Professional Documents
Culture Documents
Chronic Pain Management Fact Sheet
Chronic Pain Management Fact Sheet
Uploaded by
AdvaMedLCICopyright:
Available Formats
You might also like
- 30day Crossliftr Kettle-Bell Guide 2021 UpdateDocument43 pages30day Crossliftr Kettle-Bell Guide 2021 UpdateRandom EmailNo ratings yet
- MOH DHA HAAD Dental Study Material Part 2Document33 pagesMOH DHA HAAD Dental Study Material Part 2Junaid Ramzan89% (38)
- Neuroimaging Clinics of North America 2015 #2 PDFDocument173 pagesNeuroimaging Clinics of North America 2015 #2 PDFYully gunawan100% (1)
- Community Health Nursing Course PlanDocument14 pagesCommunity Health Nursing Course PlanPriya Sharma90% (10)
- Artikel Pain MenegementDocument19 pagesArtikel Pain Menegementrizki heriyadiNo ratings yet
- Tick 2018Document69 pagesTick 2018aliNo ratings yet
- Chronic Pain Relief Comprehensive Pain ManagementDocument3 pagesChronic Pain Relief Comprehensive Pain ManagementdracoscribdNo ratings yet
- Pain - National Cancer InstituteDocument91 pagesPain - National Cancer InstituteCarlos ArbeláezNo ratings yet
- Literature Review Chronic PainDocument7 pagesLiterature Review Chronic Painpnquihcnd100% (1)
- Chapter 005Document4 pagesChapter 005Natalia Page TrevinoNo ratings yet
- Comprehensive Pain Rehabilitation Center: Program GuideDocument16 pagesComprehensive Pain Rehabilitation Center: Program Guideniko4eyesNo ratings yet
- Who Analgesic LadderDocument55 pagesWho Analgesic LadderSyifa Nurul Asma'No ratings yet
- Articulo Journal of American Board of Family Medicine 2000Document8 pagesArticulo Journal of American Board of Family Medicine 2000cabusta111No ratings yet
- Managing PostoperativeDocument9 pagesManaging PostoperativeWardah Fauziah El SofwanNo ratings yet
- Management of Chronic Pain in Older Adults: Abdo, Delal AliDocument4 pagesManagement of Chronic Pain in Older Adults: Abdo, Delal Alidalia100% (1)
- Pain ManagementDocument9 pagesPain Managementapi-655053476No ratings yet
- Principles of Palliative Care and Pain ControlDocument12 pagesPrinciples of Palliative Care and Pain ControlvabcunhaNo ratings yet
- Nursing Care Plan and Diagnosis For Substance AbuseDocument87 pagesNursing Care Plan and Diagnosis For Substance AbuseZohrahLiaqatNo ratings yet
- Integrative Pain ManagementDocument18 pagesIntegrative Pain ManagementSarah Coelho HoraNo ratings yet
- An Approach To Chronic Pain in Primary Care - Schneiderhan - 0Document47 pagesAn Approach To Chronic Pain in Primary Care - Schneiderhan - 0Saliu Abdulrahman IremideNo ratings yet
- 7 - PainDocument22 pages7 - Painسلطان محمد فوزي سلمانNo ratings yet
- AIN Anagement: Christine K. O'NeilDocument14 pagesAIN Anagement: Christine K. O'NeilbencleeseNo ratings yet
- Pain AssessmentDocument11 pagesPain AssessmentSuvadip MaityNo ratings yet
- Thesis Rough DraftDocument42 pagesThesis Rough Draftapi-457509028100% (1)
- JPM 10 00027Document9 pagesJPM 10 00027Kepompong KupukupuNo ratings yet
- The Politics of PainDocument11 pagesThe Politics of Painmbx47No ratings yet
- Pain AssessentDocument9 pagesPain AssessentJoanna RachelNo ratings yet
- 2reconsidering Opioid Therapy Mar 2013Document6 pages2reconsidering Opioid Therapy Mar 2013Anonymous 4txA8N8etNo ratings yet
- Pain Management GuidelinesDocument3 pagesPain Management GuidelinesMr. BamsNo ratings yet
- Cancer PainDocument12 pagesCancer Painsaranya.tNo ratings yet
