Professional Documents
Culture Documents
Laser Scan Wound Care
Laser Scan Wound Care
Uploaded by
Khairani Putri UtamiCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Laser Scan Wound Care
Laser Scan Wound Care
Uploaded by
Khairani Putri UtamiCopyright:
Available Formats
CALIFORNIA HEALTHCARE FOUNDATION
April 2015
High Resolution: Laser Scans Improve
Wound Care at Kaiser Permanente
Nursing 2.0 Series
Put together, technology innovation and nursing can decrease costs, and lead to a better
patient experience and improved population
health. This series of case studies explores
different types of technology innovation being
deployed in the field of nursing. It features
members of the Innovation Learning Network,
a community of health care leaders and innovators focused on making health care better
through good design.
This case study about the use of laser scanning technology at Kaiser Permanente is part
of a series titled Nursing 2.0: How Technology
Innovations Are Enhancing Care, which can be
found at www.chcf.org/nursing-technology.
ILN
Case Study
THE
I N NOVAT I O N
L E A R N I NG
NE TWO R K
The Need for Instant
Information
urses work hard to access and share information quickly. Accurately capturing and
documenting patient information while
being efficient with time and fulfilling patients needs
are routine challenges. Old practices of storing information in three-ring binders, on hard-to-search
websites, or deep inside flow sheets in the electronic
medical record (EMR) system create impediments to
efficiency and quality. A study found that more than
30% of surgical nursing work is hunting and gathering information, people, and supplies.1
For wound care nurses, whose patients require
extensive documentation of wound appearance
and size, these challenges are pronounced. Health
care reform has heavily impacted how wound care
is delivered. The Centers for Medicare & Medicaid
Services (CMS) no longer reimburse for treatment
of wounds that develop while a patient is in the
1. Ann Hendrick et al., A 36-Hospital Time and Motion Study: How Do Medical Surgical Nurses Spend Their Time?,
The Permanente Journal 12, no. 3 (Summer 2008): 25-34, www.ncbi.nlm.nih.gov.
care patients. More than 100 patients participated in
the pilots using the device.
Immediate imaging. Laser
measurement technology
and a camera are used to
create 3-D images, which
accurately measure the
wound size and depth and
record a high-definition
image of the wound.
Image courtesy of ARANZ Medical.
hospital, requiring the hospital to shoulder this cost.
As a result, hospitals have instituted extensive skin
and wound checks when admitting a patient, which
has significantly increased the workload of the bedside nurse. Nurses specializing in wound care are
in short supply and are managing large panels of
patients.
Technology solutions for instant access to information and real-time data to better identify and
prioritize care and treat patients offer opportunities to dramatically improve the way nurses manage
information flow in the care delivery setting.
Wound Care Nurses,
Meet Laser Measuring
Kaiser Permanente, a large, integrated health care
system employing 49,000 nurses across seven
regions of the United States, recognized the need
to better document wound care. Between 2009 and
2014, Kaiser Permanente conducted several pilots
using the Silhouette, a wound-imaging, 3-D measurement and documentation system, to improve
accuracy and timeliness in assessment for wound
California HealthCare Foundation
The Silhouette, a product of ARANZ Medical, uses
laser measurement and a camera to create 3-D
images that accurately measure the wound size
and depth, and records a high-definition image of
the wound. Holding the device weighing about
as much as a large coffee cup above the wound,
the nurse lines up laser lines over the center of the
wound, clicks a button, and the data are uploaded to
a computer. The devices wound management software allows nurses and other clinicians to easily see
the data and images for a panel of patients.
Two Kaiser Permanente frontline wound care nurses
in Hawaii and a leader in Kaiser Permanentes
Innovation and Advanced Technology unit shared
their experiences with piloting the technology. Both
nurses are certified in WOC wound, ostomy (surgically created opening for waste discharge), and
continence care, a specialization that is in short
supply. One WOC nurse works in an inpatient setting, while the other works in an outpatient setting.
The technology offers a number of significant benefits and improvements for wound care and the nurses
who provide this care: greater precision and consistency in measurement, the availability of trending
data showing wound progression over time, and a
reduced need for in-person visits. Nurses involved
in the pilot also found the technology generally easy
to learn and easy to use. Somewhat unexpectedly,
they also noticed that the device had allure, observing other nurses, clinicians, and patients fascinated
by the laser camera and excited by the cool new
technology.
