Professional Documents
Culture Documents
CT Applications in Chest Pathology
CT Applications in Chest Pathology
Uploaded by
Nilanka SandunOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
CT Applications in Chest Pathology
CT Applications in Chest Pathology
Uploaded by
Nilanka SandunCopyright:
Available Formats
CT Applications in Chest Pathology
Objectives are as follows,
List the types of CT
List the indications of chest CT
Understand the applications of chest CT
Identify the radiological signs of common chest diseases on CT
Basics of CT
Two dimensional representation of a three dimensional slice
Internal structure of the organ can be reconstructed from multiple slices
Image display settings can be varied by adjusting WW & WL
Lung window
Mediastinal window (soft tissue window)
Bone window
Types of CT Scans are,
Conventional CT
High resolution CT
Conventional CT Vs HRCT
Conventional- 3 to 10 mm thick slices are obtained contiguously, imaging
100% of the lung
HRCT- 1-1.5mm thin slices of lung are obtained at non-contiguous intervals,
usually 1 to 2 cm apart, throughout the whole lung. . Only 5 to 10% of the
lung is sampled
Indications of Chest CT
Evaluation of an abnormality identified on conventional radiographs - Solitary
pulmonary nodule/ lung tumour/mediastinal mass
Diagnosing & Staging of Lung Cancer
Detection of occult pulmonary metastases
Detection of mediastinal nodes /masses
Distinction of empyema from peripheral lung abscess
Detection and evaluation of aortic disease
Pulmonary embolism
Haemoptysis
Applications of CT
1. Detection of Lung Tumours
2. Diagnosis
3. Anatomic extent of disease -Intra and/or extra thoracic disease extent , TNM
descriptors
4. Decision of therapeutic strategy -Surgery -vs- Chemotherapy -vs- Palliative
Care Resectability / Irresectability
5. Image guided biopsies
Lung tumours
Benign tumours
- Harmatoma, Adenoma, AV Malformation
Malignant tumours- Primary (Bronchial Ca, Alveolar cell Ca), Secondary
Benign tumours- Harmatoma
8% of all solitary pulmonary nodules are harmatomas
It is the most common benign lung tumour
They are mostly asymptomatic
Harmatoma
Round, smooth mass - increase in size slowly
Calcification in 15% - pathognomonic if popcorn type
Fat in 50%
Cavitation - extremely rare
2/3 are peripheral
Rarely multiple
Bronchial Adenoma
Uncommon- Possess some of the properties of malignant growth
Two histological types
1. Carcinoid tumour (relatively common)
2. Cylindroma/adenoid cystic Ca (rare)
Malignant tumours Bronchial carcinoma
Most common malignant tumour
Arises from bronchial epithelium
Pathological types
Squamous (30-35%)
Adenocarcinoma (30-35%)
Large Cell Undifferentiated (15-20%)
Small Cell (20-25%): systemic disease
Application of CT in Lung Carcinoma
1. Assess the primary tumour
2. Assess the secondary effect /complications
3. Assess the nodal/ other metastasis
CT appearances in primary malignant tumour
1. Dense irregular hilar opacity
2. Dense peripheral opacity
3. Dense irregularly cavitating lesion
4. Hilar opacity with collapse of a segment /whole lung
Malignant tumour-Secondary effects
1. Pleural effusion
2. Mediastinal widening
3. Osteolytic lesions of the rib
4. Diaphragmatic paralysis
Detection of Lung Cancer Plain Radiography vs. CT
Contrast resolution of CT is superior to plain chest radiography
Significantly more nodules detected on CT
The Stages of Lung Cancer
Stage I
No nodal metastases and surgically removable
Stage II
Adds hilar lymph node involvement (IIA) or resectable chest
wall/mediastinal
involvement (IIB)
Stage III
Stage III B Extensive but irresectable by conventional criteria but still
confined to chest, therefore
consider radical radiotherapy
Stage IV Distant metastases
A Extensive but resectable disease
