Professional Documents
Culture Documents
Sublingual Buprenorphine For Acute Renal Colic Pain Management: A Double-Blind, Randomized Controlled Trial
Sublingual Buprenorphine For Acute Renal Colic Pain Management: A Double-Blind, Randomized Controlled Trial
Uploaded by
andrew herringCopyright:
Available Formats
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5834)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (852)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (903)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (541)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (350)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (824)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (405)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Drug Education and Vice ControlDocument18 pagesDrug Education and Vice ControlKhai Loh Work100% (2)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Highland Guidelines - LDK 2013-2-15Document3 pagesHighland Guidelines - LDK 2013-2-15andrew herringNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Effect of Housing and Gender On Morphine Self-Administration in RatsDocument4 pagesThe Effect of Housing and Gender On Morphine Self-Administration in RatsGiovana Lenz100% (1)
- K Opiods For Pain BupDocument2 pagesK Opiods For Pain Bupandrew herringNo ratings yet
- Pharmacology MnemonicsDocument91 pagesPharmacology MnemonicsKnizhonki Knizhonki96% (72)
- Pharm MnemonicsDocument33 pagesPharm MnemonicsThomson George75% (4)
- Rib Fracture W: PecsDocument8 pagesRib Fracture W: Pecsandrew herring100% (1)
- Roux 2013Document7 pagesRoux 2013andrew herringNo ratings yet
- Original Article: Serratus Plane Block: A Novel Ultrasound-Guided Thoracic Wall Nerve BlockDocument7 pagesOriginal Article: Serratus Plane Block: A Novel Ultrasound-Guided Thoracic Wall Nerve Blockandrew herringNo ratings yet
- Rib Fracture SerratusDocument3 pagesRib Fracture Serratusandrew herring100% (1)
- Buprenorphine 2016-7-18Document1 pageBuprenorphine 2016-7-18andrew herringNo ratings yet
- Intravenous Lidocaine To Treat Postoperative Pain : Lidocaína Intravenosa No Tratamento Da Dor Pós-OperatóriaDocument6 pagesIntravenous Lidocaine To Treat Postoperative Pain : Lidocaína Intravenosa No Tratamento Da Dor Pós-Operatóriaandrew herringNo ratings yet
- Herring ED Intractable Abdominal pain-N+VDocument1 pageHerring ED Intractable Abdominal pain-N+Vandrew herringNo ratings yet
- Ketamine As Rescue Treatment FDocument8 pagesKetamine As Rescue Treatment Fandrew herringNo ratings yet
- 3.2.16.highland Emergency Medicine Journal Club Methods.2Document2 pages3.2.16.highland Emergency Medicine Journal Club Methods.2andrew herringNo ratings yet
- Ultrasound-Guided Block of TheDocument6 pagesUltrasound-Guided Block of Theandrew herringNo ratings yet
- Dex For Dental Pain & SwellingDocument7 pagesDex For Dental Pain & Swellingandrew herring100% (1)
- Nej MR A 1511480Document9 pagesNej MR A 1511480Tohari Masidi AminNo ratings yet
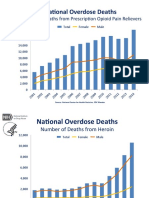
- OPR - Heroin DeathsDocument2 pagesOPR - Heroin Deathsandrew herringNo ratings yet
- CVS Action Plan v2Document1 pageCVS Action Plan v2andrew herringNo ratings yet
- Ultrasound Guided Interventional Procedures In.13Document14 pagesUltrasound Guided Interventional Procedures In.13andrew herring100% (1)
- Ultrasound Guided Interventional Procedures In.4Document13 pagesUltrasound Guided Interventional Procedures In.4andrew herringNo ratings yet
