Professional Documents
Culture Documents
Article WMC004489
Article WMC004489
Uploaded by
dyahayueCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Article WMC004489
Article WMC004489
Uploaded by
dyahayueCopyright:
Available Formats
Article ID: WMC004489
ISSN 2046-1690
Candida albicans: Colonization, role and effects of
this opportunistic pathogen on orthodontic
appliances
Peer review status:
No
Corresponding Author:
Dr. Francesca Muggiano,
Dentist, Dipartimento di Scienze Odontostomatologiche e Maxillo Facciali, Universita' degli Studi di Roma - Italy
Submitting Author:
Dr. Francesca Muggiano,
Dentist, Dipartimento di Scienze Odontostomatologiche e Maxillo Facciali, Universita' degli Studi di Roma - Italy
Other Authors:
Dr. Andrea Quaranta,
Dentist, Dipartimento di Scienze Odontostomatologiche e Maxillo Facciali, Universita degli Studi di Roma - Italy
Dr. Michele Previati,
Dentist, Azienda Sanitaria Regione Molise, Campobasso, Italy - Italy
Article ID: WMC004489
Article Type: Review articles
Submitted on:02-Jan-2014, 06:07:08 PM GMT
Published on: 03-Jan-2014, 04:57:49 AM GMT
Article URL: http://www.webmedcentral.com/article_view/4489
Subject Categories:ORTHODONTICS
Keywords:Candida albicans, orthodontics, orthodontic appliances, yeast, opportunistic pathogen, candidiasis,
oral flora, antifungal agents, IgA, fungi
How to cite the article:Muggiano F, Quaranta A, Previati M. Candida albicans: Colonization, role and effects of
this opportunistic pathogen on orthodontic appliances. WebmedCentral ORTHODONTICS
2014;5(1):WMC004489
Copyright: This is an open-access article distributed under the terms of the Creative Commons Attribution
License(CC-BY), which permits unrestricted use, distribution, and reproduction in any medium, provided the
original author and source are credited.
Source(s) of Funding:
No source of funding.
Competing Interests:
No competing interests.
WebmedCentral > Review articles
Page 1 of 8
WMC004489
Downloaded from http://www.webmedcentral.com on 03-Jan-2014, 04:57:49 AM
Candida albicans: Colonization, role and effects of
this opportunistic pathogen on orthodontic
appliances
Author(s): Muggiano F, Quaranta A, Previati M
Abstract
Candida albicans is a commensal yeast that is
normally present in the oral cavity of the population.
This opportunistic pathogen is frequently isolated from
the human mouth but its presence in the oral cavity is
not indicative of disease. Colonization of the oral
cavity by Candida albicans involves the acquisition
and maintenance of a stable yeast population.
Micro-organisms are continually being removed from
the oral cavity by host clearance mechanisms, and so,
in order to survive and inhabit this eco-system,
Candida albicans cells have to adhere and replicate.
Orthodontic and other oral appliances seem to favor
candidal presence.
The purpose of this paper is to review the literature,
with specific attention to colonization, intra-oral density
of the candidal organisms and Candida carriage status
in orthodontic patients during treatment.
Introduction
Candida albicans is a commensal yeast and its
presence in the oral cavity is not indicative of disease.
In fact, many individuals has Candida albicans as a
minor component of their oral flora, and they have no
clinical symptoms. Only a proportion of the population
is colonized by Candida albicans, and only a subset of
these individuals develops candidiasis.
Discussion
This yeast is normally present in small numbers in the
oral flora: it is an opportunistic pathogen present in
about 50-60% of the healthy human population, and
becomes pathogenic when the host immune defence
is undermined (for example in HIV infection).Therefore,
oral candidiasis results from yeast overgrowth and
penetration of the oral tissues when the host's physical
and immunological defenses have been undermined.
Tissue invasion may be assisted by secreted
hydrolytic enzymes, hyphal formation, and contact
WebmedCentral > Review articles
sensing. While these and other phenotypic
characteristics may endow certain Candida species or
strains with a competitive advantage in the oral cavity,
it is the host's immune competence that ultimately
determines whether clearance, colonization, or
candidiasis occurs.
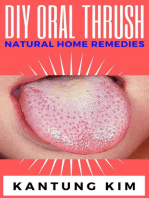
Oral candidiasis presents clinically in many forms and
this reflects the ability of the yeast to colonize different
oral surfaces and the variety of factors which
predispose the host to Candida colonization and
subsequent infection. Oral presentations of candidiasis
vary from the large white plaques of
pseudomembraneous candidiasis on the tongue and
buccal mucosa to the palatal erythematous lesions of
chronic atrophic candidiasis, and to angular cheilitis on
the labial commissures (Samaranayake, 1990; Scully
et al., 1994; Shay et al., 1997).