Improved Precision
and Teamwork
This technologys improvements to team communication and to documentation, an integral part of
wound assessment, are significant. Lynn Ikeda, RN,
family nurse practitioner and outpatient wound care
coordinator at Kaiser Permanente Hawaii, shared her
experience using the device:
Using photo documentation of wound care
is really telling more than words to tell
the provider and other nurses what to see. . . .
Something about [the device] that is even more
valuable and hopefully will be integrated into our
current EMR is the trending graph. You take the
photo, and it automatically computes the length,
width, and depth, and anything else that needs
to be captured by laser, as opposed to us manually measuring it.... I think this might help with
standardization.
Easy to use. Holding the
device weighing about
as much as a large coffee
cup above the wound,
the nurse lines up laser
lines over the center of the
wound, clicks a button, and
the data are uploaded to
the computer. In one click,
the wound is measured and
and image taken.
Image courtesy of ARANZ Medical.
Ikeda said that replacing the old tape measure
method of measuring wounds with a 3-D laser camera improves consistency of care between providers.
She also said that the ability for everyone on the care
team to see the progression of the wound over time
in the trending graph helps in their decisionmaking
process. Ikeda reported using the device on 7 or 8 of
the 30 to 40 patients she sees each morning in her
clinic during the pilot, and thinks this proportion will
grow as protocols are refined and use expands after
the pilot phase.
Benefits to Workflow
and Care Quality
Viki LaiHipp, RN, clinical coordinator of inpatient
wound care at Kaiser Permanente Hawaii, who sees
about 14 wound care patients a day, believes that
about 80% of those patients could be consulted by
telehealth technologies, rather than at an in-person
visit. She expects her workflow to greatly improve
when the 3-D camera is more widely used. As one
of the few nurses in the system with WOC nursing
certification, she could participate in more consultations by viewing images taken by other nurses and
providing treatment recommendations remotely. In
the future, with the accuracy and documentation
advantages this technology provides, patients will
not need to wait to see the WOC nurse specialist.
She explained:
There are a lot of consults we can do just through
pictures alone, and I dont have to be right there
to come up with recommendations. It opens up
a big door there. . . . A photograph, like they
say, speaks a thousand words. It can give you an
accurate description of what you would be looking at [during an in-person visit].
particularly younger, tech-savvy patients. LaiHipp
shared this:
Suzanne Furuya, MPH, MBA, innovation accelerator for Kaiser Permanentes Innovation Fund
for Technology, said that this technologys ability to reduce the need for in-person visits will help
nurses serve all patients better, especially Medicare
patients, who are often seen by nurses at home and
at outpatient facilities. The technology increases the
potential for telehealth visits.
Ive never had a patient refuse to let me use it....
I think its actually comforting to patients. Theyre
excited about the technology. Lets face it, everyone out there has heard about technology like
this, but not everyone has participated with it.
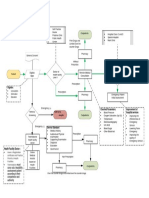
Summary of the Technologys
Wound Care Benefits
AA Precision
Patient Approval
Initial patient feedback on the device was also positive. Furuya noted that patients appreciated not
needing to have their wounds touched as frequently
as the tape measure method requires.
of 3-D laser measurements compared
to old method of using a tape measure, which
has more room for human error.
AA Greater
consistency in measurements across
users, including nurses.
AA Trend
Both Ikeda and LaiHipp said their patients were
generally intrigued and impressed by the device,
data available through a graph showing wound progression over time, which can
be uploaded to the EMR and seen by all team
members.
Central database. Communication, clinical
decisionmaking, and risk management are
facilitated through a database of patient
information. Care providers can see changes
over time and quickly understand the
wounds story.
Image courtesy of ARANZ Medical.
High Resolution: Laser Scans Improve Wound Care at Kaiser Permanente
AA Quality
of imaging and ability for the whole team
to view the wound in the same way at any time
in the EMR.
AA Easy
to learn, easy to use. The nurses noted that
hands-on training was key.
AA Reduced
need for in-person visits, makes remote
consultation more viable.
AA Sped-up
development of wound care and recov-
ery plan.
AA Positive
patient experience patients enjoyed
both not having to have their wounds touched
as frequently and feeling they were getting topnotch care with cutting-edge technology.