- Substance AbuseDocument19 pagesSubstance AbuseVrushank Ram100% (1)
- 5424 The Halogeno Morphides and Codides and The Mechanism of The Morphine Apomorphine Transformation3dc4Document16 pages5424 The Halogeno Morphides and Codides and The Mechanism of The Morphine Apomorphine Transformation3dc4Jo JohNo ratings yet
- Introduction To PainDocument21 pagesIntroduction To Painayanle Abdi AliNo ratings yet
- Attenuation of Heroin Withdrawl Syndrome by The Administration of High Dose Vitamin C 27.4Document9 pagesAttenuation of Heroin Withdrawl Syndrome by The Administration of High Dose Vitamin C 27.4Madalina FeraruNo ratings yet
- Cdi 8Document37 pagesCdi 8Bencio AizaNo ratings yet
- US - Article - 1col - Peri-Op - June22Document12 pagesUS - Article - 1col - Peri-Op - June22Odett NuñezNo ratings yet
- Lecture 16-17 - Opioids AnalgesicsDocument20 pagesLecture 16-17 - Opioids AnalgesicsJedoNo ratings yet
- Intro To Med. ChemDocument30 pagesIntro To Med. ChemF ParikhNo ratings yet
- Jur Nista TabDocument17 pagesJur Nista Tabnela sharonNo ratings yet
- Desomorfina - KrokodilDocument45 pagesDesomorfina - Krokodilbetsy cadena tenorioNo ratings yet
- سندDocument38 pagesسندAshkan AbbasiNo ratings yet
- Yellow List: List of Narcotic Drugs Under International ControlDocument25 pagesYellow List: List of Narcotic Drugs Under International ControlAMSNo ratings yet
- 防制藥物濫用外語宣導手冊 (英文版)Document40 pages防制藥物濫用外語宣導手冊 (英文版)Bong Sze WeeNo ratings yet
- Cdi Drugs Art 1218Document213 pagesCdi Drugs Art 1218Gian Antonio L. AbdonNo ratings yet
- Facts and Figures From PDEA Catchillar Stephanie L. NSTPDocument5 pagesFacts and Figures From PDEA Catchillar Stephanie L. NSTPJovilleNo ratings yet
- WHO Step Ladder For PainDocument5 pagesWHO Step Ladder For PainRizKyImanSariNo ratings yet
- Drug StudyDocument9 pagesDrug StudyChristine PunsalanNo ratings yet
- FDA Fails To Follow The Science On KratomDocument21 pagesFDA Fails To Follow The Science On KratomAnonymous r6OHQrqLOtNo ratings yet
- Stabilis Monographie Ketorolac TromethamineDocument5 pagesStabilis Monographie Ketorolac Tromethamineintan kusumaningtyasNo ratings yet
- Studies On Drug Codein (MM - Ardhi Mukhoffah Bil'Ilmi 13670012)Document7 pagesStudies On Drug Codein (MM - Ardhi Mukhoffah Bil'Ilmi 13670012)ArdhieEl-ilmieNo ratings yet
- Gpat 4Document17 pagesGpat 4GANESH KUMAR JELLANo ratings yet
- Cdi Lecture 1Document10 pagesCdi Lecture 1TJ del MarNo ratings yet
- Learning Objectives: Nstp-Cwts I Module 1 - Drug Education in The PhilippinesDocument13 pagesLearning Objectives: Nstp-Cwts I Module 1 - Drug Education in The PhilippinesALMONIA, GEZZIEL GANIRNo ratings yet
- Mir & MCRDocument1 pageMir & MCRMhmoud NabehNo ratings yet
- Anaesthesia LMRP 2019Document24 pagesAnaesthesia LMRP 2019Prabhat KcNo ratings yet
- Misuse of Drugs Regulations (Document57 pagesMisuse of Drugs Regulations (Terrence LiNo ratings yet
Sublingual Buprenorphine For Acute Renal Colic Pain Management: A Double-Blind, Randomized Controlled Trial
Sublingual Buprenorphine For Acute Renal Colic Pain Management: A Double-Blind, Randomized Controlled Trial
Uploaded by
andrew herringOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Sublingual Buprenorphine For Acute Renal Colic Pain Management: A Double-Blind, Randomized Controlled Trial
Sublingual Buprenorphine For Acute Renal Colic Pain Management: A Double-Blind, Randomized Controlled Trial
Uploaded by
andrew herringCopyright:
Available Formats
Payandemehr et al.
