Professional Documents
Culture Documents
Acute Management Hipercianotic Spells
Acute Management Hipercianotic Spells
Uploaded by
Sigit Sutanto0 ratings0% found this document useful (0 votes)
65 views2 pagescyanotic spell
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Documentcyanotic spell
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Download as docx, pdf, or txt
0 ratings0% found this document useful (0 votes)
65 views2 pagesAcute Management Hipercianotic Spells
Acute Management Hipercianotic Spells
Uploaded by
Sigit Sutantocyanotic spell
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Download as docx, pdf, or txt
You are on page 1of 2
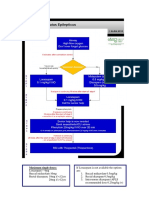
Acute Management
A hypercyanotic attack is a medical emergency and requires prompt
management to break the hypoxic cycle.
Call for help early and inform the cardiologist in charge.
Depending on the severity of attack, institute one or more of the following.
Try to calm the infant.
Have the parent hold the infant over the parents shoulder, or place the child in a
knee-chest position.
Administration of oxygen (although this will not reverse cyanosis due to
intracardiac shunting). Avoid if such attempts further aggravate the child.
Drugs (in order or preference, unless contraindicated)
IV sodium bicarbonate is necessary to correct metabolic acidosis. The
dosage is 1-2 meq/kg as 1-2 ml/kg of 8.4% NaHCO3 slow IV bolus. For infants less
than 3 months of age, administer as 4.2% NaHCO3 (dilute the 8.4% NaHCO3 1:1 with
normal saline). Ensure the intravenous access is secure before administration as
extravasation can lead to severe tissue injury.
-adrenergic blockade with intravenous propranolol (0.15 - 0.25
mg/kg given slowly over 5 - 10 minutes; dose can be repeated once). In the acute
attack, propranolol slows the heart rate and reduces the right ventricular outflow
obstruction; it also has a sedative effect. IV Esmolol (0.5 mg/kg over 1 minute and can
be given as an infusion at 50 mcg/kg/min) is an alternative.
o
-agonists: phenylephrine (0.1 mg/kg SC or IM, 0.01 mg/kg IV, or as an
infusion 0.1 - 0.5 mcg/kg/min) or metaraminol (Aramine)(0.01 mg/kg IV and repeated
PRN, can be given as an infusion 0.1-1.0 mcg/kg/min), increases systemic vascular
resistance (SVR) and reduces right to left shunting.
Ketamine (1-2 mg/kg IV or 5-10 mg/kg IM) is a drug, which
simultaneously increases the SVR, sedates the patient. Both effects are known to
terminate the spell.
Morphine (0.1 mg/kg IV or SC). Mechanism of action is via suppression of
the respiratory centre and abolishing hyperpnoea. However, its disadvantages include
slow onset and respiratory depression. Be ready to intubate.
Ventilatory support if necessary.
General anaesthesia or emergency Blalock-Taussig shunt in intractable cases.
Maintenance therapy
Propranolol and sedation as required.
Propranolol acts by its peripheral actions of stabilizing the reactivity of the
systemic arteries, thereby preventing a sudden decrease in the systemic vascular
resistance. Oral dose is 0.2-0.5 mg/kg/dose 6-12 hourly, and can be slowly increased to
maximum of 1 mg/kg/dose 6 hourly as needed.
Sedation may be with chloral hydrate or diazepam. However, avoid midazolam,
which reduces systemic vascular resistance further.
Treat fever aggressively and ensure adequate hydration.
Avoid epinephrine, dopamine, dobutamine, digitalis, and digoxin, which have
positive inotropic effects and may therefore, worsen Tet spells.
