Professional Documents
Culture Documents
Smell and Taste Dysfunction Following Minor Stroke: A Case Report
Smell and Taste Dysfunction Following Minor Stroke: A Case Report
Uploaded by
Prasaundra TriantoniOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Smell and Taste Dysfunction Following Minor Stroke: A Case Report
Smell and Taste Dysfunction Following Minor Stroke: A Case Report
Uploaded by
Prasaundra TriantoniCopyright:
Available Formats
Smell and taste dysfunction
following minor stroke: A case report
By Theresa L. Green, Lisa D. McGregor and Kathryn M. King
Abstract
Smell (olfactory) and taste (gustatory) are key senses in the regulation of nourishment and individual safety. Olfactory and gustatory dysfunctions have been infrequently reported together in
patients following stroke (Landis et al., 2006; Leopold et al., 2006).
This case report details two patients who experienced smell and
taste dysfunction following minor stroke events. Symptoms reported included hyposmia (diminished sense of smell) and anosmia
(complete loss of smell), and dysgeusia (distorted taste). Patients
sense of smell and taste were assessed in an ambulatory care
stroke prevention clinic eight months following their strokes.
Patient A presented with minor stroke due to a lesion in the anterior circulation, patient B with a lesion in the posterior circulation. Both patients reported intense olfactory and gustatory dysfunction immediately following their strokes. Examination
revealed a general inability to detect subtle odours and the ability
to identify only sweet tastes for both patients. In addition, both
patients reported heavily salting or sweetening their food to mask
the distorted and unpleasant taste, which also impacted comorbid conditions such as hypertension and diabetes. Patients and
their spouses reported a decrease in their appreciation of familyrelated activities due to the patients olfactory and gustatory dysfunction. Patients reported weight loss, lack of energy and strength,
likely due to poor nutrition. Olfactory and gustatory dysfunctions
are potentially deleterious outcomes following minor stroke and
should be assessed by health care professionals prior to patient
discharge. Assistance may be required to promote the health and
well-being of patients and their carers if smell and taste are
impacted by the stroke event.
Introduction
Smell (olfactory) and taste (gustatory) are key senses in the
regulation of nourishment and safety. For example, they alert
humans to dangers such as spoiled food, fire, and smoke
inhalation (Hummel, & Welge-Luessen, 2006; Cereda, Ghika,
Maeder, & Bogousslavsky, 2002). Furthermore, smell and taste
are interdependent; patients may have difficulty distinguishing between the two, often confusing the concepts of smell
and taste (Mann, 2002; Bromley, 2000). Though olfactory dysfunction is relatively common in the general population, disorders of smell, as well as taste have been infrequently reported. Is there an incidence to quantify in patients following
stroke (Landis, Leuchter, San Millan, Lacroix, & Landis, 2006;
Leopold, Holbrook, Noell, & Mabry, 2006)?
These disorders may be a symptom of underlying disease and
can have a significant impact on quality of life. The most common causes of smell disturbances include nasal and sinus disease, upper respiratory infection, medications, smoking, head
trauma or other neurological conditions including parkinsonism, Alzheimer disease, Huntington chorea, or multiple sclerosis, endocrine disorders including diabetes mellitus,
10
hypothyroidism, and hypogonadism, depression, and aging,
in which loss of olfactory sensitivity occurs (Mann, 2002;
Bromley, 2000). Clinical manifestations of smell disorders
include hyposmia (diminished sense of smell); dysosmia (distorted smell identification) either parosmia (abberent odour
perception), phantosmia (without an odour stimulus), or
agnosia (with an odour stimulus but unable to classify); and
anosmia (total loss of smell) (Mann, 2002).