International Journal of Emergency Medicine 2014, 7:1
http://www.intjem.com/content/7/1/1
ORIGINAL RESEARCH
Open Access
Sublingual buprenorphine for acute renal colic
pain management: a double-blind, randomized
controlled trial
Pooya Payandemehr1, Mohammad Jalili1*, Babak Mostafazadeh Davani2 and Ahmad Reza Dehpour3
Abstract
Background: The aim of this study was to compare the efficacy and safety of sublingual buprenorphine with
intravenous morphine sulfate for acute renal colic in the emergency department.
Methods: In this double-dummy, randomized controlled trial, we enrolled patients aged 18 to 55 years who had a
clinical diagnosis of acute renal colic. Patients received either 2 mg sublingual buprenorphine with an IV placebo,
or 0.1 mg/kg IV morphine sulfate with a sublingual placebo. Subjects graded their pain with a standard 11-point
numeric rating scale (NRS) before medication administration and 20 and 40 minutes after that. The need for rescue
analgesia and occurrence of side effects were also recorded in the two groups.
Results: Of 69 patients analyzed, 37 had received buprenorphine, and 32 had taken morphine. Baseline characteristics
were similar in both groups. NRS pain scores were reduced across time by administration of both buprenorphine (from
9.8 to 5.22 and then 2.30) and morphine (from 9.78 to 4.25 and then 1.8), significantly (P <0.0001). The two regimens did
not differ significantly for pain reduction (P = 0.260). Dizziness was more frequently reported by the buprenorphine group
(62.1% versus 37.5%, P <0.05) but other adverse effects observed within 40 minutes were similar in the two groups.
Conclusions: Sublingual buprenorphine (2 mg) is as effective as morphine sulfate (0.1 mg/kg) in acute renal colic pain
management.
Keywords: Buprenorphine; Emergency department; Pain management; Renal colic
Background
Renal colic is a severely painful condition frequently
encountered in emergency departments (EDs) [1]. As
relieving the patients pain and suffering is one of the first
responsibilities of emergency physicians, finding safe and
effective methods to accomplish this task is of paramount
importance [2]. The routine practice for pain reduction in
renal colic is intravenous (IV) administration of analgesics,
either non-steroidal anti-inflammatory drugs or opioids
[3]. IV administration of these drugs, although effective,
takes a lot of staff time, which is not ideal in constantly
overcrowded EDs. On the other hand, time to analgesia is
an indicator of ED service quality, which will be much
longer when using a parenteral route for analgesia [4]. The
ideal analgesic drug is one with enough efficacy and the
fewest side effects as well as easy route of administration.
* Correspondence: mjalili@tums.ac.ir
1
Emergency Medicine Department, Imam Hospital, Tehran University of
Medical Sciences, Keshavarz Blvd, Tehran, Iran
Full list of author information is available at the end of the article
Buprenorphine is an analgesic with mixed agonistantagonist properties which has been shown to have a
role in acute pain management in postoperative pain
and orthopedic injuries [5,6]. However, there is only one
study evaluating its effectiveness in renal colic [7] and,
to the best of our knowledge, there is no study using the
sublingual form of buprenorphine as an analgesic in
renal colic. Its sublingual form can be administered
rapidly and with no need for IV lines, and hence may be
an ideal drug for acute pain management in renal colic.
We compared the effectiveness of sublingual buprenorphine with that of IV morphine sulfate for pain
management in ED patients with renal colic.
Methods
Study design
This is a double-dummy, placebo controlled randomized
clinical trial in patients with acute renal colic in the ED.
Using block randomization (with a computer generated
sequence) and a sealed envelope mechanism for allocation
2014 Payandemehr et al.; licensee Springer. This is an open access article distributed under the terms of the Creative
Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and
reproduction in any medium, provided the original work is properly cited.
Payandemehr et al. International Journal of Emergency Medicine 2014, 7:1
http://www.intjem.com/content/7/1/1
concealment, patients were divided into two groups, one
receiving sublingual buprenorphine with IV placebo and
the other receiving IV morphine with sublingual placebo.
