Professional Documents
Culture Documents
1996 - M Bonten - AssessmentofgastricacidityinintensivecarepatientsI (Retrieved 2016-12-17)
1996 - M Bonten - AssessmentofgastricacidityinintensivecarepatientsI (Retrieved 2016-12-17)
Uploaded by
sdasdadOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
1996 - M Bonten - AssessmentofgastricacidityinintensivecarepatientsI (Retrieved 2016-12-17)
1996 - M Bonten - AssessmentofgastricacidityinintensivecarepatientsI (Retrieved 2016-12-17)
Uploaded by
sdasdadCopyright:
Available Formats
Intensive Care Med (1996) 22:220 225
(() Springer-Verlag 1996
M. J. M. Bonten
C. A. Gaillard
R. W. Stockbriigger
F. H. van Tiel
S. van der Geest
E. E. Stobberingh
Received: 14 June 1994
Accepted: 5 April 1995
This study was made possible by a grant
(28-2125) from the Praevention Foundation
M.J.M. Bonten (15N) 9R.W. Stockbriigger
S. van der Geest
Department of Internal Medicine,
University Hospital Maastricht,
P.O. Box 5800 NL-6202 AZ Maastricht,
The Netherlands
C.A. Gaillard
Department of Internal Medicine,
Eemland Hospital, Amersfoort, The
Netherlands
F.H. van Tiel. E.E. Stobberingh
Department of Medical Microbiology,
University Hospital Maastricht,
The Netherlands
ORIGINAL
Assessment of gastric acidity in intensive
care patients: intermittent pH registration
cannot replace continuous pH monitoring
Abstract Objective: To test the accuracy of colour-scaled indicator
papers to measure p H values and to
study the correlation between this
m e t h o d of measuring gastric juice
p H once daily and 24-h continuous
intragastric pH monitoring in intensive care patients.
Desion: The accuracy of indicator
papers was tested in the l a b o r a t o r y
using colourless solutions and aspirated gastric juice and was then
verified with a l a b o r a t o r y p H meter.
Continuous intragastric p H
monitoring was performed in mechanically ventilated ICU patients.
Percentages of time with a p H value
< 3.0 and median p H values by
24-h continuous intragastric p H
monitoring were c o m p a r e d to p H
values measured once daily with
indicator paper.
Setting: A mixed ICU.
Patients." A total of 150 measurements were taken by continuous p H
monitoring in 91 mechanically ventilated ICU patients.
Measurements and results: The correlation between the p H measured
with the indicator paper and subsequently verified with a l a b o r a t o r y
p H meter in colourless solutions
was 0.96 [-regression coefficient
(RC) 0.98, 95% confidence interval
(CI) 0.91-1.05]. Measured in gastric
juice it was 0.95 (RC 0.95, 95% CI
0.88-1.01). The correlation between
median p H values, determined with
24-h continuous intragastric p H
monitoring, and values measured
with indicator papers was 0.39 (RC
0.43, 95% CI 0.26-0.59). The mean
difference in pH, as determined by
the analysis of Bland and Altman
[22], was 0.9 with a SD of 4.7. The
correlation between the percentage
of time with p H < 3.0, as obtained
with continuous registration, and
median gastric p H values (also obtained with continuous registration)
was - 0.94 (RC - 0.06, 95% CI
- 0.06- - 0.05); the correlation between the time and gastric p H
values (measured with indicator paper) was - 0.40 (RC - 0.02, 95%
CI - 0.03 - 0.02).
Conclusion." The colour-scaled indicator paper is an accurate m e t h o d
of measuring p H values, but there is
a p o o r correlation between gastric
p H values measured once daily and
a total measurement derived from
24-h continuous intragastric p H
monitoring. Changes in intragastric
p H values cannot be accurately
studied when measuring acidity
once daily. The influence of various
treatment regimens on intragastric
acidity in relation to the development of gastric colonization and
221
nosocomial pneumonia should be
investigated either with continuous
intragastric monitoring or with
frequent measurements in aspirated
gastric juice.
Key words Pneumonia 9 Gastric
p H . Colonization" Stress ulcer
prophylaxis. Nutrition
Introduction
Patients and methods
Gastric colonization has been assumed to be important in the pathogenesis of nosocomial pneumonia
in mechanically ventilated ICU patients [1,2].
Bacterial overgrowth in the stomach is facilitated by
alkalinization of the intragastric environment [3-5].
Therefore, maintainance of intragastric acidity has
been used to prevent gastric colonization and pneumonia in mechanically ventilated ICU patients [6 13].
In all but one study the effect of stress ulcer prophylactic agents and enteral feeding on intragastric pH was
determined with colour-scaled indicator papers in
aspirated gastric juice samples [6 13]. Measurements were performed intermittently, in some studies
once daily [10,12 14] or with an unknown frequency [6].
It is, however, questionable whether results obtained by randomly measured intragastric pH values
with indicator papers are valid for definite conclusions
regarding modulation of intragastric acidity. In the
first place, physiologic diurnal changes of intragastric
acidity probably are not registered when samples
are obtained infrequently. Secondly, two studies
demonstrated poor accuracy of indicator papers,
when compared to values concomitantly obtained with
pH electrodes [15, 16]. The latter observations
are in contrast to those described by Levine and
coworkers, who found a good correlation between spot
measurements obtained by litmus paper and those obtained by an intragastric antimony pH probe [17].