Several studies have reported that predisposing
factors (such as mouth breathing and HIV-infection)
may increase the variability of Candida species in the
oral cavity: therefore, the health of an individual is a
predisposing factor for its colonization. The oral cavity
presents many niches for Candida albicans
colonization, and the yeast is able to adhere to a
plethora of ligands. A large number of sites in the oral
cavity can be colonized; in healthy individuals,
Candida albicans is most commonly isolated from the
midline of the middle and posterior thirds of the tongue,
the cheek, or the palatal mucosa (Arendorf and Walker,
1979, 1980; Borromeo et al., 1992).
Colonization of the oral cavity by this yeast can be
defined as the acquisition and maintenance of a stable
population of Candida albicans cells which does not
give rise to clinical disease. It depends on the rate of
yeast cells enter the oral cavity, their growth, and
removal of cells from the mouth by swallowing and
oral hygiene.
Micro-organisms are continually being removed from
the oral cavity by host clearance mechanisms, and so,
in order to survive and inhabit this eco-system,
Candida albicans cells have to adhere and replicate.
The following is an example scheme:
Rate of removal >rate of acquisition and growth
clearance.
Page 2 of 8
WMC004489
Downloaded from http://www.webmedcentral.com on 03-Jan-2014, 04:57:49 AM
Rate of removal = rate of acquisition and growth
colonization.
Rate of removal <rate of acquisition and growth (and
there is tissue damage)candidiasis.
In the table I are listed several factors that influence
candidiasis and colonization of the oral cavity by
Candida albicans.
1. Acquisition: in humans, Candida albicans
preferentially colonizes mucosal surfaces, and the
intestinal tract is believed to be a major reservoir for
infection (Odds, 1988; Cole et al., 1996). Candida
albicans can colonize practically any site in the
gastrointestinal tract, from the oral cavity to the rectum
and peri-anal tissues, allowing anal-oral inoculation to
occur (Soll et al., 1991). This yeast survives better on
moist surfaces than dry inanimate objects, but if the
degree of contamination is high enough, viable cells
will remain on dry surfaces for at least 24 hours.
Candida species can enter in the oral cavity by manual
inoculation, saliva transfer, or contaminated food and
drink.
2. Maintaning an oral Candida population: the entry of
Candida cells into the oral cavity is not sufficient for
colonization, but they must be stably maintained.
Since the oral cavity is a continuous-flow environment,
yeast cells will be washed out by saliva and swallowed
unless they adhere and replicate. Adhesion is
therefore of critical importance in colonization and it is
mediated between moieties of the Candida cell wall
and host surfaces.
3. Adherence to oral surfaces: Candida albicans can
adheres in a number of surfaces in the oral cavity
(buccal epithelial cells, inert polymers of dental
prostheses, teeth, and other oral micro-organisms).
Colonization may contribute to the deterioration of the
oral devices. This yeast showed a great adherence to
acrylic and adherence is increased on rough acrylic
and silicone rubber surfaces compared with smooth
surfaces (Verran and Maryan, 1997). The acrylic base
for dentures supported less adherence of C. albicans
than tissue conditioners and a soft liner (Okita et al.,
1991).
Many factors may influence the process of adherence
to oral epithelial cells (Tabel II).
The effects of these components on the adherence of
Candida albicans differ: some of them increase the
adhesion capacity, whereas others show inhibitory
activity. Biasoli et al. observed a correlation between
the capacity for yeast to adhere and its ability to
colonize mucosal surfaces. Candida presents the
highest values of adherence to oral epithelial cells
relative to other Candida species. Boshet al. verified
WebmedCentral > Review articles
that moderate stress may affect the process of
microbial colonization and the adherence of this
yeastto epithelial cells by altering the secretory activity
of salivary glands. Because adherence is an important
virulence factor in Candida, the inhibition of this
process is an important strategy in the prevention of
oral candidosis. Itsantigens, host proteins, antifungal
agents and antibodies have been used to inhibit
Candida albicansadherence to host cells. IgA seems
to play an important role by causing fungal
aggregation and preventing the adherence to mucosa
or oral surfaces.
4. Growth: In order to maintain Candida populations in
the oral cavity, cells must grow and multiply at a rate
at least equal to that of clearance. Anymetabolic
activity that helps this yeast acquire carbon or nitrogen
will aid its growth and survival in the oral cavity.
Competition with other oral micro-organisms
for nutrients, such as glucose, affects the growth rate
of Candida cells. It is recognized that antibiotic
treatment, which reduces the number of oral bacteria,
is a predisposing factor for oral candidiasis
(Samaranayake, 1990). Oral bacteria are present in
most oral sites at concentrations much higher than
Candida albicans, and so the Candida cells must
compete with them for adhesion sites and nutrients,
and be exposed to bacterial toxins and byproducts.
5. Evading host clearance mechanisms: immune
system defects are a major risk factor for candidiasis.
