Professional Documents
Culture Documents
Bacterial Meningitis HSV Encephalitis: Therapeutic Guidelines Antibiotic
Bacterial Meningitis HSV Encephalitis: Therapeutic Guidelines Antibiotic
Uploaded by
Betari DhiraCopyright:
Available Formats
You might also like
- Collins-Donnelly, Kate (2014) Starving The Anxiety Gremlin For Children Aged 5-9 A CBT Workbook On Anxiety ManagementDocument193 pagesCollins-Donnelly, Kate (2014) Starving The Anxiety Gremlin For Children Aged 5-9 A CBT Workbook On Anxiety ManagementG100% (1)
- Miscellaneous For FinalsDocument30 pagesMiscellaneous For Finalsjames.a.blairNo ratings yet
- Baldur's Gate - Shield of The Hidden LordDocument37 pagesBaldur's Gate - Shield of The Hidden LordJacobo Cisneros75% (4)
- Adult Placement Test: Scegli L'alternativa Corretta Per Completare Gli SpaziDocument2 pagesAdult Placement Test: Scegli L'alternativa Corretta Per Completare Gli SpaziGanchimeg Shiirev100% (1)
- Icu Antibiotic GuidelinesDocument4 pagesIcu Antibiotic GuidelinesTia MonitaNo ratings yet
- Amoxicillin 125 MG 250 MG 5 ML Oral SuspensionDocument16 pagesAmoxicillin 125 MG 250 MG 5 ML Oral SuspensionAshrafNo ratings yet
- Empiric Antibiotic Guidelines For Paediatric Intensive Care Unit (PICU)Document7 pagesEmpiric Antibiotic Guidelines For Paediatric Intensive Care Unit (PICU)Benny Chris TantoNo ratings yet
- NAG Urinary Tract InfectionsDocument14 pagesNAG Urinary Tract InfectionsJun JimenezNo ratings yet
- Antibiotic Policy 2014Document32 pagesAntibiotic Policy 2014shah007zaad100% (1)
- Medicine RotatationbookletDocument20 pagesMedicine RotatationbookletJanelle JosephsNo ratings yet
- Dosis MimsDocument21 pagesDosis MimsYulia Putri CarlianaNo ratings yet
- Azithromycin Monograph - PaediatricDocument7 pagesAzithromycin Monograph - PaediatrictynNo ratings yet
- 1 s2.0 S0163445316300123 MainDocument2 pages1 s2.0 S0163445316300123 MainZara SaeedNo ratings yet
- Champ Empiric Antimicrobial Guidelines: Consider Investigation and Treatment For Pertussis And/Or Chlamydia TrachomatisDocument2 pagesChamp Empiric Antimicrobial Guidelines: Consider Investigation and Treatment For Pertussis And/Or Chlamydia TrachomatistynNo ratings yet
- Analgesik/Pire Tik Dosis Sediaan Obat DOA OOA Drug Interaction Paracetamol IVDocument9 pagesAnalgesik/Pire Tik Dosis Sediaan Obat DOA OOA Drug Interaction Paracetamol IVNicole NgoNo ratings yet
- Drugs in Medicine by Medad Team FinalDocument5 pagesDrugs in Medicine by Medad Team Finalعبد الرحمن100% (2)
- ConnectorDocument4 pagesConnectoryetaung8No ratings yet
- Guide Paed Bone JNTDocument11 pagesGuide Paed Bone JNTDorica GiurcaNo ratings yet
- Febrile NeutropeniaDocument3 pagesFebrile Neutropeniatheseus5No ratings yet
- Updated Recommended Treatment Regimens For Gonococcal Infections and Associated Conditions - United States, April 2007Document5 pagesUpdated Recommended Treatment Regimens For Gonococcal Infections and Associated Conditions - United States, April 2007iniciate07No ratings yet
- Metoclopramide DiclofenacDocument7 pagesMetoclopramide DiclofenacRasco, Allen jayNo ratings yet
- Oxaciline PDFDocument7 pagesOxaciline PDFamatoryfictionliteraNo ratings yet
- IpsaDocument19 pagesIpsaLuisa LopezNo ratings yet
- Drug StudyDocument10 pagesDrug StudybaniniycsebNo ratings yet
- GentDocument2 pagesGentOxford666No ratings yet
- Empiric Antibiotic Treatment of Urinary Tract InfectionsDocument3 pagesEmpiric Antibiotic Treatment of Urinary Tract InfectionsVikas KumarNo ratings yet
- Cilastati Imipenem Drug InfoDocument19 pagesCilastati Imipenem Drug InfoCosmina GeorgianaNo ratings yet
- Management of The Complications of Nephrotic SyndromeDocument6 pagesManagement of The Complications of Nephrotic SyndromeRagabi RezaNo ratings yet