However, both pitfalls can be overcome by using
computerized continuous intragastric pH measurement with intraluminal electrodes. In other research
settings this method has become an established technique because of its high accuracy and reproducibility
[18 21].
We determined the accuracy of colour-scaled
indicator papers for the determination of pH in
gastric samples of intensive care patients and compared
the results of this method with a summary pH
measure obtained by continuous intragastric pH
monitoring.
Accuracy of indicator paper
The accuracy of colour-scaled indicator papers was studied in two in
vitro experiments. In the first experiment 60 measurements with
indicator paper (Schleicher & Schiill, range: 1.0 12.0 with 23 steps of
0.5) were performed using a blind test in colourless solutions with
pH values ranging from pH 1.0 to 7.5. As a standard, the pH values
of these solutions were verified with a laboratory pH meter (PHM82
Standard pH Meter, Radiometer a/s Copenhagen, Denmark). To
account for factors that possibly affect the accuracy of measurements with pH paper in gastric samples, in a second experiment the
pH values of 93 random and unprocessed gastric samples were
determined in parallel with a laboratory pH meter and with indicator paper. In all cases measurements with pH paper were taken
first and all laboratory measurements were performed by the same
technician.
Patients
For the in vivo comparison of random and continuous pH monitoring, 91 pa/ients admitted to the ICU who needed mechanical ventilalion were prospectively enrolled in the study. All patients were
endotrachcally intubatcd, had a nasogaslric tube, and received
either sucralfatc or antacids l\)r stress ulcer prophylaxis.
The protocol was approved by lhe institutional review board of
the hospital, and inl\)rmed consent was obtained fi-om all participants, or if this was not possible because of the clinical condition,
consent was obtained from a representative of the family.
lntragastric pH recording
A plI stomach probe with a glass electrode tip (LoT 440. lngold
AG, U r d o f f Switzerland) was transnasally positioned m the stomach with the tip situated approximately 10cm below the cardia.
The position of Ihe tip was verilied by radiography. The dislance
from tip to nostrils was kept constant lk)r the entire recording
period. Recording of intragastric acidity was per%rlned for 24 h and
pit values were registered every 4 s. The plt data were stored in
a I)igitrapper Mk Ill (Syneclics Medical, Alphen aan den Rijm The
Netherlands) and after the procedure transferred to a personal
computer. Analysis was perl\mncd using Esophogram software
(Gastrosoft Inc., Synectics Medical). The median value and the
percentage of time with a pH <3.0 during the recording period were
calculated from all measurements. Electrodes and recorders were
calibrated at 20 C using commercial buffer solutions at pH 7.0 and
1.3 (lngold AG), before starting every cxperiment and rcpcated
af|erwards.
222
pH recording of gastric samples
Gastric juice samples of the patients were obtained routinely once
daily at 8.00 a.m. by aspirating gastric fluid into a syringe. Thereafter, pH values were determined with indicator paper. All measurements of pH values with indicator papers were performed by the
same technician, who was unaware of the results of the continuous
intragastric pH measurements.
Data analysis
Because of the non-parametric data, the median pH and the percentage of recording time with a pH value < 3.0 were calculated from
each continuous intragastric pH measurement. The pH value of 3.0
was arbitrarily chosen. The mean pH values from continuous pH
monitoring and the pH values obtained by colour-scaled pH papers
were analysed by the Bland and Altman method [221 and by
calculating the correlation coefficient (r value) and the 95% confidence interval of the regression line.
Results
Accuracy of indicator papers
In the two laboratory experiments good correlations
were observed between pH values measured with indicator papers and those determined with a laboratory
pH meter. The correlation coefficient between the indicator paper method and the pH values of colourless
solutions was 0.96 (RC = 0.98, 95% CI 0.91-1.05). The
correlation coefficient of pH values of gastric samples,
measured in the laboratory with indicator papers and
verified with a laboratory pH meter, was 0.95
(RC -- 0.95, 95% CI 0.88 1.01).
from 24-h intragastric monitoring are listed in Table 1.
The mean pH value of aspirated gastric samples obtained with indicator paper is also listed in Table 1. The
average pH value determined from median values of
continuous intragastric measurements was lower than
the mean pH value, as determined once daily with
indicator paper (4.4 _+ 2.2 SD vs 5.3 + 2.0).
