Professional Documents
Culture Documents
Editorial The Future of Sensors and Instrumentation For Human Breath Analysis
Editorial The Future of Sensors and Instrumentation For Human Breath Analysis
Uploaded by
Lukman MahdiCopyright:
Available Formats
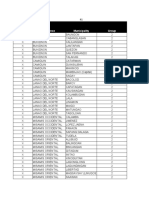
You might also like
- Bot CookbookDocument149 pagesBot Cookbookdaniel monteroNo ratings yet
- Jurnal ForensikDocument15 pagesJurnal ForensikZoehelmy HusenNo ratings yet
- Gangaram Rate List PDFDocument315 pagesGangaram Rate List PDFAmit Kumar GuptaNo ratings yet
- Production of Lime: Chemical Engineering DepartmentDocument17 pagesProduction of Lime: Chemical Engineering DepartmentDon Aries EidosNo ratings yet
- Human Exhaled Breath Analysis: CME ReviewDocument6 pagesHuman Exhaled Breath Analysis: CME ReviewJulieta SolariNo ratings yet
- 10 1 1 232 716 PDFDocument17 pages10 1 1 232 716 PDFSounak BoseNo ratings yet
- Exhaled Breath Analysis in The Differentiation of Pneumonia From Acute Pulmonary OedemaDocument7 pagesExhaled Breath Analysis in The Differentiation of Pneumonia From Acute Pulmonary OedemaAkka RakaNo ratings yet
- Jurnal BiomedikDocument10 pagesJurnal BiomedikneaNo ratings yet
- E Nose:E TongueDocument6 pagesE Nose:E TongueKilian DuchesneNo ratings yet
- Breath Analysis: Trends in Techniques and Clinical ApplicationsDocument6 pagesBreath Analysis: Trends in Techniques and Clinical ApplicationsDina MansourNo ratings yet
- Biomarkers in COPD ExacerbationsDocument12 pagesBiomarkers in COPD ExacerbationsLinto JohnNo ratings yet
- Application of Fecal Volatile Organic Compound Analysis in Clinical Practice: Current State and Future PerspectivesDocument20 pagesApplication of Fecal Volatile Organic Compound Analysis in Clinical Practice: Current State and Future PerspectiveslecongdangNo ratings yet
- Sauca (M) I6157820 BSC Thesis 2020Document33 pagesSauca (M) I6157820 BSC Thesis 2020marius saucaNo ratings yet
- 2004 Clinica Chimica ActaDocument15 pages2004 Clinica Chimica ActaDina MansourNo ratings yet
- Exhaled Breath PaperDocument16 pagesExhaled Breath PaperCristhian Manuel Durán AcevedoNo ratings yet
- Unit 7 Blood PressureDocument11 pagesUnit 7 Blood PressureQ O R Y A N INo ratings yet
- Biomarker Copd PDFDocument35 pagesBiomarker Copd PDFManoj KumarNo ratings yet
- Analysis of Volatile Organic Compounds From Deep Airway in The Lung Through Intubation SamplingDocument12 pagesAnalysis of Volatile Organic Compounds From Deep Airway in The Lung Through Intubation SamplingmoubarginNo ratings yet
- Unit 8Document11 pagesUnit 8FatmawatiNo ratings yet
- Exhaled Breath Analysis For Lung CancerDocument12 pagesExhaled Breath Analysis For Lung CancerIkaPKNo ratings yet
- Respiration - Electronic NoseDocument13 pagesRespiration - Electronic NoseCristhian Manuel Durán AcevedoNo ratings yet
- Optoelectronic PlethysmographyDocument15 pagesOptoelectronic PlethysmographygothicmetalspiritNo ratings yet
- Myeloperoxidase and Protein Oxidation in The Airways of Young Children With Cystic FibrosisDocument7 pagesMyeloperoxidase and Protein Oxidation in The Airways of Young Children With Cystic FibrosisMichael StudiofourteenohnineNo ratings yet
- Pulse Oximetry Instrumental Alternative in The Clinical Evaluation by The Bed For The DysphagiaDocument8 pagesPulse Oximetry Instrumental Alternative in The Clinical Evaluation by The Bed For The DysphagiaGabriel MaldonadoNo ratings yet
- Lung Function and Peak Oxygen Uptake in Chronic Obstructive Pulmonary Disease Phenotypes With and Without EmphysemaDocument12 pagesLung Function and Peak Oxygen Uptake in Chronic Obstructive Pulmonary Disease Phenotypes With and Without EmphysemaAndreea MoalesNo ratings yet
- 2006 129 1344-1348 Christopher E. Brightling: Clinical Applications of Induced SputumDocument7 pages2006 129 1344-1348 Christopher E. Brightling: Clinical Applications of Induced Sputumjoal510No ratings yet
- Sensors: Novel Isoprene Sensor For A Flu Virus Breath MonitorDocument7 pagesSensors: Novel Isoprene Sensor For A Flu Virus Breath MonitorJuanGabrielVillamizarNo ratings yet
- Asthma Enose IOT ReportDocument55 pagesAsthma Enose IOT ReportASHVIK JNo ratings yet
- Pulmonary Biomarkers in COPD: Peter J. BarnesDocument6 pagesPulmonary Biomarkers in COPD: Peter J. Barnesmike_helplineNo ratings yet
- Oxygen Therapy For Chronic Obstructive Pulmonary Disease PatientsDocument9 pagesOxygen Therapy For Chronic Obstructive Pulmonary Disease PatientsshielphiNo ratings yet
- 2015 - Gaspard - Aerosol Sampling Using An Electrostatic Precipitator Integrated With A Microfluidic Interface - PaperDocument9 pages2015 - Gaspard - Aerosol Sampling Using An Electrostatic Precipitator Integrated With A Microfluidic Interface - PaperNgô Đình NhânNo ratings yet
