Professional Documents
Culture Documents
Classic Signs Revisited: The Babinski Reflex
Classic Signs Revisited: The Babinski Reflex
Uploaded by
David AvetisyanOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Classic Signs Revisited: The Babinski Reflex
Classic Signs Revisited: The Babinski Reflex
Uploaded by
David AvetisyanCopyright:
Available Formats
Postgrad MedJ3 1995; 71: 645-648 C The Fellowship of Postgraduate Medicine, 1995
Classic signs revisited
The Babinski reflex
J van Gijn
Summary
The plantar response is a reflex
that involves not only the toes, but
all muscles that shorten the leg. In
the newborn the synergy is brisk,
involving all flexor muscles of the
leg; these include the toe 'extensors', which also shorten the leg
on contraction and therefore are
flexors in a physiological sense. As
the nervous system matures and
the pyramidal tract gains more
control over spinal motoneurones
the flexion synergy becomes less
brisk, and the toe 'extensors' are
no longer part of it. The toes then
often go down instead of up, as a
result of a segmental reflex involving the small foot muscles and
the overlying skin, comparable to
the abdominal reflexes. With
lesions of the pyramidal system,
structural or functional, this
segmental, downward response of
the toes disappears, the flexion
synergy may become disinhibited
and the extensor hallucis longus
muscle is again recruited into the
flexion reflex of the leg: the sign of
Babinski.
A true Babinski sign denotes
dysfunction of the pyramidal
tract, and should be clearly distinguished from upgoing toes that
do not belong to the flexion
synergy of the leg. Correct interpretation of the plantar response
depends only to a minor degree on
the method or site of stimulation
of the foot. It is therefore most
important to assess the response
in the entire leg.
Keywords: Babinski reflex
University Department of Neurology,
Academisch Ziekenhuis, PO Box 85500,
3508 GA Utrecht, The Netherlands
J van Gijn
Accepted 28 June 1995
The information that may be deduced from scratching a patient's sole, is as
important as a diagnostic sign as it is simple to elicit. When the great toe moves
upward (sign of Babinski), this signifies, as everybody knows, a disturbance of
the pyramidal tract. This explains why few patients with neurological symptoms
can avoid having their plantar reflexes examined - often to their great surprise, or
even alarm if the trouble is in the head. Unfortunately the reality is less simple
than the theory. Often it is difficult to decide whether the great toe actually does
go up: the toe movements may be slight, vacillate between up and down, seem
down one day but up the next, or be interrupted by voluntary withdrawal
movements. It is therefore no great surprise that such difficult plantar responses
give rise to wide variations between doctors, or even between different occasions
with the same observer. Under these circumstances the interpretation may be
influenced by the physician's previous expectations.' Since it is obviously
important for the diagnosis in individual patients whether or not a lesion of the
pyramidal system exists, there is a need for criteria that are both reliable and
simple. The guidelines that follow have not only been validated in practice,2'3 but
are also founded on physiological principles.
Physiology
The quintessence is that the plantar reflex entails more movements than just
those of the toes. In most mammals the limbs are automatically retracted on
painful stimulation, a defensive reflex subserved by polysynaptic pathways in the
spinal cord. The reaction is more pronounced in hind limbs, because the
forelimbs are under more direct control of the brain. The reflex is stronger as the
stimulus is more distal. Not only the skin but also deeper structures contain
receptors that may release this movement. Around the turn of the century
Sherrington extensively analyzed this phenomenon in animals; he called it the
flexion reflex, because the effect consisted of the activation of all muscles that
shortened the limb (physiological flexors). Somewhat surprisingly, the toe
extensors form part ofthis shortening synergy: the (anatomical) toe extensors are
flexor muscles in a physiological sense, and vice versa.
The reflex effects in the human leg on stimulation of the sole are completely
analogous to those in animals. This is especially clear in neonates, provided the
plantar surgace is not stimulated too gently, in which case a grasp reflex occurs.4
In the neonate there are two differences with respect to the normal adult: the
entire flexion synergy is much more brisk and, more important, the toes are part
of the synergy: they go up at the same time that flexion occurs in the ankle, knee
and hip. Again, for the anatomist these are extensory movements of the toes, for
the physiologist, flexor movements. That the movement is greatest in the great
toe results from the structure of the metacarpo-phalangeal joints; the little toes
simply cannot move up that far.
