Professional Documents
Culture Documents
BR J Ophthalmol 2013 Dong Bjophthalmol 2013 303415
BR J Ophthalmol 2013 Dong Bjophthalmol 2013 303415
Uploaded by
Icha NathaniaCopyright:
Available Formats
You might also like
- Training in Ophthalmology - 9780199237593 PDFDocument474 pagesTraining in Ophthalmology - 9780199237593 PDFMuh Rifky Abdi Jausah100% (2)
- CorneaDocument465 pagesCorneawisinasa100% (2)
- Biochemistry of VisionDocument71 pagesBiochemistry of Visionroxy8marie8chanNo ratings yet
- Corneal Ulcer Diagnosis and ManagementDocument215 pagesCorneal Ulcer Diagnosis and ManagementWisniardhy Suarnata Pradana100% (1)
- 263 FullDocument7 pages263 FullPrisky DianNo ratings yet
- Single-Step Transepithelial PHDocument9 pagesSingle-Step Transepithelial PHlenniNo ratings yet
- Referat SMILEDocument10 pagesReferat SMILEarumNo ratings yet
- 369 Full PDFDocument8 pages369 Full PDFTri Umi Maslakhatut DiniahNo ratings yet
- Long Term Follow-Up Safety and E Myopia Refractive Surgery: Ffectiveness ofDocument9 pagesLong Term Follow-Up Safety and E Myopia Refractive Surgery: Ffectiveness ofayurNo ratings yet
- Sulcus Implantation of A Single-Piece Foldable Acrylic Intraocular Lens After Posterior Capsular Rupture in Cataract SurgeryDocument6 pagesSulcus Implantation of A Single-Piece Foldable Acrylic Intraocular Lens After Posterior Capsular Rupture in Cataract SurgeryPrizilia SaimimaNo ratings yet
- The Effect of Trabeculectomy On Astigmatism .99150Document5 pagesThe Effect of Trabeculectomy On Astigmatism .99150Yulias YoweiNo ratings yet
- IJGMP - Medicine - Clinical Study of DALK in Heterogeneous Corneal Diseases - Srinivas K.HDocument6 pagesIJGMP - Medicine - Clinical Study of DALK in Heterogeneous Corneal Diseases - Srinivas K.Hiaset123No ratings yet
- JurdingDocument10 pagesJurdingThobias AndrewNo ratings yet
- Artículo 1 TransprkDocument6 pagesArtículo 1 TransprkGiancarlo Varillas MerinoNo ratings yet
- Dry Eye and Corneal Sensitivity After Small Incision Lenticule Extraction and Femtosecond Laser-Assisted in Situ Keratomileusis: A Meta-AnalysisDocument7 pagesDry Eye and Corneal Sensitivity After Small Incision Lenticule Extraction and Femtosecond Laser-Assisted in Situ Keratomileusis: A Meta-Analysismohamad safiiNo ratings yet
- Intracameral Mydriatics Versus Topical Mydriatics in Pupil Dilation For Phacoemulsification Cataract SurgeryDocument5 pagesIntracameral Mydriatics Versus Topical Mydriatics in Pupil Dilation For Phacoemulsification Cataract SurgeryGlaucoma UnhasNo ratings yet
- Prostaglandin Release During Femtosecond Laser-Assisted Cataract Surgery: Main InducerDocument4 pagesProstaglandin Release During Femtosecond Laser-Assisted Cataract Surgery: Main InducerAyen AlingNo ratings yet
- MainDocument2 pagesMainSalman Saisar HidayatNo ratings yet
- Clinical Study: Endothelial Cell Loss After Phacoemulsification According To Different Anterior Chamber DepthsDocument7 pagesClinical Study: Endothelial Cell Loss After Phacoemulsification According To Different Anterior Chamber Depthseka suryaNo ratings yet
- 2011 DelyferDocument8 pages2011 DelyferCitra Azma AnggitaNo ratings yet
- 3 Piece IOL SCL FixDocument6 pages3 Piece IOL SCL FixTvrtka BenašićNo ratings yet
- Jurnal Mata 5Document6 pagesJurnal Mata 5Dahru KinanggaNo ratings yet
- Fem To Second LaserDocument4 pagesFem To Second LaserIlham Suryo Wibowo AntonoNo ratings yet
- Are Intrastromal Treatments The Future of Refractive Surgery?Document11 pagesAre Intrastromal Treatments The Future of Refractive Surgery?lacisag100% (1)
- Contact Lens & Anterior EyeDocument4 pagesContact Lens & Anterior EyePin Han NaNo ratings yet
- Small Incision Lenticule ExtractionDocument5 pagesSmall Incision Lenticule ExtractionvrlftrNo ratings yet
- Ascrs 2Document7 pagesAscrs 2leokapilNo ratings yet
- Clinical Study: Aspheric Intraocular Lenses Implantation For Cataract Patients With Extreme MyopiaDocument6 pagesClinical Study: Aspheric Intraocular Lenses Implantation For Cataract Patients With Extreme MyopiaKevin ArdiansyahNo ratings yet
- Clinical Study: Comparison of The Optical Quality Between Small Incision Lenticule Extraction and Femtosecond Laser LASIKDocument10 pagesClinical Study: Comparison of The Optical Quality Between Small Incision Lenticule Extraction and Femtosecond Laser LASIKnicoNo ratings yet
- JMedLife 05 82 PDFDocument3 pagesJMedLife 05 82 PDFYocha BangunNo ratings yet
- Persistent Corneal Edema After Collagen Cross-Linking For KeratoconusDocument6 pagesPersistent Corneal Edema After Collagen Cross-Linking For KeratoconusRestu MegantaraNo ratings yet
- The Course of Dry Eye After Phacoemulsification Surgery: Researcharticle Open AccessDocument5 pagesThe Course of Dry Eye After Phacoemulsification Surgery: Researcharticle Open AccessDestia AnandaNo ratings yet
- Jurnal 1Document6 pagesJurnal 1r_ayuNo ratings yet
- Complication Rate in Preliminary Experience in Phacoemulsification Cataract SurgeryDocument5 pagesComplication Rate in Preliminary Experience in Phacoemulsification Cataract SurgeryimtiazbscNo ratings yet
- New Perative UlcerDocument5 pagesNew Perative UlcerkautsarreNo ratings yet
- Jurnal KeratoplastyDocument58 pagesJurnal KeratoplastyFadli LatamaNo ratings yet
- Continued Endothelial Cell Loss Ten Years After Lens ImplantationDocument10 pagesContinued Endothelial Cell Loss Ten Years After Lens ImplantationPriscila MartínezNo ratings yet
- Smile HistoryDocument12 pagesSmile HistoryCindyNo ratings yet
- Clinical Study: Two-Year Accelerated Corneal Cross-Linking Outcome in Patients With Progressive KeratoconusDocument10 pagesClinical Study: Two-Year Accelerated Corneal Cross-Linking Outcome in Patients With Progressive KeratoconusPunam RazputriNo ratings yet
- The Effectiveness of Immediate Triamcinolone Acetonide Injection After Auricular Keloid Surgery: A Prospective Randomized Controlled TrialDocument8 pagesThe Effectiveness of Immediate Triamcinolone Acetonide Injection After Auricular Keloid Surgery: A Prospective Randomized Controlled TrialMarande LisaNo ratings yet
- Journal Article 13 197Document3 pagesJournal Article 13 197lazaro maizNo ratings yet
- Glaukoma TripleDocument5 pagesGlaukoma TripleR.m. IrsanNo ratings yet
- CO 2767 Alpay 120108Document6 pagesCO 2767 Alpay 120108MaRia AnastasiaNo ratings yet
- Comparison of Refractive Outcomes Between Femtosecond Laser-Assisted Cataract Surgery and Conventional Cataract SurgeryDocument7 pagesComparison of Refractive Outcomes Between Femtosecond Laser-Assisted Cataract Surgery and Conventional Cataract SurgeryoliviaNo ratings yet
- Dry Eye Disease After LASIKDocument3 pagesDry Eye Disease After LASIKRatih Kusuma DewiNo ratings yet
- Phacoemulsification Versus Manual Small Incision Cataract Surgery in Hard NuclearDocument6 pagesPhacoemulsification Versus Manual Small Incision Cataract Surgery in Hard NuclearRagni MishraNo ratings yet
- 2016 Article 229Document7 pages2016 Article 229nisa_kartikaNo ratings yet
- Out 3Document7 pagesOut 3Oldi Nelson PatadunganNo ratings yet
- iOCT Guided Simulated Subretinal InjectionsDocument8 pagesiOCT Guided Simulated Subretinal InjectionsxuedunNo ratings yet
- Kag Rully (B.IG)Document7 pagesKag Rully (B.IG)Rully Dwi SaputraNo ratings yet
- Toric ICLDocument8 pagesToric ICLjbahalkehNo ratings yet
