Professional Documents
Culture Documents
Beta-Thalassemia Major and Pregnancy: Clinical Study
Beta-Thalassemia Major and Pregnancy: Clinical Study
Uploaded by
herryOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Beta-Thalassemia Major and Pregnancy: Clinical Study
Beta-Thalassemia Major and Pregnancy: Clinical Study
Uploaded by
herryCopyright:
Available Formats
Bratisl Lek Listy 2013; 114 (9)
DOI: 10.4149/BLL_2013_109
523 525
CLINICAL STUDY
Beta-Thalassemia major and pregnancy
Gulino FA1, Vitale SG2, Fauzia M1, Cianci S2, Pafumi C1, Palumbo MA1
Center of Physiopathology of Reproduction, Dpt of Surgery, S. Bambino Hospital, University of Catania, Italy.
vitalesalvatore@hotmail.com
Abstract: Objective: It was studied the clinical management and the medical outcomes of 6 pregnancies in 5
women affected by Beta Thalassemia major, based on last guidelines and pharmacological treatments.
Background: Paediatric Department and Department of Obstetrics and Gynaecology of the University of Catania.
Methods: These patients were taken among a group of 116 women affected by beta-thalassemia major divided
into three subgroups, according to the characteristics of their menstrual cycle: 1) women with primitive amenorrhoea, 2) women with secondary amenorrhoea and 3) women with normal menstruation. Only one woman,
affected by primitive amenorrhoea, needed the induction of ovulation. An accurate and detailed pre-pregnancy
assessment was effected before each conception. This was constituted by a series of essays, including checks
for diabetes and hypothyroidism, for B and C hepatitis and for blood group antibodies. Moreover were evaluated: cardiac function, rubella immunity and transaminases. Other pregnancy monitoring, and cares during labour and delivery were effected according to usual obstetrics practice.
Results: All the women were in labour when they were 38 week pregnant, and the outcome were six healthy babies
born at term. There were no complications related to the pregnancy and to the immediate outcome after delivery.
Conclusions: The improvements of current treatments, especially in the management of iron deposits, the prolongation of survival rate, will result in a continuous increase of pregnancies in thalassemic women. Pregnancy is
now a real possibility for women affected by such disease. Although numerous complications can occur, vigilant
monitoring by both experienced obstetricians and hematologists can lead to successful pregnancy outcomes
(Tab. 1, Fig. 1, Ref. 16). Full Text in PDF www.elis.sk.
Key words: beta-thalassemia major, fertility, pregnancy, haemoglobinopathia, amenorrhoea.
Beta-thalassemias (-thalassemias) are a group of inherited
blood disorders caused by reduced or absent synthesis of the beta
chains of haemoglobin resulting in variable phenotypes ranging
from severe anemia to clinically asymptomatic individuals.
The phenotypes of homozygous or genetic heterozygous compound beta-thalassemias include thalassemia major and thalassemia intermedia. Individuals with thalassemia major usually come
to medical attention within the first two years of life and require
regular RBC transfusions to survive.
Clinical presentation of thalassemia major occurs between 6
and 24 months. Affected infants fail to thrive and become progressively pale. Feeding problems, diarrhea, irritability, recurrent bouts
of fever, and progressive enlargement of the abdomen caused by
spleen and liver enlargement may occur (1).
The ideal management of thalassemia involves a multidisciplinary therapeutic team approach (2) and should be preferably
done at a comprehensive thalassemia care center having a team of
pediatric hematologist, pediatrician, transfusion medicine special1
Center of Physiopathology of Reproduction, Dpt of Surgery, S. Bambino
Hospital, University of Catania, Italy, and 2Azienda Ospedaliero-Universitaria Policlinico-Vittorio Emanuele G. Rodolico Operative Unit of
Obstetrics and Gynaecology- University of Catania, Italy
Address for correspondence: S.G. Vitale, Dr, Viale della Liberta No.
212, 95129 Catania (CT), Italy.
Phone: +39.3479354575
ist, endocrinologist, psychologist, social worker, and the backup
of a well-equipped blood bank (3).
If a regular transfusion program that maintains a minimum Hb
concentration of 9.5 to 10.5 g/dL is initiated, growth and development tends to be normal up to 10 to 12 years (2).
