Professional Documents
Culture Documents
Kinney: The Potential of Captive Medical Liability Insurance Carriers and Damage Caps For Real Malpractice Reform
Kinney: The Potential of Captive Medical Liability Insurance Carriers and Damage Caps For Real Malpractice Reform
Uploaded by
New England Law ReviewCopyright:
Available Formats
You might also like
- Bisb - Bank StatementDocument23 pagesBisb - Bank Statementazstartup.bhNo ratings yet
- The Profit Motive and Patient CareDocument448 pagesThe Profit Motive and Patient CareTCFdotorgNo ratings yet
- PESTLE Analysis For Rolls RoyceDocument2 pagesPESTLE Analysis For Rolls Roycephi podcastNo ratings yet
- Berman: ForewordDocument7 pagesBerman: ForewordNew England Law ReviewNo ratings yet
- Medical MalpracticeDocument469 pagesMedical MalpracticeMuhammad Ali100% (1)
- 8sfnf Medical MalpracticeDocument469 pages8sfnf Medical MalpracticeSana Khairi100% (2)
- Responsibility Verses ControlDocument25 pagesResponsibility Verses ControlrangababNo ratings yet
- Of Swords and Shields - The Role of Clinical Pratice Guidelines inDocument66 pagesOf Swords and Shields - The Role of Clinical Pratice Guidelines inAastha SinghNo ratings yet
- Heading Towards A Single Government Payer SystemDocument4 pagesHeading Towards A Single Government Payer SystemNeelkumar SoniNo ratings yet
- Health Care Policy and Delivery Systems SyllabusDocument6 pagesHealth Care Policy and Delivery Systems SyllabusDeekay100% (1)
- Izakt Bibliography-Rws1301Document5 pagesIzakt Bibliography-Rws1301api-325497433No ratings yet
- Policy Brief 3 ThelenDocument16 pagesPolicy Brief 3 ThelenCarol ThelenNo ratings yet
- Willard and Spackman's Occupational Therapy 11th Edition Chapter 74 PDF FreeDocument25 pagesWillard and Spackman's Occupational Therapy 11th Edition Chapter 74 PDF FreeTracy NguyenNo ratings yet
- Surgeons and Medical Liability PrimerDocument36 pagesSurgeons and Medical Liability PrimerJack BenaventeNo ratings yet
- Afforable Care Act FinalDocument64 pagesAfforable Care Act FinalArafat MazharNo ratings yet
- Health Care Reform DissertationDocument6 pagesHealth Care Reform DissertationDoMyPaperForMeEverett100% (1)
- Healthcare Is Not A Part of Your Bill of RightsDocument10 pagesHealthcare Is Not A Part of Your Bill of Rightsapi-643881078No ratings yet
- Lang - Diskusija ObameDocument7 pagesLang - Diskusija ObameanlaucNo ratings yet
- Annotated Bibliography Eng 112Document6 pagesAnnotated Bibliography Eng 112api-511289341No ratings yet
- Does The Doctor Need A Boss?, Cato Briefing Paper No. 111Document12 pagesDoes The Doctor Need A Boss?, Cato Briefing Paper No. 111Cato InstituteNo ratings yet
- Medical Malpractice ReformsDocument18 pagesMedical Malpractice ReformsUsman Naroo100% (1)
- Health Care Delivery Models and Nursing Practice 2Document6 pagesHealth Care Delivery Models and Nursing Practice 2DennisNo ratings yet
- Infertility Treatment Markets The Effects of CompeDocument44 pagesInfertility Treatment Markets The Effects of CompeMohamed SalahNo ratings yet
- 2011-Evaluating The Medical Malpractice System and Options ForDocument16 pages2011-Evaluating The Medical Malpractice System and Options ForHening Tirta KusumawardaniNo ratings yet
- Medical Savings Accounts: Answering The Critics, Cato Policy AnalysisDocument12 pagesMedical Savings Accounts: Answering The Critics, Cato Policy AnalysisCato InstituteNo ratings yet
- Research Paper in Health EconomicsDocument6 pagesResearch Paper in Health Economicscaqllprhf100% (1)
