Professional Documents
Culture Documents
Ectopic Pregnancy Journal
Ectopic Pregnancy Journal
Uploaded by
Siska FriedmanCopyright:
Available Formats
You might also like
- Maternal Child Nursing Care in Canada - CH1-28Document2 pagesMaternal Child Nursing Care in Canada - CH1-28Reena Rajcoomar0% (1)
- Step 2 CK Usmle Questions For Ob GynDocument48 pagesStep 2 CK Usmle Questions For Ob Gyniamdonut87% (15)
- Bleeding During Pregnancy and Nursing Care PlanDocument17 pagesBleeding During Pregnancy and Nursing Care PlanLizcelle Bihasa86% (7)
- Ass Ectopic PregnancyDocument10 pagesAss Ectopic PregnancyPriyaNo ratings yet
- Ectopic Pregnancy Kehamilan Luar RahimDocument5 pagesEctopic Pregnancy Kehamilan Luar RahimMuhamad Aminuddin Abu BakarNo ratings yet
- Information For You: An Ectopic PregnancyDocument25 pagesInformation For You: An Ectopic PregnancyAnonymous layszXmsNo ratings yet
- Management of Ectopic PregnancyDocument8 pagesManagement of Ectopic PregnancySulaiman WalizadaNo ratings yet
- Ectopic PregnancyDocument17 pagesEctopic PregnancyB.HemavarshiniNo ratings yet
- Ectopic Pregnancy April 2018 1Document6 pagesEctopic Pregnancy April 2018 1Avindya RarasatiNo ratings yet
- 2022.TP (Ectopic Pregnancy) NOUNSDocument6 pages2022.TP (Ectopic Pregnancy) NOUNSWilson BenitezNo ratings yet
- Uterus: Signs and SymptomsDocument4 pagesUterus: Signs and SymptomsmoigomezNo ratings yet
- Uterus: Signs and SymptomsDocument4 pagesUterus: Signs and SymptomsmoigomezNo ratings yet
- CASE ANALYSIS Ectopic Pregnancy Part 1Document10 pagesCASE ANALYSIS Ectopic Pregnancy Part 1Diane Celine SantianoNo ratings yet
- Uterus: Signs and SymptomsDocument11 pagesUterus: Signs and SymptomsJoy Parallag - BautoNo ratings yet
- Ectopic Pregnancy: Medlineplus TopicsDocument9 pagesEctopic Pregnancy: Medlineplus TopicsJonathan BendecioNo ratings yet
- Pi Ectopic Pregnancy Mar20Document9 pagesPi Ectopic Pregnancy Mar20Aziza TahanyNo ratings yet
- Problems in Early Pregnancy - NBT002073Document8 pagesProblems in Early Pregnancy - NBT002073ElvisNo ratings yet
- ERPC LeafletDocument4 pagesERPC Leafletjoshy221196No ratings yet
- Problems in Early PregnancyDocument11 pagesProblems in Early PregnancyRizal LeonardoNo ratings yet
- What Can I Expect in A Cesarean Procedure?Document7 pagesWhat Can I Expect in A Cesarean Procedure?abbiefayeNo ratings yet
- Ectopic PregnancyDocument4 pagesEctopic PregnancySyahriana AnaNo ratings yet
- Ectopic Pregnancy: Frequently Asked Questions FAQ155 PregnancyDocument2 pagesEctopic Pregnancy: Frequently Asked Questions FAQ155 PregnancyUlfaa MutiaaNo ratings yet
- Early MiscarriageretrjytkuyiulDocument6 pagesEarly MiscarriageretrjytkuyiulMuhammed BarznjiNo ratings yet
- Group 1. An Overview of MiscarriageDocument3 pagesGroup 1. An Overview of MiscarriageAprilia Vivilianotekowador PlantonevliamorNo ratings yet
- Dilation and Curettage - Health TeachingDocument4 pagesDilation and Curettage - Health TeachingGol D. RogerNo ratings yet
- What Is Bilateral Tubal Ligation?Document5 pagesWhat Is Bilateral Tubal Ligation?Janice UbagNo ratings yet
- O&G Counselling - TSPDocument6 pagesO&G Counselling - TSPTarran PhagooNo ratings yet
- AMODIADocument3 pagesAMODIAMarriel AmodiaNo ratings yet
- What Is Bilateral Tubal LigationDocument42 pagesWhat Is Bilateral Tubal LigationAldrich ArquizaNo ratings yet
- 27 Ovarian Cystectomy Consent FormDocument3 pages27 Ovarian Cystectomy Consent FormsekyNo ratings yet
- 11 63 Expectant Management of An Ectopic Pregnancy June 2018Document7 pages11 63 Expectant Management of An Ectopic Pregnancy June 2018Tandyo TriasmoroNo ratings yet
- Vaginal Hysterectomy and Vaginal Repair: Women's ServiceDocument16 pagesVaginal Hysterectomy and Vaginal Repair: Women's Serviceintan yulia safarinaNo ratings yet
- Abortion: Renhe Hospital Wang JunjieDocument51 pagesAbortion: Renhe Hospital Wang JunjieMadhu Sudhan PandeyaNo ratings yet
- Bleeding During Pregnancy and Nursing Care PlanDocument19 pagesBleeding During Pregnancy and Nursing Care PlanJack BangcoyoNo ratings yet
