema spots
when applied topically.
In Norway, public health nurses report several cases
where parents have had positive experiences with topic
applications of expressed human milk in eyes of children
with conjunctivitis and on eczema spots in children with
AE. We have not been able to find any studies investigating
such treatment in children with AE. However, local
use of expressed human milk has been studied for
diaper dermatitis, rhinitis and conjunctivitis [9,10].
The aim of this small pilot study was to assess the
potential positive and/or negative effects of topical
use of expressed, fresh human milk on eczema spots
in young children with AE by evaluating the eczema
areas. A secondary aim was to evaluate any bacterial
transmission from human milk to the eczema spots,
causing infection in the child. Finally the mothers
compliance to the treatment was of interest.
Page 2 of 7
Methods
Trial design
This was a split body controlled, randomized and physician
blinded study of expressed human milk and emollients on
contralateral eczema spots in children, the trial was registered at ClinicalTrials.gov Identifier, NCT02381028.
Inclusion criteria were children with AE according to
Hanifin and Rajkas criteria [11] with a mother breastfeeding
the child or a sibling. The eczema spots in the treatment
and control areas were to be similar in features and extent
as well as being localized on contralateral parts of the
body. Children were excluded if the severity of the eczema
spots indicated need for treatment with antibiotics and/or
steroids.
The study was approved by the Regional Committee for
Medical and Health Research Ethics - South East Norway.
Mothers of participating children were informed verbally
and in writing, and signed an informed consent prior to
commencing the study.
Recruitment
Study patients were recruited through advertisement
posters from three different well baby clinics in Oslo,
Norway, in the period 20082011. Mothers interested in
the study contacted the study team. The consultations
mainly took place at the hospital; a few were carried out
in the childs home. The mothers were able to contact the
examining physician if they experienced any problems
with the treatment.
Intervention
The study intervention was local application of fresh
human milk on the study area. By hand milking, the
mothers were to squeeze out and throw away the first few
droplets of milk, and then squeeze the next droplets
directly from the nipple to the eczema spot. The number of
milk droplets depended on the size of the eczema area; the
mothers were instructed to cover the whole eczema spot
with milk. After absorption of the milk droplets, both treatment and control areas were treated with moisturizing
cream (Apobase creme, Actavis Norway AS). The cream
contains: Aqua, Paraffinum Liquidum, Petrolatum, Cetearyl
Alcohol, Ceteareth-20, Ceteareth-12, Sodium Gluconate,
Caprylyl Glycol, Phenoxyethanol, with a total lipid content
of 30 percent. Both intervention and control areas were
treated with this regimen three times a day for four weeks.
Randomization and blinding
The same physician examined all the children, and was
blinded as to which areas were the control or intervention
sites. At inclusion the physician diagnosed the AE according
to Hanifin and Rajkas criteria [11]. The two contra-lateral
eczema spots to be randomized were elected; i.e. flexural
aspect of elbow, flexural aspect of knees or cheeks. Another
Berents et al. BMC Dermatology (2015) 15:7
Page 3 of 7
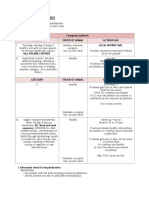
Flow Diagram
Assessed for eligibility: 9 children
with similar contralateral eczema spots
Enrollment
n=18
Excluded: None
Randomized (n=18 i.e. all)
Allocation
Allocated to intervention
(n= 9)
Allocated to control
(n=9)
Follow-Up
Lost to follow-up (n=3)
Lost to follow-up (n=3)
Discontinued intervention; one due to
remission, one due to hospitalization and one
never met for follow up
Discontinued intervention; one due to
remission, one due to hospitalization and
never met for follow up
Analysis
Analysed (n= 6)
Excluded from analysis: None
Analysed (n=6)
Excluded from analysis: None
Figure 1 Flow diagram. Nine children with atopic eczema and bilateral eczema lesions were assessed for eligibility to a small split body,
controlled, physician blinded pilot study evaluating human milk and emollient versus emollient alone on eczema lesions. Three children
were lost to follow up.
physician, who did not see the child, was responsible for the
randomization. The child was given a randomization
number and the mothers were then informed on which side
to apply the fresh expressed human milk and emollient,
and on which side to apply emollient alone.
Follow-up
After inclusion, the children were examined once weekly
for four consecutive weeks. The overall severity of AE
was evaluated by the use of SCORAD, which defines
mild disease as score <25, moderate disease between
2550 and severe disease as scores >50 [12]. The severity
of the study and control areas were evaluated by scoring
the erythema, lichenification, excoriation and pruritus on
a scale from 0 to 3, where 0 is none and 3 is severe. Study
and control areas were measured using Visitrak (Smith &
Nephew), a portable device used to measure the area of
wounds [13]. A transparent folio is placed over the area
and the borders are outlined, whereafter a computer
determines the area measured in cm2. In the present
study this device was used to follow the development
of the extent of the eczema spots.
