Professional Documents
Culture Documents
Clinical Pharmakokinetic of Kotrim
Clinical Pharmakokinetic of Kotrim
Uploaded by
Defi OktafiaCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Clinical Pharmakokinetic of Kotrim
Clinical Pharmakokinetic of Kotrim
Uploaded by
Defi OktafiaCopyright:
Available Formats
Clinical Pharmacokmetlcs 5: 405-423 (1980)
0312-5963/80/0900-0405/$04.75/0
AD IS Press Australasia Pty Ltd. All nghts reserved.
Clinical Pharmacokinetics of Co-trimoxazole
(trimethoprim-sulphamethoxazole)
Rajni B. Patel and Peter G. Welling
Center for Health Sciences. School of Pharmacy. Umversity of Wisconsin. Madison.
Wisconsin
Summary
The combillalioll trimethoprim-sulphametllOxazole (co-trimoxazole) is used c1illical(v for
the treatmelll of a \'Oriety of illfectiolls due to Gram-positil'e alld Gram-llegatipe orgallisms;
particular(I' for urillary alld respiratory tract il(fectiolls While both trimet/wprim alld sulphametlwxazole are mainly bacteriostatic when used alone. their combilled effect tellds to be bactericidal. SYllergism is due to sequelltial blockade at two separate steps ill bacterial folate
metabolism. resultillg ill illhibitioll of deoxyribollllcleic acid sylllhesis.
The optimum collcelltralioll ratio of trimetllOprim:sulphametllOxazole {i)r a bactericidal
effect paries betwf:ell 1:5 alld I :40. which is collsistellt with their relatipe minimum inhibitory
concellIration (MIC) palues against susceptible organisms. The combination is administered
principal(I' by the oral route. although it is also giwlI parellleralb' and rectalb'. A single oral
dose of 160mg trimetllOprim and 800mg sulphametllOxazole gives peak sertlm lel'els at approximately 411 of 1.2 to 2}Jg / ml trimetllOprim alld 26 to 63}Jg / ml sulpl1ametl1oxazole. After repeated 12 -I/Our(v doses. minimum sertlm /el'e/s are 1.3 to 2.8}Jg / ml and 32 to 63}Jg/ ml {i)r trinll;'tllOprim and slllphametllOxazole respectil'e(I'. The high con celli ration of slllphametllOxazole
in serum re/atil'e to that of trimethoprim is dlle to the greater tisslle penetration of trimetllOprim. The high sulphametlwxazole:trimethoprim cOllcentration ratio in serum does Iwt
always occur in extral'ascular tissues. However, this is partially compensated {i)r by tile higl1
bacteriostatic actil'ity of trimethoprim alone in tissues.
The 2 compounds are bound to plasma proteins to similar extellIs. Both trimethoprim and
sulphamethoxazole obey first order absorption. distributioll. alld elimination killetics. The disposition t!f sulphamethoxazole in the body after oral doses has been described ill .terms of onecompartment model kinetics, while both Olle-compartmelll and lII'o-compartment model
kinetics hOl'e been IIsed to describe the disposition of trimetllOprim.
Both compoullds are cleared from the body predominantly via the kidneys. slIlphametllOxazole being excreted mainly ill the acetylated {i)rm. Average elimillatioll half-lives of trimetllOprim and slIlphamethoxazole are II alld 9h respectively, althollgh there is considerable
illdividual variatioll ill these I'ailles. The clearance of both compoullds is not marked(1' affected
by declining rellal function until creatinille clearance falls be/ow 30ml/ min. /n severe renal
failure, the elimination ha(f-/ives of both drugs may increase to 45 to 60h and adJustment of
dosage is necessary to avoid renal toxicity. Both trimetlwprim alld sulphamet!Joxazole appear
406
Clinical Pharmacokinetics of Co-trimoxazole
ill bile at concelllrations similar to those observed in serum, although the sulphametllOxa-
zole:trimet/lOprim concentration ratio ill bile is somewhat less than that ill serum.
Trimet/wprim and sulphamet/lOxazole give rise to 011(1' occasional side effects, which are
characteristic of the illdividual compollnds. Principal reactions are tilOse associated with
sulphonamide sensitil'ity, alld rellaltoxicity ill patients with impaired renalfilllc/ioll. Anaemia
due to impaired folate metabolism may be a problem ill some patients.
There has been considerable clinical experience
attesting to the efficacy of the combination trimethoprim-sulphamethoxazole in the treatment of
localised and systemic infections (Avery, 1971;
Brumfitt et a\., 1973; Reeves, 1971; Wormser,
I 978). The synergistic bactericidal effect of the combination, which has been demonstrated against a wide
variety of Gram-positive and Gram-negative organisms (Brumfitt et a\., 1973; Darrell et aI., 1968;
Dornbusch, 1971; Wormser, 1978), has been attributed to sequential blockade of bacterial enzyme
systems associated with tetrahydrofolate synthesis
(Bushby, 1977). The proposed mechanism of action
of trimethoprim-sulphamethoxazole, as depicted by
Reeves (1971) is illustrated in figure I.
The sulphonamide competitively inhibits utilisation of para-aminobenzoate for the synthesis of folic
acid, while trimethoprim competitively inhibits the
activity of bacterial folate retluctase. This enzyme
normally reduces dihydrofolate to tetrahydrofolate, a
necessary step in the folate-dependent synthesis of
deoxyribonucleic acid.
The principal advantages claimed in the use of the
drug combination, compared with single drug therapy, are the reduction in overall drug minimum inhibitory concentration (MIC) values against susceptible organisms, increased bactericidal activity, and
reduced risk of the emergence of resistant strains
(Brumfitt et a\., 1973; Reeves, 1971). The latter claim
is controversial however. Similar incidences of the
emergence of bacteria resistant to the combination,
and to trimethoprim alone, have been reported during
treatment of urinary tract infections (Huovinon and
Toivanen, 1980; Pearson et. a\., 1979), while the
emergence of Shigella strains which are resistant to
trimethoprim-sulphamethoxazole may represent a
significant clinical problem (Bannatyne et a\., 1980;
Taylor et a\., 1980).
Trimethoprim was selected for the combination
because of its high broad spectrum of antibacterial activity (Roth et aI., 1962). Sulphamethoxazole was
selected as the most appropriate sulphonamide component on the basis of its similar pharmacokinetic
behaviour to that of trimethoprim. Both drugs are
characterised by efficient absorption from oral doses,
first-order absorption and elimination kinetics, and
have similar elimination half-lives. Thus, they provide a combination which yields predictable and
reproducible drug concentrations in the body, that
can be maintained at fixed dose levels and intervals
(Kaplan et aI., 1973).
I. Clinica/lndications
The degree of antibacterial synergism obtained
with the combination trimethoprim-sulphamethoxazc\e was demonstrated ill l'itro by Darrell et al. (1968)
who obtained between 2- and 8-fold potentiation of
trimethoprim activity against Staphylococcus aureUS.
Streptococcus p.l'rogelles. Streptococcus plleumolliae.
Haell10philus illfluellzae, Eschericllia coli. Klebsiella.
Sa/mollella. and Shigella species, and between 16-
and 64-fold potentiation of trimethoprim activity
against N. gOllorrllOeae and Proteus mirabi/is. by the
addition of sulphonamide.
The extent of potentiation depends on the ratio of
the 2 compounds present, and tends to be maximal
when the ratio of their concentrations is similar to
that of their respective MIC values (Bushby and
Hitchings, 1968). As MIC's for susceptible organisms range from 5 to 50ug/ml and from 0.25 to
Clinical Pharmacokinetics of Co-trimoxazole
407
2J.1g/ml for sulphamethoxazole and trimethoprim
respectively <Dornbusch, 1971), a desirable ratio for
maximum potentiation is approximately 20 parts sulphamethoxazole to I part trimethoprim (Reeves,
1971). However, th<! ratio varies widely for different
bacterial species and Bhoni (1969) has suggested an
optimum ratio range of between 5: I and 40: 1 for different organisms. In the case of N. gOllorrhoeae, the
ratio of MIC's for the 2 agents is actually reversed,
the organism in some instances being more sensitive
to sulphonamides than to trimethoprim (Reeves,
1971), and a more recent study has shown ill I'ilro
that a 19: I sulphamethoxazole: trimethoprim concentration ratio is minimally synergistic and sometimes antagonistic to gonococci (Rein et aI., 1980).
The generally accepted sequential mechanism of
sulphamethoxazole-trimethoprim synergism ill I'itro
has been challenged by Lacey (1979), who favours a
mechanism involving simultaneous binding of both
drugs to bacterial dihydrofolate reductase (Poe,
I 977). Lacey also disputes the incidence of synergism
due to the combination in vivo, and suggests that trimethoprim alone may be adequate to treat most urinary tract infections, and a variety of other infections.
The combination has been used clinically for a
number of infections including those of the respiratory tract; gonococcal urethritis, cervicitis and
pharyngitis; enteric infections; bacterial meningitis;
Nocardia infections; some cases of bacterial endocarditis; infections due to Pllellll1o(l'stis carillii, and brucellosis. The major use of trimethoprim-sulphamethoxazole has, however, been in the treatment of
acute and chronic urinary tract infections, and also
for prophylaxis in recurrent urinary tract infections.
The combination is superior to ampicillin in the treatment of chronic urinary tract infections due to ampicillin-sensitive Escherichia coli (Gleckman, 1975),
and has been shown to be superior to methenamine
PABA
Sulphonamide -
- iFolic
acid
Trimethoprim -
-iFolinic
acid
.Precursors
~+
Purines
~
DNA
Fig. 1. Summary of the mode of action of trimethoprim and sulphonamide (after Journal of Clinical Pathology 24: 430-437,
1971; by permission of author and editor).
Clinical Pharmacokinetics of Co-trimoxazole
408
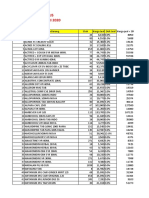
Table I. Dosage routes and pharmacokinetic values for trimethoprim and sulphamethoxazole administered in combination"
Parameter
Value
TMpC
References
SMZC
Routes of administration
Oral
Kaplan et al. (1973)
Intramuscular
Lazaro et al. (1978)
Rectal
Liedtke and Haase (1979)
Intravenous
Bailey (1977);
Grose et al. (1979);
Schmidt et al. (1979)
Siber et al. (1979)
Intravesical
Hachen (1978)
Pharmacokinetics
Absorption efficiency
Highb
Absorption lag time (h)
1.4-2.4
0.5-2.7
Welling et al. (1973)
Absorption half-life (h)
0.4-2.0
0.7-2.0
Welling et al. (1973)
1-8
1-2
3-8
4
Welling et al. (1973)
Kaplan et al. (1973)
Bach et al. (1973)
1.6-1.7 f
1.9-5.09
1.2f
26-28 f
41-63 f
37.1f
Bach et al. (1973)
Schwartz and Rieder (1970)
Welling et al .. (1973)
Schwartz and Ziegler (1969)
Bach et al. (1973)
Kaplan et al. (1973)
Welling et al. (1973)
16
17
31
Kaplan et al. (1973)
Kremers et al. (1974)
Rieder et al. (1974)
Welling et al. (1973)
Elimination half-life (h)
8.3-25.3
8.9-11.8
7.5-27.0
11.4
6.1-22.5
7.6-9.3
62-8.7
9.3
Percent bound to plasma
45
66
37-79
70-135
(14-48)
100
(30)
(72h)
Kaplan et al. (1973)
(96h)
Kremers et al. (1974)
81
98
(16)
(96h)
Schwartz and Rieder (1970)
55
70
(31)
(48h)
Welling et al. (1973)
Percent of oral dose
excreted unchanged
in urine
75
Schwartz and Rieder (1970)
Cknical Pharmacokinetics of Co-trimoxazole
409
Table I. (contd.)
