Professional Documents
Culture Documents
365 Full PDF
365 Full PDF
Uploaded by
razgriz110Copyright:
Available Formats
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5820)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (845)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (898)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (349)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- 1.1 - Staph AureusDocument22 pages1.1 - Staph Aureusrazgriz1100% (1)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- 1.3 - Strep Pyogenes (Group A Strep)Document27 pages1.3 - Strep Pyogenes (Group A Strep)razgriz110No ratings yet
- AWS Vs Azure Vs Google Cloud - A Detailed Comparison of The Cloud Services Giants PDFDocument10 pagesAWS Vs Azure Vs Google Cloud - A Detailed Comparison of The Cloud Services Giants PDFSakthivel PNo ratings yet
- 1.2 - Staph EpidermidisDocument13 pages1.2 - Staph Epidermidisrazgriz110No ratings yet
- Falls in The ElderlyDocument32 pagesFalls in The Elderlyrazgriz110100% (1)
- Eaton DX-RT 6000 VA (Long Back UP) 1x1 UPS SystemDocument4 pagesEaton DX-RT 6000 VA (Long Back UP) 1x1 UPS SystemPhaniNo ratings yet
- OrDocument3 pagesOrsatishsaga1990No ratings yet
- Gr11 Mock Exam Schedule 2024Document13 pagesGr11 Mock Exam Schedule 2024potrillo0330No ratings yet
- 30 Top HTML Interview Questions and AnswersDocument15 pages30 Top HTML Interview Questions and AnswersAurobindaNo ratings yet
- Bishop 1997Document25 pagesBishop 1997Celina AgostinhoNo ratings yet
- Final DKSSKDocument79 pagesFinal DKSSKSarita Latthe100% (2)
- Letters From England: by Don Manuel Alvarez EspriellaDocument2 pagesLetters From England: by Don Manuel Alvarez EspriellaPickering and ChattoNo ratings yet
- CH 12Document31 pagesCH 12asin12336No ratings yet
- Tesa-60150 MSDSDocument11 pagesTesa-60150 MSDSBalagopal U RNo ratings yet
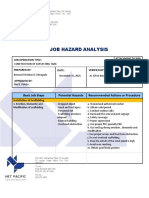
- Job Hazard Analysis: Basic Job Steps Potential Hazards Recommended Actions or ProcedureDocument3 pagesJob Hazard Analysis: Basic Job Steps Potential Hazards Recommended Actions or ProcedureBernard Christian DimaguilaNo ratings yet
- PDS - SP-9888 Tank Lining PDFDocument6 pagesPDS - SP-9888 Tank Lining PDFSherif AbdelhameedNo ratings yet
- IGST CH Status As On 01.01.2018Document443 pagesIGST CH Status As On 01.01.2018SK Business groupNo ratings yet
- Make Wire Transfers Through Online Banking From AnywhereDocument2 pagesMake Wire Transfers Through Online Banking From AnywhereDani PermanaNo ratings yet
- ISO 9001 Awareness AmaDocument51 pagesISO 9001 Awareness AmaHisar SimanjuntakNo ratings yet
- GPRS Evolution PH 2Document43 pagesGPRS Evolution PH 2Nur AfiyatNo ratings yet
- Machiavellian Reflections (Part 1) : PreambleDocument9 pagesMachiavellian Reflections (Part 1) : PreambleMuhammet Fatih Cantepe100% (1)
- SOAL MID TERM ENGLISH 13 Tyad 1Document6 pagesSOAL MID TERM ENGLISH 13 Tyad 1ani julitaNo ratings yet
- A1 (2 3 4) F./... D 6905 Af/1Document3 pagesA1 (2 3 4) F./... D 6905 Af/1GERALD SIMONNo ratings yet
- Arts Lessonplantemplatevisualarts2019Document18 pagesArts Lessonplantemplatevisualarts2019api-451772183No ratings yet
- Pioneering Urban Practices in Transition SpacesDocument10 pagesPioneering Urban Practices in Transition SpacesFloorin OlariuNo ratings yet
- A Button Die Is Used As A Part Inserted in A Die PlateDocument6 pagesA Button Die Is Used As A Part Inserted in A Die PlateMeyyappan VeerappanNo ratings yet
- 1884 Journey From Heraut To Khiva Moscow and ST Petersburgh Vol 2 by Abbott S PDFDocument342 pages1884 Journey From Heraut To Khiva Moscow and ST Petersburgh Vol 2 by Abbott S PDFBilal AfridiNo ratings yet
- Eb 12Document25 pagesEb 12SrewaBenshebilNo ratings yet
- NO Memo No. 21 S. 2018 Adherence To Training Policy PDFDocument10 pagesNO Memo No. 21 S. 2018 Adherence To Training Policy PDFKemberly Semaña PentonNo ratings yet
- OceanofPDF - Com Ruination - Anthony ReynoldsDocument440 pagesOceanofPDF - Com Ruination - Anthony ReynoldsiAmNewbita100% (1)