- Drug StudyDocument16 pagesDrug StudyJhann0% (1)
- Acyclovir Drug StudyDocument3 pagesAcyclovir Drug StudyJessie Cauilan Cain100% (1)
- Acyclovir Drug CardDocument3 pagesAcyclovir Drug CardLisaNo ratings yet
- K25. Malaria Pada AnakDocument39 pagesK25. Malaria Pada AnakayapillaiNo ratings yet
- 9 Drug StudyDocument11 pages9 Drug StudyJessa Mae Mauricio CastilloNo ratings yet
- Castration-Recurrent Prostate Cancer First-Line Therapy: No Visceral MetastasesDocument2 pagesCastration-Recurrent Prostate Cancer First-Line Therapy: No Visceral Metastasesalberto cabelloNo ratings yet
- Internal Abdominal Infection Treatment ProtocolDocument9 pagesInternal Abdominal Infection Treatment Protocolhatem newishyNo ratings yet
- Bone and Joint Infections BNHFT 2010 PDFDocument3 pagesBone and Joint Infections BNHFT 2010 PDFDanissa Fidia PuteriNo ratings yet
- Profil Ampicillin SulbactamDocument12 pagesProfil Ampicillin SulbactamasriNo ratings yet
- Antipyretics: Instiaty Tropical Infection Module 2017-2018 Dept of Pharmacology and Therapeutics FkuiDocument22 pagesAntipyretics: Instiaty Tropical Infection Module 2017-2018 Dept of Pharmacology and Therapeutics Fkuisalsa2506No ratings yet
- Guidelines For First-Line Empirical Antibiotic Therapy in AdultsDocument1 pageGuidelines For First-Line Empirical Antibiotic Therapy in AdultsAnonymous s4yarxNo ratings yet
- Metoclopramide: GIT Regulators, Antiflatulents & Anti-Inflammatories Antiemetics See Available Brands of MetoclopramideDocument9 pagesMetoclopramide: GIT Regulators, Antiflatulents & Anti-Inflammatories Antiemetics See Available Brands of MetoclopramideDominique RamosNo ratings yet
- Metoclopramide: GIT Regulators, Antiflatulents & Anti-Inflammatories Antiemetics See Available Brands of MetoclopramideDocument9 pagesMetoclopramide: GIT Regulators, Antiflatulents & Anti-Inflammatories Antiemetics See Available Brands of MetoclopramideDominique RamosNo ratings yet
- Terapi AnakDocument10 pagesTerapi AnakIka KrastanayaNo ratings yet
- Common TreatmentsDocument5 pagesCommon TreatmentsRaj MandumulaNo ratings yet
- Opiates (E.g. Codeine, Heroin, Pethidine, Morphine, Methadone)Document7 pagesOpiates (E.g. Codeine, Heroin, Pethidine, Morphine, Methadone)Ali HussnainNo ratings yet
- Omeprazole Drug StudyDocument4 pagesOmeprazole Drug StudyFeliza Therese A. DeloriaNo ratings yet
- Pseudomonas Aeruginosa PfizerDocument3 pagesPseudomonas Aeruginosa PfizerPutri Kania DewiNo ratings yet
- Management of Tuberculosis in Special Situations: Prof. Dr. Zafar Hussain IqbalDocument27 pagesManagement of Tuberculosis in Special Situations: Prof. Dr. Zafar Hussain IqbalFahadKamalNo ratings yet
- PP ObatDocument7 pagesPP ObatSaifan AbdurrohmanNo ratings yet
- Pharma - CCRDocument24 pagesPharma - CCRPrathik YanalaNo ratings yet
- Drugs of MineDocument16 pagesDrugs of MineJoan GungobNo ratings yet
- Phenytoin Dosage: Usual Adult Dose For SeizuresDocument4 pagesPhenytoin Dosage: Usual Adult Dose For SeizuresHarish Ayu LNo ratings yet
- Final Haad (DOH) ExamDocument9 pagesFinal Haad (DOH) ExamsenthamizhselvanNo ratings yet
- Meropenem - Drug Information - UpToDate-2Document8 pagesMeropenem - Drug Information - UpToDate-2Vh TRNo ratings yet
- Meropenem - Drug Information - UpToDate-2Document8 pagesMeropenem - Drug Information - UpToDate-2Vh TRNo ratings yet
- Drug Study GentamicinDocument3 pagesDrug Study GentamicinEARL GERALD RICAFRANCANo ratings yet
- AntifungalDocument7 pagesAntifungalKhor Chin PooNo ratings yet
- uk-spc-nexium-sachet-10mg-DRESS-update-GI 21 0012aDocument17 pagesuk-spc-nexium-sachet-10mg-DRESS-update-GI 21 0012aDeisy ClerkeNo ratings yet