You might also like
- Prof DR Amit Gupta AITSC Trauma Registry & Trauma Quality Improvement in IndiaDocument77 pagesProf DR Amit Gupta AITSC Trauma Registry & Trauma Quality Improvement in IndiaBruno67% (3)
- Endocrine Anesthesia MCQsDocument18 pagesEndocrine Anesthesia MCQsMuhammad Aasim Maan100% (2)
- 05 IV Induction Agents PDFDocument0 pages05 IV Induction Agents PDFjuniorebinda100% (1)
- Naplex Complete Study Outline A Topic-Wise Approach DiabetesFrom EverandNaplex Complete Study Outline A Topic-Wise Approach DiabetesRating: 4 out of 5 stars4/5 (3)
- B 10 Ctsta 831Document6 pagesB 10 Ctsta 831Andhi Soesilo100% (1)
- Auto PEEPDocument9 pagesAuto PEEPJoãoBrasil100% (1)
- Facilitate Mechanical Ventilation in Intensive Care: AdultDocument2 pagesFacilitate Mechanical Ventilation in Intensive Care: AdultVaniNo ratings yet
- Anaesthesia Drugs Used CommonlyDocument6 pagesAnaesthesia Drugs Used CommonlyAmar Mahesh KalluNo ratings yet
- Obat Ayu (Anestesi)Document11 pagesObat Ayu (Anestesi)Ayu PratiwiNo ratings yet
- Fentanyl ParenteralDocument7 pagesFentanyl Parenteralstring44No ratings yet
- Drug StudyDocument7 pagesDrug StudydivineNo ratings yet
- Status Epilepticus and ICPDocument9 pagesStatus Epilepticus and ICPjoomds51No ratings yet
- Cloxacillin, Sodium: How Should I Take Cloxacillin?Document7 pagesCloxacillin, Sodium: How Should I Take Cloxacillin?Stacy MC PelitoNo ratings yet
- Status Epilepticus Pediatric DR - RPDocument4 pagesStatus Epilepticus Pediatric DR - RPAdnin NugrohoNo ratings yet
- Antidotes in Clinical Practice SeminarDocument77 pagesAntidotes in Clinical Practice Seminarkhaled eissaNo ratings yet
- Drug StudyDocument5 pagesDrug StudyKristoff CamposNo ratings yet
- Anaphylaxis Anaphylactoid ReactionDocument8 pagesAnaphylaxis Anaphylactoid Reactionsringeri2No ratings yet
- 038 AnaphylaxisDocument5 pages038 AnaphylaxisabbuahmedibbuNo ratings yet
- Epilepsi Status EpileptikusDocument35 pagesEpilepsi Status EpileptikusLussy HendrikNo ratings yet
- Should Be Available at All Sites If Feasible, Include at Sites (Not Required)Document5 pagesShould Be Available at All Sites If Feasible, Include at Sites (Not Required)Ahmed QlhamdNo ratings yet
- Receiving Concurrent Moderate CYP3A4 Inhibitors (Erythromycin, Saquinavir, Verapamil, Fluconazole) - 25 MG Once Daily InitiallyDocument272 pagesReceiving Concurrent Moderate CYP3A4 Inhibitors (Erythromycin, Saquinavir, Verapamil, Fluconazole) - 25 MG Once Daily InitiallyFatima Doran PandaogNo ratings yet
- Drugs Used in AneasthesiaDocument73 pagesDrugs Used in AneasthesiaCabdiladif Ahmed McrfNo ratings yet
- Circulation: Anectine Succinylcholine ChlorideDocument12 pagesCirculation: Anectine Succinylcholine ChlorideJeralyn BugayongNo ratings yet
- Status Epilepticus - APLSDocument3 pagesStatus Epilepticus - APLSMuhammadafif SholehuddinNo ratings yet
- Anasthetic DrugsDocument62 pagesAnasthetic DrugsMilda InayahNo ratings yet
- Lec 4 CNSDocument12 pagesLec 4 CNShusainozelNo ratings yet
- Succinylcholine ChlorideDocument19 pagesSuccinylcholine ChlorideAgungBudiPamungkas100% (1)
- High Alert MedicationsDocument17 pagesHigh Alert MedicationsJoanna Marie Datahan EstomoNo ratings yet
- Pediatric Life SupportDocument33 pagesPediatric Life SupportAndre montolaluNo ratings yet
- Anaphylaxis: How To Recognize, Treat, and Prevent Potentially Fatal AttacksDocument8 pagesAnaphylaxis: How To Recognize, Treat, and Prevent Potentially Fatal AttacksИван Марковић ИскеNo ratings yet
