Professional Documents
Culture Documents
Salivary Gland PDF
Salivary Gland PDF
Uploaded by
abdulaleem1Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Salivary Gland PDF
Salivary Gland PDF
Uploaded by
abdulaleem1Copyright:
Available Formats
Pathology Patterns Reviews
Review of Fine-Needle Aspiration Cytology of Salivary
Gland Neoplasms, With Emphasis on Differential Diagnosis
Perkins Mukunyadzi, MD
Key Words: Salivary gland; Neoplasm; Fine-needle aspiration; Differential diagnosis
DOI: 10.1309/5FECYJ9639CMQM0L
Abstract
The widespread use of fine-needle aspiration (FNA)
biopsy of salivary gland lesions in many centers is
testimony to its usefulness and acceptance as a
diagnostic technique. Many pertinent questions
concerning a mass arising in the salivary gland can be
answered by evaluation of FNA cytologic material, and
these include whether the mass is truly of salivary
gland origin, whether the lesion is inflammatory or
neoplastic, and if neoplastic, whether benign or
malignant. On diagnosis of a neoplastic salivary gland
lesion, the next important issue is to correctly classify
the tumor, particularly if malignant. Specific cytologic
diagnoses can be achieved in the majority of cases, thus
enabling the clinician and patient to make appropriate
informed decisions. The cytologic evaluation of salivary
gland tumors, however, is limited by the wide range and
heterogeneous nature of benign and malignant tumors
arising in this area, many of which share similar or
show overlapping cytologic features, making the
diagnosis of rare tumors problematic. In this review, the
cytologic features of the major salivary gland
neoplasms, the differential diagnoses, and the salient
points that, if examined carefully, help achieve a
specific diagnosis are discussed.
S100
S100
Am J Clin Pathol 2002;118(Suppl 1):S100-S115
DOI: 10.1092/5FECYJ9639CMQM0L
Fine-needle aspiration (FNA) biopsy as a diagnostic
procedure is well established and widely used to evaluate
palpable lesions and, with the aid of imaging studies, is
equally applicable to deep-seated lesions.1,2 In the head and
neck area, lesions of the salivary glands frequently are evaluated by this technique; in fact in many centers, this is the first
tissue-based procedure applied to establish a diagnosis before
any surgical intervention. While use of needles to aspirate
palpable lesions of the salivary glands is not new, this technique (coupled with the availability of improved fast stains on
air-dried smears) has been refined over the years with the use
of very thin needles.3,4 Nowadays, in many centers trained
cytopathologists rather than surgeons perform FNA of salivary gland lesions using 23- or 25-gauge needles.5,6
The usefulness of salivary gland FNA relates to the fact
that it is easy to perform, is minimally invasive, smear evaluation is immediate, and the procedure can be repeated several
times to obtain more tissue for diagnosis or special studies.7,8
When a malignant diagnosis is given, the surgeon and the
patient are in a better position to discuss and plan for the next
course of action, while the diagnosis of a benign lesion
provides immediate relief to the patient, sparing the anxiety
of waiting several days for a surgical biopsy diagnosis.2,9
A review of the FNA cytologic findings of salivary
gland lesions is presented, starting with a brief discussion of
normal salivary gland cytology, comments on diagnostic
accuracy, and post-FNArelated tissue changes. The review
focuses on the detailed cytologic findings of each of the
major neoplasms of the salivary glands and the differential
possibilities that need consideration in particular situations.
In addition, a synoptic discussion of nonneoplastic inflammatory lesions that clinically and cytologically can mimic
malignancy is given.
American Society for Clinical Pathology
Pathology Patterns Reviews
Accuracy of Salivary Gland FNA
It is generally agreed by many cytopathologists that
FNA of salivary glands is a good diagnostic test with
reasonable sensitivity and specificity, ranging from 60%
to 100% and 90% to 100%, respectively.5 However, as
pointed out by Stanley10 and Schwarz et al,11 it is difficult
to compare the accuracy of statistical data because many
of the published series are small and, in others, unsatisfactory or nondiagnostic cases were excluded in the overall
figures. False-negative and false-positive results occur in
salivary gland FNA. False-negative results are due mainly
to errors of underdiagnosing low-grade tumors because of
their bland cytologic features and the difficult evaluation
of hypocellular cystic lesions so common in this area,
while false-positive diagnoses emanate from overcalls
of reactive changes, such as occur in the setting of associated inflammatory reactions.12,13 But perhaps more problematic and challenging is the heterogeneity of benign and
malignant tumors, whose underlying cytologic features
are similar, with differences in some cases being quantitative rather than qualitative. The shared cytomorphologic
features account for the indeterminate or suspicious
diagnoses and long lists of differential possibilities given
at times. However, in the hands of experienced
cytopathologists ensuring proper sampling and specimen
handling, the diagnosis of many salivary gland lesions is
possible.14-16
Normal Salivary Gland FNA Cytology
Normal salivary glands are rarely aspirated. However,
normal salivary gland tissue is observed in the inadvertently aspirated normal tissue obtained together with
abnormal tissue or in cases in which the target lesion is
missed.17,18 Normal salivary gland FNA cytology recapitulates the normal histologic features Image 1 and shows a
mixture of acinar cells, duct cells, adipose tissue Image
2, and scattered inflammatory cells. The acinar cells are
disposed of in grape-like arrangements, composed of
round or pyramidal cells, usually with uniform eccentric
nuclei and abundant granular or vacuolated cytoplasm.
Duct cells often form small groups or linear arrangements
and appear crowded compared with acinar cells because of
the lesser amount of cytoplasm that they possess. Duct
cells are smaller than acinar cells, and if they lose their
cytoplasm, they can easily be confused with lymphocytes.
It is not uncommon to observe adipocytes, normal
constituents of salivary gland tissue, associated with tissue
fragments, particularly in FNA samples of the parotid
gland.17,19
American Society for Clinical Pathology
Image 1 Normal salivary gland tissue showing acinar
structures and the ductal system. Note the presence of
adipose tissue (H&E, 200).
FNA-Related Tissue Changes
The issue of post-FNArelated tissue changes is important, as these changes may affect the histologic interpretation
of resected specimens. However, Mukunyadzi et al6 found
that the use of very thin (25-gauge) needles leads to insignificant bleeding and minor tissue damage. Potential tissue
changes include tumor infarction, hemorrhage, granulation
tissue, and metaplastic changes.20,21 Granulation tissue and
metaplastic cellular changes potentially can be confused with
sarcoma, carcinosarcoma, or both.22 Post-FNA tumor infarction and other changes have been reported in the literature,
although most tissue changes often were focal and insignificant.23 Seeding of the needle tract by tumor cells, a potential
serious complication of FNA, has been reported in the literature but remains extremely rare.24 In a study of 94 salivary
gland masses, when 25-gauge needles were exclusively used
in the aspiration of salivary gland lesions, the resultant tissue
changes were, in many cases, minor and did not preclude
histologic interpretation of the resected specimen.6 However,
despite the rarity of significant post-FNA tissue changes,
surgical pathologists need to be aware of such changes to
avoid potential diagnostic errors in the histologic interpretation of the resected specimens.
Classification of Salivary Gland Lesions
Any tumefacient lesion of the salivary glands is
amenable to evaluation by FNA cytology. The salivary gland
Am J Clin Pathol 2002;118(Suppl 1):S100-S115
S101 DOI: 10.1092/5FECYJ9639CMQM0L
S101
S101
Mukunyadzi / FINE-NEEDLE ASPIRATION CYTOLOGY OF SALIVARY GLAND NEOPLASMS
mass lesions can be broadly classified into inflammatory,
nonneoplastic, and neoplastic tumors. A listing of the salivary gland tumors includes the more common pleomorphic
adenoma, Warthin tumor, adenoid cystic carcinoma,
mucoepidermoid carcinoma, acinic cell carcinoma, various
cystic entities, and many rare tumors that are infrequently
encountered in FNA cytology. This review focuses on the
discussion of neoplastic salivary gland tumors.
Benign Salivary Gland Neoplasms
This group of salivary gland tumors constitutes the
majority of salivary gland tumors, accounting for about 85%,
63% and 14% in the parotid, submandibular, and sublingual
glands, respectively. More than 50% of the tumors of the
minor salivary glands are adenomas. They include the
common pleomorphic adenoma and Warthin tumor and other
relatively rare tumors such as myoepithelioma, oncocytoma,
sebaceous adenoma, cystadenoma, and papillomas.10,25,26
Pleomorphic Adenoma
A great number of salivary gland FNA aspirates, particularly of the parotid gland, will turn out to be pleomorphic
adenomas, synonymously and more appropriately known as
benign mixed tumor. In the parotid gland, pleomorphic
adenoma accounts for more than 70% of all the tumors, but it
is rare in the sublingual gland.1,19 More cases of pleomorphic
adenoma are seen in females than males and usually manifest during the fourth decade as slow-growing masses. On
palpation, the tumor feels firm, round, or bosselated and may
be movable. In rare situations or cases of long duration, pleomorphic adenoma may be fixed to the underlying tissues,
show ulceration, or manifest with pain, clinical findings that
are highly suggestive of malignancy.27-29
The appearance of the aspirated material of pleomorphic adenoma (if the specimen is not too bloody) is characteristic, showing droplets of thick or pasty mucoid material,
and the material should be grossly inspected. Smear cellularity is variable, but many cases are usually quite cellular.