- Adult: IV Nosocomial Pneumonia Empiric Therapy For Febrile Neutropenic Patients 4.5Document3 pagesAdult: IV Nosocomial Pneumonia Empiric Therapy For Febrile Neutropenic Patients 4.5Chris Denver BancaleNo ratings yet
- Paracetamol Package InsertDocument3 pagesParacetamol Package InsertDiane ApostolNo ratings yet
- STREPTOMYCIN MonographDocument3 pagesSTREPTOMYCIN Monographfayrouz fathiNo ratings yet
- Concise Guide to Clinical Dentistry: Common Prescriptions In Clinical DentistryFrom EverandConcise Guide to Clinical Dentistry: Common Prescriptions In Clinical DentistryNo ratings yet
- Critical Care Medications: Anti-Arrhythmics Study Guide: Critical Care EssentialsFrom EverandCritical Care Medications: Anti-Arrhythmics Study Guide: Critical Care EssentialsNo ratings yet
- Ulcerative Colitis, A Simple Guide To The Condition, Treatment And Related ConditionsFrom EverandUlcerative Colitis, A Simple Guide To The Condition, Treatment And Related ConditionsNo ratings yet
- Preeklamsia: Portofolio Kasus EmergencyDocument1 pagePreeklamsia: Portofolio Kasus EmergencyBetari DhiraNo ratings yet
- Refrensi: Implications For The Assessment of Hepatic Encephalopathy. Hepatology 50:2014Document1 pageRefrensi: Implications For The Assessment of Hepatic Encephalopathy. Hepatology 50:2014Betari DhiraNo ratings yet
- Journal NeurologiDocument9 pagesJournal NeurologiBetari DhiraNo ratings yet
- Journal NeuroDocument6 pagesJournal NeuroBetari DhiraNo ratings yet
- Presentasi Journal ReadingDocument8 pagesPresentasi Journal ReadingBetari DhiraNo ratings yet
- A Histeria - Teoria e Clínica PsicanalíticaDocument653 pagesA Histeria - Teoria e Clínica PsicanalíticaDaniel BraunaNo ratings yet
- Position Paper Martial LawDocument3 pagesPosition Paper Martial LawLeoncio BocoNo ratings yet
- The Victim's Autopsy ReportDocument2 pagesThe Victim's Autopsy ReportShan KNo ratings yet
- CHEM 101 Chapter 2Document78 pagesCHEM 101 Chapter 2mikayla sirovatkaNo ratings yet
- In Re SantiagoDocument2 pagesIn Re SantiagoKing BadongNo ratings yet
- Annotated BibliographyDocument4 pagesAnnotated Bibliographyapi-302549909No ratings yet
- ATPAR ReviewerDocument25 pagesATPAR ReviewerJohn Paul BuliyatNo ratings yet
- Jamer Module 3 Foreignization and DomesticationDocument5 pagesJamer Module 3 Foreignization and DomesticationRenzo JamerNo ratings yet
- Effect of IBA and NAA With or Without GA Treatment On Rooting Attributes of Hard Wood Stem Cuttings of Pomegranate (Punica Granatum L.)Document5 pagesEffect of IBA and NAA With or Without GA Treatment On Rooting Attributes of Hard Wood Stem Cuttings of Pomegranate (Punica Granatum L.)warlord_ckNo ratings yet
- Indian Feminism - Class, Gendera & Identity in Medieval AgesDocument33 pagesIndian Feminism - Class, Gendera & Identity in Medieval AgesSougata PurkayasthaNo ratings yet
- Ariston As 600 V DryerDocument40 pagesAriston As 600 V DryermmvdlpNo ratings yet
- Repair Appx V3Document18 pagesRepair Appx V3soniaNo ratings yet
- Eslprintables 2009810153647888645279Document1 pageEslprintables 2009810153647888645279Mathéo DE OLIVEIRANo ratings yet
- Book Project FinalDocument12 pagesBook Project FinalAuguste RiedlNo ratings yet
- TAX Calalang v. LorenzoDocument3 pagesTAX Calalang v. LorenzoAnathea CadagatNo ratings yet
- CH 6 Properties of Lasers in Introduction To OpticsDocument34 pagesCH 6 Properties of Lasers in Introduction To OpticsmoatazNo ratings yet
- Psychoanalysis: ArticleDocument21 pagesPsychoanalysis: ArticleAqsa ParveenNo ratings yet
- RHPA46 FreeDocument5 pagesRHPA46 Freeheyimdee5No ratings yet
- Research in Organizational Behavior: Sabine SonnentagDocument17 pagesResearch in Organizational Behavior: Sabine SonnentagBobby DNo ratings yet