At each visit, samples for bacterial cultures were taken at
eczema spots and from breastmilk, using Amies Agar Gel
with CharcoalTM, Copan Venturi Transystem (Copan,
Brescia, Italy). Sampling from eczema spots was done by
carefully rubbing the cotton swab over the eczema spot.
Sampling of breastmilk was done from milk expressed by
hand milking. The specimens were cultivated on blood
agar plates and selective media for S. aureus and for
gram-negative rods.
Outcome
The primary outcome was to register proportional change
in the area of the eczema spot from baseline, as measured
by Visitrak. The secondary outcome was to assess transmission of bacteria from mothers milk to eczema spots in
the child. The mothers compliance was also evaluated.
Statistical methods
Descriptive statistics were performed. The areas of the
intervention and control sites for each child were not
identical; therefore differences were calculated as
percentages: Changes in the areas of the control and
Berents et al. BMC Dermatology (2015) 15:7
intervention sites each week were calculated as change in
proportion of area related to baseline area.
Results
Study population
Nine children, four male, were recruited for the study
through advertisement posters from three different well
baby clinics in Oslo, Norway in the period 20082011.
Three of these nine children were lost to follow-up
consultations; one experienced remission from AE, the
second suffered from severe AE and was hospitalized, the
third never met for follow up (Figure 1). Two children
were treated with mothers milk produced for a younger
sibling. The mean age of the children was 18.5 months
(min, max; 4, 32). At inclusion mean SCORAD was 35
(min, max; 22, 45) and at the end of the study mean
SCORAD was 34 (min, max; 18, 52). The spots examined
were localized on the arms or legs in five of the children
and on the cheeks in one. The spots were similar in severity,
however the extent differed some.
Changes in measured area of eczema
The weekly change in the control and intervention eczema
area related to baseline eczema area is illustrated in
Figure 2. At the end of the study, child number one
and seven displayed less area involvement in the area
treated with human milk compared to the emollient
Page 4 of 7
treated area. In child number two, five and nine the
emollient treated area showed at study end less
involvement than the area treated with human milk.
The eczema spots in child number eight disappeared
after inclusion.
Most of the children showed an improvement of their
general eczema, except for child five, who showed a
slight increase. Child seven differs from the other children:
this child experienced a worsening of the total eczema,
having mild atopic eczema at inclusion, and severe atopic
eczema at week four.
Changes in presence of bacterial species
Four of the children had positive S. aureus cultures in
their eczema once or more (Table 1). However, only in
four of twelve occasions this coincided with clinical signs
of infection. Gram-negative rods were found in child
number one at one visit. S. aureus, alfa haemolytic
streptococci or coagulase-negative staphylococci were
detected in three of the 28 human milk samples. Only
on one occasion the same bacteria (S. aureus) were
detected in both the eczema lesions and the human
milk (child number five), and signs of clinical infection
were present (Table 1). The intervention areas differed
some from the control areas, as S. aureus was found in
intervention area but not in the control area on four
occasions in three different children (Table 1).
Figure 2 Change in eczema area. This figure illustrates the weekly difference between control and intervention sites based on the area change
from baseline in six children with atopic eczema included in a split body, controlled, physician blinded pilot study evaluating human milk and
emollient versus emollient alone on eczema lesions. Each line represents one child. The difference is calculated as: control area week 1, 2, 3 or 4
divided by control area at week 0 minus intervention area week 1, 2, 3 or 4 divided by intervention area at week 0. Lines above zero represent
improvement of the intervention area, and lines below zero represent the relative increase of the eczema areas of the intervention sites.