Cytologically, the smears show 3 main components: extracellular matrix, myoepithelial and ductal cells present in
various proportions, and stroma. In many cases, myoepithelial cells dominate the smear, forming irregular tissue fragments and scattered background single cells. The myoepithelial cells have tremendous potential for differentiating
into various cytomorphologic forms, a finding that is more
striking in cytologic smears than in histologic sections and
includes plasmacytoid Image 3, spindled, and stellate cells
and clear cell changes. Ductal cells are less conspicuous and
usually show flat sheets composed of small cuboidal cells
with round nuclei. The third component of pleomorphic
adenoma, the stroma, is seen often as the metachromatic
magenta chondromyxoid matrix (Image 3).27,28 This matrix
S102
S102
Am J Clin Pathol 2002;118(Suppl 1):S100-S115
DOI: 10.1092/5FECYJ9639CMQM0L
Image 2 Smear of normal salivary gland aspirate demonstrating acinar cells arranged as a bunch of grapes cluster.
Smaller ductal cells can be identified in the center of the
cluster, while fragments of adipose tissue also are present
(Papanicolaou, 200).
Image 3 Pleomorphic adenoma. This very cellular smear
shows loose clusters of plasmacytoid myoepithelial cells and
metachromatic chondromyxoid stroma (rapid Romanowsky,
400).
usually is mixed intimately with the cellular elements and
may be so abundant as to obscure the latter. On Papanicolaou-stained slides, the matrix is cyanophilic and appears
fibrillary Image 4.29 In rare cases, additional minor components such as metaplastic squamous cells, cystic fluid, sebaceous cells, inflammatory cells, and even tyrosine crystals
may be identified.30,31
American Society for Clinical Pathology
Pathology Patterns Reviews
Image 4 Smear of pleomorphic adenoma showing the
characteristic fibrillary appearance of the matrix. Note the
presence of myoepithelial cells intimately admixed with the
stroma (Papanicolaou, 400).
The diagnosis of pleomorphic adenoma is usually
obvious after the identification of the 3 components just
described.15 However, the considerable variation in the
proportions of the constituent elements is a challenge
because of the resultant long list of differential diagnoses
Table 1. Stroma-deficient or cellular cases may be difficult
to recognize as pleomorphic adenoma and may be confused
with other tumors of the salivary gland. The differential diagnoses include low-grade carcinomas, and the monomorphic
adenoma, metastases, and the plasmacytoid appearance of
the myoepithelial cells may be mistaken for malignant
lymphoma or plasma cell proliferations.8,32,33
Monomorphic Adenoma (Basal Cell Adenoma)
Monomorphic adenoma, also synonymously known as
basal cell adenoma, represents a group of benign salivary
gland neoplasms characterized by a monomorphic population of small blue or basaloid cells. The histologic subclassification of basal cell adenomas is based on the growth
patterns, hence the recognition of several types: tubular,
trabecular, solid, membranous or dermal analogue, and
canalicular.19,33-35 The diagnostic dilemma in the evaluation
of monomorphic adenomas relates to their resemblance to
other primary or secondary small blue cell tumors that may
be encountered in the salivary glands. The list of such tumors
includes adenoid cystic carcinoma (particularly the solid
variant), cellular variant of pleomorphic adenoma, basal
adenocarcinoma, metastatic cutaneous basal cell carcinoma,
metastatic small cell carcinoma, and pilomatrixoma.32,33,36,37
As a group, the basal cell adenomas are rather
uncommon tumors (2% of all salivary gland neoplasms) and
are encountered infrequently in FNA of the salivary
glands.25,38 The smears of monomorphic adenomas often are
cellular but variable, showing cohesive, irregular, jigsaw
puzzle configurations or flat trabecular patterns and scattered
(naked) single cells. A hint of peripheral palisading may be
present in some clusters. Individual cells appear small and
basaloid, exhibiting high nuclear/cytoplasmic (N/C) ratios
and scant cytoplasm. The nuclei appear round to ovoid,
show even distribution of fine chromatin, and are without
obvious nucleoli. Basal cell adenomas may contain
metachromatic collagenous matrix, analogous to the matrix
of pleomorphic adenoma or adenoid cystic carcinoma,
although it is usually nonfibrillary on Papanicolaou stain.
When the matrix assumes the form of cylinders and spheres,
it becomes difficult to distinguish monomorphic adenoma
from adenoid cystic carcinoma Table 2. However, the
matrix of basal cell adenoma tends to show interdigitation
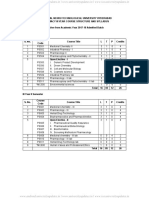
Table 1
Differential Diagnoses for Pleomorphic Adenoma*
Cytologic Finding
(Pleomorphic Adenoma)
Plasmacytoid myoepithelial cells
Increased duct cells
Matrix-poor tumor cells
Increased stroma with or
without hyaline globules
Nuclear atypia (mild to moderate
and focal)
Mucoid background
Differential Diagnosis
Diagnostic Hints
Malignant lymphoma
Plasmacytoma
Low-grade carcinoma
Monomorphic adenoma
Low-grade carcinoma
Myoepithelioma
Metastases
Adenoid cystic carcinoma
Polymorphous low-grade adenocarcinoma
Carcinoma ex pleomorphic adenoma
Identify myoepithelial cells
Matrix and nuclear detail; no lymphoglandular bodies
Careful characterization of matrix
Matrix
Nuclear detail
Difficult to exclude
Necrosis, mitosis, nuclear detail, history
Identify myoepithelial cells
Evaluate stroma-cell interface
Identify typical myoepithelial cell features
Low-grade mucoepidermoid carcinoma
Different staining characteristics on rapid Romanowsky/
MGG stains; no mucous and intermediate cells
MGG, May-Grnwald-Giemsa.
* For proper matrix characterization, both air-dried, rapid Romanowskystained and fixed Papanicolaou-stained smears are needed.
American Society for Clinical Pathology
Am J Clin Pathol 2002;118(Suppl 1):S100-S115
S103 DOI: 10.1092/5FECYJ9639CMQM0L
S103
S103
Mukunyadzi / FINE-NEEDLE ASPIRATION CYTOLOGY OF SALIVARY GLAND NEOPLASMS
Table 2
Differential Diagnoses for Monomorphic Adenoma (Basaloid Cell Adenoma)
Cytologic Finding (Monomorphic Adenoma)
Basaloid small cells
Differential Diagnosis
Basal cell adenocarcinoma
Adenoid cystic carcinoma
Polymorphous low-grade adenocarcinoma
(problem: hyaline globules of stroma)
Cellular pleomorphic adenoma
Metastatic small cell carcinoma
with tumor cells at the periphery, and, in addition, delicate
vessels and spindle cells may be present, embedded in the
stroma. In contrast, in adenoid cystic carcinoma, the
stromatumor cell interface is sharply defined; the matrix is
commonly acellular and devoid of blood vessels. The dermal
analogue subtype of basal cell adenoma is virtually indistinguishable cytologically from adenoid cystic cell carcinoma.10,36,39 Clinical history and imaging studies are crucial
in the diagnosis of metastatic small cell carcinoma and cutaneous basal cell carcinoma, entities that cytologically
resemble basal cell adenomas. Presence of high-grade
nuclear features, mitosis, nucleoli, and necrosis are more
suggestive of carcinoma than of monomorphic adenoma.40,41
Warthin Tumor
Warthin tumor is a benign tumor commonly encountered
in salivary gland FNA specimens. Warthin tumor occurs
Image 5 Warthin tumor. Histologic examination reveals a
bilayer of oncocytes lining the cyst wall and abundant
lymphocytes in the subepithelial stroma (H&E, 400).
S104
S104
Am J Clin Pathol 2002;118(Suppl 1):S100-S115
DOI: 10.1092/5FECYJ9639CMQM0L
Diagnostic Hints
Necrosis, mitosis, high-grade nuclear features, pleomorphism favors
malignancy; may be impossible to distinguish
Abnormal nuclear detail, necrosis favors malignancy
May be impossible to distinguish; palisading favors adenoma; site of
tumor origin
Identify myoepithelial cells; naked nuclei favor monomorphic adenoma
Clinical data, nuclear molding, necrosis, no stroma favor malignancy
frequently in the parotid gland, is slightly more common in
females, shows an association with cigarette smoking, and may
be bilateral in about 10% of the cases. On palpation, most
Warthin tumors feel soft or boggy but in situations of increased
fluid accumulation they may feel quite tense and firm.1,10,42
Histologic examination of Warthin tumor reveals the
characteristic cystic spaces lined by a bilayer of oncocytic
cells and abundant lymphocytes in the subepithelial stroma
Image 5. The aspirated material appears chocolate brown.
The cellularity of the smears is variable and may be quite
hypocellular owing to fluid dilution. The 3 main components
that characterize the FNA cytology of Warthin tumor are
oncocytes, lymphocytes, and the fluid background Image 6.
Oncocytes usually are seen as flat, cohesive sheets 2 to 3
cells in thickness and often devoid of stroma. The oncocytes
have abundant dense cytoplasm, relatively large but bland
nuclei, and uniformly low N/C ratios.19 The cytoplasmic
Image 6 Smear of Warthin tumor aspirate showing the
small flat sheets of oncocytes, scattered lymphocytes, and a
granular cystic background. The oncocytes display
abundant granular cytoplasm with sharp cytoplasmic borders
and bland nuclear features (Papanicolaou, 400).
American Society for Clinical Pathology
Pathology Patterns Reviews
granularity and eosinophilia, characteristic features of oncocytes, may be difficult to detect on rapid Romanowsky and
Papanicolaou-stained FNA material, but they are obvious on
H&E-stained cell-block material.
The accompanying lymphoid component of Warthin
tumor shows mostly small, mature background lymphocytes.