- Gas Supply Agreement 148393.1Document5 pagesGas Supply Agreement 148393.1waking_days100% (1)
- AP Biology Syllabus 2009-2010Document10 pagesAP Biology Syllabus 2009-2010yulianaholicNo ratings yet
- TM I RubenDocument165 pagesTM I RubenMark Kevin DaitolNo ratings yet
- M-Sand in Tamil NaduDocument9 pagesM-Sand in Tamil Nadurameshkanu1No ratings yet
- TarzanDocument2 pagesTarzanmaris quilantangNo ratings yet
- Big Data Insurance Case Study PDFDocument2 pagesBig Data Insurance Case Study PDFVivek SaahilNo ratings yet
- The Role of Majority and Minority Language Input in The Early Development of A Bilingual VocabularyDocument15 pagesThe Role of Majority and Minority Language Input in The Early Development of A Bilingual VocabularyPoly45No ratings yet
- 723PLUS Digital Control - WoodwardDocument40 pages723PLUS Digital Control - WoodwardMichael TanNo ratings yet
Bacterial Meningitis HSV Encephalitis: Therapeutic Guidelines Antibiotic
Bacterial Meningitis HSV Encephalitis: Therapeutic Guidelines Antibiotic
Uploaded by
Betari DhiraOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Bacterial Meningitis HSV Encephalitis: Therapeutic Guidelines Antibiotic
Bacterial Meningitis HSV Encephalitis: Therapeutic Guidelines Antibiotic
Uploaded by
Betari DhiraCopyright:
Available Formats
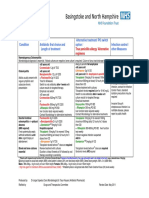
SESIAHS
ADULT Empiric Antibiotic Guidelines1
CNS
Bacterial
meningitis
Ceftriaxone 2g IV every 12 hours
If the patient is immunocompromised or Listeria is suspected ADD
benzylpenicillin 2.4g IV every 4 hours
HSV
encephalitis
Aciclovir 10mg per kg IV every 8 hours for at least 14 days
(adjust dose if reduced renal function)
URINARY
Acute cystitis
Non-pregnant women: Trimethoprim 300mg orally daily for 3 days
Pregnant women: Cephalexin 500mg orally every 12 hours for 5 days
Men: Trimethoprim 300mg orally daily for 14 days
Acute
pyelonephritis
Mild: Cephalexin 500mg orally every 6 hours for 10 days
Severe: Ampicillin 2g IV every 6 hours PLUS
gentamicin2 4 to 6mg per kg IV daily for max of 3 doses
If gentamicin contraindicated: Ceftriaxone 1g IV daily as a single agent
GASTROINTESTINAL
Cholecystitis
Ampicillin 1g IV every 6 hours PLUS
gentamicin2 4 to 6mg per kg IV daily for max of 3 doses
(PLUS metronidazole 500mg IV every 12 hours if biliary obstruction)
Cholangitis
Ampicillin 1g IV every 6hours PLUS
gentamicin2 4 to 6mg per kg IV daily for max of 3 doses (PLUS
metronidazole 500mg IV every 12 hours if biliary surgery or obstruction)
If gentamicin contraindicated: Ceftriaxone 1g IV daily (PLUS
metronidazole 500mg IV every 12 hours if biliary surgery or obstruction)
Peritonitis due
to perforation
Ampicillin 1g IV every 6 hours PLUS gentamicin2 4 to 6mg per kg IV
daily for max of 3 doses PLUS metronidazole 500mg IV every 12 hours
If gentamicin contraindicated, as single agent: Ticarcillin with clavulanate
3.1g IV every 6 hours OR piperacillin with tazobactam 4.5g IV every 8 hours
SKIN and SOFT TISSUE
Cellulitis
Assess exposure
risk for gram
negative organisms
(and seek expert
advice)
Mild outpatient therapy
Flucloxacillin 500mg orally every 6 hours for 7 to 10 days, OR
Cephazolin 2g IV daily PLUS probenecid 1g orally daily
Requiring admission
Flucloxacillin 2g IV every 6 hours OR cephazolin 2g IV every 8 hours
If MRSA risk (prior colonisation, MRSA infection or hospital association):
ADD vancomycin 1.5g IV every 12 hours (adjust in renal impairment and
check level at 48 hours)
This guideline must not replace clinical judgement. May not apply to immunocompromised
patients
Detailed guidelines available via CIAP on intranet: Therapeutic Guidelines Antibiotic v 14, 2010.