Innate defenses include the epithelial barrier and
anti-candidal compounds in saliva (such as lysozyme,
histatins, lactoferrin, and calprotectin). Acquired
immunity includes the production of immunoglobulins
and, if tissues are penetrated, the involvement
of macrophages and polymorphonuclear leukocytes.
The major immunoglobulin in saliva is secretory IgA.
As already said, the primary etiological agent of oral
candidiasis is the yeast Candida albicans; however,
other species that cause disease less commonly
include Candida tropicalis, Candida glabrata, Candida
krusei, Candida parapsilosis, Candida guilliermondii
and Candida dubliniensis.
Among the many factors that contribute to the higher
prevalence of Candida albicansin the oral cavity are its
excellent ability to adhere and the presence of many
cell receptors, which confer versatility and resistance
to removal by the fluids that bathe these surfaces.
Adhesion and colonization of the oral cavity by
Candida albicansis an initial step in candidosis. The
pathogenicity of Candidaspp. is due to enzyme
production, tissue invasion, and their capacity to
adhere to oral mucosa.
Page 3 of 8
WMC004489
Downloaded from http://www.webmedcentral.com on 03-Jan-2014, 04:57:49 AM
Orthodontic and other oral appliances seem to favor
candidal presence, so we will analyze the relationship
between this yeast and orthodontic patients. The
presence of orthodontic and other oral appliances
seems to alter the oral ecological environment. Hence,
these appliances may tip the balance to favour the
existence of Candida species.Biofilms on removable
orthodontic appliances act as reservoir of
microorganisms, capable of modifying the
environmental condition of oral cavity and are difficult
to be removed with routine hygiene measures.
Topaloglu-Ak et al. (2011) showed that mutans and
Lactobacillus sp. counts increased significantly 6
months after the insertion of fixed/removable
orthodontic appliances in the oral cavity. A significant
increase for Candida albicans presence was noted
after 3 months compared with baseline for fixed
appliances. Long-term utilization of orthodontic
appliances may have a negative effect on microbial
flora and increase the risk of new carious lesions and
periodontal problems.
Silva et al. (2013) compared the presence of
Candidaspecies in saliva and the levels of antiCandida albicansIgA in children with or without
orthodontic appliances. The results showed that
Candida albicansis the species most frequently
isolated from the oral cavities of patients in both
groups, followed by Candida tropicalis. No correlation
was observed between the level of
anti-Candidaalbicans IgA in saliva and the presence of
this yeastor its adherence to epithelial cells. In this
study, the quantity of IgA was low in children of both
the experimental group (who were users of removable
orthodontic appliances for at least 6 months) and the
control group (who were not users of any orthodontic
appliances). Salivary IgA generally increases with age
because the secretory immunological mechanism
develops simultaneously with the humoral immune
system. In patients with dental prosthesis or
removable orthodontic devices, salivary IgA reduces
the adherence of Candida albicansto polystyrene.
Their results indicate that anti- Candida albicansIgA is
not the most important factor to determine
Candidacarrier status.
Hence, Candida colonization is a consequence
of orthodontic treatment and can lead to oral
candidosis as a complication of removable appliance
treatment. The installation of metal devices leads to an
increase in the salivary concentration of metal ions
and in the growth of salivary Candida spp. Ronsani et
al. (2011) examined the relationship between released
metal ions (Ni++, Fe+++, Cr+++, Co++ or a mixture of
these metal ions) and Candida virulence, in order to
WebmedCentral > Review articles
evaluate whether metal ions affect fungal virulence.
The results revealed that all ions, except Co++,
caused increases in biofilm biomass. Their results
indicate that metal ions released during the
degradation of orthodontic appliances can modulate
virulence factors in C. albicans biofilms.
Therefore, during orthodontic treatment, it is important
to minimize colonization to prevent active infection that
could consequently interfere with treatment. Hygiene
is the most important factor in managing colonization.
In their study, Decelis et al. (2012) tested the efficacy
of NitrAdine to reduce Candida and they concluded
that it may reduce the Candida burden in maxillary
removable appliances. Carvalhinho et al. (2012)
analyzed the susceptibilities to antifungal agents
(fluconazole, econazole, miconazole and ketoconazole,
amphotericin B and nystatin), mouth rinses and
essential oils of patient's mouth with fixed
orthodontic appliances. The results showed that all
isolates tested were susceptible to amphotericin B,
nystatin and fluconazole; one isolate was resistant to
econazole (2.5%) and the other to ketoconazole
(2.5%). Econazole and ketoconazole had the highest
percentages of susceptible dose dependent (SDD), 55
and 95%, respectively. The study of mouth rinses
showed a high variability of efficacy against C.
albicans. The results showed that the isolates
susceptibility to essential oils differed. The profile
activity was: cinnamon > laurel > mint > eucalyptus
> rosemary > lemon > myrrh > tangerine. The
susceptibility of econazole-SDD isolates to cinnamon
and lemon was higher than those of the econazole-S
yeasts. In contrast, econazole-SDD isolates were less
affected by laurel than econazole-S counterparts.