- Endometrial Biopsy and CervicaDocument2 pagesEndometrial Biopsy and CervicaFahmi NugrahaNo ratings yet
- What is Postpartum HemorrhageDocument7 pagesWhat is Postpartum HemorrhageEmerson De SilvaNo ratings yet
- Togdher University Lectural Asma Da, Ud Kahin Class of Midwifery and Nursing Course Title Reproductive HealthDocument18 pagesTogdher University Lectural Asma Da, Ud Kahin Class of Midwifery and Nursing Course Title Reproductive HealthHoodo AhmedNo ratings yet
- Vaginal Bleeding in Early PregnancyDocument8 pagesVaginal Bleeding in Early PregnancyBal Ri Mekoleu100% (1)
- Brief Description: Ectopic PregnancyDocument6 pagesBrief Description: Ectopic PregnancyQueenet BelingonNo ratings yet
- Placenta Abruptio - Topic OverviewDocument8 pagesPlacenta Abruptio - Topic OverviewLei AbellarNo ratings yet
- Spotting in Early Pregnancy - Is It Common, Causes, and Seeing A DoctorDocument9 pagesSpotting in Early Pregnancy - Is It Common, Causes, and Seeing A DoctorlastmadanhireNo ratings yet
- Ovulation Induction and Intra Uterine InseminationDocument4 pagesOvulation Induction and Intra Uterine InseminationmasdipoNo ratings yet
- Vaginal Bleeding in Early PregnancyDocument8 pagesVaginal Bleeding in Early PregnancyRudi LadoNo ratings yet
- What Is An Episiotomy?: Reasons For The ProcedureDocument9 pagesWhat Is An Episiotomy?: Reasons For The ProcedureYusephAwangSanaaniNo ratings yet
- What Is An Episiotomy?: Reasons For The ProcedureDocument11 pagesWhat Is An Episiotomy?: Reasons For The ProcedureYusephAwangSanaaniNo ratings yet
- What Is A Miscarriage and Abortion Similarities and DifferencesDocument9 pagesWhat Is A Miscarriage and Abortion Similarities and DifferencesOvais HussaiinNo ratings yet
- Before Starting The Presentation, I Am Requesting You All To Get A HandkerchiefDocument35 pagesBefore Starting The Presentation, I Am Requesting You All To Get A HandkerchiefOng KarlNo ratings yet
- Congenital Conditions.: by Mayo Clinic StaffDocument3 pagesCongenital Conditions.: by Mayo Clinic StaffDaisy Ann IñigoNo ratings yet
- Nursing DiagnosisDocument16 pagesNursing DiagnosisShemie TutorNo ratings yet
- 3 Conditions To Watch For After Childbirth: 1. Postpartum PreeclampsiaDocument4 pages3 Conditions To Watch For After Childbirth: 1. Postpartum PreeclampsiaM. MaulanaNo ratings yet
- CF433 Medical Management of An Ectopic Pregnancy Using MethotrexateDocument11 pagesCF433 Medical Management of An Ectopic Pregnancy Using MethotrexateponekNo ratings yet
- Laparoscopy and Laparoscopic SurgeryDocument4 pagesLaparoscopy and Laparoscopic SurgerySidra AnjumNo ratings yet
- Ectopic PregnancyDocument4 pagesEctopic PregnancyJovie Anne BorjaNo ratings yet
- What Exactly Is Uterine Prolapse?Document3 pagesWhat Exactly Is Uterine Prolapse?Ika SriNo ratings yet
- EPU Surgical Management of MiscarriageDocument8 pagesEPU Surgical Management of MiscarriagedommyNo ratings yet
- Incompetent CervixDocument4 pagesIncompetent CervixjastinmoralesNo ratings yet
- Diagnosis of Abruptio Placentae: Placenta PreviaDocument42 pagesDiagnosis of Abruptio Placentae: Placenta PreviaRirin Dwi LestariNo ratings yet
- Placenta PreviaDocument3 pagesPlacenta PreviaVicente TurasNo ratings yet
- 99 11 Laparoscopy Sterilisations 2011Document12 pages99 11 Laparoscopy Sterilisations 2011Vivien KrajczNo ratings yet
- It's Not Just a Heavy Period; The Miscarriage HandbookFrom EverandIt's Not Just a Heavy Period; The Miscarriage HandbookRating: 2 out of 5 stars2/5 (1)
- Undescended Testis, (Cryptorchidism) A Simple Guide To The Condition, Treatment And Related ConditionsFrom EverandUndescended Testis, (Cryptorchidism) A Simple Guide To The Condition, Treatment And Related ConditionsRating: 5 out of 5 stars5/5 (2)
- Can You Help Fairies Find Their HomeDocument1 pageCan You Help Fairies Find Their HomeSiska FriedmanNo ratings yet
- D - Rochmanita Safitri (Skoliosis)Document59 pagesD - Rochmanita Safitri (Skoliosis)Siska FriedmanNo ratings yet
- B - Yonanda Adi (Stroke)Document10 pagesB - Yonanda Adi (Stroke)Siska FriedmanNo ratings yet
- Pre EclampsiaDocument15 pagesPre EclampsiaSiska FriedmanNo ratings yet