- Patterned Laser TrabeculoplastyDocument8 pagesPatterned Laser TrabeculoplastyRinda AndreanditaNo ratings yet
- Reduced Cross-Linking Demarcation Line Depth at The Peripheral Cornea After Corneal Collagen Cross-LinkingDocument5 pagesReduced Cross-Linking Demarcation Line Depth at The Peripheral Cornea After Corneal Collagen Cross-LinkingMashhoor AlfayezNo ratings yet
- Suturas Liberables Ejo.5000718Document8 pagesSuturas Liberables Ejo.5000718Emile NumberNo ratings yet
- Therapeutic Effectiveness of Toric Implantable Collamer Lens in Treating Ultrahigh Myopic AstigmatismDocument7 pagesTherapeutic Effectiveness of Toric Implantable Collamer Lens in Treating Ultrahigh Myopic AstigmatismStephanie PfengNo ratings yet
- Intraocular Pressure 1Document6 pagesIntraocular Pressure 1Sher KhanNo ratings yet
- Original Article Laser In-Situ Keratomileusis For Refractive Error Following Radial KeratotomyDocument4 pagesOriginal Article Laser In-Situ Keratomileusis For Refractive Error Following Radial KeratotomyngunhatNo ratings yet
- Jurnal DR Mata Elis Danun Edited 31-7-16Document16 pagesJurnal DR Mata Elis Danun Edited 31-7-16'PandeKrisnaBayuPramana'No ratings yet
- Clinical Study: The Effects of Uncomplicated Cataract Surgery On Retinal Layer ThicknessDocument7 pagesClinical Study: The Effects of Uncomplicated Cataract Surgery On Retinal Layer ThicknessJohn ElfranNo ratings yet
- Mertens - The Staar Toric ICLDocument4 pagesMertens - The Staar Toric ICLAndreea L. MihalceaNo ratings yet
- Clinical Study: Photorefractive Keratectomy For Residual Myopia After Myopic Laser in Situ KeratomileusisDocument5 pagesClinical Study: Photorefractive Keratectomy For Residual Myopia After Myopic Laser in Situ KeratomileusisayurNo ratings yet
- Aesth Plast Surg - 2019 - 43 - 652-657Document6 pagesAesth Plast Surg - 2019 - 43 - 652-657HemerobibliotecaHospitalNo ratings yet
- Surgical Procedure SmileDocument8 pagesSurgical Procedure SmilearumNo ratings yet
- Surgical Management of Childhood Glaucoma: Clinical Considerations and TechniquesFrom EverandSurgical Management of Childhood Glaucoma: Clinical Considerations and TechniquesAlana L. GrajewskiNo ratings yet
- Jadwal Ruang Icu & Nicu 2022Document14 pagesJadwal Ruang Icu & Nicu 2022Icha NathaniaNo ratings yet
- Research ReportDocument19 pagesResearch ReportIcha NathaniaNo ratings yet
- Nilai Normal Pemeriksaan Kimia Klinik 2022Document2 pagesNilai Normal Pemeriksaan Kimia Klinik 2022Icha NathaniaNo ratings yet
- Jadwal NgamprahDocument1 pageJadwal NgamprahIcha NathaniaNo ratings yet
- Extrapulmonary TuberculosisDocument2 pagesExtrapulmonary TuberculosisIcha NathaniaNo ratings yet
- Diseases of Retina: The 4th Affilitated Hospital of China Medical University Eye Hospital of China Medical UniversityDocument76 pagesDiseases of Retina: The 4th Affilitated Hospital of China Medical University Eye Hospital of China Medical UniversityIcha NathaniaNo ratings yet
- Knee Sport Injury - Martinus VTDocument62 pagesKnee Sport Injury - Martinus VTIcha NathaniaNo ratings yet
- Efek Pterygium Terhadap Ukuran Astigmatisme Dan Topografi Kornea Sebelum Dan Seteah OperasiDocument6 pagesEfek Pterygium Terhadap Ukuran Astigmatisme Dan Topografi Kornea Sebelum Dan Seteah OperasiIcha NathaniaNo ratings yet
- Sebarkan Wartanya NKB 102Document2 pagesSebarkan Wartanya NKB 102Icha NathaniaNo ratings yet
- 2015 - Progress in Retinal and Eye ResearchDocument16 pages2015 - Progress in Retinal and Eye ResearchPrasetya AnugrahNo ratings yet
- Dua's Layer PDFDocument13 pagesDua's Layer PDFtasiambdNo ratings yet
- Natomy and Physiology of Cornea: Dr.K.Mahalakshmi 1 Yr PGDocument61 pagesNatomy and Physiology of Cornea: Dr.K.Mahalakshmi 1 Yr PGMaha lakshmiNo ratings yet
- Anatomy of Cornea and Ocular Surface.4Document5 pagesAnatomy of Cornea and Ocular Surface.4Cucută Alexandru-DanielNo ratings yet
- IACLE - Anatomy & Physiology of The Anterior Segment Module 1.1 - FINALDocument30 pagesIACLE - Anatomy & Physiology of The Anterior Segment Module 1.1 - FINALbushra tufailNo ratings yet
- Applied Anatomy and Physiology of CorneaDocument116 pagesApplied Anatomy and Physiology of CorneaJoubertnassif100% (1)
- Capa de Dua en La CórneaDocument8 pagesCapa de Dua en La CórneakaritoNo ratings yet
- Atlas of Refractive Surgery PDFDocument235 pagesAtlas of Refractive Surgery PDFcongNo ratings yet
- Management of Traumatic HyphemaDocument38 pagesManagement of Traumatic HyphemaAzizi AzizanNo ratings yet
- Protective Effects of Blue Light-Blocking Shades On Phototoxicity in Human Ocular Surface CellsDocument6 pagesProtective Effects of Blue Light-Blocking Shades On Phototoxicity in Human Ocular Surface CellsHans Steven KurniawanNo ratings yet
- Mechanical Superficial Keratectomy For Corneal Haze After PRKDocument4 pagesMechanical Superficial Keratectomy For Corneal Haze After PRKPhilip McNelson100% (1)
- Anatomi Fisiologi KorneaDocument11 pagesAnatomi Fisiologi KorneaMauVeeNo ratings yet
- Cornea PDFDocument465 pagesCornea PDFputraNo ratings yet
- Survey-62-P770 Keratoconus Review - QueratoconoDocument14 pagesSurvey-62-P770 Keratoconus Review - QueratoconoMaría Antonela NicolóNo ratings yet
- Cornea HandbookDocument312 pagesCornea HandbookjhesusNo ratings yet
- Junqueira's Basic Histology Text and Atlas by Anthony L. MescherDocument34 pagesJunqueira's Basic Histology Text and Atlas by Anthony L. Mescherskvelashvili2No ratings yet
- Corneal Infection and Inflammation A Colour Atlas 1stnbsped 0367457121 9780367761561 9780367457129 9781003024897Document365 pagesCorneal Infection and Inflammation A Colour Atlas 1stnbsped 0367457121 9780367761561 9780367457129 9781003024897SemehenkaNo ratings yet
- The Eye: OphthalmologyDocument12 pagesThe Eye: OphthalmologyAshley DayagNo ratings yet
- Anatomy and Physiology of Cornea: DR - Lhacha Wangdi 1st Year Resident Department of Ophthalmology Jdwnrh/KgumsbDocument47 pagesAnatomy and Physiology of Cornea: DR - Lhacha Wangdi 1st Year Resident Department of Ophthalmology Jdwnrh/KgumsbYaman MuhaisenNo ratings yet
- Keratoconus An Inflamatory DisorderDocument17 pagesKeratoconus An Inflamatory DisorderNATALIA CARMONA REYESNo ratings yet
- Waxler Petition FDA Stop LASIK (6jan11)Document32 pagesWaxler Petition FDA Stop LASIK (6jan11)Kurt Krueckeberg100% (1)
- Peripheral Ulcerative KeratitisDocument145 pagesPeripheral Ulcerative KeratitisCarlos OrtegaNo ratings yet
- Cornea Duanes Ophthalmology 2337 2337Document75 pagesCornea Duanes Ophthalmology 2337 2337Endre Shitaye KulkiNo ratings yet
- Estadística Básica AplicadaDocument742 pagesEstadística Básica AplicadaPaola González Mejía100% (1)
- 6.ANAtomy of CORNEA SrisDocument108 pages6.ANAtomy of CORNEA SrisSristi ThakurNo ratings yet
- DR Agarwals Textbook On Contact LensesDocument312 pagesDR Agarwals Textbook On Contact LensesManish MahabirNo ratings yet
BR J Ophthalmol 2013 Dong Bjophthalmol 2013 303415
BR J Ophthalmol 2013 Dong Bjophthalmol 2013 303415
Uploaded by
Icha NathaniaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
BR J Ophthalmol 2013 Dong Bjophthalmol 2013 303415
BR J Ophthalmol 2013 Dong Bjophthalmol 2013 303415
Uploaded by
Icha NathaniaCopyright:
Available Formats
Downloaded from http://bjo.bmj.com/ on July 26, 2016 - Published by group.bmj.
