Professional Documents
Culture Documents
Intraplatelet Serotonin in Patients With Diabetes Mellitus and Peripheral Vascular Disease
Intraplatelet Serotonin in Patients With Diabetes Mellitus and Peripheral Vascular Disease
Uploaded by
Hyeon DaOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Intraplatelet Serotonin in Patients With Diabetes Mellitus and Peripheral Vascular Disease
Intraplatelet Serotonin in Patients With Diabetes Mellitus and Peripheral Vascular Disease
Uploaded by
Hyeon DaCopyright:
Available Formats
European Journal of Clinical Investigation (1 988) 18, 399-404
Intraplatelet serotonin in patients with diabetes
mellitus and peripheral vascular disease
M. A. BARRADAS, D. S. GILL, V. A. FONSECA, D. P. MIKHAILIDIS & P. DANDONA, Metabolic
Department of Chemical Pathology and Human Metabolism, Royal Free Hospital and School of Medicine,
London, U.K.
Received 8 December 1987 and in revised form 9 February 1988
Abstract. Intraplatelet serotonin (5-HT) content was
determined in 23 patients with type I (insulin-dependent) diabetes mellitus (IDDM), 23 patients with type
I1
(non-insulin-dependent)
diabetes
mellitus
(NIDDM), 29 patients with peripheral vascular disease (PVD) and 34 age-matched normal subjects.
Intraplatelet 5-HT content in normal subjects showed
an age-related decline (r = - 0.45; P < 0.008), as has
been previously demonstrated. The median 5-HT
content in platelets of the young normal subjects was
4.36 (range: 3.62-6.79) nmol
platelets, while that
in the elderly normal subjects was 3.87 (range: 2.8-6.0)
nmol lop9 platelets and that in young+elderly subjects was 4.05 (range: 2.8-6.8) nmol
platelets. The
median intraplatelet 5-HT content was significantly
lower (P<0.002) in IDDM patients: 3-0 (range 1.36.3), NIDDM patients: 2.5 (range 1.7-5.8), PVD
patients: 2.42 (range 0.94-4.98) nmol lop9 platelets
than that in all young+elderly healthy subjects. The
presence of hypertension in DM patients caused a
small but significant (P< 0.05) decrease in intraplatelet
5-HT content, whilst its presence had no effect in PVD
patients. In a smaller study, it was established that
NIDDM and PVD patients have significantly
(P< 0.002) greater plasma 5-HT concentrations than
controls. Insulin-dependent diabetes mellitus patients
had greater plasma 5-HT concentrations but this did
not achieve statistical significance despite a 66%
increment in its value. We conclude that the diminished 5-HT content in platelets and the increased
plasma levels may reflect enhanced release of 5-HT by
hyperactive platelets. This increase in plasma 5-HT
may contribute to the pathogenesis of atherosclerosis
and vasospasm.
Keywords. Platelets, serotonin, diabetes mellitus, vascular disease, hypertension.
Correspondence: Dr P. Dandona, Director, Metabolic Unit,
Department of Chemical Pathology and Human Metabolism, The
Royal Free Hospital, Pond Street, London NW3 2QG, U.K.
Introduction
Serotonin (5-HT) is a vasoactive amine stored in the
electron dense granules of platelets [l]. During activation, platelets may secret 5-HT as well as other
vasoactive substances, which may then interact with
blood vessels, resulting in vasospasm and increased
vascular permeability [2]. Platelets are also thought to
contribute to the pathogenesis of atherosclerosis [2].
Since platelet hyperaggregability and an increased
incidence of atherosclerosis have been documented in
diabetic patients and patients with peripheral vascular
disease [3], a study of the intraplatelet content in these
disease states may provide an insight into the mechanisms underlying the pathogenesis of platelet hyperaggregability and accelerated atherogenesis in these
conditions.
We therefore carried out a study to determine the
relationship between intraplatelet 5-HT and age in
healthy subjects and in the following disease states:
type I (insulin-dependent) diabetes mellitus (IDDM),
type I1 (non-insulin-dependent) diabetes mellitus
(NIDDM) and peripheral vascular disease (PVD). We
also compared the intraplatelet 5-HT content in these
disease states with that in healthy subjects of similar
ages.
Patients and methods
Study I
Two groups of healthy subjects were studied as control
populations. One group of healthy subjects, elderly
controls, attending a local Day Centre consisted of 16
elderly healthy men and women (8 men, 8 women),
median age 72 years (range 56-80). Young controls
consisted of 18 younger, healthy men and women
(11 men, 7 women) members of the medical and
laboratory staff, median age 26 years (range 21-49).
For the appropriate age comparisons we combined the
two populations, which collectively consisted of 34
young and elderly subjects (19 men, 15 women;
median age 49 years, range 21-80). None of the
399
400
M. A. BARRADAS et al.
controls had a history of diabetes, vascular disease or
hypertension.
The patients studied were attending the diabetic and
vascular out-patient clinics at The Royal Free Hospital. The IDDM group consisted of 23 patients (1 1 men,
12 women); median age 50 years (range 23-72); median
duration of diabetes 6 years (range 2-25); median
blood glucose 11.5 mmol I- (range 4.0-28.3); median
glycosylated haemoglobin 9.5% (range 5.8-1 1.3). The
NIDDM group consisted of 23 patients (15 men, 8
women), median age 66 years (range 40-86); median
duration of diabetes 10 years (range 1-15); median
blood glucose 1I .4 mmol 1 I (range 5.2- 13.7);median
glycosylated haemoglobin 10.1O/o (range 7 - 5 15.1).