Berents et al. BMC Dermatology (2015) 15:7
Page 5 of 7
Table 1 Bacteria in eczema spots and human milk
Child
Week
Clinical infected
Study area
Control area
Human milk
No
No growth
No growth
Skin flora1
No
No growth
No growth
Missing
No
No growth
Skin flora
Missing
No
Gram negative rods
Gram negative rods
Skin flora
No
Skin flora
No growth
Skin flora
No
Skin flora
Skin flora
Skin flora
No
Skin flora
Skin flora
Skin flora
No
Skin flora
Skin flora
Skin flora
No
Skin flora
Skin flora
Skin flora
No
No growth
No growth
Skin flora
No
S. aureus (rich)
S. aureus (mod.2)
Skin flora
No
S. aureus (rich)
S. aureus (rich)
S. aureus (some col.3)
Yes
S. aureus (mod.)
S. aureus (sparse)
Skin flora
No
S. aureus (rich)
S. aureus (rich)
Skin flora
Yes
S. aureus (mod.)
Skin flora
Skin flora
No
Skin flora
Skin flora
Skin flora
Yes
Skin flora
Skin flora
CNS4
No
S. aureus (some col.)
Skin flora
Skin flora
No
Skin flora
Skin flora
Skin flora
No
S. aureus (some col.)
Skin flora
Skin flora
No
Missing
Missing
Missing
No
Skin flora
Skin flora
Skin flora
No
Skin flora
Skin flora
Skin flora
No
S. aureus (some col.)
Skin flora
Skin flora
No
Skin flora
Skin flora
Skin flora
No
S. aureus (some col.)
S. aureus (sparse)
Skin flora
Yes
S. aureus (mod.)
S. aureus (rich)
AHST5
No
S. aureus (sparse)
S. aureus (mod.)
No growth
Yes
S. aureus (mod.)
S. aureus (some col.)
Skin flora
Skin flora: non-pathogen bacteria belonging to the skin flora 2 mod.: moderate, 3col. colonies, 4CNS: coagulase negative staphylococci, 5AHST alfa
haemolytic streptococci.
Bacterial presence in samples taken from eczema spots and human milk weekly, and the presence of clinically judged infection in control and intervention sites of
six children with atopic eczema included in a split body, controlled, physician blinded pilot study evaluating human milk and emollient versus emollient alone on
eczema lesions.
Compliance
The mothers experienced the application of human milk
as an uncomplicated treatment option.
Discussion
In this small, split body controlled randomized pilot
study of human milk and emollient applied topically on
eczema spots in six children, no effect was found on
eczema spots treated with the topical application of fresh
human milk. In two of five children with persistent
eczema lesions during the study, there was less
involvement of the human milk treated area compared to
the emollient area at study end compared to baseline.
However, the opposite was found in three children.
There are few studies looking at the effect of human
milk on eczema. One study of children with diaper
dermatitis examined the effect of applying human milk
after each breastfeeding or hydrocortisone 1% ointment
twice a day, detecting after one week an effect of human
milk comparable to that of hydrocortisone [9]. The
application frequency was higher than in our study,
but we still believe that an application rate of three times
a day would be enough to show an effect of human milk,
after four weeks of treatment.
Berents et al. BMC Dermatology (2015) 15:7
There are many theoretical indications of how human
milk can be effective on eczema lesions. One aspect of
atopic disease is the type 2 helper T cell (Th2) dysbalance
with production of interleukin- 4 (IL-4), IL-5, and IL-13 in
the acute phase. In the chronic phase there is a Th1/Th0
dominance with production of interferon-, IL-2, IL-5 and
granulocyte-macrophage colony-stimulating factor [2]. Of
interest, therefore, are findings from an animal model,
where the effect of human colostrum used locally on an
acute inflammatory process was shown to be as potent as
oral indomethacin and superior to oral dexamethasone at
suppressing polymorphonuclear leukocyte influx [14,15].
In humans, the milk contains, among a wide variety of
biologically active hormones, glucocorticoids. These are
transferred from plasma to the milk in levels fairly highly
correlated (in the .6-.7 range) [16].
Milk samples from healthy donors have revealed
bacteria in 1023% of the samples [17]. In the present
study, bacteria were found in three of 28 samples; 11%.
In one child only (child number five), S. aureus was
found once in both the eczema spot and in the milk.
Clinically, however, the eczema was not infected, and
this child had S. aureus on both eczema lesions at every
visit. This suggests that no iatrogenic infections due to
application of fresh mothers milk occurred. Surprisingly,
S. aureus was found in the intervention area but not in
the control area on four occasions in three different
children. One speculation might be that the preservative (eg. phenoxyethanol) in the emollient had some
antimicrobial effect when applied alone.
Human milk contains several different substances that
act against bacteria, virus and fungi, such as Secretory IgA
and Secretory IgM [18], lactoferrin, lysozyme, oligosaccharides, Toll-like receptors and fatty acids [8]. In a study
evaluating the inhibition in vitro of human colostrum
against bacterial cultures from eye swabs of neonates with
neonatal conjunctivitis, the inhibitory activity was 50%
against S. aureus and coliform bacteria, demonstrating
an antimicrobial effect also in vitro [19]. A consistent
inhibitory effect of human milk was found against
Neisseria gonorrhea in children with conjunctivitis. A
significant but less pronounced effect was also found
against Moraxella catarrhalis [10]. This strengthens the
evidence for an antimicrobial effect of human milk also
when used topically. When comparing different methods
for preventing omphalitis in newborns, an application
frequency of topical human milk twice a day demonstrated
a shorter separation time of the umbilical stump compared
to the use of antiseptics [20]. In the study of Ibhanesebhor
[19], the mean duration of inhibition of human milk against
S. aureus was three hours. Considering the huge amount of
different biologically active components and cells in human
milk, there might be a variety of candidates for explaining
the positive effects described above.
Page 6 of 7
The children participating in the present study were
recruited through advertisement posters in well baby
clinics, and responding mothers were presumably highly
motivated and inclined to trust alternative/new treatment
methods. We cannot rule out that the mothers co-treated
the intervention sites with for instance steroid cream, but
the instructions with respect to treatment of the intervention and control site were clear, and the results do not
indicate performance bias.