Gonadal function is impaired in the majority of the patients affected by the homozygous kind of this disease and, especially in females, this is expressed either by a delay in the onset of puberty and
menstruation or by secondary amenorrhoea (4). The commonest abnormality was hypogonadotropic hypogonadism, but the relatively
high prevalence of other endocrine impairments, causing multiple
endocrinopathies, is also well recognised. These kind of endocrine
complications are directly related to the serum ferritin level (5).
For delayed puberty in girls, therapy may start with the administration of ethinyl estradiol (2.55 g daily) for 6 months, followed
by hormonal reassessment. If spontaneous puberty does not occur
within 6 months, ethinyl estradiol should be used at increasing dosages (from 510 g daily) for 12 months. If breakthrough uterine
bleeding does not occur, a low oestrogenprogesterone hormone
replacement is recommended (6). When there is a lack of pubertal
progression over a year or longer (arrested puberty) oestrogenprogesterone replacement therapy in females is indicated.
Nowadays, thanks to improved paediatric and haematological
cares, patients affected by Cooley disease may live on to be forty
or fifty, and can enjoy a quite regular standard of life. So that,
Indexed and abstracted in Science Citation Index Expanded and in Journal Citation Reports/Science Edition
Bratisl Lek Listy 2013; 114 (9)
523 525
maintaining a strict therapeutic regimen, women regularly transfused and well chelated can attempt to become pregnant (79).
In this study we describe the evolution and the successful
outcome of six at term pregnancies ruled out by five women affected by transfusion dependent beta Thalassemia. In reviewing
the cares and the complications during and after their pregnancies,
we discuss the issue concerning the appropriate preconception
counselling of such patients.
5
(21.7%)
For several years we have been following 116 women affected
by transfusion dependent beta Thalassemia major, diagnosed when
they were between 6 and 8 months old at the Paediatric Department
of the University of Catania, from the endocrine and reproductive
point of view. All of them were aged between 22 to 32 and received
a blood transfusion every 1520 days, in order to maintain the haemoglobin concentration above 10 g/dl; and were in strict desferrioxamine chelating therapy, to avoid excessive iron overloads. The
patients have been divided into three groups according to their first
and successive menstruation characteristics: 1) patients with primitive amenorrhoea, 2) patients with secondary amenorrhoea and 3)
patients with normal menstruation. In detail 23 of these women, got
married: 5 were affected by primitive amenorrhoea; 6 were affected
by secondary amenorrhoea and 12 women had normal menstruation. Finally six pregnancies occurred among these 23 women: two
among the patients affected respectively by primitive and secondary amenorrhoea, and four were carried out by women with spontaneous menstruation. Considering as to the last four pregnancies,
it is remarkable that to this group belonged a woman that had two
successful childbirths; so the total number of women we followed
was five (Fig. 1, Tab. 1). Average values of ferritin fluctuated between 500 and 1000 ng/ml, and transaminases were between 25
and 100 U/l. All of them were vaccinated against Hepatitis B Virus
(HBV), and two were splenectomized, particularly the woman affected by primitive amenorrhoea and one of those with normal periods. Only the women affected by primitive amenorrhoea needed
the induction of ovulation to stimulate her pregnancy. Evaluation
of eligibility depends upon the results of a series of examinations
regarding hearth, kidneys, thyroid, pancreas and peripheral arteries.
Haemosiderotic parenchimal deterioration, particularly of the myocardium, makes these patients potentially fragile, while the induction of ovulation may be a hard stress test even for a healthy woman.
Tab. 1. Table expressing the number of married women, the pregnancies, the medium age and the amount of each group, according to a
subdivision in three categories Normal menstruation, Secondary
Amenorrhoea and Primitive Amenorrhoea in reference to the total
amount of the 116 patients we studied.
524
Married
23
(19.8%)
Primitive
Amenorrhoea
Methods
Menstruation
characteristics
married women
number of pregnancy
spontaneous pregnancy
induced pregnancy
medium age
Total patients
116
Normal
menstruation
12
4 (30 %)
4 (100 %)
23.62.4
Secondary
amenorrhoea
6
1 (16.6 %)
1 (100 %)
24.71.6
Primary
amenorrhoea
5
1 (20 %)
1 (100 %)
26.13.2
Pregnancies
1
(20%)
Secondary
Amenorrhoea
6
(26.1%)
Pregnancies
1
(16.6%)
Single
93
(80.2%)
Normal
menstruation
12
(52.2%)
Pregnancies
4
(30%)
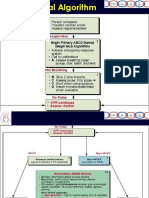
Fig. 1. Flow chart representing the distribution of 116 women affected
by Beta Thalassemia major subdivided in three categories, according
to their menstruation characteristics; considering if they are married
or singles, and the number of pregnancies carried out by each group.