The Staging of Lung Cancer: International Staging System
PRIMARY TUMOUR (T)
T1 Diameter 3cms, surrounded by lung /visceral pleura. No involvement of
lobar bronchi
T2>3cm diameter; involves main bronchus but 2cm distal to carina; invades
visceral pleura; associated with atelectasis or obstructive pneumonitis extending to
hila but not involving entire lung
T3Tumour of any size but with invasion of: chest wall,diaphragm, mediastinal pleura,
parietal pleura, parietal pericardium, or tumour in main bronchus <2cm from carina
but not involving carina; or atelectasis / obstructive pneumonitis of entire lung
T4Tumour of any size but with invasion of: heart, great vessels, trachea,
oesophagus, vertebral
body, carina; tumour with malignant pleural / pericardial
effusion; or with satellite tumour nodule(s) in ipsilateral primary-tumour lobe
The CT Staging of Lung Cancer: T1 versus T2 lesions
T
1
The CT Staging of Lung Cancer: T1 / T2 lesions
T2
The CT Staging of Lung Cancer: T3 / T4 lesions
T3
Superior sulcus tumours
The CT Staging of Lung Cancer: Nodal Staging
NO
None
N1
Ipsilateral hilar
N2
Ipsilateral mediastinal (incl subcarinal)
N3
Contralateral mediastinal / hilar or supraclavicular
Detection of Lung Cancer- BIOPSY
Central Obstructing lesion - bronchoscopy
Peripheral tumour - percutaneous biopsy under CT guidance Cytology, Histology
Cavitating Carcinoma
Metastases in Lung Cancer
Liver
33-39%
Adrenals
20-33%
Brain
16-26%
Bone
15-21%
Key point
CT remains the mainstay in the non-invasive staging of lung cancer;
Mediastinal masses
ANTERIOR MEDIASTINUM
THYMOMA
TERATOMA
INTRATHORACIC THYROID ENLARGEMENT
LYMPHOMA (3 Ts and an L)
OTHER
- LYMPHANGIOMA
ANEURYSM OF ASCENDING AORTA
Middle mediastinium Masses
Merge with hilae and cardiac borders
Lymphadenopathy
Bronchogenic cyst
Aortic aneurysm
Most middle mediastinal masses are due to enlarged nodes.
Posterior mediastinal masses
Neurogenic tumour
Extramedullary haemopoeisis
Reticulosis, myeloma
Paravertebral abscess
Enlarged paravertebral lymph nodes
Haematoma following injury to the spine
Aortic aneurysm
Hiatus hernia
Dilated oesophagus in achalasia
Thymoma CT
Retrosternal goiter
Commonest pleural masses
Mesothelioma: It is a diffuse or localised pleural mass. Large pleural effusions are
common. May have associated pleural plaques
Pleural metastases - often obscured by the accompanying effusion
Malignant mesothelioma
Lung Abscess
Aortic aneurysm
Pulmonary embolism
Indications of Chest HRCT
Detection of lung disease in patient with pulmonary signs and symptoms or
abnormal pulm function test but normal or equivocal CXR
Emphysema, Extrinisic allergic alveolitis, small airway disease,
immunocompromised patient
Evaluation of diffusely abnormal CXR
Cystic fibrosis, Sarcoidosis, interstitial lung disease Histocytosis X, ARDS
HRCT Normal lung
Basic HRCT Patterns
Lines
Nodules
Consolidation
Ground-glass Opacity
Cysts
Linear abnormalities
a) thickened interlobular septa
b) bronchovascular interstitial thickening
c) reticular change
e.g Fibrosing alveolitis Lymphangitic tumours
Fibrosing alveolitis
Lymphangitic tumour
Nodules
A nodule is a rounded density that does not correspond to a vessel.
The anatomic distribution of nodules--centrilobular, random, or interstitial--helps
to identify potential causes
e.g- bronchopneumonia gives nodules in a centrilobular distribution
Nodules Infective
Ground glass opacity
A hazy opacity that does not obscure the associated pulmonary vessels. This
appearance results from parenchymal abnormalities that are below the spatial
resolution of HRCT.
E.g. alveolar wall inflammation or thickening, with partial air-space filling, or with
some combination of the two.
Ground glass- Influenza pneumonia
Cysts
Rounded structure that is filled with air and usually has a thin wall.