Check local antibiotic restriction policies
1
doses are for normal renal function
Check eTG for gentamicin dosing
Expires Jan 2013
RESPIRATORY
Communityacquired
pneumonia
(CAP)
Mild CAP
Amoxycillin 1g orally every 8 hours for 5 to 7 days OR
Doxycycline orally, 200mg for 1st dose, then 100mg daily for 5 days
Moderate CAP (requiring admission)
Benzylpenicillin 1.2g IV every 6 hours initially then amoxycillin as above
(with CXR changes)
totalling 7 days PLUS
doxycycline 100mg orally every 12 hours for 7 days
Severe CAP (requiring HDU/ICU management)
Ceftriaxone 1g IV daily PLUS
azithromycin 500mg IV daily for 7 to 14 days
Hospitalacquired
pneumonia
(HAP)
Low MRO risk and Mild HAP
Amoxycillin with clavulanate 875/125 mg orally every 12 hours
for 5 to 7 days
If penicillin hypersensitive (but not anaphylaxis):
Cefuroxime 500 mg orally every 12 hours for 5 to 7 days
assess risk for
multi-resistant
organisms (MROs)
If patient is unable to take oral therapy: Benzylpenicillin 1.2 g IV every 6
hours PLUS gentamicin2 4 to 6 mg per kg IV daily for max of 3 doses
Low MRO risk and Moderate to Severe HAP
(switch to oral as above as improves)
Ceftriaxone 1 g IV daily OR
Benzylpenicillin 1.2 g IV every 6hours PLUS
gentamicin2 4 to 6 mg per kg IV daily for max of 3 doses
HAP in high-risk
wards for 5 days or
longer (e.g. ICU,
high-dependency
units, known specific
resistance problem)
Infective
exacerbation of
COPD
High MRO Risk and Moderate to Severe HAP
Piperacillin with tazobactam 4.5g IV every 6 hours OR
Ticarcillin with clavulanate 3.1g IV every 6 hours OR
Cefepime 2 g IV every 8 hours
If MRSA likely ADD vancomycin 1.5g IV every 12 hours and monitor levels
Consider treatment with bronchodilators and oral corticosteroids
If antibiotics required: Amoxycillin 500mg orally every 8 hours OR
doxycycline 100mg orally every 12 hours for 5 days
TIMELY CONVERSION FROM IV TO ORAL AGENTS
Reassess the need for IV antibiotic administration in your patient when they are
tolerating oral intake, have no absorption problems and show clinical improvement.
For oral formulations or suitable alternatives check with ward pharmacist.
Oral therapy is NOT suitable for initial treatment of endocarditis, meningitis, osteomyelitis,
septic arthritis or Staph. aureus bacteraemia where a high tissue antibiotic concentration is
required.
DAILY REVIEW OF ANTIBIOTIC MANAGEMENT FOR CONSIDERATION OF RATIONALISATION
AND DE-ESCALATION IS REQURIED.
This card has been produced by the Area Antimicrobial Stewardship Committee, Clinical Governance
Unit, SESIAHS. http://sesiweb.lan.sesahs.nsw.gov.au/clinical%20Governance%20unit/default.asp
Expires Jan 2013
You might also like
- Collins-Donnelly, Kate (2014) Starving The Anxiety Gremlin For Children Aged 5-9 A CBT Workbook On Anxiety ManagementDocument193 pagesCollins-Donnelly, Kate (2014) Starving The Anxiety Gremlin For Children Aged 5-9 A CBT Workbook On Anxiety ManagementG100% (1)
- Miscellaneous For FinalsDocument30 pagesMiscellaneous For Finalsjames.a.blairNo ratings yet
- Baldur's Gate - Shield of The Hidden LordDocument37 pagesBaldur's Gate - Shield of The Hidden LordJacobo Cisneros75% (4)
- Adult Placement Test: Scegli L'alternativa Corretta Per Completare Gli SpaziDocument2 pagesAdult Placement Test: Scegli L'alternativa Corretta Per Completare Gli SpaziGanchimeg Shiirev100% (1)
- Icu Antibiotic GuidelinesDocument4 pagesIcu Antibiotic GuidelinesTia MonitaNo ratings yet
- Amoxicillin 125 MG 250 MG 5 ML Oral SuspensionDocument16 pagesAmoxicillin 125 MG 250 MG 5 ML Oral SuspensionAshrafNo ratings yet