However by the advanced cardiac magnetic resonance imaging
technique, early diagnosis of heart iron will allow the currently
available iron-chelating agents (oral and parenteral) to be used in
an innovative way to improve the quality of life and improve survival of patients with beta-thalassemia (10).
All the other women had spontaneous and physiological pregnancies. It is finally important to underline that all the partners of
these women were negative as regards the thalassemic trait.
According to the guidelines previously established by Tuck
(11), a precise and detailed pre-pregnancy assessment was effected before each conception. This was constituted by a series
of clinical and laboratory essays, including checks for diabetes
and hypothyroidism, for B and C hepatitis and for blood group
antibodies. Cardiac function was assessed symptomatically and
by echocardiography and exercise electrocardiography. Rubella
immunity was checked and immunisation was given when the
woman was found to be susceptible. During pregnancy the monitoring of all these factors continued, including frequent checks of
aminotransferase (AST and ALT transaminases).
The frequency of blood transfusion had to be increased, the aim
being to maintain the pre-transfusion haemoglobin concentration.
Deferoxamine therapy was stopped as soon as pregnancy was diagnosed, because using this drug during gestation could notoriously
induce teratogenic effects on the foetus, but the average values of
ferritin were just a little higher than the normal range observed.
Probably the foetus, due to a particular chelating activity, maintains
it during gestation. This therapy was quickly resumed after delivery
(12). Other pregnancy monitoring, such as for blood pressure, for
proteinuria and for fetal growth, and cares during labour and delivery were effected according to usual obstetrics practice and criteria.
Results
Only one of the six pregnancies we have followed needed the
induction of ovulation. Moreover a same woman carried out two
of them. All the women were in labour when she were 38 week
Gulino FA et al. Reproduction in women affected by Cooley disease
xx
pregnant, and the outcome were six healthy babies born at term
weighting between 2600 and 3300gs. The caesarean delivery was
preferred because of the frequent infertility/sterility that occurs
in the natural history of such kind of patients. All of these women
were neither HIV positive nor suffered from diabetes, however
they were controlled with a diet. All of them reported transaminases raising, but only in one case it was necessary to practice a
therapy based on silimarina. Moreover all of them had transfusion-transmitted C hepatitis prior to pregnancy, but only the one
affected by secondary amenorrhoea received curses of interferon
two years before embarking on pregnancy, because she showed to
be positive for HCV-RNA. Five out of the babies born were HCV
negative, while only one was HCV positive but HCV-RNA negative, so that it was not necessary to prescribe a therapy.
Finally, there were neither cardiac dysfunctions nor kidney
diseases reported, or other important affections.
It is the doctors responsibility to decide which patient can afford ovulation induction, when needed, pregnancy and labour, with
an acceptable degree of risk, and which are the limits of this risk.
In conclusion with improved life expectancy in the hemoglobinopathies, many women with these disorders are now choosing
to become pregnant. Although numerous complications can occur,
vigilant monitoring by both experienced obstetricians and hematologists can lead to successful pregnancy outcomes.
Pregnancy does not have a deleterious effect on the course of
their disease, and on the general wellness of the foetus. It seems, in
fact, that the evaluation of cardiac function, in combination with a
low iron load and satisfactory endocrine and hepatic controls can
ensure a pregnancy outcome with minimal adverse effects, and
not severe obstetric complications except for the high incidence
of caesarean sections (17) and the risk of thrombotic events (16).
Discussion
1. Galanello R, Origa R. Beta-thalassemia. Orphanet J Rare Dis. 2010; 5: 11.
Published online 2010 May 21. doi: 10.1186/1750-1172-5-11.
We believe that several ethical and theoretical questions should
be evaluated before the observation of technical problems. We
should never forget that Beta thalassemic are fragile patients who
are knowingly exposed to a large quantity of risks.
Several hemodynamic changes during pregnancy affect cardiac
function and are known to cause an increase in maternal cardiac
stress in the gestational period. An increase in blood volume, decrease in systemic vascular resistance, and augmentation of cardiac output occurs in all normal pregnancies to match maternalfetal demands (13). In one study of echocardiography in pregnant
-thalassemia patients without cardiac impairment, an appropriate
increase in cardiac output was observed secondary to an increase in
resting heart rate and left ventricular mass (14). Although cardiac
function did appear to return to pre-pregnancy levels after delivery, a subset of -TM patients was noted to have a late decline in
cardiac reserve in the years after gestation; however, the long-term
outcome for these patients is unknown.