- Identifying and Resolving Disputes in New Accountable Care SettingsDocument10 pagesIdentifying and Resolving Disputes in New Accountable Care SettingsRothHealthLawNo ratings yet
- Ethical Case Analysis PaperDocument14 pagesEthical Case Analysis Paperapi-282129457100% (1)
- Health and Medicine LawDocument9 pagesHealth and Medicine Lawshikhar shuklaNo ratings yet
- Systemic Negligence and NHS Hospitals AnUnderutilised ArgumentDocument30 pagesSystemic Negligence and NHS Hospitals AnUnderutilised ArgumentanharjutsuNo ratings yet
- Retail Business Laws: A Critical Analysis of Health Care SectorDocument5 pagesRetail Business Laws: A Critical Analysis of Health Care SectorAKHILA GOPAKUMAR-RM 21RM905No ratings yet
- Negligence Liability in Medical Examination and Treatment in Vietnam in Comparision ReviewDocument22 pagesNegligence Liability in Medical Examination and Treatment in Vietnam in Comparision ReviewsimonpeternekesaNo ratings yet
- Five Myths About Medical NegligenceDocument12 pagesFive Myths About Medical NegligenceLateNightRomeNo ratings yet
- National Health Insurance FailureDocument4 pagesNational Health Insurance FailureGaddafi PhelixNo ratings yet
- Policy Action Plan - Physician ShortageDocument11 pagesPolicy Action Plan - Physician Shortageapi-349372265No ratings yet
- Medical MalpracticeDocument29 pagesMedical MalpracticeBuruiana Andrei Richard0% (1)
- Furrow: Adverse Events and Patient InjuryDocument37 pagesFurrow: Adverse Events and Patient InjuryNew England Law Review100% (1)
- Module Two 1Document3 pagesModule Two 1api-612975585No ratings yet
- Mining for Gold In a Barren Land: Pioneer Accountable Care Organization Potential to Redesign the Healthcare Business Model in a Post-Acute SettingFrom EverandMining for Gold In a Barren Land: Pioneer Accountable Care Organization Potential to Redesign the Healthcare Business Model in a Post-Acute SettingNo ratings yet
- Hospital As FactoryDocument4 pagesHospital As FactoryecartetescuissesNo ratings yet
- Jurnal HBMDocument10 pagesJurnal HBMSeindz OstenNo ratings yet
- Hme 2301 Topic 3Document6 pagesHme 2301 Topic 3Mofy AllyNo ratings yet
- Coursematerial 214Document16 pagesCoursematerial 214Francisco Reyes IslaNo ratings yet
- Anatomy of Health InsuranceDocument124 pagesAnatomy of Health InsurancesimerjeetNo ratings yet
- Deadly Ties and The Rise of Multi-Drug Resistant Infections: A Case For A New Health Care Practitioner Hygienic Dress CodeDocument20 pagesDeadly Ties and The Rise of Multi-Drug Resistant Infections: A Case For A New Health Care Practitioner Hygienic Dress CodeRich AzzopardiNo ratings yet
- Physicians Us Versus HospitalsDocument4 pagesPhysicians Us Versus Hospitalssavvy_as_98-1No ratings yet
- Mckeon: New York's Innovative Approach To Medical MalpracticeDocument13 pagesMckeon: New York's Innovative Approach To Medical MalpracticeNew England Law ReviewNo ratings yet
- The Fine Line of Defensive Medicine PDFDocument3 pagesThe Fine Line of Defensive Medicine PDFEMMA LAURA MORALES GONZALEZNo ratings yet
- HADM 4326 Assignment 1Document4 pagesHADM 4326 Assignment 1saraNo ratings yet
- Affordable Care Act ThesisDocument5 pagesAffordable Care Act Thesisgbtrjrap100% (1)
- DDJHPPL 23 4 661Document26 pagesDDJHPPL 23 4 661AlexNo ratings yet
- Eff Ects of The Medical Liability System in Australia, The UKDocument7 pagesEff Ects of The Medical Liability System in Australia, The UKesther kwanNo ratings yet