Occasionally elements of a reactive follicle germinal center
may be identified. The fluid of Warthin tumor often imparts
a dirty background appearance that may be confused with
tumor necrosis. In addition to the 3 main components, other
elements that can be encountered in FNA smears of Warthin
tumor include, albeit rarely, metaplastic squamous and sebaceous gland cells.
The differential diagnoses for Warthin tumor are wide
Table 3 . 16,43 In most cases (>80%), the presence and
combination of the 3 main cytologic elements establish the
diagnosis without difficulty. However, as is well known,
oncocytes, lymphocytes, and a fluid background are not
pathognomonic of Warthin tumor, as they are encountered in
several other conditions. Cysts (lymphoepithelial cysts) of
the salivary glands and chronic inflammatory and obstructive
duct lesions can accumulate fluid, show oncocytic metaplasia, and contain numerous lymphocytes and can easily be
confused with Warthin tumor.44-46 Oncocytoma and oncocytic carcinoma are rare salivary gland tumors that may be
confused with Warthin tumor, as oncocytes are common to
all 3 entities, and the former 2 tumors may contain variable
numbers of lymphocytes. In oncocytic neoplasms, the cell
clusters are bigger and 3-dimensional and are 3 or more cell
layers thick. The intermediate squamous cells of mucoepidermoid carcinoma, the uncommon oncocytic metaplasia of
pleomorphic adenoma, and metaplastic cells of squamous
cell carcinoma may all be confused with Warthin tumor.47
The cells of acinic cell carcinoma may show cytoplasmic
eosinophilia, thus resembling oncocytes and leading to diagnostic confusion. However, the presence of large zymogen
granules, prominent nucleoli, significant pleomorphism,
cytoplasmic vacuolation, and prominent large-caliber vessels
favors the diagnosis of acinic cell carcinoma over Warthin
tumor. It is important to always reaspirate any residual mass
after initial drainage of fluid from Warthin tumor cases or
any other cystic lesions to obtain more representative material, which may provide clues to the diagnosis.
Oncocytic Neoplasms
While nonneoplastic oncocytes are common and seen
regularly in the FNA biopsy smears of salivary gland lesions,
oncocytic neoplasms are rare.48 Exclusive populations of oncocytic cells showing abundant and finely granular cytoplasm
characterize oncocytic neoplasms seen in many endocrine and
other organs of the body, including the salivary glands. Most
oncocytic neoplasms represent benign oncocytoma, while the
malignant counterpart, oncocytic carcinoma (malignant oncocytoma) is extremely rare.4,49 In FNA smears of salivary gland
oncocytic neoplasms, oncocytes are present as cohesive 3dimensional clusters and are 3 or more cells thick Image 7.
The nuclei often exhibit mild atypia and prominent nucleoli.47
However, occasionally significant nuclear pleomorphism may
be seen, but mitotic figures are uncommon. On air-dried, rapid
Romanowskystained material, the cytoplasm may appear
dense bluish gray, and the cytoplasmic granules, representing
numerous mitochondria, may be difficult to detect.
The accuracy rate for the diagnosis of oncocytoma on
FNA biopsy material is high, about 92%, while false-positive
diagnoses are largely due to incorrectly diagnosed cases of
Warthin tumor.25 In general, the cell clusters in Warthin
tumor are smaller and flat, while those of oncocytoma
present as thicker 3-dimensional groups. In addition, aspiration of Warthin tumor often yields brownish fluid, which
imparts the dirty cyst fluid appearance on the smears, while
oncocytoma is less likely to be cystic or to contain as much
fluid. As already noted, the majority of oncocytic neoplasms
are benign, even if nuclear atypia is present. Nevertheless,
the cytologic distinction of oncocytoma from the extremely
rare oncocytic carcinoma is difficult and may be impossible
on FNA material.49 While the presence of significant nuclear
Table 3
Differential Diagnoses for Warthin Tumor
Cytologic Finding
(Warthin Tumor)
Cyst fluid not obvious;
oncocytes only
Rare oncocytes and
lymphocytes
Atypical metaplastic
squamous cells
Oncocytic cells and
lymphocytes
Differential Diagnosis
Oncocytoma
Various cystic lesions
Lymphoma
SCC
MEC
Acinic cell carcinoma
(lymphocyte-rich stroma)
Diagnostic Hints
Warthin tumor unlikely if only 1 cell seen; oncocytoma usually not cystic and
has fewer lymphocytes than Warthin tumor
Reaspirate any residual mass
Consider flow cytometric analysis
Warthin tumor unlikely if high-grade nuclear features, no oncocytes in SCC
Intermediate and mucous cells favor MEC
Papillary and acinar structures, cytoplasmic vacuoles, necrosis favor acinic
cell carcinoma
MEC, mucoepidermoid carcinoma; SCC, squamous cell carcinoma.
American Society for Clinical Pathology
Am J Clin Pathol 2002;118(Suppl 1):S100-S115
S105 DOI: 10.1092/5FECYJ9639CMQM0L
S105
S105
Mukunyadzi / FINE-NEEDLE ASPIRATION CYTOLOGY OF SALIVARY GLAND NEOPLASMS
atypia, mitosis, and necrosis suggests malignancy, a definitive diagnosis of carcinoma may require surgical excision
and histologic evaluation. Other lesions in the same differential category are acinic cell carcinoma, mucoepidermoid
carcinoma with oncocytic metaplasia, and oncocytosis seen
in normal salivary glands or metaplastic oncocytes associated with inflammatory lesions (Table 3).
Myoepithelioma
Myoepithelioma is an uncommon benign neoplasm that
occurs in the parotid, submandibular gland, and the palate. The
tumor is composed exclusively of plasmacytoid or spindled
cells representing myoepithelial cells (and not accompanied by
an epithelial or ductal component).50,51 Cytologically, spindleshaped or uniform plasmacytoid cells containing moderate
amounts of cytoplasm and showing distinct cytoplasmic
borders characterize the smears of myoepithelioma. Stromal
material is minimal or absent, while necrosis, mitosis, and
nuclear atypia are virtually never seen in this neoplasm.43,52
Pleomorphic adenoma and the malignant myoepithelioma are the chief differential considerations for myoepithelioma (Table 1). Identification of plasmacytoid myoepithelial
cells intimately mixed with metachromatic stroma favors
pleomorphic adenoma, although stroma-poor cases may be
difficult to distinguish from myoepithelioma. The cytologic
features of the extremely rare malignant myoepithelioma
have not been well reported, but the presence of significant
52,53
nuclear atypia and mitosis may suggest such a diagnosis.
Image 7 Oncocytoma. Smear showing exclusively
oncocytic cells forming cohesive clusters. No lymphocytes or
other cell types are present (rapid Romanowsky, 400).
Low-Grade Neoplasms
Low-Grade Mucoepidermoid Carcinoma
Mucoepidermoid carcinoma (MEC) is generally divided
into 2 histologic grades, low and high, the former characterized by a cystic growth pattern Image 8 and an abundance
of mucous cells, while high-grade MEC is defined by dominance of the solid component. Some workers recognize an
intermediate histologic grade of MEC.54-56 Proper assignment of grade requires evaluation of the entire tumor, a difficult proposition on FNA material because of sampling problems. While grading of the tumor is difficult on cytologic
material, a more serious problem is failing to correctly diagnose low-grade MEC. Low-grade MEC accounts for about
80% of all MECs and is well recognized for its potential
false-negative diagnostic pitfall, apparently owing to the
bland cytologic features and hypocellular nature of many of
these tumors. MEC occurs at any age, can involve both the
major and minor salivary glands, and is the most common
malignant salivary gland tumor in children.56,57
The aspiration of low-grade MEC usually yields fluid,
which may be mucoid, and the smears are typically hypocellular. Again, to obtain more representative material in any
S106
S106
Am J Clin Pathol 2002;118(Suppl 1):S100-S115
DOI: 10.1092/5FECYJ9639CMQM0L
Image 8 Low-grade mucoepidermoid carcinoma. Histologic
examination reveals the predominantly microcystic pattern
and numerous mucous cells (H&E, 400).
cystic lesion, the residual mass, following initial fluid aspiration, should be reaspirated. The cellular component of MEC
will show a mixture of mucus-secreting cells and intermediate cells Image 9. Both cell types show bland cytologic
features. Mucus-secreting cells exhibit abundant foamy or
vacuolated cytoplasm, low N/C ratios, and loose cellular
groups. Careful examination of the smears may reveal the
presence of goblet cells (Image 9), cells frequently seen in lowgrade MEC.25,57 When the mucous cells are present as single
cells, they can be easily confused with foamy histiocytes.
American Society for Clinical Pathology
Pathology Patterns Reviews
usually is not seen in MEC, although metastasis of low-grade
MEC to the neck and intraparotid lymph nodes may result in
a very confusing picture. Obstructive duct lesions are particularly problematic as mucous and squamous metaplasia can
be seen, mimicking the mixed cell pattern of low-grade
MEC. Identification of stone fragments excludes MEC, but
this, in the experience of many, is not a common finding in
cases of sialolithiasis. The mucoid stroma of pleomorphic
adenoma may be mistaken for the mucin of MEC, but the
mucin/stroma of the latter does not show metachromasia. A
careful search for the myoepithelial cells will help avoid
making the wrong diagnosis.10,60
Image 9 Smear of low-grade mucoepidermoid carcinoma
showing clusters of mucous cells, smaller intermediate cells,
and prominent goblet cells (rapid Romanowsky, 600).