More recent reports in -TM patients without cardiac impairment and treated with aggressive pre-pregnancy chelation have generally observed favorable outcomes. One of the largest modern studies of 58 pregnancies in -TM mothers found that impaired glucose
tolerance and gestational diabetes were frequent complications, occurring in 15 % of patients (15). Worsening of anemia during pregnancy also led to an increase in transfusion requirements of a median
of 25 mL/kg/y and a subsequent 60 % increase in baseline ferritin.
Fetal complications such as IUGR and premature delivery did appear
to be increased in -TM patients, occurring in nearly 40 % of infants;
however, because many of these women required fertility treatments,
twin pregnancies accounted for a major number of these births.
In -TI, the most significant adverse maternal outcome appeared to be thrombotic events, which occurred in 7.2 % of 83
pregnancies in one series (16). Development of anemia resulted in
a need for transfusion in 6080 % of -TI patients, 30 % of whom
had never had a transfusion before pregnancy (15, 16). IUGR and
prematurity rates were also noted to be high among -TI mothers,
occurring in 20 % and 30 % of infants, respectively (16).
2. Guide lines for the clinical management of thalassemia. 2nd ed. Nicosia Cyprus: Thalassemia International Federation; 2009. World Bank 2006, reported
joint WHO March of time meeting 2006-Quoted; p. 9.
References
3. Nadkarni A, Caraskar AC, Krishnamoorty R, Lu CY, Ghosh K, Colah R
et al. Molecular pathogenesis and clinical variability of thalassemia syndrome
among Indians. Am J Hematol 2001; 68: 7580.
4. Karagiorga-Lagana M. Fertility in Thalassemia: The Greek Experience. J
Pediatr Endocrinol Metab 1998; 11: 945951.
5. Jensen CE, Tuck SM, Old J et al. Incidence of endocrine complications and
clinical disease severity related to genotype analysis and iron overload in patients
with beta-thalassaemia. Eur J Haematol 1997; 59 (2): 7681.
6. De Sanctis V. Growth and puberty and its management in thalassemia. Horm
Res 2002; 58: 7279.
7. Kumar RM, Rizk DE, Khuranna A. Beta-Thalassemia major and successful
pregnancy. J Reprod Med 1997; 42 (5): 294298.
8. Tampakoudis P, Tsatalas C, Mamopoulos M, Tantanassis T, Christakis
JI, Sinakos Z, Mantalenakis S. Transfusion-dependent homozygous beta-Thalassaemia major: successful pregnancy in five cases. Eur J Obstet Reprod Biol
1997; 74 (2): 127131.
9. Daskalakis GJ, Papageorgiou IS, Antsaklis AJ, Michalas SK. Pregnancy and homozygous beta thalassaemia major. Br J Obstet Gynaecol 1998; 105 (9): 10281032.
10. Wonke B. Clinical management of beta-thalassemia major . Semin Hematol
2001; 38 (4): 350359.
11. Tuck SM, Jensen CE, Wonke B, Yardumian A. Pregnancy management
and outcomes in women with Thalassemia major. J Paediatr Endocrinol Metab
1998; 11 (3): 923928.
12. Pafumi C, Zizza G, Caruso S et al. Pregnancy outcome of a transfusiondependent thalassemic woman. Ann Hematol 2000; 79 (10): 571573.
13. Hill CC, Pickinpaugh J . Physiologic changes in pregnancy. Surg Clin North
Am 2008; 88 (2): 391401.
14. Aessopos A, Karabatsos F, Farmakis D et al. Pregnancy in patients with
well-treated beta-thalassemia: Outcome for mothers and newborn infants. Am J
Obstet Gynecol 1999; 180 (2 Pt 1): 360365.
15. Origa R, Piga A, Quarta G et al. Pregnancy and beta-thalassemia: An Italian
multicenter experience. Haematologica 2010; 95 (3): 376381.
16. Nassar AH, Naja M, Cesaretti C, Eprassi B, Cappellini MD, Taher A.
Pregnancy outcome in patients with beta-thalassemia intermedia at two tertiary
care centers, in Beirut and Milan. Haematologica 2010; 93 (10): 15861587.