- Learning Action Cell Implementation Plan (Tle Department)Document4 pagesLearning Action Cell Implementation Plan (Tle Department)AlmaRoxanneFriginal-TevesNo ratings yet
- 2021 HhhhhhhterqasdwqwDocument1 page2021 HhhhhhhterqasdwqwHassan KhanNo ratings yet
- Kroenke, K. Et Al (2002) The PHQ-15 - Validity of A New Measure For Evaluating The Severity of Somatic SymptomsDocument9 pagesKroenke, K. Et Al (2002) The PHQ-15 - Validity of A New Measure For Evaluating The Severity of Somatic SymptomsKristopher MacKenzie BrignardelloNo ratings yet
- Fragment D Une Statue D Osiris ConsacreDocument11 pagesFragment D Une Statue D Osiris ConsacrePedro Hernández PostelNo ratings yet
365 Full PDF
365 Full PDF
Uploaded by
razgriz110Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
365 Full PDF
365 Full PDF
Uploaded by
razgriz110Copyright:
Available Formats
Review
Synthse
Salt and water: a simple approach to hyponatremia
Karen E. Yeates, Michael Singer, A. Ross Morton
Abstract
HYPONATREMIA IS COMMON IN BOTH INPATIENTS and outpatients. Medications are often the cause of acute or chronic hyponatremia.
Measuring the serum osmolality, urine sodium concentration and
urine osmolality will help differentiate among the possible causes.
Hyponatremia in the physical states of extracellular fluid (ECF) volume contraction and expansion can be easy to diagnose but often
proves difficult to manage. In patients with these states or with normal or near-normal ECF volume, the syndrome of inappropriate
secretion of antidiuretic hormone is a diagnosis of exclusion, requiring a thorough search for all other possible causes. Hyponatremia should be corrected at a rate similar to that at which it developed. When symptoms are mild, hyponatremia should be
managed conservatively, with therapy aimed at removing the offending cause. When symptoms are severe, therapy should be
aimed at more aggressive correction of the serum sodium concentration, typically with intravenous therapy in the inpatient setting.
CMAJ 2004;170(3):365-9
Case
A 72-year-old woman presents to your office with a 2-day history of presyncope when rising from a chair. She has been taking
hydrochlorothiazide, 25 mg/d, for 5 years for systolic hypertension. Over the last week she has had a bout of viral gastroenteritis with marked diarrhea. She has been trying to replace the lost
fluids by drinking 23 L of water per day. You determine that
when she rises from a seated position, her blood pressure drops
20 mm Hg; her jugular venous pressure is low. Serum levels are
as follows: sodium 128 mmol/L, potassium 3.1 mmol/L, creatinine 125 mmol/L and urea nitrogen 10 mmol/L.
What is your approach to this womans hyponatremia?
yponatremia is common in both inpatients and
outpatients. Its causes are numerous and often
elusive. Having a simple approach to assessment
and treatment can be helpful in most cases that present in
clinical practice. This review is meant to be a simplified,
clinically based overview of the diagnosis and management
of hyponatremia. Pathophysiological details of common
and rare causes of hyponatremia and a detailed laboratory
approach to diagnosis can be found elsewhere.1
Diagnosis
The symptoms and signs of hyponatremia vary from
subtle to extreme; none is specific (Box 1). The diagnosis is
confirmed by laboratory findings. Hyponatremia is typically defined as a serum sodium concentration of less than
134 mmol/L. In the past, hyponatremia was often diag-
nosed erroneously when the patient had high levels of
serum lipids or plasma proteins. This should no longer be a
concern because of the sodium electrode method used in
almost every centre in Canada. In addition, hyponatremia
occurs, but is not usually symptomatic, when the serum osmolality is elevated by severe hyperglycemia or mannitol
infusion. The lowered serum sodium concentration is due
to dilution by osmotic shifts of water out of cells. In these
cases, the high serum osmolality will help to differentiate
these causes from other true causes.