- Dr. Ram Manohar Lohiya National Law University, Lucknow: Academic Session: 2018 - 19Document12 pagesDr. Ram Manohar Lohiya National Law University, Lucknow: Academic Session: 2018 - 19Aditi VatsaNo ratings yet
- Themedicalliability System:Essential Informationforthe HospitalistDocument12 pagesThemedicalliability System:Essential Informationforthe Hospitalistjoaquín_chavollaNo ratings yet
- How To Write A Research Paper On Health Care ReformDocument7 pagesHow To Write A Research Paper On Health Care Reformlyn0l1gamop2No ratings yet
- Thesis Statement Against The Affordable Care ActDocument6 pagesThesis Statement Against The Affordable Care Actjanetrobinsonjackson100% (2)
- American Medicine: The Quest for CompetenceFrom EverandAmerican Medicine: The Quest for CompetenceRating: 3 out of 5 stars3/5 (1)
- BibliographyDocument3 pagesBibliographyapi-253028254No ratings yet
- EpisodeBasedPayment PerspectivesforConsiderationDocument24 pagesEpisodeBasedPayment PerspectivesforConsiderationHazelnutNo ratings yet
- The New Hospital-Physician Enterprise: Meeting the Challenges of Value-Based CareFrom EverandThe New Hospital-Physician Enterprise: Meeting the Challenges of Value-Based CareNo ratings yet
- Solution Manual For Health Care Management and The Law Principles and Applications 1st EditionDocument37 pagesSolution Manual For Health Care Management and The Law Principles and Applications 1st Editioneozoicjaggern2ni4100% (19)
- Why State Constitutions MatterDocument12 pagesWhy State Constitutions MatterNew England Law ReviewNo ratings yet
- Reforming The NYPD and Its Enablers Who Thwart ReformDocument44 pagesReforming The NYPD and Its Enablers Who Thwart ReformNew England Law ReviewNo ratings yet
- 101 99% Human and 1%animal? Patentable Subject Matter and Creating Organs Via Interspecies Blastocyst Complementation by Jerry I-H HsiaoDocument23 pages101 99% Human and 1%animal? Patentable Subject Matter and Creating Organs Via Interspecies Blastocyst Complementation by Jerry I-H HsiaoNew England Law ReviewNo ratings yet
- "Swear Not at All": Time To Abandon The Testimonial OathDocument52 pages"Swear Not at All": Time To Abandon The Testimonial OathNew England Law ReviewNo ratings yet
- Reformation of The Supreme Court: Keeping Politics OutDocument22 pagesReformation of The Supreme Court: Keeping Politics OutNew England Law ReviewNo ratings yet
- The Massachusetts Sexually Dangerous Persons Statute: A Critique of The Unanimous Jury Verdict Requirement by Widmaier CharlesDocument17 pagesThe Massachusetts Sexually Dangerous Persons Statute: A Critique of The Unanimous Jury Verdict Requirement by Widmaier CharlesNew England Law ReviewNo ratings yet
- Employment Discrimination: Pretext, Implicit Bias, and The Beast of BurdensDocument27 pagesEmployment Discrimination: Pretext, Implicit Bias, and The Beast of BurdensNew England Law Review100% (1)
- The Fight Against Online Sex Trafficking: Why The Federal Government Should View The Internet As A Tool and Not A WeaponDocument16 pagesThe Fight Against Online Sex Trafficking: Why The Federal Government Should View The Internet As A Tool and Not A WeaponNew England Law ReviewNo ratings yet
- Section 43 (A) in A Vacuum: Cleaning Up False Advertising in An Unfair Competition MessDocument14 pagesSection 43 (A) in A Vacuum: Cleaning Up False Advertising in An Unfair Competition MessNew England Law ReviewNo ratings yet
- Combating The Opioid Crisis: The Department of Health and Human Services Must Update EMTALADocument21 pagesCombating The Opioid Crisis: The Department of Health and Human Services Must Update EMTALANew England Law ReviewNo ratings yet