Results and Conclusions
The limited amount of literature demonstrated that the
density of Candida increases; the most
common Candida species isolated in the orthodontic
patients is Candida albicans and that there seems to
be a direct relationship between the presence of a
removable appliance, Candida and low salivary pH
levels. It is important to emphasize that no healthy
patients developed Candida infection from the
orthodontic appliances. However, there seems to be a
trend that some non-Candida carriers converted
to Candida carriers following the insertion of the
appliances by unknown mechanism. This may indicate
a more cautious approach when providing orthodontic
treatments to immunocompromised children
concerning the possible increased risk of candidal
Page 4 of 8
WMC004489
Downloaded from http://www.webmedcentral.com on 03-Jan-2014, 04:57:49 AM
infection.
More opportunistic bacteria and fungi are detected in
orthodontic patients than in non-orthodontic patients.
Opportunistic bacteria adhere to saliva-coated metallic
brackets to the same degree as oral streptococci. The
isolation frequencies of opportunistic bacteria and
fungi increase during orthodonti treatment, suggesting
the importance of paying special attention to oral
hygiene in orthodontic patients to prevent periodontal
disease and the aggravation of systemic disease in
immunocompromised conditions.
Moreover, the use of dental devices significantly
increased the prevalence of yeasts in periodontal
pockets in patients presenting gingivitis.
In conclusion, orthodontic appliances may favor the
adherence of Candida to epithelial cells but do not
influence the presence of these yeasts in saliva, and
the levels of anti-Candida albicans IgA do not correlate
with yeast adherence or presence of this yeast in the
oral cavity.
Patients should be recalled within short time intervals
to be motivated for oral hygiene during their
orthodontic therapy.
References
1. Samaranayake LP. Essential microbiology for
dentistry, 2nd edn. Churchill Livingstone, Edimburg.ed.
2002.
2. Valletta, Matarasso, Vignogna; Malattie
odontostomatologiche ed. 2005.
3. Harrison. Principi di medicina interna. The
McGraw-Hill Companies ed. 2007.
4. Amerio PL, Bernengo MG, Calvieri S, Chimenti S,
Pippione M, Aric M, Aste N, Borroni G, Leigheb G,
Micali G, Nunzi E, Offidani AM, Tulli A. Dermatologia e
venereologia. Minerva Medica. Ed. 2009.
5. Roversi. Manuale di diagnostica e terapia. Merqurio
editore. ed. 2012.
6. Petti S, Barbato E, Simonetti D'Arca A. Effect of
orthodontic therapy with fixed and removable
appliances on oral microbiota: a six-month longitudinal
study. Microbiologica1997;20:55-62.
7. Sturtevant 1, Calderone R. Candida albicans
adhesins: biochemical aspects and virulence. Rev
Iberoam Micol. 1997;14:90-97.
8. Olsen I. Oral adhesion of yeasts. Acta Odontol
Scand. 1990 Feb;48(1):45-53.
9. Koga-Ito CY, Unterkircher CS, Watanabe H, Martins
CA, Vidotto V, Jorge AO. Caries risk tests and salivary
levels of immunoglobulins to Streptococcus mutans
and Candida albicans in monthbreathing patients.
WebmedCentral > Review articles
Caries Res. 2003 Jan-Feb;37(1):38-43.
10. Holmes AR, Bandara BM, Cannon RD. Saliva
promotes Candida albicans adherence to human
epithelial cells. J Dent Res. 2002 Jan;81(1):28-32.
11. Brito GN, Inocncio AC, Querido SM, Jorge AO,
Koga-Ito CY. In vitro antifungal susceptibility of
Candida spp. Oral isolates from HIV-positive patients
and control individuals. Braz Oral Res. 2011
Jan-Feb;25(1):28-33.
12. Gonalves e Silva CR, Melo KE, Leo MV, Ruis R,
Jorge AO. Relationship between Candida in vaginal
and oral mucosae andsalivary IgA. Rev Bras Ginecol
Obstet. 2008 Jun; 30(6): 300-5.
13. Silva CR, Oliveira LD, Leao MV, Jorge AO.
Candida spp. Adherence to oral epithelial cells and
levels of IgA in children with orthodontic appliances.
Braz Oral Res. 2013 Dec 2:0.
14. Cannon RD, Chaffin WL. Oral Colonization By
Candida Albicans. Crit Rev Oral Biol Med.
1999;10(3):359-383.
15. Pathak AK, Sharma DS. Biofilm associated
microorganisms on removable oral orthodontic
appliances in children in the mixed dentition. J Clin
Pediatr Dent. 2013 Spring;37(3):335-9.