- Empiric Antibiotic Guidelines For Paediatric Intensive Care Unit (PICU)Document7 pagesEmpiric Antibiotic Guidelines For Paediatric Intensive Care Unit (PICU)Benny Chris TantoNo ratings yet
- NAG Urinary Tract InfectionsDocument14 pagesNAG Urinary Tract InfectionsJun JimenezNo ratings yet
- Antibiotic Policy 2014Document32 pagesAntibiotic Policy 2014shah007zaad100% (1)
- Medicine RotatationbookletDocument20 pagesMedicine RotatationbookletJanelle JosephsNo ratings yet
- Dosis MimsDocument21 pagesDosis MimsYulia Putri CarlianaNo ratings yet
- Azithromycin Monograph - PaediatricDocument7 pagesAzithromycin Monograph - PaediatrictynNo ratings yet
- 1 s2.0 S0163445316300123 MainDocument2 pages1 s2.0 S0163445316300123 MainZara SaeedNo ratings yet
- Champ Empiric Antimicrobial Guidelines: Consider Investigation and Treatment For Pertussis And/Or Chlamydia TrachomatisDocument2 pagesChamp Empiric Antimicrobial Guidelines: Consider Investigation and Treatment For Pertussis And/Or Chlamydia TrachomatistynNo ratings yet
- Analgesik/Pire Tik Dosis Sediaan Obat DOA OOA Drug Interaction Paracetamol IVDocument9 pagesAnalgesik/Pire Tik Dosis Sediaan Obat DOA OOA Drug Interaction Paracetamol IVNicole NgoNo ratings yet
- Drugs in Medicine by Medad Team FinalDocument5 pagesDrugs in Medicine by Medad Team Finalعبد الرحمن100% (2)
- ConnectorDocument4 pagesConnectoryetaung8No ratings yet
- Guide Paed Bone JNTDocument11 pagesGuide Paed Bone JNTDorica GiurcaNo ratings yet
- Febrile NeutropeniaDocument3 pagesFebrile Neutropeniatheseus5No ratings yet
- Updated Recommended Treatment Regimens For Gonococcal Infections and Associated Conditions - United States, April 2007Document5 pagesUpdated Recommended Treatment Regimens For Gonococcal Infections and Associated Conditions - United States, April 2007iniciate07No ratings yet
- Metoclopramide DiclofenacDocument7 pagesMetoclopramide DiclofenacRasco, Allen jayNo ratings yet
- Oxaciline PDFDocument7 pagesOxaciline PDFamatoryfictionliteraNo ratings yet
- IpsaDocument19 pagesIpsaLuisa LopezNo ratings yet
- Drug StudyDocument10 pagesDrug StudybaniniycsebNo ratings yet
- GentDocument2 pagesGentOxford666No ratings yet
- Empiric Antibiotic Treatment of Urinary Tract InfectionsDocument3 pagesEmpiric Antibiotic Treatment of Urinary Tract InfectionsVikas KumarNo ratings yet
- Cilastati Imipenem Drug InfoDocument19 pagesCilastati Imipenem Drug InfoCosmina GeorgianaNo ratings yet
- Management of The Complications of Nephrotic SyndromeDocument6 pagesManagement of The Complications of Nephrotic SyndromeRagabi RezaNo ratings yet
- Drug StudyDocument16 pagesDrug StudyJhann0% (1)
- Acyclovir Drug StudyDocument3 pagesAcyclovir Drug StudyJessie Cauilan Cain100% (1)
- Acyclovir Drug CardDocument3 pagesAcyclovir Drug CardLisaNo ratings yet
- K25. Malaria Pada AnakDocument39 pagesK25. Malaria Pada AnakayapillaiNo ratings yet
- 9 Drug StudyDocument11 pages9 Drug StudyJessa Mae Mauricio CastilloNo ratings yet
- Castration-Recurrent Prostate Cancer First-Line Therapy: No Visceral MetastasesDocument2 pagesCastration-Recurrent Prostate Cancer First-Line Therapy: No Visceral Metastasesalberto cabelloNo ratings yet
- Internal Abdominal Infection Treatment ProtocolDocument9 pagesInternal Abdominal Infection Treatment Protocolhatem newishyNo ratings yet
- Bone and Joint Infections BNHFT 2010 PDFDocument3 pagesBone and Joint Infections BNHFT 2010 PDFDanissa Fidia PuteriNo ratings yet
- Profil Ampicillin SulbactamDocument12 pagesProfil Ampicillin SulbactamasriNo ratings yet