The PVD group consisted of 29 patients (18 men, 11
women); median age 73 years (range 47-79). All the
patients in the PVD group had: (i) intermittent
claudication for more than 6 months with (ii)
ank1e:arm systolic blood pressure (SBP) ratio < 0.85.
Patients were defined as hypertensive if they had a
diastolic blood pressure > 95 mmHg on two separate
occasions.
~
Study 2
For this study, a similar but smaller population of
patients and healthy subjects were sampled. The
control group consisted of 10 healthy subjects (7 men,
3 women); median age 50 years (range 25-68). The
IDDM group consisted of 11 patients (6 men, 5
women); median age 53 years (range 23-77); median
duration of diabetes 11 years (range 3-40). The
NIDDM group consisted of 14 patients (7 men, 7
women); median age 62 years (range 51-83); median
duration of diabetes 11 years (range 2 months-30
years). The PVD group consisted of 13 PVD patients
(10 men, 3 women); median age 68 years (range 56-83).
Patients were diagnosed as PVD according to the
criteria described in study 1.
Drugs
Healthy subjects denied taking drugs for at least 2
weeks prior to sampling. Diabetic patients were on
standard treatment regimens with insulin/oral hypoglycaemic agents and diet. Hypertensive patients (DM
and PVD) were on a combination of nifedipine and
bendrofluazide.
Blood sample collection and processing
Blood was taken from the antecubital vein of patients
and volunteers with minimal stasis, and nine parts of
bIood were added to one part of 3.8% w/v trisodium
citrate (BDH, Poole, Dorset, U.K.). To each 1 ml of
blood 100 pg of acetylsalicylic acid (BDH) were added
to prevent any release of intraplatelet constituents [4].
Plasma for serotonin measurements was prepared by
centrifuging blood for 20 min at 1500 x g at 22C. The
supernatant was frozen immediately and kept at
-40C until assay. Platelet rich plasma (PRP) was
prepared as previously described 151. Platelet counts
were then performed using a Coulter ZM counter
(Coulter Electronics Limited, Luton, Bedfordshire,
U.K.). Following counting, the PRP was centrifuged
at 1000 x g for 10 min to prepare platelet pellets. The
pellets were washed with Isoton I1 (Coulter Electronics
Limited) and stored at - 20C until analysis.
Platelet serotonin assay
Platelet pellets were resuspended in physiological
saline (0.9 w/v) and a platelet lysate prepared by
ultrasonicating the platetet pellet for 3 x 10 sec at an
amplitude of 18 microns using an MSE-Soniprep
sonicator (MSE, Sussex, U.K.). In order to ensure that
our sonication procedure fully disrupts platelets, we
counted, sized and plotted platelet populations before
and after sonication. For this purpose, platelets were
obtained from healthy subjects and the above parameters were assessed using a Coulter ZM counter with
a Channelyzer C-1000 and X-Y Recorder (Coulter
Electronics Limited). Following sonication, the platelet count was reduced to < 5 % of the original, the
mean platelet volume became unmeasurable and the
graphical plot obtained with the sonicated platelets
became indistinguishable from the plot obtained with
platelet diluent (Isoton 11). The serotonin content in
the platelet lysates was assayed by a modification of the
spectrofluorimetric method of Drummond & Gordon
[6,7]. Briefly, 6 M trichloroacetic acid (BDH) was added
to the platelet lysates to precipitate the proteins. The
samples were then centrifuged at 10 000 x g for 4 min.
A portion of the supernatants was removed and
transferred to glass test-tubes, and to each of these ophthaldialdehyde (Sigma Chemical Co., Poole, Dorset, U.K.) in HC1 was added, and the mixture heated
in boiling water for 10 min. The tubes were then cooled
in ice and washed twice with chloroform Analar
(BDH) to remove any traces of trichloroacetic acid [8].
The aqueous phase was removed and the fluorescence
was read in a Perkin-Elmer MPF-3 (Hitachi Ltd,
Tokyo, Japan) fluorescence spectrophotometer, with
excitation and emission wavelengths of 360 and 475
nm, respectively. Standards and blanks were processed
in the same way as the platelet lysates. The intra-assay
coefficient of variation (CV) for the whole procedure
was 4.0% (n = 20) and the interassay CV for the whole
procedure was 12% (n=8). As an added precaution,
samples from each of the groups studied were included
in each assay.
Plasma serotonin assay
Plasma serotonin concentrations were estimated using
a radioimmunoassay. Antisera, standards and reagents were purchased from Immunodiagnostics Ltd
(Washington, Tyne and Wear, U.K.). The intra-assay
CV for this method was 3.1% ( n = 10) and the
interassay CV was 5.1 % (n = 10).
INTRAPLATELET SEROTONIN IN DIABETES MELLITUS AND VASCULAR DISEASE
Blood glucose determination
401
when compared with platelets of younger healthy
subjects (see Table 1 for age range).
Blood glucose measurements were carried out in the
clinic at the time of blood sampling, using the YSI
Model 23 AM glucose analyser (Yellow Springs
Instruments, Yellow Springs, U.S.A.).
Comparison berween healthy subjects and diabetic
patients. Patients with IDDM had significantly
(P< 0.001) lower intraplatelet 5-HT when compared
with young elderly healthy subjects (Table 1).
Patients with NIDDM had significantly (P< 0.002)
lower intraplatelet 5-HT when compared with elderly
healthy subjects (Table 1). We selected different control populations in order to achieve comparability in
the age range with that of patients.