Parameter
Apparent dlstnbutlon
volume(q
Value
References
TMpc
SMZc
126
94
121
17.7
12
12
Liedtke and Haase (1979)
Schwartz and Rieder (1970)
Welling et al. (1973)
a All pharmacoklnetlc values are obtained after single oral doses.
b A controlled companson of tnmethopnm and sulphamethoxazole bloavallablhty for oral and parenteral dosage forms has
not been carned out.
c TMP = tnmethopnm. SMZ = sulphamethoxazole.
d Time of peak drug concentration In serum.
e Maximum concentration of drug In serum.
Data obtained from a dose of 160mg tnmethopnm and 800mg sulphamethoxazole.
g Data obtained from a dose of 400mg tnmethopnm and 2g sulphamethoxazole.
h RatiO of mean maximum sulphamethoxazole to maximum tnmethoprim concentrations In serum or plasma. regardless of
time at which the maximum levels occur.
I Urinary excretion of sulphamethoxazole represents both free and conjugated forms of the drug. The percentage of the
dose excreted as free drug IS given In parentheses.
J Calculated distribution volumes assume quantitative absorption from oral (Schwartz and Rieder. 1970; Welhng et al . 1973)
and rectal (Liedtke and Haase, 1979) doses, and are uncorrected for drug binding to plasma proteins.
(Harding and Ronald, 1974) and comparable with
nitrofurantoin (Ronald et aI., 1975) in the prevention
of urinary tract infection.
2. Assay ill Biological Fluids
The 2 principal methods which have been used to
measure the concentration of trimethoprim in biological fluids are those based on microbiological procedures similar to that first described by Bushby and
Hitchings (1968) using Bacillils pllmillis as test
organism, and on the fluorimetric method originally
described by Schwam et al. (1969). While good
agreement has been obtained between the 2 methods
(Reeves, 1971), the fluorimetric procedure has enjoyed greater use because of its greater sensitivity,
specificity, and shorter assay time. Sigel et al. (1973)
have used high performance liquid chromatography
for the separation and identification of various metabolites of trimethoprim in urine.
Sulphamethoxazole has been measured routinely
in biological fluids by the colourimetric method of
Bratton and Marshall (\939), adapted by Rieder
(1972) for the separation of unchanged sulphonamide
from its conjugated metabolites. There have been no
reports of cross-reactions between the mt;\hods for
the determination of trimethoprim and sulphamethoxazole in biological fluid when both compounds are
present.
More recently, high performance liquid chromatography methods have been described for the analysis of trimethoprim (Weinfeld and Macasieb, 1979)
and combined trimethoprim-sulphamethoxazole
(Vree et aI., 1978) in biological fluids.
3. Fundamental Pharmacokinelic Properties
The routes of administration, together with some
pharmacokinetic values, for the combination trimethoprim-sulphamethoxazole are given in table I.
ClinICal PharmacokinetICs of Co-tnmoxazole
While the combination has been administered by a
number of routes. it is generally given orally. It ha...
been used intravenously in severely ill patient..
(Bailey. 1977; Grose et al.. 1979) and also by intramuscular (Lazaro et al.. 1978) and rectal (Liedtke
and Haase. 1979) routes. Intravesical injection wa...
used successfully in patients with recent vertebral
trauma or paraplegia. suffering from severe chronic
urinary tract infections and various pathological conditions of the urinary tract.
410
ated sulphonamide (Nolte and Buttner. 1973. 1974;
Kremers et al.. 1974). Doubling the dose results in a
2-fold increa...e in circulating levels of both trimethoprim and sulphamethoxazoie. indicating doseindependent kinetics over that dosage range
<Dornbusch. 1976).
Following repeated I h intravenous infusions of
150mg trimethoprim and 750mg sulphamethoxazole
every Sh. Siber et al. (1979) reported peak plasma
concentrations of trimethoprim. measured at 5 min
3.1 Absorption
Both trimethoprim and sulphamethoxazole are
efficiently absorbed after oral administration.
whether administered alone or in combination
<Brumfitt et al.. 1969; Kaplan et al.. 1970. 1973;
Korn et al.. 1972; Schwartz and Ziegler. 1969; Welling et al.. 1973). There is however. considerable individual variation in absorption rates. Following a
single dose of 160mg trimethoprim and 800mg sulphamethoxazole. peak serum or plasma levels of 1.2
to 2~g/ml trimethoprim. 26 to 63~g/ml free sulphamethoxazole. and 35 to 65IJg/ml free and conjugated
sulphamethoxazole occur at between I and Sh
<Bach et al.. 1973; Bergan and Brodwall. 1972;
Kremers et al.. 1974; Nolte and Buttner. 1973. 1974;
Schwartz and Rieder. 1970; Schwartz and Ziegler.
1969; Welling et al.. 1973)_ Typical plasma profiles
of non-conjugated sulphamethoxazole and trimethoprim in 4 healthy individuals who received
single oral doses of 160mg trimethoprim and SOOmg
sulphamethoxazole are reproduced on a semilogarithmic scale in figure 2_
Following repeated administration of the above
dosage at 12h intervals. equilibrium circulating concentrations are achieved in 2 to 3 days_ Steady-state
minimum serum concentrations. taken immediately
before the morning or evening dose. vary between 32
and 63IJg/mi and between 1_3 and 2_8~g/ml for sulphamethoxazole and trimethoprim. respectively. At
steady-state. free circulating sulphamethoxazole comprises approximately SO % of total. free and conjug-
80
60
40
30
20
10
4
3
Fig_ 2_ Individual plasma concentration-time curves of trimetl!opnm and sulphamethoxazole in 4 healthy adult subjects
after a single oral dose of 160mg trimethoprim and SOOmg
sulphamethoxazole in the form of 2 tablets (after Chemotherapy 15: 337-355, 1970; by permission of author and editorI.
Ctinical Pharmacokinetics of Co-tnmoxazole
postinfusion of 4.2 to 10.9I1g/ml. Although circulating concentrations of sulphonamide were not described. the authors suggest that repeated intravenous
infusions may be useful to achieve peak trimethoprim
concentrations in excess of Sl1g/ml. which may be
necessary to treat pneumocystis pneumonia. Similar
observations were made by Grose et al. (1979) who
obtained mean trimethoprim and sulphamethoxazole
concentrations of 3.4 and 46.3pg/ml immediately
following a single 1h infusion of 160mg trimethoprim and 800mg sulphamethoxazole to cancer
patients. Following repeated infusions 8-hourly for 4
days. mean peak concentrations had increased to
8.8pg/ml and 106pg/ml for trimethoprim and sulphamethoxazole. respectively. No drug-related toxicity was observed during this treatment. and this
type of dosage may be appropriate for serious infections due to susceptible organisms in children and
adults (Grose et al.. 1979; Schmidt et al.. 1979; Siber
et al.. 1979).
Absorption of both compounds from rectal suppositories compares well with that from oral dosage
forms. Following repeated 8-hourly doses of suppositories containing 160mg trimethoprim and
800mg sulphamethoxazole. average steady-state serum concentrations of free and total sulphamethoxazole. and trimethoprim. were 40 to 5 I. 48 to 63. and
1.4 to 2.2pg/ml, respectively (Liedtke and Haase.
1979).
3.2 Distribution
Due to its greater fat solubility. trimethoprim is
capable of crossing biological membranes and
penetrating into extravascular and fatty tissues to a
greater extent than sulphamethoxazole. This phenomenon is reflected in a greater apparent distribution
volume of approximately 100 to 120L for trimethoprim. compared to 12 to 18L for sulphamethoxazole (Liedtke and Haa"e. 1979; Schwartz and
Rieder. 1970; Welling et al.. 1973).
The larger distribution volume of trimethoprim
compared with sulphamethoxazole together with
411
their similar absorption efficiencies. provides the
rationale for the sulphamethoxazole:trimethoprim
dosage ratio of 5: I. As a consequence of the different
distribution characteristics of the 2 compounds. a 5: 1
dosage ratio results in a plasma concentration ratio
which provides maximum antibacterial effect (Bergan
and Brodwall. 1972; Nolte and Buttner. 1973. 1974;
Rieder and Schwartz. 1975>' Thus. peak plasma or
serum ratios of sulphamethoxazole to trimethoprim
ranging from 16 to 31 have been reported (Bach et
al..1973; Kaplan et al.. 1973; Wellingetal., 1973).
Due to the similar elimination rates of the 2 compounds from the body, the favourable sulphamethoxazole:trimethoprim concentration ratio is maintained
in the circulation during at least 24h following a
single dose in both normal and uraemic individuals
(Welling et aI., 1973), and also during repeated doses
(Kremers et al.. 1974, 1975).
Although the 5: I dosage ratio gives rise to a
desirable drug concentration ratio in ~Iasma, a useful
situation for many systemic infections, the position is
reversed for some extravascular and more deep-seated
sites. A favourable drug ratio in the circulation must
be accompanied by a less favourable ratio elsewhere
in the body. However, the low MIC for trimethoprim
against many susceptible organisms may partially
compensate for thIS. An indication of the probable
relative drug distribution in man is provided by the
animal data described in table II (Bushby and Hitchings. 1968; Reeves, 1971).
Trimethoprim is 45 % and sulphamethoxazole
66% bound to plasma proteins at pH 7.4 and 37C
when added to human plasma at therapeutic concentrations (Hall, 1961; Korn et aI., 1972; Schwartz
and Rieder. 1970). While drug which is bound to
plasma proteins is in equilibrium with unbound, active drug, so that bound drug provides a potentially
active reservoir, only the drug fraction which is unbound is available to exert its antibacterial action at
anyone time. The concentrations of circulating trimethoprim and sulphamethoxazole should therefore
always be considered in terms of the percentage of
unbound drug when making comparisons with ill
vitro MIC values. Similarly. the distribution vol~mes
Clinical Pharmacokinetics of Co-trimoxazole
412
Table II. Tnmethoprim and sulphamethoxazole concentrations in ammal tissue relatIVe to concentrations In serum
(Bushby and Hitchings, 1968; Reeves, 19711
Tissue
Animal
Tissue: Serum
concentration ratio
tnmethopom
Liver
Lungs
Heart
Kidney
Brain
Rat
Mouse
Rabbit
6.2
3.2
Rat
Mouse
Rabbit
2.0
17.5
Rat
Mouse
Rabbit
1.2
6.5
Rat
Mouse
Rabbit
7.5
7.6
Rat
Rabbit
0.08
sulphamethoxazole
0.3
-a
0.25
0.4
0.5
0.35
0.6
0.6
2.4
0.05
0.25
Not reported.
for trimethoprim and sulphamethoxazole given in
table I are probably underestimates of the 'true'
volumes based on intravascular and extravascular
equilibrium of unbound drug. However, the lack of
information regarding the binding and intrinsic distribution characteristics of trimethoprim and sulphamethoxazole in extravascular tissues and fluids
precludes accurate determination of their actual distribution volumes.