- ASCIA Guidelines Acute Management Anaphylaxis 2017 Updated PDFDocument8 pagesASCIA Guidelines Acute Management Anaphylaxis 2017 Updated PDFAyu WahyuniNo ratings yet
- Atracurium BesylateDocument3 pagesAtracurium BesylateWidya WidyariniNo ratings yet
- 1st Line Medication of An e CartDocument5 pages1st Line Medication of An e CartColette Marie PerezNo ratings yet
- Emergency Drugs Drug StudyDocument15 pagesEmergency Drugs Drug StudyCathrine Sandile Tangwara100% (1)
- Drug StudyDocument34 pagesDrug StudyMarco MoralesNo ratings yet
- Atropine Drug StudyDocument3 pagesAtropine Drug StudyMaej83% (6)
- Farmakologi IntubasiDocument19 pagesFarmakologi IntubasiFANI RUDIYANTI 1No ratings yet
- Milrinone NeomedDocument4 pagesMilrinone NeomedmuarifNo ratings yet
- G CarbamazepineDocument18 pagesG CarbamazepineCLARISSA GRACE GERALDINONo ratings yet
- Seven Ps For RSI BOARDDocument2 pagesSeven Ps For RSI BOARDJames BrownNo ratings yet
- Drug Study On EPINEPHRINEDocument6 pagesDrug Study On EPINEPHRINEshadow gonzalezNo ratings yet
- Drug StudyDocument9 pagesDrug StudyChristine PunsalanNo ratings yet
- AtropinDocument9 pagesAtropinarfitaaaaNo ratings yet
- 6.1 Quick Ref Guide MNGT Antivenom Reactions SGB2021 Ver. 2Document3 pages6.1 Quick Ref Guide MNGT Antivenom Reactions SGB2021 Ver. 2anju sulishaNo ratings yet
- Pediatric General Anesthesia: Moderator-Dr Tripat Kaur. Presenter - DR Ikjot KaurDocument80 pagesPediatric General Anesthesia: Moderator-Dr Tripat Kaur. Presenter - DR Ikjot Kaurashwini priyaNo ratings yet
- TabletsDocument6 pagesTabletsRupesh Kumar DuttaNo ratings yet
- Drug StudyDocument7 pagesDrug StudyJoy Jarin100% (1)
- RSI Pharmacology For The Emergency Medicine PhysicianDocument2 pagesRSI Pharmacology For The Emergency Medicine PhysicianGuide LPNo ratings yet
- Pediatric Drug DosesDocument8 pagesPediatric Drug DosesReview20No ratings yet
- Management of SeizureDocument3 pagesManagement of SeizureNaanthini Dilly KannanNo ratings yet
- Status Epilepticus: DR Abdelmoniem SaeedDocument24 pagesStatus Epilepticus: DR Abdelmoniem SaeedYousef Al-AmeenNo ratings yet
- Neonatal Seizures: Learning ObjectivesDocument6 pagesNeonatal Seizures: Learning ObjectivesSatya Prakash TiwariNo ratings yet
- Neonatal Drugs Section Fifth Edition2012 PDFDocument163 pagesNeonatal Drugs Section Fifth Edition2012 PDFAhmed MohammedNo ratings yet
- ICU Drips: Stephanie Sanderson, RN, MSN, CNS, CCNS, CCRN Medical Cardiac ICU-UNMHDocument32 pagesICU Drips: Stephanie Sanderson, RN, MSN, CNS, CCNS, CCRN Medical Cardiac ICU-UNMHNicole Adkins100% (1)
- Drugs in ObstDocument32 pagesDrugs in ObstĶHwola ƏľsHokryNo ratings yet
- ASCIA Acute Management of Anaphylaxis Guidelines 2015Document4 pagesASCIA Acute Management of Anaphylaxis Guidelines 2015tom8989No ratings yet
- Anzcor Guideline 12 4 Medications and Fluids Aug16Document7 pagesAnzcor Guideline 12 4 Medications and Fluids Aug16flamur haskukajNo ratings yet
- Obat Emergensi Dalam AnestesiDocument32 pagesObat Emergensi Dalam AnestesiNaja NugrahaNo ratings yet
- Drug Study On Emergency DrugsDocument16 pagesDrug Study On Emergency DrugsJosepNo ratings yet
- Emergency DrugsDocument15 pagesEmergency Drugsjheverly123100% (1)
- Status Epilepticus: Kenya Medical Training CollegeDocument21 pagesStatus Epilepticus: Kenya Medical Training CollegeSalman KhanNo ratings yet
- Critical Care Medications: Anti-Arrhythmics Study Guide: Critical Care EssentialsFrom EverandCritical Care Medications: Anti-Arrhythmics Study Guide: Critical Care EssentialsNo ratings yet