Altration des sens de lodorat
et du got la suite dun AVC :
une histoire de cas
Sommaire
Les sens de lodorat et du got jouent un rle trs important
au niveau de la nutrition et de la scurit des individus. La
combinaison des troubles du sens de lodorat et du got la
suite dun accident vasculaire crbral (AVC) est rarement
mentionne dans la littrature. (Landis et al, 2006; Leopold
et al. 2006). Cette tude de cas raconte lhistoire de deux
patients ayant subi une altration des sens lodorat et du
got la suite dun AVC. Les symptmes suivants sont
apparus: lhypo-osmie (diminution de lodorat), lanosmie
(perte du sens de lodorat) et la perte du sens du got. Les
sens de lodorat et du got furent valus chez les patients
ayant souffert dun AVC dans une clinique de prvention des
AVC, huit mois aprs lAVC. Le patient A sest prsent avec
un incident mineur localis dans la circulation crbrale
antrieure, le patient B avait une lsion dans la circulation
postrieure. Des troubles graves du sens de lodorat et du
got se sont manifests chez les deux patients immdiatement aprs l AVC. Lexamen des deux patients a rvl une
dficience reconnatre les odeurs subtiles ainsi quun sens
du got se limitant discerner les aliments sucrs. De plus,
les deux patients ont avou saler et sucrer gnreusement
leur nourriture pour en masquer le mauvais got
dsagrable. Les patients et leur conjoint ont mentionn
quils sont devenus dsintresss aux activits familiales la
suite de la perte des sens de lodorat et du got. Ils ont
remarqu une perte de poids, dnergie et de force physique
du la malnutrition. Les conditions de co-morbidit tels
que lhypertension et le diabte, furent perturbes par
lapport excessif de sel et de sucre ajouts aux aliments. La
perte des sens de lodorat et du got, due `a un accident vasculaire crbral, est potentiellement trs dommageable. Elle
devrait tre value par les professionnels de la sant avant
le dpart du patient. Un plan daction au niveau personnel
et professionnel, sadressant la promotion de la sant et du
bien-tre des patients ayant subi une perte ou une diminution des sens de lodorat et du got la suite dun accident
vasculaire crbral, pourrait savrer ncessaire.
Volume 30, Issue 2, 2008 Canadian Journal of Neuroscience Nursing
Taste disorders can result from aging, inflammation of the
mouth, infection, gastric reflux, head trauma, smoking, medications used to treat such conditions as depression (e.g., trycyclic
antidepressants), epilepsy (e.g., carbamazepine or phenytoin
sodium), Parkinson disease (e.g., levodopa), migraine (e.g., tritpans), and hypertension (e.g., captorpil), or systemic conditions
such as diabetes, pernicious anemia, or Crohns disease
(Heckmann, Heckmann, Lang, & Hummel, 2003; Mann, 2002).
Types of taste dysfunction include hypoageusia (diminished
taste), dysgeusia (distorted taste), aligeusia (altered taste, usually pleasant), phantogeusia (persistent abnormal taste in the
absence of a stimulus), and ageusia (no taste). Hypogeusia, dysgeusia, and phantogeusia are the most commonly reported
types of taste disorders (Heckmann et al., 2003).
The purpose of this case report is to describe the smell and
taste dysfunction in two patients following minor cerebrovascular stroke. One patient (A) presented with hyposmia (diminished sense of smell), the other (B) with a transient anosmia
(complete loss of smell) and both patients reported dysgeusia
(distorted taste) subsequent to minor stroke. Testing of both
patients olfactory and gustatory senses was performed by a
stroke neurologist blinded to the patients medical history.
While standardized smell and taste dysfunction kits are available, they are not routinely used by clinicians at our site. Thus,
to test the sense of smell, patients were asked to inhale the scent
of common pungent spices (cloves, cinnamon, coffee, vanilla,
and lemon), through one nostril while the other nostril was
plugged. The patients were then asked to identify the scent.
The taste test assessed four taste qualities, sweet, sour, salty,
and bitter, using sugar, lemon, salt, and black coffee (Leopold et
al., 2006; Heckmann et al., 2003). A liquid concentration of each
flavour was applied to the right and left side of the anterior
third of the tongue, using a cotton swab. After each application
and with their tongue still extended, patients were asked to
identify the taste from a list of the four descriptors.
Case report A
In January 2006, while eating dinner, a 63-year-old man experienced sudden onset of left arm heaviness and weakness with left
facial droop. On admission to the tertiary care stroke unit, the
initial neurological exam revealed left arm weakness with a
pronater drift, intact sensory function, and VII cranial nerve
facial weakness. Based on neurological examination, he was
assessed as having a National Institutes of Health Stroke Scale
(NIHSS) score of 2. Admission blood pressure was 160/85mmHg
and the patient had a regular apical heart rate of 70 BPM. The
diagnostic workup included CT, MRI, magnetic resonance
angiography (MRA) and transthoracic echocardiogram/transesophogeal echocardiogram (TTE/TEE). A diagnosis
of acute right corona radiate lacunar ischemic stroke was made.
CT findings included old bilateral lacunar strokes. The MRI
revealed a right corona radiate lacune with right suprachroniod
ICA stenosis (Figure 1). CTA revealed a tight right ICA. Doppler
ultrasound revealed stenosis of the right ICA of 50% to 69%.
Finally, TEE revealed mild LV dysfunction. The patient underwent a right carotid endarterectomy five days following initial
admission and was discharged from hospital the following day.