Conclusions
The results of this small randomized, controlled pilot
study of six children with AE does not support an effect
of topical applied human milk. Treatment with fresh
expressed human milk seems safe and easy for mothers
to carry out.
Competing interests
The authors declare that they have no competing interests.
Authors contributions
TLB, BFL, JR, ES and GN were all involved in the design of the study,
drafting the protocol, analysing results and writing the paper. TLB provided
methodological considerations and carried out the clinical part. PG was
involved in analysing the bacteria cultures and in writing the paper.
All authors read and approved the final manuscript.
Acknowledgements
We thank the children and their parents for cooperation in this study.
The study team gratefully acknowledge Dr. PhD. Kristin Bergersen, Institute
of Clinical Medicine, University of Oslo and Department of Dermatology,
Oslo University Hospital, Oslo, Norway, for her important contribution to
the initial study design. The team also acknowledge preliminary analyses
provided by Mari Vrdal, Department of Biostatistics, Epidemiology and
Health Economy, Oslo University Hospital, Oslo, Norway.
Author details
1
Institute of Clinical Medicine, University of Oslo, Oslo, Norway. 2Department
of Dermatology, Oslo University Hospital, Oslo, Norway. 3Department of
Research, Education and Innovation, Oslo University Hospital, Oslo, Norway.
4
Department of Microbiology, Oslo University Hospital, Oslo, Norway.
5
Norwegian National Advisory Unit on Breastfeeding, Womens and Childrens
Division, Oslo University Hospital, Oslo, Norway.
Received: 14 February 2015 Accepted: 29 April 2015
References
1. Odhiambo JA, Williams HC, Clayton TO, Robertson CF, Asher MI.
Global variations in prevalence of eczema symptoms in children from
ISAAC phase three. J Allergy Clin Immunol. 2009;124(6):125158 e1223.
2. Bieber T. Atopic dermatitis. N Engl J Med. 2008;358(14):148394.
3. Leyden JJ, Marples RR, Kligman AM. Staphylococcus aureus in the lesions
of atopic dermatitis. British J Dermatol. 1974;90(5):52530.
4. Eichenfield LF, Tom WL, Berger TG, Krol A, Paller AS, Schwarzenberger K, et al.
Guidelines of care for the management of atopic dermatitis: section 2.
Management and treatment of atopic dermatitis with topical therapies.
J Am Acad Dermatol. 2014;71(1):11632.
5. Kojima R, Fujiwara T, Matsuda A, Narita M, Matsubara O, Nonoyama S, et al.
Factors associated with steroid phobia in caregivers of children with atopic
dermatitis. Pediat Dermatol. 2013;30(1):2935.
6. Ehrlich P. ber Immunitt durch Vererbung und Sugung. Zeitschrift fr
Hygiene und Infectionkrankheiten. 1892;12:183203.
7. Hornell A, Lagstrom H, Lande B, Thorsdottir I. Breastfeeding, introduction
of other foods and effects on health: a systematic literature review for the
5th Nordic Nutrition Recommendations. Food Nutrition Res. 2013;57:20823.
Berents et al. BMC Dermatology (2015) 15:7
8.
9.
10.
11.
12.
13.
14.
15.
16.
17.
18.
19.
20.
Page 7 of 7
Hosea Blewett HJ, Cicalo MC, Holland CD, Field CJ. The immunological
components of human milk. Adv Food Nutr Res. 2008;54:4580.
Farahani LA, Ghobadzadeh M, Yousefi P. Comparison of the Effect of
Human Milk and Topical Hydrocortisone 1% on Diaper Dermatitis.
Pediat Dermatol. 2013;30(6):7259.
Baynham JT, Moorman MA, Donnellan C, Cevallos V, Keenan JD.
Antibacterial effect of human milk for common causes of paediatric
conjunctivitis. Br J Ophthalmol. 2013;97(3):3779.
Hanifin JM, Rajka G. Diagnostic features of atopic dermatitis. Acta Derm
Venereol (Stockholm). 1980;92:447.
European Task Force on Atopic Dermatitis. Severity scoring of atopic
dermatitis: the SCORAD index. Consensus Report of the European Task
Force on Atopic Dermatitis. Dermatology. 1993;186(1):2331.
Sugama J, Matsui Y, Sanada H, Konya C, Okuwa M, Kitagawa A. A study of
the efficiency and convenience of an advanced portable wound
measurement system (VISITRAK). J Clin Nurs. 2007;16(7):12659.
Buescher ES. Anti-inflammatory characteristics of human milk: how, where,
why. Adv Exp Med Biol. 2001;501:20722.
Murphey DK, Buescher ES. Human colostrum has anti-inflammatory activity
in a rat subcutaneous air pouch model of inflammation. Pediatr Res.