com
BJO Online First, published on November 13, 2013 as 10.1136/bjophthalmol-2013-303415
Laboratory science
Small incision lenticule extraction (SMILE)
and femtosecond laser LASIK: comparison
of corneal wound healing and inammation
Zixian Dong,1 Xingtao Zhou,1 Jihong Wu,1 Zhehuan Zhang,1 Tao Li,1 Zimei Zhou,2
Shenghai Zhang,1 Gang Li1
1
Institute of Ophthalmology,
Eye and ENT Hospital, Fudan
University, Shanghai, PR China
2
Department of
Ophthalmology, Bronx Lebanon
Hospital Center, Bronx,
New York, USA
Correspondence to
Dr Xingtao Zhou, Eye and ENT
Hospital, Fudan University, 83
Fenyang Road, Shanghai
200031, PR China;
xingtaozhou@163.com
Received 17 March 2013
Revised 11 September 2013
Accepted 12 October 2013
To cite: Dong Z, Zhou X,
Wu J, et al. Br J Ophthalmol
Published Online First:
[please include Day Month
Year] doi:10.1136/
bjophthalmol-2013-303415
ABSTRACT
Aim To evaluate and compare early corneal wound
healing and inammatory responses after small incision
lenticule extraction (SMILE) versus femtosecond laser
laser in situ keratomileusis (LASIK).
Methods Thirty-six eyes of 36 rabbits underwent SMILE,
while another 36 eyes of 36 rabbits were treated with
femtosecond laser LASIK. All the eyes were subjected to
the same refractive correction of 6.00 DS/1.00 DC.
Twelve eyes that had no surgery were included for control.
After euthanisation, corneal tissue sections were
evaluated with terminal deoxyribonucleotidyl transferasemediated dUTP-digoxigenin nick-end labelling (TUNEL)
assay to detect apoptosis at postoperative 4 and 24 h,
immunocytochemistry for Ki67 to detect keratocyte
proliferation at postoperative day 3, week 1 and month 1,
and immunocytochemistry for CD11b to detect
inammation at postoperative day 1, day 3 and week 1,
respectively.
Results No adverse effects were noted after SMILE or
LASIK. Corneal healing postoperatively was uneventful in
all cases. There were signicantly fewer TUNEL-positive
corneal stromal cells after the SMILE procedure at 4 and
24 h postoperatively ( p<0.01) compared with the LASIK
procedure. In addition, immunocytochemistry showed
signicantly fewer Ki67-positive cells in the SMILE group
than those in the femtosecond laser LASIK group at day 3
and week 1 postoperatively ( p<0.05), but there was little
expression of Ki67 at month 1 postoperatively in both
groups. The CD11b-positive cells were signicantly fewer
in the SMILE group at day 1, day 3 and week 1
postoperatively ( p<0.01).
Conclusions SMILE induces less keratocyte apoptosis,
proliferation and inammation compared with
femtosecond laser LASIK.
The femtosecond laser can increase the safety, efciency, precision and versatility of the lamellar incision.1 This novel technology has been largely
applied in the creation of corneal aps in laser in
situ keratomileusis (LASIK). Recently, the femtosecond laser has also been used to create an intrastromal refractive lenticule, which is regarded as
refractive lenticule extraction (ReLEx).2 ReLEx can
be further divided into femtosecond lenticule
extraction (FLEx) and small incision lenticule
extraction (SMILE), based on how the lenticle is
removed. The former allows creating and lifting
corneal aps followed by the lenticule extraction,
while in SMILE, the lenticle is removed directly via
a small incision. It is believed that SMILE is likely
to have better corneal biomechanical stability
Dong
Z, et al. Br J Ophthalmol
2013;0:17.(or
doi:10.1136/bjophthalmol-2013-303415
Copyright
Article author
their employer) 2013. Produced
postoperatively and further studies are required to
support this clinical observation.
Corneal wound healing may have a major impact
on the biomechanical stability postoperatively.
Previously, Kim et al3 found inammatory cell inltration in rabbit corneas was signicantly greater
after the ap creation by an initial femtosecond
laser than that by a mechanical microkeratome at 4
and 24 h postoperatively. A similar observation by
Netto et al4 revealed that LASIK aps formed with
a femtosecond laser of higher energy levels
(15 KHz) may result in more keratocyte cell death,
more severe cell inammation and proliferation
compared with aps using a microkeratome or a
femtosecond laser of lower energy levels (30 or
60 KHz). Results of the 60 KHz laser and microkeratome were not signicantly different for any of
the parameters at 24 h. At present, however, few
reports of the corneal wound-healing process of
ReLEx have been published. The purpose of this
study was to evaluate early corneal wound healing
and inammatory responses after SMILE and femtosecond laser-assisted (fs-LASIK).
MATERIALS AND METHODS
Animals and study design
The study adhered to the tenets of the Association
for Research in Vision and Ophthalmology
Statement for the Use of Animals in Ophthalmic
and Vision Research and was approved by the
Animal Control Committee at Eye and ENT
Hospital, Fudan University. A total of 72 New
Zealand White rabbits (with body weights of
approximately 3.0 kg) were included. All animals
were healthy and free of clinically observable
ocular disease. The animals were randomly divided
into two groups (36 rabbits in each group) for
SMILE or fs-LASIK procedure. One eye of each
rabbit was selected randomly for surgery. Twelve
eyes that had no surgery were included for control.
Animals were premedicated with a subcutaneous
injection of diazepam and atropine (1 mg) and
anesthetised with ketamine hydrochloride (35 mg/kg
intramuscularly). For additional local anaesthesia,
oxybuprocaine 0.4% drops were instilled into the
operated eyes. The SMILE and fs-LASIK procedure
were performed by a single surgeon (ZXT) and all
eyes were subjected to the same refractive correction
of 6.00 DS/1.00 DC. Postoperative medications
included topical antibiotics (tobramycin 0.3% drops,
three times/day) and steroidal anti-inammatory
drugs (uorometholone 0.1% drops, four times/day)
for 1 week.
by BMJ Publishing Group Ltd under licence.
Downloaded from http://bjo.bmj.com/ on July 26, 2016 - Published by group.bmj.com
Laboratory science
Postoperative corneal healing was observed routinely to
exclude the possibility of postoperative complications by slit
lamp
microscopy.