As the pyramidal system matures and gains more control over spinal
motoneurones the flexion reflex changes in two respects. The first and more
important change is that after one or two years the toes are no longer part of the
flexion synergy. The second is that the entire flexion reflex becomes less brisk; in
most adults all that is left of the composite movements is a subtle contraction of
the proximal muscles, particularly of the musculus tensor fasciae latae, under the
skin of the later part of the thigh. In some adults the remaining part of the flexion
reflex stays brisk or, conversely, disappears; only asymmetry is truly
pathological, as is the case with muscle stretch reflexes. Not only do the toes of
older children and adults no longer go up on stimulation of the sole, in most cases
the movement is replaced by an opposite, downward displacement. This reflex is
mediated by the short toe flexors (anatomical term) of the sole, and has nothing to
do with flexion synergy; it is a purely cutaneous reflex, related to a single segment
of the spinal cord. The downward movement may predominate in the great toe or
the smaller toes, depending on whether the medial or the lateral part of the sole is
stimulated. Absence of the downward toe response is not pathological unless
there is a marked difference between the two sides.
646
van Gijn
The flexion reflex
* on stimulation of distal skin, or
deeper structures
* shortening of lower limb in hip,
knee, ankle and toes
* toe 'extensors' are flexors in a
physiological sense
Role of the pyramidal tract
* decreases entire flexion synergy
* inhibits participation of toe
'extensors'
* dysfunction of pyramidal tract
restores 'neonatal' situation
Lesions of the pyramidal system
The function of the pyramidal tract may not only be distrubed by structural
lesions - of myeline sheaths, axons, or both - but also by metabolic factors, for
example, hypoglycaemia or an epileptic seizure. In these cases the flexion reflex
may become brisker, by disinhibition. The sign of Babinski emerges when the
dysfunction involves those pyramidal fibres that project upon motoneurones of
foot muscles; the great toe may again be recruited into the flexion synergy in the
leg. In these cases there is almost always some degree of motor deficit in the foot often in the form of weakness, but sometimes evident only from a decreased
ability to perform rapid foot movements (eg, when the patient is asked to tap
rapidly against the bottom of the bed or the examiner's hand).5
Not all disturbances of the pyramidal system are associated with a Babinski
sign, even in cases where the descending fibres to the foot muscles are clearly
involved. The explanation for the lack of a Babinski reflex should be sought in a
dysfunction of the segmental reflex pathways, the simplest being a pressure palsy
of the peroneal nerve. In other cases there is temporary inexcitability of spinal
motoneurones, most often by a transverse lesion of the cord ('spinal shock'), but
sometimes after acute brain lesions.5 Then it is not only the up-going toe sign that
is lacking, but the entire flexion synergy of the leg.
The muscle responsible for the up-going toe sign is located in the leg: the
musculus extensor hallucis longus.6 This has practical implications. It is also of
great practical importance that an up-going toe sign rarely occurs without
accompanying reflex activity in more proximal flexor muscles ofthe leg. Babinski
himself emphasized from the outset the intimate relationship between his sign
and the shortening movements in other leg muscles. Yet subsequently, many had
eyes for the toes alone, and so got into trouble.
Positioning and stimulation
To start with, all leg muscles should be visible and in a relaxed state. This implies
that the entire leg should be uncovered (removing socks is not enough), and that
the patient should be supine, on a couch or in a bed (hoisting up the leg of a seated
patient is asking for trouble). The patient should be warned that the sole is going
to be scratched, and that it is important that the limbs remain as floppy as possible
(use of the term 'relax' is almost invariably followed by the very muscle
contractions one wishes to avoid).
It is the site of stimulation, the intensity of stimulation, and even the object
used for stimulation (from inverted patella hammer to shark's tooth or Bentley
key) that has received by far the most attention in relation to difficulties in
interpreting the plantar response. Any instrument will do provided it is not too
sharp and has not been used on other patients. My own favourite instrument is
the end of a thin wooden stick, of the type that may have a piece of cotton wool at
the other end. Any part of the leg can be stimulated, but the chance of producing
an up-going toe response in the presence of pyramidal tract dysfunction is
greatest if the lateral plantar border is chosen, rather than the medial side, which
overlies the flexor hallucis brevis muscle. Stimulation at that site is therefore
more likely to make the toe go down. Ideally the stimulus should continue along
the lateral border of the sole, and should be rather slow.7 On the other hand,
repeated interference by voluntary movements the patient is unable to suppress
may make it desirable to use a shorter stimulus, or a stimulus at a different site.