- 8 Chronic Pain ManagementDocument14 pages8 Chronic Pain ManagementEndang Dwi KurniaNo ratings yet
- 8:30-9:10 Final Exam Review 9:10-9:20 Break 9:20-10:00 Trauma Survivor Interview 10:00-10:10 BreakDocument37 pages8:30-9:10 Final Exam Review 9:10-9:20 Break 9:20-10:00 Trauma Survivor Interview 10:00-10:10 Breakchrisx1396No ratings yet
- CSP Physiotherapy Works MSK June 2013Document2 pagesCSP Physiotherapy Works MSK June 2013WasemBhatNo ratings yet
- Bonakar 2017Document18 pagesBonakar 2017Luis Alberto Caneo VergaraNo ratings yet
- Babington 2020Document9 pagesBabington 2020Jessica CampoNo ratings yet
- Chapter 17. Improving The Quality of Care Through Pain Assessment and ManagementDocument30 pagesChapter 17. Improving The Quality of Care Through Pain Assessment and ManagementNur MiladiyahNo ratings yet
- Pain Management Research PaperDocument6 pagesPain Management Research Paperafnhbijlzdufjj100% (1)
- C Chew Graham - Pain Assessment and Pain Treatment For Community Dwelling People With Dementia...Document29 pagesC Chew Graham - Pain Assessment and Pain Treatment For Community Dwelling People With Dementia...jody F.HNo ratings yet
- Pharmacological Manage of Persistent Pain Older 1Document22 pagesPharmacological Manage of Persistent Pain Older 1Borja Carreño MarambioNo ratings yet
- Art Dolor GeriátricoDocument9 pagesArt Dolor GeriátricoarrlyNo ratings yet
- Jurnal Sosbud AgungDocument7 pagesJurnal Sosbud Agungalfin azhariNo ratings yet
- Introduction To PainDocument21 pagesIntroduction To Painayanle Abdi AliNo ratings yet
- Postoperative Pain Management - ESRA GuidelinesDocument34 pagesPostoperative Pain Management - ESRA GuidelinesAlex Apsokardos100% (1)
- Thomas 2017Document8 pagesThomas 2017Uswatun HasanahNo ratings yet
- Oxycontin KOL Slide FINALDocument107 pagesOxycontin KOL Slide FINALEznal MahidinNo ratings yet
- Integrative Medicine and Patient Centered Care PDFDocument35 pagesIntegrative Medicine and Patient Centered Care PDFCristobal Carrasco100% (1)
- PAMI Basic Principles of Pain Management FinalDocument130 pagesPAMI Basic Principles of Pain Management FinalJisaNo ratings yet
- Integrated Therapeutics IiiDocument21 pagesIntegrated Therapeutics IiiSalahadinNo ratings yet
- Pecial Eport: T ABC M PDocument19 pagesPecial Eport: T ABC M PSergio A. MeloNo ratings yet
- Guidelines For Regenerative Injection Therapy RIT Utilizing Platelet Rich Plasma PRP. Revised February 1 2014 Doc. AutosavedDocument28 pagesGuidelines For Regenerative Injection Therapy RIT Utilizing Platelet Rich Plasma PRP. Revised February 1 2014 Doc. AutosavedHüseyin GündüzNo ratings yet
- Telecare Collaborative Management of Chronic Pain in PrimaryDocument9 pagesTelecare Collaborative Management of Chronic Pain in PrimaryJared WebbNo ratings yet
- Concept MapDocument6 pagesConcept Mapmenickel3100% (1)
- Unit 5 Healthcare_240427_102550Document9 pagesUnit 5 Healthcare_240427_102550t7n48cd5zqNo ratings yet
- Challenges To Treatment of Chronic Pain and Addiction During The Bopioid CrisisDocument3 pagesChallenges To Treatment of Chronic Pain and Addiction During The Bopioid CrisisamalfgaribNo ratings yet
- P AcutepainmgmtDocument5 pagesP AcutepainmgmtLeticia Quiñonez VivasNo ratings yet
- PAMI Module 6 Prehospital Pain ManagementDocument135 pagesPAMI Module 6 Prehospital Pain ManagementMeena CtNo ratings yet