Following single oral doses of the trimethoprimsulphamethoxazole combination to patients, serum
profiles of both free and conjugated sulphamethoxazole have been adequately described by one-compartment model kinetics, with first-order absorption,
metabolism, and excretion. In the case of trimethoprim, however, while one-compartment model
kinetics adequately described serum and urine drug
profiles in some individuals, two-compartment model
kinetics provided a more satisfactory description of
the data in others (Welling et aI., 1973). Application
of two-compartment model kinetics is consistent with
the extensive tissue distribution of trimethoprim.
Trimethoprim distributes into saliva to a greater
extent than sulphamethoxazole. In healthy individuals, the saliva:plasma concentration ratios of trimethoprim and sulphamethoxazole were 1.13 and
0.016 respectively (Eatman et at, 1977), These
values are in reasonable agreement with predicted
values based on the degree of ionisation of the weakly
basic trimethoprim (pKa 7.3) and the weakly acidic
sulphamethoxazole (pKa 5.6) in blood and saliva.
Following oral doses to patients, however, trimethoprim concentrations in saliva were 1 to 8 times
higher than those in serum (Hansen et aI., 1973).
Superior penetration by trimethoprim, relative to
sulphamethoxazole, has been reported for human
breast milk (Miller and Salter, 1973), non-inflamed
prostatic tissue (Dabhoiwala et a!., 1976; Madsen et
aI., 1976; Oosterlink et aI., 1975), seminal fluid
(Gnarpe and Friberg, 1976; Malmborg et aI., 1975),
vaginal fluid (Stamey and Condy, 1975), normal and
inflamed lung tissue (Hansen et aI., 1973), and bile
fluid (Rieder, 1973a; Rieder et aI., I 974a).
In some cases, however, tissue penetration of trimethoprim has been shown not to be significantly
different from that of sulphamethoxazole. The levels
of trimethoprim and sulphamethoxazole in cerebrospinal fluid were 30 to 509(., and approximately
209(., respectively of plasma concentrations (Fries et
aI., 1975), while aqueous humour:plasma concentration ratios of between 0.1 and 1.0, and 0.25, have
been reported for trimethoprim and sulphamethoxazole respectively (Pohjanpelto et aI., 1974; Salmon et
aI., 1975).
3.3 Placental Transfer
Both trimethoprim and sulphamethoxazole cross
the human placenta (Reid et aI., 1975; Ylikorkala et
413
Clinical Pharmacokinetics of Co-tnmoxazole
aI., 1973). In healthy women undergoing therapeutic
abortion, equilibrium levels of the 2 compounds in
fetal serum were statistically indistinguishable from
those in maternal serum. Concentrations of trimethoprim in amniotic fluid, cord blood, and some
fetal tissues were 27 4, 62, and 46 W. respectively of
maternal serum concentrations, while corresponding
values for sulphamethoxazole were 25, 71, and 4 W.
(Reid et aI., 1975).
3.4 Metabolism
Studies by Schwartz et al. (1970), and subsequently by Sigel et al. (1973), showed that 10 to 20 W.
of trimethoprim is metabolised, the balance being excreted unchanged in the urine. Principal metabolites
of trimethoprim are the 1-, and 3-oxides. and the 3'-,
and 4'-hydroxyderivatives. A minor a-hydroxy metabolite has also been identified. The metabolites, which
have been shown to be bacteriologically inactive, or to
have much reduced activity in an ill 1'i1'o mouse
model, are excreted mainly as conjugates in urine
(Rieder, I 973b; Sigel et al.. 1973).
Metabolism of sulphamethoxazole occurs predominantly by N 4 -acetylation, although the
glucuronide conjugate has also been identified
(Rieder, 1972). The acetylated metabolite, which does
not possess significant antibacterial activity. comprises approximately 20!J{, of total sulphonamide in
the circulation, but accounts for 60 to 80'!(, of total
urinary sulphamethoxazole (Kremers et aI., 1974;
Kuhne et al.. 1976; Schwartz and Rieder, 1970;
Welling et aI., 1973).
50',-----------------------------------------,
40
I
I
30
Trimethopnm (TMP)
o Sulphamethoxazole (SMZ)
08
fo
...,
":--..
1MP Cy a 28x- OI8 ; r=0.716)
~--~~~'==~::::~----~-,~~----,- _____ _
5MZ Cy=39x-029 ;
20
40
60
Creatinine clearance (ml/min)
r=o;;;;------OO--il
.
0
e
80
100
120
140
Fig. 3. Relation between half-lives of tnmethopnm and sulphamethoxazole and creatinine clearance follOWing a single oral
dose of 160mg tnmethopnm and 800mg sulphamethoxazole.
Patient A had the longest half-life for tnmethopnm (46.3h) but the shortest half-life for sulphamethoxazole (21.8h). ThiS
patient had a consistently alkaline unne (pH / 7.5). Patient B had the longest half-life for sulphamethoxazole (50.2h) but a
remarkably short half-life for trimethoprim (13.8h), and persistently aCid urine (pH < 4.9) [after Annals of Internal Medicine 78:
491-497, 1973; by permission of author and editod
Chnlcal Pharmacokinetics of Co-tnmoxazole
~~4~*8-1~2~16-2~0'---~3~O--~4~O~~~
Time (hours)
Fig. 4. Unne concentrations of tnmethoprim I. ... } and
sulphamethoxazole ( - - \ In normal subJects, and of tnmethoprim (- . -) and sulphamethoxazole (---) In uraemic
subjects follOWing a single oral dose of 160mg tnme!hopnm
and 800mg sulphamethoxazole (after Journal of InfectiOUs
Diseases 128 (5uppl.): 5556-5566, Nov 1973: by permission of
author and edltorl.
3.5 Renal Excretion
Both trimethoprim and the free and conjugated
forms of sulphamethoxazole are cleared from the
body predominantly I'ia the urine. With normal renal
function, the plasma (elimination) half-life of sulphamethoxazole is approximately 9h, while that of trimethoprim, is approximately II h, although there is
considerable individual variation in these values
(Kaplan et aI., 1973; Rieder et aI., 1974b; Welling et
aI., 1973). There appears to be no phenotype effect in
the rate of sulphamethoxazole acetylation (Vree et al..
1978). Vree et al. (1978, 1979) have shown that N4_
acetyl-sulphamethoxazole has an elimination half-life
of 3.5h, i.e., one-third that of the parent drug, and its
414
renal clearance is independent of urine pH and urine
flow.
Cumulative 72 to 96h urinary recovery accounts
for 80 to 90 % of oral doses as unchanged trimethoprim and 95 % as total sulphonamide. Urinary
excretion of trimethoprim is favoured in acid urine
while excretion of sulphamethoxazole tends to increase in alkaline urine (Craig and Kunin, 1973;
Welling et al.. 1973). These observations are consistent with renal tubular reabsorption of the un-ionised
forms of these compounds.
The elimination rate of neither compound is significantly affected by impaired renal function for
creatinine clearance values above 30ml/min. However. for creatinine clearances below this value. and
especially in severe renal impairment, the elimination
half-lives of both drugs may increase to as much as
45 to 60h. and the quantity of drug cleared in the
urine decreases.
The similar behaviour of trimethoprim and sulphamethoxazole in declining renal function is demonstrated in figure 3. Although a considerable prolongation in the elimination half-life in renal impairment is
expected for trimethoprim, which is cleared predominantly unchanged in urine, a marked prolongation is
not the case for sulphamethoxazole, which is extensively conjugated. Delayed elimination of sulphamethoxazole in severely impaired renal function may,
however. be further exacerbated due to product inhibition by the acetylated metabolite of sulphamethoxazole, whose concentrations in the body may be elevated in uraemic patients (Wel1ing et aI., 1973). Both
trimethoprim and sulphamethoxazole are efficiently
removed from the circulation by haemodialysis
(Craig and Kunin, 1973). However, this may not be
the case with acetylsulphamethoxazole (Baethke et aI.,
1972).
The concentrations of trimethoprim and sulphamethoxazole normal1y observed in urine far exceed
the MIC values for most ~usceptible organisms (Bach
et aI., 1973; Bergan and Brodwal1, 1976; Kaplan et
aI., 1973; Rieder et aI., 1974b). Although urinary
levels of both compounds are reduced in renal impairment, they stil1 exceed MIC values in most cases, and
Climcal Pharmacokinetics of Co-tnmoxazole
415
also maintain a favourable therapeutic ratio for bactericidal effect <Baethke et aI., 1972; Rieder et aI.,
1974b; Sharpstone, 1969). Typical mean urinary
concentrations during 48h following single oral doses
of 160mg trimethoprim and 800mg sulphamethoxazole in normal and uraemic subjects are shown in
figure 4 (Welling et a\., 1973), while the relationship
between trimethoprim and sulphamethoxazole levels
in urine in variable renal function and representative
MIC values for susceptible organisms are shown in
figure 5.
While the distribution characteristics of trimethoprim appear to be unaffected by uraemia, distribution of sulphamethoxazole into tissues appears to
increase with declining renal function, presumably
because of reduced binding to serum proteins (Craig
and Kunin, 1973; Welling et a\., 1973).
In the nephrotic syndrome. the concentrations of
both trimethoprim and sulphamethoxazole in urine
are higher, and the elimination half-lives somewhat
shorter. than might be expected from the degree of
impaired renal function <Bergan and Brodwall. 1976).
It is suggested that in this condition. which is often
associated with proteinuria, protein entering urine
may carry with it protein-bound substances.
Dosage adjustment in patient!> with impaired renal
function is discussed in section 7.
3.6 Biliary Excretion
Trimethoprim is excreted in bile at higher concentrations relative to those in !>erum than sulphamethoxazole. However, both compounds appear in
400
Tnmethoprim
200
100
80
60
40
20
10
8
6
4
"i
t.
..
.1.,.
MlCe.-1
..
I I;.
VT'~.-::.,,"'7\~::r:#!U-EBrr'i:"":i!~~i':'ii;;7:i;;~_1m~IT:.~+ml0~~,rn!
Sulphamethoxazole
o 20
40 sb 8'0 100 120 140 b
Creatinine clearance (ml/min)
Fig. 5. Relation between urine concentration of tnmethopnm and sulphamethoxazole In urine collected dunng 0-2, 2-4, 4-6
and 6-12h following a single oral dose of 160mg trimethopnm and 800mg sulphamethoxazole, and creatimne clearance.
The shaded areas represent literature MIC values for some susceptible bactena (after Annals of Internal MediCine 78: 491-497,
1973; by permission of author and editor).
Clinical Pharmacokinetics of Co-trlmoxazole
bile at concentrations, and at a concentration ratio,
considered to be effective for infections of the biliary
system (Neuman et aI., 1972; Rieder, 1973a; Rieder
et a\., 1974a; Sharpstone et a\., 1972).
In 10 female patients with T-tubes introduced into
the bile duct after cholecystectomy, and who had
received 160mg trimethoprim and 800mg sulphamethoxazole orally the concentration of trimethoprim in bile decreased from 140-267 ')(, of
plasma levels at 4h to 26-88 ')(, at 24h afterdosing. In
contrast, the concentration of sulphamethoxazole in
bile increased from 46-50 '1(, of plasma levels at 4h to
73-111 'l(, at 24h (Rieder et a\., 1974a). Thus, the rate
of biliary excretion of the 2 compounds tends, after a
single administration, to change in a reciprocal man-.
ner with time. Consistent with thIS, the mean half-life
of the decline in bIliary levels of trimethoprim, from
limited data, was 7. 7h compared with 14h in plasma,
while the equivalent biliary and plasma elimination
half-lives for sulphamethoxazole were 11.8h and
7.2h, respectively.