True hyponatremia occurs when the serum osmolality
or tonicity is decreased. For this defect to occur, there has
to be some inability of the body to excrete free water
through the kidneys despite continued water intake. This
can occur in the following 3 settings (Table 1).
Contracted extracellular fluid (ECF) volume
With ECF volume contraction from any cause (diarrhea,
vomiting, excessive sweating, diuretic use), the release of
antidiuretic hormone (ADH) is stimulated to defend ECF
volume; this makes the kidneys distal tubules more permeable to water reabsorption. Furthermore, renin is released in
response to the decreased renal perfusion secondary to ongoing volume contraction, and this signals the kidneys to
avidly retain sodium. This concomitant retention of water
and sodium is appropriate in this setting and is supported by
a low urine sodium concentration (< 20 mmol/L) and, often,
a low urine volume. Often the person who has a contracted
ECF volume will drink water or another low-solute fluid
(e.g., tea), which contributes further to the hyponatremia.
These patients, by definition, have serum sodium and body
water levels that are lower than normal but have more loss
of sodium relative to loss of water.4,5
Box 1: Symptoms and signs
of hyponatremia
None
Headache
Lethargy
Dizziness and ataxia
Mild confusion
Psychosis
Seizures
Coma
CMAJ FEB. 3, 2004; 170 (3)
2004 Canadian Medical Association or its licensors
365
Yeates et al
Normal or near-normal ECF volume
In the setting of hyponatremia and clinically normal or
near-normal ECF volume, ADH release or renal tubular
responsiveness to ADH may be unrelated to serum tonicity
or ECF volume contraction. In these situations, the patient
is said to have the syndrome of inappropriate secretion of
ADH (SIADH) or a reset osmostat.3,610 In SIADH, the
serum sodium concentration falls as the kidneys inappropriately retain free water. The patients normal amount of
body sodium is functionally diluted by the retained water.
The patient appears to have a normal ECF volume or mild
ECF volume overload (near normal). The urine sodium
concentration is typically greater than 40 mmol/L.
The many causes of SIADH (Box 2) include almost any
pulmonary or neurologic problem. Some lung cancers can
produce ectopic ADH, which signals inappropriately to the
kidney. Numerous medications can have an ADH-like effect on the renal tubules or potentiate the effect of endogenous ADH: some of the more common agents are presented in Box 3. Other stimuli include pain and excessive
nausea and vomiting.1114
Two other potential causes of hyponatremia in patients
with normal or near-normal ECF volume are hypothyroidism and adrenal insufficiency. A diagnosis of SIADH
can be made only when these conditions have been ruled
out by appropriate tests (e.g., determining the serum concentration of thyroid stimulating hormone or performing
the cortisol stimulation test) and cannot be made when the
patient has renal failure or an abnormal ECF volume.
In the rarer setting of a reset osmostat, which can occur
in various chronic and debilitating disease states, there is
felt to be a lowered setting of osmoreceptors. In these
cases, the receptors will stimulate ADH release at lower
serum osmolalities. Typically this resetting is chronic and
the diagnosis is suspected because the serum sodium concentration, although lower (typically 124134 mmol/L), is
stable and remains at these levels for long periods. By definition, as in the diagnosis of SIADH, these patients must
have normal renal, thyroid and adrenal function. Although
beyond the scope of this review, the diagnosis of reset osmostat can be made by challenging these patients with a
water load and measuring the ability to maximally dilute
the urine osmolality.35
Box 2: Causes of syndrome of inappropriate
secretion of antidiuretic hormone (SIADH)
Malignant disease
Bronchogenic carcinoma
Pulmonary disorders
Viral and bacterial pneumonias
Tuberculosis
Neurologic disorders
Encephalitis
Meningitis
Trauma
Stroke
Alcohol withdrawal
Other
HIV/AIDS
Acute psychosis
Acute intermittent porphyria
Idiopathic
Table 1: Causes and characteristics of hyponatremia*
Volume of extracellular fluid
Variable
Normal or
near normal
Contracted
Expanded
Causes
Diarrhea; vomiting;
excessive sweating; poor
water intake; diuretic use
Syndrome of inappropriate
secretion of antidiuretic
hormone; hypothyroidism;
adrenal insufficiency
Congestive heart failure;
cirrhotic liver disease;
nephrotic syndrome
Serum osmolality
Low
Low
Low
Urine osmolality,
mOsm/L
> 500
> 100
> 100
Urine volume
Usually decreased
Varies with intake
Usually decreased
Urine sodium
concentration, mmol/L
< 20
> 40
< 20
Response to 0.9% saline
infusion
Clinical and biochemical
improvement
No change or worsening of
hyponatremia
Little change in hyponatremia;
worsening of edema
*For simplicity, conditions such as cerebral salt wasting2 and reset osmostat3 have been omitted.