The study was performed in the emergency department of
Imam Hospital, a tertiary referral center with approximately 50,000 visits per year. The ethics committee
approved the study protocol and the study was registered
in www.clinicaltrials.gov (NCT01546701).
Page 2 of 5
respiratory rate and oxygen saturation during the study.
Hypotension was defined as a drop of more than 20
mmHg in systolic blood pressure, and respiratory
depression as a respiratory rate below 12 (if it was
initially more than 12 per minute). The patients were also
asked about their feelings of nausea, vomiting, dizziness,
pruritus, or drowsiness.
Data analysis
Study setting and population
Eligible patients for our study were those with acute
colicky pain aged between 18 and 55 years old and who
had a clinical diagnosis of acute renal colic based on
medical history and a positive urinalysis for hematuria.
The numerical rating scale (NRS), validated by Bijur
et al., was used to measure severity of pain [8]. All
patients with a pain score of more than 3 who signed
the informed consent, were enrolled in the study. We
excluded patients with previous history of seizure;
cardiovascular, hepatic, renal or metabolic diseases;
febrile patients (T >38C); hemodynamically unstable
patients (systolic blood pressure <90 mmHg); and pregnant patients. We also excluded patients with abdominal
tenderness as a sign of peritoneal inflammation and
those with any clinical suspicion for diseases other than
urolithiasis, including abdominal aortic aneurysm or
dissection. Patients with a history of drug addiction or
known allergy to opioids and those who had received
analgesics 6 hours before arriving at the ED were also
excluded to prevent any possible drug reactions.
Study protocol
Eligible patients were randomly allocated into two
groups to receive either sublingual buprenorphine as 2
mg tablets plus IV injection of 0.1 mL/kg sterile water
or a sublingual placebo plus 0.1 mg/kg IV morphine
sulfate (1 mg/mL). All the researchers and participants
remained blind to the treatment and results throughout
the study.
Outcome measures
The primary outcome was the efficacy of the drug with
regards to reducing the NRS 20 and 40 minutes after
administration and the need for rescue analgesia, which
was an IV injection of fentanyl (0.75 g/kg). The secondary
outcome was the occurrence of adverse effects.
Baseline demographic and clinical variables were compared using independent Students t-tests or exact tests.
Repeated measure ANOVA was used to assess the effect
of intervention on pain scores across time and between
the study groups at each time point. Side effects were
compared using 2 tests and P <0.05 was considered
statistically significant. The sample size was calculated as
25 for each group according to the study conducted by
Finlay et al. [7] with and error being 0.05 and 0.20,
respectively. We enrolled 80 patients to cover possible
withdrawals from the study. All analyses were performed
using the Statistical Package for Social Science version
15 (SPSS Inc., Chicago, IL, USA).
Results
Patient characteristics
Between March 2011 and April 2012, 118 patients with
acute renal colic were assessed for eligibility, 38 were
excluded from randomization because they did not meet
the inclusion criteria and 80 were enrolled and randomized into the two treatment groups. During the study
period, 11 patients were lost to follow-up. Of 69 patients
whose data were finally analyzed, 37 and 32 received
buprenorphine and morphine, respectively (Figure 1).
Baseline characteristics were similar in the two groups
(Table 1).
Primary outcome
There was no significant difference between NRS scores
of the two study groups at the beginning of the study.
The NRS pain scores showed a significant reduction
across time (P <0.001) when analyzed using the repeated
measure ANOVA in both groups (Table 2). The two
groups did not differ significantly for pain reduction
(P = 0.260) (Figure 2). The use of rescue analgesia was
not significantly different in the two groups (Table 2).