The cyst contents are as dark as air surrounding the patient
E.g.Cystic bronchiectasis
Chronic interstitial fibrosis (subpleural honeycombing)
Langerhans cell Histiocytosis
Lymphangioleiomyomatosis
Cystic Bronchiectasis
Consolidation
You might also like
- Lung CancerDocument19 pagesLung Cancerj.doe.hex_87No ratings yet
- Lung Cancer Presentation FinalDocument48 pagesLung Cancer Presentation Finalراس زهد ارفنندNo ratings yet
- Lung CancerDocument15 pagesLung CancerO.r. CadzNo ratings yet
- Pulmon Ology MCQ SDocument280 pagesPulmon Ology MCQ SSai ShankerNo ratings yet
- Lung Tumours: Bronchogenic Carcinoma Bronchial Carcinoid and Other Tumours Metastatic TumoursDocument41 pagesLung Tumours: Bronchogenic Carcinoma Bronchial Carcinoid and Other Tumours Metastatic Tumoursvintock1979No ratings yet
- Lung Cancer Presentation FinalDocument37 pagesLung Cancer Presentation FinalemanuelgregorymanimoNo ratings yet
- Askep CA Paru OkDocument70 pagesAskep CA Paru OkLisa KurniaNo ratings yet
- Presentation Small Cell Lung CancerDocument59 pagesPresentation Small Cell Lung Cancerprudhviraj mNo ratings yet
- Respiration 11 Bronchogenic CarcinomaDocument48 pagesRespiration 11 Bronchogenic Carcinomaapi-19641337No ratings yet
- Chest Imaging PT 2Document70 pagesChest Imaging PT 2Andrei RomanNo ratings yet
- Lung Cancer: by Holly Winn and Cathy Mac DonaldDocument49 pagesLung Cancer: by Holly Winn and Cathy Mac DonaldfajarnugrahamulyaNo ratings yet
- Lung Cancer: Dr. Bhupendra Kaushik Dr. Deepti Sharma MU-2Document49 pagesLung Cancer: Dr. Bhupendra Kaushik Dr. Deepti Sharma MU-2sharmadeepti1992No ratings yet
- Lung Cancer 1Document44 pagesLung Cancer 1DR.OMAR ABDALLANo ratings yet
- Lung CancerDocument51 pagesLung Cancercharansri821No ratings yet
- CT Chest: IndicationsDocument14 pagesCT Chest: IndicationsArnette Castro de GuzmanNo ratings yet
- Bronkogenik KarsinomaDocument55 pagesBronkogenik KarsinomaPandu AlanNo ratings yet
- Lung Cancer: By: Faezah Nur Mohd Redzwan Nooratiqah RahmatDocument30 pagesLung Cancer: By: Faezah Nur Mohd Redzwan Nooratiqah RahmatDumora FatmaNo ratings yet
- Bronchogenic Carcinoma: DR Ayman El-DibDocument40 pagesBronchogenic Carcinoma: DR Ayman El-DibMuhdZaeedNo ratings yet
- 11 Lung CancerDocument30 pages11 Lung CancerMuhammadNo ratings yet
- Bronchogenic Malignancy and Metastatic Disease: Hilar MassesDocument4 pagesBronchogenic Malignancy and Metastatic Disease: Hilar MassesTira SariNo ratings yet
- Lung Cancer Presentation FinalDocument40 pagesLung Cancer Presentation Finaljamestarerakshal7329No ratings yet
- Pulmonary Nodule, FK Unlam Oktober 2015Document35 pagesPulmonary Nodule, FK Unlam Oktober 2015aldoNo ratings yet
- Textbook of MedicineDocument5 pagesTextbook of MedicineSudip DevadasNo ratings yet
- Lung Cancer and AllDocument55 pagesLung Cancer and AllAjengNo ratings yet
- Lung CancerDocument8 pagesLung CancerGian Arlo Hilario CastroNo ratings yet
- 2.lung NeoplasmDocument50 pages2.lung Neoplasmtesfayegermame95.tgNo ratings yet
- EMPYEMA ReviewDocument95 pagesEMPYEMA ReviewBijay KumarNo ratings yet
- SGL5 - HaemoptysisDocument73 pagesSGL5 - HaemoptysisDarawan MirzaNo ratings yet
- Lec40 - Bronchogenic Carcinoma - 231205 - 120925 - 231205 - 141812Document37 pagesLec40 - Bronchogenic Carcinoma - 231205 - 120925 - 231205 - 141812mahmoudsalameh192000No ratings yet
- Lung Cancer Presentation FinalDocument48 pagesLung Cancer Presentation FinalMarc Andrew100% (3)