16. Hibino K, Wong RW, Hagg U,Samaranayake LF.
The effects of Orthodonticappliances on Candidain the
human mouth. Int J Paediatr Dent. 2009
Sep;19(5):301-8.
17. Decelis S, Camilleri S, Zahra EV, Scerri E, De
Wever B. The effect of NitrAdine on the Candida levels
of maxillary removable appliances. Quintessence
Int.2012 Mar;43(3):239-45.
18. Carvalhinho S, Costa AM, Coelho AC, Martins E,
Samoaio A. Susceptibilities of Candida albicans mouth
isolates to antifungal agents, essentials oils and mouth
rinses. Mycopathologia. 2012 Jul;174(1):69-76.
19. Wellmer A, Bernhardt H. Adherence on buccal
epithelial cells and germ tube formation in the
continuous flow culture of clinical Candida albicans
isolates. Mycoses 1997;40:363-368.
20. Topaloglu-Ak A, Ertugrul F, Eden E, Ates M, Bulut
H. Effect of orthodontic appliances on oral
microbiota--6 month follow-up. J Clin Pediatr Dent.
2011 Summer;35(4):433-6.
21. Verran J, Maryan CJ. Retention of Candida
albicans on acrylic resin and silicone of different
surface topography. I Prosthet Dent. 1997;77:535-539.
22. Ronsani MM, Mores Rymovicz AU, Meira TM,
Trinidade Grgio AM, Guariza Filho O, Tanaka OM,
Ribeiro Rosa EA. Microb Pathog. Virulence
modulation of Candida albicans biofilms by metal ions
commonly released from orthodontic devices. 2011
Dec;51(6):421-5.
23. Cannon RD, Holmes AR, Mason AB, Monk BC.
Page 5 of 8
WMC004489
Downloaded from http://www.webmedcentral.com on 03-Jan-2014, 04:57:49 AM
Oral Candida: clearance, colonization, or candidiasis?
Dent Res.1995 May;74(5):1152-61.
24. Kitada K, de Toledo A, Oho T. Increase in
detectable opportunistic bacteria in the oral cavity of
orthodontic patients. Int J Dent Hyg. 2009
May;7(2):121-5.
25. Biasoli MS, Tosello ME, Magaro HM. Adherence of
Candida strains isolated from the human
gastrointestinal
tract.
Mycoses.
2002
Dec;45(11-12):465-9.
26. Biasoli MS, Tosello ME, Magaro HM. Adherence of
Candida strains isolated from the human
gastrointestinal
tract.
Mycoses.
2002
Dec;45(11-12):465-9.
27. Bosch JA, Turkenburg M, Nazmi K, Veerman EC,
de Geus EJ, Nieuw Amerongen AV. Stress as a
determinant of salivamediated adherence and
coadherence of oral and nonoral microorganisms.
Psychosom Med. 2003 Jul-Aug;65(4):604-12.
28. Jewtuchowicz VM, Brusca MI, Mujica MT, Gliosca
LA, Finquelievich JL, Lovannitti CA, Rosa AC.
Subgingival distribution of yeast and their antifungal
susceptibility in immunocompetent subjects with and
without dental devices. Acta Odontol
Latinoam.2007;20(1):17-22.
29. Davies TM, Shaw WC, Wothington HV, Addy M,
Dummer P, Kingdon A. The effect of orthodontic
treatment on plaque and gingivitis. Am J Orthod
Dentofacial Orthop 1991;99:155-61.
WebmedCentral > Review articles
Page 6 of 8
WMC004489
Downloaded from http://www.webmedcentral.com on 03-Jan-2014, 04:57:49 AM
Illustrations
Illustration 1
Table I: Factors that influence candidiasis and colonization of the oral cavity.