Medications upon discharge included Hydrochlorthiazide 12.5
mg daily, Atorvastatin 40 mg daily, ASA 81 mg daily, Felopidine
10 mg daily, Glyburide 2.5 mg daily, and Metformin 500 mg
daily. Comorbid conditions included hypertension, dyslipidemia,
and diabetes and a remote history of smoking (quit > 20 years
ago). He also had a history of cardiac disease and had undergone
coronary artery bypass graft surgery six months previously.
Immediately after the stroke, this patient noticed a general
reduced sense of smell with the smell of meat particularly
described as unpleasant with a slightly rotten odour. Over the
first three months post-discharge, his sense of smell remained
diminished. He described one potential benefit, however, in
that he could no longer detect the smell of cigarette smoke. He
complained food eaten while in-hospital tasted unpleasant
and post-discharge described the taste of most food as either
unpleasant, bitter, or as having no taste. While he was able to
identify a food item as tasting sweet he was unable to name
the actual flavour (e.g., chocolate). During this period, he
reported a weight loss of two kilograms.
A smell and taste test conducted eight months post-stroke
revealed the patient was able to faintly appreciate the smell of
cloves, but was unable to detect cinnamon or coffee. He was
also able to faintly identify a sweet taste, but had no appreciation of sour, salty, or bitter tastes. There was no difference
detected between sides of the tongue in discriminating between
tastes. At this time, his weight loss was more significant. The
patient reported losing 4 kg and had to make himself eat as
some foods, specifically meats, triggered an extreme revulsion
reaction (retching). He noted that his loss of appetite and lack
of energy resulted in fatigue, which impacted the ability to
work, and a general inability to enjoy family-related activities.
This patient described a similar experience with loss of smell
and taste following a cerebral concussion received many years
(> 20 years) prior to his stroke, with these senses returning to
normal approximately one year later.
Case report B
Figure 1. 3-T MRI scan patient A
This 61-year-old man experienced a minor stroke in February
2006. He awoke at 0500 hours with loss of coordination on the
right side and blurring of vision in both eyes, but did not describe
Canadian Journal of Neuroscience Nursing Volume 30, Issue 2, 2008
11
any limb weakness, sensory loss, or speech disturbances. A
headache with severe nausea began at 1000 hours that morning.
On admission to the tertiary care stroke unit, his neurological
exam revealed normal motor strength bilaterally, right dysmetria,
and intact cranial nerve testing. His sensory exam revealed
decreased pinprick to the right face and oculomotor examination
revealed right superior quadrantanopia, tortional nystagmus in
all directions, and bidirectional horizontal nystagmus. Admission
vital signs were normal, with a BP of 134/84 mmHg and a pulse
of 80/minute. He was assessed as having an NIHSS score of 2.
Diagnostic workup included CT, MRI, MRA, TTE/TEE and modified barium swallow. An acute right superior cerebellar infarct
was revealed on CT and MRI imaging. His MRI scan also
revealed a small acute right posteriolateral medulla lacunar
infarct (Figure 2). TTE showed a mild to moderate impairment of
left ventricular systolic function secondary to an inferior and
inferolateral wall motion abnormality and mild to moderate pulmonary hypertension. A barium swallow exam revealed incomplete inversion of the epiglottis with pooling within the volleculae
and pirifom sinuses. Co-morbid conditions and risk factors
included hypertension, dyslipidemia, and current smoking. He
also had a history of ischemic heart disease. There was no history
of depression noted. Discharge medications included hydrochlorthiazide 12.5 mg daily and atenolol 5 mg daily.
Interestingly, this patient reported the sudden onset of smell and
taste dysfunction approximately one month prior to his current
stroke event although the symptoms were subtle. At that time,
his family physician prescribed a course of antibiotics for a suspected sinus infection. However, this did not eliminate the smell
and taste symptoms. A subsequent visit to an otolaryngologist
did not reveal any anatomical abnormalities. However, following his admission for the current stroke event, a review of CT and
MRI imaging revealed a subacute left-sided lentiform stroke.
Following his current stroke, the patient reported his olfactory
and gustatory sensory disturbance became intense and food
smelled and tasted like vomit.Over the subsequent eight months,
the impaired sense of smell and taste resulted in weight loss
(reported to be approximately 9 kg overall, 5-6 kg over the first
three months post-stroke), fatigue and lack of energy due to loss of
appetite and poor nutrition, and a decrease in quality of life due
to loss of interest in food. During the first three months post-stroke
when these dysfunctions were most severe, the patient could tolerate only very sweet candies, such as chocolate. The smell and
taste of breads, pasta, coffee and meat made him ill. At six
months post-stroke, he noted a change in his ability to taste. He
could now detect food items that were heavily sweet or sour. He
described heavily salting his food in order to mask the actual
taste, and reported hot foods had little or no taste, but were tolerated better than cold food items, which remained unpleasant.