- LungDocument18 pagesLungmuneera salimNo ratings yet
- What Is Ultrasound?Document15 pagesWhat Is Ultrasound?Al-Mukashfi TahaNo ratings yet
- Carcinoma Lung and Lymhangitis Carcinomatosa 2Document43 pagesCarcinoma Lung and Lymhangitis Carcinomatosa 2Jagan MaxNo ratings yet
- Lung NeoplasmsDocument29 pagesLung NeoplasmsZ-shan iftikharNo ratings yet
- WelcomeDocument64 pagesWelcomeAngel LeeNo ratings yet
- Session 3 Nursing Care of The Patient With Lung CancerDocument29 pagesSession 3 Nursing Care of The Patient With Lung Cancersalomenandi643No ratings yet
- Lung CancerDocument29 pagesLung CancerMierre SiriusNo ratings yet
- Bronchogenic Carcinoma: Dr. Vineet ChauhanDocument49 pagesBronchogenic Carcinoma: Dr. Vineet ChauhanRaviNo ratings yet
- Dr. Lamin B.A Jaiteh General SurgeryDocument17 pagesDr. Lamin B.A Jaiteh General Surgerymomodou s jallowNo ratings yet
- BronchoDocument15 pagesBronchoCharleneBunquinNo ratings yet
- Lung Cancer. Clinic. Diagnosis PresentationDocument18 pagesLung Cancer. Clinic. Diagnosis Presentationdrshah533No ratings yet
- Lung Cancer 2020Document68 pagesLung Cancer 2020ebkai98No ratings yet
- Chest İmagi̇ngDocument83 pagesChest İmagi̇ngHamza EljoeidiNo ratings yet
- 2022.8.18 Lung CA IMD StudentDocument65 pages2022.8.18 Lung CA IMD StudentashmangalNo ratings yet
- Imaging in Bronchogenic CarcinomaDocument86 pagesImaging in Bronchogenic CarcinomaSandipan NathNo ratings yet
- Case (PGH)Document32 pagesCase (PGH)Roland AngelesNo ratings yet
- High Resolution Computed Tomography of The LungsDocument26 pagesHigh Resolution Computed Tomography of The LungsTessa AcostaNo ratings yet
- Surgery of The ChestDocument30 pagesSurgery of The ChestLidia KetaNo ratings yet
- Oncology Disorders StudentDocument41 pagesOncology Disorders StudentshougNo ratings yet
- Lung CancerDocument6 pagesLung Cancerzaid nabeelNo ratings yet
- Imaging of Lung Tumors: Roshan ValentineDocument79 pagesImaging of Lung Tumors: Roshan ValentineCitra AryantiNo ratings yet
- CT Thoracic: University of Perpetual HelpDocument9 pagesCT Thoracic: University of Perpetual Help3ulalaNo ratings yet
- Lung CancerDocument5 pagesLung Cancerreshmivunni100% (1)
- Emad Efat Chest CT BestDocument260 pagesEmad Efat Chest CT Bestdr Mohit TaylorNo ratings yet
- Pleural Diseases 32Document15 pagesPleural Diseases 32Anushka SharmaNo ratings yet
- 27 Mediastinal and Other Neoplasms Part 2 Other Lung NeoplasmsDocument25 pages27 Mediastinal and Other Neoplasms Part 2 Other Lung NeoplasmsjimmyneumologiaNo ratings yet
- Clinical Pharmacy PPT 1Document44 pagesClinical Pharmacy PPT 1Umair MazharNo ratings yet
- Lung Cancers: Cause ForDocument19 pagesLung Cancers: Cause Formiaaudina72No ratings yet
- Lung TumorsDocument44 pagesLung Tumorsx8jx8dcsyvNo ratings yet
- Tacar High Resolution Computed Tomography of The LungsDocument79 pagesTacar High Resolution Computed Tomography of The Lungssindy suarezNo ratings yet
- Pancoast Syndrome, (Apical Lung Cancer) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandPancoast Syndrome, (Apical Lung Cancer) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Diagnostic Procedures in Respiratory DiseaseDocument41 pagesDiagnostic Procedures in Respiratory DiseaseVio Mincu50% (2)
- G.R. No. 176832 May 21, 2009 Government Service Insurance System, Petitioner, vs. MARIAN T. VICENCIO RespondentDocument2 pagesG.R. No. 176832 May 21, 2009 Government Service Insurance System, Petitioner, vs. MARIAN T. VICENCIO RespondentAriza ValenciaNo ratings yet