Intraplatelet 5-HT concentrations in IDDM and
NIDDM patients did not differ significantly. There
was no correlation between platelet 5-HT and age in
either IDDM or NIDDM patients, or when these
patients were pooled together (IDDM: n = 20,
r = - 043, P < 0.9; NIDDM: n = 22, r = - 0.2, P < 0.63;
IDDM + NIDDM: n = 42, r = - 0.04, P < 0.79). There
was also no significant correlation between platelet 5HT content and duration of diabetes (n=40,
r = - 0-04, P < 0.87), blood glucose (n=46, r = -0.2,
P = 0.2 1) and blood HbAl concentration (n = 22,
r = -0.02, P=O.93). There was no significant difference between IDDM and NIDDM with regard to
blood glucose concentrations or HbAl levels.
Glycosylated HbAl determination
Glycosylated HbAl measurements (electrophoretic
technique) were performed on whole blood using the
German-Hawksley glycosylated haemoglobin kit
(German-Hawksley, Northampton, U.K.).
Statistical analysis and expression of results
Platelet 5-HT content is expressed as nmol per lo9
platelets. Since the distribution of the data was nonparametric, the results are expressed as medians with
the range in parentheses.
The Mann-Whitney U-test (two-tailed) was used for
comparing unpaired data. Details of comparisons are
included in the appropriate tables. The Chi-square test
was used for the analysis of frequency. Linear regression analysis was carried out using a validated computer program in use in the Department of Chemical
Pathology and Human Metabolism at The Royal Free
Hospital.
Comparison between healthy subjects and patients
with PVD. Patients with PVD had significantly
(P< 0.002) lower intraplatelet 5-HT content when
compared with normal subjects of similar ages (Table
1). The presence of hypertension in PVD patients was
not associated with a further decrease in intraplatelet
5-HT (see below).
The median age and (range) of the PVD patients
studied (n=26) was 73 (47-79) years and the median
and (range) intraplatelet 5-HT (nmol lop9 platelets)
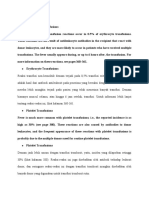
Results
Study I
Comparison between young and elderly healthy
subjects. In healthy subjects platelet 5-HT content
decreased with increasing age (n= 34, r = - 0.45,
P < 0.008). There was a significantly ( P < 0.05) lower 5HT content in the platelets of elderly healthy subjects
platelets) in young control subjects, elderly control subjects,
Table 1. Intraplatelet serotonin (5-HT) content (nmol
young+ elderly control subjects, insulin-dependent diabetic (IDDM), non-insulin-dependent diabetic (NIDDM), diabetics
(DM: IDDM + NIDDM) with high blood pressure (HBP) and with normal blood pressure (NBP), peripheral vascular disease
(PVD) with HBP and with NBP patients
Control subjects
D M patients
PVD patients
Young
Elderly Young+
elderly
IDDM
NIDDM
DM
DM
PVD
with NBP with HBP
No. subjects
18
16
34
23
23
26
18
29
12
12
Age (years)
26
21-49
72
56-80
49
21-80
50
23-72
66
40-86
56
31-76
65
56-73
73
47-79
71
56-78
74
56-78
5-HTcontent 4.36
3.87
4.05
3.62-6.79 2.8-6.0 2.8-6.79
PVD
PVD
with NBP with HBP
3.01t
2.461:
2-97**tt 2,487**$$ 2.42
2.77g
1.26-6.34 1.74--5.83 1-92-6.34 1.26-5.81 094-4.98 1.7-4.9
3.0111
0.6-4.82
Values are shown as median and range.
* vs. elderly subjects, P i 0.05; t vs. young+elderly subjects, P<O.OOI; 1: vs. elderly subjects, P i 0.002; 9 vs. elderly subjects,
PcO.002; 1 vs. D M with NBP, P<O.O5, ** vs. young+elderly subjects, P<O.OOI; tt vs. elderly subjects, P<0.003; $1vs. elderly
subjects, P<O.OOI; @ vs. elderly subjects, P i 0.04; 11 vs. elderly subjects, PiO.004.
There were no significant differences in intraplatelet 5-HT content when IDDM, N I D D M and PVD patients were compared
with each other.
402
M. A. BARRADAS et al.
Table 2. Intraplatelet 5-HT content and plasma concentrations in control
subjects, insulin-dependentdiabetics (IDDM), non-insulin dependent diabetics (NIDDM) and peripheral vascular disease (PVD) patients
Control/patient
population
Age
No.
patients (years)
Control
subjects
PVD patients
10
13
IDDM patients
I1
NIDDM patients 14
50
(25-68)
68
(56-83)
53
(23-77)
62
(51-83)
Plasma 5-HT
Intraplatelet 5-HT
(nmol
platelets) (nmol I ')
~
3.85
(1.84.05)
2.29*
(1.67-4.50)
2.24*
(1.26-3.75)
2.19t
(0.94-3.10)
100
(43-284)
2231
(165-767)
I66
(56-264)
291f
(108-938)
A separate, smaller population of control subjects and patients were
sampled for this study. See study 2 in the Patients and methods section.
* vs. control subjects, P < 0.05; t vs. control subjects, P < 0.02-P< 0.002;
1vs. control subjects: P i 0.002.
was 2.42 (0-94-4.98). There was no correlation
between intraplatelet 5-HT content and age in PVD
patients (n = 26, r = -0.04, P < 0.85).
A few patients with both PVD and DM were also
studied. These had a platelet 5-HT content that was
similar to that found in PVD and NIDDM patients.
The platelet 5-HT content of PVD patients did not
differ significantly from that in IDDM or NIDDM
patients.