Intermediate cells are small uniform cells with scant cytoplasm
and frequently are present in tight cohesive clusters. Cells
showing true or mature squamous cell differentiation (keratinization) are almost never seen in low-grade MEC.10,19,56
As stated before, underdiagnosis of low-grade MEC is a
common problem because the malignant nature of the lesion
may be overlooked for reasons mentioned before and
because the foamy cells resemble histiocytes.1,9,10,58 One
should always first exclude the possibility of low-grade MEC
before a specific diagnosis is given in the cytologic evaluation of any cystic lesion of the salivary glands. The differential diagnosis of low-grade MEC includes Warthin tumor,
benign salivary gland cysts (lymphoepithelial cysts),
branchial cleft cyst, sialolithiasis or chronic sialadenitis
complicated by cystic dilatation, and pleomorphic adenoma
with excess mucoid stroma Table 4.49,54,59 To differentiate
Warthin tumor from low-grade MEC, one should look for the
presence of numerous oncocytes (especially in cohesive clusters), the dirty cystic background, and lymphocytes. The
presence of oncocytes and lymphocytes in large numbers
Acinic Cell Carcinoma
Acinic cell carcinoma, the third major common malignant tumor of the salivary gland, is seen in adults and children and occurs mainly in the parotid gland, although the
submandibular glands can be involved as well. Ten percent
of acinic cell carcinomas will recur despite wide resection,
but the overall prognosis is good, with a 10-year survival rate
of about 90%. Several histologic growth patterns of acinic
cell carcinoma are recognized, including the solid, follicular
(resembles thyroid follicles), microcystic, papillary Image
10, and mixed patterns.61,62
Cytologically, acinic cell carcinoma can be divided into
well-, moderately, and poorly differentiated forms, but the
cytologic diagnosis depends on the identification of acinar
cells and/or recognition of the acinar-glandular arrangement.
In many cases, the FNA smears are quite cellular (cystic
cases may be hypocellular), showing both single cells and
large irregular clusters; the central portions of the latter often
contain large-caliber vessels, while the periphery demonstrates frayed borders Image 11.63-65 The tumor cells in
well-differentiated acinic cell carcinoma closely resemble
normal acinar cells, are large and polyhedral with abundant
bluish gray vacuolated Image 12 and granular cytoplasm on
rapid Romanowskystained material, and have eccentric
nuclei. The cytoplasmic granules are much larger than the
granules of oncocytic cells. In some cases, however, the
granules may be degranulated and, therefore, may not be
identified. The cytoplasm is delicate and can rupture easily
Table 4
Differential Diagnoses for Low-Grade MEC*
Cytologic Finding (MEC)
Squamous and mucous cells,
cyst fluid, foamy cells
Hypocellular mucoid smears
(with or without foamy cells)
Oncocyte-like cells (rare)
Differential Diagnosis
Diagnostic Hints
Metaplastic cells seen in sialolithiasis
and Kuttner tumor (submandibular)
Cysts
Goblet cells favor MEC; painful aspirate and stone fragments
favor inflammation (may defer to histologic examination)
Mixed cellsgoblet and goblet cellsfavor MEC
Warthin tumor
True oncocytes favor Warthin tumor; mucous and
intermediate cells favor MEC
MEC, mucoepidermoid carcinoma.
* The differential diagnosis of low-grade mucoepidermoid carcinoma is particularly difficult and warrants extreme caution.
American Society for Clinical Pathology
Am J Clin Pathol 2002;118(Suppl 1):S100-S115
S107 DOI: 10.1092/5FECYJ9639CMQM0L
S107
S107
Mukunyadzi / FINE-NEEDLE ASPIRATION CYTOLOGY OF SALIVARY GLAND NEOPLASMS
Image 10 Acinic cell carcinoma. Histologic section showing
papillary configuration. Vacuolation and clear cytoplasm are
apparent in the tumor cells. This appearance could be
confused with metastatic renal cell carcinoma (H&E, 600).
Image 11 Tumor cells of acinic cell carcinoma are seen
attached to the centrally placed vessels (rapid Romanowsky,
600).
during the smearing process, leading to the presence of
numerous naked nuclei and a granular background. The lessdifferentiated tumors show smaller cells that may appear
cuboidal. Nuclear atypia remains minimal to moderate, but
necrosis may be present. On occasion, cells with clear cytoplasm may be identified.63,64
A major differential diagnostic consideration of acinic
cell carcinoma is normal salivary gland acinar cells or
sialosis Table 5.66 Normal acinar cells are usually seen as
3-dimensional cohesive clusters of cells like a bunch of
grapes and may be mixed with groups of smaller ductal cells
and adipose tissue fragments, whereas in acinic cell carcinoma, in addition to clusters, there are relatively more single
cells. Furthermore, the clusters of cells in acinic cell carcinoma are larger and more irregular than those of normal
acini. Because the tumor grows in an expansive manner, all
normal tissues (including adipose and ductal cells) are
pushed away to the periphery and generally are not represented in the smears. Neoplasms in the differential diagnosis
of acinic cell carcinoma include epithelial-myoepithelial
carcinoma, MEC, Warthin tumor, pleomorphic adenoma,
oncocytoma, and metastatic renal carcinoma.4,67 The presence of clear cells or vacuolated cells should lead to the
consideration of epithelial-myoepithelial carcinoma and
metastatic renal cell carcinoma. However, the identification
of acellular hyaline stroma (and spindle-shaped myoepithelial cells) favors epithelial-myoepithelial carcinoma, whereas
the presence of numerous naked nuclei in the background
favors acinic cell carcinoma. Clinical history of a kidney
carcinoma should lead to strong consideration of metastasis.
The vacuolated cells of low-grade MEC may be confused
with acinic cell carcinoma. An effort should be made to look
for mucus-producing and goblet cells that are characteristic
of low-grade MEC. In addition, zymogen granules are not
seen in low-grade MEC but may be present in acinic cell
carcinoma. Identification of the strikingly metachromatic
stroma and plasmacytoid cells will help in the distinction of
cellular pleomorphic adenoma from acinic cell carcinoma. The
tumor cells of acinic cell carcinoma may appear oncocytic and,
S108
S108
Am J Clin Pathol 2002;118(Suppl 1):S100-S115
DOI: 10.1092/5FECYJ9639CMQM0L
Image 12 Another irregular cluster of acinic cell carcinoma
showing cytoplasmic vacuoles, eccentric nuclei, and
occasional nucleoli (rapid Romanowsky, 600).
American Society for Clinical Pathology
Pathology Patterns Reviews
Table 5
Differential Diagnoses for ACC
Cytologic Finding (ACC)
Eosinophilic, oncocyte-like cells,
cytoplasmic vacuoles
Oncocyte-like cells and lymphocytes
Hypocellular (cystic ACC)
Acinar cells, normal looking
(well-differentiated ACC)
Papillary structures, vacuolated
or clear cytoplasm
Differential Diagnosis
Diagnostic Hints
High-grade mucoepidermoid carcinoma
No mixed cell pattern in ACC
Warthin tumor; oncocytoma
Variety of cystic lesions
Normal salivary gland tissue; sialosis
Acinar arrangements and naked nuclei favor ACC
Reaspirate
No normal elements (adipocytes and ductal cells),
favor ACC
Clinical history and imaging studies
Metastasis: renal cell carcinoma
(rare but known to go to unusual sites)
ACC, acinic cell carcinoma.
together with the presence of scattered naked nuclei (resembling lymphocytes), acinic cell carcinoma may be confused
with oncocytoma and Warthin tumor. However, more
commonly, acinar cell arrangements are seen in acinic cell
carcinoma but not in oncocytoma or Warthin tumor, and, in
addition, lymphocytes rather than naked nuclei typify
Warthin tumor.
Adenoid Cystic Carcinoma
Adenoid cystic carcinoma is one of the major and more
common malignant salivary gland neoplasms. It occurs
mainly in the minor glands and submandibular gland,
accounting for about 10% of all salivary gland and 3% of
parotid tumors. Adenoid cystic carcinoma manifests as a
slow-growing mass, and, in about 10% of the cases, patients
may complain of pain or show facial muscle weakness (clinical findings strongly suggestive of malignancy), and the
clinical behavior is characterized by persistent growth and
recurrences.10,68
Cytologically, the smear patterns of adenoid cystic
carcinoma are characterized by a mixture of small, uniform,
basaloid cells with high N/C ratios and metachromatic
stroma. The cytologic architecture frequently mimics the
histologic patterns Image 13, showing cribriform or tubular
structures, while exclusively solid sheets of tumor cells are
seen in the solid variant or anaplastic adenoid cystic carcinoma. The chromatin appears coarse but uniform without
identifiable nucleoli, and nuclear pleomorphism is minimal.
Necrosis is a rare cytologic finding, but when seen usually is
indicative of the anaplastic variant of adenoid cystic carcinoma. The background of adenoid cystic carcinoma usually
is populated by scattered naked nuclei of tumor cells.
Although the stroma of adenoid cystic carcinoma is characteristic, it can be seen in several other salivary gland tumors.
In the classic cribriform or tubular adenoid cystic carcinoma,
balls or spheres and cylinders of magenta stroma are seen on
air-dried, rapid Romanowskystained material Image 14.