- Detox of The Opiate Dependent Pain Patient and Ongoing Pain Control No Diag 12 13 08Document14 pagesDetox of The Opiate Dependent Pain Patient and Ongoing Pain Control No Diag 12 13 08Rick Chavez, M.D.100% (1)
- RH Palliative Care FsDocument2 pagesRH Palliative Care FsPhilo NabisawaNo ratings yet
- Chemotherapy GuideDocument79 pagesChemotherapy GuidePrincess AglibutNo ratings yet
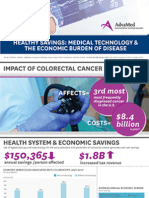
- Infographic: IMPACT OF HEART DISEASEDocument1 pageInfographic: IMPACT OF HEART DISEASEAdvaMedLCINo ratings yet
- Infographic: IMPACT OF COLORECTAL CANCERDocument1 pageInfographic: IMPACT OF COLORECTAL CANCERAdvaMedLCINo ratings yet
- LCI Wound Treatment Toolkit 2015Document8 pagesLCI Wound Treatment Toolkit 2015AdvaMedLCINo ratings yet
- 2015 Innovation AgendaDocument1 page2015 Innovation AgendaAdvaMedLCINo ratings yet
- The Anatomy of Medical ResearchDocument16 pagesThe Anatomy of Medical ResearchAdvaMedLCI0% (1)
- Innovation Agenda: February 2015Document4 pagesInnovation Agenda: February 2015AdvaMedLCINo ratings yet
- Pulse Redefining Medical Technology InnovationDocument64 pagesPulse Redefining Medical Technology InnovationAdvaMedLCINo ratings yet
- Oct 2012 King Report FINALDocument16 pagesOct 2012 King Report FINALAdvaMedLCINo ratings yet
- Innovation Scorecard - Report FINAL - External UNSECUREDDocument50 pagesInnovation Scorecard - Report FINAL - External UNSECUREDAdvaMedLCINo ratings yet
- QuizDocument16 pagesQuizAmy Ramirez100% (1)
- 1) MDH-SingaporeDocument2 pages1) MDH-SingaporeTERAS HYDRANo ratings yet
- Dedication: Oral Maxillofacial Surg Clin N Am 20 (2008) XiiiDocument1 pageDedication: Oral Maxillofacial Surg Clin N Am 20 (2008) XiiiГулпе АлексейNo ratings yet
- Activity-Sheets ParaydayDocument2 pagesActivity-Sheets ParaydayJohn Vincent ParaydayNo ratings yet
- Libro de Endocrino y FertilidadDocument684 pagesLibro de Endocrino y FertilidadClaudia Mercedes Alonso Cuevas100% (1)
- Fikadu MirutsDocument58 pagesFikadu MirutsTenbite ErmiasNo ratings yet
- Marriage - Fertility and Births HandoutDocument1 pageMarriage - Fertility and Births Handoutuntung jakaNo ratings yet
- Brigada EskwelaDocument133 pagesBrigada EskwelaMay Anne AlmarioNo ratings yet
- CeftriaxoneDocument2 pagesCeftriaxoneFlora Angeli PastoresNo ratings yet
- Justin Acala: EducationDocument2 pagesJustin Acala: Educationapi-507064816No ratings yet
- PHE Lesson 2Document7 pagesPHE Lesson 2Via Mae VirtousaNo ratings yet
- Evidence Based Data in Hand Surgery and TherapyDocument638 pagesEvidence Based Data in Hand Surgery and TherapyMochammad Syarif Hidayat100% (1)
- AbcDocument4 pagesAbcAquinnaNo ratings yet
- A Dissection of Health Care ReformDocument10 pagesA Dissection of Health Care ReformLinda de Sosa100% (1)
- Giorgi Khakhutaishvili - English B2-2 PresentationDocument8 pagesGiorgi Khakhutaishvili - English B2-2 PresentationGiorgi KhakhutaishviliNo ratings yet
- Bingli 1Document5 pagesBingli 1Indah T.INo ratings yet
- Overview of The Postpartum Period - Normal Physiology and Routine Maternal Care - UpToDateDocument33 pagesOverview of The Postpartum Period - Normal Physiology and Routine Maternal Care - UpToDateTrần Ngọc BíchNo ratings yet
- MicrobiologyDocument26 pagesMicrobiologyHemadevi Karunakaran100% (1)
- Public Health Dentistry Thesis TopicsDocument5 pagesPublic Health Dentistry Thesis Topicss0kuzej0byn2100% (2)
- Board Exam 1Document18 pagesBoard Exam 1Kira100% (3)