- Harvesting Hope: Regulating and Incentivizing Organ DonationDocument31 pagesHarvesting Hope: Regulating and Incentivizing Organ DonationNew England Law ReviewNo ratings yet
- Cuz I'm Young & I'm Black & My Hat's Real Low: Constitutional Rights To The Political Franchise For Parolees Under Equal Protection by Shaylen Roberts, Esq.Document33 pagesCuz I'm Young & I'm Black & My Hat's Real Low: Constitutional Rights To The Political Franchise For Parolees Under Equal Protection by Shaylen Roberts, Esq.New England Law ReviewNo ratings yet
- The Shadowy Law of Modern Surveillance by Gina AbbadessaDocument3 pagesThe Shadowy Law of Modern Surveillance by Gina AbbadessaNew England Law ReviewNo ratings yet
- An "Obvious Truth": How Underfunded Public Defender Systems Violate Indigent Defendants' Right To CounselDocument30 pagesAn "Obvious Truth": How Underfunded Public Defender Systems Violate Indigent Defendants' Right To CounselNew England Law ReviewNo ratings yet
- Trademarks and Twitter: The Costs and Benefits of Social Media On Trademark Strength, and What This Means For Internet-Savvy CelebsDocument25 pagesTrademarks and Twitter: The Costs and Benefits of Social Media On Trademark Strength, and What This Means For Internet-Savvy CelebsNew England Law ReviewNo ratings yet
- Revealing A Necessary Evil: The United States Must Continue To Use Some Form of Domesticated Counter-Terrorism Program by Daniel R. GodefroiDocument17 pagesRevealing A Necessary Evil: The United States Must Continue To Use Some Form of Domesticated Counter-Terrorism Program by Daniel R. GodefroiNew England Law ReviewNo ratings yet
- Outer Space and International Geography Article II and The Shape of Global OrderDocument29 pagesOuter Space and International Geography Article II and The Shape of Global OrderNew England Law ReviewNo ratings yet
- Augustine and Estabrook: Defying The Third-Party Doctrine by Michael LockeDocument13 pagesAugustine and Estabrook: Defying The Third-Party Doctrine by Michael LockeNew England Law ReviewNo ratings yet
- “The Legalization of Recreational Marijuana in Massachusetts and the Limits of Social Justice for Minorities and Communities Disproportionately Impacted by Prior Marijuana Laws and Drug Enforcement Policies”Document13 pages“The Legalization of Recreational Marijuana in Massachusetts and the Limits of Social Justice for Minorities and Communities Disproportionately Impacted by Prior Marijuana Laws and Drug Enforcement Policies”New England Law ReviewNo ratings yet
- Death by 1000 Lawsuits: The Public Litigation in Response To The Opioid Crisis Will Mirror The Global Tobacco Settlement of The 1990s by Paul L. KeenanDocument26 pagesDeath by 1000 Lawsuits: The Public Litigation in Response To The Opioid Crisis Will Mirror The Global Tobacco Settlement of The 1990s by Paul L. KeenanNew England Law ReviewNo ratings yet
- Ojukwu Final 3Document26 pagesOjukwu Final 3New England Law ReviewNo ratings yet
- Ignorance Is Bliss: Why The Human Mind Prevents Defense Attorneys From Providing Zealous Representation While Knowing A Client Is GuiltyDocument25 pagesIgnorance Is Bliss: Why The Human Mind Prevents Defense Attorneys From Providing Zealous Representation While Knowing A Client Is GuiltyNew England Law ReviewNo ratings yet