At eight months post-stroke, a test of olfactory function revealed
a general inability to detect subtle odours. However, stronger
odours such as coffee, cloves, and lemon could be detected with
the left nostril. The patient reported these smells to be bad.
Taste testing revealed a generally unpleasant rating with
sweetness faintly detected on the left side of the tongue. Bitter,
sour, and salty items could not be detected on either side of the
tongue. This patient reported occasional difficulties with swallowing, most notable when tired or eating late in the evening.
12
Discussion
In both cases, patients reported intense olfactory and gustatory
dysfunction immediately following their minor strokes.
Anatomically, one patient presented with minor stroke due to a
lesion in the anterior cerebral circulation; the other with a lesion
in the posterior circulation. Functional MRI has been used to
show the cortical areas associated with the processing of gustatory stimuli are found in areas of the brain perfused by the anterior or the posterior circulatory systems, including the insula,
the parietal and frontal opercula, and the orbitofrontal cortex
(Heckmann et al., 2003; Cereda et al., 2002). Kobayakawa et al.
(2005), through the use of magnetoencephalography, identified
the transition area between the posterior insula and parietal
operculum as the primary gustatory area in humans. In addition, strokes occurring in the pons can result in altered taste
sensation. MR imaging for patient A in this review revealed
chronic small vessel disease on the left side of the pons; patient
B experienced a medullary lacunar infarction.
The natural aging process may have been a factor in diminished smell and taste experienced in both these patients. A
natural reduction in smell and taste senses has been reported
in patients over 60 years of age (Boyce & Shone, 2006; Landis
et al., 2006). However, neither patient noted any general
diminishing of these senses over time prior to their stroke.
Both patients were also hypertensive, treated with
hydrochlorthiazide. Antihypertensive medications, particularly ACE inhibitors, but also hydrochlorthiazide have been
associated with loss of smell and taste (Bromley, 2000).
Nonetheless, this medication was utilized over an extended
period prior to the stroke event (> 5 years), with neither
patient reporting changes to smell or taste. As well, patient A
was diabetic; a condition associated in the general population
with diminished sense of taste (Mann, 2002; Bromley, 2000).
Still, this patient had been diabetic for many years, without
noting deterioration in his sense of taste. Similarly, patient B,
with phantosmia and dysgeusia, identified that throughout his
20+ year history of smoking, these extreme smell and taste
aversions were not present.
Figure 2. 3-T MRI scan patient B
Volume 30, Issue 2, 2008 Canadian Journal of Neuroscience Nursing
Heckman et al. (2003) noted that patients do not often report
problems with taste, particularly if other stroke symptoms are
present. Thus, assessment of olfactory and gustatory function
tends to be an overlooked entity in the plan of care during the
acute stage of illness. This is especially problematic for
patients with minor stroke, as hospital stay is typically very
short, often only three to four days. The impact of this disorder may, therefore, not be seen until later in the recovery
process, as with the second patient.
The duration of olfactory and gustatory dysfunction poststroke is variable, although symptoms seem to spontaneously
abate or resolve over time (Landis et al., 2006; Deems, Yen,
Kreshak, & Doty, 1996). However, the techniques employed
by the patients described here to counter the taste dysfunction included such things as heavily salting food items or consuming very sweet foods. Given their comorbid conditions,
which included hypertension, hypercholesterolemia, and diabetes, these tactics could contribute to difficulty in maintaining adequate control of these conditions.
Conclusions
While the senses of smell and taste are not considered crucial to
life, impairment can affect everyday enjoyment of food and may
contribute to anxiety, depression, anorexia, nutritional deficiencies, and subsequent deterioration in quality of life (Hummel &
Welge-Luessen, 2006; Leopold et al., 2006). In both case reports,
the patients and their wives reported being profoundly impacted by the patients distorted sense of taste. Life quality was
affected in that the patients experienced difficulty attending to
work-related tasks due to lack of energy and strength. Wives
bore the burden of finding nutritional food that could be tolerated and, as a couple, social outings were limited. It is important
to note this was not a mere inconvenience for the patient and his
wife, but a significant factor in the recovery trajectory.
Patients with minor stroke are often discharged very quickly
from acute care following their stroke event and, given the
emphasis on other physical sequelae of stroke, disturbances of
smell and taste may not be identified by patients. Nurses may
also be challenged to a) identify all pertinent post-stroke issues,
and b) deliver optimal patient education. Nurse-patient interac-
tions at this time often focus on education related to poststroke functional/physical needs and recovery, medication and
follow-up appointments. Less emphasis is given to other elements of post-stroke recovery, including issues that may impact
life quality such as diminished smell and taste. This is an important consideration, as measures taken to enhance the palatability of food may be detrimental to overall health and well-being,
such as heavily salting food or reliance on excessive sweetening.