4. TrimetllOprim-SulphametllOxazole
in Children
The combination trimethoprim-sulphamethoxazole has been used successfully in children for a
variety of infections, including non-typhoid Sa/mO/lel/a gastroenteritis (Marks, 1975; Marks et a\.,
1973), urinary tract infections <Howard and Howard,
1978; Lewin el al.. 1973; Smellie et aI., 1976;
Wilfert, 1973; Wilfert and Gutman, 1975),
osteomyelitis, pneumonia, empyema, septicaemia,
congenital renal abnormalities (Wilfert, 1973;
Wilfert and Gutman, 1975) and acute otitis media
(Lewin et aI., 1973),
Absorption of both compounds in children appears to be efficient, even in cases of gastroenteritis
(Marks, 1975; Marks et a\., 1973) and in other
serious illnesses (Fowle et a\., 1975; Wilfert and Gutman, 1975).
Mean serum concentrations of both compounds in
I 0 children receiving a suspension dosage form pro-
416
viding 200mg trimethoprim and 1000mg sulphamethoxazole per m 2 body surface area daily in 2
divided doses, are shown in figure 6. Serum sampling
times were infrequent, but were sufficient to
demonstrate initial peak levels of I )Jg/ml and
20)Jg/ ml trimethoprim and sulphamethoxazole,
respectively. Accumulation then occurred during 24
hours to approach steady-state peak levels of
1.6)Jg/01I trimethoprim and 40llg/ ml sulphamethoxazole Although satisfactory clinical response wa!. obtained with this regimen, it is suggested that the levels
of trimethoprim and sulphamethoxazole obtained
may be insufficient for the treatment of invasive
parenchymal infections (Wilfert and Gutman, 1975).
Evidence has been pre!.ented that the elimination
half-life of sulphamethoxazole is considerably longer
during the first 10 days of life than in the adult. It
then falls rapidly to about 9h at 3 weeks of age, and
even further to 4-5h at I year through until 6 to 8
years when it increases, to approach the adult value
<Brumfitt et al.. 1973).
Some support for the concept of shorter half-lives
of both compounds in children, compared with
adults, is provided in the study of Lewin et al. (1973),
which showed no significant accumulation in plasma
concentrations during repeated dosing to 5 female infants and one II-year-old child who received 18Smg
trimethoprim and 925mg sulphamethoxazole daily in
2 divided doses. However, the lack of drug accumulation with repeated doses was inconsistent with the observation that pla.<;ma concentrations 'of both drugs
were prolonged following the initial dose.
5. Adl'erse Reactio/ls
Trimethoprim-sulphamethoxazole therapy is generally well tolerated, and the incidence of side effects
is low. The drug combination nevertheless exposes
the patient to possible toxicities of 2 different medications (Brumfitt et ai, 1973; Gleckman, 1973;
Kasanen et aI., 1974).
Toxic reactions to trimethoprim are uncommon,
partially because of the far greater sensitivity of bac-
417
Clinical Pharmacokinetics of Co-tnmoxazole
terial dihydrofolate reductase to the action of trimethoprim compared with the mammalian system.
The concentration of trimethoprim necessary to inhibit E.\chericllia coli dihydrofolate reductase by 50
percent is approximately 5 x 10 4 times less than that
required for the same degree of inhibition of the
mammalian enzyme (Brumfitt et aI., 1973). On the
usual daily therapeutic dosage of 320mg trimethoprim, 160mg sulphamethoxazole haematological changes suggestive of abnormal metabolism are
rare. even with chronic administration (Bateson et aI.,
1976; Girdwood, 1976; Jenkins et aI., 1970). No abnormalities of hepatic, haematopoietic, or renal function were observed in 25 children who received
20mg/kg trimethoprim, 100mg/kg sulphamethoxazole daily for 7 days, although mean serum concentrations measured 2h after the ninth dose were
9.6~g/ml and 174~g/ml for trimethoprim and ~ul-
phamethoxazole, respectively (Marks et al.. 1973).
However, in patients with folic acid deficiency
(Bateson et aI., 1976; Dawborn et aI., 1973; Girdwood, 1976; Jenkins et aI., 1970), alcoholics, patients
with malabsorption syndrome, pregnant women, and
elderly patients with chronic megaloblastic anaemia
(Chanarin and England, 1972: Hill and Kerr, 1973),
supplementary folate may be required with trimethoprim.
Sulphamethoxazole gives rise to the side effects
and sensitivity reactions associated with the sulphonamides in general. Gastrointestinal symptoms
(Bernstein, 1975; Frisch, 1973) occur in less than
3 % of patients. Skin eruptions are seen less frequently, but reactions such as the Stevens-Johnson
syndrome, toxic epidermal necrolysis, and exfoliative
dermatitis, although rare, may be serious and even
fatal (Bernstein, 1975; Frisch, 1973). The acetylated
2D.-------------------------------------0E~~An
15
1.0
E
'~
E
.t:
0.
,g 0.5
a;
E
'S
Time (hours)
Fig. 6. Means of trimethopnm (TMP) and sulphamethoxazole (SMZ) concentrations In serum of 10 children receiving daily
doses of 200mg trimethoprim and 1000mg sulphamethoxazole per m 2 in two equal doses [after Canadian Medical Association
Journal 112 (Supp\.): 73-76. June 1975; by permission of author and edltorL
Clmical Pharmacokinetics of Co-tnmoxazole
418
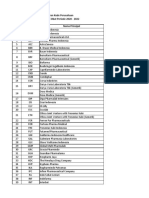
Table III. Proposed dOSIng schedule for tnmethopnm-suphamethoxazole in varying degrees of impaired renal functIOn. based
on both creatinine clearance and serum creatinine values (Hansen. 1978; Rieder et al.. 1974bl
Kidney functIOn
creatinine
clearance
(ml/mlnl
Recommended dosage regimen"
serum
creatlnlne b
(mg/100mll
Men < 3.0
Women < 2.0
Dosage as for patient With normal renal function
15-25
Men 3.0-7.0
Women 2.0-4.5
One standard dose 12-hourly for 3 days. later 1 standard
dose every 24h. as determined by control analYSIS C
< 15
Men >7.0
Women >4.5
One half to 1 standard dose every 24h as determined by control
analYSIS d
>25
a Standard dose for adults -- 2 tablets containing 160mg tnmethopnm and 800mg suphamethoxazole. 12-hourly.
b Serum creatinine can be used as a baSIS for dose adlustment In cases of chronic but not acute or subacute kidney failure
(see funher Blornsson. 1979).
c Total sulphamethoxazole should be measured In plasma 12h after every 3rd day of treatment. Treatment should be stopped If the plasma concentration exceeds 150lIg/ml. and continued as recommended when levels are' 120llg/ml.
d Control analysIS as in (cl. but With plasma sulphamethoxazole determinations every second day as a minimum.
metabolite of sulphamethoxazole can give rise to
crystalluria, which may be prevented by adequate
fluid intake (Buchanan, 1978; Siegel, 1977).
The combination trimethoprim-sulphamethoxazole may cause a decrease in creatinine clearance, and
an increase in serum creatinine levels, in patients with
normal renal function (Berglund et aI., 1975; Bye,
1976). This effect appears to be because of interference with renal tubular secretIon of creatinine, and
glomerular filtration measured by other techniques is
not affected.
Deterioration of renal function may be produced
by trimethoprim-sulphamethoxazole in patients with
underlying renal disease, but renal function is
restored in most cases upon discontinuation of the
drug (Bailey and little, 1976; Kalowski et al., 1973).
The combination has been free of this side effect in
other studies which have included patients with abnormal renal function (Denneberg et aI., 1976;
Rosenfeld et al., 1975; Tasker et aI., 1975). Animal
studies have not supported the suggestion of trimethoprim-sulphamethoxazole ill renal failure
(Robinson et al., 1977), and observed deterioration of
renal function may have been related to sulphamethoxazole hypersensitivity (Richmond et aI., 1979).
Miscellaneous side effects of trimethoprim-sulphamethoxazole include headache, confusion, hal1ucinations, depression, tremor, fever, and vasculitis (Girdwood, 1976; Wahlin and Rosman, 1976). Haematological abnormalities such as thrombocytopenia,
leucopenia, and agranulocytosis have been reported in
patients receiving the combination therapy (Bernstein,
1975; Girdwood, 1976; Salter, 1973). No evidence
has been presented of dysmorphogenicity in man
(Brumfitt and Pursell, 1973), but because of the
theoretical risk of impaired folate metabolism in the
fetus and risk of dysmorphogenic effects, its use is not
recommended during pregnancy.
6. Drug Interactiolls
The possibility of interactions between trimethoprim-sulphamethoxazole and other substances
419
Chnical Pharmacokinetics of Co- trimoxazole
is of concern in patients receiving concomitant therapy. Thus, there is an increased risk of thrombocytopenia in patients receiving diuretics (Frisch,
1973), and the combination has been shown to potentiate the activity of suI phony lurea oral hypoglycaemic
agents (Mihic et a]., 1975), and also of oral coumarin
anticoagulants (Barnett and Hancock, 1975; Errick
and Keys, 1978; Hassall et aI., 1975). Although trimethoprim-sulphamethoxazole displaces warfarin
from its binding to plasma proteins to a small degree
(Tilstone et aI., 1977), the primary mechanism for
anticoagulant potentiation appears to be associated
with increased circulating concentrations and a longer
elimination half-life of the more potent S-enantiomorph of warfarin (O'Reilly, 1980). This pharmacokinetic interaction was concealed in previous
studies using racemic warfarin due to an opposite
effect by trimethoprim-sulphamethoxazole on the less
potent R-warfarin resulting in reduced circulating
concentrations of this enantiomorph (O'Reilly and
Motley, 1979). There is no clinical evidence of interaction between the combination and phenindione
(deSwiet, 1975).
Trimethoprim-sulphamethvxazole
may
also
decrease the hepatic clearance and prolong the
biological half-life of phenytoin (Hansen et aI., 1975).
7. Dosage in Clinical Use
The usual adult oral dose of trimethoprim-sulphamethoxazole is 2 standard tablets, each containing
80mg trimethoprim and 400mg sulphamethoxazole,
twice a day (Klastersky, I 973). A double strength
tablet is also available, and an oral suspension containing the equivalent of 40mg trimethoprim and
200mg sulphamethoxazole per 5ml. Optimum dosage
regimens for the treatment of gonorrhoea, where
high doses may be needed, are not well defined.
In uraemic patients, no dose modification is necessary if creatinine clearance exceeds 30ml/ min (see
section 3.5). However, dose adjustment is required in
patients with creatinine clearances below this value
(Bailey et aI., 1976; Kalowski et al., 1973).
The mean steady-state level (C ~ ) of a drug administered at regular intervals is given by the expression
FD
Vkel'T
where F is the fraction of the dose D which is absorbed into the systemic circulation, V is the distribution volume, kel is the overall first-order elimination
rate constant, and T is the dosage interval (Wagner et
al., 1965).