Values less than 100 imply an appropriate pituitary and renal response to hyponatremia, as would be expected with psychogenic polydipsia. The variability in urine
osmolality results in low sensitivity and specificity for causes of hyponatremia in which the osmolality is greater than 100 mOsm/L.
May be greater than 20 with diuretic use.
366
JAMC 3 FVR. 2004; 170 (3)
Diagnosis and management of hyponatremia
Management
Box 3: Drugs causing hyponatremia
Drugs that stimulate the release of antidiuretic
hormone (ADH)
Carbamazepine
Antidepressants
Clofibrate
Chlorpropamide
Opiates
Drugs that potentiate ADH in the kidneys
NSAIDs
Cyclophosphamide
Drugs whose mechanism is unclear
Haloperidol
Amitriptyline
Ecstasy (methylenedioxymethamphetamine)
Expanded ECF volume
The key to effective management of hyponatremia is establishing the type and its cause, so that the cause can be
removed, if possible, and the management will be appropriate. Paramount is clarifying whether the hyponatremia has
developed quickly (over a few days) and is acute or whether
it has developed over days to weeks and is chronic. The rapidity of correction of the serum sodium concentration
should be closely linked to the suspected time over which
the hyponatremia has developed.
If the patient has only mild symptoms of hyponatremia
(headache, lethargy, dizziness), or is asymptomatic, and the
hyponatremia is not severe (sodium level > 125 mmol/L),
we recommend a conservative approach. Discontinuation of
all possible offending drugs is important. In SIADH or the
edema-producing states, a trial of water restriction to less
than 1 to 1.25 L/d (depending on the degree of hyponatremia) can be attempted; the serum sodium level should be
measured at regular intervals to look for improvement.4,812
If the serum sodium level continues to fall, the patient
may require an intravenous trial of normal saline to clarify
the diagnosis. If the patient has ECF volume contraction
(which may not be clinically apparent), a trial of saline will
always improve the serum sodium level. If the patient has
SIADH, the hyponatremia will worsen. The trial should be
done with caution, following the rules for sodium correction (Box 4). Rapid correction can result in osmotic demyelination syndrome, with resultant severe brain injury
and potentially death.912,15
Hyponatremia that has developed slowly (over several
weeks) must be clearly distinguished from acute, newly developed hyponatremia. Patients with chronically low serum
sodium concentrations tend to be the least symptomatic
The cause of this type of hyponatremia is usually easy to
identify. Edema-producing states, such as chronic congestive
heart failure, cirrhosis and nephrotic syndrome, can all cause
hyponatremia. The patients have an ECF volume overload
and an elevated body content of sodium and water but, by
definition, have more water relative to sodium. However,
these patients often have a low effective circulating volume
and poor renal perfusion. Because the kidney does not distinguish between a low effective circulating volume and ECF
volume contraction, it will avidly retain sodium and water,
which leads to edema. The urine sodium concentration is
usually less than 20 mmol/L but may be higher if the patient
is receiving diuretic therapy. These patients may also have ECF volume contraction from correctible causes and may reBox 4: Rules for sodium correction
spond to a gentle oral challenge of isotonic
In general, correct the serum sodium concentration at an hourly rate
salt and water. Nephrotic syndrome can
of no more than 0.5 mmol/L.
be ruled out by testing a urine sample and
a 24-hour urine collection for protein; the
If symptoms are severe, more rapid correction is necessary in the first
few hours, since the patient is at risk of cerebral edema.