Accessible data. Synchronized via the Internet,
wound information becomes centrally available to
care teams, specialists, and administrators. It can
be integrated with the facilitys EMR.
Challenges and
Considerations
Four main challenges emerged during the pilots:
Challenge: EMR integration. The biggest challenge
the nurses faced in using the device during the pilots
was the lack of integration with their EMR system,
Kaiser Permanente HealthConnect. EMR integration
is a complex process that continues to be a challenge for many organizations. Although integration is
underway, nurses have had to perform several extra
steps to manually upload the photos and patient
information. Both Ikeda and LaiHipp said that this
process factors into their decision about whether to
use the device with a patient, as they dont always
have time to manually upload data. However, they
believe this issue will be alleviated when integration is complete. Furuya noted that how to integrate
with the EMR for example, during a successful
pilot versus later, when expansion plans are set
is an ongoing debate in the process of piloting and
spreading technology innovation.
How to overcome. Integration with KP Health
Connect is underway. As technology evolves and
devices become more connected, this integration
will be important for efficient and coordinated care.
Image courtesy of ARANZ Medical.
Challenge: The device is cumbersome. The nurses
noted that they found the device difficult to set up
and clean at first, and they wish it were wireless.
Ikeda said:
To tell you the truth, [the set up] weighs on my
decision of whether or not to use it because I have
California HealthCare Foundation
to think about it before I go in the room, and its
one more thing to prepare.
How to overcome. Establishing standards for use
are addressing workflow challenges presented by
the new technology. For example, LaiHipp said that
although figuring out how to clean the device was
initially a challenge, her team was able to develop
recommendations that have helped make the process easier. The results of pilot studies like this are
informing manufacturers about adaptations needed
to further the benefits of technological innovation in
practice.
Challenge: Not for all types of wounds. As they
use the device, the nurses consider which patients
and wound types are the best match for the technology. Ikeda said the device is great for patients with
new wounds, and for those with serious wounds that
may worsen over time, because she can track the
healing trend. The device does not capture tunneling wounds, which look like surface wounds but have
decay under the skin and muscle that is not visible.
How to overcome. Findings from the pilot and
feedback from the WOCN specialists will inform
protocols for use. These protocols will help nurses
know how to use the technology, which patients and
wounds are most appropriate for its use, and how to
ensure the data are shared among care team members. The pilot also informs how the device changes
workflows to better meet patient needs.
Challenge: User error leading to poor image
quality. Because the device involves a camera,
both Ikeda and LaiHipp said there were challenges
with making sure the lighting and positioning were
appropriate. LaiHipp said that the camera can sometimes pick up shadows and produce images of poor
quality. She thinks that these issues will be addressed
through staff training and improved technique with
more frequent use.
How to overcome. Developing training sessions on
how to use the equipment and recommendations for
camera positioning and lighting will address these
technical issues.
Looking Ahead and
Lessons Learned
Given the positive experience of the pilots, Kaiser
Permanente plans to spread use of the device
throughout the organization nationally. Further evaluation data, including more metrics, will be available
in late 2015 to inform this process. Overall, both
nurses who shared their experiences piloting the
device felt that most of the challenges they encountered will be addressed as the pilot is complete
and solutions integrated into the broader rollout.
Protocols and best-practice recommendations
will reduce challenges among other nurses using
the device for the first time. Nurses, patients, and
change management leaders all expressed enthusiasm to see use of the technology expand to more
settings.
Authors
Anne Boyd Rabkin, MPA
Consultant
Dan Weberg, PhD, RN
Director of Nursing Innovation
Innovation & Advanced Technology
Kaiser Permanante
Contributors
Suzanne Furuya, MPH, MBA
Innovation Accelerator
Innovation Fund for Technology
Innovation & Advanced Technology
Kaiser Permanente
Oakland, CA
Lynn Ikeda, FNP, CWOCN
Family Nurse Practitioner
Outpatient Wound Care Coordinator
Kaiser Permanente Hawaii
Viki LaiHipp, BSN, RN, CWOCN
Clinical Coordinator
Inpatient Wound Care
Kaiser Permanente Hawaii
About the Foundation
The California HealthCare Foundation works as a
catalyst to fulfill the promise of better health care
for all Californians. We support ideas and innovations that improve quality, increase efficiency, and
lower the costs of care. For more information, visit
www.chcf.org.