1993;34(2):20812.
Grey KR, Davis EP, Sandman CA, Glynn LM. Human milk cortisol is
associated with infant temperament. Psychoneuroendocrinology.
2013;38(7):117885.
Lindemann PC, Foshaugen I, Lindemann R. Characteristics of breast milk
and serology of women donating breast milk to a milk bank. Arch Dis Child
Fetal Neonatal Ed. 2004;89(5):F4401.
Brandtzaeg P. The mucosal immune system and its integration with the
mammary glands. J Pediatr. 2010;156(2 Suppl):S815.
Ibhanesebhor SE, Otobo ES. In vitro activity of human milk against the
causative organisms of ophthalmia neonatorum in Benin City. Nigeria J
Trop Pediatr. 1996;42(6):3279.
Vural G, Kisa S. Umbilical cord care: a pilot study comparing topical human
milk, povidone-iodine, and dry care. J Obstet Gynecol Neonatal Nurs.
2006;35(1):1238.
Submit your next manuscript to BioMed Central
and take full advantage of:
Convenient online submission
Thorough peer review
No space constraints or color gure charges
Immediate publication on acceptance
Inclusion in PubMed, CAS, Scopus and Google Scholar
Research which is freely available for redistribution
Submit your manuscript at
www.biomedcentral.com/submit
You might also like
- Open RubricDocument71 pagesOpen RubricNgcwalisa Ntwalana100% (1)
- Risk RangerDocument31 pagesRisk Rangeranaiq82No ratings yet
- All RecallsDocument301 pagesAll RecallsFA Khan100% (2)
- Navidas-Case StudyDocument5 pagesNavidas-Case StudyFran LanNo ratings yet
- PolicyBookletV2 Child CareDocument163 pagesPolicyBookletV2 Child Carekiks101No ratings yet
- Artaud, Antonin - Collected Works, Vol. 4Document231 pagesArtaud, Antonin - Collected Works, Vol. 4stsddd83% (6)
- Pi Is 0196064409002704Document7 pagesPi Is 0196064409002704adesamboraNo ratings yet
- Emollient Enhancement of The Skin Barrier From Birth Offers Effective Atopic Dermatitis PreventionDocument6 pagesEmollient Enhancement of The Skin Barrier From Birth Offers Effective Atopic Dermatitis PreventionAditya Praja'schNo ratings yet
- Madu Colostomy PDFDocument6 pagesMadu Colostomy PDFdiahNo ratings yet
- Ijd 12764Document6 pagesIjd 12764onlymechelleNo ratings yet
- Probiotics in The Prevention of Eczema A Randomised Controlled Trial 2014 Archives of Disease in ChildhoodDocument7 pagesProbiotics in The Prevention of Eczema A Randomised Controlled Trial 2014 Archives of Disease in ChildhoodThiago TartariNo ratings yet
- Probiotics in Late Infancy Reduce The Incidence of Eczema: A Randomized Controlled TrialDocument6 pagesProbiotics in Late Infancy Reduce The Incidence of Eczema: A Randomized Controlled TrialarditaNo ratings yet
- Screening Neonatal PDFDocument12 pagesScreening Neonatal PDFDarly ReveloNo ratings yet
- Oral Ivermectin For Infants and Children Under 15 KG Appears To Be A Safe and Effective Treatment For ScabiesDocument1 pageOral Ivermectin For Infants and Children Under 15 KG Appears To Be A Safe and Effective Treatment For ScabiesALMFSNo ratings yet
- Literature Review of EczemaDocument6 pagesLiterature Review of Eczemaafmabkbhckmajg100% (1)
- Abstracts 853 125: 4 OCTOBER 2005: BackgroundDocument1 pageAbstracts 853 125: 4 OCTOBER 2005: BackgroundkelbmutsNo ratings yet
- Milk Oral Immunotherapy Is Effective in School-Aged ChildrenDocument6 pagesMilk Oral Immunotherapy Is Effective in School-Aged ChildrenAnry UmarNo ratings yet
- Probiotics in Pregnant Women To Prevent Allergic Disease: A Randomized, Double-Blind TrialDocument8 pagesProbiotics in Pregnant Women To Prevent Allergic Disease: A Randomized, Double-Blind TrialarditaNo ratings yet
- 403 PDFLVDocument7 pages403 PDFLVMaria Candida Junqueira ZachariasNo ratings yet
- DermatitisDocument6 pagesDermatitisAmalia Zulfa AmandaNo ratings yet
- Efficacy of Topical Sucralfate Versus Topical Zinc Oxide in Diaper Dermatitis: A Randomized, Double Blind StudyDocument4 pagesEfficacy of Topical Sucralfate Versus Topical Zinc Oxide in Diaper Dermatitis: A Randomized, Double Blind StudyDita Rahmita IlyasNo ratings yet