24-hour amount will be greater than 3.0 g
in nephrotic syndrome.
With intravenous therapy, correct the serum sodium concentration by
Rarely, in the outpatient setting, a pano more than 12 mmol/L in the first 1216 hours, or 0.51.0 mmol/L
per hour.
tient will present with hyponatremia secondary to psychogenic polydipsia. Typi Choose an intravenous solution according to the symptoms. Reserve
cally seen in patients with schizophrenia or
hypertonic saline (5 mmol/10 mL) for patients with severe symptoms.
Given at a rate of 25 mL/h, this solution should correct the serum
other psychiatric diseases, this disorder is
sodium concentration by about 10 mmol/L over the first day. Isotonic
due to ingestion of large volumes of water
saline should, as a rule, raise the serum sodium concentration by
(> 20 L) over a short period. The hypona12 mmol/L per litre of infused saline.
tremia, which can cause confusion or
In extracellular fluid (ECF) volume contraction, isotonic saline should
seizures, develops temporarily and resolves
be the first choice for therapy, as it will expand the ECF volume,
quickly as the kidneys work to excrete the
which will lead to decreased ADH release and help correct the serum
excessive free water.4,5,7 The urine is dilute
sodium concentration.
(osmolality < 100 mOsm/L), as is the
serum (normal range, 280295 mOsm/L).
CMAJ FEB. 3, 2004; 170 (3)
367
Yeates et al
and are at highest risk of severe side effects if the sodium
concentration is corrected too rapidly.1624
The long-term management of SIADH can be difficult
when no offending agent can be found or the process at
work is not reversible (as with bronchogenic or other carcinomas). It is possible to inhibit the renal effects of ADH
with lithium carbonate, but this agent has a narrow thera-
peutic index.19 Demeclocycline (a tetracycline), 600 mg
daily, may also be used, since it inhibits cyclic adenosine
monophosphate, which diminishes the intracellular effects
of ADH on the renal tubular cells.19
The management of hyponatremia in patients with hypervolemia can be difficult. Water restriction to less than
1.25 L/d is essential. Sodium restriction to 70 mmol/d
Is the hyponatremia severe?
([Na+] < 125 mmol/L)
Yes
No
Significant
sequelae unlikely
Are there symptoms?
(confusion, ataxia, headache,
seizures, obtundation)
Yes
No
Hyponatremia likely
chronic
What is the duration of
the hyponatremia?
Acute
(< 48 h)
Chronic/unknown
(> 48 h)
Emergency correction with
hypertonic (3%) saline (12 mL/kg
hourly until [Na+] > 125 mmol/L)
Urgent correction with 0.9% saline or, until
symptoms resolve, with hypertonic (3%) saline
(12 mL/kg hourly); thereafter, correct at rate of
about 0.5 mmol/L hourly with 0.9% saline
Urgent intervention
unnecessary. Assess ECF
volume and correct
[Na+] at hourly rate of
about 0.5 mmol/L
What is the ECF volume status?
Contracted
Discontinue offending medications;
restore intravascular volume with 0.9%
saline, given intravenously; then give
salt and water orally
Normal or near normal
Rule out hypothyroidism and
hypoadrenalism; discontinue offending
medications; restrict fluids to 7501500
mL/d; give demeclocylcine, 600 mg/d
Expanded
Optimize treatment of underlying
problems (cardiac, hepatic, renal);
restrict salt and water intake; give
diuretics
Fig. 1: Algorithm for the recommended management of hyponatremia. [Na+] = serum sodium concentration; ECF = extracellular fluid.
368
JAMC 3 FVR. 2004; 170 (3)
Diagnosis and management of hyponatremia
(with the aid of a dietitian) will help with edema. A loop diuretic should be used to promote sodium and water excretion by the kidneys. In both congestive heart failure and
cirrhosis, the addition of a potassium-sparing diuretic is
useful to prevent hypokalemia and lessen edema (and ascites). Referral to a cardiologist or hepatologist may be necessary in cases of refractory heart failure or cirrhotic ascites.