2015 California HealthCare Foundation
High Resolution: Laser Scans Improve Wound Care at Kaiser Permanente
You might also like
- Working at Height Rescue Mock Drill!Document36 pagesWorking at Height Rescue Mock Drill!S RNo ratings yet
- 26 Transfer To Hospital of Choice FormDocument2 pages26 Transfer To Hospital of Choice FormAina Haravata100% (1)
- Nursing Informatics 1 - ScribdDocument3 pagesNursing Informatics 1 - ScribdBianca BalmoresNo ratings yet
- VedantaDocument3 pagesVedantaSomesh Siddharth100% (1)
- Artificial Intelligence - Imaging's Next FrontierDocument8 pagesArtificial Intelligence - Imaging's Next FrontierEdgar DauzonNo ratings yet
- Technology and Nursing-1Document2 pagesTechnology and Nursing-1Today ViralNo ratings yet
- SsssssssssssssssssssssssDocument3 pagesSsssssssssssssssssssssssfatima ghaffarNo ratings yet
- Nursing Technologies - EditedDocument6 pagesNursing Technologies - EditedmelkyNo ratings yet
- Are Quiet Alarms, Real-Time Advice and AI The Future of Intensive Care?Document6 pagesAre Quiet Alarms, Real-Time Advice and AI The Future of Intensive Care?czeremar chanNo ratings yet
- Eng120-Week 14 - Final Essay - FinalDocument9 pagesEng120-Week 14 - Final Essay - Finalapi-626793332No ratings yet
- 2.health Care: Applications of Computer Vision in HealthcareDocument2 pages2.health Care: Applications of Computer Vision in HealthcareDivya Prakash SinghNo ratings yet
- Elevated XDocument11 pagesElevated Xkarthikvvvk2005No ratings yet
- Nursing Info Week 5 - Final ProjectDocument9 pagesNursing Info Week 5 - Final Projectapi-458308352No ratings yet
- Research Updates On Orthopedics 5 Years AgoDocument5 pagesResearch Updates On Orthopedics 5 Years AgoLYNDLY AGAGEONo ratings yet
- MOLINA, CHRISTINE JOY BSN 2B Nursing Informatics Assignment1Document3 pagesMOLINA, CHRISTINE JOY BSN 2B Nursing Informatics Assignment1Christine Joy MolinaNo ratings yet
- Technology (Computer) and Nursing WorkDocument6 pagesTechnology (Computer) and Nursing WorkEfjayNo ratings yet
- Final ProjectDocument14 pagesFinal Projectapi-298975236No ratings yet
- Week 6 Research Paper - Ravi TejaDocument5 pagesWeek 6 Research Paper - Ravi TejamymastertutorsNo ratings yet
- Radiation Safety PaperDocument4 pagesRadiation Safety Paperapi-530130628No ratings yet
- Advantages and DisadvantagesDocument2 pagesAdvantages and DisadvantagesJewel Berbano IINo ratings yet
- Roils 1Document4 pagesRoils 1api-574059920No ratings yet
- Continuous Quality Improvements and SafetyDocument3 pagesContinuous Quality Improvements and Safetyapi-518020510No ratings yet
- Lit ReviewDocument8 pagesLit Reviewapi-314668605No ratings yet
- Nursing InformaticsDocument8 pagesNursing InformaticsWac GunarathnaNo ratings yet
- TQM 02 Public and Government ServicesDocument3 pagesTQM 02 Public and Government ServicesCarmela Tuquib RebundasNo ratings yet
- Final Paper Nur410Document10 pagesFinal Paper Nur410api-598929897No ratings yet
- Final Paper Business Proposal Ar in Surgery Centers 12Document15 pagesFinal Paper Business Proposal Ar in Surgery Centers 12api-648597244No ratings yet
- Patient Treatment Interval Used in Forecast Algorithm and Solicitations in Hospital Queuing ManagementDocument5 pagesPatient Treatment Interval Used in Forecast Algorithm and Solicitations in Hospital Queuing Managementloly5788No ratings yet
- Oronce - Mod 1 EBJDocument6 pagesOronce - Mod 1 EBJCarlos OronceNo ratings yet
- Radiation Oncology Incident Learning System Case StudyDocument4 pagesRadiation Oncology Incident Learning System Case Studyapi-527613255No ratings yet