- Cyto Lungtumorbook1Document104 pagesCyto Lungtumorbook1ixNo ratings yet
- Lung Atlas 2014 CPRDocument187 pagesLung Atlas 2014 CPRelessar2001100% (1)
- Bronchoalveolar Lavage As A Diagnostic T PDFDocument15 pagesBronchoalveolar Lavage As A Diagnostic T PDFAndy Rusgi KribowNo ratings yet
- Waypa G. and Schumacker P. O2 Sensing in Hypoxic Pulmonary Vasoconstriction The Mitochondrial Door Re-Opens. Respir. Physiol. Neurobiol. (2002)Document11 pagesWaypa G. and Schumacker P. O2 Sensing in Hypoxic Pulmonary Vasoconstriction The Mitochondrial Door Re-Opens. Respir. Physiol. Neurobiol. (2002)benjabmbNo ratings yet
- Ijms 13 13894Document17 pagesIjms 13 13894osama mosaNo ratings yet
- Indice AclaramientoDocument4 pagesIndice AclaramientoPaola Vicenta Chalco MorenoNo ratings yet
- Aiomt 106Document10 pagesAiomt 106AyestinNo ratings yet
- Symptomatic Patients Without Airflow Obstruction2016Document4 pagesSymptomatic Patients Without Airflow Obstruction2016Ella EllaNo ratings yet
- Bal 3BDocument29 pagesBal 3BLian Marie ViñasNo ratings yet
- Case Analysis PneumoniaDocument5 pagesCase Analysis PneumoniaLorence RamosNo ratings yet
- Natural History and Mechanisms of COPD: Invited Review Series: Copd: New HorizonsDocument24 pagesNatural History and Mechanisms of COPD: Invited Review Series: Copd: New HorizonsSebastian RamirezNo ratings yet
- Pulmonary Functional Imaging: Basics and Clinical ApplicationsFrom EverandPulmonary Functional Imaging: Basics and Clinical ApplicationsYoshiharu OhnoNo ratings yet
- An Adverse Outcome Pathway For Lung Surfactant Functio - 2021 - Current ResearchDocument12 pagesAn Adverse Outcome Pathway For Lung Surfactant Functio - 2021 - Current ResearchAadityarajsinh GohilNo ratings yet
- Proteome Profiling of Lung Tissues in ChronicDocument8 pagesProteome Profiling of Lung Tissues in ChronicAndreea MoalesNo ratings yet
- MocoyN Acetilcisteinaene2018Document9 pagesMocoyN Acetilcisteinaene2018mariela carlo tancaraNo ratings yet
- Frontiers in Respiratory Physiology - Grand ChallengeDocument2 pagesFrontiers in Respiratory Physiology - Grand ChallengeAlfi OktafaniNo ratings yet
- 2019 - Chronic Obstructive Pulmonary Disease andDocument6 pages2019 - Chronic Obstructive Pulmonary Disease andAndreea MoalesNo ratings yet
- Lung Sounds in Bronchial Asthma: Review ArticleDocument11 pagesLung Sounds in Bronchial Asthma: Review ArticleSophia RoseNo ratings yet
- Bronkiolitis AkutDocument10 pagesBronkiolitis AkutNamira Firdha KNo ratings yet
- Journal of Neurochemistry - 2011 - Gacki ReDocument12 pagesJournal of Neurochemistry - 2011 - Gacki ReantoniorNo ratings yet
- Research Paper On OxygenDocument5 pagesResearch Paper On Oxygenegya6qzc100% (1)
- Time To Throw AwayDocument10 pagesTime To Throw AwayPuteri Indah Achmad HasyimNo ratings yet
- 1 s2.0 S0304416511001358 MainDocument8 pages1 s2.0 S0304416511001358 MainjackashcaNo ratings yet
- Markers of Pulmonary Oxygen Toxicity in Hyperbaric Oxygen Therapy Using Exhaled Breath AnalysisDocument9 pagesMarkers of Pulmonary Oxygen Toxicity in Hyperbaric Oxygen Therapy Using Exhaled Breath AnalysisThijs WingelaarNo ratings yet
- Chest: The Role of CT Scanning in Multidimensional Phenotyping of COPDDocument9 pagesChest: The Role of CT Scanning in Multidimensional Phenotyping of COPDAtika Indah SariNo ratings yet
- Cigarette Smoke Promotes Dendritic Cell Accumulation in COPD A Lung Tissue Research Consortium StudyDocument13 pagesCigarette Smoke Promotes Dendritic Cell Accumulation in COPD A Lung Tissue Research Consortium StudyArry SetyowatiNo ratings yet
- FullDocument13 pagesFullgregor alexanderNo ratings yet
- American Thoracic Society DocumentsDocument19 pagesAmerican Thoracic Society DocumentsPhanNo ratings yet
- 744 FullDocument5 pages744 FullBogdan NechitaNo ratings yet
- PATH Recommendations - EditedDocument2 pagesPATH Recommendations - EditedJohnNo ratings yet
- 1jebp PDFDocument14 pages1jebp PDFekarusningwatiNo ratings yet
- MocoyN Acetilcisteinaene2018Document9 pagesMocoyN Acetilcisteinaene2018Alejandra JimenezNo ratings yet
- Alhena Eng Rev06Document7 pagesAlhena Eng Rev06Steven BrownNo ratings yet
- Indomethacin From Anti-Inflammatory To Anticancer AgentDocument26 pagesIndomethacin From Anti-Inflammatory To Anticancer AgentYaqeen Alhaqq F. GhaziNo ratings yet
- Brochure - Ancient Rock Salt, Gourmet Salts PDFDocument16 pagesBrochure - Ancient Rock Salt, Gourmet Salts PDFLaraib AliNo ratings yet
- GCU ELM-305 Topic 5 Discussion Question ResponsesDocument3 pagesGCU ELM-305 Topic 5 Discussion Question ResponsesKristin HensleyNo ratings yet