Median gastric pH values and percentages of time
with gastric pH values below 3.0, both obtained with
continuous intragastric pH measurement, are plotted
Table 1 Results of continuous intragastric pH measurements and
the indicator paper technique
Intragastric
pH monitoring
No. of recordings
150"
(91 patients)
Mean of pH values _+ SD
4.4 _+ 2.2 b
Range
0.5 8.0
Mean % of time with pH < 3.0 + SD 34.2 _+ 34.9
Range
0-100
No. of recordings with pH < 3.0
46 (31%)c
100
The average of the median pH values and the average
percentage of time with pH values below 3.0 obtained
5.3 2.0
1.0-8.5
24 (]6%)
-~
eeOo
9
e O
80
4,
Iv)
V
O.
a~
60
",'t 9
9
40
7 ~
W O
*o
20
0
I
0
Comparison of once-daily measurements and
continuous intragastric pH monitoring
150
Number of Iong-term measurements performed
b Mean of median values
~Median pH value < 3.0
Patients
In total, 150 episodes of intragastric pH monitoring
were performed in 91 patients. The mean age (_+ SD) of
the patients was 61 _+ 18 years with a range from 19 to
88 years and a mean APACHE II score on admission of
21 (SD = 8) with a range from 6 to 40. Thirty-seven
patients were surgical, 22 medical, 15 pulmonary,
9 trauma and 8 neurological. All patients were mechanically ventilated. In 46 patients more than one episode
of 24-h intragastric pH monitoring was recorded (2
episodes n = 36, 3 episodes n = 7 and 4 episodes n = 3).
Indicator
paper
P
2
4
Median
I
6
I
8
I
10
ci p H
Fig. 1 Correlation between median pH values (median ci pH, xaxis) and the percentage of time with pH values <3.0 (% pH <3,
y-axis), both obtained by continuous intragastric pH monitoring,
r = - 0.9425
223
100
10
t
80
@
9
I'@
1'3
V
60
'
"r
a.
"I"
a.
00
@@@
@@ @
41
40
0
O
l o l : l . , .
9
@
@
9
9
9
@@
10
10
in Fig. 1 (r =
0.94, R C 0.06, 95% CI 0.060.05). In contrast, the correlation between the gastric
pH values, obtained once daily with indicator paper,
and the percentages of time with pH values below 3.0
was only - 0 . 4 0 , ( R C - - 0 . 0 2 ,
95% C l - 0 . 0 3 0.02, Fig. 2).
The median pH values from continuous intragastric
recordings and the corresponding pH value of the indicator paper method are plotted in Fig. 3. Considerable
differences between the two methods were observed.
The analysis according to Bland and Altman [22] is
shown in Fig. 4: The averages ofpH data obtained with
the two methods are plotted against their differences.
The average difference between the two methods was
0.9, S D
OO0
Median ci pH
pH
Fig. 2 Correlation between p H values obtained by indicator papers
(stick pH, x-axis) a n d the percentage of time with pH values < 3 . 0
obtained by c o n t i n u o u s intragastric p H m o n i t o r i n g (% p H < 3 ,
y-axis), r
0.3998
09
410
0~
Ore'
Stick
@@
9 8 oe 9 9
9
aid
W,@O
9
,.
qlNP@ 9
m'
0@
0004U,@
9
9 0 09
I(/I
20
GI,
qn,@
Q,
o f 4.7.
Fig. 3 C o r r e l a t i o n between m e d i a n p H values as o b t a i n e d with 24-h
intragastric m o n i t o r i n g (median ci pH, x-axis) a n d p H wdues as
obtained with indicator papers (stick pH, y-axis), r = 0.3920
"~"
6
o9
........
7 ...................
"i-
9~
....
ta - 2
09
/. 9
-4
E:Z
-" , ,~
;0 9
-0.9
-.
9
-8
00 9 9
t.l.I
ta-
-6
Ii Ib
-----
...;.
*9
9149 9
3.8
. . . . . . . .
I
2
'f-~iP-
- - -* . . . . . . . . . . . . . .
I
4
I
6
I
8
5.6
I
10
Mean (ci pH and stick pH)
Discussion
The main feature of the present study is that there is
a poor correlation between the results of gastric pH
values obtained once daily with colour-scaled indicator
paper and summary pH measures obtained with continuous 24-h intragastric pH monitoring. It seems unlikely that the difference between the two methods was
caused by inaccuracies in either one. Continuous
intragastric pH measurements have been validated
Fig. 4 D i s a g r e e m e n t between pH paper (stick pH) and c o n t i n u o u s
pH m o n i t o r i n g (ci pH) values as assessed by the difference between
m e t h o d s ( c o n t i n u o u s m o n i t o r i n g m i n u s pH paper). T h e + 2 SD of
thc diffcrences range is 9.4 pH units
repeatedly [16], and in this study calibration of the
electrodes was performed before each measurement
and verified afterwards. Moreover, the indicator
paper method showed a good correlation with
measurements performed with a laboratory pH meter,
224
both in colourless solutions and in gastric juice. This is in
line with observations made by others [17, 23], although
two other studies have demonstrated a poor accuracy
of the indicator paper method [15, 16]. In one study the
indicator paper method had a sensitivity of 67% and
a specificity of 95% for determining pH values > 4,
taking electrode measurements as the gold standard.
The authors suggested that the inhomogeneous mixture of gastric acid, mucus, bile pigments and antacids
interfered with the accurate measurement of pH values
with the indicator paper [16]. Caballero et al. also
demonstrated poor accuracy of the indicator paper
method, as compared to a standard laboratory meter in
a clinical setting [15]. However, in that study results
were obtained from different hospitals [15]. The fact
that all pH measurements with indicator papers in the
present study were performed by the same technician
might explain the accuracy observed in this study.