- Pneumonia Detection Using Machine Learning With X-Ray ImagesDocument5 pagesPneumonia Detection Using Machine Learning With X-Ray ImagesInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Project Control of Augmented RealityDocument25 pagesProject Control of Augmented RealityHarpreet singhNo ratings yet
- Anesthesia Information Mgmtsys 1014 pp346 351Document6 pagesAnesthesia Information Mgmtsys 1014 pp346 351Rafi ramdhanNo ratings yet
- Jennifer Bautista A.K.A. Minah Bautista A.K.A. Mildred Narvarte A.K.A. Malinda Sirue A.K.ADocument24 pagesJennifer Bautista A.K.A. Minah Bautista A.K.A. Mildred Narvarte A.K.A. Malinda Sirue A.K.AmalindaNo ratings yet
- MOLINA, CHRISTINE JOY BSN 2B Nursing Informatics Assignment1Document4 pagesMOLINA, CHRISTINE JOY BSN 2B Nursing Informatics Assignment1Christine Joy MolinaNo ratings yet
- Telemedicine For Healthcare CapabilitiesDocument12 pagesTelemedicine For Healthcare CapabilitiesSandiNo ratings yet
- Android App For Online OPD Appointment and Hospital Information SystemDocument8 pagesAndroid App For Online OPD Appointment and Hospital Information SystemIJRASETPublicationsNo ratings yet
- Use of Computers in Hospital and CommunityDocument7 pagesUse of Computers in Hospital and CommunityDelphy VargheseNo ratings yet
- Group 4 Nursing InformaticsDocument5 pagesGroup 4 Nursing InformaticsMj GalanoNo ratings yet
- Research Paper Nursing InformaticsDocument8 pagesResearch Paper Nursing Informaticsgz8bjzmj100% (1)
- Final Use Computer in Hospital and CommunityDocument20 pagesFinal Use Computer in Hospital and CommunityParul Pandey86% (7)
- Nursing Informatics NCM110Document89 pagesNursing Informatics NCM110Lacangan, Thea YvonneNo ratings yet
- Techs Effect in Nursing Education Nydia GriffithsDocument12 pagesTechs Effect in Nursing Education Nydia Griffithsapi-384815898No ratings yet
- Smart InhalerDocument4 pagesSmart InhalerHemanth RajuNo ratings yet
- AI in HealthcareDocument12 pagesAI in HealthcareDharshan KumarNo ratings yet
- Disease Prediction Using Machine Learning Algorithms KNN and CNNDocument7 pagesDisease Prediction Using Machine Learning Algorithms KNN and CNNIJRASETPublications100% (1)
- Case Study Year 1Document5 pagesCase Study Year 1Harshita ChoudharyNo ratings yet
- Radiation Safety Paper - 1Document3 pagesRadiation Safety Paper - 1api-270166579No ratings yet
- Effects of TechnologyDocument3 pagesEffects of TechnologymelaniebacayoNo ratings yet
- The Effects of Information Technology On Perioperative NursingDocument16 pagesThe Effects of Information Technology On Perioperative NursingBagus Adi PratamaNo ratings yet
- An Integrative Literature Review On Accuracy in Anesthesia Information Management SystemsDocument8 pagesAn Integrative Literature Review On Accuracy in Anesthesia Information Management SystemseldcahvkgNo ratings yet
- The Future of Medical Imaging: White PaperDocument7 pagesThe Future of Medical Imaging: White PaperSukhmander SinghNo ratings yet
- Artificial IntelligenceDocument5 pagesArtificial IntelligenceKariuki KimaniNo ratings yet
- Nursing InformaticsDocument6 pagesNursing InformaticsChancy Jenine H. ValerioNo ratings yet
- Patient Safety and TechnologyDocument5 pagesPatient Safety and TechnologyAditya Toga100% (1)
- Rising To The Challenge Xtelligent Media PDFDocument7 pagesRising To The Challenge Xtelligent Media PDFshyamchepurNo ratings yet
- Radiation SafetyDocument3 pagesRadiation Safetyapi-484027891No ratings yet
- Radiation Safety PaperDocument4 pagesRadiation Safety Paperapi-632529930No ratings yet