- Lab 5 ImineDocument10 pagesLab 5 ImineCheng FuNo ratings yet
- Director Manager Payroll CPP in Seattle WA Resume Michael HoernerDocument1 pageDirector Manager Payroll CPP in Seattle WA Resume Michael HoernerMichaelHoerner2No ratings yet
- Leisure in My Life - ReportDocument16 pagesLeisure in My Life - ReportnuriNo ratings yet
- Learning Disabilities OtDocument48 pagesLearning Disabilities OtReeva de SaNo ratings yet
- Full Download Test Bank For Personal Nutrition 7th Edition Boyle PDF Full ChapterDocument36 pagesFull Download Test Bank For Personal Nutrition 7th Edition Boyle PDF Full Chaptertetrazosubaud0q5f100% (22)
- Actuator Ari PremioDocument12 pagesActuator Ari Premioluthfie.swaciptaNo ratings yet
- 4-Point Action Plan by Esperanza and Brian CabralDocument6 pages4-Point Action Plan by Esperanza and Brian CabralRapplerNo ratings yet
- A 26 V 14 N 02Document6 pagesA 26 V 14 N 02faustinopateiro3497No ratings yet
- IA Findings ProcurementDocument2 pagesIA Findings ProcurementSreekanth PCNo ratings yet
- Rotonivo: Series RN 3000 / 6000Document34 pagesRotonivo: Series RN 3000 / 6000Strato VariusNo ratings yet
- Platts Nucleonics Week 19 July2012Document15 pagesPlatts Nucleonics Week 19 July2012Jovi Savitri Eka PutriNo ratings yet
- Relative Pronouns and TenseseDocument4 pagesRelative Pronouns and TenseseKarla TorresNo ratings yet
- Flojet Beverage CatDocument24 pagesFlojet Beverage CatRacil EzzedineNo ratings yet
- 2021-2023 FO X RFR Tracker - KC NCDDP AFDocument147 pages2021-2023 FO X RFR Tracker - KC NCDDP AFJestoni Gonzales TortolaNo ratings yet
- Playground Antonyms PDFDocument2 pagesPlayground Antonyms PDFChayne RodilNo ratings yet
- Pre-Cast Concrete SpecialistsDocument24 pagesPre-Cast Concrete SpecialistsSilas MangwendeNo ratings yet
- Azidus Laboratories - BA BE Capabilities Slide Deck - Feb 2019 PDFDocument35 pagesAzidus Laboratories - BA BE Capabilities Slide Deck - Feb 2019 PDFDeepakNo ratings yet
- Jurnal 3Document6 pagesJurnal 3Zaimatul HamdiyahNo ratings yet
- Building Maintenance ChecklistDocument5 pagesBuilding Maintenance ChecklistcajaroNo ratings yet
- Task 1 - Three Phase (Ø) Electrical Installation Direct On Line (Dol) Forward Motor ControlDocument4 pagesTask 1 - Three Phase (Ø) Electrical Installation Direct On Line (Dol) Forward Motor Controlmoganraj8munusamyNo ratings yet
- Electrical Safety HAE EM EPS GDCC ES PDFDocument17 pagesElectrical Safety HAE EM EPS GDCC ES PDFkhleifat_613891No ratings yet
- Sustainability 14 07022 v2Document22 pagesSustainability 14 07022 v2Osman DenizNo ratings yet
- Valleylab Ft10 Energy Platform Users GuideDocument174 pagesValleylab Ft10 Energy Platform Users Guideavanteb ajamNo ratings yet
Editorial The Future of Sensors and Instrumentation For Human Breath Analysis
Editorial The Future of Sensors and Instrumentation For Human Breath Analysis
Uploaded by
Lukman MahdiOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Editorial The Future of Sensors and Instrumentation For Human Breath Analysis
Editorial The Future of Sensors and Instrumentation For Human Breath Analysis
Uploaded by
Lukman MahdiCopyright:
Available Formats
IEEE SENSORS JOURNAL, VOL. 10, NO.
1, JANUARY 2010
Editorial
The Future of Sensors and Instrumentation for
Human Breath Analysis
HE previous three decades have provided a wealth of information on the identity of chemical compounds that are
exhaled in human breath. Also during this time pioneering advances in the analytical assessment of chemical constituents and
metabolites exhaled in human breath have helped to push forward the research field. While the physiological relevance and
presence of many components in breath is not yet fully elucidated, it is evident that the composition of exhaled breath (EB)
and breath condensate (EBC) provide a complex mirror image
of the biochemical processes within the body, which may be correlated to the physiological status, disease progression, or therapeutic progress of a patient.
Much progress has been made on determining the identities
of many volatile and nonvolatile breath biomarkers using
mainly bench-top traditional analytical equipment. Although
work still continues and is still urgently needed in the biomarker
area, more recent engineering research efforts on this topic area
have concentrated on advancing compact analytical techniques,
in particular, novel sensor concepts enabling monitoring of
known biomarker constituents in EB at appropriate concentration levels.
It is anticipated that in the coming decade a wealth of technologies will emerge as commercial products, making clinical
breath analysis tests and personalized breath monitors a reality.