- C - Kavinan Subramaniam - Heart FailureDocument5 pagesC - Kavinan Subramaniam - Heart FailureSiska FriedmanNo ratings yet
- Ectopic PregnancyDocument3 pagesEctopic PregnancySiska FriedmanNo ratings yet
- Hyperemesis GravidarumDocument12 pagesHyperemesis GravidarumSiska FriedmanNo ratings yet
- FigureDocument1 pageFigureSiska FriedmanNo ratings yet
- From: Ectopic Pregnancy: JAMA. 2012 308 (8) :829-829. Doi:10.1001/jama.2012.6215Document1 pageFrom: Ectopic Pregnancy: JAMA. 2012 308 (8) :829-829. Doi:10.1001/jama.2012.6215Siska FriedmanNo ratings yet
- Plant Start Up Timeline - 24 Aug 09 - Rev 1Document1 pagePlant Start Up Timeline - 24 Aug 09 - Rev 1Siska FriedmanNo ratings yet
- 2019 Midwife CVDocument2 pages2019 Midwife CVapi-455508133No ratings yet
- Family Planning MethodsDocument7 pagesFamily Planning MethodsAngelika PadawanNo ratings yet
- SynopsisDocument10 pagesSynopsisAhmedMalikNo ratings yet
- Zeemcqselfwith AnswerDocument49 pagesZeemcqselfwith Answera7332773No ratings yet
- PubertyDocument18 pagesPubertyNuhaYahyaNo ratings yet
- Ob Ati StudyDocument22 pagesOb Ati Studylpirman0580% (5)
- Baby of Siti FauziahDocument3 pagesBaby of Siti FauziahjabirNo ratings yet
- Women's Health: HysterectomyDocument7 pagesWomen's Health: HysterectomySuci RahmayeniNo ratings yet
- Geethu, 2016Document6 pagesGeethu, 2016laborraNo ratings yet
- 9 - Postterm PregnancyDocument22 pages9 - Postterm PregnancyMara Medina - BorleoNo ratings yet
- Teenage PregnancyDocument26 pagesTeenage PregnancyAnne Kathria Bernadette Gabriel100% (1)
- 1.female Reproductive System PDFDocument21 pages1.female Reproductive System PDFTrang KhúcNo ratings yet
- Perfect-Use and Typical-Use Pearl Index of A Contraceptive Mobile AppDocument6 pagesPerfect-Use and Typical-Use Pearl Index of A Contraceptive Mobile AppRaven DelargeNo ratings yet
- Obstetric Safety ProtocolsDocument10 pagesObstetric Safety ProtocolsApril LilianNo ratings yet
- Curretage Abortus SetDocument4 pagesCurretage Abortus Sethijabian idNo ratings yet
- Lecture 3 Estrous Cycle and Estrus Signs in Domestic AnimalsDocument33 pagesLecture 3 Estrous Cycle and Estrus Signs in Domestic AnimalsgnpobsNo ratings yet
- Discuss The Mechanism of Labor (Vertex Presentation) : Key Stages of LabourDocument2 pagesDiscuss The Mechanism of Labor (Vertex Presentation) : Key Stages of LabourGwyneth Nicole BudayNo ratings yet
- Ob Au Ca2Document243 pagesOb Au Ca2ervin_agena394No ratings yet
- CerazetteDocument36 pagesCerazetteSuhazeli AbdullahNo ratings yet
- Exercise 2 - FP Form 1 A and B (1) TDocument2 pagesExercise 2 - FP Form 1 A and B (1) TJohn Alfred TanNo ratings yet
- Ob - Abnormalities of The Third Stage of Labor andDocument108 pagesOb - Abnormalities of The Third Stage of Labor andapi-3856051100% (2)
- Obstetrics 4Document9 pagesObstetrics 4Darrel Allan MandiasNo ratings yet
- Abnormal Vaginal Discharge (Vaginitis) - Children's Hospital of PhiladelphiaDocument1 pageAbnormal Vaginal Discharge (Vaginitis) - Children's Hospital of PhiladelphiaHabtamu tamiruNo ratings yet
- Care and Management of Antepartal WomanDocument4 pagesCare and Management of Antepartal WomanGeuel PilapilNo ratings yet
- Stages of Prenatal DevelopmentDocument15 pagesStages of Prenatal DevelopmentsoraruNo ratings yet
- Book Garba SamskaraDocument3 pagesBook Garba SamskaraYogaguru NehaNo ratings yet
- Abnormal Uterine Bleeding: Dr. Jasmina Begum Assistant Professor AIIMS, BhubaneswarDocument80 pagesAbnormal Uterine Bleeding: Dr. Jasmina Begum Assistant Professor AIIMS, BhubaneswarSharoon KumarNo ratings yet
- Pelvic Inflammatory Disease (PID) : Basim Abu-RafeaDocument26 pagesPelvic Inflammatory Disease (PID) : Basim Abu-Rafeaedwin mudumiNo ratings yet
Ectopic Pregnancy Journal
Ectopic Pregnancy Journal
Uploaded by
Siska FriedmanOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Ectopic Pregnancy Journal
Ectopic Pregnancy Journal
Uploaded by
Siska FriedmanCopyright:
Available Formats
Womens Health Service
Ectopic Pregnancy
Information for patients
What is an Ectopic Pregnancy?