- Role of Social Workers in RehabilitationDocument45 pagesRole of Social Workers in RehabilitationPatie N Tome100% (2)
- Novilyn C. Pataray BSN - Ii Otitis Media: St. Paul College of Ilocos SurDocument1 pageNovilyn C. Pataray BSN - Ii Otitis Media: St. Paul College of Ilocos SurCharina AubreyNo ratings yet
- And The Tooth CrackedDocument20 pagesAnd The Tooth Crackedpablogdv956No ratings yet
- To: All Employees From: The School Principal Subject: Covid-19 Guidelines in Maintaining Safe School Operations DATE: MAY 26, 2020Document1 pageTo: All Employees From: The School Principal Subject: Covid-19 Guidelines in Maintaining Safe School Operations DATE: MAY 26, 2020Irene DulayNo ratings yet
- A Study to Assess the Knowledge Regarding Needle Stick Injuries among Staff Nurses in Selected Hospitals at Bangalore with a View to Develop an Information Booklet on Prevention of Needle Stick InjuriesDocument3 pagesA Study to Assess the Knowledge Regarding Needle Stick Injuries among Staff Nurses in Selected Hospitals at Bangalore with a View to Develop an Information Booklet on Prevention of Needle Stick InjuriesInternational Journal of Innovative Science and Research Technology100% (1)
- Emergency PreparednessDocument14 pagesEmergency PreparednessV Subramanyam QCNo ratings yet
Chronic Pain Management Fact Sheet
Chronic Pain Management Fact Sheet
Uploaded by
AdvaMedLCICopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Chronic Pain Management Fact Sheet
Chronic Pain Management Fact Sheet
Uploaded by
AdvaMedLCICopyright:
Available Formats
Chronic Pain Management
The Value of Medical Technology
Pain is the number one reason that patients access the health care system.
Cases of chronic pain are the leading cause of adult disability in the United
States.1 Chronic pain also adversely affects mental and emotional well-being.2
The Impact of Chronic Pain
One in three Americans suffers from chronic pain.
40 percent of Americans experience daily pain.
Chronic pain costs up to $635 billion each year in medical
treatment and lost productivity.3
The U.S. Department of Health and
Human Services has issued the National
Pain Strategy, a comprehensive national
plan to address chronic pain as a
complex disease. It calls for:
More awareness of pain treatment
options and their risks
Improved patient and provider
access to a larger range of pain
treatment options
Improved care through increased
research
Better provider education and
training about pain management6
Managing Chronic Pain
Chronic pain has traditionally been managed through physical therapy, the
use of over-the-counter pain medication, or the use of prescription opioids.4
Long-term use of opioids can result in the need for escalating doses, and
increases the risk of physical dependence, immune and hormone system
dysfunction, and overdose.5
Medical Technology and Chronic Pain
Medical technology can provide solutions to managing chronic pain that can lessen a patients use of opioids
and other oral pain medications, and improve quality of life.7 These solutions target the source of pain.
Medical technologies that can help manage chronic pain include:
Spinal Cord Stimulators (SCS)
Use electrical signals to block pain signals from reaching the brain.
The system is minimally invasive and is trialed for efficacy before a patient receives a permanent implant.
Covered by Medicare and most commercial health insurance plans.