However, success in these areas will largely depend on how
well the adapted sensing concepts will meet a range of engineering, design, and analytical challenges that are specific to
breath analyte detection. This Special Topics Issue provides an
overview of currently explored sensing techniques and methods
that are being researched and developed in academic and industrial settings, often at various technology maturity levels. The
purpose of this Special Issue is to represent a sampling of research approaches from within this dynamic development area,
and to also educate readers as to the demanding challenges of
this emerging research area.
I. HISTORY OF BREATH ANALYSIS
There is historical anecdotal evidence that both ancient
Greek and Chinese medical texts mention the idea that unique
Digital Object Identifier 10.1109/JSEN.2009.2035675
breath smells can frequently be associated with physiological
disorders or disease. It was not, however, until the modern
era that researchers have approached the concept of breath
analysis with scientific rigor to understand the problem. In the
late 1790s, Lavoisier and Laplace renewed interest in studying
respiration and breath constituents, and their work resulted
in an increasing range of instrumentation for studying the
function of the lungs and breath mechanics. This renaissance
of medical diagnostics allowed for more functional physical
lung diagnostics utilizing percussion and auscultation (e.g.,
listening with a stethoscope) later that decade. With the development of the first spirometer by John Hutchinson in the
mid-1800s, instrumental techniques for studying breath and
lung function established a continuous presence in clinical
diagnostics. This has subsequently been followed by a wide
variety of technological improvements enabling quantitative
analysis of respiratory activity, as well as operation outside a
traditional hospital environment.
Before the introduction of X-ray techniques, prevalent community-acquired respiratory diseases such as tuberculosis were
increasingly diagnosed utilizing breath function tests largely
based on spirometric techniques. During the 1900s, this simple
test was then augmented with methods for the analysis of blood
gas (work by Severinghaus), and lung and thoracic pressure
(work by DuBois).
While physical measurement techniques have contributed
early on to the diagnosis of diseases affecting or relating to the
respiratory system, it was not until the early 1970s when Linus
Pauling pioneered the analytical assessment of breath components by gas chromatographic (GC) analysis of exhaled air. He
identified a wide range of blood-borne volatile organic compounds (VOCs) that were exhaled via the blood/air interface
in the lungs [1]. Historically, the analysis of breath is probably
among the oldest diagnostic techniques in medical practice
utilizing disease-specific odors for assigning a physiological
status to a patient. However, the molecular complexity of breath
has rendered the quantitative analysis of breath constituents
up
and metabolites present at nanomolar to picomolar (
mol/L) concentration levels an analytical challenge
to
requiring modern instrumental techniques with adequate sensitivity and discriminatory power at a molecular level.
1530-437X/$26.00 2009 IEEE
IEEE SENSORS JOURNAL, VOL. 10, NO. 1, JANUARY 2010
II. THE COMPLEXITY OF BREATH
Breath is composed of a highly complex molecular matrix,
which contains both abundant chemical mixtures as well as
trace constituents. The abundant compounds, such as nitrogen,
oxygen, water, and carbon dioxide are prevalent at very high
concentration levels, while the nearly 3500 volatile organic
compounds exist at extremely low concentrations [2]. Related
studies utilizing measures in the late 1980s and 1990s have
estimated that approximately 50% of the identified VOCs are
of endogenous origin with approximately 200 VOCs detected
in average breath samples, although further instrumentation
development in the last decade has lengthened the list of compounds that are reported in the literature.
From the biological side of the problem, a further complication of representative breath analysis for diagnostic purposes
results from the within-patient variations and patient-to-patient
variations. Across diverse studies, the most prevalent endogenous VOCs appear to be isoprene, which is a by-product of
cholesterol synthesis during the conversion of mevalonate to
mevanolate-5-pyrophosphate and isopentenyl pyrophosphate,
and acetone, which is a metabolic component occurring in
blood, urine, and human breath resulting from endogenous
fatty acid oxidation. In addition, small molecules including,
e.g., ammonia, methane, or carbon monoxide add to the complexity of the molecular breath signature, which also spans a
wide range of molecular weights and dimensions next to the
molecular functionality.
Clearly, constituent signatures characteristic for certain disease pathologies, therapeutic progress, or diagnosis have to be
quantitatively discriminated against a molecularly complex and
widely varying background composed of endogenous and exogenous compounds. Given these considerations, it appears unlikely that a single constituent may emerge as a sufficiently indicative diagnostic marker for a disease. Hence, it is fair to hypothesize that similar to gene regulation entire regulatory patterns of biomarkers in EB may have the potential serving as reliable diagnostic panels for diagnosing and tracing diseases and
their progression.
As a consequence, the breath matrix and its variability
present a significant analytical challenge that requires quantitatively tracing patterns of molecular signatures within entire
biomarker panels with sufficient reliability providing a solid
basis for clinical diagnosis. Therefore, the successful implementation of diagnostic devices analyzing EB requires that
the characteristic changes of such biomarker patterns are unambiguously assigned to certain pathological or physiological
conditions, and/or an associated therapeutic progress.
III. CHALLENGES IN BREATH ANALYSIS
Next to appropriate sampling techniques, the analysis of
breath requires either separation, selective preconcentration,
or direct analysis with analytical techniques providing appropriate molecular selectivity. Frequently, diagnostically
relevant biomarker concentration levels of indicative markers
are estimated to range from the (parts-per-billion) ppb down to
parts-per-trillion (ppt) concentration levels, which are difficult
to address with most conventional instrumental techniques.
Hence, breath sample collection and/or preconcentration are
frequently mandatory prior to analysis. However, EB is not
inherently a homogeneous sample, and each breath consists
of approximately 150 mL of air from the upper airways in
an area with only gas exchange with blood (also known as
the dead volume) and approximately 350 mL of air from
the blood-vessel rich tissue of the lungs (also known as the
alveaolar volume). This second fraction of EB has extensive
gas exchange with the blood, and by directly sampling this
fraction into an analyzer or onto a preconcentrator, one can
achieve superior analytical results.