- Antipyretics: Instiaty Tropical Infection Module 2017-2018 Dept of Pharmacology and Therapeutics FkuiDocument22 pagesAntipyretics: Instiaty Tropical Infection Module 2017-2018 Dept of Pharmacology and Therapeutics Fkuisalsa2506No ratings yet
- Guidelines For First-Line Empirical Antibiotic Therapy in AdultsDocument1 pageGuidelines For First-Line Empirical Antibiotic Therapy in AdultsAnonymous s4yarxNo ratings yet
- Metoclopramide: GIT Regulators, Antiflatulents & Anti-Inflammatories Antiemetics See Available Brands of MetoclopramideDocument9 pagesMetoclopramide: GIT Regulators, Antiflatulents & Anti-Inflammatories Antiemetics See Available Brands of MetoclopramideDominique RamosNo ratings yet
- Metoclopramide: GIT Regulators, Antiflatulents & Anti-Inflammatories Antiemetics See Available Brands of MetoclopramideDocument9 pagesMetoclopramide: GIT Regulators, Antiflatulents & Anti-Inflammatories Antiemetics See Available Brands of MetoclopramideDominique RamosNo ratings yet
- Terapi AnakDocument10 pagesTerapi AnakIka KrastanayaNo ratings yet
- Common TreatmentsDocument5 pagesCommon TreatmentsRaj MandumulaNo ratings yet
- Opiates (E.g. Codeine, Heroin, Pethidine, Morphine, Methadone)Document7 pagesOpiates (E.g. Codeine, Heroin, Pethidine, Morphine, Methadone)Ali HussnainNo ratings yet
- Omeprazole Drug StudyDocument4 pagesOmeprazole Drug StudyFeliza Therese A. DeloriaNo ratings yet
- Pseudomonas Aeruginosa PfizerDocument3 pagesPseudomonas Aeruginosa PfizerPutri Kania DewiNo ratings yet
- Management of Tuberculosis in Special Situations: Prof. Dr. Zafar Hussain IqbalDocument27 pagesManagement of Tuberculosis in Special Situations: Prof. Dr. Zafar Hussain IqbalFahadKamalNo ratings yet
- PP ObatDocument7 pagesPP ObatSaifan AbdurrohmanNo ratings yet
- Pharma - CCRDocument24 pagesPharma - CCRPrathik YanalaNo ratings yet
- Drugs of MineDocument16 pagesDrugs of MineJoan GungobNo ratings yet
- Phenytoin Dosage: Usual Adult Dose For SeizuresDocument4 pagesPhenytoin Dosage: Usual Adult Dose For SeizuresHarish Ayu LNo ratings yet
- Final Haad (DOH) ExamDocument9 pagesFinal Haad (DOH) ExamsenthamizhselvanNo ratings yet
- Meropenem - Drug Information - UpToDate-2Document8 pagesMeropenem - Drug Information - UpToDate-2Vh TRNo ratings yet
- Meropenem - Drug Information - UpToDate-2Document8 pagesMeropenem - Drug Information - UpToDate-2Vh TRNo ratings yet
- Drug Study GentamicinDocument3 pagesDrug Study GentamicinEARL GERALD RICAFRANCANo ratings yet
- AntifungalDocument7 pagesAntifungalKhor Chin PooNo ratings yet
- uk-spc-nexium-sachet-10mg-DRESS-update-GI 21 0012aDocument17 pagesuk-spc-nexium-sachet-10mg-DRESS-update-GI 21 0012aDeisy ClerkeNo ratings yet
- Adult: IV Nosocomial Pneumonia Empiric Therapy For Febrile Neutropenic Patients 4.5Document3 pagesAdult: IV Nosocomial Pneumonia Empiric Therapy For Febrile Neutropenic Patients 4.5Chris Denver BancaleNo ratings yet
- Paracetamol Package InsertDocument3 pagesParacetamol Package InsertDiane ApostolNo ratings yet
- STREPTOMYCIN MonographDocument3 pagesSTREPTOMYCIN Monographfayrouz fathiNo ratings yet
- Concise Guide to Clinical Dentistry: Common Prescriptions In Clinical DentistryFrom EverandConcise Guide to Clinical Dentistry: Common Prescriptions In Clinical DentistryNo ratings yet
- Critical Care Medications: Anti-Arrhythmics Study Guide: Critical Care EssentialsFrom EverandCritical Care Medications: Anti-Arrhythmics Study Guide: Critical Care EssentialsNo ratings yet
- Ulcerative Colitis, A Simple Guide To The Condition, Treatment And Related ConditionsFrom EverandUlcerative Colitis, A Simple Guide To The Condition, Treatment And Related ConditionsNo ratings yet