Candidiasis
Colonization
Tissue colonized
Acquisition (entry of cells into the oral cavity)
Virulence factors expressed by the Candida cells
Attachment and growth of cells
Host response
Penetration of tissues
Removal of cells from he oral cavity
WebmedCentral > Review articles
Page 7 of 8
WMC004489
Downloaded from http://www.webmedcentral.com on 03-Jan-2014, 04:57:49 AM
Illustration 2
Table II: Factors that influenced the adherence of Candida to oral epithelial cells
Yeast-related factors
Host-related factors
expression of adhesion proteins
sexual hormones
presence of germinative tubes
presence of fibrin and fibrinogen
production of extracellular polymers and enzymes
presence of salivary compounds (including mucine,
salivary proteins, and secretory IgA)
WebmedCentral > Review articles
Page 8 of 8
You might also like
- Medical Excuse From Jury Duty TemplateDocument2 pagesMedical Excuse From Jury Duty TemplateBalkiss TouzriNo ratings yet
- ASSH Manual of Hand Surgery PDFDocument653 pagesASSH Manual of Hand Surgery PDFChis Alexandra100% (1)
- Drug-Induced Oral Candidiasis - A Case ReportDocument4 pagesDrug-Induced Oral Candidiasis - A Case ReportFajarRahmantiyoNo ratings yet
- Weight Loss Book For Weight AssingmentDocument16 pagesWeight Loss Book For Weight AssingmentBob Cook0% (5)
- Hematology Control: Manufactured For: Boule Medical AB Stockholm, Sweden E-MailDocument1 pageHematology Control: Manufactured For: Boule Medical AB Stockholm, Sweden E-MailTarunNo ratings yet
- Kins 205 - Sport Psychologist ResumeDocument5 pagesKins 205 - Sport Psychologist Resumeapi-356744486No ratings yet
- Candida-Associated Denture StomatitisDocument5 pagesCandida-Associated Denture StomatitisAyik DarkerThan BlackNo ratings yet
- Review Article Candida Species Revealed by High-Throughput TechnologiesDocument6 pagesReview Article Candida Species Revealed by High-Throughput TechnologiesNovia HartantiNo ratings yet
- Host's Immunity and Candida Species Associated With Denture Stomatitis. A Narrative ReviewDocument21 pagesHost's Immunity and Candida Species Associated With Denture Stomatitis. A Narrative ReviewCatalina AguayoNo ratings yet
- Oral Candidiasis - ReviewDocument9 pagesOral Candidiasis - ReviewAdhelia Galuh PrmtsrNo ratings yet
- Chapter 18interactions Between Candida Species and Bacteria in Mixed InfectionsDocument13 pagesChapter 18interactions Between Candida Species and Bacteria in Mixed InfectionsRisca ArianiNo ratings yet
- Egyptian: Denture Biofilm and Dentureassociated Stomatitis, A Literature ReviewDocument13 pagesEgyptian: Denture Biofilm and Dentureassociated Stomatitis, A Literature ReviewShankar arumugamNo ratings yet
- Chap 2Document13 pagesChap 2Aamna HanifNo ratings yet
- Micro Bio LogoDocument52 pagesMicro Bio LogoBayan HamedNo ratings yet
- Shweta PPT ThesisDocument10 pagesShweta PPT ThesisAKSHAY WAKTENo ratings yet
- Candidiasis - Red and White Manifestations in The Oral CavityDocument8 pagesCandidiasis - Red and White Manifestations in The Oral CavityFajarRahmantiyoNo ratings yet
- ReferenceDocument163 pagesReferenceAjay IyerNo ratings yet
- Fmicb 06 01391 PDFDocument10 pagesFmicb 06 01391 PDFChellaPremitaNo ratings yet
- Periodontology 2000 - 2022 - Kitamoto - Periodontal Connection With Intestinal Inflammation Microbiological andDocument12 pagesPeriodontology 2000 - 2022 - Kitamoto - Periodontal Connection With Intestinal Inflammation Microbiological andSekarSukomasajiNo ratings yet
- Management and Treatment of Fungal Infection in The Oral CavityDocument4 pagesManagement and Treatment of Fungal Infection in The Oral CavityKIU PUBLICATION AND EXTENSIONNo ratings yet
- Health Notions, Volume 4 Number 2 (February 2020) Issn 2580-4936Document5 pagesHealth Notions, Volume 4 Number 2 (February 2020) Issn 2580-4936Kamado NezukoNo ratings yet
- Health Notions, Volume 4 Number 2 (February 2020) Issn 2580-4936Document5 pagesHealth Notions, Volume 4 Number 2 (February 2020) Issn 2580-4936Kamado NezukoNo ratings yet
- Jurnal 3 (Biofilm) Fixed PDFDocument5 pagesJurnal 3 (Biofilm) Fixed PDFNovia SillaNo ratings yet
- Role of Oral Microbiota in Preserving Health and Disease ManagementDocument17 pagesRole of Oral Microbiota in Preserving Health and Disease ManagementAthenaeum Scientific PublishersNo ratings yet