- Hypoglycemia, A Simple Guide To The Condition, Treatment And Related ConditionsFrom EverandHypoglycemia, A Simple Guide To The Condition, Treatment And Related ConditionsNo ratings yet
- Komplikasi Pain ManagementDocument60 pagesKomplikasi Pain ManagementSigit SutantoNo ratings yet
- DORVDocument23 pagesDORVSigit SutantoNo ratings yet
- DORVDocument23 pagesDORVSigit SutantoNo ratings yet
- tmd175 Slide Sepsis PDFDocument42 pagestmd175 Slide Sepsis PDFRezky Fitria YandraNo ratings yet
- Normal Uterine InvolutionDocument2 pagesNormal Uterine Involutionapi-273469220100% (1)
- Magnification in EndodonticsDocument15 pagesMagnification in EndodonticsmoatazendoNo ratings yet
- Pendampingan Minum Tablet Tambah Darah T PDFDocument8 pagesPendampingan Minum Tablet Tambah Darah T PDFDeli fitNo ratings yet
- Electrotherapy On The Web - Pulsed Shortwave TherapyDocument10 pagesElectrotherapy On The Web - Pulsed Shortwave Therapyakheel ahammedNo ratings yet
- Drug Study Furosemide and MidazolamDocument2 pagesDrug Study Furosemide and MidazolamCuttie Anne GalangNo ratings yet
- N A B H PDFDocument92 pagesN A B H PDFtapan_tsgNo ratings yet
- Nursing Care Plan For Impaired Environmental Interpretaion NCPDocument4 pagesNursing Care Plan For Impaired Environmental Interpretaion NCPderic100% (2)
- Smile Analysis PDFDocument4 pagesSmile Analysis PDFtikaNo ratings yet
- Water Seal Chest DrainageDocument5 pagesWater Seal Chest DrainageAmadelle FaithNo ratings yet
- Enteral Dosage Forms-Tri Murini (2016) - 2Document48 pagesEnteral Dosage Forms-Tri Murini (2016) - 2RobertOktaChandraNo ratings yet
- Patch Adams 02Document3 pagesPatch Adams 02api-3750171No ratings yet
- Cyproheptadine FinalDocument3 pagesCyproheptadine FinalkaitlynmannNo ratings yet
- Bottle JawDocument35 pagesBottle Jawhansmeet100% (1)
- Congenital Dysplasia of Hip (CDH) Developmental Dysplasia of The Hip (DDH)Document50 pagesCongenital Dysplasia of Hip (CDH) Developmental Dysplasia of The Hip (DDH)NarishaAmeliaNo ratings yet
- Wound Care Management 1Document99 pagesWound Care Management 1Jan Oliver YaresNo ratings yet
- KetorolacDocument2 pagesKetorolacJacqueline LimNo ratings yet
- Summary of Key Points: Tetanus Vaccines: WHO Position Paper - February 2017Document19 pagesSummary of Key Points: Tetanus Vaccines: WHO Position Paper - February 2017rendha sasongkoNo ratings yet
- Thsesis TopicsDocument17 pagesThsesis Topicsvvb_frndNo ratings yet
- Consti 2 Bill of Rights First 52 CasesDocument1 pageConsti 2 Bill of Rights First 52 CasesRolly Herida100% (1)
- Mechanical Ventilation During Anesthesia in Adults - UptoDate 2022Document34 pagesMechanical Ventilation During Anesthesia in Adults - UptoDate 2022Angy KarakostaNo ratings yet
- Temperoray Internal Jugular Catheter (Ijc) For Chronic Hemodialysis PatientsDocument2 pagesTemperoray Internal Jugular Catheter (Ijc) For Chronic Hemodialysis PatientsBobby Chin SinghNo ratings yet
- Chapter 5 - Provider Reimbursement MethodsDocument18 pagesChapter 5 - Provider Reimbursement MethodsAdityaNo ratings yet
- PHOSGENE Incident Management v2Document10 pagesPHOSGENE Incident Management v2djsp5009No ratings yet
- Case DigestDocument5 pagesCase DigestHannah OrosNo ratings yet
- D.R. Immediate Newborn Cord Care FormDocument4 pagesD.R. Immediate Newborn Cord Care FormZebeah Angela Balgos ValdezNo ratings yet
- Misericordia LetterDocument2 pagesMisericordia LetterKatie DangerfieldNo ratings yet