Stroking the lateral dorsum of the foot (figure 1) is often helpful in such cases,
and may even be more effective in producing a Babinski sign. This is also because
irritation of the sole can give rise to voluntary clawing of the toes.
Interpretation of the plantar response
The following three rules governing the relationship between the Babinski sign
and the flexion synergy were determined in a study of patients with equivocal
plantar respones in whom clinical and electromyographic features were
compared.2
Upward movement of the great toe is pathological only if caused by contraction of the
extensor hallucis longus muscle
In most patients tightening of the tendon can be seen or at least felt, on the
dorsum of the great toe and the foot (figure 1). The hallux may move upwards
without contraction of the extensor hallucis longus muscle on dorsiflexion of the
foot as a whole, a movement that often occurs as part of the flexion reflex and
which is not pathological in itself.6 In addition, the great toe may go up merely
after having flexed, and a brisk flexion synergy of the leg may conceal this initial
The Babinski reflex
647
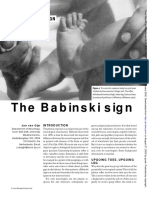
Figure 1 Babinski sign (in this case evoked
by stroking the lateral part of the dorsum
rather than of the sole, in order to avoid
voluntary withdrawal by ticklishness). Note
the protrusion of the tendon of the extensor
longus muscle on the dorsum of the great toe
and the foot
Is an up-going toe a Babinski sign?
* watch the tendon of the musculus
extensor hallucis longus
* if the muscle does contract, other
flexor muscles should do as well
* if the toe goes up once with the
flexor synergy, it should do so again
movement. Finally, an illusion of the big toe going up may be created if the other
toes go gently down, the big toe being actually immobile.
Contraction of the extensor hallucis longus muscle is pathological only if it occurs
synchronously with reflex activity in other flexor muscles
The flexion synergy may be weak in some subjects, but as contraction of the
tensor fasciae and hamstring muscles constitutes the minimal response,8
tightening of these muscles occurs at the same time as a true Babinski response.
Whenever one examines the plantar response it is extremely important to look
not only at the toe itself but also at the outer thigh and at the tendons of the
hamstring muscles, as a reference for what is part of the flexion synergy and what
is not (figure 2). Sometimes it may seem that the up-going toe is the minimal
response of the flexion reflex, but one should keep in mind that the big toe is
lighter than the foot, leg or thigh, and palpation of the hamstring tendons may
uncover small degrees of contraction that were not readily visible.8 In most cases,
however, the flexion synergy will lead to some displacement of the leg, and the
examiner can not only see but also feel this with the hand that supports the foot
while the other hand stimulates it.
A true up-going toe sign is reproducible, unlike voluntary withdrawal of the toes
To avoid (more or less) voluntary reactions in patients with ticklish feet, the first
useful measure is to tell the patient what is going to happen. Furthermore, one
should adapt the stimulus as much as possible to what the patient can tolerate.
Little is gained by faithfully completing a textbook manoeuvre while the patient
is writhing on the couch. In such cases it often helps to stroke the lateral dorsum
of the foot rather than the lateral sole (figure 1). One cannot see the normal
downard response of the big toe, but the main purpose of the test is to see whether
or not there is a Babinski sign. If stroking the full length of the dorsum is still too
much for the patient, repeating stroking of only a few centimetres of skin will, in
the case of flexion reflex, produce an approximately similar fraction of the
synergy each time, whereas volumtary retraction will be abolished, or inconstant.
Fatigue of the Babinski sign is extremely uncommon. Finally, voluntary
withdrawal does not involve the tensor fasciae latae, and may preceed or outlast
the stimulus.
Myths dispelled
The Babinski sign is so venerable that it has become the subject ofidees res'ues that
are, on closer scrutiny unfounded.
'The stimulus should be painful.' This is incorrect, as the necessary intensity
depends on the degree of disinhibition of the flexion reflex. In some patients a
mere touch anywhere on the leg is sufficient for releasing a brisk withdrawal of
the entire leg, including the up-going toe sign.