Patients who use SCS have reported a 50 percent or greater reduction in pain, improving quality of life
and reducing disability.8
Neuroablation
Uses minimally invasive surgery to heat up a small area of nerve or tissue, blocking pain signals traveling
from the pain area to the brain.
Can be performed as an outpatient procedure and usually does not require general anesthesia.
Implantable Drug Pumps
Deliver pain medication directly to the fluid surrounding the spinal cord.
Reduce the amount of opioids needed to relieve pain.9
Diagnostic Tests
Monitor pain medication use, helping assure the appropriate treatment for patients who can be helped
by medications.
Eliminate or significantly curtail opioid abuse.10
1.
Institute of Medicine. Relieving Pain in America: A Blueprint for Transforming Prevention,
Care, Education, and Research. National Academies Press, 2011.
2.
American Chronic Pain Association. ACPA Resource Guide To Chronic Pain Medication &
Treatment. 2015.
3.
Institute of Medicine, Relieving Pain in America.
4.
ACPA, Resource Guide To Chronic Pain Medication & Treatment.
5.
Dowell D, Haegerich TM, Chou R. CDC Guideline for Prescribing Opioids for Chronic Pain
United States, 2016. MMWR Recomm Rep 2016;65:149.
http://dx.doi.org/10.15585/mmwr.rr6501e1.
6.
US Department of Health and Human Services. National Pain Strategy. 2016.
https://iprcc.nih.gov/docs/HHSNational_Pain_Strategy.pdf.
7.
ACPA, Resource Guide To Chronic Pain Medication & Treatment.
8.
International Neuromodulation Society. Neurostimulation lowers need for opioids in
chronic pain. ScienceDaily, 2013.
www.sciencedaily.com/releases/2013/06/130610084019.htm.
9.
Hamza M, Doleys D, Wells M, et al. Prospective study of 3-year follow-up of lowdose
intrathecal opioids in the management of chronic nonmalignant pain. Pain Med.
2012;13:1304-1313.
10.
Milone MC. Laboratory Testing for Prescription Opioids. Journal of Medical Toxicology.
2012;8(4):408-416. doi:10.1007/s13181-012-0274-7.
You might also like
- 30day Crossliftr Kettle-Bell Guide 2021 UpdateDocument43 pages30day Crossliftr Kettle-Bell Guide 2021 UpdateRandom EmailNo ratings yet
- MOH DHA HAAD Dental Study Material Part 2Document33 pagesMOH DHA HAAD Dental Study Material Part 2Junaid Ramzan89% (38)
- Neuroimaging Clinics of North America 2015 #2 PDFDocument173 pagesNeuroimaging Clinics of North America 2015 #2 PDFYully gunawan100% (1)
- Community Health Nursing Course PlanDocument14 pagesCommunity Health Nursing Course PlanPriya Sharma90% (10)
- Artikel Pain MenegementDocument19 pagesArtikel Pain Menegementrizki heriyadiNo ratings yet
- Tick 2018Document69 pagesTick 2018aliNo ratings yet
- Chronic Pain Relief Comprehensive Pain ManagementDocument3 pagesChronic Pain Relief Comprehensive Pain ManagementdracoscribdNo ratings yet
- Pain - National Cancer InstituteDocument91 pagesPain - National Cancer InstituteCarlos ArbeláezNo ratings yet
- Literature Review Chronic PainDocument7 pagesLiterature Review Chronic Painpnquihcnd100% (1)
- Chapter 005Document4 pagesChapter 005Natalia Page TrevinoNo ratings yet
- Comprehensive Pain Rehabilitation Center: Program GuideDocument16 pagesComprehensive Pain Rehabilitation Center: Program Guideniko4eyesNo ratings yet
- Who Analgesic LadderDocument55 pagesWho Analgesic LadderSyifa Nurul Asma'No ratings yet