Effect of hypertension on 5-HT content of platelets in
patients with DM and PVD.Diabetes mellitus patients
(IDDM + NIDDM pooled together) with hypertension had a significantly(P< 0.05) lower median intraplatelet 5-HT content than that in normotensive DM
patients. Chi-square analysis of the DM-hypertension/
no hypertension patients showed no significant difference in the frequency of NIDDMfIDDM in these
groups. Diabetes mellitus patients (IDDMNIDDM) with and without hypertension had significantly (P< 0.001) lower intraplatelet 5-HT than
young +elderly control subjects. Diabetes mellitus
patients with hypertension had significantly lower
(P< 0.001) intraplatelet 5-HT than elderly control
subjects (Table 1). Normotensive DM patients had
significantly (P< 0.003) lower intraplatelet 5-HT than
elderly control subjects (Table 1). The DM hypertension/no hypertension patients were compared with
both young elderly and elderly control subjects to
allow for better age matching between these groups.
There was no significant difference between the platelet
5-HT content of hypertensive and normotensive PVD
patients. Hypertensive PVD patients had a median
intraplatelet 5-HT content that was significantly
(P< 0.004) lower than that in elderly control subjects.
Normotensive PVD patients also had significantly
(P< 0.04) lower intraplatelet 5-HT concentration than
that in elderly control subjects.
Study 2
Plasma and intraplatelet 5-HTin healthy subjects and
IDDM, NIDDM and PVD patients. Plasma 5-HT
concentration was significantly raised in NIDDM and
PVD patients when compared with healthy subjects
(Table 2). Plasma 5-HT concentration in IDDM
patients was higher (66% increase) than in healthy
subjects but did not achieve statistical significance.
Plasma 5-HT concentrations in hypertensive
(n=10) and normotensive ( n = 1 5 ) DM (IDDM
+NIDDM) patients (170; 56-938 and 199; 63-497
nmol 1 - I , respectively) did not differ significantly.
Similarly, plasma 5-HTconcentration in the hypertensive ( n = 6 ) and normotensive ( n = 7 ) PVD patients
(230; 165-369 and 205; 170-767 nmol I-', respectively)
did not differ significantly.
Intraplatelet 5-HT concentrations broadly paralleled those described in study 1 .
Discussion
Our results show clearly for the first time that the 5-HT
content of platelets in NIDDM and PVD patients is
significantly lower than that in controls, and that
plasma 5-HT concentration in NIDDM and PVD
patients is also greater than that in controls. Our
observations also demonstrate that the 5-HT content
of platelets in IDDM is significantly lower than that in
controls; this is consistent with data recently reported
in a preliminary communication [9].
Previous studies that considered the uptake [ 101 or
content [9] of 5-HT by DM and PVD platelets are
limited by the absence of age-matched controls. This
factor was considered in the present study in view of
the evidence of an age-related decline in platelet 5-HT
content [ll]. We have also assessed the effect of
hypertension in our patients, since there is evidence
INTRAPLATELET SEROTONIN IN DIABETES MELLITUS AND VASCULAR DISEASE
that this factor is associated with decreased platelet
5-HT content [12-141.
Since platelets do not synthesize 5-HT [15], the
intraplatelet content of this amine is likely to be
dependent upon the net balance of uptake and release.
One previous study, although limited by the absence of
adequate controls, shows that platelet 5-HT uptake in
PVD patients and diabetics with retinopathy is diminished [ 101. There is also evidence that hyperaggregable platelets obtained from DM patients with vascular complications release more 5-HT than platelets
prepared from healthy subjects or diabetics without
vascular complications [16]. It is relevant to mention
that both DM and PVD are associated with hyperaggregability and an increase in the release of other
intraplatelet products (e.g. B-TG [3,17], PF-4 [3,18]
and TXA2 [19,20]). Even in young diabetics with no
obvious vascular complications, platelet hyperaggregability has been demonstrated using more sensitive
techniques such as whole blood impedance aggregation [21] or the measurement of platelet lifespan [3,22].
Thus, it is possible that the low 5-HT content of
platelets in these two conditions is the result of a
combination of decreased uptake and increased
release. This conclusion implies an increased plasma
pool of 5-HT, which is also known to enhance platelet
aggregation [23]. This latter change was reported in the
present study. It does not appear that the duration of
DM, or the quality of diabetic control, influences
intraplatelet 5-HT concentrations.
Our methodology using PRP for platelet 5-HT
determination may also have disadvantages: for example, higher density platelets with increased 5-HT
granule content may be lost during the centrifugation
procedure required to prepare PRP; however, this
potential artefact probably does not occur since we
found (using identical methodology) a significantly
increased and an unaltered intraplatelet histamine
content in PVD and DM patients, respectively [24].
This is of relevance since histamine, like 5-HT, is stored
in the dense granules 1251. An artefact would therefore
be expected to influence the intracellular content of
both these bioamines in a similar way. Furthermore,
alternative methodologies for homogeneous platelet
preparation (e.g. density gradients [26]) are comparatively more time-consuming and therefore unsuitable
for screening large numbers of patients.
The increase in plasma 5-HT concentrations
observed in the various patient groups could result in a
tendency to vasospasm, which is relevant to both
structural vascular disease (e.g. atherosclerosis) and to
secondary vasospastic disease (e.g. Raynauds phenomenon in systemic sclerosis). It is also relevant that
raised plasma levels of 5-HT have been reported in
hypertension [27], another condition associated with
low intraplatelet 5-HT f 131 and increased platelet
hyperaggregability [28]. Increased plasma concentrations of 5-HT may, to some extent, be self-perpetuating, since it could result in the activation of platelets
and the consequent further release of 5-HT from
403
platelets 1231. Whether this is true in DM and PVD
remains to be determined. Whether the increase in
plasma 5-HT concentrations is due to an increase in
the synthesis of this amine, or whether it merely reflects
a decrease in intraplatelet storage, is not clear. This
aspect requires further elucidation.