- The Open Dentistry Journal: Root Canal Irrigation: Chemical Agents and Plant Extracts AgainstDocument12 pagesThe Open Dentistry Journal: Root Canal Irrigation: Chemical Agents and Plant Extracts Againstaulia lubisNo ratings yet
- Review Article: Isolation and Identification of From The Oral CavityDocument7 pagesReview Article: Isolation and Identification of From The Oral CavitysitisalwiahNo ratings yet
- CandidiasisDocument6 pagesCandidiasismirayanti astariNo ratings yet
- Ganoderma Lucidum Against Candida AlbicansDocument8 pagesGanoderma Lucidum Against Candida AlbicansCsikós IlonaNo ratings yet
- Sodio OralDocument6 pagesSodio OralBoris QuelcaNo ratings yet
- Oral Health in America A Report of The Surgeon General (Prosiding)Document4 pagesOral Health in America A Report of The Surgeon General (Prosiding)Zkdlin SpaceNo ratings yet
- Resolviendo La Etiologia de La Caries Dental PDFDocument7 pagesResolviendo La Etiologia de La Caries Dental PDFYesenia Jopia OrellanaNo ratings yet
- Occurrence of Candida Albicans in Periodontitis PDFDocument7 pagesOccurrence of Candida Albicans in Periodontitis PDFAbdoNo ratings yet
- (844 857) V10N5CTDocument14 pages(844 857) V10N5CTChristine Elaine Batusin IlaganNo ratings yet
- Dental Plaque and CalculusDocument32 pagesDental Plaque and Calculus蔡長家No ratings yet
- Jurnal OM 2Document6 pagesJurnal OM 2Reiza PrabandanaNo ratings yet
- Candidiasis Red and WhiteDocument8 pagesCandidiasis Red and WhitejnrrszrnvmNo ratings yet
- Oral CandidiasisDocument28 pagesOral CandidiasisjnrrszrnvmNo ratings yet
- Chakraborti-Das2020 Article DysbiosisOfOralMicrobiotaAndItDocument12 pagesChakraborti-Das2020 Article DysbiosisOfOralMicrobiotaAndItraunak81No ratings yet
- Normal Oral Microbial FloraDocument17 pagesNormal Oral Microbial FloraNeeraj Rajendra MehtaNo ratings yet
- Candidiasis Red and White Manifestations in The Oral CavityDocument8 pagesCandidiasis Red and White Manifestations in The Oral CavityDaniela Juárez CastellanosNo ratings yet
- Polymicrobial Candida Biofilms: Friends and Foe in The Oral CavityDocument14 pagesPolymicrobial Candida Biofilms: Friends and Foe in The Oral CavityYerly Ramirez MuñozNo ratings yet
- Understanding The Role of Candida Abicans in The Development of Cancer Cells, Its Progression Mechanism, Possible Preventive Measures and TreatmentDocument13 pagesUnderstanding The Role of Candida Abicans in The Development of Cancer Cells, Its Progression Mechanism, Possible Preventive Measures and TreatmentInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Opportunistic Yeast InfectionDocument14 pagesOpportunistic Yeast Infectionelsa_imamNo ratings yet
- Microbes and Unsuccessful Endo TreatmentDocument9 pagesMicrobes and Unsuccessful Endo TreatmentkariNo ratings yet
- 10.2478 - Aoj 2022 0006Document12 pages10.2478 - Aoj 2022 0006Cindy SuNo ratings yet
- Santosh 2017Document22 pagesSantosh 2017Srii WulaandariiNo ratings yet
- Apical Periodontitis - Virulence Factors of Enterococcus: Faecalis and Candida AlbicansDocument5 pagesApical Periodontitis - Virulence Factors of Enterococcus: Faecalis and Candida AlbicansEfika ChoirunnisaNo ratings yet
- Oral Candidiasis: Etiology and PathogenesisDocument5 pagesOral Candidiasis: Etiology and PathogenesisNovita Indah PratiwiNo ratings yet
- 446 P Singh - 0620188 PDFDocument9 pages446 P Singh - 0620188 PDFVibhor Kumar JainNo ratings yet
- Review Article: What Makes Oral Candidiasis Recurrent Infection? A Clinical ViewDocument6 pagesReview Article: What Makes Oral Candidiasis Recurrent Infection? A Clinical ViewAF KoasNo ratings yet
- Resistance To Antibiotics Used in Treating Gum Infections: A Cross-Sectional Study Based On Gum Disease Patients in Syria in The Period of Covid 19Document8 pagesResistance To Antibiotics Used in Treating Gum Infections: A Cross-Sectional Study Based On Gum Disease Patients in Syria in The Period of Covid 19International Journal of Innovative Science and Research TechnologyNo ratings yet
- Articulo 1 MicroDocument5 pagesArticulo 1 MicroSusanaNo ratings yet
- b.8 Oral CandidiasisDocument14 pagesb.8 Oral Candidiasisbryamjbriceno100% (1)