Secondary outcome
Measurements
Patients were asked to rate their pain in a verbally
administered NRS with 0 representing no pain and 10
the worst imaginable pain. The severity of pain was reevaluated at 20 and 40 minutes after analgesic administration. The patients were monitored for any change in
their vital signs including blood pressure, pulse rate,
There was also no significant difference between the
study groups regarding patients vital signs after administration of the medications except for the respiratory
rate 20 minutes after treatment, which was significantly
lower in the morphine group (mean 11.41 bpm vs. 12.27
bpm) (P = 0.017). No significant difference between the
two groups was noted in terms of respiratory depression
Payandemehr et al. International Journal of Emergency Medicine 2014, 7:1
http://www.intjem.com/content/7/1/1
Page 3 of 5
Figure 1 Flow of participants through trial.
and hypotension. There was no significant difference
between the two groups regarding the occurrence of
nausea, vomiting or pruritus, except that the patients in
buprenorphine group reported dizziness more frequently
(P <0.05) (Table 3). There were no cases of seizure or
loss of consciousness in either group.
Table 1 Baseline demographic and clinical characteristics
of study participants
Group
Buprenorphine n = 37
Morphine n = 32
9.84 (0.50)
9.78 (0.55)
35 (10)
31 (10)
Respiratory rate (per minute)*
13.38 (1.55)
13.13 (1.28)
Pulse rate (per minute)*
90.95 (9.40)
94.63 (11.48)
Female (%)
Mean age (year)*
*Values in mean (SD).
Discussion
The results of this study demonstrated that administration of 2 mg sublingual buprenorphine effectively
reduced pain in patients with acute renal colic. Although
the number of patients was not enough to perform
equivalency tests, the results showed that the analgesic
effect of buprenorphine was comparable to 0.1 mg/kg IV
morphine.
Table 2 Pain scores in study groups
Group
NRS0*
NRS20*
NRS40*
Rescue analgesia**
Buprenorphine
9.84 (0.50)
5.22 (2.66)
2.30 (2.09)
5 (13.5%)
Morphine
9.78 (0.55)
4.25 (2.51)
1.78 (2.45)
2 (6.25%)
*Mean numerical rating score (SD) at baseline and after 20 and 40 minutes.
**Number of patients who needed rescue analgesia after 40 minutes.
Payandemehr et al. International Journal of Emergency Medicine 2014, 7:1
http://www.intjem.com/content/7/1/1
Page 4 of 5
Figure 2 NSR pain score over the study period.
To the best of our knowledge, there are no other studies
on sublingual buprenorphine in the treatment of renal
colic in the ED. However, our results are compatible with
the results of a previous study in this center on the effectiveness of sublingual buprenorphine in acute bone
fractures [6]. In that study, patients with acute extremity
fractures received either sublingual buprenorphine (0.4 mg)
or IV morphine (5 mg). The pain scores were compared
after 30 and 60 minutes and there was no significant difference between the two groups [6]. Our results are also
comparable with the results of Risbo et al. [9] and Abid
et al. [10], who studied buprenorphine in post-operative
pain management. In the first study, buprenorphine was
compared with intramuscular morphine as an analgesic for
pain management after elective knee joint surgery, where
they demonstrated similar efficacy [9]. In the second study,
Abid et al. found buprenorphine as effective as morphine
for post-operative pain management in patients undergoing
a Caesarean section [10]. Furthermore, according to the
findings of this study, patients in the buprenorphine group
reported dizziness more frequently but other adverse effects
observed within 40 minutes were similar in the two groups.
Walsh et al. [11] showed that increasing buprenorphine
dose will increase its analgesic effect but not its side effects.
Comparing to the results of a study in which lower dose of
buprenorphine was used (0.4 mg) and no adverse effect
was reported [6], it seems that higher doses will increase
analgesic efficacy without affecting the side effects.