The
terminal
deoxyribonucleotidyl
transferase-mediated dUTP-digoxigenin nick-end labelling
(TUNEL) assay was used to detect apoptotic cells at 4 and 24 h
after surgery. Immunouorescent assays were performed to
observe the expression of Ki67, a cell marker of the G1-M
phase of mitosis, at postoperative day 3, week 1 and month
1. In addition, CD11b, a marker of monocytes, was tested at
postoperative day 1, day 3 and week 1. Six corneal samples
were obtained for histological analysis at each time point.
The procedure
SMILE procedure
The intrastromal refractive lenticule was created by a 500 kHz
femtosecond laser (VisuMax, Carl Zeiss Meditec, Jena,
Germany) and the energy density was approximately 130 nJ.
The femtosecond incisions were performed in the following
sequence5: the posterior surface of the lenticule, the lenticule
border, the anterior surface of the lenticule and the side cut
incision for the access to the lenticule. The lenticule diameter
was set at 5.5 mm and the stromal cap was completed at
100 m depth, 6.5 mm diameter centred at the pupil. The side
cut was set at 3.5 mm width and located in the 12 oclock position. After the femtosecond laser cutting procedure, a thin
spatula was inserted via the side-cut incision to make the blunt
dissection of intrastromal lenticule. The refractive lenticule was
then grasped with forceps and extracted from the cornea. The
intrastromal pocket was then ushed with a balanced salt
solution.
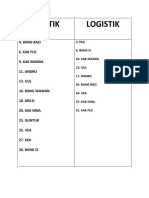
Figure 2 A bar graph showing the number of transferase-mediated
dUTP-digoxigenin nick-end labelling (TUNEL)-positive cells in the
central cornea at different time points postoperatively. The refractive
lenticule extraction (ReLEx) group had signicantly fewer
TUNEL-positive cells at 4 and 24 h after surgery compared with the
laser in situ keratomileusis (LASIK) group. **p<0.01.
centred at the pupil. The energy density was approximately
185 nJ. After lifting the ap, the underlying stroma received
refractive corrections of 6.00 DS/1.00 DC by using an
excimer laser (MEL 80; Carl Zeiss Meditec). Its uence was
180 mJ/cm2 at a frequency of 250 Hz. The optical zone diameter was 5.5 mm and the transition zone diameter was 1.0 mm
larger than the optical zone diameter in all cases. The corneal
stromal bed was ushed with a balanced salt solution. The ap
was then repositioned and sutured in the 5 and 7 oclock position using a 10-0 nylon line.
Tissue xation and sectioning
fs-LASIK procedure
The same femtosecond laser was used to create a stromal ap
with an upper hinge at 100 m corneal depth, 7 mm diameter
The corneas of operated and control eyes were harvested from
the globe. The corneas were embedded in liquid OCT compound (Leica Microsystems, Germany). The frozen tissue blocks
Figure 1 Transferase-mediated dUTP-digoxigenin nick-end labelling (TUNEL) assay of the central cornea of different groups postoperatively. (A) 4 h
after laser in situ keratomileusis (LASIK). (B) 4 h after refractive lenticule extraction (ReLEx). (C) 24 h after LASIK. (D) 24 h after ReLEx (original
magnication 400).
2
Dong Z, et al. Br J Ophthalmol 2013;0:17. doi:10.1136/bjophthalmol-2013-303415
Downloaded from http://bjo.bmj.com/ on July 26, 2016 - Published by group.bmj.com
Laboratory science
were stored at 80C until sectioning. Central corneal sections
(10 m thickness) were cut using a cryostat (Leica CM 3050S,
Germany). Sections were air dried and maintained at 80C
until staining.
Biological analysis
TUNEL assay
To detect fragmentation of DNA associated with apoptosis,
tissue sections were xed in acetone at 20C for 2 min, dried
Figure 3 Immunohistochemical staining for Ki67 of the central cornea of different groups postoperatively. (A) 3 days after laser in situ
keratomileusis (LASIK). (B) 3 days after refractive lenticule extraction (ReLEx). (C) 1 week after LASIK. (D) 1 week after ReLEx. (E) 1 month after
LASIK. (F) 1 month after ReLEx. (G) The control group (original magnication 200).
Dong Z, et al. Br J Ophthalmol 2013;0:17. doi:10.1136/bjophthalmol-2013-303415
Downloaded from http://bjo.bmj.com/ on July 26, 2016 - Published by group.bmj.com
Laboratory science
at room temperature for 5 min, and subsequently placed in
balanced salt solution. A uorescence-based TUNEL assay
(ApopTag, Cat. No. S7165; Intergen Corp, USA) was performed
according to the manufacturers instructions. Negative controls
(sections from unwounded corneas) were included in each assay.
Immunocytochemistry assays
Sections was incubated with either mouse monoclonal antibody
against CD11b (Thermo Corp, USA) diluted 1:100 or with
mouse monoclonal antibody against Ki67 (DAKO Corp,
Denmark) diluted 1:100 for 1.5 h at 37C. The secondary antibodies, uorescein-conjugated goat anti-mouse IgG (Kangcheng
Corp, China) diluted 1:800, was applied for 30 min at 37C.
Slides were mounted with medium containing 40 ,6 diamidino-2phenylindole (Thermo) to observe all cell nuclei in the tissue.
Negative controls with secondary antibody alone were included.
Photographs were obtained with a uorescence microscope
(Leica DM 4000B, Germany). All of the stained cells in seven
non-overlapping, full-thickness columns from the anterior to
the posterior stromal surface were counted. The columns where
counts were performed were randomly selected from the central
cornea of each specimen.
Figure 4 A bar graph showing the number of Ki67-positive cells in
the central cornea at 3 days, 1 week and 1 month postoperatively. The
refractive lenticule extraction (ReLEx) group had signicantly fewer
Ki67-positive cells at each time point after surgery compared with the
laser in situ keratomileusis (LASIK) group. *p<0.05, **p<0.01.
control corneas. Figure 6 depicts the quantication of the
number of CD11b-positive cells in the central corneal stroma.
Statistical analysis
Statistical analysis was performed using Microsoft Excel 2007
(Microsoft; Redmond, Washington DC, USA) and SPSS V.13.0
software (SPSS Inc, Chicago, Illinois, USA). Comparisons
between the two groups at each time point were performed
using one-way analysis of variance (ANOVA). When the
ANOVA normality assumption was incorrect by the
KolmogorovSmirnov test, the non-parametric MannWhitney
U test was used. A p value <0.05 was considered statistically
signicant.
RESULTS
No adverse effects were noted during the SMILE and fs-LASIK
procedure. The slit lamp biomicroscopy showed a little oedema
of the corneas within 1 week in both groups. All rabbits could
open their eyes naturally and resume their daily activities within
1 day postoperatively. No infection or diffuse lamellar keratitis
was noticed during the corneal healing process.
TUNEL outcomes
All corneas that underwent the SMILE or fs-LASIK procedure
had TUNEL-positive cells at the interface in the central stroma
at 4 and 24 h postoperatively (gure 1). There were signicantly
fewer TUNEL-positive stromal cells in corneas in the SMILE
group at each time point ( p<0.01). No TUNEL-positive
stromal cells were identied in control corneas. Quantitative
analysis of the number of TUNEL-positive cells in the central
corneal stroma is depicted in gure 2.
Immunohistochemisty outcomes
Both groups displayed Ki67-positive cells in the stroma at postoperative day 3 and week 1, but there was little expression of
Ki67 at 1 month postoperatively (gure 3). The SMILE group
showed fewer Ki67-positive cells when compared with the
fs-LASIK group at day 3 and week 1 postoperatively ( p<0.05).
No Ki67-positive stromal cells were detected in control corneas.