In renal failure, the value of kel decreases so that,
notwithstanding possible changes in the apparent distribution volume of sulphamethoxazole (Welling et
al., 1973), the value of C'~ can be maintained
reasonably close to normal levels by adjusting the
dose or dosage interval. Since the mean elimination
rates of trimethoprim and sulphamethoxazole are
generally decreased 2- to 3-fold in severe uraemia
(section 3.5), although a greater effect may be observed in some individuals, it is appropriate to administer a normal initial dose with subsequent doses
reduced to one-half to one-third the normal dose,
with a dosage interval maintained at 12h (Craig and
Kunin, 1973; Welling et aI., 1973). An alternative,
more detailed general dosing scheme for trimethoprim-sulphamethoxazole at varying degrees of
Table IV. Dosage schedule for treatment of acute otitis
media and Urinary tract infections In children 2 months of age
or older (Wormser, 1978)
Weight
Ib
Dose every 12 hours
kg
teaspoonfuls(ml)
tablets
20
1(5)
0.5
40
18
2(10)
1.0
60
27
3 (15)
1.5
80
36
4(20)
2.0
a Each tablet contains 80mg trimethoprlm and 400mg
sulphamethoxazole.
Chnlcal Pharmacokinetics of Co-trimoxazole
impaired renal function, based on both creatinine
clearance and serum creatinine values, is given in
table 111 !Hansen. 1978; Rieder et aI., 1974b).
As mentioned previously (section 3.5), the acetylated metabolite of sulphamethoxazole may not dialyse
a..<; efficiently as the parent drug, so that monitoring of
this compound may be necessary in dialysis patients
(Baethke et aI., 1972).
Trimethoprim-sulphamethoxazole is not recommended for infants younger than 2 months. For infants older than 2 months, and older children,
Wormser (J 978) has suggested the dosage schedule
shown in table IV.
References
Avery. G S. Trimethopnmsulphamethoxazole: A revIew. Drugs
I 7-53 (1971).
Bach. M.C.~ Gold. O. and Fmland. M . AbsorptIon and urInary
excretion of tnmethoprim. sulfamethoxazole. and tnmethoprim-sulfamethoxazole results wIth Mngle doses in normal young adults and prelIminary observatIons dunng therapy
WIth trimethoprimsulfamethoxazole Journal of Infectious
Diseases 128 (Suppl.l 584-598 (Nov 1973).
Baethke. R.: Golde. G. and Gahl. G.: Sulphamethoxazolel
tnmethoprim' pharmacokinetic ,tudle, In pallenl~ WIth
chronIC renal failure European Journal of Clinical Pharmacology 4: 233-240 (\ 972).
BaIley. R R Intravenous co-tnmoxazole ('Bactnm') in the treatment of acute pyelonephritIs. Chemotherapy 23: 710 (1977).
Bailey. R.R. and Little. PJ.: Detenoration in renal function m
a.,-~oClatlon with co-tnmoxazole therapy Medical Journal of
Australia I. 914 (1976)
Bannatyne. R.M ~ Toma. S.~ Cheung. Rand Hu. G.: Resistance to
tnmethoprim and other antIbiotics m Ontario Shigellae. Lancet
I 425-426 (1980).
Barnett. D.B and Hancock. B.W .. Anticoagulant resistance: an
unu,ual ca.~. Bntlsh Medical Journal I. 608-609 (1975)
Bateson. M.C ~ Hayes. J P. and Pendharkar. p. Co-trimoxazole
and folate metabolIsm. Lancet 2 339-340 (1976).
Bergan. T and Brodwall. E.K Human pharmacokinetics of a
~ulfamethoxazole-trimethopnm combination
Acta Medica
Scandmavlca 192 483-492 (1972).
Bergan. T. and Brodwall. E.K. The pharmacokmetlc profile of cotrimoxazole. Sc,mdInavlan Journal of Infectious DIseases 8
(Suppl.) 42-49 (1976).
Berglund. F.: Killander. J. and PompelUs. R Effect of trimethoprim-sulphamethoxazole on the renal excretion of
creatinme In man. Journal of Urology 114 802-808 (f 975).
420
BernsteIn. L.S Adverse reacuons to tnmethoprim-sulfamethoxazole WIth particular reference to long-term therapy CanadIan
MedIcal A,soclallon Journal 112(Suppl ). 96-98 (June 1975).
Bjorn~son. T.D: U~ of ~rum cre~linlne c()ncentratlon~ to deter
mIne renal functIon Climcal Pharmacokmeti~ 4. 200-222
(1979).
Bohni. E.: Vergleichende bakteriologlsche unter,uchungen mil der
Kombination Tnmethopnm!wlfamethoxazole m VIlro und in
VIVO Chemotherapy 14 (Suppl.l: 1-21 (1969).
Bratton. A.C. and Marshall. E K . <\ new coupling component for
sulfonamIde determInation. Journal of BiologIcal Chemistry
128: 537-550 (1939)
Brumfitt. W .. Falers. M.C ~ Pursell. R E.~ Reeve,. D S. and
Turnbull. <\.R Bacteriological. pharmacologIcal and clinic
stud ie, WIth tnmethopnm-~ulfonamide combInatIons WIth
particular reference to the treatment of urinary tract infectIOn,
Postgraduate Medical Journal 45 (Suppl) 56-61 (Nov 1969)
Brumfitt. W : HamIlton-MIller and Ko,mldl'. J.. Trimethoprimsulfamethoxazole. The pre~ent p(Ntion Journal of InfectIous
DIsease, 128 (Suppl.l 778-791 (Nov 1973)
Brumfitt. W. and Pursell. R E .. Tnmethoprim-,ulfamethoxazole
In the treatment of bactenuna. Journal of Infectious DIseases
128 (Suppl ). 657 -663 (Nov 197 J).
Buchanan. N: Sulphamethoxazole. hypoalbuminaemla. crystalluria. and renal faIlure. Bntlsh MedIcal Journal 2 172 (1978).
Bushby. S R M. Synergy of tnmethopnm and sulfonamlde,_
history and current 'tatu~: In WoodbIne. M (Ed) AntibIotics
and AntibIOSIS In Agriculture. pp.64-79 (Butterworths. London 1977)
Bushby. S R.M and HItchIngs. G.H Trimethopnm. A ,ulfonamlde potentiator. Br. J Pharmacol. 33 72-90 (1968).
Bye. <\ . Drug interference with creatInIne assay ClInical ChemIStry 22. 283 (1976).
Chanarin. l. and, England. J M. TOXICIty of trimethoprimsulfamethoxazole in patlenl, with megaloblastIC haemopOlesis
Bntish Medical Journal I. 651-653 (1972).
CraIg. \V A. and Kunin. C.M.: Trimethoprim-sulfamethoxazole:
pharmacodynamic effect, of urinary pH and impaIred renal
function. Annals of Internal MedICIne 78 491-497 (1973)
DabhOlwala. N.F .. Bye. A. and Clandge. M.: A ,tudy of concentrations of trimethopnm-sulphamethoxazole In the human
prostate gland. Bntish Journal of Urology 48. 77-81 (1976).
Darell. J.H.~ Garrod. L P. and Waterworth. P M. Trimethopnm
laboratory and clInical studies. Journal of ClInIcal Pathology
21 202-209 (! 968)
Dawborn. J.K .. Ca.~taldl. P A.~ KIlgour. A .. ParkIn. J D and Pattison. G" Prolonged use of tnmethoprim-sulfonamide in unnary infection. Med. J. Austral. I (Supp\.): 52-56 (June 1973).
Denneberg. T .. Ekberg. M ~ Erickson. C. and Han~n. A .. Co-tnmoxazole In the long-term treatment of pyelonephritis with
normal and impaired renal functIOn. Scandinavian Journal of
InfectIOUs Diseases 8 (Suppl.l: 61-65 (1976)
de Swie!. J.' Potenriation of warfarin by co-trimoxazole. BrilIsh
421
Clinical Pharmacokinetics of Co-trimoxazole
MedIcal Journal 3 491 (1975).
Dornbu!>Ch. K.. Regrt)l,.,ion Ime analysIs of the synergistIc effect
for the combmatlon of tnmethoprim/sulphamethoxazole.
Chemotherapy 16: 229238 (1971)
Dornbusch. K : Trimethoprim and sulfamethoxazole determmatlon of bactenal sen'ltlvlty and drug concentratIons 10 human
!.erum ScandinavIan Journal of Infectiou, Di,eao.;es 8 (Suppl ).
20-24 (1976).
Eatman. F B. 'VIagglO. A c.. Pocelmko. R : Boxenbaum. K A :
GeItner. A.: Glover. W : Macasleb. T . Holazo, A.: Wemfeld.
R.E and Kaplan. S.A : Blood and !.allvary concentratIon, of
sulfamethoxazole and tnmethopnm 10 man. Journal of Pharmacokmetlc~ and BlopharmaceutlC!. 5 615-624 (1977)
Errick. J.K. and Key,. P W Cotnmoxazole and warfann: Cao.;e
report of an mteractlon. Amencan Journal of Ho,pital Pharmacy 35 1399-1401 (1978)
Fowle. A .S. E . Bye, A : Harin. F : M Iddlemis~. D and NafJCy. K.
The dO!.age of cotnmoxa70le 10 chIldhood European Journal
of Climcal Pharmacology 8: 217-222 (1975).
Fne,. N .. Keuth. U. and Braun. J.S. Unter,uchungen zur IIquorganglgkeit von trimethopnm 1m kmde,alter. Fort,chnlte der
MedlZln 93 11781183 (J 975).
Frisch. J M. Cllmcal experience with advero.;e reactlon~ to trimethopnm-,ulfamethoxazole. Journal of Infectiou, Diseru-e,
128 (Suppl ): 607-611 (Nov 1973).
Girdwood. R.H .. The nature of possible adverse reaction, of cotrimoxa70le Scandinavian Journal of Infectlou, D"ea~es 8
(SuppU. 10-16 (J 976).
Gleckman. R A.' A cooperative controlled 'tudy of the use of trio
methoprim-sulfamethoxazole in chronic unnary tract infections. J. Infect. Dis. 128 (SuppU. 647-651 (Nov 1973).
Gleckman. R.A . Tnmethoprim-sulfamethoxazole vs amplcllhn in
chronic urinary tract infectIon A double blind multIcenter cooperative controlled ,tudy. Journal of American Medical
ASSOCIation 233 427-431 (1975).
Gnarpe. H and Friberg. J.' The penetratIon of tnmethoprim into
semmal nuid and serum ScandinaVIan Journal of Infectlou~
Diseases 8 (Suppl ): 50- 5 2 () 976).
Grose. W.E.: Bodey. G P and Loo. Ti Li Clinical pharmacology
of intravenously admimstered tnmethopnmsulfamethoxazole.
Antimicrobial Agents and Chemotherapy 15 449-451 (1979)
Hachen. H,J.. Bladder mstlllatlons with trimethoprim-sulfamethoxazole m the treatment of unnary mfectlOn Chemotherapy 24. 5560 (J 978).
Hall, P. W. Renal secretory T m for sulfonamide Climcal Research
9 248 (196 II.
Hansen. I.B.: The combination tnmethoprim-sulfamethoxazole.
Antibiot. Chemother. 25. 217-232 (Karger. Basel 1978).