It appears that measurements of pH values in aspirated gastric samples performed once daily do not
accurately reflect 24-h pH values in the intragastric
milieu. Our results are in line with the observations
made by others, indicating a good correlation when pH
measurements are performed half-hourly or even hourly [19 21,24]. The need for frequent assessment of
intragastric acidity was also stressed by investigators
who studied the efficacy of antacids to prevent gastrointestinal bleeding in critically ill patients [25, 26].
In these studies it was emphasized that intragastric
acidity should be checked at least every 2 h.
Several studies in which incidental pH measurements of gastric juice were used have addressed the
effect of modifying gastric juice pH on gastric bacterial
colonization and the development of nosocomial pneumonia (Table 2). As demonstrated in Table 2, significant differences in pH values for the different stress
Table 2 F r e q u e n c i e s a n d results
of p H m e a s u r e m e n t s in
aspirated gastric juice u s i n g
colour-scaled indicator paper
Author
D r i k s et al. [6]
T r y b a [7]
K a p p s t e i n et al. [8]
E d d l e s t o n et al. [9]
S i m m s et al. [11]
P r o d ' h o r n et al. [12] e
ulcer prophylactic agents were observed in all studies
[6-9, 11, 12]. However, the frequency of measurements
ranged from 1 to 12 times per day. In the study of Driks
et al. 805 gastric samples were obtained from 130
patients with a mean ICU stay of 10 days, which
implies that gastric acidity was measured every second
day [6]. In addition to the studies listed in Table 2, the
effects of modulation of intragastric aciditiy by gastric
feeding were addressed in three other studies [10, 13, 14].
Heyland et al. compared the influence of acidified gastric feeding (pH 3.5) as compared to nonacidified feeding (pH 6.5) administered either in the stomach or the
duodenum, while Lee et al. and Spilker et al. compared
the effects of continuously or intermittently administered gastric feeding on intragastric acidity [10, 13]. In
these three studies gastric pH was measured once daily
with colour-scaled papers in aspirated gastric juice.
Despite the fact that the mean difference between
once daily and continuous measurements was less than
one pH unit, we feel that the results regarding intragastric acidity from studies where pH values were not
measured continuously should be interpreted with caution. Whether this is a clinically important difference
resulting in different rates of colonization and pneumonia remains to be established.
Computerized continuous intragastric monitoring
is expensive and may not be available to all investigators. Moreover, computerized intragastric pH monitoring may not be feasible in patients who remain in
a study protocol for weeks to months. Therefore, the
minimal number of measurements in a 24-h period that
is required to determine accurately long-term intragastric acidity with indicator paper in aspirated gastric
juice should be established by comparing this method
with different frequencies of measurement and computerized intragastric monitoring.
Frequency
of m e a s u r e m e n t
(per day)
P r o p o r t i o n of samples
with P H < 4.0 (%)
Test C o n t r o l s
Unknown
3
_< 6
4
12
47.9 a 25.3 b (p < 0.001)
46.5 a t0.4 c (p < 0.01)
1.3-1.5
20.0 a 11.1 c
9.4 a (p > 0.05)
46.7 a 3.9 c
10.9 d
Test patients received sucralfate
b C o n t r o l patients received antacids a n d / o r H 2 a n t a g o n i s t s
c C o n t r o l patients received antacids
a C o n t r o l patients received H2 a n t a g o n i s t
e Values are expressed in m e d i a n p H per patient
Mean pH
Test C o n t r o l s
4.34 ~'
4.26 a
4.73 a
4.30 a
4.84 d
5.50 d
5.55 ~
5.06 d
7.10 c
6.27 d
(P
(P
(P
(P
<
<
<
>
0.05)
0.01)
0.01)
0.05)
(P < 0.0001)
225
Despite the excellent accuracy of indicator papers,
as determined in the present study and by others
[17], we conclude that changes in intragastri
pH values cannot be accurately studied when measuring acidity only once daily or even less frequently.
The correlation between modulation of intragastric
acidity by different treatment regimens and the subsequent development of gastric bacterial colonization
and nosocomial pneumonia should be re-evaluated using either continuous intragastric pH monitoring or
a frequent measurement of pH in samples of aspirated
gastric juice.
References
1. Heyland D, Mandell LA (1992) Gastric
colonization by gram-negative bacilli
and nosocomial pneumonia in the
intensive care unit patients: evidence for
causation. Chest 101:187 193
2. Tryba M (1991) The gastropulmonary
route of infection fact or fiction? Am
J Med 91 [Suppl 2A]: 135 146
3. Du Moulin, Paterson DG, HedleyWhite J, Libson A (1982) Aspiration of
gastric bacteria in antacid-treated patients: a frequent cause of postoperative
colonisation of the airway. Lancet:
242 245
4. Hillman KM, Riordan T, O'Farrel SM,
Tabaqchal S (19821 Colonization of
gastric contents in critically ill patients.