Quantitative analysis of the number of Ki67-positive cells in the
central corneal stroma is shown in gure 4. In addition, the
CD11b-positive cells were signicantly fewer in the SMILE
group at day 1, day 3 and week 1 postoperatively (gure 5)
( p<0.01). There were no CD11b-positive stromal cells in
4
DISCUSSION
It has been accepted that the corneal wound-healing response
after refractive surgical procedures is a remarkably complex
cascade.6 Epithelial injury triggers release of various kinds of
cytokines and growth factors,710 including interleukin (IL)-1,
tumour necrosis factor (TNF)-, epidermal growth factor and
platelet-derived growth factor. These cytokines directly induce
keratocyte apoptosis, hence initiating the complex cascading
response. Surrounding live keratocytes are activated and transformed into broblasts or myobroblasts, and migrate to
repopulate the depleted stroma. Meanwhile, chemokines
released from the epithelium or keratocytes would attract
inammatory cells, including monocytes, granulocytes and lymphocytes, into the corneal stroma to phagocytise the apoptotic
and necrotic debris. Subsequently, the remodelling of the extracellular matrix and the stroma was achieved by myobroblasts
through production of collagen, glycosaminoglycans, collagenases, gelatinases and matrix metalloproteinases.11 Clinically, it
has been reported by several studies that SMILE could make the
correction of ametropia with safety, efcacy, predictability and
stability12 13 However, few reports have been published on the
wound-healing and inammatory responses after SMILE. In the
present study, we demonstrated SMILE could induce less keratocyte apoptosis, proliferation and inammation compared with
fs-LASIK.
The ReLEx and fs-LASIK procedures make a refractive correction via different mechanisms. The ReLEx procedure involves
intrastromal dissection using a femtosecond laser followed by
tissue extraction, while fs-LASIK allows the stroma ablation by
an excimer laser. As we know, the excimer laser uses ultraviolet
light to break molecular bonds in the corneal stroma, whereas
the femtosecond laser is a near-infrared laser making the photodisruption of stromal tissue with less tissue injury. Moreover,
creating and lifting corneal aps is necessary in fs-LASIK and
FLEx,14 15 but not in SMILE. Thus, SMILE may stimulate less
inammatory reaction and cell death compared with fs-LASIK.
It has been demonstrated that the keratocyte apoptosis peaks
at approximately 4 h after epithelial injury and may last till
1 week after the initial insult.16 Both 4 and 24 h postoperatively
were the common time points chosen to evaluate the stromal
Dong Z, et al. Br J Ophthalmol 2013;0:17. doi:10.1136/bjophthalmol-2013-303415
Downloaded from http://bjo.bmj.com/ on July 26, 2016 - Published by group.bmj.com
Laboratory science
Figure 5 Immunohistochemical staining for CD11b of the central cornea of different groups postoperatively. (A) 1 day after laser in situ
keratomileusis (LASIK). (B) 1 day after refractive lenticule extraction (ReLEx). (C) 3 days after LASIK. (D) 3 days after ReLEx. (E) 1 week after LASIK. (F)
1 week after ReLEx. (G) The control group (original magnication 200).
cell death in previous studies.17 18 In our study, TUNEL-positive
cells were detected at the interface after SMILE and fs-LASIK
procedures at postoperative 4 and 24 h. The distribution of
apoptotic cells, mediated by proinammatory cytokines such as
IL-1 and TNF after epithelial trauma, was determined by the
Dong Z, et al. Br J Ophthalmol 2013;0:17. doi:10.1136/bjophthalmol-2013-303415
principle of the procedures.19 It has been documented that
apoptotic cells were located near the interface after LASIK,
while TUNEL-positive cells could be observed at the supercial
stroma after surface ablation procedures.20 SMILE and fs-LASIK
involve the creation of a corneal cap or ap, which facilitates
5
Downloaded from http://bjo.bmj.com/ on July 26, 2016 - Published by group.bmj.com
Laboratory science
Figure 6 A bar graph showing the number of CD11b-positive cells in
the central cornea at 1 day, 3 days and 1 week postoperatively. The
refractive lenticule extraction (ReLEx) group had signicantly fewer
CD11b-positive cells at each time point after surgery compared with
the laser in situ keratomileusis (LASIK) group. **p<0.01.
the dispersion of cytokines at the interface via tear and epithelial
debris. As a result, more severe damage would occur close to
the lamellar interface after both procedures. However, fs-LASIK
also exerts an excimer ablation effect in addition to the femtosecond laser dissection compared with SMILE. Furthermore,
SMILE would induce less epithelial trauma by small incision
and less contact with cytokines for free of lifting the cap. All
these factors may play a role, which results in fewer
TUNEL-positive stromal cells in the SMILE group than in the
fs-LASIK group ( p<0.01).
The expression of Ki67 can be used to indicate the keratocyte
proliferation that begins within 1224 h after epithelial injury.
Mohan et al21 compared the expression of Ki67 in rabbit eyes
following LASIK compared with that following photorefractive
keratectomy during 3 months postoperatively. The Ki67-positive
cells can be detected signicantly at day 3 and week 1 in the
LASIK group. In this study, Ki67-positive cells in the SMILE
group were signicantly fewer than those in the fs-LASIK group
at postoperative day 3 and week 1 ( p<0.05), indicating that
SMILE may stimulate less keratocyte proliferation. Our data are
consistent with previous ndings in post-FLEx eyes reported by
Riau et al22 Besides, there was little expression of Ki67 in both
groups at month 1 after surgery, indicating both SMILE and
fs-LASIK can initiate mild proliferation.
Also, immunohistochemical testing for the antibody
anti-CD11b was used to identify the expression of monocytes
that play a major role in inammatory inltration 824 h after
injury. OBrien et al23 studied the inammatory response in
early 1 week after excimer laser keratectomy and reported that
macrophages may contribute to transient corneal haze postoperatively. Santhiago et al24 reported that signicantly more
CD11b-positive cells were noted in the stroma after intracorneal
inlay implantation compared with the control group at 24 and
48 h postoperatively in rabbits ( p<0.05). In our study,
CD11b-positive monocyte mediated inammation was signicantly less severe in postoperative week 1 in the SMILE group
compared with the fs-LASIK group. We hypothesise that this
could be due to the following reasons: a small incision for the
lenticule extraction will produce fewer chemokines to attract
inammatory cells in the injury; the intrastromal dissection by a
femtosecond laser contributes to reduced tissue injury compared
with the stroma ablation by an excimer laser; there was less necrotic debris in the interface after ReLEx.
The femtosecond laser energy level may have an impact on
the extent of corneal cell death and inammatory response after
6
ap formation by a femtosecond laser.25 Previously, Netto et al4
found that rabbit corneas that had aps formed by the 15 KHz
laser had more stromal cell death, greater stromal cell proliferation and greater monocyte inux in the cornea at 24 h after
surgery than corneas that had aps formed with the 30 or
60 KHz laser. Similarly, de Medeiros et al26 reported that
higher energy levels can trigger more cell death and inammatory inltration when the femtosecond laser is used to create
corneal aps. The energy density of the VisuMax femtosecond
laser in our study was 130 nJ for the lenticule and 185 nJ for
the ap at a repetition rate of 500 kHz. This may induce mild
keratocyte apoptosis and corneal inammation.
In summary, our animal study showed that ReLEx induces a
lower degree of keratocyte apoptosis, proliferation and inammation compared with fs-LASIK. Further studies are needed to
evaluate whether this novel procedure may induce less postoperative regression.
Contributors ZD and XZ: design and conduction of the study; ZD, XZ, JW, ZZ, TL,
ZZ, SZ and GL: data analysis and interpretation; ZD: manuscript preparation; JW, ZZ,
TL, ZZ, SZ and GL: manuscript review; XZ and JW: nal approval of the manuscript.
Funding Supported in part by National Natural and Science Program Grant
A040413 and Pudong Science and Technology Development and Innovation fund
Grant PKJ2009-Y01.
Competing interests None.
Provenance and peer review Not commissioned; externally peer reviewed.
Open Access This is an Open Access article distributed in accordance with the
Creative Commons Attribution Non Commercial (CC BY-NC 3.0) license, which
permits others to distribute, remix, adapt, build upon this work non-commercially,
and license their derivative works on different terms, provided the original work is
properly cited and the use is non-commercial. See: http://creativecommons.org/
licenses/by-nc/3.0/
REFERENCES
1
2
3
4
6
7
10
11
12
13
14
Soong HK, Malta JB. Femtosecond lasers in ophthalmology. Am J Ophthalmol
2009;147:18997.