The interface between tumor cells and stroma often is
American Society for Clinical Pathology
sharply demarcated. On Papanicolaou staining, the stroma
appears cyanophilic but shows no fibrillary architecture, an
important distinguishing feature when the differential
consideration is pleomorphic adenoma (Image 13).15,69
The diagnosis of the well-differentiated or cribriform
type of adenoid cystic carcinoma is relatively straightforward. The microcystic spaces containing the hyaline globules and cylinders of metachromatic stroma are easily identified in such cases. However, metachromatic stroma is not
specific for or unique to adenoid cystic carcinoma; it also is
found in cases of polymorphous low-grade adenocarcinoma,
basal cell adenoma, and pleomorphic adenoma and even in
epithelial-myoepithelial carcinoma and basal cell
carcinoma. 36 Thus, cases of adenoid cystic carcinoma
lacking cribriform architecture may be impossible to distinguish from other basaloid tumors. The identification of
hyaline stroma is, however, always critical to the diagnosis of
adenoid cystic carcinoma, as most cases almost always
(excerpt the solid variant) show its presence.70 There are no
clear nuclear and cytoplasmic features that permit discrimination of adenoid cystic carcinoma from its mimics. Because
the surgical treatment of adenoid cystic carcinoma may
involve sacrificing the facial nerve, it is crucial to make the
correct cytologic diagnosis. In addition, the overall prognosis
between different tumor types may be vastly different. In
difficult cases, definitive diagnosis may need to be deferred
to the surgical specimen (or frozen section) evaluation.
Adenoid cystic carcinoma always should be considered in
the differential diagnosis of any basaloid small blue cell
tumors of the salivary gland (Table 2).
Polymorphous Low-Grade Adenocarcinoma
Polymorphous low-grade adenocarcinoma occurs
predominantly in the minor salivary glands, in particular on
the hard palate and other intraoral sites. In rare instances, the
major salivary glands and neck lymph nodes may be
involved. The average age of patients with polymorphous
low-grade adenocarcinoma is 60 years.71-73
Am J Clin Pathol 2002;118(Suppl 1):S100-S115
S109 DOI: 10.1092/5FECYJ9639CMQM0L
S109
S109
Mukunyadzi / FINE-NEEDLE ASPIRATION CYTOLOGY OF SALIVARY GLAND NEOPLASMS
Image 13 Adenoid cystic carcinoma. A, The typical cribriform
architecture seen on histologic sections (H&E, 400). B,
Aspirate smear indicating the nonfibrillary cyanophilic cylinders
and globules of the matrix and showing tumor cells lined up
on the outer aspect of the matrix (Papanicolaou, 400).
Image 14 The brightly metachromatic matrix forming
hyaline cylinders and spheres with a sharp interface between
the matrix and tumor cells are characteristic findings for
adenoid cystic carcinoma (rapid Romanowsky, 400).
Mixed patterns of irregular sheets and pseudopapillary
or papillary fragments of tumor cells and metachromatic
stroma characterize the cytology of polymorphous low-grade
adenocarcinoma. The tumor cells are oval or polyhedral with
moderate amounts of nonvacuolated cytoplasm. Because the
cytoplasm is delicate, naked nuclei of tumor cells often are
seen in the background. The nuclei appear uniform, show
delicate chromatin, and contain small or inconspicuous
nucleoli. The stroma may be mixed intimately with tumor
cells or may form hyaline globules that closely resemble the
hyaline globules of adenoid cystic carcinoma.74
The chief differential considerations for polymorphous
low-grade adenocarcinoma include adenoid cystic carcinoma,
epithelial-myoepithelial carcinoma, and pleomorphic adenoma
(Table 2). The distinction of polymorphous low-grade adenocarcinoma from adenoid cystic carcinoma may be quite difficult, because, when present, the stromal hyaline globules are
similar. However, the tumor cells of polymorphous low-grade
adenocarcinoma generally are larger and more uniform than
the cells of adenoid cystic carcinoma, and in addition, the
presence of pseudopapillary fragments is uncommon in
adenoid cystic carcinoma. Epithelial-myoepithelial carcinoma
may be impossible to distinguish from polymorphous lowgrade adenocarcinoma when the 2 cell types, ductal and
myoepithelial cells, that characterize this tumor are not seen
together. The metachromatic stroma of polymorphous lowgrade adenocarcinoma may lead to the consideration of a
cellular pleomorphic adenoma; however, the globular hyaline
deposits are less common in the latter. In addition, the tumor
cells of pleomorphic adenoma usually show plasmacytoid
features of the myoepithelial cells, and the cells do not form
the well-defined pseudopapillary or tubular structures typical
of polymorphous low-grade adenocarcinoma.25,73
S110
S110
Am J Clin Pathol 2002;118(Suppl 1):S100-S115
DOI: 10.1092/5FECYJ9639CMQM0L
High-Grade Neoplasms
High-Grade MEC
The diagnosis of high-grade MEC, in contrast with that
of low-grade MEC, is relatively easy, as more atypical cells
showing squamoid features are seen.10 Nevertheless, other
constituent elements such as intermediate cells and mucusproducing or goblet cells should be sought and identified to
complete the diagnostic picture. It should be noted,
however, that the histologic classification of high-grade
MEC is not based primarily on the presence of high-grade
nuclear features; rather it is dependent on the extent of the
solid component.10,73 The implication of this requirement
with regard to FNA cytology is thorough sampling of the
lesion to obtain representative material. The differential
diagnosis of high-grade MEC includes squamous cell carcinoma. Primary squamous cell carcinoma of the salivary
glands is rare, while metastasis or contiguous involvement
from cutaneous or intraoral locations is more common.26 As
noted by Schindler et al19 and Feldman et al,75 both highgrade MEC and squamous cell carcinoma can show cystic
components, making this feature nondiscriminative. Squamous cell carcinoma metastatic from the tonsillar crypts is
particularly likely to show cystic metastasis19,75 Table 6.
American Society for Clinical Pathology
Pathology Patterns Reviews
Table 6
Differential Diagnoses for High-Grade Neoplasms
Neoplasm
SDC (may be impossible to distinguish from metastatic
breast carcinoma)
High-grade mucoepidermoid carcinoma
SCC (primary rare, intraparotid lymph node metastasis
or contiguous spread from skin)
Metastasis: adenocarcinoma, undifferentiated carcinoma
Cytologic Finding
High-grade nuclear features; cribriform pattern; necrosis and hyalinized
collagen bands
Mixture of cells: intermediate, squamous differentiation, and mucous cells;
nuclear atypia not as severe as in SDC or SCC
Pleomorphic cells with high-grade nuclei; dense keratinized cytoplasm;
keratin debris
Difficulty differential; need full clinical data and imaging studies
SCC, squamous cell carcinoma; SDC, salivary duct carcinoma.
Salivary Duct Carcinoma
Salivary duct carcinoma is a rare, high-grade malignant
tumor, accounting for about 2.8% of the salivary gland
malignant tumors. More than 80% of the cases occur in the
parotid gland of older men. At diagnosis, the majority of the
patients will have local lymph node metastases and/or extra
parotid extension into adjacent soft tissue. The histologic
similarities of salivary duct carcinoma to mammary duct
carcinoma have been well described and include the cribriform pattern of tumor growth Image 15 and the presence of
comedo-type necrosis.26,76,77
Cytologically, the diagnosis of a malignant process is
straightforward in these cases because the nuclear features are
often high-grade and easy to recognize as such. However,
recognizing the tumor as a primary tumor of the salivary
gland and correctly classifying it may be difficult. The smears
of salivary duct carcinoma usually are very cellular, showing
tumor cell groups disposed of in cribriform or pseudopapillary formations Image 16, often associated with necrosis.
Nuclei are large and irregular with thickened membranes and
prominent nucleoli. The cytoplasm is generally moderate to
abundant and appears eosinophilic.78 A nonspecific but useful
diagnostic feature seen in invasive salivary duct carcinoma is
the presence of bands of hyalinized collagen (Image 16), a
stromal response to tumor infiltration.79-81
Initial recognition of salivary duct carcinoma as a highgrade neoplasm is crucial as this tumor carries a dismal prognosis. However, salivary duct carcinoma should be differentiated from high-grade MEC, squamous cell carcinoma, and
metastatic breast carcinoma (Table 6). MEC consists of a
mixture of cell types, including mucous cells, intermediate
cells, and cells showing squamous differentiation. The squamous differentiation seen in MEC is subtle and does not
usually show full maturation, and the degree of nuclear atypia
is often mild. The cytoplasm of salivary duct carcinoma may
appear dense and squamoid, but obvious squamous differentiation and the presence of keratin material and high-grade nuclei
are more consistent with squamous cell carcinoma Image 17
Image 15 Salivary duct carcinoma. A histologic section
demonstrates the cribriform and infiltrative growth pattern of
this high-grade tumor (H&E, 400).
Image 16 The smear pattern of salivary duct carcinoma
shows irregular clusters of high-grade nuclei tumor cells and
bands of hyalinized collagen (rapid Romanowsky, 600).