- Chaudhary2012 PDFDocument5 pagesChaudhary2012 PDFSnehaNo ratings yet
- Management of Dyspnoea - DR Yeat Choi LingDocument40 pagesManagement of Dyspnoea - DR Yeat Choi Lingmalaysianhospicecouncil6240No ratings yet
- Eating For Energy NEWDocument272 pagesEating For Energy NEWCARLOSWAR101100% (4)
- Oncology NursingDocument12 pagesOncology NursingDick Morgan Ferrer80% (5)
- Beyond ChemoteraphyDocument16 pagesBeyond ChemoteraphyDewiWahyuKartika100% (1)
- English For Academic and Professional PurposesDocument10 pagesEnglish For Academic and Professional Purposesazileinra OhNo ratings yet
- Ulangan Akhir Semester Ganjil Bhs InggrisDocument7 pagesUlangan Akhir Semester Ganjil Bhs InggrisWhilda BayuNo ratings yet
- ID LncRNA CARD8-AS1Document8 pagesID LncRNA CARD8-AS1Samuel Salinas AguirreNo ratings yet
- Pollution-Related Chronic Respiratory Disease: Dr. Dr. Agus Dwi Susanto, SP.P (K), FISR, FAPSRDocument46 pagesPollution-Related Chronic Respiratory Disease: Dr. Dr. Agus Dwi Susanto, SP.P (K), FISR, FAPSRRosi AmaliaNo ratings yet
- Lung Cancer - WikipediaDocument25 pagesLung Cancer - WikipediaMaria Vanda Ribeiro Moreira MoreiraNo ratings yet
- Paraneoplastic DermatosesDocument57 pagesParaneoplastic DermatosesMohamed Riyaz100% (1)
- Public Speaking 2010Document5 pagesPublic Speaking 2010Francisous Mee100% (1)
- Lung Cancer Lecture Notes (Quick Summary)Document4 pagesLung Cancer Lecture Notes (Quick Summary)Ibrahim FoondunNo ratings yet
- Example of Research Paper About CancerDocument8 pagesExample of Research Paper About Cancerjuzel0zupis3100% (1)
- Sun Pharma Laboratories LTD Vs Intas PharmaceuticaDE202020012016162849COM195096Document50 pagesSun Pharma Laboratories LTD Vs Intas PharmaceuticaDE202020012016162849COM195096Siddharth soniNo ratings yet
- Interventional Radiology Cases-Oxford University Press (2015) PDFDocument337 pagesInterventional Radiology Cases-Oxford University Press (2015) PDFCasandra Quezada Torres100% (3)
- Wiki Resp Mcqs ExplainedDocument7 pagesWiki Resp Mcqs ExplainedArvinth Guna SegaranNo ratings yet
- Cancer of PresentationDocument44 pagesCancer of PresentationAnna TrầnNo ratings yet
- Dr. Handoko T, SPP: Sub Departemen Penyakit Paru Dan AlergiDocument54 pagesDr. Handoko T, SPP: Sub Departemen Penyakit Paru Dan AlergiMUHAMMAD BAGIR ALJUFRINo ratings yet
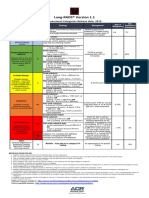
- Lung RADS® Version 1.1: Assessment Categories Release Date: 2019Document1 pageLung RADS® Version 1.1: Assessment Categories Release Date: 2019S Francisco MotNo ratings yet
- Pentax Medical & Hitachi Endobronchial Ultrasound Mini Atlas - Case StudiesDocument15 pagesPentax Medical & Hitachi Endobronchial Ultrasound Mini Atlas - Case StudiesdodyNo ratings yet
- Triple Negative Breast Cancer, Experience of Military Hospital Rabat: About 52 CasesDocument10 pagesTriple Negative Breast Cancer, Experience of Military Hospital Rabat: About 52 CasesIJAR JOURNALNo ratings yet
- Lung Disease Prediction System Using Naive Bayes and K Means ClusteringDocument36 pagesLung Disease Prediction System Using Naive Bayes and K Means ClusteringMohammad FarhanNo ratings yet
- Chest Surgery DelhiDocument3 pagesChest Surgery DelhiAnonymous OrzzzvmnnDNo ratings yet
- 27 de On Vao 10 deDocument77 pages27 de On Vao 10 deNguyen ManhNo ratings yet
- JeremyDocument2 pagesJeremyManjuNo ratings yet