648
van
Gijn
Figure 2 Babinski sign. Contraction of the
extensor hallucis longus muscle occurs simultaneously with contraction of other muscles
that shorten the leg: the tibialis anterior
(tendon lateral to the tibial ridge), the knee
flexors or hamstring muscles (tendons at the
back of the knee), and the M tensor fasciae
latae (subcutaneous in the lateral thigh;
arrow). Reproduced from the Nederlands
Tijdschrift voor Geneeskunde, with permission9
0~-
Dispelled myths
* stimulates need not be painful
* different sites of stimulation: same
flexion reflex
* eponyms serve only to torture
students
* first toe movement may or may not
be the response that counts
* Babinski sign may be slow or fast
* fanning of the toes is not a
prerequisite
'In doubtful cases one should apply variants of the Babinski sign.' Indeed the
up-going toe sign can be elicited from many different sites at the foot or even the
leg, but the physician (or student!) should not be deterred by the variety of
eponyms. Wherever one scratches or pinches, any ensuing response of the toes is
part and parcel of the flexion synergy of the lower limb. Any stimulus is
legitimate as long as it is not applied more distally than the ball of the foot, as this
may produce false-positive results.
'The movement should occur at the metatarsophalangeal joint.' The rationale of this
criterion is to exclude passive upward movements of the great toe, merely by
dorsiflexion of the foot. But a more sensitive method than inspecting the joint is
to concentrate on the tendon of the extensor hallucis longus muscle (figure 1),
from which the movement originates. This tendon has its insertion at the
terminal phalanx; it may tighten even without any visible displacement of the toe.
'The movement should be the first'. It is difficult to see why a patient cannot make a
voluntary movement before the onset of reflex action. Sometimes a trace of a
downward response precedes the recruitment of the great toe into the flexion
reflex synergy.
'The movement should be slow'. This view is echoed by many textbooks. But what
is the definition of slowness? Moreover, reports abound of brisk reflexes and
Babinski signs.
'In doubtful cases the 'fan sign' is a useful measure'. Fanning of the toes is of
historical interest only. Babinski described this sign a few years after his
discovery of the up-going toe sign, but he added that it may also occur in normal
subjects. It may cause errors not only of observation but also of interpretation if
more attention is paid to this phenomenon that it deserves.
In conclusion, the real question in interpreting the plantar response is not
whether the great toe goes up or not, but whether an up-going toe is a
pathological response. For an appropriate answer the method of watching is
much more important than the method of scratching.
1 Van Gijn J, Bonke B. Interpretation of plantar
reflexes: biasing effects of other signs and symptoms. J Neurol Neurosurg Psychiatry 1977; 40:
787-9.
2 Van Gijn J. Equivocal plantar responses: a
clinical and electromyographic study. J Neurol
Neurosurg Psychiatry 1976; 39: 275-82.
3 Raijmakers PGHM, Castro Cabezas M, Smal
JA, Van Gijn J. Teaching the plantar reflex. Clin
Neurol Neurosurg 1991; 93: 201-4.
4 Dietrich HF. A longitudinal study of the Babinski and plantar grasp reflexes in infancy. Am J
Dis Child 1957; 94: 265-71.
5 Van Gijn J. The Babinski sign and the pyramidal
syndrome. J Neurol Neurosurg Psychiatry 1978;
41: 865-73.
6 Van Gijn J. Babinski response: stimulus and
effector.J Neurol Neurosurg Psychiatry 1975; 38:
180-6.
7 Dohrmann GJ, Nowack WJ. The upgoing great
toe - optimal method of elicitation. Lancet 1973;
i: 339-41.
8 Walshe FMR. The physiological significance of
the reflex phenomena in spastic paralysis of the
lower limbs. Brain 1914; 37: 269-336.
9 Van Gijn J, van Crevel H, De voetzoolreflex.
Ned Tijdschr Geneeskd 1978; 122: 1299-302.