- Secret Law and The Snowden Revelations: A Response To The Future of Foreign Intelligence: Privacy and Surveillance in A Digital Age, by Laura K. Donohue by HEIDI KITROSSERDocument10 pagesSecret Law and The Snowden Revelations: A Response To The Future of Foreign Intelligence: Privacy and Surveillance in A Digital Age, by Laura K. Donohue by HEIDI KITROSSERNew England Law ReviewNo ratings yet
- A Citizens Commission For The 28 Amendment: Massachusetts Advances Constitutional Reform of Our Broken Political SystemDocument8 pagesA Citizens Commission For The 28 Amendment: Massachusetts Advances Constitutional Reform of Our Broken Political SystemNew England Law ReviewNo ratings yet
- Remnants of Information Privacy in The Modern Surveillance State by Lawrence FriedmanDocument15 pagesRemnants of Information Privacy in The Modern Surveillance State by Lawrence FriedmanNew England Law ReviewNo ratings yet
- Unconstitutional Constitutional Change by Courts: NtroductionDocument23 pagesUnconstitutional Constitutional Change by Courts: NtroductionNew England Law ReviewNo ratings yet
- New Light On State Constitutional ChangeDocument4 pagesNew Light On State Constitutional ChangeNew England Law ReviewNo ratings yet
- Mechanisms of Accountability Fundamental To An Independent JudiciaryDocument6 pagesMechanisms of Accountability Fundamental To An Independent JudiciaryNew England Law ReviewNo ratings yet
- Collins Final 3Document20 pagesCollins Final 3New England Law ReviewNo ratings yet
- V.51-3 TOC FinalDocument2 pagesV.51-3 TOC FinalNew England Law ReviewNo ratings yet
- 1LOC005 - How Do I Allocate Legs To A Drivers Run SheetDocument2 pages1LOC005 - How Do I Allocate Legs To A Drivers Run Sheetguolidong2017No ratings yet
- Slug LowDocument13 pagesSlug LowDr Mohammed AzharNo ratings yet
- The Elusive Chemical Potential PDFDocument12 pagesThe Elusive Chemical Potential PDFbonesisaliveNo ratings yet
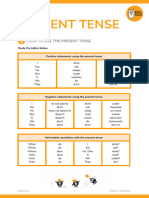
- (TV) Present TenseDocument8 pages(TV) Present TenseDe Aparicio DenisseNo ratings yet
- The Company Name Has Evolved Over Its 100 Years in BusinessDocument6 pagesThe Company Name Has Evolved Over Its 100 Years in BusinessFrancisco UrizarNo ratings yet
- Biography of Jamgön Ju MiphamDocument6 pagesBiography of Jamgön Ju MiphamBLhundrupNo ratings yet
- Result Phase III - A, B - Lot (23!03!2024)Document15 pagesResult Phase III - A, B - Lot (23!03!2024)xxxlordimpalerxxxNo ratings yet
- Vine-Vpdc Report As of Feb. 3, 2022Document9 pagesVine-Vpdc Report As of Feb. 3, 2022Elbert Ryan OcampoNo ratings yet
- Assembly BuildingDocument1 pageAssembly BuildingHarshit RajNo ratings yet
- Wvsu NCM 106 Sample Lesson PlanDocument10 pagesWvsu NCM 106 Sample Lesson Plangreen_archerNo ratings yet
- Online Marketing EssentialsDocument508 pagesOnline Marketing EssentialsElena BotezatuNo ratings yet
- Gravoca 1C 본문 170705 인쇄용Document192 pagesGravoca 1C 본문 170705 인쇄용GreysenNo ratings yet
- Class - 12th Annual ReportDocument4 pagesClass - 12th Annual ReportPreksha SharmaNo ratings yet
- MDR11 InstructionsDocument4 pagesMDR11 Instructionsjuan tellezNo ratings yet
- Ceramics II Project Ideas Spring 2019Document2 pagesCeramics II Project Ideas Spring 2019api-170572422No ratings yet
- Surface Preparation Standards JotunDocument2 pagesSurface Preparation Standards JotunbacabacabacaNo ratings yet
- Konsep Pendidikan Religius RasionalDocument14 pagesKonsep Pendidikan Religius RasionalSri ParwatiNo ratings yet
- How Deep Is Your LoveDocument1 pageHow Deep Is Your LoveJanina JaworskiNo ratings yet