- Articulo Journal of American Board of Family Medicine 2000Document8 pagesArticulo Journal of American Board of Family Medicine 2000cabusta111No ratings yet
- Managing PostoperativeDocument9 pagesManaging PostoperativeWardah Fauziah El SofwanNo ratings yet
- Management of Chronic Pain in Older Adults: Abdo, Delal AliDocument4 pagesManagement of Chronic Pain in Older Adults: Abdo, Delal Alidalia100% (1)
- Pain ManagementDocument9 pagesPain Managementapi-655053476No ratings yet
- Principles of Palliative Care and Pain ControlDocument12 pagesPrinciples of Palliative Care and Pain ControlvabcunhaNo ratings yet
- Nursing Care Plan and Diagnosis For Substance AbuseDocument87 pagesNursing Care Plan and Diagnosis For Substance AbuseZohrahLiaqatNo ratings yet
- Integrative Pain ManagementDocument18 pagesIntegrative Pain ManagementSarah Coelho HoraNo ratings yet
- An Approach To Chronic Pain in Primary Care - Schneiderhan - 0Document47 pagesAn Approach To Chronic Pain in Primary Care - Schneiderhan - 0Saliu Abdulrahman IremideNo ratings yet
- 7 - PainDocument22 pages7 - Painسلطان محمد فوزي سلمانNo ratings yet
- AIN Anagement: Christine K. O'NeilDocument14 pagesAIN Anagement: Christine K. O'NeilbencleeseNo ratings yet
- Pain AssessmentDocument11 pagesPain AssessmentSuvadip MaityNo ratings yet
- Thesis Rough DraftDocument42 pagesThesis Rough Draftapi-457509028100% (1)
- JPM 10 00027Document9 pagesJPM 10 00027Kepompong KupukupuNo ratings yet
- The Politics of PainDocument11 pagesThe Politics of Painmbx47No ratings yet
- Pain AssessentDocument9 pagesPain AssessentJoanna RachelNo ratings yet
- 2reconsidering Opioid Therapy Mar 2013Document6 pages2reconsidering Opioid Therapy Mar 2013Anonymous 4txA8N8etNo ratings yet
- Pain Management GuidelinesDocument3 pagesPain Management GuidelinesMr. BamsNo ratings yet
- Cancer PainDocument12 pagesCancer Painsaranya.tNo ratings yet
- 8 Chronic Pain ManagementDocument14 pages8 Chronic Pain ManagementEndang Dwi KurniaNo ratings yet
- 8:30-9:10 Final Exam Review 9:10-9:20 Break 9:20-10:00 Trauma Survivor Interview 10:00-10:10 BreakDocument37 pages8:30-9:10 Final Exam Review 9:10-9:20 Break 9:20-10:00 Trauma Survivor Interview 10:00-10:10 Breakchrisx1396No ratings yet
- CSP Physiotherapy Works MSK June 2013Document2 pagesCSP Physiotherapy Works MSK June 2013WasemBhatNo ratings yet
- Bonakar 2017Document18 pagesBonakar 2017Luis Alberto Caneo VergaraNo ratings yet
- Babington 2020Document9 pagesBabington 2020Jessica CampoNo ratings yet
- Chapter 17. Improving The Quality of Care Through Pain Assessment and ManagementDocument30 pagesChapter 17. Improving The Quality of Care Through Pain Assessment and ManagementNur MiladiyahNo ratings yet
- Pain Management Research PaperDocument6 pagesPain Management Research Paperafnhbijlzdufjj100% (1)
- C Chew Graham - Pain Assessment and Pain Treatment For Community Dwelling People With Dementia...Document29 pagesC Chew Graham - Pain Assessment and Pain Treatment For Community Dwelling People With Dementia...jody F.HNo ratings yet
- Pharmacological Manage of Persistent Pain Older 1Document22 pagesPharmacological Manage of Persistent Pain Older 1Borja Carreño MarambioNo ratings yet
- Art Dolor GeriátricoDocument9 pagesArt Dolor GeriátricoarrlyNo ratings yet