- ZZZZZZZZZZZZZZDocument8 pagesZZZZZZZZZZZZZZchloramphenicolNo ratings yet
- Emollient Use Alters Skin Barrier and Microbes in Infants at Risk For Developing Atopic DermatitisDocument17 pagesEmollient Use Alters Skin Barrier and Microbes in Infants at Risk For Developing Atopic DermatitisM TarmiziNo ratings yet
- Anaphylaxis in Infants - UpToDateDocument21 pagesAnaphylaxis in Infants - UpToDatealinaNo ratings yet
- A Pilot Study of Emollient Therapy For The Primary Prevention of Atopic DermatitisDocument7 pagesA Pilot Study of Emollient Therapy For The Primary Prevention of Atopic DermatitisAndia ReshiNo ratings yet
- Protective Effect of Breast Milk On Urinary Tract Infection in Children Aged 0-3 YearsDocument5 pagesProtective Effect of Breast Milk On Urinary Tract Infection in Children Aged 0-3 YearsChika FebrianiNo ratings yet
- The Effect of Topical Ointment On Neonatal Sepsis in Preterm InfantsDocument4 pagesThe Effect of Topical Ointment On Neonatal Sepsis in Preterm InfantsJill R SendowNo ratings yet
- Aloe Vera Calendula Officinalis: Clinical StudyDocument5 pagesAloe Vera Calendula Officinalis: Clinical StudyZeila OmarNo ratings yet
- Atopic DermatitisDocument31 pagesAtopic DermatitisityNo ratings yet
- JURNAL READINGnejmoa1007174Document11 pagesJURNAL READINGnejmoa1007174Sukma WinahyuNo ratings yet
- Achten 2018Document6 pagesAchten 2018bram AyuNo ratings yet
- Effect of Foot Reflexology On Neonatal JaundiceDocument7 pagesEffect of Foot Reflexology On Neonatal JaundiceSarini Suryadi100% (1)
- Comparative Study of 5 % Potassium Hydroxide Solution Versus 0.05% Tretinoin Cream For Molluscum Contagiosum in ChildrenDocument4 pagesComparative Study of 5 % Potassium Hydroxide Solution Versus 0.05% Tretinoin Cream For Molluscum Contagiosum in ChildrenMitha Sari IINo ratings yet
- Medical News in The World of Atopic Dermatitis First Quarter 2016Document5 pagesMedical News in The World of Atopic Dermatitis First Quarter 2016anon_384025255No ratings yet
- Probiotics For The Prevention of Allergy A Systematic ReviewDocument10 pagesProbiotics For The Prevention of Allergy A Systematic ReviewadhyNo ratings yet
- Atopic DermatitisDocument10 pagesAtopic DermatitisIboy ZulhamNo ratings yet
- JurnallDocument27 pagesJurnallMelan JustariNo ratings yet
- Emollients in Infancy To Prevent Atopic Dermatitis A Systematic Review and Meta-Analysis PDFDocument15 pagesEmollients in Infancy To Prevent Atopic Dermatitis A Systematic Review and Meta-Analysis PDFnita prmtasariNo ratings yet
- General Practice: Are Antibiotics Indicated As Initial Treatment For Children With Acute Otitis Media? A Meta-AnalysisDocument5 pagesGeneral Practice: Are Antibiotics Indicated As Initial Treatment For Children With Acute Otitis Media? A Meta-AnalysisJuan Carlos Aguayo RomeroNo ratings yet
- Timolol Maleate 0.5% or 0.1% Gel-Forming Solution For Infantile Hemangiomas: A Retrospective, Multicenter, Cohort StudyDocument4 pagesTimolol Maleate 0.5% or 0.1% Gel-Forming Solution For Infantile Hemangiomas: A Retrospective, Multicenter, Cohort Studydesta israwandaNo ratings yet
- Kulit Jurnal ReadingDocument20 pagesKulit Jurnal ReadingaulianmediansyahNo ratings yet
- Algorithm For Treatment of ImpetigoDocument9 pagesAlgorithm For Treatment of Impetigodrmostafa087No ratings yet
- Jung 2013Document10 pagesJung 2013drphvmNo ratings yet
- Probiotics and Prebiotics For Treatment and Prevention of Allergic DiseaseDocument9 pagesProbiotics and Prebiotics For Treatment and Prevention of Allergic Disease98043693No ratings yet
- Asian Paci Fic Journal of Tropical BiomedicineDocument5 pagesAsian Paci Fic Journal of Tropical BiomedicineYosia KevinNo ratings yet
- PR 2013 2 E8 PDFDocument4 pagesPR 2013 2 E8 PDFagashiNo ratings yet
- Insulin Allergy Can Be Successfully Managed by A Systematic ApproachDocument6 pagesInsulin Allergy Can Be Successfully Managed by A Systematic Approachjames antonyNo ratings yet