It is also important to consider the needs of the primary carer
in the home, as the responsibility for meal preparation and
social interactions often is their responsibility. It may be worthwhile, therefore, for clinicians to add a simple question about
smell-taste-related problems to the pre-discharge education
component of patient care. A question such as, Do you have
difficulty recognizing food or beverages as sweet, sour, salty, or
bitter may lead to identification of problems with these senses
and, by extension, to assistance and support with management.
About the authors
Theresa L. Green, RN, PhD, Faculty of Nursing, University of
Calgary, Calgary, AB. She is a post-doctoral fellow in the
Department of Clinical Neurosciences.
Correspondence regarding this article should be addressed to
Dr. Theresa L. Green, Calgary Stroke Program, Department
of Clinical Neurosciences, University of Calgary, Foothills
Hospital, Rm C1101A, 1403 29th Street NW, Calgary, AB
T2N 2T9. E-mail: greentl@ucalgary.ca
Lisa D. McGregor, RN, MSc, Research Assistant, Faculty of
Nursing, University of Calgary, AB.
Kathryn M. King, RN, PhD, Professor, Faculty of Nursing,
University of Calgary, AB.
Acknowledgements and funding
Dr. Green is funded by the Heart and Stroke Foundation of
Canada, the Canadian Stroke Network, Canadian Institutes
for Health Research and the Alberta Heritage Foundation
for Medical Research. Dr. King is a Population Health
Investigator funded by the Alberta Heritage Foundation for
Medical Research.
References
Boyce, J.M., & Shone, G.R. (2006). Effects of ageing on
smell and taste. Postgraduate Medical Journal, 82, 239241.
Bromley, S.M. (2000). Smell and taste disorders: A primary
care approach. American Family Physician, 61, 427438.
Cereda, C., Ghika, J., Maeder, P., & Bogousslavsky, J.
(2002). Strokes restricted to the insular cortex. Neurology,
59, 19501955.
Deems, D., Yen, D., Kreshak, A., & Doty, R. (1996).
Spontaneous resolution of dysgeusia. Archives of
Otolaryngol Head and Neck Surgery, 122, 961963.
Heckmann, J.G., Heckmann, S.M., Lang, C.J., &
Hummel, T. (2003). Neurological aspects of taste disorders.
Archives of Neurology, 60, 667671.
Hummel, T., & Welge-Luessen, A. (2006). Assessment
of olfactory function. Advances in Oto-Rhino-Laryngology,
63, 8489.
Kobayakawa, T., Wakita, M., Saito, S., Gotow, N., Sakai,
N., & Ogawa, H. (2005). Location of the Primary Gustatory
Area in Humans and its Properties, Studied by
Magnetoencephalography. Chemical Senses, 30 (supplement),
226227.
Landis, B.N., Leuchter, I., San Millan, R.D., Lacroix, J.S.,
& Landis, T. (2006). Transient hemiageusia in cerebrovascular
lateral pontine lesions. Journal of Neurology, Neurosurgery
& Psychiatry, 77, 680683.
Leopold, D.A., Holbrook, E., Noell, C., & Mabry, R.
(2006). Disorders of taste and smell. emedicine [On-line].
Retrieved from www.emedicine.com/ent/topic333
Mann, N. (2002). Management of smell and taste
problems. Cleveland Clinic Journal of Medicine, 69,
329336.