In conclusion, DM and PVD are associated with
diminished platelet 5-HT content over and above the
diminution caused by age. This decrease may be of
significance in the pathogenesis of atherosclerosis,
vasospasm and platelet hyperaggregability in these
conditions.
Acknowledgments
We thank Dr R. K. Menon and N. Carr for helpful
discussions, and Pamela Dale for preparing the manuscript.
References
1 Da Prada M, Richards JG, Kettler R. Amine storage organelles
in platelets. In: Gordon JL, ed. Platelets in Biology and
Pathology-2. Amsterdam: Elsevier/North Holland Biomedical
Press, 1981:107-45.
2 Cohen RA, Vanhoutte PM. Platelets, serotonin and endothelial
cells. In: Vanhoutte PM, ed. Serotonin and the Cardiovascular
System. New York: Raven Press, 1985:105-12.
3 Banga JD, Sixma JJ. Diabetes mellitus, vascular disease and
thrombosis. In: Chesterman CN, ed. Clinics in Haematology.
Eastbourne: WB Saunders, 1986:465-72.
4 Peerschke EIB. Calcium mobilization and fibrinogen binding of
platelets refractory to adenosine diphosphate stimulation. J Lab
Clin Med 1985;106:111-2.
5 Mikhailidis DP, Jenkins WJ, Barradas MA, Jeremy JY, Dandona P. Platelet function defects in chronic alcoholism. Br Med J
1986;293:715-8.
6 Dangelmeier CA, Holmsen H. Platelet dense granule and
lysosome content. In: Harker LA, Zimmerman T, eds. Measurements of Platelet Function. Edinburgh: Churchill Livingstone,
1983192-114.
7 Drummond AH, Gordon JL. Rapid, sensitive bioassay for
platelet 5-HT. Thromb Diath Haemorrh (Stuttgart)
1974;31:366-7.
8 Thompson JH, Spzia CA, Angulo M. Fluorimetric detection of
5-hydroxytryptamine using orthophthaldialdehyde: an improvement. Experientia 1970;26:327-9.
9 Winocour P, Kilmuik PS, Grennan A, Weinkove C. Platelet
serotonin levels in insulin dependent diabetes mellitus (IDDM)
and systemic sclerosis (SS). Clin Sci 1987;72:19-20P (abstr).
10 van Oost BA, Veldhuyzen BFE, van Houwelingen HC, Timmermans APM, Sixma JJ. Tests for platelet changes, acute phase
reactants and serum lipids in diabetes mellitus and peripheral
vascular disease. Thromb Haemost (Stuttgart) l982;48:
289-93.
11 Shuttleworth RD, OBrien JR. Intraplatelet and plasma
5-hydroxyindoles in health and disease. Blood 1981;57:505-9.
12 Bhargava KP, Raina N, Misra N, Shanker K, Vrat S. Uptake of
serotonin by human platelets and its relevance to CNS involvement in hypertension. Life Sci 1979;25:195-200.
13 Kamal LA, Le Quan-Bui KH, Meyer P. Decreased uptake of
3H-serotonin and endogenous content of serotonin in blood
platelets in hypertensive patients. Hypertension 1984;6:568-73.
14 Baudouin-Legros M, Le Quan-Bui KH, Gincheney P, Kamal
LA, Meyer P. Platelet serotonin in essential hyptertension and
mental depression. J Cardiovasc Pharmacol 1985;7(suppl
7):S12-4.
15 Pletscher A, Affolter H, Cesrua AM, Erne P, Muller P. Blood
platelets as models of neurones: similarities of the 5-hydroxy-
404
M. A. BARRADAS et al.
tryptamine system. In: Schlossberger HB, Kochen W, Lizen B,
Steinhart H, eds. Progress in Tryptophan and Serotonin
Research. Berlin: Walter de Gruyter, 1984:231-9.
16 Peacock I, Hawkins M, Heptinstall S. Platelet behaviour in noninsulin-dependent diabetes-influence of vascular complications, treatment and metabolic control. Thromb Haemostas
1986;55:361-5.
17 Cella G, Zahavi J, De Haas HA, Kakkar VV. b-thromboglobulin, platelet production time and platelet function in vascular
disease. Br J Haematol 1979;43:127-36.
18 Betteridge DJ, Zahavi J, Jones NAG, Shine B, Kakkar VV,
Galton DJ. Platelet function in diabetes mellitus in relationship
to complications, glycosylated haemoglobin and serum lipoproteins. Eur J Clin Invest 1981;11:273-7.
19 Mikhailidis DP, Barradas MA, Jeremy JY, Mohiuddin J,
Gracey L, Dandona P. Endogenous platelet thromboxane A2
production in diabetic patients with and without peripheral
vascular disease. Diabetologia l983;25:180-1 (abstr).
20 Zahavi J, Zahavi M. Enhanced platelet release, shortened
platelet survival time and increased platelet aggregation and
plasma thromboxane B2 in chronic obstructive arterial disease.
Thromb Haemost (Stuttgart) 1985;53:105-9.
21 Jones RJ, Delamothe AP, Curtis LD, Machin SJ, Betteridge DJ.
Measurement of platelet aggregation in diabetics using the new
electronic aggregometer. Diabete Med 1985;2: 105-9.
22 Ferguson JE, Mackay N, Phillip JAD, Summer DJ. Determination ofplatelet and fibrinogen half-life with (75 Se) selenomethionone studies in normal and diabetic subjects. Clin Sci Mol Med
1975;49:115-20.