Crit Care Med 10:444 447
5. Garvey BM, McCambley JA, Tnxeu DV
(1989) Effects of gastric colonization on
bacterial colonizalion in critically ill
patients. Crit Carc Med 17:211 216
6. l)riks MR. Craven I)E, Celli BR, Manning M. Burkc RA. Garvin GM, Kunchcs
I.M~ Farber HW, Wedel SA, McCabc
WR (1987) Nosocomial pneulnonia
in intubated patients given sucralfate as
compared with antacids of histamine
type 2 blockers. N Engl J Med 317:
1376 1382
7. Tryba M (1987) Risk of acute stress and
nosocomial pneumonia in ventilated intensive care patients: sucralfate versus
antacids. Am J Med 83 [Suppl 3B]:
117 124
8. Kappstein 1, Schulgen G. Friedrich T,
ttellinger P, Geigcr K, Daschner FI)
( 1991 ) Incidence of pneumonia in mechanically ventilated patients treated with
sucralfalc or cimelidine as prophylaxis
for stress bleeding: bacterial colonization of the slomach. Am J Med 91
[Suppl2A]: 125S 131S
9. Eddleston JM, Vohra A, Sco(t P, Tooth
JA. Pearson RC, McCloy RF. Morton
AK, l)oran BH (1991) A comparison of
the frequency of stress ulceration and
secondary pneumonia in sucralfate- or
ranitidinc-trcated
intensive
care
patients. Crit Care Med 19:1491 1496
10. Lee B, Chang RWS, Jacobs S (1990)
Intermittent
nasogastric
feeding:
a simple and effective method to reduce
pneumonia among ventilated ICU
patients. Clin Intensive Care 1 : 100 102
11. Simms HH, DeMaria E, McDonald L,
Peterson D, Robinson A, Burchard K W
(1991) Role of gastric colonization in the
development of pneumonia in critically
ill trauma patients: results of a prospectivc randomized trial. J Trauma
31:531 537
12. Prod'horn G, Leuenberger P, Koerter J,
Blum A. Chiolero R, Schaller MD, Perret C, Spinnler O. Blondel J, Siegrist H,
Saghali L, Blanc D, Francioli P (1994)
Nosocomial p n e u m o n i a - i n mechanically ventilated patients receiving antacid, ranitidine, or sucralf~te as prophylaxis for stress nicer. Ann Intern Med
120:653 662
13. Spitker CA. llinthron DR. Pmglelon
SK (1993) lnternri/tcnt enleral l~eding
and gastric colonization in critically ill
patients (abstract). Am Rev Respir Dis
147:A200
14. Hcyland D, Bradley C, Mandell LA
(1992) Effcc/ of acidi/icd enteral li:edings
on gastric colonization in the critically
ill patient. Crit Care Mcd 20:1388 1394
15. Caballero GA, Ausmau RK. Quebbeman EJ. Schultc WJ, Lin L (1990)
Gastric secretion pH measurement:
whal you see is not what you get! Crit
Care Med 18:396 399
16. Dobkin El), Valcour A. McCloskey CR,
Allen L. Kambe JC, Gleason E, Orlando
R 111, Bcrgcr R~ Yeslon NS (1990) Does
ptt paper accurately reflect gastric pH?
Crit Care Med 18:985 988
17. Levine RL, Fromln RE, Mojlahedzadeh
M, Baghaie AA, Opekun AR (1994)
Eqniwdence of lilmus paper and intragastric pH probes l\)r intragastric pH
monitoring in the intensive care unit.
Crit Care Med 22:945 948
18. Fimlnel C J, Etienne A, Ciluffo T, cl al
(1985) Long-term ambulatory gastric
pH monitoring: validation of a new
method and effccl of H2-antagonists.
Gastroenterology 88:1842 1851
19. Savarino V, Mela GS, Scalabrini P,
Magnolia MR, Percario G, Di Timoteo
E, Celle G (1987) 24-h Comparison
between pH values of continuous intraluminal recording and simultaneous
gastric aspiration. Scand J Gastroenterol 22:135 140
20. Anderson J, Naesdal J, Str/~m (1988)
Identical 24-hour gastric pH profiles
when using intragastric antimony or
glass electrodes or aspirated gastric
21.
22.
23.
24.
25.
26.