Limitations
Our study faced several limitations. First, many patients
had to be excluded due to previous use of opioids or
addiction. Secondly, some of the patients might have
been drug seekers and IV drug users imitating renal
colic to get morphine. It is possible that they were not
recognized and were included in study. Thirdly, NRS
may be an inappropriate measurement upon arrival of
the patients as they tend to choose the highest NRS
(i.e., 10), assuming that this will accelerate their treatment process. It may justify the number of patients
Table 3 Occurrence of side effects in the study groups
Group
Nausea
Vomiting
Drowsiness
Pruritus
Dizziness
Respiratory depression
Hypotension
Buprenorphine
20 (54%)
4 (10.8%)
6 (16.2%)
0 (0%)
23 (62.1%)*
10 (27%)
17 (45.9%)
20 (62.5%)
3 (9.3%)
6 (18.7%)
1 (3.1%)
12 (37.5%)
11 (34.3%)
15 (46.8%)
0.47
1.000
0.782
0.464
0.041
0.508
0.938
Morphine
P value
*Statistically significant (P <0.05).
2
test, Fishers exact test.
Payandemehr et al. International Journal of Emergency Medicine 2014, 7:1
http://www.intjem.com/content/7/1/1
whose NRS was 10 at the beginning; however, this situation is expected to be similar in both groups and does
not seem to influence the change in NRS during the
observation time. Another limitation of our study was
the use of 2 mg buprenorphine tablets which may be the
cause of slightly higher rate of side effects in this group;
using smaller doses and then titrating it to effect may
reduce the occurrence of side effects. Finally, this study
did not find a significant difference between the two
groups probably because of the small sample size.
Page 5 of 5
10. Abid A, Benhamou D, Labaille T: Postoperative analgesia after cesarean
section: sublingual buprenorphine versus subcutaneous morphine.
Ann Fr Anesth Reanim 1990, 9:275279.
11. Walsh SL, Preston KL, Stitzer ML, Cone EJ, Bigelow GE: Clinical pharmacology
of buprenorphine: ceiling effects at high doses. Clin Pharmacol Ther 1994,
55:569580.
doi:10.1186/1865-1380-7-1
Cite this article as: Payandemehr et al.: Sublingual buprenorphine for
acute renal colic pain management: a double-blind, randomized
controlled trial. International Journal of Emergency Medicine 2014 7:1.
Conclusions
In conclusion, sublingual buprenorphine can be used as
an effective analgesic with minor side effects for acute
pain relief in patients with renal colic, and its effectiveness is comparable to that of IV morphine.
Abbreviations
ED: Emergency department; IV: Intravenous; NRS: Numeric rating scale.
Competing interests
All authors declare that they have no competing interests.
Authors contributions
PP and MJ developed the study questions, designed the methods for data
acquisition, and supervised the collection of data. BMD performed statistical
analysis. PP, MJ, and BMD jointly participated in drafting the manuscript. AD
helped in the interpretation of data and also revised the manuscript critically.
All authors read and approved the final version of the manuscript.
Author details
1
Emergency Medicine Department, Imam Hospital, Tehran University of
Medical Sciences, Keshavarz Blvd, Tehran, Iran. 2Tehran University of Medical
Sciences, Keshavarz Blvd, Tehran, Iran. 3Department of Pharmacology, School
of Medicine, Tehran University of Medical Sciences, Poursina St, Keshavarz
Blvd, Tehran, Iran.
Received: 26 July 2013 Accepted: 16 December 2013
Published: 3 January 2014
References
1. Hesse A, Brandle E, Wilbert D, Khrmann K-U, Alken P: Study on the prevalence
and incidence of urolithiasis in Germany comparing the years 1979 vs. 2000.
Eur Urol 2003, 44:709713.
2. Graham CA: Pain relief in the emergency department. Eur J Emerg Med
2010, 17:1.
3. Engeler DS, Schmid S, Schmid HP: The ideal analgesic treatment for acute
renal colictheory and practice. Scand J Urol Nephrol 2008, 42:137142.
4. Terrell KM, Hustey FM, Hwang U, Gerson LW, Wenger NS, Miller DK: Quality
indicators for geriatric emergency care. Acad Emerg Med 2009,
16:441449.
5. Vadivelu N, Anwar M: Buprenorphine in postoperative pain management.
Anesthesiol Clin 2010, 28:601609.
6. Jalili M, Fathi M, Moradi-Lakeh M, Zehtabchi S: Sublingual buprenorphine
in acute pain management: a double-blind randomized clinical trial.