- 1430-Article Text-4196-2-10-20220929Document21 pages1430-Article Text-4196-2-10-20220929Annisa SophiaNo ratings yet
- Samsung Brittle Fracture Evaluation - Additional Scope P23-0105-R3Document5 pagesSamsung Brittle Fracture Evaluation - Additional Scope P23-0105-R3Vipin NairNo ratings yet
- Anyone Who Had A Heart - A Case Study in PhysiologyDocument9 pagesAnyone Who Had A Heart - A Case Study in PhysiologyJohnSnow0% (1)
- NXF Perforated Cable Tray en 2017Document65 pagesNXF Perforated Cable Tray en 2017LANKAPALLISURINo ratings yet
- Birth QnaDocument8 pagesBirth QnaaliazgarNo ratings yet
- PDF - Marine Bio Semester One Review SheetDocument2 pagesPDF - Marine Bio Semester One Review Sheetapi-205313794No ratings yet
- Unit 1 Prog Logic DevelopmentDocument8 pagesUnit 1 Prog Logic DevelopmentAtharv KhadatareNo ratings yet
- Test Report Quadplexer 4in1outDocument8 pagesTest Report Quadplexer 4in1outHagniAryaGunadiNo ratings yet
- Safety Instrumented Systems: GlobalDocument410 pagesSafety Instrumented Systems: Globalmohammed el erianNo ratings yet
- Model Name: GA-B75M-D2V: Gigabyte TechnologyDocument26 pagesModel Name: GA-B75M-D2V: Gigabyte TechnologyMaaf GarenaNo ratings yet
Kinney: The Potential of Captive Medical Liability Insurance Carriers and Damage Caps For Real Malpractice Reform
Kinney: The Potential of Captive Medical Liability Insurance Carriers and Damage Caps For Real Malpractice Reform
Uploaded by
New England Law ReviewOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Kinney: The Potential of Captive Medical Liability Insurance Carriers and Damage Caps For Real Malpractice Reform
Kinney: The Potential of Captive Medical Liability Insurance Carriers and Damage Caps For Real Malpractice Reform
Uploaded by
New England Law ReviewCopyright:
Available Formats
KINNEY FINAL (DO NOT DELETE)
3/31/2012 11:29 AM
The Potential of Captive Medical Liability
Insurance Carriers and Damage Caps for
Real Malpractice Reform
ELEANOR D. KINNEY
ABSTRACT
Medical malpractice continues to be a contentious health policy issue
particularly from the perspective of physicians and patients. The medical
malpractice insurance market as a whole has changed considerably since
the mid-1970s, with widely fluctuating premium prices and crises in the
availability and affordability of medical malpractice insurance. More
recently, hospitals and physicians have increasingly chosen to self-insure
through a variety of vehicles including captive insurance companies.
This Article suggests that two existing strategies can be intentionally
designed and coordinated to facilitate the fair and expeditious resolution of
medical malpractice claims. Specifically, captive insurance companies
operating in states with damage caps can work more effectively with
healthcare providers to resolve identified malpractice claims, and they can
identify and compensate medical injury where claims are not pressed. This
knowledge establishes space for the providers and the captive insurers to
settle claims expeditiously and fairly. The space also enables the providers
and the captive insurers to go further and express apologies to patients
who have been injured in the care process. However, the National
Practitioner Data Bank under the Health Care Quality Improvement Act of
1986 poses challenges for physicians in participating in captives. This
article explores how captives can be structured and barriers addressed to
mitigate the problems for physicians and to improve the management of
medical error for all stakeholders.