American Society for Clinical Pathology
Am J Clin Pathol 2002;118(Suppl 1):S100-S115
S111 DOI: 10.1092/5FECYJ9639CMQM0L
S111
S111
Mukunyadzi / FINE-NEEDLE ASPIRATION CYTOLOGY OF SALIVARY GLAND NEOPLASMS
papillary cystic adenoma, and papillary adenocarcinoma,
true malignant mixed tumors, mesenchymal lesions such as
schwannoma, and others. Proper recognition of the individual cell constituents and correlation with the clinical
picture is critical in making the correct diagnosis.83,84
FNA of Lymphoid Lesions
Image 17 Squamous cell carcinoma of the parotid gland. In
this smear tumor cells with obvious high-grade nuclei,
pleomorphism, and keratinized cytoplasm are present. This
degree of atypia and squamous maturation is not seen in
mucoepidermoid carcinoma (rapid Romanowsky, 600).
than salivary duct carcinoma. Pleomorphic adenoma is distinguished from salivary duct carcinoma by the identification of
plasmacytoid myoepithelial cells, lack of high-grade nuclear
features, and the absence of necrosis. Metastasis from breast
carcinoma to the parotid gland is uncommon, but both entities
frequently involve neck lymph nodes, making the cytologic
differentiation from lymph node aspiration material difficult if
not impossible. Thus, historic clinical data and immunostaining
for androgen receptors (positive in salivary duct carcinoma)
may assist in making the correct diagnosis.80
Carcinoma Ex Pleomorphic Adenoma
Carcinoma ex pleomorphic adenoma accounts for about
2.2% of all salivary gland tumors, and the malignant component
can manifest synchronously or metachronously with pleomorphic adenoma. The malignant component often is high-grade
and includes MEC, salivary duct carcinoma, undifferentiated
carcinoma, and others. Low-grade tumors also can arise from
pleomorphic adenoma. Cytologically, in the synchronous type,
the benign pleomorphic adenoma and the malignant component
may be identified in the same smear, but more likely one
component is present or dominates the smear pattern.11,44,82
Other Rare Neoplasms and Nonneoplastic Tumefacient
Lesions
There are many extremely uncommon neoplastic
tumors that can occur in salivary glands and, therefore, may
be encountered in FNA cytologic material. These include
sebaceous adenoma, sebaceous lymphadenoma, papilloma,
S112
S112
Am J Clin Pathol 2002;118(Suppl 1):S100-S115
DOI: 10.1092/5FECYJ9639CMQM0L
Lymphoid lesions of the salivary gland include normal
intraparotid lymph node, benign lymphoepithelial lesions, and
malignant lymphoma.26,85-88 The presence of lymphocytes in
Warthin tumor and many epithelial salivary gland neoplasms
has been described. Malignant lymphoma accounts for about
5% of all salivary gland tumors. Secondary involvement of the
salivary gland or intraparotid lymph nodes can be suspected in
patients known to have lymphoma. Of the primary lymphomas,
the high-grade type is relatively easy to diagnose. However,
follicular lymphomas and lymphomas of mucosa-associated
tissue type (MALT) may be very difficult to identify.89 A high
index of suspicion is required whenever an abundance of
lymphoid cells is identified, and flow cytometric analysis
should be performed. MALT lymphomas are low-grade tumors
that occur in association with benign lymphoepithelial lesions
and, therefore, will show a polymorphous picture composed of
reactive or benign and malignant lymphoid cells. Flow cytometric analysis and histologic evaluation are required for the
definitive diagnosis of lymphomas.86-88
Chronic Sialadenitis and Sialolithiasis
Nonneoplastic inflammatory lesions, including the
tumefacient Kuttner tumor (chronic sclerosing sialadenitis)
of the submandibular gland, frequently are encountered in
FNA of the salivary glands. Included in this group is
sialolithiasis with duct obstruction.18,88 Clinically, such
lesions appear neoplastic. Long-standing chronic inflammation and sialolithiasis, as alluded to previously, may lead to
metaplastic changes in the ductal epithelium including squamous, mucous Image 18, and oncocytic metaplasia. These
cytologic changes result from a sequence of events initiated
by duct obstruction, followed by continued accumulation of
secretions (mucus) distally, eventually leading to cystic
dilatation, atrophy of the acinar cell component, fibrosis, and
metaplastic changes. Duct obstruction may be due to production of viscid secretions or calculi. Regardless of the pathogenesis, the importance of the cytologic changes relates to
the fact that they potentially may be confused with a variety
of salivary gland neoplasms. Metaplastic squamous and
mucous cells may be mistaken for intermediate or squamous
cells and mucus-producing cells of MEC, and when these cells
American Society for Clinical Pathology
Pathology Patterns Reviews
Image 18 Chronic sialadenitis and sialolithiasis. Scattered
chronic inflammatory infiltrate cells, fibrosis, mucous metaplasia
of the ductal epithelium. Acinar atrophy and dilatation of
some ducts are obvious in this histologic section (H&E, 400).
Image 19 Atypical squamous metaplasia in an aspirate
smear from a case of sialolithiasis and chronic sialadenitis
(rapid Romanowsky, 600).
are seen in situations where there is cystic dilatation with fluid
accumulation, an erroneous diagnosis of MEC is reinforced.
Squamous metaplastic cells with atypia Image 19 also may
raise the possibility of squamous cell carcinoma, although the
degree of atypia usually is mild in the former. When oncocytic
metaplasia is accompanied by chronic inflammatory cells
(small lymphocytes), an incorrect diagnosis of Warthin tumor
may be made. FNA of chronic sialadenitis may yield fibrotic
stroma that may show metachromasia on rapid Romanowsky
stain and, when seen together with ductal cells (which dominate such smears because of acinar cell atrophy) showing
metaplastic squamous differentiation, a diagnosis of pleomorphic adenoma may be considered. Although rare, identification of stone fragments in FNA smears of the salivary glands
should dissuade one from a diagnosis of a neoplastic tumor.
From the Department of Pathology, University of Arkansas for
Medical Sciences and Central Arkansas Veterans Healthcare
System, Little Rock.
Conclusion
FNA biopsy is a minimally invasive technique that has a
pivotal role in the diagnosis and management of patients with
salivary gland tumors. When performed properly, FNA
cytology can provide useful preoperative information about a
mass lesion arising in the salivary gland, permitting the clinician to appropriately manage the patient. However, extreme
care and recognition of the limitations of cytology are essential in the evaluation of salivary gland FNA material to
achieve the correct diagnoses, as there are many common
and rare tumors that can cause diagnostic confusion.
American Society for Clinical Pathology
Address reprint requests to Dr Mukunyadzi: Dept of
Pathology, Slot LR/113, Central Arkansas Veterans Healthcare
System, 4301 W 7th St, Little Rock, AR 72205.
References
1. ODwyer P, Farrar WB, James AG, et al. Needle aspiration
biopsy of major salivary gland tumors: its value. Cancer.
1986;57:867-869.
2. Jayaram N, Ashim D, Rajwanshi A, et al. The value of fine
needle aspiration biopsy in the cytodiagnosis of salivary gland
lesions. Diagn Cytopathol. 1989;5:349-354.
3. Dudgeon LS, Patrick CV. A new method for the rapid
microscopical diagnosis of tumours: with an account of 200
cases so examined. Br J Surg. 1927;15:250.
4. Qizilbash AH, Sianos J, Young JEM, et al. Fine needle
aspiration biopsy cytology of major salivary glands. Acta Cytol.
1985;29:503-512.
5. Layfield LJ, Tan P, Glasgow BJ. Fine-needle aspiration of
salivary gland lesions: comparison with frozen sections and
histologic findings. Arch Pathol Lab Med. 1987;111:346-353.
6. Mukunyadzi P, Bardales RH, Palmer HE, et al. Tissue effects of
salivary gland fine-needle aspiration: does this procedure
preclude accurate histologic diagnosis? Am J Clin Pathol.
2000;114:741-745.
7. Sauer T, Freng A, Djupesland P. Immediate interpretation of
FNA smears of the head and neck region. Diagn Cytopathol.
1992;8:116-122.
8. MacLeod CB, Frable WJ. Fine-needle aspiration biopsy of the
salivary gland: problem cases. Diagn Cytopathol. 1993;9:216-225.
Am J Clin Pathol 2002;118(Suppl 1):S100-S115
S113 DOI: 10.1092/5FECYJ9639CMQM0L
S113
S113
Mukunyadzi / FINE-NEEDLE ASPIRATION CYTOLOGY OF SALIVARY GLAND NEOPLASMS
9. Heller KS, Dubner S, Chess Q, et al. Value of fine needle
aspiration biopsy of salivary gland masses in clinical decision
making. Am J Surg. 1992;164:667-670.
10. Stanley MW. Head and neck cytology. In: Silverberg SG, ed.
Principles and Practice of Surgical Pathology and Cytopathology.
Vol 2. 3rd ed. New York, NY: Churchill Livingstone;
1997:995-1037.
11. Schwarz R, Chan NH, MacFarlane JK. Fine needle aspiration
cytology in the evaluation of head and neck masses. Am J
Surg. 1990;159:482-485.
12. Hajdu SI, Melamed MR. Limitations of aspiration cytology in
the diagnosis of primary neoplasms. Acta Cytol. 1984;28:337-345.
13. Cohen MB, Ljung B-ME, Boles R. Salivary gland tumors:
fine-needle aspiration vs frozen-section diagnosis. Arch
Otolaryngol Head Neck Surg. 1986;112:867-869.
14. Zakowski MF. Fine-needle aspiration of tumors: diagnostic
accuracy and potential pitfalls. Cancer Invest. 1991;12:505-515.
15. Layfield LJ, Glasgow BJ. Diagnosis of salivary gland tumors by
fine needle aspiration cytology: a review of clinical utility and
pitfalls. Diagn Cytopathol. 1991;7:267-272.
16. Kocjan G, Nayagam M, Harris M. Fine needle aspiration
cytology of salivary gland lesions: advantages and pitfalls.
Cytopathology. 1990;1:269-275.
17. Henry-Stanley MJ, Beneke J, Bardales RH, et al. Fine needle
aspiration of normal tissue from enlarged salivary glands:
sialosis, or missed target? Diagn Cytopathol. 1995;13:300-302.
18. Stanley MW, Bardales RH, Beneke J, et al. Sialolithiasis:
differential diagnostic problems in fine-needle aspiration
cytology. Am J Clin Pathol. 1996;106:229-233.
19. Schindler S, Nayar R, Dutra J, et al. Diagnostic challenges in
aspiration cytology of the salivary glands. Semin Diagn Pathol.
2001;18:124-146.
20. Kern SB. Necrosis of a Warthins tumor following fine needle
aspiration. Acta Cytol. 1988;32:207-208.
21. Pinto RG, Couto F, Mandreker S. Infarction after fine needle
aspiration: a report of four cases. Acta Cytol. 1996;40:739-741.