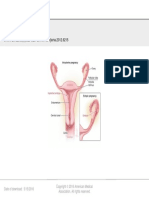
An ectopic pregnancy is where the fertilised
egg implants outside the uterus (womb), most
commonly in the fallopian tube (the tube that
connects the ovary to the uterus).
Rarely an ectopic pregnancy can occur in the
ovary, cervix or abdominal cavity. It usually occurs
in the first ten weeks of pregnancy.
About 1 in 100 pregnancies in is ectopic. This
figure rises to 5 in 100 after assisted conception
therapies and to 20-30 in 100 after tubal damage
due to infection or tubal surgery.
What are the possible causes of an
ectopic pregnancy?
The chances of having an ectopic pregnancy can
be increased by the following:
Tubal damage from pelvic infection,
endometriosis or appendicitis
Women who have had previous abdominal
surgery (scar tissue and adhesions develop)
Women using the IUCD (coil) as a
contraceptive and become pregnant are at
risk, though a pregnancy is very rare
In most cases the cause of the pregnancy
developing outside the uterus is never
discovered
What are the symptoms of an
ectopic pregnancy?
Symptoms typically develop around the 6th week
of pregnancy. This is about 2 weeks after a missed
period if you have regular periods. However,
symptoms may develop anytime between 4 and 10
weeks of pregnancy. You may not be aware that
you are pregnant. For example, your periods may
not be regular, or you may be using contraception
and not realise it has failed. Symptoms may
start about the time a period is due. At first you
may think the symptoms are just a late period.
Symptoms include one or more of the following.
Pain on one side of the lower abdomen. It
may develop sharply, or may slowly get
worse over several days. It can become
severe.
Vaginal bleeding often occurs, but not
always. It is often different to the bleeding of
a period. For example, the bleeding may be
heavier or lighter than a normal period. The
blood may look darker. However, you may
think the bleeding is a late period.
Other symptoms may occur such as
diarrhoea, feeling faint, or pain on passing
faeces (stools).
Shoulder-tip pain may develop. This is due
to some blood leaking into the abdomen and
irritating the diaphragm (the muscle used to
breathe).
If the fallopian tube ruptures and causes
internal bleeding, you may develop severe
pain or collapse. This is an emergency as
the bleeding is heavy.
Sometimes there are no warning symptoms
(such as pain) before the tube ruptures.
Therefore collapse due to sudden heavy
internal bleeding is sometimes the first sign
of an ectopic pregnancy.
How is an ectopic pregnancy
confirmed?
If you have symptoms that may indicate an
ectopic pregnancy you will be sent to hospital
immediately.
Issued August 2012 / Review August 2015 / ID W&CHD GA PIB-52 Vn 2
A urine test can confirm that you are
pregnant.
An ultrasound scan may confirm an ectopic
pregnancy. However, the scan may not
be clear if the pregnancy is very early. A
few days of observation may be needed if
symptoms are not severe. A repeat scan
a few days later may clarify the site of the
pregnancy.
Blood tests that show changes in the
pregnancy hormones are also helpful.
A look inside the abdomen with a special
telescope (laparoscopy) is sometimes
advised to confirm an ectopic pregnancy.
If the ultrasound shows an empty uterus, but the
pregnancy test is positive, an ectopic pregnancy
is possible, although you may have had a
miscarriage.
It is not always possible to see an ectopic
pregnancy on ultrasound scan and if you feel well,
you will have some blood taken to measure the
pregnancy hormone level and this will be repeated
over the next few days to confirm the diagnosis.
What are the treatment options for
ectopic pregnancy?