Kim P, Sutton GL, Rootman DS. Applications of the femtosecond laser in corneal
refractive surgery. Curr Opin Ophthalmol 2011;22:23844.
Kim JY, Kim MJ, Kim TI, et al. A femtosecond laser creates a stronger ap than a
mechanical microkeratome. Invest Ophthalmol Vis Sci 2006;47:599604.
Netto MV, Mohan RR, Medeiros FW, et al. Femtosecond laser and microkeratome
corneal aps: comparison of stromal wound healing and inammation. J Refract
Surg 2007;23:66776.
Vestergaard A, Ivarsen AR, Asp S, et al. Small-incision lenticule extraction for
moderate to high myopia: predictability, safety, and patient satisfaction. J Cataract
Refract Surg 2012;38:200310.
Dupps WJ Jr, Wilson SE. Biomechanics and wound healing in the cornea. Exp Eye
Res 2006;83:70920.
Tuominen IS, Tervo TM, Teppo AM, et al. Human tear uid PDGF-BB, TNF-alpha
and TGF-beta1 vs corneal haze and regeneration of corneal epithelium and
subbasal nerve plexus after PRK. Exp Eye Res 2001;72:63141.
Wilson SE, He YG, Weng J, et al. Epithelial injury induces keratocyte apoptosis:
hypothesized role for the interleukin-1 system in the modulation of corneal tissue
organization and wound healing. Exp Eye Res 1996;62:3257.
Mohan RR, Mohan RR, Kim WJ, et al. Modulation of TNF-alpha induced apoptosis
in corneal broblasts by transcription factor NF-kb. Invest Ophthalmol Vis Sci
2000;41:132734.
Wilson SE, Chen L, Mohan RR, et al. Expression of HGF, KGF, EGF and receptor
messenger RNAs following corneal epithelial wounding. Exp Eye Res
1999;68:37797.
Funderburgh JL, Mann MM, Funderburgh ML. Keratocyte phenotype mediates
proteoglycan structure: a role for broblasts in corneal brosis. J Biol Chem
2003;278:4562937.
Shah R, Shah S, Sengupta S. Results of small incision lenticule extraction: all-in-one
femtosecond laser refractive surgery. J Cataract Refract Surg 2011;37:12737.
Sekundo W, Kunert KS, Blum M. Small incision corneal refractive surgery using the
small incision lenticule extraction (SMILE) procedure for the correction of myopia
and myopic astigmatism: results of a 6 month prospective study. Br J Ophthalmol
2011;95:3359.
Sekundo W, Kunert K, Russmann C, et al. First efcacy and safety study of
femtosecond lenticule extraction for the correction of myopia: six-month results.
J Cataract Refract Surg 2008;34:151320.
Dong Z, et al. Br J Ophthalmol 2013;0:17. doi:10.1136/bjophthalmol-2013-303415
Downloaded from http://bjo.bmj.com/ on July 26, 2016 - Published by group.bmj.com
Laboratory science
15
16
17
18
19
20
Blum M, Kunert K, Schrder M, et al. Femtosecond lenticule extraction for the
correction of myopia: preliminary 6-month results. Graefes Arch Clin Exp
Ophthalmol 2010;248:101927.
Netto MV, Mohan RR, Ambrsio R Jr, et al. Wound healing in the cornea: a review
of refractive surgery complications and new prospects for therapy. Cornea
2005;24:50922.
Song JS, Kim JH, Yang M, et al. Mitomycin-C concentration in cornea and aqueous
humor and apoptosis in the stroma after topical mitomycin-C application: effects of
mitomycin-C application time and concentration. Cornea 2007;26:4617.
Netto MV, Mohan RR, Sinha S, et al. Effect of prophylactic and therapeutic
mitomycin C on corneal apoptosis, cellular proliferation, haze, and long-term
keratocyte density in rabbits. J Refract Surg 2006;22:56274.
Wilson SE, Netto M, Ambrsio R Jr. Corneal cells: chatty in development,
homeostasis, wound healing, and disease. Am J Ophthalmol 2003;136:5306.
Wilson SE, Kim W-J. Keratocyte apoptosis: implications on corneal wound healing,
tissue organization, and disease. Invest Ophthalmol Vis Sci 1998;39:2206.
Dong Z, et al. Br J Ophthalmol 2013;0:17. doi:10.1136/bjophthalmol-2013-303415
21
22
23
24
25
26
Mohan RR, Hutcheon AE, Choi R, et al. Apoptosis, necrosis, proliferation, and
myobroblast generation in the stroma following LASIK and PRK. Exp Eye Res
2003;76:7187.
Riau AK, Angunawela RI, Chaurasia SS, et al. Early corneal wound healing and
inammatory responses after refractive lenticule extraction (ReLEx). Invest
Ophthalmol Vis Sci 2011;52:621321.
OBrien TP, Li Q, Ashraf MF, et al. Inammatory response in the early stages of
wound healing after excimer laser keratectomy. Arch Ophthalmol
1998;116:14704.
Santhiago MR, Barbosa FL, Agrawal V, et al. Short-term cell death and
inammation after intracorneal inlay implantation in rabbits. J Refract Surg
2012;28:1449.
Santhiago MR, Wilson SE. Cellular effects after laser in situ keratomileusis ap
formation with femtosecond lasers: a review. Cornea 2012;31:198205.
de Medeiros FW, Kaur H, Agrawal V, et al. Effect of femtosecond laser energy level
on corneal stromal cell death and inammation. J Refract Surg 2009;25:86974.
Downloaded from http://bjo.bmj.com/ on July 26, 2016 - Published by group.bmj.com
Small incision lenticule extraction (SMILE)
and femtosecond laser LASIK: comparison of
corneal wound healing and inflammation
Zixian Dong, Xingtao Zhou, Jihong Wu, Zhehuan Zhang, Tao Li, Zimei
Zhou, Shenghai Zhang and Gang Li
Br J Ophthalmol published online November 13, 2013
Updated information and services can be found at:
http://bjo.bmj.com/content/early/2013/11/13/bjophthalmol-2013-30341
5
These include:
References
This article cites 26 articles, 6 of which you can access for free at:
http://bjo.bmj.com/content/early/2013/11/13/bjophthalmol-2013-30341
5#BIBL
Open Access
This is an Open Access article distributed in accordance with the Creative
Commons Attribution Non Commercial (CC BY-NC 3.0) license, which
permits others to distribute, remix, adapt, build upon this work
non-commercially, and license their derivative works on different terms,
provided the original work is properly cited and the use is
non-commercial. See: http://creativecommons.org/licenses/by-nc/3.0/
Email alerting
service
Receive free email alerts when new articles cite this article. Sign up in the
box at the top right corner of the online article.