Received December 2, 2010.
Accepted January 27, 2013.
525
You might also like
- PH Red Cross First Aid and BLS (Edited)Document41 pagesPH Red Cross First Aid and BLS (Edited)ctuagent75% (8)
- Case Analysis: Arnold Palmer HospitalDocument20 pagesCase Analysis: Arnold Palmer HospitalAlexis Rebano100% (3)
- Pregnancy in Patients With B-Thalassemia Intermedia: Outcome of Mothers and NewbornsDocument4 pagesPregnancy in Patients With B-Thalassemia Intermedia: Outcome of Mothers and NewbornsIlham RamadhanisNo ratings yet
- FTP PDFDocument4 pagesFTP PDFIzat FuadiNo ratings yet
- 1 PB PDFDocument7 pages1 PB PDFAmanda Mustika AdiNo ratings yet
- Leucemia Aguda en El Embarazo, 2021Document10 pagesLeucemia Aguda en El Embarazo, 2021AdrianNo ratings yet
- Ijrm 9 009 PDFDocument6 pagesIjrm 9 009 PDFWahyu PermataNo ratings yet
- Med Term JounralDocument6 pagesMed Term JounralKaroline FarleyNo ratings yet
- EG0800339 Hyperhomocysteinemia in Recurrent Miscarriage: Kh. R. Gaber, M. K. Farag, S. ET. Soliman, M. A. Abd Al-KaderDocument6 pagesEG0800339 Hyperhomocysteinemia in Recurrent Miscarriage: Kh. R. Gaber, M. K. Farag, S. ET. Soliman, M. A. Abd Al-KaderElena VisterniceanNo ratings yet
- Hum. Reprod.-2004-Carp-191-5Document5 pagesHum. Reprod.-2004-Carp-191-5venkayammaNo ratings yet
- Beta-Thalassemia Major and Pregnancy: September 2013Document4 pagesBeta-Thalassemia Major and Pregnancy: September 2013Wahyu PermataNo ratings yet
- Abnormal Uterine BleedingDocument11 pagesAbnormal Uterine BleedingKharmell Waters AndradeNo ratings yet
- 2017 Article 784Document5 pages2017 Article 784Elena ZepedaNo ratings yet
- Nama: Zaimah Shalsabilla Kelas: Alpha NIM: 04011181520071Document11 pagesNama: Zaimah Shalsabilla Kelas: Alpha NIM: 04011181520071shalsaNo ratings yet
- Inherited and Acquired Thrombophilia - Pregnancy Outcome and TreatmentDocument22 pagesInherited and Acquired Thrombophilia - Pregnancy Outcome and TreatmentLuiza RadulescuNo ratings yet
- Pre EclampsiaDocument12 pagesPre EclampsiaJohn Mark PocsidioNo ratings yet
- 1 s2.0 S1110569015300042 MainDocument5 pages1 s2.0 S1110569015300042 MainAzam alausyNo ratings yet
- Gong Fei (Orcid ID: 0000-0003-3699-8776) Li Xihong (Orcid ID: 0000-0002-0986-760X)Document21 pagesGong Fei (Orcid ID: 0000-0003-3699-8776) Li Xihong (Orcid ID: 0000-0002-0986-760X)Clarithq LengguNo ratings yet
- Acute Pyelonephritis in Pregnancy: An 18-Year Retrospective AnalysisDocument6 pagesAcute Pyelonephritis in Pregnancy: An 18-Year Retrospective AnalysisIntan Wahyu CahyaniNo ratings yet
- Management of HypertensionDocument6 pagesManagement of HypertensionRioNo ratings yet
- Thalassemic Mothers and Their Babies: AbstractDocument4 pagesThalassemic Mothers and Their Babies: AbstractWahyu PermataNo ratings yet
- Roush An 2011Document3 pagesRoush An 2011hamadahutpNo ratings yet
- Ojsadmin, 276Document6 pagesOjsadmin, 276komalvaid5No ratings yet
- Outcome of Pregnancy in Patients With Liver CirrhosisDocument7 pagesOutcome of Pregnancy in Patients With Liver CirrhosisSamirAyadNo ratings yet
- Management of The Critically Ill Obstetric Patient: ReviewDocument9 pagesManagement of The Critically Ill Obstetric Patient: ReviewAripinSyarifudinNo ratings yet
- Piis0002937811009185 PDFDocument24 pagesPiis0002937811009185 PDFLailatuss LelaNo ratings yet
- Recurrent Pregnancy Loss - Management - UpToDateDocument19 pagesRecurrent Pregnancy Loss - Management - UpToDateJean CarlosNo ratings yet