- Urticaria in Children and Adolescents: An Updated Review of The Pathogenesis and ManagementDocument18 pagesUrticaria in Children and Adolescents: An Updated Review of The Pathogenesis and ManagementEduardo Brustolin XavierNo ratings yet
- Cow S Milk Allergic ChildrenDocument12 pagesCow S Milk Allergic ChildrenNurul Huda KowitaNo ratings yet
- Nagel Et Al-2009-Pediatric Allergy and ImmunologyDocument8 pagesNagel Et Al-2009-Pediatric Allergy and ImmunologyKrishna PriyakaNo ratings yet
- Effect of Lactobacillus Sakei Supplementation in Children With Atopic Eczema - Dermatitis SyndromeDocument6 pagesEffect of Lactobacillus Sakei Supplementation in Children With Atopic Eczema - Dermatitis SyndromePutri Halla ShaviraNo ratings yet
- Ijerph 18 11555 PublishedDocument11 pagesIjerph 18 11555 PublishedMohamed L TarawalieNo ratings yet
- Comparison of Permethrin-Based Treatment Strategies Against Scabies in Infants and Young ChildrenDocument6 pagesComparison of Permethrin-Based Treatment Strategies Against Scabies in Infants and Young ChildrenNur Syah Fitriyana RamadhaniNo ratings yet
- Journ 3Document7 pagesJourn 3Yanasta Yudo PratamaNo ratings yet
- Full Text 01Document22 pagesFull Text 01Ronny BudimanNo ratings yet
- A Specific Synbiotic-Containing Amino Acid-Based Formula in Dietary Management of Cow's Milk AllergyDocument11 pagesA Specific Synbiotic-Containing Amino Acid-Based Formula in Dietary Management of Cow's Milk AllergyFabiola VaniaNo ratings yet
- Does Atopic Dermatitis Cause Food Allergy? A Systematic ReviewDocument8 pagesDoes Atopic Dermatitis Cause Food Allergy? A Systematic ReviewInten WulandariNo ratings yet
- M CAD Ermatol PrilDocument1 pageM CAD Ermatol PrilValentina AdindaNo ratings yet
- Ijpedi2019 1054943Document9 pagesIjpedi2019 1054943niaNo ratings yet
- Check Unit 555 November Immunology V3 PDFDocument25 pagesCheck Unit 555 November Immunology V3 PDFdragon66No ratings yet
- RCT Dimenhydrinate in Children With Infectious Gastroenteritis: A ProspectiveDocument13 pagesRCT Dimenhydrinate in Children With Infectious Gastroenteritis: A ProspectiveNamira AhmedNo ratings yet
- Listeriosis in PregnancyDocument4 pagesListeriosis in PregnancyMadalina VladNo ratings yet
- Two Methods of Cord Care in High-Risk Newborns: Their Effects On Hydration, Temperature, PH, and Floras of The Cord AreaDocument12 pagesTwo Methods of Cord Care in High-Risk Newborns: Their Effects On Hydration, Temperature, PH, and Floras of The Cord AreaFatma ElzaytNo ratings yet
- Feasibility of Eliminating Ocular Chlamydia Trachomatis With Repeat Mass Antibiotic TreatmentsDocument5 pagesFeasibility of Eliminating Ocular Chlamydia Trachomatis With Repeat Mass Antibiotic TreatmentsAmelia RoziantyNo ratings yet
- Characteristics of Atopic Dermatitis in Puskesmas (Public Health Center) Masaran 1 Sragen RegencyDocument8 pagesCharacteristics of Atopic Dermatitis in Puskesmas (Public Health Center) Masaran 1 Sragen RegencyShafira Nur LNo ratings yet
- Atopic Dermatitis: New Perspectives on Managing a Chronic Inflammatory DiseaseFrom EverandAtopic Dermatitis: New Perspectives on Managing a Chronic Inflammatory DiseaseRating: 5 out of 5 stars5/5 (1)
- CREZIERDocument1 pageCREZIERrahmawati aliwarmanNo ratings yet
- Without You (Reference Vocal) : Posting Lirik Ini Di Blog AndaDocument1 pageWithout You (Reference Vocal) : Posting Lirik Ini Di Blog Andarahmawati aliwarmanNo ratings yet
- Desviat 2006 CcaDocument4 pagesDesviat 2006 Ccarahmawati aliwarmanNo ratings yet
- All by MyselfDocument2 pagesAll by Myselfrahmawati aliwarmanNo ratings yet
- Steven Johnson SindromDocument5 pagesSteven Johnson Sindromrahmawati aliwarmanNo ratings yet
- JCN 11 262Document6 pagesJCN 11 262rahmawati aliwarmanNo ratings yet
- Histamine Antagonists For Treatment of Peripheral Vertigo: A Meta-AnalysisDocument5 pagesHistamine Antagonists For Treatment of Peripheral Vertigo: A Meta-Analysisrahmawati aliwarmanNo ratings yet