Topic
Collections
Articles on similar topics can be found in the following collections
Open access (226)
Ophthalmologic surgical procedures (1203)
Notes
To request permissions go to:
http://group.bmj.com/group/rights-licensing/permissions
To order reprints go to:
http://journals.bmj.com/cgi/reprintform
To subscribe to BMJ go to:
http://group.bmj.com/subscribe/
You might also like
- Training in Ophthalmology - 9780199237593 PDFDocument474 pagesTraining in Ophthalmology - 9780199237593 PDFMuh Rifky Abdi Jausah100% (2)
- CorneaDocument465 pagesCorneawisinasa100% (2)
- Biochemistry of VisionDocument71 pagesBiochemistry of Visionroxy8marie8chanNo ratings yet
- Corneal Ulcer Diagnosis and ManagementDocument215 pagesCorneal Ulcer Diagnosis and ManagementWisniardhy Suarnata Pradana100% (1)
- 263 FullDocument7 pages263 FullPrisky DianNo ratings yet
- Single-Step Transepithelial PHDocument9 pagesSingle-Step Transepithelial PHlenniNo ratings yet
- Referat SMILEDocument10 pagesReferat SMILEarumNo ratings yet
- 369 Full PDFDocument8 pages369 Full PDFTri Umi Maslakhatut DiniahNo ratings yet
- Long Term Follow-Up Safety and E Myopia Refractive Surgery: Ffectiveness ofDocument9 pagesLong Term Follow-Up Safety and E Myopia Refractive Surgery: Ffectiveness ofayurNo ratings yet
- Sulcus Implantation of A Single-Piece Foldable Acrylic Intraocular Lens After Posterior Capsular Rupture in Cataract SurgeryDocument6 pagesSulcus Implantation of A Single-Piece Foldable Acrylic Intraocular Lens After Posterior Capsular Rupture in Cataract SurgeryPrizilia SaimimaNo ratings yet
- The Effect of Trabeculectomy On Astigmatism .99150Document5 pagesThe Effect of Trabeculectomy On Astigmatism .99150Yulias YoweiNo ratings yet
- IJGMP - Medicine - Clinical Study of DALK in Heterogeneous Corneal Diseases - Srinivas K.HDocument6 pagesIJGMP - Medicine - Clinical Study of DALK in Heterogeneous Corneal Diseases - Srinivas K.Hiaset123No ratings yet
- JurdingDocument10 pagesJurdingThobias AndrewNo ratings yet
- Artículo 1 TransprkDocument6 pagesArtículo 1 TransprkGiancarlo Varillas MerinoNo ratings yet
- Dry Eye and Corneal Sensitivity After Small Incision Lenticule Extraction and Femtosecond Laser-Assisted in Situ Keratomileusis: A Meta-AnalysisDocument7 pagesDry Eye and Corneal Sensitivity After Small Incision Lenticule Extraction and Femtosecond Laser-Assisted in Situ Keratomileusis: A Meta-Analysismohamad safiiNo ratings yet
- Intracameral Mydriatics Versus Topical Mydriatics in Pupil Dilation For Phacoemulsification Cataract SurgeryDocument5 pagesIntracameral Mydriatics Versus Topical Mydriatics in Pupil Dilation For Phacoemulsification Cataract SurgeryGlaucoma UnhasNo ratings yet
- Prostaglandin Release During Femtosecond Laser-Assisted Cataract Surgery: Main InducerDocument4 pagesProstaglandin Release During Femtosecond Laser-Assisted Cataract Surgery: Main InducerAyen AlingNo ratings yet
- MainDocument2 pagesMainSalman Saisar HidayatNo ratings yet
- Clinical Study: Endothelial Cell Loss After Phacoemulsification According To Different Anterior Chamber DepthsDocument7 pagesClinical Study: Endothelial Cell Loss After Phacoemulsification According To Different Anterior Chamber Depthseka suryaNo ratings yet
- 2011 DelyferDocument8 pages2011 DelyferCitra Azma AnggitaNo ratings yet
- 3 Piece IOL SCL FixDocument6 pages3 Piece IOL SCL FixTvrtka BenašićNo ratings yet
- Jurnal Mata 5Document6 pagesJurnal Mata 5Dahru KinanggaNo ratings yet
- Fem To Second LaserDocument4 pagesFem To Second LaserIlham Suryo Wibowo AntonoNo ratings yet
- Are Intrastromal Treatments The Future of Refractive Surgery?Document11 pagesAre Intrastromal Treatments The Future of Refractive Surgery?lacisag100% (1)
- Contact Lens & Anterior EyeDocument4 pagesContact Lens & Anterior EyePin Han NaNo ratings yet
- Small Incision Lenticule ExtractionDocument5 pagesSmall Incision Lenticule ExtractionvrlftrNo ratings yet
- Ascrs 2Document7 pagesAscrs 2leokapilNo ratings yet
- Clinical Study: Aspheric Intraocular Lenses Implantation For Cataract Patients With Extreme MyopiaDocument6 pagesClinical Study: Aspheric Intraocular Lenses Implantation For Cataract Patients With Extreme MyopiaKevin ArdiansyahNo ratings yet
- Clinical Study: Comparison of The Optical Quality Between Small Incision Lenticule Extraction and Femtosecond Laser LASIKDocument10 pagesClinical Study: Comparison of The Optical Quality Between Small Incision Lenticule Extraction and Femtosecond Laser LASIKnicoNo ratings yet
- JMedLife 05 82 PDFDocument3 pagesJMedLife 05 82 PDFYocha BangunNo ratings yet
- Persistent Corneal Edema After Collagen Cross-Linking For KeratoconusDocument6 pagesPersistent Corneal Edema After Collagen Cross-Linking For KeratoconusRestu MegantaraNo ratings yet
- The Course of Dry Eye After Phacoemulsification Surgery: Researcharticle Open AccessDocument5 pagesThe Course of Dry Eye After Phacoemulsification Surgery: Researcharticle Open AccessDestia AnandaNo ratings yet
- Jurnal 1Document6 pagesJurnal 1r_ayuNo ratings yet
- Complication Rate in Preliminary Experience in Phacoemulsification Cataract SurgeryDocument5 pagesComplication Rate in Preliminary Experience in Phacoemulsification Cataract SurgeryimtiazbscNo ratings yet
- New Perative UlcerDocument5 pagesNew Perative UlcerkautsarreNo ratings yet
- Jurnal KeratoplastyDocument58 pagesJurnal KeratoplastyFadli LatamaNo ratings yet
- Continued Endothelial Cell Loss Ten Years After Lens ImplantationDocument10 pagesContinued Endothelial Cell Loss Ten Years After Lens ImplantationPriscila MartínezNo ratings yet
- Smile HistoryDocument12 pagesSmile HistoryCindyNo ratings yet
- Clinical Study: Two-Year Accelerated Corneal Cross-Linking Outcome in Patients With Progressive KeratoconusDocument10 pagesClinical Study: Two-Year Accelerated Corneal Cross-Linking Outcome in Patients With Progressive KeratoconusPunam RazputriNo ratings yet
- The Effectiveness of Immediate Triamcinolone Acetonide Injection After Auricular Keloid Surgery: A Prospective Randomized Controlled TrialDocument8 pagesThe Effectiveness of Immediate Triamcinolone Acetonide Injection After Auricular Keloid Surgery: A Prospective Randomized Controlled TrialMarande LisaNo ratings yet
- Journal Article 13 197Document3 pagesJournal Article 13 197lazaro maizNo ratings yet
- Glaukoma TripleDocument5 pagesGlaukoma TripleR.m. IrsanNo ratings yet
- CO 2767 Alpay 120108Document6 pagesCO 2767 Alpay 120108MaRia AnastasiaNo ratings yet
- Comparison of Refractive Outcomes Between Femtosecond Laser-Assisted Cataract Surgery and Conventional Cataract SurgeryDocument7 pagesComparison of Refractive Outcomes Between Femtosecond Laser-Assisted Cataract Surgery and Conventional Cataract SurgeryoliviaNo ratings yet
- Dry Eye Disease After LASIKDocument3 pagesDry Eye Disease After LASIKRatih Kusuma DewiNo ratings yet
- Phacoemulsification Versus Manual Small Incision Cataract Surgery in Hard NuclearDocument6 pagesPhacoemulsification Versus Manual Small Incision Cataract Surgery in Hard NuclearRagni MishraNo ratings yet
- 2016 Article 229Document7 pages2016 Article 229nisa_kartikaNo ratings yet