- Pregnancy Complications and Outcomes in Women With Epilepsy: Mirzaei Fatemeh, Ebrahimi B. NazaninDocument5 pagesPregnancy Complications and Outcomes in Women With Epilepsy: Mirzaei Fatemeh, Ebrahimi B. NazaninMentari SetiawatiNo ratings yet
- Konstantopoulos 2020Document14 pagesKonstantopoulos 2020Corey WoodsNo ratings yet
- The Impact of Preeclampsia in Pregnancy: Original ArticleDocument4 pagesThe Impact of Preeclampsia in Pregnancy: Original ArticleAnonymous YYWsfmocYNo ratings yet
- Acute Pyelonephritis in PregnancyDocument7 pagesAcute Pyelonephritis in PregnancyKvmLlyNo ratings yet
- Approach To The Patient With New-Onset Secondary Amenorrhea: Is This Primary Ovarian Insufficiency?Document11 pagesApproach To The Patient With New-Onset Secondary Amenorrhea: Is This Primary Ovarian Insufficiency?Patricia Rearte CarvalhoNo ratings yet
- Postpartum HemorrhageDocument22 pagesPostpartum HemorrhageReynaldiReikyHadiwijayaNo ratings yet
- Anticoagulants in PregnancyDocument8 pagesAnticoagulants in PregnancyNoha Mousa DarweashNo ratings yet
- Midwifery Triage of First Trimester Bleeding: Susan A. Krause,, and Barbara W. GravesDocument12 pagesMidwifery Triage of First Trimester Bleeding: Susan A. Krause,, and Barbara W. GravesRival Risvaldi RusliNo ratings yet
- Critical Illness in Pregnancy Part I: An Approach To A Pregnant Patient in The ICU and Common Obstetric DisordersDocument12 pagesCritical Illness in Pregnancy Part I: An Approach To A Pregnant Patient in The ICU and Common Obstetric Disordersgustavo1rodriguesNo ratings yet
- Hamil AnggurDocument7 pagesHamil AnggurIchunx MelissaNo ratings yet
- ShowText-1 (1) UnlockedDocument5 pagesShowText-1 (1) Unlocked12ock312No ratings yet
- Abnormal Uterine Bleeding in The Adolescent CME 2020Document7 pagesAbnormal Uterine Bleeding in The Adolescent CME 2020Mariana HernandezNo ratings yet
- Abnormal Bleeding in AdolescentDocument7 pagesAbnormal Bleeding in AdolescentRosa AlvaradoNo ratings yet
- Uterine Bleeding-A Case StudyDocument4 pagesUterine Bleeding-A Case StudyRoanne Lagua0% (1)
- Women's Health ArticleDocument15 pagesWomen's Health ArticleYuli HdyNo ratings yet
- Menstrual DisordersDocument8 pagesMenstrual DisordersBangkit Pank BuminataNo ratings yet
- Abstrak Makalah Bebas MedanDocument11 pagesAbstrak Makalah Bebas Medandr.raziNo ratings yet
- Nakimuli2016 Article TheBurdenOfMaternalMorbidityAnDocument8 pagesNakimuli2016 Article TheBurdenOfMaternalMorbidityAnPriscilla AdetiNo ratings yet
- Renal Disease and Pregnancy: Ghumman Surveen, Goel Neerja, Rajaram Shalini, HarshaDocument5 pagesRenal Disease and Pregnancy: Ghumman Surveen, Goel Neerja, Rajaram Shalini, HarshalukitaNo ratings yet
- 1 s2.0 S0020729209615502 Main PDFDocument1 page1 s2.0 S0020729209615502 Main PDFPaula UrsuNo ratings yet
- Distribution of Causes of Abnormal Uterine Bleeding Using The New FIGO Classification SystemDocument3 pagesDistribution of Causes of Abnormal Uterine Bleeding Using The New FIGO Classification SystemirmaarmiyahNo ratings yet
- Case Presentation Case 2Document19 pagesCase Presentation Case 2Daniel Andre S. SomorayNo ratings yet
- Materials and MethodsDocument1 pageMaterials and MethodsImtihanamiseNo ratings yet
- Thrombocytopenia at Different Stages of PregnancyDocument3 pagesThrombocytopenia at Different Stages of PregnancyInternational Journal of Clinical and Biomedical Research (IJCBR)No ratings yet