Hansen. I.: Nielsen. M.L.: Heerfordt. L.. Hennksen. B. and Ber,
telsen. S. Trimethopnm 10 normal and pathological human
lung tissue Chemotherapy 19 221-234 (J 973)
Hansen. J.M.: SiersbaekNlelsen. K: Skovsted. L.. Kampmann.
J.P. and Lumholtz. B.' PotentiatIon of warfarin by cotrimox
azole Briti,h Medical Journal 2 684 (1975)
Hardmg. G.K. and Ronald. A.R. A controlled Mudy of anti
mIcrobIal prophylaxis of recurrent unnary infection 10
women. N. Engl. J. Med 291: 597-601 (1974).
Ha~sall. C. et al. PotentiatIon of warfann by co-tnmoxazole
Lancet 2: 11551156 ()975).
HIli. A\'. and Kerr. D.N Toxicity of co-trimoxazole in nutntional haematinic deficiency. Postgraduate MedIcal Journal 49
596598 () 97 3)
Howard. J.B and Howard. J.E. Trimethopnm-sulfamethoxazole
vs sulfamethoxazole for acute unnary tract infecllons 10
children. Am. J. Di,. Child 132: 1085-1087 (J978).
Huovmen. P. and TOIvanen. p. Tnmethopnm re'l,tance in Finland after five years' use of plam trimethoprim Bnti~h Medical Journal 280 7274 (1980).
Jenl..m" G.C . Hughe,. D.T and Hall. PC. A haematologlcal
,tudy of patients recelvmg long-term treatment WIth tnmethopnm and ,ulfonamide Journal ofChmcal Pathology 23
392-396 (1970).
Kalowskl. S: Nanra. R.S .. Mathew. T.H and Smith. P.K.
DeterioratIon," renal function in a~!o.Oclatlon with co-trimoxazole therapy Lancet I .>94-397 (1973)
Kaplan. S.A .. Wemfeld. R.E.: "bruzzo. C.W. Cotler. Sand
Alexander. K: Pharmacokmetlc profile of tnmethopnm 10
dog and man. J. Pharm. Sci 49: 358-363 (1970).
Kaplan. S.A . Wemfeld. R E.. Abruzzo. C W .. MacFdden. K.
Jack. M.L. and Wel,sman. L.. Pharmacokmetlc profile of trimethopnm,ulfamethoxazole in man Journal of Infectlou,
DIseases 128 (Suppl) 547555 (Nov 1973)
Ka~nen. A .. Kaarsalo. E. Hiltunen. Rand Somi. V
Compan,on of long-term. lowdo~ge mtrofurantom. methenamme
hippurate. trimethopnm and tnmethopnm-,ulfamethoxa70le
in the control of recurrent unnary tract InfeCllon Annal, of
Clinical Research 6: 285-289 (J 974)
Klastersky. J.' Double-blind tnalto compare two dosage, of cotrimoxazole 10 the treatment of hospital mfectlOn,. Chemotherapy 18 358-368 (J 913)
Korn. A : Hltzenberger, G and Ja,chek. I : Pharmacokinetlc, of
the combmatlon of tnmethoprim-sulfamethoxazole. Ad Antimicrob. Antineopl. Chemother. III. 2\-24 (Prague 1972).
Kremers. P .. Clae",ens. Hand Heu,ghem. C . Comparative pharo
macoklOetic, 10 man of parenterally and orally admini,tered
cotnmoxazole. Medikon 4. 1921 () 975)
Kremers. P .. Duvivler. J. and Heusghem. C. Pharmacokmetic
studies or cotnmoxazole 10 man after 'Ingle and repeated
doses. Journal of Chmcal Pharmacology 14 112\17 (1974).
Kuhne. J : Kohlmann. F W .. Seydel. J.K. and Wempe. E.. Pharo
makokinetik der kombination sulfamoxol/tnmethoprim (CN
3123) bei tIer und mensch. ArznelmlttelForschung 26
651657 (J 976)
Lacey. R W.: Mechanism or action of tnmethoprim and
sulphonamides: Relevance to synergy ill
Journal of AntimicrobIal Chemotherapy 5(Suppl.'B) 75-83 () 979).
"/I'"
Clinical Pharmacokinetics of Co-tnmoxazole
Lazaro. A .. Badia. A .. Ca~tells. I and Mylonakis. N. Tnmethoprim and ,ulfamethoxazole blood levels in man after mtramu\cular admml,tratlon Journal of Antimicrobial Chemotherapy 4. 287-289 (197R).
Lewm. E.B. Klem. J.O and Finland. M Trimethopnmsulfamethaxozole Absorption. excretion and toxicity m SIX
children J. Infect DIS 128 (Suppl ). 618-621 (Nov 1973).
Liedtke. R. and Haa\C. W' Steady-,tate pharmacokmetlc, of
\ulfamethoxazole and trimethopnm m man after rectal application Armelmlltel-For~hung 29: 345-349 (1979)
Mad!.en. P.O .. Kjaer. T B. and Baumueller. A. Pro,tatlc tls,ue and
flUid concentratilm, of trimethopnm and ,ulfamethoxazole
Urology 8 129-132 (1976)
Malmborg. I\. . Dornbu,ch. K.. Elia",on. Rand Lindholmer. C .
ConcentratIOn of antlbactenal\ in human seminal pla\ma Proceedmg, of 9th Congre" of Chemotherapy 53-59 (London
1975)
Mark\. M I Pharmacokmetb and efficacy of tnntethoprim,ulfamethoxa70le m the treatment of ga'troent~ntl\ m
children. Canadian Medical I\. "ociatlOn Journal I 12 (Suppl )
33-34 (June 1975).
Marks. M I: Ka7eml. M. Hale,. Band Neml\. I\. H Pharmacokmetlc \tudle, of trimethopnm-\ulfamethoxazole m
children with ga,troentent" Journal of Infectlou\ Di,ea\e,
128 (Suppl.l 622-625 (Nov 1973)
Mlhlc. M .. Mautner. L S .. Lene". J.Z and Grant. K Effect of tnmethopnm-,ulfamethoxa70le on blood msulin and gluco!.e
concentratlon\ of dlabetlc\ Canadian Medical I\.s~Clatlon
Journal 112 (Suppl.l. 80-82 (June 1975)
Miller. R D and Salter. A.J
The pas!.age of tnmethopnm/sulphamethoxazole mto breast milk and its slgmficance.
Proc. 8th Congr. Chemother I: 687-691 (Athen~ 1973)
Neuman. M.: Kazmierczak. A. and Charbonnier. I\. Etat fonctionnel du fOie et pouvoir antlbacterien de l'a~~ciatlOn tnmethoprime-~ulfamethazole dan' Ie !.ang. la bile et Ie, urme,
che, I'homme Therapie 27 1069-1080 (1972).
Nolte. H. and Buttner. H . Pharmacokmetlcs of tnmethopnm and
its combination with sulfamethoxazole in man after single and
chromc oral admmistratlon. Chemother. 18: 274-284 (1973).
Nolte. H and Buttner. H Investigations on plasma level\ of
sulfamethoxazole m man aftcr smgle and chronic oral administration alone and m combmatlon with tnmethopnm
Chemotherapy 20: 321-330 (1974).
Oosterlink. W. Defoor!. R. and Renders. G. A study of concentrations of ,ulfamethoxazole and tnmethoprim 10 human
prostate gland. British Journal of Urology 47 301-304 (1975).
OReilly. R A.. Stereoselectlve interaction of trimethopnmsulphamethoxazole with the separated enantiomorphs of
racemic warfarin In man. Med. Intell. 302. 33-35 (( 980)
ORellly. R.A and Motley. C.H RacemiC warfann and trimethoprim-sulfamethoxazole mteractlon 10 humans. Annals
of Internal Medicine 91: 34-36 (1979)
Pearson. N.J.: Towner, K..I : McSherry. A.M .. Cattell. W.R. and
422
OGrady. F Emergence of tnmethopnm-re"stant enterobactena 10 patient, recelvmg long-term co-trimoxa70le for the
control of mtractable urinary-tract infection Lancet 2
1205-1209 (1979)
Poe. M. -\ntlbactenal 'ynergl\m. I\. proposal for chemotherapeutic
poten\iatlon
between
tnmethopnm
and
,ulphamethoxazole SCience 194 533-535 (1977)
Pohjanpelto. P E J . Sarmela. T J and Raine,. T Penetration of
trimethopnm and ~ulphamethoxazole mto the aqueou,
humour Br J Ophthalmol 58. 606-608 (( 974).
Reeve\. D S . Sulfamethoxa70le/tnmethopnm. the fiN two year,.
Journal of Climcal Pathology 24 430-437 (1971).
Reid. D.\\ J. Caille. G and Kaufmann. N R Maternal and
tran,placental kmetlc\ of tnmethopnm and \ulfamethoxa70le.
,eparately and 10 combmatlOn Canadian Medical A,,,-,clatlon
Journal III (Suppl.l. 67-72 (June 1975).
Rein. '1 F . Elliott. \\' C : Swen,on. J A and Thorn,berry. C .
Sulfamethoxazole-tnmethopnm \ynergism for Nd\.wril1 1(011orr/weae I\.ntlmlcrob Ag Chemother 17: 247-250 (1980).
Richmond. J ~t.: Whitworth. J I\. . Falrely. K.F and KmcaldSmith. p. Co-tnmoxa70le nephrotoxIcity Lancet I 493
(1979)
Rieder. J : Quantitative determination of the bacterio,tatlcally active fraction of ,ulfonamlde and the ,urn of their mactlve
metabolite\ 10 the body nUld Chemotherapy 17 1-21 (1972)
Rieder. 1.. Excretion of sulfamethoxazole and tnmethoprim mto
human bile. J Infect DIS 128 (Suppl.l. 547 (Nov 1973a)
Rieder. J.' \Ietaboli'm and le~hnlque, for a,say of tnmethopnm
and ,ulfamethoxa70le. Journal of Infectiou, Dlsea.\~ 128
(Suppl.l 567-573 (Nov I 97Jb).
Rieder. J : Schwarl7. DE. Fernex. M. Bergan. T . Brodwall,
E K. Blumberg. -\.: Cottier. P and Scheitlin. W. Pharmacokmellc, of the antlbactenal combmallon ,ulfamethoxa70le plu, tnmethopnm 10 patient, With normal or Impaired
kidney function
I\.nllbiotlc, Chemotherapy Vol
18.
pp.148-198 (Karger. Ba,el 1974b).
Rieder. J. Schwart7. DE. and Zangaglia. O. Pa\!.agc of
\ulfamethoxazole and tnmethopnm mto the bile m man
Chemotherapy 20 65-81 (I 974a)
Rieder. J and Schwartz. DE.' Pharmakokmetik der wlrk,offkombmanation tnmethopnm + ,ulfamethoxazol bel
leberkranken 1m vergleich zu ge,unden ArznelmillelFo"chung 25 656-666 (1975).
Robinson. M.F: Campbell. G.R and Craswell. P W. Co-tnmoxazole 10 chromc renal failure A controlled experiment in
Wistar rat'. Climcal TOXicology 10. 411-415 (1977)
Ronald. A R .. Harding. G K.M . Mathia,. R .. Wong. C K and
MUIr. P.. ProphylaXIS of recurnng unnary tract mfection in
females. a compan'On of nitrofurantoin With tnmethopnmsulfamethoxazole Canadian Medical A,~clatlon Journal I 12
(Suppl) 13-16 (June. 1975)
Rosenfeld. J.B . Najen'On. T and Grosswater. Z Effect of longterm co-tnmoxazole therapy on renal function. Medical Jour-
Clinical Pharmacokinetics of Co-tnmoxazole
nal of Australia 2 546-548 (1975).