- Informatics ProjectDocument7 pagesInformatics ProjectShannon TerrellNo ratings yet
- Clinical Epidemiology and Global Health: Mohd Javaid, Abid HaleemDocument6 pagesClinical Epidemiology and Global Health: Mohd Javaid, Abid HaleemFelipe RuizNo ratings yet
- Nursing Informatics of Efficiencies and Outcomes of The Patients - Edited PDFDocument5 pagesNursing Informatics of Efficiencies and Outcomes of The Patients - Edited PDFCamille Joy BaliliNo ratings yet
- ResearchDocument3 pagesResearchJehira OcampoNo ratings yet
- Health informatics: Improving patient careFrom EverandHealth informatics: Improving patient careBCS, The Chartered Institute for ITRating: 3 out of 5 stars3/5 (1)
- 739-Article Text-5753-1-10-20211229Document11 pages739-Article Text-5753-1-10-20211229Ziana UtariNo ratings yet
- CDP Interim G12Document134 pagesCDP Interim G12Muhammadh MANo ratings yet
- Accredited Overseas Healthcare Facilities (FWHS) Updated April 2022Document15 pagesAccredited Overseas Healthcare Facilities (FWHS) Updated April 2022Furqan ArchNo ratings yet
- Malpractice 4DDocument45 pagesMalpractice 4DthiaraNo ratings yet
- India 2Document132 pagesIndia 2Bala KrishnanNo ratings yet
- Amarillo Globe Times - July 30, 1956 - Page 1Document1 pageAmarillo Globe Times - July 30, 1956 - Page 1Jamie BurchNo ratings yet
- Reading Comprehension 2 "Giving Direction"Document7 pagesReading Comprehension 2 "Giving Direction"Ardi KendariNo ratings yet
- My ResumeDocument4 pagesMy ResumeJal-Fem AngelesNo ratings yet
- Business Proposal For Sathya Sai HospitalDocument3 pagesBusiness Proposal For Sathya Sai HospitalTriveni ChopraNo ratings yet
- List of Accredited Hospitals - Clinics-1Document70 pagesList of Accredited Hospitals - Clinics-1Jobel LucenaNo ratings yet
- Opscom AugustDocument19 pagesOpscom AugustMichelle Motin ToledoNo ratings yet
- Resume 0619Document2 pagesResume 0619api-512508582No ratings yet
- NotificationDocument4 pagesNotificationArtiNo ratings yet
- Medical Negligence in Hong KongDocument320 pagesMedical Negligence in Hong KongErvin TanNo ratings yet
- Level 1 Hospital - FGL GRP 2Document6 pagesLevel 1 Hospital - FGL GRP 2KRIZIA CORRINE CAINGCOY SAN PEDRONo ratings yet
- Amang Rodriguez For ADB PDFDocument67 pagesAmang Rodriguez For ADB PDFKristine Presbitero100% (1)
- Judith de Guzman: Mariano Marcos State UniversityDocument2 pagesJudith de Guzman: Mariano Marcos State UniversitymacNo ratings yet
- Seemandhra Pres Secs 2014-15Document20 pagesSeemandhra Pres Secs 2014-15Rajeev VenegallaNo ratings yet
- June 2023 Radiologic Technologists and X-Ray Technologists Special Professional Licensure Examinations ResultsDocument9 pagesJune 2023 Radiologic Technologists and X-Ray Technologists Special Professional Licensure Examinations ResultsRapplerNo ratings yet
- My Explanation W.r.t.claim No.28702508Document2 pagesMy Explanation W.r.t.claim No.28702508Vivek ShambharkarNo ratings yet
- Sunita Mam Sam Mam Report March 2023Document6 pagesSunita Mam Sam Mam Report March 2023SEEMA KUMARINo ratings yet
- Sec SCH Historical InvestigationDocument11 pagesSec SCH Historical Investigationreiko.potterheadNo ratings yet
- Hvac Design of HospitalDocument9 pagesHvac Design of HospitalSaurav Verma0% (1)
- HOSPITAL AS A SOCIAL SYSTEMDocument8 pagesHOSPITAL AS A SOCIAL SYSTEMdanielnwuzor35No ratings yet
- Neopuff Product Benefit Brochure PM 185047316 BDocument1 pageNeopuff Product Benefit Brochure PM 185047316 BDeya PrastikaNo ratings yet
- 2021 Alur Remote Medical ConsultationDocument1 page2021 Alur Remote Medical ConsultationRahmad FahrezaNo ratings yet