- Uterine AtonyDocument33 pagesUterine AtonyNonie 'Erni' HastiriniNo ratings yet
- AbortionDocument16 pagesAbortionAnatholeNo ratings yet
- Blood Reviews: Galit Sarig, Guy Vidergor, Benjamin BrennerDocument5 pagesBlood Reviews: Galit Sarig, Guy Vidergor, Benjamin BrennerMohamed Abd El DayemNo ratings yet
- Fetomaternal Outcome in Pregnancy With Severe ThrombocytopeniaDocument4 pagesFetomaternal Outcome in Pregnancy With Severe ThrombocytopeniaMuhammad AdithiaNo ratings yet
- Fetomaternal Outcome of Pregnancy With Hepatitis E InfectionDocument4 pagesFetomaternal Outcome of Pregnancy With Hepatitis E InfectionNZ FreelancersNo ratings yet
- Management of Malignant Gliomas During Pregnancy: A Case SeriesDocument6 pagesManagement of Malignant Gliomas During Pregnancy: A Case Seriesppds ui jan2017No ratings yet
- Pregnant Woman TemplateDocument11 pagesPregnant Woman TemplateRegine Mae Morales EncinadaNo ratings yet
- Pregnancy in A Patient With Recurrent GlioblastomaDocument6 pagesPregnancy in A Patient With Recurrent GlioblastomaNoraNo ratings yet
- Podocyturia As A DiagnosticMarker For Preeclampsia 2012Document6 pagesPodocyturia As A DiagnosticMarker For Preeclampsia 2012Diapositivas08No ratings yet
- Csii-Pregnancy in Patients With Mechanical Prosthetic ValvesDocument6 pagesCsii-Pregnancy in Patients With Mechanical Prosthetic Valvesapi-205989841No ratings yet
- Complementary and Alternative Medical Lab Testing Part 9: GynecologyFrom EverandComplementary and Alternative Medical Lab Testing Part 9: GynecologyNo ratings yet
- Antenatal Corticosteroid Therapy For Fetal Maturation - ACOGDocument21 pagesAntenatal Corticosteroid Therapy For Fetal Maturation - ACOGherryNo ratings yet
- Dr. Isngadi, Mkes, SpAn, KAO - Intrathecal Low Dose Levobupivacaine For ERACSDocument33 pagesDr. Isngadi, Mkes, SpAn, KAO - Intrathecal Low Dose Levobupivacaine For ERACSherryNo ratings yet
- Miscarriage or Early Pregnancy Loss-Diagnosis and ManagementDocument22 pagesMiscarriage or Early Pregnancy Loss-Diagnosis and ManagementherryNo ratings yet
- BNI Mobile Banking: Histori TransaksiDocument1 pageBNI Mobile Banking: Histori TransaksiherryNo ratings yet
- Pamorelin Larutan Injeksi Liofilisasi 11.25 MG Per 10 ML - Triptorelin - DKI1954400144B1 - 2020Document20 pagesPamorelin Larutan Injeksi Liofilisasi 11.25 MG Per 10 ML - Triptorelin - DKI1954400144B1 - 2020herryNo ratings yet
- BJSTR MS Id 003341Document4 pagesBJSTR MS Id 003341herryNo ratings yet
- Nihms 599061Document31 pagesNihms 599061herryNo ratings yet
- Estrogen Receptors and Endometriosis: Molecular SciencesDocument17 pagesEstrogen Receptors and Endometriosis: Molecular SciencesherryNo ratings yet
- Post Hysteroscopic Progesterone Hormone Therapy in The Treatment of Endometrial PolypsDocument5 pagesPost Hysteroscopic Progesterone Hormone Therapy in The Treatment of Endometrial PolypsherryNo ratings yet
- Diagnosis of Transposition of The Great ArteriesDocument7 pagesDiagnosis of Transposition of The Great ArteriesherryNo ratings yet
- NCCN: Continuing Education: Accreditation StatementsDocument26 pagesNCCN: Continuing Education: Accreditation StatementsherryNo ratings yet
- Culture-Confirmed Typhoid Fever and Pregnancy: K. Sulaiman, A.R. SarwariDocument5 pagesCulture-Confirmed Typhoid Fever and Pregnancy: K. Sulaiman, A.R. SarwariherryNo ratings yet