With few exceptions such as alcohol tests, nitric oxide (NO)
analysis, the absence of clinical breath
tests, and isotopic
testsand even less so personalized breath monitorsmay be
attributed to the absence of reliable, compact, and rapidly responding analytical devices and sensing techniques capable of
addressing diagnostic biomarker panels within this complex matrix with sufficient molecular selectivity and sensitivity in real
time. Currently, analysis of EB is predominantly performed by
GC in combination with mass spectrometric (GC/MS) detection for separation and identification of trace constituents, which
may be considered the gold standard in breath research [3]. Consequently, an increased adoption of breath analysis in routine
clinical environments, and the future introduction of personalized breath monitors requires the accelerated development of
advanced portable sensing system for EB analysis.
IV. ARE NOVEL SENSORS THE SOLUTION?
The evident progress in chemical sensor and biosensor technology during the recent decades has clearly established sensors as a supporting pillar of modern analytical chemistry and
instrumental analysis next to the separation sciences, mass spectrometry, optical spectroscopies, and electrochemical analysis.
Coincidentally, medical analysis and clinical diagnostics are increasingly adopting novel concepts developed in these areas
for advancing analytical platforms used in the health sciences
toward enhanced reliability and throughput. The most evident
convergence between medical needs and technical solutions is
currently observed in the area of personalized medicine, which
demands for advanced miniaturized analyzers providing reliable
diagnostic data outside a hospital environment.
An important prerequisite for personalized diagnostics is the
noninvasive access to an excreted matrix of the human body
that reflects a disease state or progression in molecular detail.
In contrast to saliva and urine, EB appears to be the matrix
with the highest diagnostic value, which is most conveniently
EDITORIALTHE FUTURE OF SENSORS AND INSTRUMENTATION FOR HUMAN BREATH ANALYSIS
accessed, sampled, and analyzed within any environment.
Hence, the combination of adequate sensor technology with EB
as the diagnostic matrix appears a highly promising approach
toward personalized noninvasive diagnostics for ubiquitously
monitoring the physiological status.
One of the most challenging obstacles that the sensor
community still needs to overcome, is the ability to measure
multiple constituents with sensitivity at trace levels. This
feature along with molecular selectivity while dealing with a
frequently changing background signal makes breath sensor
research a challenging task.
It is expected that first-generation commercial breath sensors
may not be able to directly diagnose some prevalent diseases
(e.g., pulmonary diseases such as ARDS, or various cancers),
but they may assist in the identification whether a patient respondsor notto treatment with certain drug regimes. For
many disease pathologies, it is essential to discriminate responders from potential nonresponders for deciding on the correct
treatment or medication strategy, and so this function alone will
provide an advance to the medical community. Still, within reasonable timeframes in the upcoming decade, it seems possible
that commercial breath tests for very specific diagnoses will become widely used. For all of these reasons, we hope that this
Special Topics Issue will help to organize new and important
work in the field and motivate others to enter this exciting research area.
ACKNOWLEDGMENT
Our team of Guest Editors would like to thank the authors
who have contributed to this Special Issue. We appreciate the
conscientious reviewers who spent time evaluating manuscripts,
and the IEEE staff who helped to make this Special Issue a
reality.
Cristina E. Davis
University of California Davis
Davis, CA 95616 USA
cedavis@ucdavis.edu
Matthias Frank
Lawrence Livermore National Laboratory
Livermore, CA 94551 USA
frank1@llnl.gov
Boris Mizaikoff
University of Ulm
Institute of Analytical and Bioanalytical Chemistry
Ulm, 89081 Germany
boris.mizaikoff@uni-ulm.de
Harald Oser
SRI International, Inc.
Menlo Park, CA 94025 USA
harald.oser@sri.com
REFERENCES
[1] L. Pauling, A. B. Robinson, R. Teranish, and P. Cary, Quantitative
analysis of urine vapor and breath by gas-liquid partition chromatography, in Proc. Nat. Acad. Sci. USA, 1971, vol. 68, p. 2374.
[2] M. Phillips, J. Herrera, S. Krishnan, M. Zain, J. Greenberg, and R.
N. Cataneo, Variation in volatile organic compounds in the breath of
normal humans, J. Chromatography B, vol. 729, pp. 7588, 1999.
[3] M. Phillips, Method for the collection and assay of volatile organic
compounds in breath, Anal. Biochem., vol. 247, pp. 272278, 1997.
Cristina Davis received the B.S. degree with a double major in mathematics and biology from
Duke University, Durham, NC, in 1994, and the M.S. and Ph.D. degrees in biomedical engineering
from the University of Virginia, Charlottesville, in 1996 and 1999, respectively.
She is an Assistant Professor at the University of California, Davis, where her research program
focuses on design and implementation of chemical and biological sensors using micro- and nanofabrication technologies. She trained as a Postdoctoral Fellow at the Johns Hopkins University,
Baltimore, MD, from 1999 to 2001. She then worked in industry for over half a decade designing
and implementing sensors systems. She has been at the University of California, Davis, since 2005.
IEEE SENSORS JOURNAL, VOL. 10, NO. 1, JANUARY 2010
Matthias Frank received the Ph.D. degree in physics from the Max-Planck Institute for Physics
and the Technical University of Munich, Munich, Germany, in 1993.