23 Holmsen H. Platelet activation and serotonin. In: Vanhoutte
PM, ed. Serotonin and the Cardiovascular System. New York:
Raven Press, 1985:75-86.
24 Gill DS, Barradas MA, Fonseca VA, Gracey L, Dandona P.
Increased histamine content in leucocytes and platelets of
patients with peripheral vascular disease. Am J Clin Patholl988,
in press.
25 Fukami MH, Holmsen H, Ugorbil K. Histamine uptake in pig
platelets and isolated dense granules. Biochem Pharmacol
1984;33:3869-74.
26 Mezzano D, Aranda E, Foradori A. Comparative study of size,
total protein, fibrinogen and 5-HT content of human and canine
platelet density subpopulations. Thromb Haemost (Stuttgart)
1986;56:288-92.
27 Biondi ML, Agostini A, Marasini B. Serotonin levels in hypertension. J Hypertension 1986;4 (suppl 1):S39-41.
28 Van Houtte PM, Luscher TF. Serotonin and the blood vessel
wall. J Hypertension 1986;4 (suppl l):S29-35.
You might also like
- Chapter 29: Hematologic System Introduction Linton: Medical-Surgical Nursing, 7th EditionDocument5 pagesChapter 29: Hematologic System Introduction Linton: Medical-Surgical Nursing, 7th EditionStacey100% (1)
- NCP Risk For Bleeding Related To Decreased Platelet CountDocument2 pagesNCP Risk For Bleeding Related To Decreased Platelet CountKC Ignacio83% (24)
- Guidelines For The Rational Use of Blood Blood ProductsDocument120 pagesGuidelines For The Rational Use of Blood Blood ProductsHafiz Hamidi100% (1)
- Pathology of NoaDocument164 pagesPathology of NoaAnonymous milwFDXNo ratings yet
- High Risk of Coagulopathy Among Type-2 Diabetes Mellitus Clients at A Municipal Hospital in GhanaDocument7 pagesHigh Risk of Coagulopathy Among Type-2 Diabetes Mellitus Clients at A Municipal Hospital in GhanaLovi AnaNo ratings yet
- Thyroid Function and The Metabolic Syndrome in Older Persons: A Population-Based StudyDocument7 pagesThyroid Function and The Metabolic Syndrome in Older Persons: A Population-Based StudyAlifia RahmaNo ratings yet
- Cardiac Troponin T Is Not Increased in PatientsDocument5 pagesCardiac Troponin T Is Not Increased in PatientsAnanda Putri ImsezNo ratings yet
- HR 2008203Document6 pagesHR 200820322125327No ratings yet
- Jdpo 3 4 299 303Document5 pagesJdpo 3 4 299 303NAMPEWO ELIZABETHNo ratings yet
- 1 s2.0 0049384887903586 MainDocument8 pages1 s2.0 0049384887903586 Mainong251183No ratings yet
- PrintDocument8 pagesPrintannarchyNo ratings yet
- Biomedj 256 14R11Document15 pagesBiomedj 256 14R11Bassem RefaatNo ratings yet
- Admin Journal Manager 10 CebeciDocument9 pagesAdmin Journal Manager 10 CebeciBilal BilimNo ratings yet
- Epidemiology of Hypertension and Metabolic Disorders: 10.1016/j.ijcard.2011.08.581Document2 pagesEpidemiology of Hypertension and Metabolic Disorders: 10.1016/j.ijcard.2011.08.581Mirza RisqaNo ratings yet
- Rawalpindi Army Hosp HypothyDocument5 pagesRawalpindi Army Hosp Hypothyhinduja reddipilliNo ratings yet
- 1471 2261 5 7 PDFDocument10 pages1471 2261 5 7 PDFAfifah Raisa HalimNo ratings yet
- Turkish Journal Subclinical HypothyroidismDocument5 pagesTurkish Journal Subclinical HypothyroidismAminaNo ratings yet
- Paper Title: (16 Bold)Document9 pagesPaper Title: (16 Bold)vegeto portmanNo ratings yet
- Metabolic Cardiovascular Disease Risk Factors and Their Clustering in Subclinical HypothyroidismDocument7 pagesMetabolic Cardiovascular Disease Risk Factors and Their Clustering in Subclinical HypothyroidismMaria Alice BourneufNo ratings yet
- CometDocument9 pagesCometSohail AhmedNo ratings yet
- Accumulation of Cells With Short Telomeres Is Associated With Impaired Zinc Homeostasis and Infl Ammation in Old Hypertensive ParticipantsDocument7 pagesAccumulation of Cells With Short Telomeres Is Associated With Impaired Zinc Homeostasis and Infl Ammation in Old Hypertensive ParticipantsGabriela Elizabeth Delgado LeijaNo ratings yet
- Nejmoa1603825 PDFDocument11 pagesNejmoa1603825 PDFPsikiatri KlenderNo ratings yet
- Evaluation of Stress Hormones in Traumatic Brain Injury Patients With Gastrointestinal BleedingDocument7 pagesEvaluation of Stress Hormones in Traumatic Brain Injury Patients With Gastrointestinal BleedingIvonne SoelionoNo ratings yet
- Cholesterol Efflux Capacity, High-Density Lipoprotein Function, and AtherosclerosisDocument9 pagesCholesterol Efflux Capacity, High-Density Lipoprotein Function, and AtherosclerosisReza HariansyahNo ratings yet
- 2014 Monea Can Thyroid Dysfunction Induce Periodontal DiseaseDocument10 pages2014 Monea Can Thyroid Dysfunction Induce Periodontal DiseaseEm EryNo ratings yet