Ruptured ectopic pregnancy
Emergency surgery is needed if a fallopian tube
ruptures with heavy bleeding. The main aim is to
stop the bleeding. The ruptured fallopian tube and
remnant of the early pregnancy are then removed.
The operation is often life saving.
Early ectopic pregnancy - before rupture
Ectopic pregnancy is often diagnosed before
rupture. Your doctor will advise on the treatment
options, which may include the following.
Surgery
A planned operation is the usual treatment.
Removal of the tube and the ectopic pregnancy
is the traditional treatment. More recently, better
surgical techniques mean that it is sometimes
possible to preserve the fallopian tube. Operations
by keyhole surgery are becoming more popular.
Laparoscopy - insertion of scope (camera)
into the abdomen through your navel (key
hole surgery)
Laparotomy - incision (open cut) into the
abdominal cavity
Salpingectomy - removal of the fallopian
tube
Salpingotomy - cut open the tube and
removing the ectopic pregnancy alone
(preserving the tube)
Medical treatment
A medicine called methotrexate may be an option.
It works by stopping the cells of the pregnancy
growing in the fallopian tube. It is normally
only advised if the pregnancy is very early. The
advantage is that you do not need an operation.
The disadvantage is that you will need close
observation for several weeks with repeated
blood tests to check it has worked. Also, sideeffects affect some women. If this treatment is
not successful, further surgery to remove the tube
may be necessary.
Expectant management (wait and see)
Some ectopic pregnancies that have not ruptured
clear without treatment. The pregnancy often dies
in a way similar to a miscarriage. A possible option
is to see how things go if you have mild or no
symptoms. You can have treatment if symptoms
become worse. However, a wait and see approach
is not often advised. This is because there is a
chance of a sudden rupture of the fallopian tube.
This will need emergency surgery. You will need
close observation and repeated scans and blood
tests to check on how things are developing.
You may experience some bleeding for few days
after surgery/medical treatment, due to the fact
that you have been pregnant and the lining of
the womb has thickened. The above is a brief
description of treatment options. A gynaecologist
will advise on the pros and cons of each
treatment.
If you have a Rhesus negative blood group, you
will require Anti D Immunoglobulin. This will be
arranged by the staff prior to you leaving hospital.
What about future pregnancy?
Although you may want to try again, it is best to
wait until you and your partner are ready, both
physically and emotionally.
It is advisable to wait until 4-6 weeks after surgery
before resuming sexual intercourse. If you have
had medical treatment, your doctor will advise you
accordingly.
If one tube was removed, you will continue to
ovulate as before, but your chances of conceiving
may be reduced. This varies with each individual.
One common question is what is the chance of
having a future normal pregnancy after an ectopic
pregnancy? Even if one fallopian tube is removed,
you have about a 7 in 10 chance of having a future
normal pregnancy. (The other fallopian tube will
still usually work.) There is also a 1 in 10 chance
of a repeat ectopic pregnancy. As soon as you
suspect you are pregnant, you must contact your
GP immediately and be monitored closely.
Once an ectopic pregnancy has been excluded,
the pregnancy would be anticipated to continue
normally and no further close monitoring would be
required.
What about returning to work or
normal activities?
You will need possibly up to 4- 6 weeks to
recuperate after surgery. It is advisable to build
up your strength gradually. Having an ectopic
pregnancy can be traumatic because you are
dealing with the loss of a pregnancy as well as
trying to recover from emergency surgery.
It is common to feel anxious or depressed for
a while after treatment. Worries about possible
future ectopic pregnancy, the affect on fertility,
and sadness over the loss of the pregnancy are
normal. Do talk with a doctor about these and any
other concerns following treatment.
If you would like any further information, or would
like to talk to someone who has been through the
experience of an ectopic pregnancy, please refer to
contact details on the reverse of this booklet.
Contact details:
Womens Clinics-Acute Assessment,
Level 3 North, Wellington Hospital
Phone 04 8060 740
Ward 4 North, Level 4, Wellington Hospital,
Phone 04 8060 880
Wellington Miscarriage Support Group
Support and information for women and
their families who have lost a baby through
miscarriage or ectopic pregnancy.
04 384 4272 (answerphone and they will call
back).