- Antimicrob. Agents Chemother. 2006 Chongtrakool 1001 12Document13 pagesAntimicrob. Agents Chemother. 2006 Chongtrakool 1001 12rahmawati aliwarmanNo ratings yet
- A Critical New Pathway For Toxin Secretion?: Clinical Implications of Basic ResearchDocument2 pagesA Critical New Pathway For Toxin Secretion?: Clinical Implications of Basic Researchrahmawati aliwarmanNo ratings yet
- Should We Use Ceftriaxone To Treat Staphylococcal.2Document2 pagesShould We Use Ceftriaxone To Treat Staphylococcal.2rahmawati aliwarmanNo ratings yet
- Was Darwin Wrong? National Geographic MagazineDocument8 pagesWas Darwin Wrong? National Geographic MagazineKarol DuranNo ratings yet
- NCP Deficient KnowlwdgeDocument2 pagesNCP Deficient KnowlwdgeMICHELLE MALLARENo ratings yet
- FULL Download Ebook PDF Krasners Microbial Challenge 4th Edition PDF EbookDocument41 pagesFULL Download Ebook PDF Krasners Microbial Challenge 4th Edition PDF Ebookconnie.vasquez242100% (43)
- Infection Control in PediatricDocument13 pagesInfection Control in PediatricToka HessenNo ratings yet
- Module Six Resource GuideDocument28 pagesModule Six Resource Guidejade tagabNo ratings yet
- Management TB MOH Singapore PDFDocument123 pagesManagement TB MOH Singapore PDFLindsley GruvyNo ratings yet
- American Journal of Infection ControlDocument5 pagesAmerican Journal of Infection ControlEileen Le RouxNo ratings yet
- (IJCST-V9I3P10:Akshat Rustagi, Rudrangshu Tarafder, J. Rene BeulahDocument7 pages(IJCST-V9I3P10:Akshat Rustagi, Rudrangshu Tarafder, J. Rene BeulahEighthSenseGroupNo ratings yet
- Module 8 Lesson 2Document15 pagesModule 8 Lesson 2Holly HepbourneNo ratings yet
- 6 Vol. 7 Issue 9 September 2016 IJPSR RE 1915Document9 pages6 Vol. 7 Issue 9 September 2016 IJPSR RE 1915Nur KhasanahNo ratings yet
- Antibiotic Prescribing Patterns at COVID-19 Dedicated Wards in Bangladesh: Findings From A Single Center StudyDocument5 pagesAntibiotic Prescribing Patterns at COVID-19 Dedicated Wards in Bangladesh: Findings From A Single Center Studyاحمد عرفاتNo ratings yet
- Naturamore English Flyer 2020 - 29012021123727Document6 pagesNaturamore English Flyer 2020 - 29012021123727Siddhi patidarNo ratings yet
- Kings Phlebotomists HCP Information BookletDocument7 pagesKings Phlebotomists HCP Information Bookletapi-94821083No ratings yet
- Ceva NecropsyDocument18 pagesCeva NecropsyNanda Ayu Cindy KashiwabaraNo ratings yet
- Rabies SupplementalsDocument6 pagesRabies SupplementalsJoher Bolante MendezNo ratings yet
- Microbiology and ParasitologyDocument11 pagesMicrobiology and ParasitologyNeil GuntingNo ratings yet
- Costochondritis OverviewDocument5 pagesCostochondritis Overviewice cold killaNo ratings yet
- Committee For Proprietary Medicinal Products (CPMP) : London, 31 May 2001 CPMP/BWP/41450/98Document11 pagesCommittee For Proprietary Medicinal Products (CPMP) : London, 31 May 2001 CPMP/BWP/41450/98samirneseemNo ratings yet
- Gpat Cracker Sample PDF Fundamental PharmacyDocument24 pagesGpat Cracker Sample PDF Fundamental PharmacyMohd Uzair AnsariNo ratings yet
- Dwnload Full Nursing Interventions and Clinical Skills 5th Edition Perry Test Bank PDFDocument35 pagesDwnload Full Nursing Interventions and Clinical Skills 5th Edition Perry Test Bank PDFbenjaminlaw0o100% (13)
- Antibacterial and Antifungal Drugs: Department of Chemistry University of HullDocument60 pagesAntibacterial and Antifungal Drugs: Department of Chemistry University of HullIrawan RiyanNo ratings yet
- Family Spirochaetaceae AND LeptospiraceaeDocument33 pagesFamily Spirochaetaceae AND Leptospiraceaeyosef awokeNo ratings yet
- Care and Support Needs of People Living With Hiv and AidsDocument13 pagesCare and Support Needs of People Living With Hiv and AidsSalihu MustaphaNo ratings yet
- Sample Rapid Test ResultDocument1 pageSample Rapid Test ResultKenneth Ann AsuncionNo ratings yet