- Hemostasis Blok Hemato 2015Document15 pagesHemostasis Blok Hemato 2015herryNo ratings yet
- Bacterial VaginosisDocument4 pagesBacterial VaginosisherryNo ratings yet
- Hepatitis B in PregnancyDocument6 pagesHepatitis B in PregnancyherryNo ratings yet
- Care of The Pediatric Oncology PatientDocument67 pagesCare of The Pediatric Oncology PatientMaria Lourdes ReyesNo ratings yet
- Urinary CathetersDocument5 pagesUrinary CathetersJyoti Pariyar100% (1)
- Definitive Airway Management After Prehospital Supraglottic Rescue Airway in Pediatric Trauma PDFDocument5 pagesDefinitive Airway Management After Prehospital Supraglottic Rescue Airway in Pediatric Trauma PDFikm fkunissulaNo ratings yet
- Browerville Blade - 03/20/2014Document12 pagesBrowerville Blade - 03/20/2014bladepublishingNo ratings yet
- Health Literacy New Vital SignDocument6 pagesHealth Literacy New Vital Signapi-257281959No ratings yet
- Referat PeritonitisDocument18 pagesReferat PeritonitisWilliam Grandinata Soeseno100% (2)
- 14 Antibiotik Dan Antiseptik Untuk IskDocument40 pages14 Antibiotik Dan Antiseptik Untuk IskSintaKleoNo ratings yet
- Consent Transsphenoidal SurgeryDocument10 pagesConsent Transsphenoidal SurgeryAbhinav GuptaNo ratings yet
- Heart SoundsDocument17 pagesHeart SoundsAlfrin Antony100% (3)
- Introduction To Clinical Research: Drug DevelopmentDocument7 pagesIntroduction To Clinical Research: Drug Developmentapi-3810976No ratings yet
- Personal Development Plan Learner TemplateDocument2 pagesPersonal Development Plan Learner TemplateDhaval VaghaniNo ratings yet
- Laserasi PerineumDocument9 pagesLaserasi PerineumisnaNo ratings yet
- DAFTAR PUSTAKA Case BronkiolitisDocument2 pagesDAFTAR PUSTAKA Case BronkiolitisAnilNo ratings yet
- Bio TransplantDocument5 pagesBio TransplantYing_Hui99No ratings yet
- Viva Questions 1Document15 pagesViva Questions 1Reeba Mary PrinceNo ratings yet
- 2018.5.15 Insite Colo ContentDocument21 pages2018.5.15 Insite Colo ContentKatrinaBennettNo ratings yet
- Nasopharyngeal CarcinomaDocument25 pagesNasopharyngeal Carcinomananda surastyo100% (1)
- Alice in Wonderland SyndromeDocument6 pagesAlice in Wonderland SyndromeNilly NagyNo ratings yet
- Therapeutic Use of MagicDocument7 pagesTherapeutic Use of Magicapi-355156097No ratings yet
- Alcoholic Liver Disease HarrisonDocument3 pagesAlcoholic Liver Disease HarrisonJesly Charlies0% (1)
- VF-VT AlgorithmDocument10 pagesVF-VT AlgorithmPuskesmas Pinang JayaNo ratings yet
- Treating Discus Hernia Using A Self Developed Method - A New Technology Without Surgical InterventionDocument6 pagesTreating Discus Hernia Using A Self Developed Method - A New Technology Without Surgical InterventionlazarstosicNo ratings yet
- Exam ReviewDocument9 pagesExam ReviewjaxtradeNo ratings yet
- SJT Answers & RationaleDocument76 pagesSJT Answers & RationaleFarhan SakunNo ratings yet
- Anatomy Lecture Notes Unit 7 Circulatory System - The HeartDocument7 pagesAnatomy Lecture Notes Unit 7 Circulatory System - The Heartrapunzel777No ratings yet
- Membership of The Royal College of PhysiciansDocument3 pagesMembership of The Royal College of PhysiciansMatin Ahmad KhanNo ratings yet
- Operational Plan 2017 - 2020: East Metropolitan Health ServiceDocument12 pagesOperational Plan 2017 - 2020: East Metropolitan Health ServiceAhmed M. RafatNo ratings yet
- DIS IPD Ceftriaxone KonsulDocument28 pagesDIS IPD Ceftriaxone KonsulTriana MaulidyahNo ratings yet