- Preeklamsia: Portofolio Kasus EmergencyDocument1 pagePreeklamsia: Portofolio Kasus EmergencyBetari DhiraNo ratings yet
- Refrensi: Implications For The Assessment of Hepatic Encephalopathy. Hepatology 50:2014Document1 pageRefrensi: Implications For The Assessment of Hepatic Encephalopathy. Hepatology 50:2014Betari DhiraNo ratings yet
- Journal NeurologiDocument9 pagesJournal NeurologiBetari DhiraNo ratings yet
- Journal NeuroDocument6 pagesJournal NeuroBetari DhiraNo ratings yet
- Presentasi Journal ReadingDocument8 pagesPresentasi Journal ReadingBetari DhiraNo ratings yet
- A Histeria - Teoria e Clínica PsicanalíticaDocument653 pagesA Histeria - Teoria e Clínica PsicanalíticaDaniel BraunaNo ratings yet
- Position Paper Martial LawDocument3 pagesPosition Paper Martial LawLeoncio BocoNo ratings yet
- The Victim's Autopsy ReportDocument2 pagesThe Victim's Autopsy ReportShan KNo ratings yet
- CHEM 101 Chapter 2Document78 pagesCHEM 101 Chapter 2mikayla sirovatkaNo ratings yet
- In Re SantiagoDocument2 pagesIn Re SantiagoKing BadongNo ratings yet
- Annotated BibliographyDocument4 pagesAnnotated Bibliographyapi-302549909No ratings yet
- ATPAR ReviewerDocument25 pagesATPAR ReviewerJohn Paul BuliyatNo ratings yet
- Jamer Module 3 Foreignization and DomesticationDocument5 pagesJamer Module 3 Foreignization and DomesticationRenzo JamerNo ratings yet
- Effect of IBA and NAA With or Without GA Treatment On Rooting Attributes of Hard Wood Stem Cuttings of Pomegranate (Punica Granatum L.)Document5 pagesEffect of IBA and NAA With or Without GA Treatment On Rooting Attributes of Hard Wood Stem Cuttings of Pomegranate (Punica Granatum L.)warlord_ckNo ratings yet
- Indian Feminism - Class, Gendera & Identity in Medieval AgesDocument33 pagesIndian Feminism - Class, Gendera & Identity in Medieval AgesSougata PurkayasthaNo ratings yet
- Ariston As 600 V DryerDocument40 pagesAriston As 600 V DryermmvdlpNo ratings yet
- Repair Appx V3Document18 pagesRepair Appx V3soniaNo ratings yet
- Eslprintables 2009810153647888645279Document1 pageEslprintables 2009810153647888645279Mathéo DE OLIVEIRANo ratings yet
- Book Project FinalDocument12 pagesBook Project FinalAuguste RiedlNo ratings yet
- TAX Calalang v. LorenzoDocument3 pagesTAX Calalang v. LorenzoAnathea CadagatNo ratings yet
- CH 6 Properties of Lasers in Introduction To OpticsDocument34 pagesCH 6 Properties of Lasers in Introduction To OpticsmoatazNo ratings yet
- Psychoanalysis: ArticleDocument21 pagesPsychoanalysis: ArticleAqsa ParveenNo ratings yet
- RHPA46 FreeDocument5 pagesRHPA46 Freeheyimdee5No ratings yet
- Research in Organizational Behavior: Sabine SonnentagDocument17 pagesResearch in Organizational Behavior: Sabine SonnentagBobby DNo ratings yet
- Gas Supply Agreement 148393.1Document5 pagesGas Supply Agreement 148393.1waking_days100% (1)
- AP Biology Syllabus 2009-2010Document10 pagesAP Biology Syllabus 2009-2010yulianaholicNo ratings yet
- TM I RubenDocument165 pagesTM I RubenMark Kevin DaitolNo ratings yet
- M-Sand in Tamil NaduDocument9 pagesM-Sand in Tamil Nadurameshkanu1No ratings yet
- TarzanDocument2 pagesTarzanmaris quilantangNo ratings yet
- Big Data Insurance Case Study PDFDocument2 pagesBig Data Insurance Case Study PDFVivek SaahilNo ratings yet
- The Role of Majority and Minority Language Input in The Early Development of A Bilingual VocabularyDocument15 pagesThe Role of Majority and Minority Language Input in The Early Development of A Bilingual VocabularyPoly45No ratings yet
- 723PLUS Digital Control - WoodwardDocument40 pages723PLUS Digital Control - WoodwardMichael TanNo ratings yet