He is the group leader for the Advanced Diagnostics and Instrumentation Group of the Physics
Division in the Physical and Life Sciences Directorate, Lawrence Livermore National Laboratory,
Livermore, CA. He has an extensive background in biodetection and related analytical instrumentation such as mass spectrometry and UV laser induced fluorescence. He also has an extensive background in advanced instrumentation for X-ray detection and spectroscopy. He is currently working
on advanced mass spectrometric techniques for the analysis of single cells, aerosol particles, human
effluents and breath with applications in both national/homeland security and biomedicine.
Boris Mizaikoff received the Ph.D. degree in analytical chemistry from the Vienna University of
Technology, Vienna, Austria, in 1996.
He is currently the Chair of the Department of Chemistry, University of Ulm, Ulm, Germany.
He previously was an Associate Professor at the Georgia Institute of Technology, Atlanta, GA,
from 2000 to 2008. Today, his research interests focus on multifunctional scanning nanoprobes
(e.g., combination AFM-SECM, NSOMSECM), scanning probe tip integrated nano(bio)sensors,
optical sensors, biosensors and biomimetic sensors operating in the midinfrared spectral range,
novel IR light sources (e.g., quantum cascade lasers), system miniaturization and integration based
on micro and nanofabrication, focused ion beam techniques, development of chemical recognition
layers for separation and sensing applications (e.g., molecularly templated materials, functionalized
sol-gels), chemometric data evaluation, advanced vibrational spectroscopic techniques including
SEIRA and SERS, environmental analytical chemistry, process analytical chemistry, and biomedical diagnostics.
Harald Oser received the Ph.D. degree in physical chemistry from the University of Stuttgart,
Stuttgart, Germany, in 1992.
He is a Senior Research Physicist at the Molecular Physics Laboratory, SRI Internationalm Inc.,
Manlo Park, CA. He has 15 years experience in laser spectroscopy, mass spectrometry, and chemical kinetics. His areas of expertise include laser and molecular physics; nonlinear optics; multiphoton excitation; chemical kinetics of flame relevant reaction; high-resolution laser spectroscopy;
mass spectrometry; ion-optical design; photon ionization instrumentation and its field applications;
laser-based environmental monitoring, explosives detection, and surface analysis. Current research
includes the development and application of mass spectrometric techniques for breath analysis and
real-time characterization of pyrolysis gases during ablator thermal decomposition.
You might also like
- Bot CookbookDocument149 pagesBot Cookbookdaniel monteroNo ratings yet
- Jurnal ForensikDocument15 pagesJurnal ForensikZoehelmy HusenNo ratings yet
- Gangaram Rate List PDFDocument315 pagesGangaram Rate List PDFAmit Kumar GuptaNo ratings yet
- Production of Lime: Chemical Engineering DepartmentDocument17 pagesProduction of Lime: Chemical Engineering DepartmentDon Aries EidosNo ratings yet
- Human Exhaled Breath Analysis: CME ReviewDocument6 pagesHuman Exhaled Breath Analysis: CME ReviewJulieta SolariNo ratings yet
- 10 1 1 232 716 PDFDocument17 pages10 1 1 232 716 PDFSounak BoseNo ratings yet
- Exhaled Breath Analysis in The Differentiation of Pneumonia From Acute Pulmonary OedemaDocument7 pagesExhaled Breath Analysis in The Differentiation of Pneumonia From Acute Pulmonary OedemaAkka RakaNo ratings yet
- Jurnal BiomedikDocument10 pagesJurnal BiomedikneaNo ratings yet
- E Nose:E TongueDocument6 pagesE Nose:E TongueKilian DuchesneNo ratings yet
- Breath Analysis: Trends in Techniques and Clinical ApplicationsDocument6 pagesBreath Analysis: Trends in Techniques and Clinical ApplicationsDina MansourNo ratings yet
- Biomarkers in COPD ExacerbationsDocument12 pagesBiomarkers in COPD ExacerbationsLinto JohnNo ratings yet
- Application of Fecal Volatile Organic Compound Analysis in Clinical Practice: Current State and Future PerspectivesDocument20 pagesApplication of Fecal Volatile Organic Compound Analysis in Clinical Practice: Current State and Future PerspectiveslecongdangNo ratings yet
- Sauca (M) I6157820 BSC Thesis 2020Document33 pagesSauca (M) I6157820 BSC Thesis 2020marius saucaNo ratings yet
- 2004 Clinica Chimica ActaDocument15 pages2004 Clinica Chimica ActaDina MansourNo ratings yet
- Exhaled Breath PaperDocument16 pagesExhaled Breath PaperCristhian Manuel Durán AcevedoNo ratings yet
- Unit 7 Blood PressureDocument11 pagesUnit 7 Blood PressureQ O R Y A N INo ratings yet
- Biomarker Copd PDFDocument35 pagesBiomarker Copd PDFManoj KumarNo ratings yet
- Analysis of Volatile Organic Compounds From Deep Airway in The Lung Through Intubation SamplingDocument12 pagesAnalysis of Volatile Organic Compounds From Deep Airway in The Lung Through Intubation SamplingmoubarginNo ratings yet