- Prehypertensive State, Mild Hypertension, Metabolic Syndrome and Cardiovascular Risk Factors Among Young Adults in Rural MalaysiaDocument8 pagesPrehypertensive State, Mild Hypertension, Metabolic Syndrome and Cardiovascular Risk Factors Among Young Adults in Rural MalaysiaIndah SundariNo ratings yet
- Homocysteine and Markers of Coagulation and Endothelial Cell ActivationDocument7 pagesHomocysteine and Markers of Coagulation and Endothelial Cell ActivationMaya RustamNo ratings yet
- Applied-A Correlative Study of Hypertension-Raksha GoyalDocument8 pagesApplied-A Correlative Study of Hypertension-Raksha GoyalImpact JournalsNo ratings yet
- Nutrition Parameters As Hemodialysis Adequacy Markers: Original ArticleDocument5 pagesNutrition Parameters As Hemodialysis Adequacy Markers: Original ArticleMariska Widya WNo ratings yet
- Association of Coagulation Profile With Microvascular Complications and Glycemic Control in Type 2 Diabetes Mellitus - A Study ADocument1 pageAssociation of Coagulation Profile With Microvascular Complications and Glycemic Control in Type 2 Diabetes Mellitus - A Study Aseneh17198No ratings yet
- Plasma Homocysteine and Total Thiol Content in Patients With Exudative Age-Related Macular DegenerationDocument5 pagesPlasma Homocysteine and Total Thiol Content in Patients With Exudative Age-Related Macular DegenerationAnonymous 1jCVqQuNo ratings yet
- Stratified Treatment of HypertensionDocument7 pagesStratified Treatment of HypertensionMohamad MuntahaNo ratings yet
- HOMA Medicion EJIM2003Document6 pagesHOMA Medicion EJIM2003Dr Dart05No ratings yet
- Relationship Between Serum Thyrotropin CDocument7 pagesRelationship Between Serum Thyrotropin Ciluhvina16No ratings yet
- Predictors of The Intracerebral Hemorrhage Volume in Hypertensive PatientsDocument5 pagesPredictors of The Intracerebral Hemorrhage Volume in Hypertensive PatientsNouchan NoupNo ratings yet
- Serum Ischemia Modified Albumin, Fibrinogen, HSCRP in DMT2 With and Without HypertensionDocument9 pagesSerum Ischemia Modified Albumin, Fibrinogen, HSCRP in DMT2 With and Without HypertensionMarcellia AngelinaNo ratings yet
- Mehran 2017Document9 pagesMehran 2017pelinNo ratings yet
- Oct1821 2Document10 pagesOct1821 2Jawaid AhmedNo ratings yet
- Jurnal Bu Sulis 1Document6 pagesJurnal Bu Sulis 1PitoAdhiNo ratings yet
- DR +Niket+Sonpal+-+Research+AbstractsDocument7 pagesDR +Niket+Sonpal+-+Research+AbstractsamiqtNo ratings yet
- Long-Term Follow-Up After Tight Control of Blood Pressure in Type 2 DiabetesDocument12 pagesLong-Term Follow-Up After Tight Control of Blood Pressure in Type 2 DiabetesnovywardanaNo ratings yet
- Serum Prolactin Levels in Psoriasis VulgarisDocument3 pagesSerum Prolactin Levels in Psoriasis VulgarispancholarpancholarNo ratings yet
- Thyroid Status and Death Risk in US Veterans WithDocument13 pagesThyroid Status and Death Risk in US Veterans WithrojorojilloNo ratings yet
- Dyslipidemia in-WPS OfficeDocument7 pagesDyslipidemia in-WPS OfficeMateNo ratings yet
- IOSR Journal of Pharmacy (IOSRPHR)Document6 pagesIOSR Journal of Pharmacy (IOSRPHR)IOSR Journal of PharmacyNo ratings yet
- #4 (Sofà A)Document6 pages#4 (Sofà A)Sofia OrduñoNo ratings yet
- Differences Between Human Plasma and Serum Metabolite ProfilesDocument6 pagesDifferences Between Human Plasma and Serum Metabolite ProfilesjoaquimmendesNo ratings yet
- Lipid Profile in CKDDocument4 pagesLipid Profile in CKDAmiyanshu BeheraNo ratings yet
- Primary Hyperparathyroidism Detected in A Health Screening: The Tromsø StudyDocument6 pagesPrimary Hyperparathyroidism Detected in A Health Screening: The Tromsø StudyMisaeldpdNo ratings yet
- Chan Et Al (2000)Document6 pagesChan Et Al (2000)badrishNo ratings yet
- Proton-Pump Inhibitors Therapy and Blood Pressure ControlDocument6 pagesProton-Pump Inhibitors Therapy and Blood Pressure ControlTeky WidyariniNo ratings yet
- 0120 2448 Amc 44 03 8Document8 pages0120 2448 Amc 44 03 8Lejla HusicNo ratings yet
- Review Article: Animal Models of Hypertension: An OverviewDocument14 pagesReview Article: Animal Models of Hypertension: An OverviewrodrigodaliascienceNo ratings yet
- 7decaf9c Cb18 4623 Bced Ecef2197e451Document25 pages7decaf9c Cb18 4623 Bced Ecef2197e451PrabhuNo ratings yet
- Paper Title: (16 Bold Blue Color)Document9 pagesPaper Title: (16 Bold Blue Color)Fauzi RusdiantoNo ratings yet
- Quandt 2018Document9 pagesQuandt 2018Andres Vásquez ChNo ratings yet