juice. Scand J Gastroenterol 23:
375 379
Savarino V, Mela (IS, Zentilin P, Magnolia MR, Scalabrini P, Valle F, Moretti
M, Bonif:/cino G, Celle G (1989) Gastric
aspiration versus antimony and glass
pH electrodes. A simultaneous con>
parative in vivo study. Scand J Gastroenterol 24:434 439
ISland J M, Airman DG (1986) Statislical
methods for assessing agrccmcn/ between two me/hods of clinical measurement. Lancet 1:307
Mcincrs D. C/ift S. Kaminski D (1982)
Ewdualion of various techniques to
monitor intragastric pH. Arch Surg 117:
288 291
Albin M, Friedlos .1, Hillman K (1985)
Continuous intragastric pH measuremenl in lhe critically ill and treatment
with parenteral ranitidine. Intensive
Care Med I1:295 299
Hastings PR, Skillman J.l. Bushnell LS,
Silen W (1978) Anlacid litration in the
prevcnlion of acute gastrointestinal
bleeding. A controlled, randomized trial
in 100 critically ill patients. N Engl
J Med 298:1041 1045
Priebe IlL Skillman J J, Bushnell LS,
Long PC, Silen W (1980) Antacid versus
cimetidine in preventing acute gastrointestinal bleeding. A randomized trial in
75 critically ill patients. N Engl J Med
302:426 430
You might also like
- Risk Assessment Asphalt WorksDocument7 pagesRisk Assessment Asphalt Workskannanjaduzz100% (1)
- Legal Medicine Compiled CasesDocument194 pagesLegal Medicine Compiled CasesKarmaranthNo ratings yet
- Ebola Class 12 Biology Investigatory ProjectDocument15 pagesEbola Class 12 Biology Investigatory ProjectVaijal PatelNo ratings yet
- Vasectomy SummaryDocument12 pagesVasectomy SummaryKevin ZornNo ratings yet
- University College of DublinDocument2 pagesUniversity College of DublinDawitNo ratings yet
- Anticolinergice Si BRGEDocument6 pagesAnticolinergice Si BRGEZahan LorenaNo ratings yet
- AbdomenDocument9 pagesAbdomenjose salgadoNo ratings yet
- Aliment Pharmacol Ther - 2001 - Fackler - Ambulatory Gastric PH Monitoring Proper Probe Placement and Normal ValuesDocument8 pagesAliment Pharmacol Ther - 2001 - Fackler - Ambulatory Gastric PH Monitoring Proper Probe Placement and Normal ValuesSofia CorreaNo ratings yet
- Literatur - Rohs, Et - Al. Esomeprazole Compared To Other PPIsDocument9 pagesLiteratur - Rohs, Et - Al. Esomeprazole Compared To Other PPIsChristine LilyanaNo ratings yet
- PoiafnewjDocument2 pagesPoiafnewjrekaNo ratings yet
- Comparison of Three Methods For Measurement of Blood Hba1c As To ReliabilityDocument5 pagesComparison of Three Methods For Measurement of Blood Hba1c As To ReliabilityRakesh BagrajiNo ratings yet
- Helicobacter Pylori Eradication: Changes in Gastric Acid Secretion Assayed by Endoscopic Gastrin Test Before and AfterDocument7 pagesHelicobacter Pylori Eradication: Changes in Gastric Acid Secretion Assayed by Endoscopic Gastrin Test Before and AfterFariz NurNo ratings yet
- Wang 2012Document7 pagesWang 2012priskaNo ratings yet
- The Laryngoscope - 2019 - Weitzendorfer - Pepsin and Oropharyngeal PH Monitoring To Diagnose Patients WithDocument7 pagesThe Laryngoscope - 2019 - Weitzendorfer - Pepsin and Oropharyngeal PH Monitoring To Diagnose Patients WithfelitaNo ratings yet
- Relative Potency of Proton-Pump Inhibitors-ComparisonDocument13 pagesRelative Potency of Proton-Pump Inhibitors-ComparisonTonii SoberanisNo ratings yet
- Validacion de AgaDocument7 pagesValidacion de AgaSATURNONo ratings yet
- The Effectiveness of Sputum PH Analysis in The Prediction of Response To Therapy in Patients With Pulmonary TuberculosisDocument1 pageThe Effectiveness of Sputum PH Analysis in The Prediction of Response To Therapy in Patients With Pulmonary Tuberculosislouie john abilaNo ratings yet
- Salivary Microbial and Nonmicrobial Parameters in Children With Fixed Orthodontic AppliancesDocument6 pagesSalivary Microbial and Nonmicrobial Parameters in Children With Fixed Orthodontic AppliancesRavanth KumarNo ratings yet
- Inter DHL 5Document3 pagesInter DHL 5supi4nl4mpuukNo ratings yet
- EshofagusDocument452 pagesEshofagusAga Bagas D'jailNo ratings yet
- Ambulatory Esophageal MonitoringDocument25 pagesAmbulatory Esophageal MonitoringKaty BebsNo ratings yet
- Effect of An Antireflux Bed Wedge On Gastro Esophageal Reflux Symptoms and Acid Reflux 1467Document5 pagesEffect of An Antireflux Bed Wedge On Gastro Esophageal Reflux Symptoms and Acid Reflux 1467abel assefaNo ratings yet
- Anaesthesia, Pain & Intensive CareDocument5 pagesAnaesthesia, Pain & Intensive CareFeri FadillahNo ratings yet
- Proteína C Reactiva en Suero Como Complemento de La Identificación de Derrames Paraneumónicos ComplicadosDocument5 pagesProteína C Reactiva en Suero Como Complemento de La Identificación de Derrames Paraneumónicos ComplicadosLulú García VargasNo ratings yet