Ann Emerg Med 2012, 59:276280.
7. Finlay IG, Scott R, McArdle CS: Prospective double-blind comparison of
buprenorphine and pethidine in ureteric colic. Br Med J (Clin Res Ed) 1982,
284:18301831.
8. Bijur PE, Latimer CT, Gallagher EJ: Validation of a verbally administered
numerical rating scale of acute pain for use in the emergency
department. Acad Emerg Med 2003, 10:390392.
9. Risbo A, Chraemmer Jorgensen B, Kolby P, Pedersen J, Schmidt JF:
Sublingual buprenorphine for premedication and postoperative pain
relief in orthopaedic surgery. Acta Anaesthesiol Scand 1985, 29:180182.
Submit your manuscript to a
journal and benet from:
7 Convenient online submission
7 Rigorous peer review
7 Immediate publication on acceptance
7 Open access: articles freely available online
7 High visibility within the eld
7 Retaining the copyright to your article
Submit your next manuscript at 7 springeropen.com
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5834)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (852)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (903)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (541)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (350)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (824)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (405)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Drug Education and Vice ControlDocument18 pagesDrug Education and Vice ControlKhai Loh Work100% (2)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Highland Guidelines - LDK 2013-2-15Document3 pagesHighland Guidelines - LDK 2013-2-15andrew herringNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Effect of Housing and Gender On Morphine Self-Administration in RatsDocument4 pagesThe Effect of Housing and Gender On Morphine Self-Administration in RatsGiovana Lenz100% (1)
- K Opiods For Pain BupDocument2 pagesK Opiods For Pain Bupandrew herringNo ratings yet
- Pharmacology MnemonicsDocument91 pagesPharmacology MnemonicsKnizhonki Knizhonki96% (72)
- Pharm MnemonicsDocument33 pagesPharm MnemonicsThomson George75% (4)
- Rib Fracture W: PecsDocument8 pagesRib Fracture W: Pecsandrew herring100% (1)
- Roux 2013Document7 pagesRoux 2013andrew herringNo ratings yet
- Original Article: Serratus Plane Block: A Novel Ultrasound-Guided Thoracic Wall Nerve BlockDocument7 pagesOriginal Article: Serratus Plane Block: A Novel Ultrasound-Guided Thoracic Wall Nerve Blockandrew herringNo ratings yet
- Rib Fracture SerratusDocument3 pagesRib Fracture Serratusandrew herring100% (1)
- Buprenorphine 2016-7-18Document1 pageBuprenorphine 2016-7-18andrew herringNo ratings yet
- Intravenous Lidocaine To Treat Postoperative Pain : Lidocaína Intravenosa No Tratamento Da Dor Pós-OperatóriaDocument6 pagesIntravenous Lidocaine To Treat Postoperative Pain : Lidocaína Intravenosa No Tratamento Da Dor Pós-Operatóriaandrew herringNo ratings yet
- Herring ED Intractable Abdominal pain-N+VDocument1 pageHerring ED Intractable Abdominal pain-N+Vandrew herringNo ratings yet
- Ketamine As Rescue Treatment FDocument8 pagesKetamine As Rescue Treatment Fandrew herringNo ratings yet
- 3.2.16.highland Emergency Medicine Journal Club Methods.2Document2 pages3.2.16.highland Emergency Medicine Journal Club Methods.2andrew herringNo ratings yet
- Ultrasound-Guided Block of TheDocument6 pagesUltrasound-Guided Block of Theandrew herringNo ratings yet
- Dex For Dental Pain & SwellingDocument7 pagesDex For Dental Pain & Swellingandrew herring100% (1)