www.miscarriagesupport.org.nz
info@miscarriagesupport.org.nz
You might also like
- Maternal Child Nursing Care in Canada - CH1-28Document2 pagesMaternal Child Nursing Care in Canada - CH1-28Reena Rajcoomar0% (1)
- Step 2 CK Usmle Questions For Ob GynDocument48 pagesStep 2 CK Usmle Questions For Ob Gyniamdonut87% (15)
- Bleeding During Pregnancy and Nursing Care PlanDocument17 pagesBleeding During Pregnancy and Nursing Care PlanLizcelle Bihasa86% (7)
- Ass Ectopic PregnancyDocument10 pagesAss Ectopic PregnancyPriyaNo ratings yet
- Ectopic Pregnancy Kehamilan Luar RahimDocument5 pagesEctopic Pregnancy Kehamilan Luar RahimMuhamad Aminuddin Abu BakarNo ratings yet
- Information For You: An Ectopic PregnancyDocument25 pagesInformation For You: An Ectopic PregnancyAnonymous layszXmsNo ratings yet
- Management of Ectopic PregnancyDocument8 pagesManagement of Ectopic PregnancySulaiman WalizadaNo ratings yet
- Ectopic PregnancyDocument17 pagesEctopic PregnancyB.HemavarshiniNo ratings yet
- Ectopic Pregnancy April 2018 1Document6 pagesEctopic Pregnancy April 2018 1Avindya RarasatiNo ratings yet
- 2022.TP (Ectopic Pregnancy) NOUNSDocument6 pages2022.TP (Ectopic Pregnancy) NOUNSWilson BenitezNo ratings yet
- Uterus: Signs and SymptomsDocument4 pagesUterus: Signs and SymptomsmoigomezNo ratings yet
- Uterus: Signs and SymptomsDocument4 pagesUterus: Signs and SymptomsmoigomezNo ratings yet
- CASE ANALYSIS Ectopic Pregnancy Part 1Document10 pagesCASE ANALYSIS Ectopic Pregnancy Part 1Diane Celine SantianoNo ratings yet
- Uterus: Signs and SymptomsDocument11 pagesUterus: Signs and SymptomsJoy Parallag - BautoNo ratings yet
- Ectopic Pregnancy: Medlineplus TopicsDocument9 pagesEctopic Pregnancy: Medlineplus TopicsJonathan BendecioNo ratings yet
- Pi Ectopic Pregnancy Mar20Document9 pagesPi Ectopic Pregnancy Mar20Aziza TahanyNo ratings yet
- Problems in Early Pregnancy - NBT002073Document8 pagesProblems in Early Pregnancy - NBT002073ElvisNo ratings yet
- ERPC LeafletDocument4 pagesERPC Leafletjoshy221196No ratings yet
- Problems in Early PregnancyDocument11 pagesProblems in Early PregnancyRizal LeonardoNo ratings yet
- What Can I Expect in A Cesarean Procedure?Document7 pagesWhat Can I Expect in A Cesarean Procedure?abbiefayeNo ratings yet
- Ectopic PregnancyDocument4 pagesEctopic PregnancySyahriana AnaNo ratings yet
- Ectopic Pregnancy: Frequently Asked Questions FAQ155 PregnancyDocument2 pagesEctopic Pregnancy: Frequently Asked Questions FAQ155 PregnancyUlfaa MutiaaNo ratings yet
- Early MiscarriageretrjytkuyiulDocument6 pagesEarly MiscarriageretrjytkuyiulMuhammed BarznjiNo ratings yet
- Group 1. An Overview of MiscarriageDocument3 pagesGroup 1. An Overview of MiscarriageAprilia Vivilianotekowador PlantonevliamorNo ratings yet
- Dilation and Curettage - Health TeachingDocument4 pagesDilation and Curettage - Health TeachingGol D. RogerNo ratings yet
- What Is Bilateral Tubal Ligation?Document5 pagesWhat Is Bilateral Tubal Ligation?Janice UbagNo ratings yet
- O&G Counselling - TSPDocument6 pagesO&G Counselling - TSPTarran PhagooNo ratings yet
- AMODIADocument3 pagesAMODIAMarriel AmodiaNo ratings yet
- What Is Bilateral Tubal LigationDocument42 pagesWhat Is Bilateral Tubal LigationAldrich ArquizaNo ratings yet
- 27 Ovarian Cystectomy Consent FormDocument3 pages27 Ovarian Cystectomy Consent FormsekyNo ratings yet
- 11 63 Expectant Management of An Ectopic Pregnancy June 2018Document7 pages11 63 Expectant Management of An Ectopic Pregnancy June 2018Tandyo TriasmoroNo ratings yet
- Vaginal Hysterectomy and Vaginal Repair: Women's ServiceDocument16 pagesVaginal Hysterectomy and Vaginal Repair: Women's Serviceintan yulia safarinaNo ratings yet
- Abortion: Renhe Hospital Wang JunjieDocument51 pagesAbortion: Renhe Hospital Wang JunjieMadhu Sudhan PandeyaNo ratings yet
- Bleeding During Pregnancy and Nursing Care PlanDocument19 pagesBleeding During Pregnancy and Nursing Care PlanJack BangcoyoNo ratings yet