Patients with nephrotic syndrome should be referred to a
nephrologist, as specific therapies (e.g., with corticosteroids
and immunosuppressive drugs) may be directed at the
cause of their disease and reduce proteinuria.
Fig. 1 presents a suggested management algorithm.
The case revisited
The patient has clinical signs of ECF volume contraction. The most likely cause is gastrointestinal losses of salt
and water, with only water replacement. It is also likely that
the thiazide diuretic is contributing to the hyponatremia.
Thiazides impair the kidneys ability to produce a dilute
urine.19 Both thiazides and loop diuretics (e.g., furosemide)
impair the kidneys ability to reabsorb sodium, but thiazides also impair free water excretion.24,25 With continued
fluid intake and impaired excretion of water, hyponatremia
can develop rapidly. The ECF volume contraction, diarrheal losses and diuretic use have also resulted in hypokalemia in this patient. As ECF volume contraction develops, the kidneys actively excrete potassium in exchange for
sodium in an attempt to preserve ECF volume.
Another factor potentially contributing to this patients
hyponatremia may be the tea and toast phenomenon. In
elderly patients with a diet poor in protein and sodium, hyponatremia may be worsened by their low solute intake.
The kidneys need to excrete solutes aids in water excretion. An increase in dietary protein and salt can help improve water excretion. By a mechanism similar to that in
the tea and toast phenomenon, hyponatremia can occur
with excessive beer drinking, although this was unlikely in
our patient. Beer-drinkers potomania is caused by a beer
diet that is high in fluid but low in solute. In both situations, a 24-hour urine collection will reveal a solute excretion of less than 500 mOsm/d.
The management of our patient should include temporary discontinuation of the thiazide diuretic. Although her
hyponatremia has developed over about a week, she has clear
evidence of ECF volume contraction. Volume restoration
with normal saline and potassium replacement is required until the postural drop in blood pressure is less than 10 mm Hg.
She should then be treated conservatively with oral sodium
and potassium replacement. She should be reassessed frequently to ensure improvement. An alternative medication
should be sought to treat her systolic hypertension.26 If the
thiazide diuretic is to be reintroduced, measurement of the
serum electrolyte concentrations should be undertaken
57 days later to ensure that hyponatremia has not recurred.
This article has been peer reviewed.
From the Department of Medicine, Division of Nephrology, Queens University,
Kingston, Ont. (all authors)
Competing interests: None declared.
Contributors: Dr. Yeates was the principal author and revised and prepared the final version. Dr. Morton assisted in redesigning the algorithms and boxes.
Drs. Morton and Singer critically reviewed and revised the article for important
intellectual content. All authors approved the version to be published.
References
1. Haralampos J, Milionis GL, Elisaf MS. The hyponatremic patient: a systematic approach to laboratory diagnosis [review]. CMAJ 2002;166(8):1056-62.
2. Palmer BF. Hyponatremia in neurosurgical patients: syndrome of inappropriate antidiuretic hormone versus cerebral salt wasting. Nephrol Dial Transplant
2000;15:262-8.
3. Kahn T. Reset osmostat and salt and water retention in the course of severe
hyponatremia. Medicine (Baltimore) 2003;82:170-6.
4. Halperin M, Goldstein M. Fluid, electrolyte and acid-base physiology: a problem
based approach. 3rd ed. Philadelphia: WB Saunders Company; 1998.
5. Preston R. Acid-base, fluids and electrolytes made ridiculously simple. Miami:
Medmaster; 1997.
6. Adrogue HJ, Madias NE, Hyponatremia. N Engl J Med 2000;342:1581-86.
7. Chung HM, Kluge R, Schrier R. Clinical assessment of extracellular fluid volume in hyponatremia. Am J Med 1987;83:905-8.
8. Anderson RJ. Hospital associated hyponatremia. Kidney Int 1986;29:1237-47.
9. Sterns RH, Cappuccio JD, Silver SM, Cohen EP. Neurologic sequelae after
treatment of severe hyponatremia: A multicenter perspective. J Am Soc
Nephrol 1994;4:1522-30.
10. Sterns RH, Thomas DJ, Herndon RM. Brain dehydration and neurologic deterioration after correction of hyponatremia. Kidney Int 1989;35:69-75.