- Jurnal Sosbud AgungDocument7 pagesJurnal Sosbud Agungalfin azhariNo ratings yet
- Introduction To PainDocument21 pagesIntroduction To Painayanle Abdi AliNo ratings yet
- Postoperative Pain Management - ESRA GuidelinesDocument34 pagesPostoperative Pain Management - ESRA GuidelinesAlex Apsokardos100% (1)
- Thomas 2017Document8 pagesThomas 2017Uswatun HasanahNo ratings yet
- Oxycontin KOL Slide FINALDocument107 pagesOxycontin KOL Slide FINALEznal MahidinNo ratings yet
- Integrative Medicine and Patient Centered Care PDFDocument35 pagesIntegrative Medicine and Patient Centered Care PDFCristobal Carrasco100% (1)
- PAMI Basic Principles of Pain Management FinalDocument130 pagesPAMI Basic Principles of Pain Management FinalJisaNo ratings yet
- Integrated Therapeutics IiiDocument21 pagesIntegrated Therapeutics IiiSalahadinNo ratings yet
- Pecial Eport: T ABC M PDocument19 pagesPecial Eport: T ABC M PSergio A. MeloNo ratings yet
- Guidelines For Regenerative Injection Therapy RIT Utilizing Platelet Rich Plasma PRP. Revised February 1 2014 Doc. AutosavedDocument28 pagesGuidelines For Regenerative Injection Therapy RIT Utilizing Platelet Rich Plasma PRP. Revised February 1 2014 Doc. AutosavedHüseyin GündüzNo ratings yet
- Telecare Collaborative Management of Chronic Pain in PrimaryDocument9 pagesTelecare Collaborative Management of Chronic Pain in PrimaryJared WebbNo ratings yet
- Concept MapDocument6 pagesConcept Mapmenickel3100% (1)
- Unit 5 Healthcare_240427_102550Document9 pagesUnit 5 Healthcare_240427_102550t7n48cd5zqNo ratings yet
- Challenges To Treatment of Chronic Pain and Addiction During The Bopioid CrisisDocument3 pagesChallenges To Treatment of Chronic Pain and Addiction During The Bopioid CrisisamalfgaribNo ratings yet
- P AcutepainmgmtDocument5 pagesP AcutepainmgmtLeticia Quiñonez VivasNo ratings yet
- PAMI Module 6 Prehospital Pain ManagementDocument135 pagesPAMI Module 6 Prehospital Pain ManagementMeena CtNo ratings yet
- Detox of The Opiate Dependent Pain Patient and Ongoing Pain Control No Diag 12 13 08Document14 pagesDetox of The Opiate Dependent Pain Patient and Ongoing Pain Control No Diag 12 13 08Rick Chavez, M.D.100% (1)
- RH Palliative Care FsDocument2 pagesRH Palliative Care FsPhilo NabisawaNo ratings yet
- Chemotherapy GuideDocument79 pagesChemotherapy GuidePrincess AglibutNo ratings yet
- Infographic: IMPACT OF HEART DISEASEDocument1 pageInfographic: IMPACT OF HEART DISEASEAdvaMedLCINo ratings yet
- Infographic: IMPACT OF COLORECTAL CANCERDocument1 pageInfographic: IMPACT OF COLORECTAL CANCERAdvaMedLCINo ratings yet
- LCI Wound Treatment Toolkit 2015Document8 pagesLCI Wound Treatment Toolkit 2015AdvaMedLCINo ratings yet
- 2015 Innovation AgendaDocument1 page2015 Innovation AgendaAdvaMedLCINo ratings yet
- The Anatomy of Medical ResearchDocument16 pagesThe Anatomy of Medical ResearchAdvaMedLCI0% (1)
- Innovation Agenda: February 2015Document4 pagesInnovation Agenda: February 2015AdvaMedLCINo ratings yet
- Pulse Redefining Medical Technology InnovationDocument64 pagesPulse Redefining Medical Technology InnovationAdvaMedLCINo ratings yet
- Oct 2012 King Report FINALDocument16 pagesOct 2012 King Report FINALAdvaMedLCINo ratings yet
- Innovation Scorecard - Report FINAL - External UNSECUREDDocument50 pagesInnovation Scorecard - Report FINAL - External UNSECUREDAdvaMedLCINo ratings yet