- Nej MR A 1511480Document9 pagesNej MR A 1511480Tohari Masidi AminNo ratings yet
- OPR - Heroin DeathsDocument2 pagesOPR - Heroin Deathsandrew herringNo ratings yet
- CVS Action Plan v2Document1 pageCVS Action Plan v2andrew herringNo ratings yet
- Ultrasound Guided Interventional Procedures In.13Document14 pagesUltrasound Guided Interventional Procedures In.13andrew herring100% (1)
- Ultrasound Guided Interventional Procedures In.4Document13 pagesUltrasound Guided Interventional Procedures In.4andrew herringNo ratings yet
- Substance AbuseDocument19 pagesSubstance AbuseVrushank Ram100% (1)
- 5424 The Halogeno Morphides and Codides and The Mechanism of The Morphine Apomorphine Transformation3dc4Document16 pages5424 The Halogeno Morphides and Codides and The Mechanism of The Morphine Apomorphine Transformation3dc4Jo JohNo ratings yet
- Introduction To PainDocument21 pagesIntroduction To Painayanle Abdi AliNo ratings yet
- Attenuation of Heroin Withdrawl Syndrome by The Administration of High Dose Vitamin C 27.4Document9 pagesAttenuation of Heroin Withdrawl Syndrome by The Administration of High Dose Vitamin C 27.4Madalina FeraruNo ratings yet
- Cdi 8Document37 pagesCdi 8Bencio AizaNo ratings yet
- US - Article - 1col - Peri-Op - June22Document12 pagesUS - Article - 1col - Peri-Op - June22Odett NuñezNo ratings yet
- Lecture 16-17 - Opioids AnalgesicsDocument20 pagesLecture 16-17 - Opioids AnalgesicsJedoNo ratings yet
- Intro To Med. ChemDocument30 pagesIntro To Med. ChemF ParikhNo ratings yet
- Jur Nista TabDocument17 pagesJur Nista Tabnela sharonNo ratings yet
- Desomorfina - KrokodilDocument45 pagesDesomorfina - Krokodilbetsy cadena tenorioNo ratings yet
- سندDocument38 pagesسندAshkan AbbasiNo ratings yet
- Yellow List: List of Narcotic Drugs Under International ControlDocument25 pagesYellow List: List of Narcotic Drugs Under International ControlAMSNo ratings yet
- 防制藥物濫用外語宣導手冊 (英文版)Document40 pages防制藥物濫用外語宣導手冊 (英文版)Bong Sze WeeNo ratings yet
- Cdi Drugs Art 1218Document213 pagesCdi Drugs Art 1218Gian Antonio L. AbdonNo ratings yet
- Facts and Figures From PDEA Catchillar Stephanie L. NSTPDocument5 pagesFacts and Figures From PDEA Catchillar Stephanie L. NSTPJovilleNo ratings yet
- WHO Step Ladder For PainDocument5 pagesWHO Step Ladder For PainRizKyImanSariNo ratings yet
- Drug StudyDocument9 pagesDrug StudyChristine PunsalanNo ratings yet
- FDA Fails To Follow The Science On KratomDocument21 pagesFDA Fails To Follow The Science On KratomAnonymous r6OHQrqLOtNo ratings yet
- Stabilis Monographie Ketorolac TromethamineDocument5 pagesStabilis Monographie Ketorolac Tromethamineintan kusumaningtyasNo ratings yet
- Studies On Drug Codein (MM - Ardhi Mukhoffah Bil'Ilmi 13670012)Document7 pagesStudies On Drug Codein (MM - Ardhi Mukhoffah Bil'Ilmi 13670012)ArdhieEl-ilmieNo ratings yet
- Gpat 4Document17 pagesGpat 4GANESH KUMAR JELLANo ratings yet
- Cdi Lecture 1Document10 pagesCdi Lecture 1TJ del MarNo ratings yet
- Learning Objectives: Nstp-Cwts I Module 1 - Drug Education in The PhilippinesDocument13 pagesLearning Objectives: Nstp-Cwts I Module 1 - Drug Education in The PhilippinesALMONIA, GEZZIEL GANIRNo ratings yet
- Mir & MCRDocument1 pageMir & MCRMhmoud NabehNo ratings yet
- Anaesthesia LMRP 2019Document24 pagesAnaesthesia LMRP 2019Prabhat KcNo ratings yet
- Misuse of Drugs Regulations (Document57 pagesMisuse of Drugs Regulations (Terrence LiNo ratings yet