- Endometrial Biopsy and CervicaDocument2 pagesEndometrial Biopsy and CervicaFahmi NugrahaNo ratings yet
- What is Postpartum HemorrhageDocument7 pagesWhat is Postpartum HemorrhageEmerson De SilvaNo ratings yet
- Togdher University Lectural Asma Da, Ud Kahin Class of Midwifery and Nursing Course Title Reproductive HealthDocument18 pagesTogdher University Lectural Asma Da, Ud Kahin Class of Midwifery and Nursing Course Title Reproductive HealthHoodo AhmedNo ratings yet
- Vaginal Bleeding in Early PregnancyDocument8 pagesVaginal Bleeding in Early PregnancyBal Ri Mekoleu100% (1)
- Brief Description: Ectopic PregnancyDocument6 pagesBrief Description: Ectopic PregnancyQueenet BelingonNo ratings yet
- Placenta Abruptio - Topic OverviewDocument8 pagesPlacenta Abruptio - Topic OverviewLei AbellarNo ratings yet
- Spotting in Early Pregnancy - Is It Common, Causes, and Seeing A DoctorDocument9 pagesSpotting in Early Pregnancy - Is It Common, Causes, and Seeing A DoctorlastmadanhireNo ratings yet
- Ovulation Induction and Intra Uterine InseminationDocument4 pagesOvulation Induction and Intra Uterine InseminationmasdipoNo ratings yet
- Vaginal Bleeding in Early PregnancyDocument8 pagesVaginal Bleeding in Early PregnancyRudi LadoNo ratings yet
- What Is An Episiotomy?: Reasons For The ProcedureDocument9 pagesWhat Is An Episiotomy?: Reasons For The ProcedureYusephAwangSanaaniNo ratings yet
- What Is An Episiotomy?: Reasons For The ProcedureDocument11 pagesWhat Is An Episiotomy?: Reasons For The ProcedureYusephAwangSanaaniNo ratings yet
- What Is A Miscarriage and Abortion Similarities and DifferencesDocument9 pagesWhat Is A Miscarriage and Abortion Similarities and DifferencesOvais HussaiinNo ratings yet
- Before Starting The Presentation, I Am Requesting You All To Get A HandkerchiefDocument35 pagesBefore Starting The Presentation, I Am Requesting You All To Get A HandkerchiefOng KarlNo ratings yet
- Congenital Conditions.: by Mayo Clinic StaffDocument3 pagesCongenital Conditions.: by Mayo Clinic StaffDaisy Ann IñigoNo ratings yet
- Nursing DiagnosisDocument16 pagesNursing DiagnosisShemie TutorNo ratings yet
- 3 Conditions To Watch For After Childbirth: 1. Postpartum PreeclampsiaDocument4 pages3 Conditions To Watch For After Childbirth: 1. Postpartum PreeclampsiaM. MaulanaNo ratings yet
- CF433 Medical Management of An Ectopic Pregnancy Using MethotrexateDocument11 pagesCF433 Medical Management of An Ectopic Pregnancy Using MethotrexateponekNo ratings yet
- Laparoscopy and Laparoscopic SurgeryDocument4 pagesLaparoscopy and Laparoscopic SurgerySidra AnjumNo ratings yet
- Ectopic PregnancyDocument4 pagesEctopic PregnancyJovie Anne BorjaNo ratings yet
- What Exactly Is Uterine Prolapse?Document3 pagesWhat Exactly Is Uterine Prolapse?Ika SriNo ratings yet
- EPU Surgical Management of MiscarriageDocument8 pagesEPU Surgical Management of MiscarriagedommyNo ratings yet
- Incompetent CervixDocument4 pagesIncompetent CervixjastinmoralesNo ratings yet
- Diagnosis of Abruptio Placentae: Placenta PreviaDocument42 pagesDiagnosis of Abruptio Placentae: Placenta PreviaRirin Dwi LestariNo ratings yet
- Placenta PreviaDocument3 pagesPlacenta PreviaVicente TurasNo ratings yet
- 99 11 Laparoscopy Sterilisations 2011Document12 pages99 11 Laparoscopy Sterilisations 2011Vivien KrajczNo ratings yet
- It's Not Just a Heavy Period; The Miscarriage HandbookFrom EverandIt's Not Just a Heavy Period; The Miscarriage HandbookRating: 2 out of 5 stars2/5 (1)
- Undescended Testis, (Cryptorchidism) A Simple Guide To The Condition, Treatment And Related ConditionsFrom EverandUndescended Testis, (Cryptorchidism) A Simple Guide To The Condition, Treatment And Related ConditionsRating: 5 out of 5 stars5/5 (2)
- Can You Help Fairies Find Their HomeDocument1 pageCan You Help Fairies Find Their HomeSiska FriedmanNo ratings yet
- D - Rochmanita Safitri (Skoliosis)Document59 pagesD - Rochmanita Safitri (Skoliosis)Siska FriedmanNo ratings yet