22. Skalova A, Starek I, Michal M, et al. Malignancy-simulating
change in parotid gland oncocytoma following fine needle
aspiration: a report of 3 cases. Pathol Res Pract. 1999;195:399405.
23. Batsakis JG, Sneige N, El-Naggar AK. Fine-needle aspiration
of salivary glands: its utility and tissue effects. Ann Otol Rhinol
Laryngol. 1992;101:185-188.
24. Moloo Z, Finley RJ, Lefcoe MS, et al. Possible spread of
bronchogenic carcinoma to the chest wall after a
transthoracic fine needle aspiration biopsy: a case report. Acta
Cytol. 1985;29:167-169.
25. Klijanienko J, Vielh P. Salivary Gland Tumours. Vol 15. Basel,
Switzerland: Karger; 2000:141.
26. Ellis GL, Auclair PL. Tumors of the Salivary Glands.
Washington, DC: Armed Forces Institute of Pathology;
1996:468. Atlas of Tumor Pathology; Third Series, Fascicle 17.
27. Viguer JM, Vicandi B, Jimenez-Heffernan JA, et al. Fine
needle aspiration cytology of pleomorphic adenoma: an
analysis of 212 cases. Acta Cytol. 1997;41:786-794.
28. Klijanienko J, Vielh P. Fine-needle sampling of salivary gland
lesions, I: cytology and histology correlation of 412 cases of
pleomorphic adenoma. Diagn Cytopathol. 1996;14:195-200.
29. Elsheikh TM, Bernacki EG. Fine needle aspiration cytology of
cellular pleomorphic adenoma. Acta Cytol. 1996;40:1165-1175.
30. Batsakis JG, El-Naggar AK. Sebaceous lesions of salivary glands
and oral cavity. Ann Otol Rhinol Laryngol. 1990;99:416-418.
S114
S114
Am J Clin Pathol 2002;118(Suppl 1):S100-S115
DOI: 10.1092/5FECYJ9639CMQM0L
31. Stanley MW, Lowhagen T. Mucin production by pleomorphic
adenomas of the parotid gland: a cytologic spectrum. Diagn
Cytopathol. 1990;6:49-52.
32. Hruban RH, Erozan YS, Zinreich SJ, et al. Fine needle
aspiration cytology of monomorphic adenomas. Am J Clin
Pathol. 1988;90:46-51.
33. Sparrow SA, Frost FA. Salivary monomorphic adenomas of
dermal analogue type: report of two cases. Diagn Cytopathol.
1993;9:300-303.
34. Gupta RK. Aspiration cytodiagnosis of dermal analogue
tumor, a rare subtype of salivary gland monomorphic
adenoma: a case report. Acta Cytol. 1996;40:331-334.
35. Kolda TF, Ardaman TDT, Schwartz MR. Eccrine spiradenoma
mimicking adenoid cystic carcinoma on fine needle
aspiration: a case report. Acta Cytol. 1997;41:852-858.
36. Stanley MW, Horwitz CA, Rollins SD, et al. Basal
(monomorphic) and minimally pleomorphic adenoma of the
salivary glands: distinction from the solid (anaplastic) type
adenoid cystic carcinoma in fine-needle aspiration. Am J Clin
Pathol. 1996;106:35-41.
37. Pisharodi LR. Basal cell adenocarcinoma of the salivary gland:
diagnosis by fine-needle aspiration cytology. Am J Clin Pathol.
1995;103:603-608.
38. Batsakis JG. Basal cell adenoma of the parotid gland. Cancer.
1972;29:226-230.
39. Hood IC, Qizilbash AH, Salama SS, et al. Basal cell
adenoma of the parotid: difficulty of differentiation from
adenoid cystic carcinoma on aspiration biopsy. Acta Cytol.
1983;27:515-520.
40. Brown D, Konzen B, Kashkari S. Fine needle aspiration
cytology of basal cell adenocarcinoma of salivary gland
[abstract]. Acta Cytol. 1994;38:853.
41. Klijanienko J, El-Naggar AK, Vielh P. Comparative cytologic
and histologic study of fifteen salivary basal-cell tumors:
differential diagnostic considerations. Diagn Cytopathol.
1999;21:30-34.
42. Chen KTK. Aspiration of metaplastic Warthins tumor
mimicking squamous cell carcinoma. Diagn Cytopathol.
1991;7:330-331.
43. Orell SR. Diagnostic difficulties in the interpretation of fine
needle aspirates of salivary gland lesions: the problem revisited.
Cytopathology. 1995;6:285-300.
44. Ballo MS, Shin HJC, Sneige N. Sources of diagnostic error in
the fine-needle aspiration diagnosis of Warthins tumor and
clues to a correct diagnosis. Diagn Cytopathol. 1997;17:230-234.
45. Finfer MD, Gallo L, Perchick A, et al. Fine needle aspiration
biopsy of cystic benign lymphoepithelial lesion of the parotid
gland in patients at risk for the acquired immune deficiency
syndrome. Acta Cytol. 1990;34:821-826.
46. Elliot JN, Oertel YC. Lymphoepithelial cysts of the salivary
glands: histologic and cytologic features. Am J Clin Pathol.
1990;93:39-43.
47. Klijanienko J, Vielh P. Fine-needle sampling of salivary gland
lesions, II: cytology and histology correlation of 71 cases of
Warthins tumor (adenolymphoma). Diagn Cytopathol.
1997;16:221-225.
48. Brandwein MS, Huvos AG. Oncocytic tumors of major
salivary glands: a study of 68 cases with follow-up of 44
patients. Am J Surg Pathol. 1984;15:514-528.
49. Abdul-Karim FW, Weaver MG. Needle aspiration cytology of
an oncocytic carcinoma of the parotid gland. Diagn
Cytopathol. 1991;7:420-422.
American Society for Clinical Pathology
Pathology Patterns Reviews
50. Dodd LG, Caraway NP, Luna MA, et al. Myoepithelioma of
the parotid: report of a case initially examined by fine needle
aspiration biopsy. Acta Cytol. 1994;38:417-421.
51. Batsakis JG. Myoepithelioma. Ann Otol Rhinol Laryngol.
1985;94:523-524.
52. Di Palma S, Alasio L, Pilotti S. Fine needle aspiration
appearances of malignant myoepithelioma of the parotid
gland. Cytopathology. 1996;7:357-365.
53. Katsuyama E, Kaneoka A, Higuchi K, et al. Myoepithelioma
of the soft palate. Acta Cytol. 1997;41:1856-1858.
54. Kumar N, Kapila K, Verma K. Fine needle aspiration cytology
of mucoepidermoid carcinoma: a diagnostic problem. Acta
Cytol. 1991;35:357-359.
55. Zajicek J, Eneroth CM, Jakobsson P. Aspiration biopsy of
salivary gland tumors, VI: morphologic studies on smears and
histologic sections from mucoepidermoid carcinoma. Acta
Cytol. 1966;20:35-41.
56. Evans HL. Mucoepidermoid carcinoma of salivary glands: a
study of 69 cases with special attention to histologic grading.
Am J Clin Pathol. 1984;81:696-701.
57. Klijanienko J, Vielh P. Fine-needle sampling of salivary gland
lesions, IV: review of 50 cases of mucoepidermoid carcinoma
with histologic correlation. Diagn Cytopathol. 1997;17:92-98.
58. Dejmek A, Lindholm K. Fine needle aspiration biopsy of
cystic lesion of the head and neck, excluding the thyroid. Acta
Cytol. 1990;34:443-448.
59. Hamed G, Shmookler BM, Ellis GL, et al. Oncocytic
mucoepidermoid carcinoma of the parotid gland. Arch Pathol
Lab Med. 1994;118:313-314.
60. Auclair PL. Tumor-associated lymphoid proliferation in the
parotid gland: a potential diagnostic pitfall. Oral Surg Oral
Med Oral Pathol. 1994;77:19-26.
61. Batsakis JG, Chinn EK, Weimert TA, et al. Acinic cell
carcinoma: a clinicopathologic study of thirty-five cases. J
Laryngol Otol. 1979;93:325-340.
62. Perzin KH, LiVolsi VA. Acinic cell carcinoma arising in the
salivary glands: a clinicopathologic study. Cancer.
1979;44:1434-1457.
63. Nagel H, Laskawi R, Butter JJ, et al. Cytologic diagnosis of
acinic-cell carcinoma of salivary glands. Diagn Cytopathol.
1997;16:402-412.
64. Klijanienko J, Vielh P. Fine-needle sampling of salivary gland
lesions, V: cytology of 22 cases of acinic cell carcinoma with
histologic correlation. Diagn Cytopathol. 1997;17:347-352.
65. Sauer T, Jebsen PW, Olshot R. Cytologic features of papillarycystic variant of acinic-cell adenocarcinoma: a case report.
Diagn Cytopathol. 1994;10:30-32.
66. Layfield LJ, Glasgow BJ. Aspiration cytology of clear-cell
lesions of the parotid gland: morphologic features and
differential diagnosis. Diagn Cytopathol. 1993;9:705-712.
67. Palma O, Torri AM, de Cristofaro JA, et al. Fine needle
aspiration cytology in two cases of well-differentiated aciniccell carcinoma of the parotid gland: discussion of diagnostic
criteria. Acta Cytol. 1985;29:516-521.
68. Klijanienko J, Vielh P. Fine-needle sampling of salivary gland
lesions, III: cytology and histologic correlation of 75 cases of
adenoid cystic carcinoma: review and experience at the
Institut Curie with emphasis on cytologic pitfalls. Diagn
Cytopathol. 1997;17:36-41.