11. Berl T. Treating hyponatremia: Damned if we do and damned if we dont [review]. Kidney Int 1990;37:1006-18.
12. Laureno R, Karp BI. Myelinolysis after correction of hyponatremia. Ann Intern Med 1997;126:57-62.
13. Holden R, Jackson MA. Near-fatal hyponatremic coma due to vasopressin
over-secretion after ecstasy (3,4-MDMA). Lancet 1996;347:1052-3.
14. Maesaka JK. An expanded view of SIADH, hyponatremia and hypouricemia.
Clin Nephrol 1996;46:79-83.
15. Ayus JC, Arieff AI. Chronic hyponatremic encephalopathy in postmenopausal
women: association of therapies with morbidity and mortality. JAMA 1999;
281:2299-304.
16. Strange K. Regulation of solute and water balance and cell volume in the central nervous system. J Am Soc Nephrol 1992;3:12-27.
17. Ellis SJ. Severe hyponatremia: complications and treatment. Q J Med 1995;
88:905-9.
18. Ayus JC, Wheeler JM, Arief AI. Postoperative hyponatremia encephalopathy
in menstruant women. Ann Intern Med 1992;117:891-7.
19. Forrest JN, Cox M, Hong C, et al. Superiority of demeclocycline over
lithium in the treatment of chronic syndrome of inappropriate secretion of
antidiuretic hormone. N Engl J Med 1978;298:173-81.
20. Arieff AI. Hyponatremia, convulsions, respiratory arrest, and permanent brain
damage after elective surgery in healthy women. N Engl J Med 1986;314:
1529-40.
21. Sterns RH. The management of symptomatic hyponatremia. Semin Nephrol
1990;10:503-14.
22. Sterns RH. The treatment of hyponatremia: First do no harm. Am J Med
1990;88:557-60.
23. Lien YH, Shapiro JI, Chan L. Study of brain electrolytes and osmolytes during correction of chronic hyponatremia. Implications for the pathogenesis of
central pontine myelinolysis. J Clin Invest 1991;88:303-9.
24. Friedman E, Shadel M, Hallan H, Fardel Z. Thiazide induced hyponatremia.
Reproducibility by single-dose challenge and analysis of pathogenesis. Ann Intern Med 1989;110:24-9.
25. Clark BA, Shannon RP, Rosa RM, Epstein FH. Increased susceptibility to thiazide induced hyponatremia in the elderly. J Am Soc Nephrol 1994;5:1106-11.
26. Campbell NRC, Drouin D, Feldman RD; Canadian Hypertension Recommendations Working Group. The 2001 Canadian hypertension recommendations: take-home messages [erratum in CMAJ 2002;167(9):989]. CMAJ
2002;167(6):661-8.
Correspondence to: Dr. Karen E. Yeates, University Health
Network, 620 University Ave., Toronto, ON M5G 2C1
CMAJ FEB. 3, 2004; 170 (3)
369
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5820)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (845)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (898)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (349)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- 1.1 - Staph AureusDocument22 pages1.1 - Staph Aureusrazgriz1100% (1)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- 1.3 - Strep Pyogenes (Group A Strep)Document27 pages1.3 - Strep Pyogenes (Group A Strep)razgriz110No ratings yet
- AWS Vs Azure Vs Google Cloud - A Detailed Comparison of The Cloud Services Giants PDFDocument10 pagesAWS Vs Azure Vs Google Cloud - A Detailed Comparison of The Cloud Services Giants PDFSakthivel PNo ratings yet
- 1.2 - Staph EpidermidisDocument13 pages1.2 - Staph Epidermidisrazgriz110No ratings yet
- Falls in The ElderlyDocument32 pagesFalls in The Elderlyrazgriz110100% (1)
- Eaton DX-RT 6000 VA (Long Back UP) 1x1 UPS SystemDocument4 pagesEaton DX-RT 6000 VA (Long Back UP) 1x1 UPS SystemPhaniNo ratings yet