- Hofmaenner - Association Between Hypocholesterolemia and Mortality in Critically Ill Patients With Sepsis - A Systematic Review and Meta-AnalysisDocument10 pagesHofmaenner - Association Between Hypocholesterolemia and Mortality in Critically Ill Patients With Sepsis - A Systematic Review and Meta-AnalysisgiadungdanamallNo ratings yet
- Atherogenic Dyslipidemia in Patients With Established Coronary Artery DiseaseDocument6 pagesAtherogenic Dyslipidemia in Patients With Established Coronary Artery DiseasebilahalvirayuNo ratings yet
- Accepted Manuscript: 10.1016/j.rvsc.2017.04.004Document39 pagesAccepted Manuscript: 10.1016/j.rvsc.2017.04.004Omary2jNo ratings yet
- Association of Dyslipidemia and Ischemic Stroke in Pakistan Institute of Medical SciencesDocument3 pagesAssociation of Dyslipidemia and Ischemic Stroke in Pakistan Institute of Medical SciencesvenniariskiaNo ratings yet
- Antioxidant Effects of Zinc Supplementation in Tunisians With Type 2 Diabetes MellitusDocument6 pagesAntioxidant Effects of Zinc Supplementation in Tunisians With Type 2 Diabetes MellitusgautomsahariaNo ratings yet
- Arterioscler Thromb Vasc Biol 2002 Von Bahr 1129 35Document7 pagesArterioscler Thromb Vasc Biol 2002 Von Bahr 1129 35widyaanggariniNo ratings yet
- Enmet DMDocument7 pagesEnmet DMAreef MuarifNo ratings yet
- Complementary and Alternative Medical Lab Testing Part 3: CardiologyFrom EverandComplementary and Alternative Medical Lab Testing Part 3: CardiologyRating: 1 out of 5 stars1/5 (1)
- Practical Hematology Manual #1Document48 pagesPractical Hematology Manual #1Michelle P100% (2)
- Atherosclerosis PathophysiologyDocument11 pagesAtherosclerosis PathophysiologyCandice ChengNo ratings yet
- Sysmex SEED 4 2013 Automated Haematology Sample Interferences Flagging and Results Interpretation - Part 1 enDocument8 pagesSysmex SEED 4 2013 Automated Haematology Sample Interferences Flagging and Results Interpretation - Part 1 enPieter Du Toit-Enslin50% (2)
- Monocyte: FunctionDocument9 pagesMonocyte: FunctionMatelyn OargaNo ratings yet
- Blood Composition PowerpointDocument40 pagesBlood Composition PowerpointJeremy Wallace100% (3)
- Extracorporeal Circulation in Cardiac Surgery Inflmmatory Response, Controversies and Future DirectionsDocument13 pagesExtracorporeal Circulation in Cardiac Surgery Inflmmatory Response, Controversies and Future DirectionsInternational Medical PublisherNo ratings yet
- Chart Transfused Blood ProductsDocument2 pagesChart Transfused Blood ProductsAORN2008No ratings yet
- Benzimidazole - A Medicinally Important Heterocyclic MoietyDocument15 pagesBenzimidazole - A Medicinally Important Heterocyclic MoietyKeyvanNo ratings yet
- 1 - Introduction To HematologyDocument38 pages1 - Introduction To HematologyMelanie Tran100% (1)
- Ascp StudyDocument18 pagesAscp StudyJamaica EstorninosNo ratings yet
- Thrombocytopenia: Pathophysiology and ClassificationDocument4 pagesThrombocytopenia: Pathophysiology and Classificationvenni dimitriNo ratings yet
- v25 n8Document482 pagesv25 n8Anonymous NR7pnLbNo ratings yet
- Lecture 2 MLTDocument24 pagesLecture 2 MLTAbood dot netNo ratings yet
- PathologyDocument48 pagesPathologyAjay DivvelaNo ratings yet
- 1996 Human Biomaterials Applications PDFDocument453 pages1996 Human Biomaterials Applications PDFNataliaNo ratings yet
- Blood Clinical CorellaionsDocument12 pagesBlood Clinical Corellaionssinte beyuNo ratings yet
- Blood Transfusion - Marino - The Icu BookDocument3 pagesBlood Transfusion - Marino - The Icu BookWilliam OmarNo ratings yet
- Hemodynamic Disorders: BY Dr. Birhane H (MD)Document88 pagesHemodynamic Disorders: BY Dr. Birhane H (MD)Biruck BirhanuNo ratings yet
- Bloodhana 2019 PDFDocument41 pagesBloodhana 2019 PDFAngelica Parreñas BayonaNo ratings yet
- Low Platelet Count - Causes and Top 10 Natural Remedies PDFDocument6 pagesLow Platelet Count - Causes and Top 10 Natural Remedies PDFMaria Eduarda VianaNo ratings yet
- MABB Presentation 5 24 2022Document39 pagesMABB Presentation 5 24 2022Ayman MehassebNo ratings yet
- Forensic ScienceDocument5 pagesForensic ScienceSarthak ShankarNo ratings yet
- Cardiovascular Disease and Diabetes: The Vulnerable Patient: Katharina Hess, Nikolaus Marx, and Michael LehrkeDocument10 pagesCardiovascular Disease and Diabetes: The Vulnerable Patient: Katharina Hess, Nikolaus Marx, and Michael Lehrkekrungi21No ratings yet
- Microsurgery Selected Readings Plastic SurgeryDocument63 pagesMicrosurgery Selected Readings Plastic Surgeryhaytham almalahyNo ratings yet
- Acute Infectious Purpura FulminansDocument15 pagesAcute Infectious Purpura FulminansFranklin Aranda100% (2)
- Merck Veterinary ManualDocument264 pagesMerck Veterinary Manualschmooshie91% (11)