Roth. B; falco. EA.; HltchlOgs. G.H. and Bushby. S.R.M. 5Bem.yl-2A-diamlOopynmldines a.~ antibactenal agenl~. I Synthe~" and antibactenal activIty 10 VItro. Journal of Medicinal
and PharmaceutIcal Chemistry 5. 1103-1123 (1962).
Salmon. J D.. Fowle. A S E. and Bye. A.' Concentratlon~ of tnmethopnm and ~ulfamethoxazole 10 aqueou~ humour and
pla~ma from regime~ of co-trimoxazole in man. Journal of
AntImicrobial Chemotherapy I 205-211 (1975).
Salter. A J.' The toxicIty prolile of trimethopnm-~ulfamethoxazole
after 4 year~ of wide~pread u~ Medical Journal of Au~tralia I
(Suppl ). 70-74 (1973).
Schmidt. U ; Sen. P ; Kapila. R ; Lewy. F ; Lange. M . MIddleton.
J and Louna. D. B. Chnlcal experience with intravenou~ trimethoprim-~ulfamethoxa70le (SXn for ~nous infectIons.
11th InternatIOnal Congre~~ of Chemotherapy and 19th Inter~ience Conference on AntImIcrobIal Agent~ and Chemotherapy. Ab,tract 371 (8o~ton 1979)
Schwam. DE. Koechlln. B A. and Weinfeld. R.E.. Spectrofluonmetnc method for the determination of trimethoprim
10 body fluld~ Chemotherapy 14 (Supp\.) 22-29 (1969).
Schwam. D.E and RIeder. J Pharmacokinetb of ~ulfamethox
a70le + tnmethopnm 10 man and theIr di,tnbullon in the rat.
Chemotherapy 15 337-355 (1970)
Schwam. DE. Veller. Wand Englert. G. Tnmethopnm metabolile~ in ral. dog and man
quahtallve and quanlltative
~tudle,. A r70elOlIllel-For,chung 20. 1867 -18 71 (1970).
Schwam. D E. and ZeIgler. W H : "say and pharmacokineti~
of tnmethopnm In man and anima" Postgrdduate Medical
Journal 45 .'2-37 (1969).
Sharp~tone. P. The renal handling of tnmethoprim and ,ulfamethoxazole in man. Po~tgraduate MedIcal Journal 45 (Suppi), 38-42 (Nov 19(9).
Sharpstone. P.. Pickard. J. and William~. R.: Concentrations of
trimethoprim and ,ulphamethoxa70le in human bile Proceeding, of 7th Congre" of Chemotherapy I: 1269-1971 (Prague
1972).
Siber. G.; Gorham. C. DurblO. W ; Le~ko. L and Lewin. M.:
The pharmacology of IV tnmethopnm-~ulfamethoxazole
(TMP/SMZ) (Bactrim) 10 children and adult,. 11th International Congres, of Chemotherapy and 19th Intersclence Conference on Antimicrobial Agent, and Chemotherapy. Abstract
344 (8o,ton 1979)
Siegel. W.H : Unusual comphcallon of therapy with ,ulfamethoxa70le-trimethoprim. Journal of Urology 117 397 (1977)
Sigel. C W.; Grace. ME. and Nichol. C "-.' Metabolism of trimethopnm 10 man and mea~urement of a new metabolite' a
new fluore~cence a.~say Journal of Infectiou~ Di~a.~s 128
(Suppl ): 580-583 (Nov 1973).
Smelhe. J.M : Gruneberg. R N .. Leaky. A and "-tkin. W.S.
Long-term low-dosage co-tnmoxa70le in the management of
unnary tract infectIon 10 children. Journal of Antimicrobial
Chemotherapy 2 287-291 (1976)
423
Stamey. T.A and Condy. M.: The dIffUSIon and concentration of
trimethoprim 10 human vaginal fluid Journal of Infecllou~
Di~ea.~e, 131 261-266 (1975).
Ta.~ker. P.R.W .. MacGregor. G A and De Wardener. HE: Use
of cO-lrImoxazole 10 chroniC renal faIlure. Lancet I .
1216-1218 (1975)
Taylor. D E.; Key~tone . .I S and Devlin. H R Correspondence
Lancet I 426 (1980).
TI"tone. W.J.; Gray. J.M B; Nimmo-Smith. R H. and Law~n.
D.H.: Interaction between warfann and ,ulphamethoxazole
POMgraduate MedIcal Journal 53. 385-390 (1977)
Vree. T.B.; Hek~ter. Y.A .. Saar,. A.M. Dan,ma. J.E and KleiJn.
E. V D. DetermlOatlon of trimethopnm and ,ulfamethoxazole
Ico-trimoxazole) 10 body flUId, of man by mean, of hIgh-performance hquld chromatography Journal of Chromatography
146 103-112 (1978)
Vrce. T B; Hek,ter. Y.A .. Dam~ma. J E; van der KlelJn. and
OReilly. W.J: Pharmacokmetlc, of N,-acetyl- and N.acetylsulph,amethoxazole 10 man Clinical PharmacoklOetl~ 4.
310-319 ([979).
Wagner. J.G : Northam. J I.. Alway. CD. and Carpenter. 0 S
Blood levels of drug at the equllibnum ,tate after multIple do~109 Nature 207 1301-1302 (1965).
Wahlin. A and Ro~man. N .. Skin manifestatIon, WIth ra.~cuhti,
due to co-trimoxa70le Lancet 2 (leller): 1415 (1976)
\\' elOfcld. R E and Maca."eb. T.e Determmatlon of Inmethopnm 10 biologIcal fluid~ by hIgh-performance liqUId
chromatography Journal of Chromatography 164 73-84
( 1979)
Welling. P G .. CraIg. W.A; Amidon. GLand Kunin. eM
Pharmacokinetlc, of tnmethopnm and ,ulfamethoxazole 10
normal ~ubject' and in patient~ with renal failure Journal of
Infectiou, DI~a.~e~ 128 (SuppU- 556-566 (Nov 1973)
Wilfert. eM. Trimethopnm-,ulfamethoxazole in children Pharmacokinetic, and clmical Mudie, Journal of Infectlou,
Disea'es 128 (Supp\.): 613-617 (Nov 1973).
Wilfert. eM and Gutman. L T Pharmacokmetlc, of trimethoprim-,ulfamethoxazole 10 children. CanadIan Medical
A,~clation Journal 112 (SuppU- 73-76 (June 1975)
Wormser. G.P. Trimethopnm-sulfamethoxazole II. Chnical
Stud Ie, New York State Journal or MedIcine 2058-2067
(1978).
Yllkorkala. 0 .. SjoMedl. E; Jarvinen. P A .. Tlkkanen. R. and
Rames. T
Tnmethopnm-~ulfonamlde combination admini~tered orally and intravaginally 10 the Iir~t trimester of
pregnancy Its absorptIon into ~rum and transfer to amniotic
fluid Acta Ob,tetrica et Gynecologlca Scandinavlca 52
229-234 (1973).
Author'~ addre~ Prof. Peter G. Welli"g, Center for Health
Sciences. School of Pharmacy. Univer~lty of WIsconsin. 425
N. Charter Street. Madison. W;\(O",;" .'U70f> (USA)
You might also like
- Adult Infectious Disease Bulletpoints HandbookFrom EverandAdult Infectious Disease Bulletpoints HandbookRating: 4.5 out of 5 stars4.5/5 (9)
- Board Questions in PharmacologyDocument12 pagesBoard Questions in PharmacologyJo Anne100% (6)
- Serotonin SyndromeDocument19 pagesSerotonin SyndromeNur Atiqah Mohd AzliNo ratings yet
- J. Antimicrob. Chemother.-1996-Van Der Ven-75-80Document6 pagesJ. Antimicrob. Chemother.-1996-Van Der Ven-75-80Andrea RivaNo ratings yet
- Theme 22. Synthetic Chemotherapeutic Drugs: General Structure of Streptocides Paraaminobenzoic AcidDocument12 pagesTheme 22. Synthetic Chemotherapeutic Drugs: General Structure of Streptocides Paraaminobenzoic Acidfatima ALArrayedhNo ratings yet
- PharmaDocument7 pagesPharmaDocter SycoNo ratings yet
- Drug Interactions With Azithromycin and The Macrolides: An OverviewDocument10 pagesDrug Interactions With Azithromycin and The Macrolides: An OverviewAranel BomNo ratings yet
- Bioorganic & Medicinal Chemistry Letters: SciencedirectDocument5 pagesBioorganic & Medicinal Chemistry Letters: SciencedirectHaroon Ur RashidNo ratings yet
- Why Fosfomycin Trometamol As First Line Therapy For UncomplicatedDocument5 pagesWhy Fosfomycin Trometamol As First Line Therapy For UncomplicatedEdwin MontañezNo ratings yet
- PatoDocument10 pagesPatoYiro YazawaNo ratings yet
- Basic Mechanisms of Chemotherapy: Mitchison, M.BDocument10 pagesBasic Mechanisms of Chemotherapy: Mitchison, M.BDecolagueNo ratings yet
- Tratamiento de Infecciones Fúngicas Sistémicas Primera Parte: Fluconazol, Itraconazol y VoriconazolDocument13 pagesTratamiento de Infecciones Fúngicas Sistémicas Primera Parte: Fluconazol, Itraconazol y VoriconazolKenyi CristianNo ratings yet
- Pharmaceuticals 14 00984Document23 pagesPharmaceuticals 14 00984Walid Ebid ElgammalNo ratings yet
- UGTs For TamoxifenDocument18 pagesUGTs For TamoxifenCutest guddyNo ratings yet
- Effect of Diammonium Glycyrrhizinate On Pharmacokinetics of Omeprazole by Regulating Cytochrome P450 Enzymes and Plasma Protein Binding RateDocument7 pagesEffect of Diammonium Glycyrrhizinate On Pharmacokinetics of Omeprazole by Regulating Cytochrome P450 Enzymes and Plasma Protein Binding RateFitra AlfaniNo ratings yet
- Artigo ChagasDocument5 pagesArtigo ChagasDam LaignierNo ratings yet
- Quinolones, Folic Acid Antagonist, and Urinary Tract AntisepticsDocument29 pagesQuinolones, Folic Acid Antagonist, and Urinary Tract AntisepticsAliImadAlKhasakiNo ratings yet
- TMP 260 CDocument15 pagesTMP 260 CFrontiersNo ratings yet
- Short-Course Nitrofurantoin For The Treatment of Acute Uncomplicated Cystitis in WomenDocument6 pagesShort-Course Nitrofurantoin For The Treatment of Acute Uncomplicated Cystitis in WomenHanifah RifdaNo ratings yet
- 22 1-S2.0-S0924857908002392-MainDocument3 pages22 1-S2.0-S0924857908002392-MainLookpear ShiiNo ratings yet
- Huovinen 1987 Trimethoprim ResistanceDocument6 pagesHuovinen 1987 Trimethoprim Resistanceschrumpel123No ratings yet
- 060 JimenezDocument6 pages060 JimenezAri Puji AstutiNo ratings yet
- Sulfonamides Mechanism of Action & Antimicrobial ActivityDocument9 pagesSulfonamides Mechanism of Action & Antimicrobial ActivityMuhammad L RusydiNo ratings yet
- Tetracyclines: Mechanism of ActionDocument16 pagesTetracyclines: Mechanism of Actionammar amerNo ratings yet