- Out 3Document7 pagesOut 3Oldi Nelson PatadunganNo ratings yet
- iOCT Guided Simulated Subretinal InjectionsDocument8 pagesiOCT Guided Simulated Subretinal InjectionsxuedunNo ratings yet
- Kag Rully (B.IG)Document7 pagesKag Rully (B.IG)Rully Dwi SaputraNo ratings yet
- Toric ICLDocument8 pagesToric ICLjbahalkehNo ratings yet
- Patterned Laser TrabeculoplastyDocument8 pagesPatterned Laser TrabeculoplastyRinda AndreanditaNo ratings yet
- Reduced Cross-Linking Demarcation Line Depth at The Peripheral Cornea After Corneal Collagen Cross-LinkingDocument5 pagesReduced Cross-Linking Demarcation Line Depth at The Peripheral Cornea After Corneal Collagen Cross-LinkingMashhoor AlfayezNo ratings yet
- Suturas Liberables Ejo.5000718Document8 pagesSuturas Liberables Ejo.5000718Emile NumberNo ratings yet
- Therapeutic Effectiveness of Toric Implantable Collamer Lens in Treating Ultrahigh Myopic AstigmatismDocument7 pagesTherapeutic Effectiveness of Toric Implantable Collamer Lens in Treating Ultrahigh Myopic AstigmatismStephanie PfengNo ratings yet
- Intraocular Pressure 1Document6 pagesIntraocular Pressure 1Sher KhanNo ratings yet
- Original Article Laser In-Situ Keratomileusis For Refractive Error Following Radial KeratotomyDocument4 pagesOriginal Article Laser In-Situ Keratomileusis For Refractive Error Following Radial KeratotomyngunhatNo ratings yet
- Jurnal DR Mata Elis Danun Edited 31-7-16Document16 pagesJurnal DR Mata Elis Danun Edited 31-7-16'PandeKrisnaBayuPramana'No ratings yet
- Clinical Study: The Effects of Uncomplicated Cataract Surgery On Retinal Layer ThicknessDocument7 pagesClinical Study: The Effects of Uncomplicated Cataract Surgery On Retinal Layer ThicknessJohn ElfranNo ratings yet
- Mertens - The Staar Toric ICLDocument4 pagesMertens - The Staar Toric ICLAndreea L. MihalceaNo ratings yet
- Clinical Study: Photorefractive Keratectomy For Residual Myopia After Myopic Laser in Situ KeratomileusisDocument5 pagesClinical Study: Photorefractive Keratectomy For Residual Myopia After Myopic Laser in Situ KeratomileusisayurNo ratings yet
- Aesth Plast Surg - 2019 - 43 - 652-657Document6 pagesAesth Plast Surg - 2019 - 43 - 652-657HemerobibliotecaHospitalNo ratings yet
- Surgical Procedure SmileDocument8 pagesSurgical Procedure SmilearumNo ratings yet
- Surgical Management of Childhood Glaucoma: Clinical Considerations and TechniquesFrom EverandSurgical Management of Childhood Glaucoma: Clinical Considerations and TechniquesAlana L. GrajewskiNo ratings yet
- Jadwal Ruang Icu & Nicu 2022Document14 pagesJadwal Ruang Icu & Nicu 2022Icha NathaniaNo ratings yet
- Research ReportDocument19 pagesResearch ReportIcha NathaniaNo ratings yet
- Nilai Normal Pemeriksaan Kimia Klinik 2022Document2 pagesNilai Normal Pemeriksaan Kimia Klinik 2022Icha NathaniaNo ratings yet
- Jadwal NgamprahDocument1 pageJadwal NgamprahIcha NathaniaNo ratings yet
- Extrapulmonary TuberculosisDocument2 pagesExtrapulmonary TuberculosisIcha NathaniaNo ratings yet
- Diseases of Retina: The 4th Affilitated Hospital of China Medical University Eye Hospital of China Medical UniversityDocument76 pagesDiseases of Retina: The 4th Affilitated Hospital of China Medical University Eye Hospital of China Medical UniversityIcha NathaniaNo ratings yet
- Knee Sport Injury - Martinus VTDocument62 pagesKnee Sport Injury - Martinus VTIcha NathaniaNo ratings yet
- Efek Pterygium Terhadap Ukuran Astigmatisme Dan Topografi Kornea Sebelum Dan Seteah OperasiDocument6 pagesEfek Pterygium Terhadap Ukuran Astigmatisme Dan Topografi Kornea Sebelum Dan Seteah OperasiIcha NathaniaNo ratings yet
- Sebarkan Wartanya NKB 102Document2 pagesSebarkan Wartanya NKB 102Icha NathaniaNo ratings yet
- 2015 - Progress in Retinal and Eye ResearchDocument16 pages2015 - Progress in Retinal and Eye ResearchPrasetya AnugrahNo ratings yet
- Dua's Layer PDFDocument13 pagesDua's Layer PDFtasiambdNo ratings yet
- Natomy and Physiology of Cornea: Dr.K.Mahalakshmi 1 Yr PGDocument61 pagesNatomy and Physiology of Cornea: Dr.K.Mahalakshmi 1 Yr PGMaha lakshmiNo ratings yet
- Anatomy of Cornea and Ocular Surface.4Document5 pagesAnatomy of Cornea and Ocular Surface.4Cucută Alexandru-DanielNo ratings yet
- IACLE - Anatomy & Physiology of The Anterior Segment Module 1.1 - FINALDocument30 pagesIACLE - Anatomy & Physiology of The Anterior Segment Module 1.1 - FINALbushra tufailNo ratings yet
- Applied Anatomy and Physiology of CorneaDocument116 pagesApplied Anatomy and Physiology of CorneaJoubertnassif100% (1)
- Capa de Dua en La CórneaDocument8 pagesCapa de Dua en La CórneakaritoNo ratings yet
- Atlas of Refractive Surgery PDFDocument235 pagesAtlas of Refractive Surgery PDFcongNo ratings yet
- Management of Traumatic HyphemaDocument38 pagesManagement of Traumatic HyphemaAzizi AzizanNo ratings yet
- Protective Effects of Blue Light-Blocking Shades On Phototoxicity in Human Ocular Surface CellsDocument6 pagesProtective Effects of Blue Light-Blocking Shades On Phototoxicity in Human Ocular Surface CellsHans Steven KurniawanNo ratings yet
- Mechanical Superficial Keratectomy For Corneal Haze After PRKDocument4 pagesMechanical Superficial Keratectomy For Corneal Haze After PRKPhilip McNelson100% (1)
- Anatomi Fisiologi KorneaDocument11 pagesAnatomi Fisiologi KorneaMauVeeNo ratings yet
- Cornea PDFDocument465 pagesCornea PDFputraNo ratings yet
- Survey-62-P770 Keratoconus Review - QueratoconoDocument14 pagesSurvey-62-P770 Keratoconus Review - QueratoconoMaría Antonela NicolóNo ratings yet
- Cornea HandbookDocument312 pagesCornea HandbookjhesusNo ratings yet
- Junqueira's Basic Histology Text and Atlas by Anthony L. MescherDocument34 pagesJunqueira's Basic Histology Text and Atlas by Anthony L. Mescherskvelashvili2No ratings yet
- Corneal Infection and Inflammation A Colour Atlas 1stnbsped 0367457121 9780367761561 9780367457129 9781003024897Document365 pagesCorneal Infection and Inflammation A Colour Atlas 1stnbsped 0367457121 9780367761561 9780367457129 9781003024897SemehenkaNo ratings yet
- The Eye: OphthalmologyDocument12 pagesThe Eye: OphthalmologyAshley DayagNo ratings yet
- Anatomy and Physiology of Cornea: DR - Lhacha Wangdi 1st Year Resident Department of Ophthalmology Jdwnrh/KgumsbDocument47 pagesAnatomy and Physiology of Cornea: DR - Lhacha Wangdi 1st Year Resident Department of Ophthalmology Jdwnrh/KgumsbYaman MuhaisenNo ratings yet
- Keratoconus An Inflamatory DisorderDocument17 pagesKeratoconus An Inflamatory DisorderNATALIA CARMONA REYESNo ratings yet
- Waxler Petition FDA Stop LASIK (6jan11)Document32 pagesWaxler Petition FDA Stop LASIK (6jan11)Kurt Krueckeberg100% (1)
- Peripheral Ulcerative KeratitisDocument145 pagesPeripheral Ulcerative KeratitisCarlos OrtegaNo ratings yet
- Cornea Duanes Ophthalmology 2337 2337Document75 pagesCornea Duanes Ophthalmology 2337 2337Endre Shitaye KulkiNo ratings yet
- Estadística Básica AplicadaDocument742 pagesEstadística Básica AplicadaPaola González Mejía100% (1)
- 6.ANAtomy of CORNEA SrisDocument108 pages6.ANAtomy of CORNEA SrisSristi ThakurNo ratings yet
- DR Agarwals Textbook On Contact LensesDocument312 pagesDR Agarwals Textbook On Contact LensesManish MahabirNo ratings yet