- QuizDocument16 pagesQuizAmy Ramirez100% (1)
- 1) MDH-SingaporeDocument2 pages1) MDH-SingaporeTERAS HYDRANo ratings yet
- Dedication: Oral Maxillofacial Surg Clin N Am 20 (2008) XiiiDocument1 pageDedication: Oral Maxillofacial Surg Clin N Am 20 (2008) XiiiГулпе АлексейNo ratings yet
- Activity-Sheets ParaydayDocument2 pagesActivity-Sheets ParaydayJohn Vincent ParaydayNo ratings yet
- Libro de Endocrino y FertilidadDocument684 pagesLibro de Endocrino y FertilidadClaudia Mercedes Alonso Cuevas100% (1)
- Fikadu MirutsDocument58 pagesFikadu MirutsTenbite ErmiasNo ratings yet
- Marriage - Fertility and Births HandoutDocument1 pageMarriage - Fertility and Births Handoutuntung jakaNo ratings yet
- Brigada EskwelaDocument133 pagesBrigada EskwelaMay Anne AlmarioNo ratings yet
- CeftriaxoneDocument2 pagesCeftriaxoneFlora Angeli PastoresNo ratings yet
- Justin Acala: EducationDocument2 pagesJustin Acala: Educationapi-507064816No ratings yet
- PHE Lesson 2Document7 pagesPHE Lesson 2Via Mae VirtousaNo ratings yet
- Evidence Based Data in Hand Surgery and TherapyDocument638 pagesEvidence Based Data in Hand Surgery and TherapyMochammad Syarif Hidayat100% (1)
- AbcDocument4 pagesAbcAquinnaNo ratings yet
- A Dissection of Health Care ReformDocument10 pagesA Dissection of Health Care ReformLinda de Sosa100% (1)
- Giorgi Khakhutaishvili - English B2-2 PresentationDocument8 pagesGiorgi Khakhutaishvili - English B2-2 PresentationGiorgi KhakhutaishviliNo ratings yet
- Bingli 1Document5 pagesBingli 1Indah T.INo ratings yet
- Overview of The Postpartum Period - Normal Physiology and Routine Maternal Care - UpToDateDocument33 pagesOverview of The Postpartum Period - Normal Physiology and Routine Maternal Care - UpToDateTrần Ngọc BíchNo ratings yet
- MicrobiologyDocument26 pagesMicrobiologyHemadevi Karunakaran100% (1)
- Public Health Dentistry Thesis TopicsDocument5 pagesPublic Health Dentistry Thesis Topicss0kuzej0byn2100% (2)
- Board Exam 1Document18 pagesBoard Exam 1Kira100% (3)
- Role of Social Workers in RehabilitationDocument45 pagesRole of Social Workers in RehabilitationPatie N Tome100% (2)
- Novilyn C. Pataray BSN - Ii Otitis Media: St. Paul College of Ilocos SurDocument1 pageNovilyn C. Pataray BSN - Ii Otitis Media: St. Paul College of Ilocos SurCharina AubreyNo ratings yet
- And The Tooth CrackedDocument20 pagesAnd The Tooth Crackedpablogdv956No ratings yet
- To: All Employees From: The School Principal Subject: Covid-19 Guidelines in Maintaining Safe School Operations DATE: MAY 26, 2020Document1 pageTo: All Employees From: The School Principal Subject: Covid-19 Guidelines in Maintaining Safe School Operations DATE: MAY 26, 2020Irene DulayNo ratings yet
- A Study to Assess the Knowledge Regarding Needle Stick Injuries among Staff Nurses in Selected Hospitals at Bangalore with a View to Develop an Information Booklet on Prevention of Needle Stick InjuriesDocument3 pagesA Study to Assess the Knowledge Regarding Needle Stick Injuries among Staff Nurses in Selected Hospitals at Bangalore with a View to Develop an Information Booklet on Prevention of Needle Stick InjuriesInternational Journal of Innovative Science and Research Technology100% (1)
- Emergency PreparednessDocument14 pagesEmergency PreparednessV Subramanyam QCNo ratings yet