- Pathophysiology of Oral CandidiasisDocument11 pagesPathophysiology of Oral CandidiasisAldyTriawanNo ratings yet
- 204-Article Text-650-2-10-20200909Document9 pages204-Article Text-650-2-10-20200909Ridha AprillahNo ratings yet
- The Oral Microbiome and Human Health: Yoshihisa Yamashita and Toru TakeshitaDocument6 pagesThe Oral Microbiome and Human Health: Yoshihisa Yamashita and Toru TakeshitaLedy OrduñaNo ratings yet
- Assignment Hdb10503 Basic MicrobiologyDocument4 pagesAssignment Hdb10503 Basic MicrobiologyNida RidzuanNo ratings yet
- Fungal Diseases of The Oral MucosaDocument5 pagesFungal Diseases of The Oral MucosaManar AlsoltanNo ratings yet
- Angular Chelitis in Complete Dentures: Sharmila.R, N.P MuralidharanDocument2 pagesAngular Chelitis in Complete Dentures: Sharmila.R, N.P MuralidharanindahdwitasariNo ratings yet
- Seminario Biologia 2Document11 pagesSeminario Biologia 2Daniela Rizo AlvarezNo ratings yet
- Prevalence of Oral Pathogens in Oral Cavities, Dental Implants, Fixed Bridges Among The People in South IndiaDocument7 pagesPrevalence of Oral Pathogens in Oral Cavities, Dental Implants, Fixed Bridges Among The People in South IndiaSubash Arunagiri (RA1911009010004)No ratings yet
- Caries Vaccine: Guided By: Presented byDocument5 pagesCaries Vaccine: Guided By: Presented byharishgnrNo ratings yet
- Endodontic MicrobiologyDocument11 pagesEndodontic MicrobiologydigdouwNo ratings yet
- Cancer Case StudyDocument15 pagesCancer Case StudyRobin HaliliNo ratings yet
- Management of A Growing Skeletal Class II Patient: A Case ReportDocument7 pagesManagement of A Growing Skeletal Class II Patient: A Case ReportCuan JuiceNo ratings yet
- Basic Principles of Wound ManagementDocument26 pagesBasic Principles of Wound ManagementAlina Nica GurgutaNo ratings yet
- Psychopharmacology NewestDocument43 pagesPsychopharmacology NewestRegina PunNo ratings yet
- Adapalene 0.1% (Adaferin Cream)Document6 pagesAdapalene 0.1% (Adaferin Cream)ddandan_2No ratings yet
- ResumeDocument2 pagesResumeapi-422782277No ratings yet
- Aaos 2013Document152 pagesAaos 2013Yusufa ArdyNo ratings yet
- Venipuncture WorksheetDocument5 pagesVenipuncture WorksheetAmy YmaNo ratings yet
- Choroid Plexus CystsDocument2 pagesChoroid Plexus Cystsvalerius83No ratings yet
- CTRI RA Ay Med Guru Snigdha Guna of Kapha - Clin Higwadi Curna - Sunthyadi Kvath in Ama VataDocument3 pagesCTRI RA Ay Med Guru Snigdha Guna of Kapha - Clin Higwadi Curna - Sunthyadi Kvath in Ama VataMSKCNo ratings yet
- Argumentative Essay Final DraftDocument9 pagesArgumentative Essay Final Draftcchurc13No ratings yet
- Dr. R. W. Bernard - Science Discovers The Psychological Value of ContinenceDocument31 pagesDr. R. W. Bernard - Science Discovers The Psychological Value of ContinenceOliveros2012No ratings yet
- 2016 43 1 - 1 PDFDocument16 pages2016 43 1 - 1 PDFMSshy RPhNo ratings yet
- Polo Labs, IVY Hospital, Sector Polo Labs, IVY Hospital, Sector-71, MohaliDocument1 pagePolo Labs, IVY Hospital, Sector Polo Labs, IVY Hospital, Sector-71, MohaliRaman ChandiNo ratings yet
- Carpal TunnelDocument10 pagesCarpal TunnelasimulhaqNo ratings yet
- Client Who Is BlindDocument17 pagesClient Who Is BlindArasi MuniandyNo ratings yet
- Final Adaptation Sick Young Infant Module PDFDocument76 pagesFinal Adaptation Sick Young Infant Module PDFAngelica AmandoNo ratings yet
- Approach To ShockDocument28 pagesApproach To ShockSyasya ZulkiffliNo ratings yet
- Ranikhet Disease-2008-09 PDFDocument7 pagesRanikhet Disease-2008-09 PDFnamgeshNo ratings yet
- Jurnal CuaDocument13 pagesJurnal CuaErma YuniartiNo ratings yet
- Health N: Edrelyn A. Venturanza, RNDocument32 pagesHealth N: Edrelyn A. Venturanza, RNJamesBuensalidoDellavaNo ratings yet
- 3D Printing Technology The Impetus Concept in The Drug DeliveryDocument4 pages3D Printing Technology The Impetus Concept in The Drug DeliveryEditor IJTSRDNo ratings yet
- Mull Issue 1 2010Document8 pagesMull Issue 1 2010jspradeepscribdNo ratings yet
- CEBM Levels of Evidence Introduction 2.1Document3 pagesCEBM Levels of Evidence Introduction 2.1Anida SaNiia BecKzNo ratings yet
- Citizen's Charter For PSWDODocument2 pagesCitizen's Charter For PSWDOAlejandro CoronaNo ratings yet