- Tamoxifen Pathway and PharmacokineticsDocument9 pagesTamoxifen Pathway and PharmacokineticsCutest guddyNo ratings yet
- Sulfamethoxazole Trimethoprim PDFDocument10 pagesSulfamethoxazole Trimethoprim PDFAsi SyyffaNo ratings yet
- Trimethoprim/Sulfamethoxazole Prophylaxis in Neutropenic PatientsDocument9 pagesTrimethoprim/Sulfamethoxazole Prophylaxis in Neutropenic PatientsSusy OsorioNo ratings yet
- European Journal of Medicinal Chemistry: Research PaperDocument12 pagesEuropean Journal of Medicinal Chemistry: Research PaperlizNo ratings yet
- PharChm2 - TetracyclinesDocument9 pagesPharChm2 - TetracyclinesEdrick RamoranNo ratings yet
- Indolmicin PDFDocument3 pagesIndolmicin PDFMaria-LuizaGhidrasanNo ratings yet
- Petroianu 2005Document5 pagesPetroianu 2005Bilel ChefiratNo ratings yet
- EMMM 11 E10292Document21 pagesEMMM 11 E10292Mónica GuizarNo ratings yet
- Antibacterial and Antifungal DrugsDocument7 pagesAntibacterial and Antifungal Drugszzb9k9w9gzNo ratings yet
- MH BukuDocument33 pagesMH Bukunurul rezki fitrianiazisNo ratings yet
- Final Draft EsomeprazoleDocument4 pagesFinal Draft EsomeprazoleHassan Raza GilalNo ratings yet
- Jurnal CimetidineDocument7 pagesJurnal CimetidineAidahNo ratings yet
- Wu 2013Document4 pagesWu 2013Luisa Fernanda Rojas DiazNo ratings yet
- Enantiomers Evaluation CetirizineDocument4 pagesEnantiomers Evaluation Cetirizinebebel555No ratings yet
- Agriculture, Ecosystems & Environment Volume 64 Issue 2 1997 (Doi 10.1016/s0167-8809 (97) 00033-9) J.A. Pickett L.J. WadhamsDocument8 pagesAgriculture, Ecosystems & Environment Volume 64 Issue 2 1997 (Doi 10.1016/s0167-8809 (97) 00033-9) J.A. Pickett L.J. WadhamsJacqueline HaroNo ratings yet
- Paparella: Volume I: Basic Sciences and Related Disciplines Section 6: Pharmacology Chapter 28: Antibiotics Leonard P. RybakDocument16 pagesPaparella: Volume I: Basic Sciences and Related Disciplines Section 6: Pharmacology Chapter 28: Antibiotics Leonard P. RybakDiana Mihaela BadescuNo ratings yet
- Synthesis and in Vitro Anticancer Activity of New Thiadiazolines and Thiazolinones Containing A Chromenyl ScaffoldDocument15 pagesSynthesis and in Vitro Anticancer Activity of New Thiadiazolines and Thiazolinones Containing A Chromenyl ScaffoldWalid Ebid ElgammalNo ratings yet
- StandartDocument14 pagesStandartEder AlbertoNo ratings yet
- Chat GPTDocument9 pagesChat GPTbiplob royNo ratings yet
- Aic 28 4 2000 363Document12 pagesAic 28 4 2000 363danielguerinNo ratings yet
- Antifungal PDFDocument34 pagesAntifungal PDFUmashankar SharmaNo ratings yet
- Antitumor Components From Naematoloma FasciculareDocument4 pagesAntitumor Components From Naematoloma Fascicularelucaste50No ratings yet
- Genotoxicity and Anti-Genotoxicity of Some Traditional Medicinal HerbsDocument9 pagesGenotoxicity and Anti-Genotoxicity of Some Traditional Medicinal HerbsJonathan Vasquez CaveroNo ratings yet
- Bioorganic & Medicinal Chemistry: Article InfoDocument7 pagesBioorganic & Medicinal Chemistry: Article InfoMarcelo GanozaNo ratings yet
- Antifungal AgentsDocument7 pagesAntifungal AgentstenawNo ratings yet
- Fasciola GiganticaDocument11 pagesFasciola GiganticaAyu RadiatunNo ratings yet
- Clinical Pediatrics: Antiminth (Pyrantel Pamoate) : The Clinical Evaluation of A New Broad-Spectrum AnthelminthicDocument9 pagesClinical Pediatrics: Antiminth (Pyrantel Pamoate) : The Clinical Evaluation of A New Broad-Spectrum AnthelminthicLoh Chuan TuckNo ratings yet
- Adade. 2013 PDFDocument13 pagesAdade. 2013 PDFJuan Felipe Osorio MendezNo ratings yet
- Bedside Discussion Q&A: 1. Target SPO2 For COAD Patient?Document5 pagesBedside Discussion Q&A: 1. Target SPO2 For COAD Patient?Muhammad MuhammadNo ratings yet
- Tithonia Identificacion (Extraccion Metanol)Document7 pagesTithonia Identificacion (Extraccion Metanol)Miki CruzNo ratings yet
- Zithromax Tablet: Rawan Amr Abd Elaal MohammedDocument7 pagesZithromax Tablet: Rawan Amr Abd Elaal MohammedAbdelrhman AboodaNo ratings yet
- Pharma Uro Cotrimoxazole +fqsDocument14 pagesPharma Uro Cotrimoxazole +fqsHussein AlhaddadNo ratings yet
- Chat GPTDocument8 pagesChat GPTbiplob royNo ratings yet
- CHAABANE Association of Hyperhomocysteinemia With Genetic Variants in Key Enzymes of Homocysteine Metabolism and Methotrexate Toxicity in Rheumatoid Arthritis PatientsDocument8 pagesCHAABANE Association of Hyperhomocysteinemia With Genetic Variants in Key Enzymes of Homocysteine Metabolism and Methotrexate Toxicity in Rheumatoid Arthritis PatientsusmfdocNo ratings yet
- SulfonamideDocument2 pagesSulfonamideAbo DowiaNo ratings yet
- The Oncologist 2007 Jordan 1143 50Document8 pagesThe Oncologist 2007 Jordan 1143 50Rafael Eduardo Toro ManotasNo ratings yet
- Antibacterial Chemotherapy HB3 Sem2 2023 - 230522 - 113027Document77 pagesAntibacterial Chemotherapy HB3 Sem2 2023 - 230522 - 113027Csparkz beautyNo ratings yet
- 1.sulfonamide FinalDocument31 pages1.sulfonamide FinalPrasad SangishettyNo ratings yet
- Body Surface Area: Average Adult Dose: ExampleDocument3 pagesBody Surface Area: Average Adult Dose: ExampleDefi OktafiaNo ratings yet
- Mechanism of ResistenceDocument26 pagesMechanism of ResistenceDefi OktafiaNo ratings yet
- Comparison of Pharmacokinetics and Efficacy of Oral and Injectable MedicineDocument35 pagesComparison of Pharmacokinetics and Efficacy of Oral and Injectable MedicineDefi OktafiaNo ratings yet
- 004 11 ParacetamolDocument1 page004 11 ParacetamolDefi OktafiaNo ratings yet
- Mycophenolate Mofetil Versus Cyclophosphamide ForllDocument10 pagesMycophenolate Mofetil Versus Cyclophosphamide ForllAgitNo ratings yet
- Sympathomimetics 2023 MCQDocument12 pagesSympathomimetics 2023 MCQHossam MohamedNo ratings yet
- Certificate For COVID-19 Vaccination: Beneficiary DetailsDocument1 pageCertificate For COVID-19 Vaccination: Beneficiary DetailsDIGITAL 143No ratings yet
- Drug Study AdalatDocument4 pagesDrug Study AdalatLea CelestialNo ratings yet
- Emergency Trolley ListDocument2 pagesEmergency Trolley ListDiptanshu Das100% (7)
- Eskag Pharma Pvt. LTD., Haridwar, Unit-I Department: Quality Assurance Product MatrixDocument20 pagesEskag Pharma Pvt. LTD., Haridwar, Unit-I Department: Quality Assurance Product MatrixMohit ChauhanNo ratings yet
- Lap S5tock 29 Februari 2020Document47 pagesLap S5tock 29 Februari 2020Ridho SaputraNo ratings yet
- Kode Perusahaan Peserta Standarisasi Obat PDFDocument3 pagesKode Perusahaan Peserta Standarisasi Obat PDFHandry HuaNo ratings yet
- OXACILLINDocument1 pageOXACILLINJust nowNo ratings yet
- Biperiden (C)Document2 pagesBiperiden (C)Mae Ann Bueno CastillonNo ratings yet
- Book 1Document2,540 pagesBook 1widnyana ngurahNo ratings yet
- Betadine GargleDocument1 pageBetadine GargleReemALMousawiNo ratings yet
- Introduction To Pharmacology by ZebDocument31 pagesIntroduction To Pharmacology by ZebSanam MalikNo ratings yet
- Week 10: Drugs Administered For The Treatment of Diabetes MellitusDocument7 pagesWeek 10: Drugs Administered For The Treatment of Diabetes Mellitusashley larsonNo ratings yet
- CDER/OC/OMQ Update and Recent Cross Contamination Case StudiesDocument54 pagesCDER/OC/OMQ Update and Recent Cross Contamination Case StudieshuykhiemNo ratings yet
- CephalexinDocument3 pagesCephalexinapi-3797941100% (1)
- Daftar Pustaka SpoKDocument3 pagesDaftar Pustaka SpoKRisha PanggabeanNo ratings yet
- Unit UCUM - Codetable - 2020 12 18Document492 pagesUnit UCUM - Codetable - 2020 12 18pathuri rangaNo ratings yet
- MBBS - General Medicine Reg Id: KMC - 142105 RX ID: 406824261Document1 pageMBBS - General Medicine Reg Id: KMC - 142105 RX ID: 406824261Dipam HalderNo ratings yet
- Drug Policy 1982Document18 pagesDrug Policy 1982নোমানআবদিল্লাহ100% (1)
- MB Questions PharmaDocument15 pagesMB Questions Pharmapriyanshi goyalNo ratings yet
- Drugs On RespiratoryDocument17 pagesDrugs On RespiratoryIrwan M. IskoberNo ratings yet
- Final Pharmacology MCQDocument12 pagesFinal Pharmacology MCQSiraj Choudhari0% (1)
- Daftar Harga HD Juni 2020Document34 pagesDaftar Harga HD Juni 2020Kean KhamidaaNo ratings yet
- Id Resident TDDocument2 pagesId Resident TDapi-534214500No ratings yet
- Test Bank For Pharmacology For The Surgical Technologist 4th Edition by SnyderDocument36 pagesTest Bank For Pharmacology For The Surgical Technologist 4th Edition by Snyderjoysome.scaur.542kcf100% (46)
- Email List of PharmaceuticalsDocument9 pagesEmail List of Pharmaceuticalsprachi tayalNo ratings yet
- Madopar PI - 20190213 - ENDocument11 pagesMadopar PI - 20190213 - ENRonni Untung HNo ratings yet
- Drug Study - LosartanDocument2 pagesDrug Study - LosartanCath Bril50% (2)