- Unit 8Document11 pagesUnit 8FatmawatiNo ratings yet
- Exhaled Breath Analysis For Lung CancerDocument12 pagesExhaled Breath Analysis For Lung CancerIkaPKNo ratings yet
- Respiration - Electronic NoseDocument13 pagesRespiration - Electronic NoseCristhian Manuel Durán AcevedoNo ratings yet
- Optoelectronic PlethysmographyDocument15 pagesOptoelectronic PlethysmographygothicmetalspiritNo ratings yet
- Myeloperoxidase and Protein Oxidation in The Airways of Young Children With Cystic FibrosisDocument7 pagesMyeloperoxidase and Protein Oxidation in The Airways of Young Children With Cystic FibrosisMichael StudiofourteenohnineNo ratings yet
- Pulse Oximetry Instrumental Alternative in The Clinical Evaluation by The Bed For The DysphagiaDocument8 pagesPulse Oximetry Instrumental Alternative in The Clinical Evaluation by The Bed For The DysphagiaGabriel MaldonadoNo ratings yet
- Lung Function and Peak Oxygen Uptake in Chronic Obstructive Pulmonary Disease Phenotypes With and Without EmphysemaDocument12 pagesLung Function and Peak Oxygen Uptake in Chronic Obstructive Pulmonary Disease Phenotypes With and Without EmphysemaAndreea MoalesNo ratings yet
- 2006 129 1344-1348 Christopher E. Brightling: Clinical Applications of Induced SputumDocument7 pages2006 129 1344-1348 Christopher E. Brightling: Clinical Applications of Induced Sputumjoal510No ratings yet
- Sensors: Novel Isoprene Sensor For A Flu Virus Breath MonitorDocument7 pagesSensors: Novel Isoprene Sensor For A Flu Virus Breath MonitorJuanGabrielVillamizarNo ratings yet
- Asthma Enose IOT ReportDocument55 pagesAsthma Enose IOT ReportASHVIK JNo ratings yet
- Pulmonary Biomarkers in COPD: Peter J. BarnesDocument6 pagesPulmonary Biomarkers in COPD: Peter J. Barnesmike_helplineNo ratings yet
- Oxygen Therapy For Chronic Obstructive Pulmonary Disease PatientsDocument9 pagesOxygen Therapy For Chronic Obstructive Pulmonary Disease PatientsshielphiNo ratings yet
- 2015 - Gaspard - Aerosol Sampling Using An Electrostatic Precipitator Integrated With A Microfluidic Interface - PaperDocument9 pages2015 - Gaspard - Aerosol Sampling Using An Electrostatic Precipitator Integrated With A Microfluidic Interface - PaperNgô Đình NhânNo ratings yet
- Cyto Lungtumorbook1Document104 pagesCyto Lungtumorbook1ixNo ratings yet
- Lung Atlas 2014 CPRDocument187 pagesLung Atlas 2014 CPRelessar2001100% (1)
- Bronchoalveolar Lavage As A Diagnostic T PDFDocument15 pagesBronchoalveolar Lavage As A Diagnostic T PDFAndy Rusgi KribowNo ratings yet
- Waypa G. and Schumacker P. O2 Sensing in Hypoxic Pulmonary Vasoconstriction The Mitochondrial Door Re-Opens. Respir. Physiol. Neurobiol. (2002)Document11 pagesWaypa G. and Schumacker P. O2 Sensing in Hypoxic Pulmonary Vasoconstriction The Mitochondrial Door Re-Opens. Respir. Physiol. Neurobiol. (2002)benjabmbNo ratings yet
- Ijms 13 13894Document17 pagesIjms 13 13894osama mosaNo ratings yet
- Indice AclaramientoDocument4 pagesIndice AclaramientoPaola Vicenta Chalco MorenoNo ratings yet
- Aiomt 106Document10 pagesAiomt 106AyestinNo ratings yet
- Symptomatic Patients Without Airflow Obstruction2016Document4 pagesSymptomatic Patients Without Airflow Obstruction2016Ella EllaNo ratings yet
- Bal 3BDocument29 pagesBal 3BLian Marie ViñasNo ratings yet
- Case Analysis PneumoniaDocument5 pagesCase Analysis PneumoniaLorence RamosNo ratings yet
- Natural History and Mechanisms of COPD: Invited Review Series: Copd: New HorizonsDocument24 pagesNatural History and Mechanisms of COPD: Invited Review Series: Copd: New HorizonsSebastian RamirezNo ratings yet
- Pulmonary Functional Imaging: Basics and Clinical ApplicationsFrom EverandPulmonary Functional Imaging: Basics and Clinical ApplicationsYoshiharu OhnoNo ratings yet
- An Adverse Outcome Pathway For Lung Surfactant Functio - 2021 - Current ResearchDocument12 pagesAn Adverse Outcome Pathway For Lung Surfactant Functio - 2021 - Current ResearchAadityarajsinh GohilNo ratings yet
- Proteome Profiling of Lung Tissues in ChronicDocument8 pagesProteome Profiling of Lung Tissues in ChronicAndreea MoalesNo ratings yet
- MocoyN Acetilcisteinaene2018Document9 pagesMocoyN Acetilcisteinaene2018mariela carlo tancaraNo ratings yet
- Frontiers in Respiratory Physiology - Grand ChallengeDocument2 pagesFrontiers in Respiratory Physiology - Grand ChallengeAlfi OktafaniNo ratings yet
- 2019 - Chronic Obstructive Pulmonary Disease andDocument6 pages2019 - Chronic Obstructive Pulmonary Disease andAndreea MoalesNo ratings yet
- Lung Sounds in Bronchial Asthma: Review ArticleDocument11 pagesLung Sounds in Bronchial Asthma: Review ArticleSophia RoseNo ratings yet
- Bronkiolitis AkutDocument10 pagesBronkiolitis AkutNamira Firdha KNo ratings yet