- Pylori BiogaiaDocument8 pagesPylori BiogaiaAlejandro NavarreteNo ratings yet
- Diagnostic Accuracy of Xpert MTB/RIF On Bronchoscopy Specimens in Patients With Suspected Pulmonary TuberculosisDocument6 pagesDiagnostic Accuracy of Xpert MTB/RIF On Bronchoscopy Specimens in Patients With Suspected Pulmonary TuberculosisMARTIN FRANKLIN HUAYANCA HUANCAHUARENo ratings yet
- Laryngopharyngeal Reflux: A Review of New Diagnostic MethodsDocument7 pagesLaryngopharyngeal Reflux: A Review of New Diagnostic MethodsEve MacíasNo ratings yet
- Sepsis 2019Document12 pagesSepsis 2019EviNo ratings yet
- Phphenylephrine Vs EphedrinerineDocument42 pagesPhphenylephrine Vs EphedrinerineDr.Deb Sanjay NagNo ratings yet
- A34 Loustaud Et Al 2008Document9 pagesA34 Loustaud Et Al 2008enzo22No ratings yet
- 10.2217@fmb 2019 0280Document8 pages10.2217@fmb 2019 0280Khoa DoNo ratings yet
- Actividad 2 Periodoncia Avanzada ElizabethDocument16 pagesActividad 2 Periodoncia Avanzada ElizabethElizabeth MartinezNo ratings yet
- Comparison of Quick and Owren Prothrombin Time With Regard To The Harmonisation of The International Normalised Ratio (INR) SystemDocument5 pagesComparison of Quick and Owren Prothrombin Time With Regard To The Harmonisation of The International Normalised Ratio (INR) SystemOngNo ratings yet
- Art:10.1186/s12876 014 0225 7Document6 pagesArt:10.1186/s12876 014 0225 7Silvestri PurbaNo ratings yet
- Detection of Hepatitis C Virus RNA in Saliva of Patients With Active Infection Not Associated With Periodontal or Liver Disease SeverityDocument7 pagesDetection of Hepatitis C Virus RNA in Saliva of Patients With Active Infection Not Associated With Periodontal or Liver Disease SeverityKiana TehraniNo ratings yet
- Infrared Comparison With Conventional Gravimetric and Titrimetric MethodsDocument4 pagesInfrared Comparison With Conventional Gravimetric and Titrimetric MethodsZil ArdiNo ratings yet
- 2010-Fasting For Haematological TestDocument6 pages2010-Fasting For Haematological Testpedro vargasNo ratings yet
- GadarDocument5 pagesGadarTiasfebriantiNo ratings yet
- Alumno: Martos Grau Cesar IvánDocument7 pagesAlumno: Martos Grau Cesar IvánIván MartosNo ratings yet
- Junal DispepsiaDocument6 pagesJunal DispepsiaJesryn Kaur DhillonNo ratings yet
- Esophageal Motility AnalyzersDocument21 pagesEsophageal Motility AnalyzersTwinny2001No ratings yet
- Effects of Dopamine, Norepinephrine and Dobutamine On Gastric Mucosal PH of Septic Shock PatientsDocument4 pagesEffects of Dopamine, Norepinephrine and Dobutamine On Gastric Mucosal PH of Septic Shock PatientsChiboyKrenzNo ratings yet
- The Use of Frequency Scale For The Symptoms of GERD in Assessment of Gastro-Oesophageal Re Ex Symptoms in AsthmaDocument5 pagesThe Use of Frequency Scale For The Symptoms of GERD in Assessment of Gastro-Oesophageal Re Ex Symptoms in AsthmaShahnaz RizkaNo ratings yet
- 27 Jurnal BaruDocument4 pages27 Jurnal Baruaulia sufarnapNo ratings yet
- Sen 2006Document5 pagesSen 2006ROBINSON ELIOTT GONZ�LEZ P�EZNo ratings yet
- Nutrition Parameters As Hemodialysis Adequacy Markers: Original ArticleDocument5 pagesNutrition Parameters As Hemodialysis Adequacy Markers: Original ArticleMariska Widya WNo ratings yet
- G.Chemistry Exp.7Document5 pagesG.Chemistry Exp.7sayar.emre888No ratings yet
- Carraro 2013 RSBMTV 46 N 2 P 161Document5 pagesCarraro 2013 RSBMTV 46 N 2 P 161Emerson CarraroNo ratings yet
- A Quantitative Review and Meta-Models of The Variability and Factors Affecting Oral Drugs Absorption-Part I Gastrointestinal PHDocument13 pagesA Quantitative Review and Meta-Models of The Variability and Factors Affecting Oral Drugs Absorption-Part I Gastrointestinal PHAdiel Esteban SbNo ratings yet
- Total Error KolesterolDocument15 pagesTotal Error KolesterolNadia Nur fadilahNo ratings yet
- Research ArticleDocument9 pagesResearch Articleade muchlasNo ratings yet
- Grila de Evaluare A Unui Articol StiintificDocument4 pagesGrila de Evaluare A Unui Articol StiintificAndrei DamaschinNo ratings yet
- 5.J Clin Pathol 2012 Salinas 928 33Document7 pages5.J Clin Pathol 2012 Salinas 928 33Nofiyanty NicolasNo ratings yet
- Relative Potency of Proton-Pump Inhibitors of Effects On Intragastric PHDocument13 pagesRelative Potency of Proton-Pump Inhibitors of Effects On Intragastric PHbbmguyNo ratings yet
- Jurnal THT FiksDocument6 pagesJurnal THT FiksverlitautamiNo ratings yet