- B - Yonanda Adi (Stroke)Document10 pagesB - Yonanda Adi (Stroke)Siska FriedmanNo ratings yet
- Pre EclampsiaDocument15 pagesPre EclampsiaSiska FriedmanNo ratings yet
- C - Kavinan Subramaniam - Heart FailureDocument5 pagesC - Kavinan Subramaniam - Heart FailureSiska FriedmanNo ratings yet
- Ectopic PregnancyDocument3 pagesEctopic PregnancySiska FriedmanNo ratings yet
- Hyperemesis GravidarumDocument12 pagesHyperemesis GravidarumSiska FriedmanNo ratings yet
- FigureDocument1 pageFigureSiska FriedmanNo ratings yet
- From: Ectopic Pregnancy: JAMA. 2012 308 (8) :829-829. Doi:10.1001/jama.2012.6215Document1 pageFrom: Ectopic Pregnancy: JAMA. 2012 308 (8) :829-829. Doi:10.1001/jama.2012.6215Siska FriedmanNo ratings yet
- Plant Start Up Timeline - 24 Aug 09 - Rev 1Document1 pagePlant Start Up Timeline - 24 Aug 09 - Rev 1Siska FriedmanNo ratings yet
- 2019 Midwife CVDocument2 pages2019 Midwife CVapi-455508133No ratings yet
- Family Planning MethodsDocument7 pagesFamily Planning MethodsAngelika PadawanNo ratings yet
- SynopsisDocument10 pagesSynopsisAhmedMalikNo ratings yet
- Zeemcqselfwith AnswerDocument49 pagesZeemcqselfwith Answera7332773No ratings yet
- PubertyDocument18 pagesPubertyNuhaYahyaNo ratings yet
- Ob Ati StudyDocument22 pagesOb Ati Studylpirman0580% (5)
- Baby of Siti FauziahDocument3 pagesBaby of Siti FauziahjabirNo ratings yet
- Women's Health: HysterectomyDocument7 pagesWomen's Health: HysterectomySuci RahmayeniNo ratings yet
- Geethu, 2016Document6 pagesGeethu, 2016laborraNo ratings yet
- 9 - Postterm PregnancyDocument22 pages9 - Postterm PregnancyMara Medina - BorleoNo ratings yet
- Teenage PregnancyDocument26 pagesTeenage PregnancyAnne Kathria Bernadette Gabriel100% (1)
- 1.female Reproductive System PDFDocument21 pages1.female Reproductive System PDFTrang KhúcNo ratings yet
- Perfect-Use and Typical-Use Pearl Index of A Contraceptive Mobile AppDocument6 pagesPerfect-Use and Typical-Use Pearl Index of A Contraceptive Mobile AppRaven DelargeNo ratings yet
- Obstetric Safety ProtocolsDocument10 pagesObstetric Safety ProtocolsApril LilianNo ratings yet
- Curretage Abortus SetDocument4 pagesCurretage Abortus Sethijabian idNo ratings yet
- Lecture 3 Estrous Cycle and Estrus Signs in Domestic AnimalsDocument33 pagesLecture 3 Estrous Cycle and Estrus Signs in Domestic AnimalsgnpobsNo ratings yet
- Discuss The Mechanism of Labor (Vertex Presentation) : Key Stages of LabourDocument2 pagesDiscuss The Mechanism of Labor (Vertex Presentation) : Key Stages of LabourGwyneth Nicole BudayNo ratings yet
- Ob Au Ca2Document243 pagesOb Au Ca2ervin_agena394No ratings yet
- CerazetteDocument36 pagesCerazetteSuhazeli AbdullahNo ratings yet
- Exercise 2 - FP Form 1 A and B (1) TDocument2 pagesExercise 2 - FP Form 1 A and B (1) TJohn Alfred TanNo ratings yet
- Ob - Abnormalities of The Third Stage of Labor andDocument108 pagesOb - Abnormalities of The Third Stage of Labor andapi-3856051100% (2)
- Obstetrics 4Document9 pagesObstetrics 4Darrel Allan MandiasNo ratings yet
- Abnormal Vaginal Discharge (Vaginitis) - Children's Hospital of PhiladelphiaDocument1 pageAbnormal Vaginal Discharge (Vaginitis) - Children's Hospital of PhiladelphiaHabtamu tamiruNo ratings yet
- Care and Management of Antepartal WomanDocument4 pagesCare and Management of Antepartal WomanGeuel PilapilNo ratings yet
- Stages of Prenatal DevelopmentDocument15 pagesStages of Prenatal DevelopmentsoraruNo ratings yet
- Book Garba SamskaraDocument3 pagesBook Garba SamskaraYogaguru NehaNo ratings yet
- Abnormal Uterine Bleeding: Dr. Jasmina Begum Assistant Professor AIIMS, BhubaneswarDocument80 pagesAbnormal Uterine Bleeding: Dr. Jasmina Begum Assistant Professor AIIMS, BhubaneswarSharoon KumarNo ratings yet
- Pelvic Inflammatory Disease (PID) : Basim Abu-RafeaDocument26 pagesPelvic Inflammatory Disease (PID) : Basim Abu-Rafeaedwin mudumiNo ratings yet