You might also like
- Ford Transit 2006.5 04.2006 Workshop Manual ( (04.2006-) )Document834 pagesFord Transit 2006.5 04.2006 Workshop Manual ( (04.2006-) )slawek100% (2)
- Geology of Johannesburg ReadingDocument2 pagesGeology of Johannesburg ReadingKavish DayaNo ratings yet
- Alexander Verl, Alin Albu-Schaffer, Oliver Brock, Annika Raatz (Eds.) - Soft Robotics Transferring Theory To Application-Springer (2015) PDFDocument293 pagesAlexander Verl, Alin Albu-Schaffer, Oliver Brock, Annika Raatz (Eds.) - Soft Robotics Transferring Theory To Application-Springer (2015) PDFSergio Castillo SanchoNo ratings yet
- Middle East Chemical Market: Trends and Opportunities (2015-2019) - New Report by Daedal ResearchDocument16 pagesMiddle East Chemical Market: Trends and Opportunities (2015-2019) - New Report by Daedal ResearchDaedal ResearchNo ratings yet
- Pathologic Reflexes & FisiologisDocument9 pagesPathologic Reflexes & FisiologiswadejackNo ratings yet
- Plantar ReflexDocument5 pagesPlantar ReflexrazakmdpaedNo ratings yet
- Equinus ContracturesDocument7 pagesEquinus Contracturesa013bsy2496No ratings yet
- Working With Ankle Mobility, Part I (Myofascial Techniques)Document5 pagesWorking With Ankle Mobility, Part I (Myofascial Techniques)Advanced-Trainings.com100% (4)
- BabinskilDocument3 pagesBabinskilImounan FatimaNo ratings yet
- Cerebral Palsy: and Its Sequelae.. (Consequences)Document143 pagesCerebral Palsy: and Its Sequelae.. (Consequences)Agus SarjonoNo ratings yet
- Healing by Direct Union (Primary Bone Healing)Document6 pagesHealing by Direct Union (Primary Bone Healing)Cakradenta YPNo ratings yet
- Plantar ReflexDocument19 pagesPlantar Reflexfidaafsal99No ratings yet
- SpondylolisthesisDocument9 pagesSpondylolisthesiswangNo ratings yet
- Congenital AbnormalitiesDocument37 pagesCongenital AbnormalitiesrezkadehaNo ratings yet
- Gait AssessmentDocument4 pagesGait Assessmentvijay1234568883No ratings yet
- Anatomy AnglesDocument27 pagesAnatomy AnglesKiko KikoNo ratings yet
- Diagnosis and Management of The Painful Ankle Foot Part 1Document25 pagesDiagnosis and Management of The Painful Ankle Foot Part 1Kamila PeñaililloNo ratings yet
- International Journalof Pediatricsand Neonatology Planter ReflexDocument4 pagesInternational Journalof Pediatricsand Neonatology Planter ReflexUmesh BabuNo ratings yet
- NervetibialDocument6 pagesNervetibialandres felipe delgadoNo ratings yet
- President's Address: Trick MovementsDocument3 pagesPresident's Address: Trick MovementsDr. Rushikesh K. Joshi100% (1)
- Pandi Culat I OnDocument7 pagesPandi Culat I OnOscar RamirezNo ratings yet
- Doug Keller - Pelvic Balance Slides - Part TwoDocument41 pagesDoug Keller - Pelvic Balance Slides - Part Twoshivnair100% (8)
- GALS Screen: G Gait A Arms L Legs S SpineDocument6 pagesGALS Screen: G Gait A Arms L Legs S SpineJoseph FreerNo ratings yet
- The Javelin Throwers ShoulderDocument11 pagesThe Javelin Throwers ShoulderJoão Pedro Adegas CarvalhoNo ratings yet
- 02 Padure, L. Spastic Hip in Cerebral PalsyDocument4 pages02 Padure, L. Spastic Hip in Cerebral PalsyminichoixNo ratings yet
- Ankle&fEET Written Procedure-MagsombolDocument2 pagesAnkle&fEET Written Procedure-Magsombolhazell_aseronNo ratings yet
- Gait AnalysisDocument49 pagesGait AnalysisKrishna KumariNo ratings yet
- A Comprehensive Treatment Guide For Frozen ShoulderDocument15 pagesA Comprehensive Treatment Guide For Frozen ShoulderHoan TrầnNo ratings yet