Canadian Journal of Neuroscience Nursing Volume 30, Issue 2, 2008
13
You might also like
- Sample-Anatomy and Physiology The Unity of Form and Function 9th 9EDocument30 pagesSample-Anatomy and Physiology The Unity of Form and Function 9th 9Erist0% (1)
- Case Scenario-Study 2Document6 pagesCase Scenario-Study 2J100% (1)
- Clinical Toxicology 2013 CompleteDocument364 pagesClinical Toxicology 2013 Completenuttiya_w3294No ratings yet
- Absolute Proof of Marijuana's Critical Medical Value in The Treatment of Conn's SyndromeDocument6 pagesAbsolute Proof of Marijuana's Critical Medical Value in The Treatment of Conn's Syndrome420infoNo ratings yet
- Astrology and Ayurvedic PlantsDocument16 pagesAstrology and Ayurvedic Plantsch_poddar100% (1)
- Dialysis Vintage, Body Composition, and Survival in Peritoneal Dialysis PatientsDocument4 pagesDialysis Vintage, Body Composition, and Survival in Peritoneal Dialysis PatientsCynthia MelindaNo ratings yet
- Qara Syifa Fachrani - 2010221030 - Description of Ventricular Arrhythmia After Taking Herbal Medicines in Middle-Aged CouplesDocument4 pagesQara Syifa Fachrani - 2010221030 - Description of Ventricular Arrhythmia After Taking Herbal Medicines in Middle-Aged CouplesQara Syifa FNo ratings yet
- Anaphylaxis Med Case UCDDocument10 pagesAnaphylaxis Med Case UCDAl Qur'anNo ratings yet
- Cardiovascular Complications of Antipsychotic MedicationsDocument3 pagesCardiovascular Complications of Antipsychotic MedicationsAakash ShahNo ratings yet
- Rajiv Gandhi University of Health Sciences Bangalore, Karnataka Annexure-IiDocument14 pagesRajiv Gandhi University of Health Sciences Bangalore, Karnataka Annexure-IiJoy Deb ChowdhuryNo ratings yet
- Laporan - Pendahuluan PJK FixDocument8 pagesLaporan - Pendahuluan PJK FixNndaydnaNo ratings yet
- Cardiovascular Risk Related To Alcohol ConsumptionDocument11 pagesCardiovascular Risk Related To Alcohol Consumptionapi-658183316No ratings yet
- Read The Report On The Iced Tea PoisoningDocument20 pagesRead The Report On The Iced Tea PoisoningSue Goetinck AmbroseNo ratings yet
- Read The Report On The Iced Tea PoisoningDocument4 pagesRead The Report On The Iced Tea PoisoningSue Goetinck AmbroseNo ratings yet
- International Journal of Medical Research & Health SciencesDocument11 pagesInternational Journal of Medical Research & Health ScienceseditorijmrhsNo ratings yet
- Heiser 2010Document6 pagesHeiser 2010asujan58pNo ratings yet
- Abstract: Objective: To Verify The Relationship Between Systemic ArterialDocument10 pagesAbstract: Objective: To Verify The Relationship Between Systemic Arterialprofesor conanNo ratings yet
- Kidney (Group10)Document35 pagesKidney (Group10)tonyfee02No ratings yet
- Medicine CasesDocument56 pagesMedicine Casesmohamed muhsinNo ratings yet
- Study of Drug Use in Essential Hypertension and Their ComplianceDocument13 pagesStudy of Drug Use in Essential Hypertension and Their ComplianceRachmat MuhammadNo ratings yet
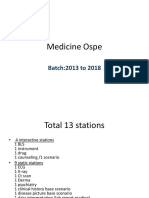
- Medicine Ospe Final SlidesDocument75 pagesMedicine Ospe Final SlidesZeemal ShakeelNo ratings yet
- Essential HypertensionDocument8 pagesEssential HypertensionAparajitaNo ratings yet
- Amyotrophic Lateral Sclerosis Recovery From Allergy After Removal of Dental Amalgam FillingsDocument11 pagesAmyotrophic Lateral Sclerosis Recovery From Allergy After Removal of Dental Amalgam FillingsMaria A Padilla100% (1)
- Business CommunicationDocument7 pagesBusiness Communicationsujal vermaNo ratings yet
- Asa Ora PDFDocument8 pagesAsa Ora PDFwyndinkNo ratings yet
- Clinical Diagnosis and Treatment of Olfactory Dysfunction: Seok Hyun ChoDocument9 pagesClinical Diagnosis and Treatment of Olfactory Dysfunction: Seok Hyun ChoAnonymous 3Uy0HjXKNo ratings yet
- Thermal Medicine in Elderly PatientsDocument36 pagesThermal Medicine in Elderly PatientsThermalBathsforActivNo ratings yet
- Approach To PoisoningDocument66 pagesApproach To PoisoningKapil SharmaNo ratings yet