- OrDocument3 pagesOrsatishsaga1990No ratings yet
- Gr11 Mock Exam Schedule 2024Document13 pagesGr11 Mock Exam Schedule 2024potrillo0330No ratings yet
- 30 Top HTML Interview Questions and AnswersDocument15 pages30 Top HTML Interview Questions and AnswersAurobindaNo ratings yet
- Bishop 1997Document25 pagesBishop 1997Celina AgostinhoNo ratings yet
- Final DKSSKDocument79 pagesFinal DKSSKSarita Latthe100% (2)
- Letters From England: by Don Manuel Alvarez EspriellaDocument2 pagesLetters From England: by Don Manuel Alvarez EspriellaPickering and ChattoNo ratings yet
- CH 12Document31 pagesCH 12asin12336No ratings yet
- Tesa-60150 MSDSDocument11 pagesTesa-60150 MSDSBalagopal U RNo ratings yet
- Job Hazard Analysis: Basic Job Steps Potential Hazards Recommended Actions or ProcedureDocument3 pagesJob Hazard Analysis: Basic Job Steps Potential Hazards Recommended Actions or ProcedureBernard Christian DimaguilaNo ratings yet
- PDS - SP-9888 Tank Lining PDFDocument6 pagesPDS - SP-9888 Tank Lining PDFSherif AbdelhameedNo ratings yet
- IGST CH Status As On 01.01.2018Document443 pagesIGST CH Status As On 01.01.2018SK Business groupNo ratings yet
- Make Wire Transfers Through Online Banking From AnywhereDocument2 pagesMake Wire Transfers Through Online Banking From AnywhereDani PermanaNo ratings yet
- ISO 9001 Awareness AmaDocument51 pagesISO 9001 Awareness AmaHisar SimanjuntakNo ratings yet
- GPRS Evolution PH 2Document43 pagesGPRS Evolution PH 2Nur AfiyatNo ratings yet
- Machiavellian Reflections (Part 1) : PreambleDocument9 pagesMachiavellian Reflections (Part 1) : PreambleMuhammet Fatih Cantepe100% (1)
- SOAL MID TERM ENGLISH 13 Tyad 1Document6 pagesSOAL MID TERM ENGLISH 13 Tyad 1ani julitaNo ratings yet
- A1 (2 3 4) F./... D 6905 Af/1Document3 pagesA1 (2 3 4) F./... D 6905 Af/1GERALD SIMONNo ratings yet
- Arts Lessonplantemplatevisualarts2019Document18 pagesArts Lessonplantemplatevisualarts2019api-451772183No ratings yet
- Pioneering Urban Practices in Transition SpacesDocument10 pagesPioneering Urban Practices in Transition SpacesFloorin OlariuNo ratings yet
- A Button Die Is Used As A Part Inserted in A Die PlateDocument6 pagesA Button Die Is Used As A Part Inserted in A Die PlateMeyyappan VeerappanNo ratings yet
- 1884 Journey From Heraut To Khiva Moscow and ST Petersburgh Vol 2 by Abbott S PDFDocument342 pages1884 Journey From Heraut To Khiva Moscow and ST Petersburgh Vol 2 by Abbott S PDFBilal AfridiNo ratings yet
- Eb 12Document25 pagesEb 12SrewaBenshebilNo ratings yet
- NO Memo No. 21 S. 2018 Adherence To Training Policy PDFDocument10 pagesNO Memo No. 21 S. 2018 Adherence To Training Policy PDFKemberly Semaña PentonNo ratings yet
- OceanofPDF - Com Ruination - Anthony ReynoldsDocument440 pagesOceanofPDF - Com Ruination - Anthony ReynoldsiAmNewbita100% (1)
- Learning Action Cell Implementation Plan (Tle Department)Document4 pagesLearning Action Cell Implementation Plan (Tle Department)AlmaRoxanneFriginal-TevesNo ratings yet
- 2021 HhhhhhhterqasdwqwDocument1 page2021 HhhhhhhterqasdwqwHassan KhanNo ratings yet
- Kroenke, K. Et Al (2002) The PHQ-15 - Validity of A New Measure For Evaluating The Severity of Somatic SymptomsDocument9 pagesKroenke, K. Et Al (2002) The PHQ-15 - Validity of A New Measure For Evaluating The Severity of Somatic SymptomsKristopher MacKenzie BrignardelloNo ratings yet
- Fragment D Une Statue D Osiris ConsacreDocument11 pagesFragment D Une Statue D Osiris ConsacrePedro Hernández PostelNo ratings yet