- Joint Instability: Hendradi Khumarga SPOT. FICSDocument48 pagesJoint Instability: Hendradi Khumarga SPOT. FICSJoshua ObrienNo ratings yet
- Neonatal HypotoniaDocument7 pagesNeonatal HypotoniaShirley KoehNo ratings yet
- Peranan Fisioterapi Pada Kasus Hallux Valgus (Bunion) Dengan Intervensi NMT Dan Strengthening Untuk Mengurangi NyeriDocument7 pagesPeranan Fisioterapi Pada Kasus Hallux Valgus (Bunion) Dengan Intervensi NMT Dan Strengthening Untuk Mengurangi NyeriShalmaa LarasatiNo ratings yet
- Papers - Tibial PosteriorDocument10 pagesPapers - Tibial PosteriorGiancarlo Gardella MartínezNo ratings yet
- Anomalies of Skeletal System-1Document44 pagesAnomalies of Skeletal System-1Meena Koushal100% (1)
- Coxa SaltansDocument6 pagesCoxa SaltansignashyaNo ratings yet
- Gastrocnemius SoleusDocument8 pagesGastrocnemius SoleusgoldfishxNo ratings yet
- LUMBAR DISC NotesDocument7 pagesLUMBAR DISC NotesPrasadNo ratings yet
- Plantar ReflexDocument3 pagesPlantar Reflexhalu89No ratings yet
- Bow Leg (Final) 3.9.20Document23 pagesBow Leg (Final) 3.9.20Gerald EthelieNo ratings yet
- Excessive Genu Valgum FINALDocument13 pagesExcessive Genu Valgum FINALMeeraNo ratings yet
- Organ System Muscular Skeletal SystemsDocument7 pagesOrgan System Muscular Skeletal SystemsJehannaMarEnggingAbdurahmanNo ratings yet
- Motor SystemDocument8 pagesMotor SystemEman LabNo ratings yet
- CHAPTER 4 BiomechanicsDocument20 pagesCHAPTER 4 BiomechanicsAaliyaan KhanNo ratings yet
- Health Assess - CH 22 Key TermsDocument2 pagesHealth Assess - CH 22 Key TermsAllison Doubek GibsonNo ratings yet
- Improving Ankle and Knee Joint Stability: Proprioceptive Balancefit Discs DrillsFrom EverandImproving Ankle and Knee Joint Stability: Proprioceptive Balancefit Discs DrillsNo ratings yet
- Posture EvaluationDocument12 pagesPosture EvaluationpaconscribdNo ratings yet
- Flat Foot SurgeryDocument5 pagesFlat Foot SurgeryManoj KandoiNo ratings yet
- Congenital Hips DislocationDocument6 pagesCongenital Hips DislocationMar OrdanzaNo ratings yet
- Short Right Leg 1Document4 pagesShort Right Leg 1Simo AsterNo ratings yet
- (NS) Spinal Cord InjuryDocument2 pages(NS) Spinal Cord Injuryapi-3769252No ratings yet
- Congenital Talipes Equinovarus 222Document10 pagesCongenital Talipes Equinovarus 222jjjj30No ratings yet
- Shoulder Application SolutionsDocument3 pagesShoulder Application SolutionsDNo ratings yet
- Lower Limb Neurological Examination OSCE GuideDocument15 pagesLower Limb Neurological Examination OSCE GuideLeen abusarhanNo ratings yet
- Pes Planus - Synopsis of CausationDocument14 pagesPes Planus - Synopsis of CausationSari HestiyariniNo ratings yet
- Ankle and FootDocument31 pagesAnkle and FootmetoNo ratings yet
- Hip Dislocation in Dogs and Cats (Wendy Brooks, DVM)Document8 pagesHip Dislocation in Dogs and Cats (Wendy Brooks, DVM)Muhammad KholifhNo ratings yet
- Safari - Feb 21, 2024 at 11:44 AM 2Document1 pageSafari - Feb 21, 2024 at 11:44 AM 2syansyncNo ratings yet
- Ankle Sprain TreatmentDocument5 pagesAnkle Sprain TreatmentTushar GajjarNo ratings yet
- Neurological History and ExaminationDocument30 pagesNeurological History and ExaminationMaria Agatha100% (1)
- Babinski & Parachute Reflex PPT Group 3 Bsn2aDocument23 pagesBabinski & Parachute Reflex PPT Group 3 Bsn2aPaula AbadNo ratings yet
- VSAQS Imp - Biom.Document8 pagesVSAQS Imp - Biom.Meenakshiputraeashwarprasad MacherlaNo ratings yet