- A Prospective Study of Cardiovascular Risk Factors and Incident Hearing Loss in Men LaryngoscopeDocument5 pagesA Prospective Study of Cardiovascular Risk Factors and Incident Hearing Loss in Men LaryngoscopeGirish SubashNo ratings yet
- Ojsadmin, 1034Document5 pagesOjsadmin, 1034杨嘉宜No ratings yet
- Alcohol Withdrawal Syndrome by AAFPDocument8 pagesAlcohol Withdrawal Syndrome by AAFPWayTernMahNo ratings yet
- Case 22-2010 - AmyloidDocument9 pagesCase 22-2010 - AmyloidDaniela SalvadorNo ratings yet
- 2021 Sexual Activity After Myocardial Revascularizat 2021 Current Problems in Ca1Document17 pages2021 Sexual Activity After Myocardial Revascularizat 2021 Current Problems in Ca1Angie OvandoNo ratings yet
- Case Analysis Presentation Group 1 Almost Done 2 1Document75 pagesCase Analysis Presentation Group 1 Almost Done 2 1Vhince Norben PiscoNo ratings yet
- NIH Public Access: Author ManuscriptDocument14 pagesNIH Public Access: Author ManuscriptCésar LópezNo ratings yet
- TastePlate JRN 2021Document7 pagesTastePlate JRN 2021Marce SiuNo ratings yet
- International Journal of Health Sciences and ResearchDocument9 pagesInternational Journal of Health Sciences and ResearchYounanda PutriNo ratings yet
- Radiotherapy-Induced Taste ImpairmentDocument7 pagesRadiotherapy-Induced Taste Impairmentbud.wisden9806No ratings yet
- Abstract of Re-Orientation Course For Ayurvedic DoctorsDocument22 pagesAbstract of Re-Orientation Course For Ayurvedic DoctorsYoga FMUNo ratings yet
- 4372 8856 1 SPDocument8 pages4372 8856 1 SPNurul FadhilahNo ratings yet
- Lifestyle Related Risk Factors in The Aetiology of Gastro-Oesophageal RefluxDocument6 pagesLifestyle Related Risk Factors in The Aetiology of Gastro-Oesophageal RefluxazlinaNo ratings yet
- AntipsychoticsDocument5 pagesAntipsychoticsapi-639751111No ratings yet
- PheochromocytomaDocument24 pagesPheochromocytomacamelle sisonNo ratings yet
- FF 304dysgeusia1Document3 pagesFF 304dysgeusia1Manuel HuamanNo ratings yet
- Drug-Induced Taste Disorders in Clinical Practice and Preclinical Safety EvaluationDocument10 pagesDrug-Induced Taste Disorders in Clinical Practice and Preclinical Safety EvaluationBharat NarumanchiNo ratings yet
- ESCALA de Somnolencia de Epworth en Un Centro de Salud FamiliarDocument10 pagesESCALA de Somnolencia de Epworth en Un Centro de Salud FamiliarEnith VilelaNo ratings yet
- Altered Mental Status in Cirrhosis: Etiologies and Outcomes: Riginal RticleDocument7 pagesAltered Mental Status in Cirrhosis: Etiologies and Outcomes: Riginal RticleTheRainMelodyNo ratings yet
- Alcohol-Related Psychosis Clinical PresentationDocument5 pagesAlcohol-Related Psychosis Clinical PresentationRavi KumarNo ratings yet
- 1 PBDocument6 pages1 PBDINDA PUTRI SAVIRANo ratings yet
- Nursing Care in Patient With Acute Cardiogenic Pulmonary EdemaDocument5 pagesNursing Care in Patient With Acute Cardiogenic Pulmonary EdemaAyyu Sandhi100% (1)
- Musictherapy DementiaDocument16 pagesMusictherapy DementiaConsuelo VelandiaNo ratings yet
- Evaluation of The Effects of Music Therapy Using Todi Raga of Hindustani Classical Music On Blood Pressure, Pulse Rate and Respiratory Rate of Healthy Elderly MenDocument8 pagesEvaluation of The Effects of Music Therapy Using Todi Raga of Hindustani Classical Music On Blood Pressure, Pulse Rate and Respiratory Rate of Healthy Elderly MenAprilinda SafitriNo ratings yet
- A Nos MiaDocument17 pagesA Nos Miaintan_ekleNo ratings yet
- Dhara HypertensionDocument4 pagesDhara Hypertensionapi-3747054No ratings yet
- Sudden Cardiac Death in Anabolic Androgenic Steroids Abuse: Case Report and Literature ReviewDocument8 pagesSudden Cardiac Death in Anabolic Androgenic Steroids Abuse: Case Report and Literature ReviewmjkoNo ratings yet
- Jurnal Terapi MusikDocument20 pagesJurnal Terapi MusikWendy GoxilNo ratings yet
- WEEK 9 - Environmental Health and ToxicologyDocument81 pagesWEEK 9 - Environmental Health and ToxicologyRechelle Anne RondaelNo ratings yet