- Journal of Neurochemistry - 2011 - Gacki ReDocument12 pagesJournal of Neurochemistry - 2011 - Gacki ReantoniorNo ratings yet
- Research Paper On OxygenDocument5 pagesResearch Paper On Oxygenegya6qzc100% (1)
- Time To Throw AwayDocument10 pagesTime To Throw AwayPuteri Indah Achmad HasyimNo ratings yet
- 1 s2.0 S0304416511001358 MainDocument8 pages1 s2.0 S0304416511001358 MainjackashcaNo ratings yet
- Markers of Pulmonary Oxygen Toxicity in Hyperbaric Oxygen Therapy Using Exhaled Breath AnalysisDocument9 pagesMarkers of Pulmonary Oxygen Toxicity in Hyperbaric Oxygen Therapy Using Exhaled Breath AnalysisThijs WingelaarNo ratings yet
- Chest: The Role of CT Scanning in Multidimensional Phenotyping of COPDDocument9 pagesChest: The Role of CT Scanning in Multidimensional Phenotyping of COPDAtika Indah SariNo ratings yet
- Cigarette Smoke Promotes Dendritic Cell Accumulation in COPD A Lung Tissue Research Consortium StudyDocument13 pagesCigarette Smoke Promotes Dendritic Cell Accumulation in COPD A Lung Tissue Research Consortium StudyArry SetyowatiNo ratings yet
- FullDocument13 pagesFullgregor alexanderNo ratings yet
- American Thoracic Society DocumentsDocument19 pagesAmerican Thoracic Society DocumentsPhanNo ratings yet
- 744 FullDocument5 pages744 FullBogdan NechitaNo ratings yet
- PATH Recommendations - EditedDocument2 pagesPATH Recommendations - EditedJohnNo ratings yet
- 1jebp PDFDocument14 pages1jebp PDFekarusningwatiNo ratings yet
- MocoyN Acetilcisteinaene2018Document9 pagesMocoyN Acetilcisteinaene2018Alejandra JimenezNo ratings yet
- Alhena Eng Rev06Document7 pagesAlhena Eng Rev06Steven BrownNo ratings yet
- Indomethacin From Anti-Inflammatory To Anticancer AgentDocument26 pagesIndomethacin From Anti-Inflammatory To Anticancer AgentYaqeen Alhaqq F. GhaziNo ratings yet
- Brochure - Ancient Rock Salt, Gourmet Salts PDFDocument16 pagesBrochure - Ancient Rock Salt, Gourmet Salts PDFLaraib AliNo ratings yet
- GCU ELM-305 Topic 5 Discussion Question ResponsesDocument3 pagesGCU ELM-305 Topic 5 Discussion Question ResponsesKristin HensleyNo ratings yet
- Lab 5 ImineDocument10 pagesLab 5 ImineCheng FuNo ratings yet
- Director Manager Payroll CPP in Seattle WA Resume Michael HoernerDocument1 pageDirector Manager Payroll CPP in Seattle WA Resume Michael HoernerMichaelHoerner2No ratings yet
- Leisure in My Life - ReportDocument16 pagesLeisure in My Life - ReportnuriNo ratings yet
- Learning Disabilities OtDocument48 pagesLearning Disabilities OtReeva de SaNo ratings yet
- Full Download Test Bank For Personal Nutrition 7th Edition Boyle PDF Full ChapterDocument36 pagesFull Download Test Bank For Personal Nutrition 7th Edition Boyle PDF Full Chaptertetrazosubaud0q5f100% (22)
- Actuator Ari PremioDocument12 pagesActuator Ari Premioluthfie.swaciptaNo ratings yet
- 4-Point Action Plan by Esperanza and Brian CabralDocument6 pages4-Point Action Plan by Esperanza and Brian CabralRapplerNo ratings yet
- A 26 V 14 N 02Document6 pagesA 26 V 14 N 02faustinopateiro3497No ratings yet
- IA Findings ProcurementDocument2 pagesIA Findings ProcurementSreekanth PCNo ratings yet
- Rotonivo: Series RN 3000 / 6000Document34 pagesRotonivo: Series RN 3000 / 6000Strato VariusNo ratings yet
- Platts Nucleonics Week 19 July2012Document15 pagesPlatts Nucleonics Week 19 July2012Jovi Savitri Eka PutriNo ratings yet
- Relative Pronouns and TenseseDocument4 pagesRelative Pronouns and TenseseKarla TorresNo ratings yet
- Flojet Beverage CatDocument24 pagesFlojet Beverage CatRacil EzzedineNo ratings yet
- 2021-2023 FO X RFR Tracker - KC NCDDP AFDocument147 pages2021-2023 FO X RFR Tracker - KC NCDDP AFJestoni Gonzales TortolaNo ratings yet
- Playground Antonyms PDFDocument2 pagesPlayground Antonyms PDFChayne RodilNo ratings yet
- Pre-Cast Concrete SpecialistsDocument24 pagesPre-Cast Concrete SpecialistsSilas MangwendeNo ratings yet
- Azidus Laboratories - BA BE Capabilities Slide Deck - Feb 2019 PDFDocument35 pagesAzidus Laboratories - BA BE Capabilities Slide Deck - Feb 2019 PDFDeepakNo ratings yet
- Jurnal 3Document6 pagesJurnal 3Zaimatul HamdiyahNo ratings yet
- Building Maintenance ChecklistDocument5 pagesBuilding Maintenance ChecklistcajaroNo ratings yet
- Task 1 - Three Phase (Ø) Electrical Installation Direct On Line (Dol) Forward Motor ControlDocument4 pagesTask 1 - Three Phase (Ø) Electrical Installation Direct On Line (Dol) Forward Motor Controlmoganraj8munusamyNo ratings yet
- Electrical Safety HAE EM EPS GDCC ES PDFDocument17 pagesElectrical Safety HAE EM EPS GDCC ES PDFkhleifat_613891No ratings yet
- Sustainability 14 07022 v2Document22 pagesSustainability 14 07022 v2Osman DenizNo ratings yet
- Valleylab Ft10 Energy Platform Users GuideDocument174 pagesValleylab Ft10 Energy Platform Users Guideavanteb ajamNo ratings yet