- SpondylolysisDocument13 pagesSpondylolysisYang100% (1)
- Drop Claw FootDocument3 pagesDrop Claw FootfmtaNo ratings yet
- NN LBPDocument50 pagesNN LBPEdmonLagartoNo ratings yet
- Healthy Hips Handbook: Exercises for Treating and Preventing Common Hip Joint InjuriesFrom EverandHealthy Hips Handbook: Exercises for Treating and Preventing Common Hip Joint InjuriesNo ratings yet
- ASMi 54CDocument8 pagesASMi 54Cs_meherNo ratings yet
- SUSTECH MathDocument24 pagesSUSTECH Matht0xic.369xNo ratings yet
- Digital VocabDocument2 pagesDigital Vocabdesikudi9000No ratings yet
- A New Classification Scheme For Periodontal and Peri and Conditions - Introduction and Key Changes From The 1999 ClassificationDocument8 pagesA New Classification Scheme For Periodontal and Peri and Conditions - Introduction and Key Changes From The 1999 ClassificationOner Man0% (1)
- Silane BrochureDocument12 pagesSilane Brochurehakanaltiparmak88No ratings yet
- Neural Networks ExamDocument3 pagesNeural Networks Examfruit1991No ratings yet
- HarvestlandDocument687 pagesHarvestlandJanetNo ratings yet
- CvACC ProceduresDocument21 pagesCvACC ProceduresAnonymous sWlFP3gFNo ratings yet
- Plum Concrete WallsDocument4 pagesPlum Concrete WallsnileshNo ratings yet
- SelectaDocument55 pagesSelectaHuong Cam ThuyNo ratings yet
- Motivation Letter University of Barcelona PDFDocument2 pagesMotivation Letter University of Barcelona PDFPatricia PuertoNo ratings yet
- DC DC: Table 5.13: Overhead Line Conductor - Hard Drawn CopperDocument8 pagesDC DC: Table 5.13: Overhead Line Conductor - Hard Drawn CopperVino VinoNo ratings yet
- Introductory Botulinum PresentationDocument113 pagesIntroductory Botulinum Presentationprontaprintpottersbar100% (5)
- CSB02 CSE02 CSH02 CDB02 Project Planning R911338962 - 03Document146 pagesCSB02 CSE02 CSH02 CDB02 Project Planning R911338962 - 03DylanNo ratings yet
- NFA 2010 ResultsDocument4 pagesNFA 2010 ResultsAnto AbatilliNo ratings yet
- BehaviouralismDocument4 pagesBehaviouralismZoya FazarNo ratings yet
- Cognitive Approaches To TranslationDocument10 pagesCognitive Approaches To TranslationKhali74No ratings yet
- DR Bach Flower Remedies 03-02-2017Document70 pagesDR Bach Flower Remedies 03-02-2017sadam ameerjohnNo ratings yet
- English 4 3rd Quarter ExamDocument2 pagesEnglish 4 3rd Quarter ExamRodel Corpuz MagbanuaNo ratings yet
- 4 - Liber XIII - Graduum Montis AbiegniDocument10 pages4 - Liber XIII - Graduum Montis AbiegniMts JlnNo ratings yet
- Neptune in Pisces - Quietly Working To Destroy FearDocument3 pagesNeptune in Pisces - Quietly Working To Destroy FearReiki MasterNo ratings yet
- 02nd To 04th December 2023 International Cotton Advisory Committee - 81st Plenary Meeting 2023Document11 pages02nd To 04th December 2023 International Cotton Advisory Committee - 81st Plenary Meeting 2023sabirNo ratings yet
- Mpman High-Tech Mini Electric Scooter User Manual Model: TR800Document18 pagesMpman High-Tech Mini Electric Scooter User Manual Model: TR800ChrisNo ratings yet
- Food Microbiology Laboratory For The Food Science Student: Cangliang Shen Yifan ZhangDocument164 pagesFood Microbiology Laboratory For The Food Science Student: Cangliang Shen Yifan ZhangQonita RachmahNo ratings yet
- DME Model QuesDocument3 pagesDME Model QuesSiva RamanNo ratings yet
- Global Problem AMR-NAP - EATDocument32 pagesGlobal Problem AMR-NAP - EATWolfy D Harold100% (1)