- Capitol Intoxicatii 3Document17 pagesCapitol Intoxicatii 3AncaNo ratings yet
- Diabetic EmergenciesDocument9 pagesDiabetic EmergenciesIlyes FerenczNo ratings yet
- Holstege2008 PDFDocument25 pagesHolstege2008 PDFjhon862No ratings yet
- Treatment of Adrenalectomy Intraoperative Complications in A Patient With Adrenal Tumor Accompanied by Hypercortisol ManifestationDocument13 pagesTreatment of Adrenalectomy Intraoperative Complications in A Patient With Adrenal Tumor Accompanied by Hypercortisol ManifestationRainbow DashieNo ratings yet
- Disorders of Blood Pressure Regulation: Phenotypes, Mechanisms, Therapeutic OptionsFrom EverandDisorders of Blood Pressure Regulation: Phenotypes, Mechanisms, Therapeutic OptionsNo ratings yet
- Christopher Cheung Approach To Cardiac History Taking: Cyanosis or SyncopeDocument6 pagesChristopher Cheung Approach To Cardiac History Taking: Cyanosis or SyncopeApryl Phyllis JimenezNo ratings yet
- Vhince Pisco BSN III NCM 117 - Drug StudyDocument3 pagesVhince Pisco BSN III NCM 117 - Drug StudyVhince Norben PiscoNo ratings yet
- By William Goh Dragon Fish Industry Booth No: 928Document13 pagesBy William Goh Dragon Fish Industry Booth No: 928rrpenolioNo ratings yet
- Exercise 1: Rewrite The Following Sentences That Keep The Same MeaningDocument10 pagesExercise 1: Rewrite The Following Sentences That Keep The Same Meaningthanhvan2012No ratings yet
- Refeeding Syndrome GuidelineDocument5 pagesRefeeding Syndrome GuidelinePejman AhmadiNo ratings yet
- Krok 1 Medicine 2014Document24 pagesKrok 1 Medicine 2014bose_lowe11No ratings yet
- Gestational HypertensionDocument34 pagesGestational HypertensionRANIELLE SIMNo ratings yet
- q1 Edited Assessment in English 10 As of December 9 2020Document9 pagesq1 Edited Assessment in English 10 As of December 9 2020Angelo Bagaoisan PascualNo ratings yet
- Scored Patient-Generated Subjective Global Assessment (PG-SGA)Document2 pagesScored Patient-Generated Subjective Global Assessment (PG-SGA)Misbah sabirNo ratings yet
- Misasmatic PrescribingDocument28 pagesMisasmatic PrescribingAli AkbarNo ratings yet
- GenDec SV0638 22-May-2024 (AMM1441GD)Document1 pageGenDec SV0638 22-May-2024 (AMM1441GD)Ahmad AzaizehNo ratings yet
- Susp Appendicitis Akut - Dr.edwin - SP.BDocument13 pagesSusp Appendicitis Akut - Dr.edwin - SP.Bchaer assofiNo ratings yet
- Paederus Dermatitis An Outbreak On A Medical Mission AmazonDocument3 pagesPaederus Dermatitis An Outbreak On A Medical Mission AmazonrrrawNo ratings yet
- CV 2016 New BhadramDocument4 pagesCV 2016 New BhadramVeerabhadram YeshalaNo ratings yet
- Pathology Mcqs Week 11: 1. in Adult Respiratory Distress SyndromeDocument4 pagesPathology Mcqs Week 11: 1. in Adult Respiratory Distress Syndromeمجتبى علي100% (5)
- Atrial Fibrilliation Part 1 Pathophysiology C CottrellDocument5 pagesAtrial Fibrilliation Part 1 Pathophysiology C CottrellA Farid WajdyNo ratings yet
- Cervical SpondylosisDocument8 pagesCervical SpondylosisRicha AgarwallaNo ratings yet
- Kawana 1987Document5 pagesKawana 1987Andreea CiorneaNo ratings yet
- Burning Mouth Syndrome: EtiologyDocument5 pagesBurning Mouth Syndrome: EtiologyFitri AngginiNo ratings yet
- Acute Tubular NecrosisDocument15 pagesAcute Tubular NecrosisDeepak patelNo ratings yet
- Revision de Coccidiasen CamelidosDocument15 pagesRevision de Coccidiasen CamelidosKeny Arnold ApazaNo ratings yet
- Granulomatous Mastitis: A Masquerading Entity: Punyashetty Kajal B., Patil Tejeshwini, Singh ChitraDocument6 pagesGranulomatous Mastitis: A Masquerading Entity: Punyashetty Kajal B., Patil Tejeshwini, Singh Chitrasantri safiraNo ratings yet
- Effects of The 1st HouseDocument22 pagesEffects of The 1st HousepankajmadhavNo ratings yet
- BRS PediatricsDocument971 pagesBRS Pediatricstycobb6375% (8)
- Essay and Outline FaiqaDocument3 pagesEssay and Outline FaiqaFaiqa Himma EmaliaNo ratings yet
- CholangiocarcinomaDocument9 pagesCholangiocarcinomaloloalpsheidiNo ratings yet
- Baiae NCPDocument1 pageBaiae NCPreignyfayeNo ratings yet