69. Nagel H, Hotze HJ, Laskawi R, et al. Cytologic diagnosis of
adenoid cystic carcinoma of the salivary glands. Diagn
Cytopathol. 1999;20:258-366.
American Society for Clinical Pathology
70. Cameron WR, Johansson L, Tennvall J. Small cell carcinoma
of the parotid: fine needle aspiration and immunochemical
findings in a case. Acta Cytol. 1990;34:837-841.
71. Haba R, Kobayashi S, Miki H, et al. Polymorphous low-grade
adenocarcinoma of submandibular gland origin. Acta Cytol.
1993;43:774-778.
72. Gibbons D, Saboorian MH, Vuitch F, et al. Fine-needle
aspiration findings in patients with polymorphous low grade
adenocarcinoma of the salivary glands. Cancer. 1999;87:31-36.
73. Evans HL, Batsakis JG. Polymorphous low-grade
adenocarcinoma of minor salivary glands: a study of 14 cases
of a distinctive neoplasm. Cancer. 1984;53:935-942.
74. Ritland F, Lubensky I, LiVolsi VA. Polymorphous low-grade
adenocarcinoma of the parotid salivary gland. Arch Pathol Lab
Med. 1993;117:1261-1263.
75. Feldman PS, Kaplan MJ, Johns ME, et al. Fine-needle
aspiration in squamous cell carcinoma of the head and neck.
Arch Otolaryngol. 1983;109:735-742.
76. Delgado R, Klimstra D, Albores-Saavedra J. Low grade
salivary duct carcinoma, a distinctive variant with a low grade
histology and a predominant intraductal growth pattern.
Cancer. 1996;78:958-967.
77. Colecchia M, Frigio B, Leopardi O. Salivary duct carcinoma
of the parotid gland. Acta Cytol. 1997;41:593-597.
78. Elsheikh T, Bernaacki E, Pisharodi L. Fine-needle aspiration
cytology of salivary duct carcinoma. Diagn Cytopathol.
1994;11:47-51.
79. Klijanienko J, Vielh P. Cytologic characteristics and
histomorphologic correlations of 21 salivary duct carcinomas.
Diagn Cytopathol. 1998;19:333-337.
80. Khurana KK, Pitman MB, Powers CN, et al. Diagnostic
pitfalls of aspiration cytology of salivary duct carcinoma.
Cancer. 1997;81:373-378.
81. Chen KT. Cytology of salivary duct carcinoma. Diagn
Cytopathol. 2000;22:132-134.
82. Anand A, Brockie ES. Cytomorphological features of salivary
duct carcinoma ex pleomorphic adenoma: diagnosis by fine
needle aspiration biopsy with histologic correlation. Diagn
Cytopathol. 1999;20:375-378.
83. Derias NW, Chong WH, Pambakian H. Sebaceous adenoma
of parotid gland: a rare tumour diagnosed by fine needle
aspiration cytology. Cytopathology. 1994;5:392-395.
84. Latkovich P, Johnson RL. Carcinosarcoma of the parotid
gland; report of a case with cytohistologic correlation and
immunohistochemical findings. Arch Pathol Lab Med.
1998;122:743-746.
85. Tao LC, Gullane PJ. HIV infectionassociated
lymphoepithelial lesions of the parotid gland: aspiration
biopsy cytology, histology, and pathogenesis. Diagn Cytopathol.
1991;7:158-162.
86. Harris NL. Lymphoid proliferations of the salivary glands. Am
J Clin Pathol. 1999;111(1 suppl 1):S94-S103.
87. Tworek JA, Michael CW. Parotid gland mucosa associated
lymphomas and their cytologic mimics. Semin Diagn.
2001;18:147-150.
88. Chai C, Dodd LG, Glasgow BJ, et al. Salivary gland lesions
with a prominent lymphoid component: cytologic findings
and differential diagnosis by fine-needle aspiration biopsy.
Diagn Cytopathol. 1997;17:183-190.
89. Stewart CJ, Jackson R, Farquharson M, et al. Fine-needle
aspiration cytology of extranodal lymphoma. Diagn
Cytopathol. 1998;19:260-266.
Am J Clin Pathol 2002;118(Suppl 1):S100-S115
S115 DOI: 10.1092/5FECYJ9639CMQM0L
S115
S115
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5822)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (852)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (898)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (349)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (403)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- (Arthritis) - Away With ArthritisDocument3 pages(Arthritis) - Away With ArthritisPedpix Pedpix100% (1)
- SexDocument74 pagesSexbill jons0% (1)
- Healthy Vision-Prevent and Reverse Eye Disease Through Better NutritionDocument105 pagesHealthy Vision-Prevent and Reverse Eye Disease Through Better NutritionAnh Ngô Đức100% (2)
- The Use of Soothers and Nipple ShieldsDocument4 pagesThe Use of Soothers and Nipple Shieldsabdulaleem1No ratings yet
- Fellowship in CytopathologyDocument6 pagesFellowship in Cytopathologyabdulaleem1No ratings yet
- Union Health Care - Premium Chart (2021-22) : Age Less Than 45Document1 pageUnion Health Care - Premium Chart (2021-22) : Age Less Than 45abdulaleem1No ratings yet
- Slide Presentation Handout For SCE ASC 2014Document48 pagesSlide Presentation Handout For SCE ASC 2014abdulaleem1No ratings yet
- Vista KeyDocument1 pageVista Keyabdulaleem1No ratings yet
- Gynae Cyto GlandularDocument50 pagesGynae Cyto Glandularabdulaleem1No ratings yet
- Lecture 7Document68 pagesLecture 7Gay TonyNo ratings yet
- Cure Is Not A 4 Letter WordDocument3 pagesCure Is Not A 4 Letter WordraineeeeeNo ratings yet
- Mental Retardation: By: Louwella G. Padasas Bsed-English IiDocument19 pagesMental Retardation: By: Louwella G. Padasas Bsed-English IiJustine Sican QueNo ratings yet
- DeFronzo Et Al-2012-Diabetes, Obesity and MetabolismDocument10 pagesDeFronzo Et Al-2012-Diabetes, Obesity and MetabolismlguerreroNo ratings yet
- Developmental Disturbances in Oral CavityDocument14 pagesDevelopmental Disturbances in Oral CavityYashmeen XNo ratings yet
- PKC Activation During Training Restores Mushroom Spine Synapses and Memory in The Aged RatDocument19 pagesPKC Activation During Training Restores Mushroom Spine Synapses and Memory in The Aged RatAnonymous BOEbvxUqBNo ratings yet
- Site-Directed Mutagenesis - Wikipedia, The Free EncyclopediaDocument6 pagesSite-Directed Mutagenesis - Wikipedia, The Free EncyclopediaAlviro CossemeNo ratings yet
- LachmannnDocument40 pagesLachmannnSai ManishaNo ratings yet
- History of The SADS Foundation and Long QT SyndromeDocument4 pagesHistory of The SADS Foundation and Long QT Syndromeapi-341217779No ratings yet
- Approach To Pancytopenia: Moderator - DR Vishal Gupta MD Medicine Presented By-Dr Narendra Singh Resident Doctor 2Document35 pagesApproach To Pancytopenia: Moderator - DR Vishal Gupta MD Medicine Presented By-Dr Narendra Singh Resident Doctor 2ntnquynhproNo ratings yet
- ArachnophobiaDocument2 pagesArachnophobiapopoNo ratings yet
- Nutrients 06 01782Document27 pagesNutrients 06 01782jasonc13No ratings yet
- Historyof Genetics QuizDocument2 pagesHistoryof Genetics QuizGelli NancaNo ratings yet
- Human Immunodeficiency VirusDocument87 pagesHuman Immunodeficiency Virustummalapalli venkateswara raoNo ratings yet
- IOSR Journal of Pharmacy (IOSRPHR)Document4 pagesIOSR Journal of Pharmacy (IOSRPHR)IOSR Journal of PharmacyNo ratings yet
- Big Data and GenomicsDocument54 pagesBig Data and GenomicsNational Press FoundationNo ratings yet
- NocardiaDocument3 pagesNocardiasujithas0% (1)
- Soal AdaptiveDocument4 pagesSoal AdaptiveLiany SusantiNo ratings yet
- How To Transfer A Mobilizable Plasmid From A Cell Without A Conjugative Plasmid?Document14 pagesHow To Transfer A Mobilizable Plasmid From A Cell Without A Conjugative Plasmid?m86544422No ratings yet
- 7-Pediatric - Drug TherapyDocument42 pages7-Pediatric - Drug TherapyDyn Adriani100% (1)
- Pt. Pathlab Indonesia: (Laboratorium Klinik)Document1 pagePt. Pathlab Indonesia: (Laboratorium Klinik)Aghiest Utungga Al BirruNo ratings yet
- ST LuciaDocument39 pagesST LuciablinkshiftNo ratings yet
- Drug-Induced Taste Disorders in Clinical Practice and Preclinical Safety EvaluationDocument10 pagesDrug-Induced Taste Disorders in Clinical Practice and Preclinical Safety EvaluationBharat NarumanchiNo ratings yet
- CH 2 & 3 - Theories and PrenatalDocument21 pagesCH 2 & 3 - Theories and PrenatalScribdNo ratings yet
- Caspofungin: InvitedarticleDocument13 pagesCaspofungin: InvitedarticleIris GalvánNo ratings yet
- Monosodium Glutamate (MSG) : The Cause of Chinese Restaurant SyndromeDocument7 pagesMonosodium Glutamate (MSG) : The Cause of Chinese Restaurant SyndromeWidjaya HS TeacherNo ratings yet
- Aspergillus SPDocument10 pagesAspergillus SPSandu PaulNo ratings yet