- Prediction of Outcome Following Paraquat Poisoning by Arterial Lactate Concentration Time DataDocument5 pagesPrediction of Outcome Following Paraquat Poisoning by Arterial Lactate Concentration Time DataLeslie StephensNo ratings yet
- 2 Heartburn PDFDocument8 pages2 Heartburn PDFjeyaprakash jayaramanNo ratings yet
- Administration of Mucolytic Solution Before Upper Endoscopy - Double-Blind, Monocentric, Randomized StudyDocument5 pagesAdministration of Mucolytic Solution Before Upper Endoscopy - Double-Blind, Monocentric, Randomized StudyginaNo ratings yet
- Assessment of Oral Malodor: A Comparison of The Organoleptic Method With Sulfide MonitoringDocument9 pagesAssessment of Oral Malodor: A Comparison of The Organoleptic Method With Sulfide MonitoringMarian Si Teofana HasnaNo ratings yet
- LkjkusteiDocument8 pagesLkjkusteiPeriyasami GovindasamyNo ratings yet
- Ijcm 2014012415343834 PDFDocument5 pagesIjcm 2014012415343834 PDFangela_karenina_1No ratings yet
- Citation 11084227Document1 pageCitation 11084227Adiyanto DidietNo ratings yet
- Factors Affecting The Prevalence of Gastro-Oesophageal Reflux in Childhood Corrosive Oesophageal StricturesDocument6 pagesFactors Affecting The Prevalence of Gastro-Oesophageal Reflux in Childhood Corrosive Oesophageal StricturesAlinaRellyyNo ratings yet
- Stricture EsofagealDocument11 pagesStricture EsofagealInes Camilla PutriNo ratings yet
- Complementary and Alternative Medical Lab Testing Part 5: GastrointestinalFrom EverandComplementary and Alternative Medical Lab Testing Part 5: GastrointestinalNo ratings yet
- Rakan NiagaDocument12 pagesRakan NiagaPahlawan NiagaNo ratings yet
- PUSINGDocument3 pagesPUSINGFritzel Pallon SusbillaNo ratings yet
- Australia Medical Carriage RequirementsDocument28 pagesAustralia Medical Carriage Requirementsdoğancan uzunNo ratings yet
- Pesticide Residues and MycotoxinsDocument42 pagesPesticide Residues and MycotoxinsRahul RajeshNo ratings yet
- No Timestamp Nama Lengkap Email Nomor Handphone OrganisasiDocument16 pagesNo Timestamp Nama Lengkap Email Nomor Handphone OrganisasiMeta WulandariNo ratings yet
- Lifebuoy Case AnalysisDocument3 pagesLifebuoy Case Analysisanon_659483030No ratings yet
- Investing in The Growing-Sleep-Health-EconomyDocument8 pagesInvesting in The Growing-Sleep-Health-EconomyZheyu ShanNo ratings yet
- Test Bank For Nursing A Concept Based Approach To Learning Volume II 3rd Edition 3rd EditionDocument93 pagesTest Bank For Nursing A Concept Based Approach To Learning Volume II 3rd Edition 3rd EditionLarry Cessor100% (34)
- Effects of Predisposing, Enabling, and Reinforcing Factors On Completeness of Child Immunization in Pamekasan, MaduraDocument13 pagesEffects of Predisposing, Enabling, and Reinforcing Factors On Completeness of Child Immunization in Pamekasan, MadurananaNo ratings yet
- Psychosocial Support For Parents of Extremely PretDocument13 pagesPsychosocial Support For Parents of Extremely PretDag AraNo ratings yet
- Patricia Benner Novice To ExpertDocument6 pagesPatricia Benner Novice To ExpertVien WhitlockNo ratings yet
- Medical Management Include Drug Therapy: Hydatidiform MoleDocument2 pagesMedical Management Include Drug Therapy: Hydatidiform MoleMaye ArugayNo ratings yet
- Donor Health Check For New and Returning DonorsDocument1 pageDonor Health Check For New and Returning DonorsGaoudam NatarajanNo ratings yet
- MystudyDocument5 pagesMystudyErica MarianeNo ratings yet
- FPCS-QI TOR - Guideline - Dr. NizamDocument13 pagesFPCS-QI TOR - Guideline - Dr. NizamSaidur Rahman MilonNo ratings yet
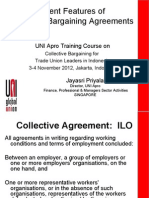
- Salient Features of CBADocument15 pagesSalient Features of CBAalipansNo ratings yet
- Interpretation of Clinical Biochemical TestsDocument24 pagesInterpretation of Clinical Biochemical TestsaddwrNo ratings yet
- Violence Against Women in The PhilippinesDocument2 pagesViolence Against Women in The PhilippinesJhonavil ReyesNo ratings yet
- Nutrition Folio (Basal Metabolic Rate)Document15 pagesNutrition Folio (Basal Metabolic Rate)Nursakinah NajwahNo ratings yet
- PericarditisDocument29 pagesPericarditisPavin KumarNo ratings yet
- Exploratory Study On Bach Flower RemediesDocument39 pagesExploratory Study On Bach Flower RemediesNarayananSrinivasan100% (1)
- MSDS Adsorb 13X 18 NA ENDocument9 pagesMSDS Adsorb 13X 18 NA ENMelixaxNo ratings yet
- Basic Concepts of 5S-KAIZEN-TQM ApproachDocument33 pagesBasic Concepts of 5S-KAIZEN-TQM ApproachAkash Kumar GuptaNo ratings yet
- The Future of Medical Device RegulationDocument296 pagesThe Future of Medical Device RegulationImtiazAhmedNo ratings yet
- What Is Your Nick NameDocument4 pagesWhat Is Your Nick NameIndha Findrayani RNo ratings yet