*J.D., Duke University School of Law, 1973; MPH, University of North Carolina School
of Public Health, 1979; Hall Render Professor of Law Emerita, Hall Center for Law and
Health, Indiana University Robert H. McKinney School of Law. I would like to thank Mark
Harbin and Miriam Murphy for their contributions to this Article.
489
KINNEY FINAL (DO NOT DELETE)
490
3/31/2012 11:29 AM
New England Law Review
v. 46 | 489
INTRODUCTION
edical malpractice continues to be a contentious health policy
issue particularly from the perspective of physicians and other
healthcare providers.1 For patients, physicians, and other
healthcare providers, medical injury and liability are difficult problems.
Physicians and their associations devote more time and energy advocating
for the reform of medical liability systems than almost any other health
policy issue.2 They argue that physicians practice defensive medicine to
reduce their exposure to medical malpractice claims and that this
phenomenon is a great contributor to escalating healthcare costs.3 Some
evidence suggests that the claims about the problem of medical malpractice
and the impact of defensive medicine on medical costs are overblown.4
Nevertheless, the issue of medical malpractice clearly animates the medical
profession, as well as patients, and warrants action by policymakers.
The medical malpractice insurance market as a whole has changed
considerably since the mid-1970s and years following, with widely
fluctuating premium prices and crises in the availability and affordability
of medical malpractice insurance. 5 States enacted laws to slow the increase
in medical malpractice premium rates through reducing the frequency and
severity of claims.6 Physicians formed mutual, nonprofit insurance
1 See William M. Sage & Rogan Kersh, Introduction to MEDICAL MALPRACTICE AND THE U.S.
HEALTHCARE SYSTEM 1 (William M. Sage & Rogan Kersh eds., 2006); FRANK A. SLOAN &
LINDSEY M. CHEPKE, MEDICAL MALPRACTICE 1-2 (2008); Kenneth E. Thorpe, The Medical
Malpractice Crisis: Recent Trends and the Impact of State Tort Reforms, HEALTH AFF., W4-20 (Jan.
21, 2004), http://content.healthaffairs.org/content/early/2004/01/21/hlthaff.w4.20.full.pdf+html.
2 See Current Topics in Advocacy, AM. MED. ASSN, http://www.ama-assn.org/ama/pub/
advocacy/current-topics-advocacy.page (last visited Mar. 30, 2012).
3 See Daniel P. Kessler & Mark B. McClellan, Do Doctors Practice Defensive Medicine? 111 Q.J.
ECON. 353, 354 (1996); Daniel P. Kessler & Mark B. McClellan, How Liability Law Affects Medical
Productivity, 21 J. HEALTH ECON. 931, 935 (2002); Daniel P. Kessler & Mark B. McClellan, The
Effects of Malpractice Pressure and Liability Reforms on Physicians Perceptions of Medical Care, 60
LAW & CONTEMP. PROBS. 81, 82-83 (1997).
4 See Patricia M. Danzon, Liability for Medical Malpractice, in 1 HANDBOOK OF HEALTH
ECONOMICS 1339, 1368-69 (Anthony J. Culyer & Joseph P. Newhouse eds., 2000); see also
OFFICE OF TECH. ASSESSMENT, U.S. CONG., OTA-H-602, DEFENSIVE MEDICINE AND MEDICAL
MALPRACTICE 2 (1994), available at http://www.fas.org/ota/reports/9405.pdf; TOM BAKER, THE
MEDICAL MALPRACTICE MYTH 3 (2005); Henry J. Aaron & Paul B. Ginsburg, Is Health Spending
Excessive? If So, What Can We Do About It?, 28 HEALTH AFF. 1260, 1270 (2009).
5 Eleanor D. Kinney, Malpractice Reform in the 1990s: Past Disappointments, Future Success?,
20 J. HEALTH POL. POLY & L. 99, 101-02 (1995) (stating tort reform likely made medical
malpractice insurance more widely available but not necessarily less expensive).
6 Id. at 101; see Randall R. Bovbjerg, Legislation on Medical Malpractice: Further Developments
and a Preliminary Report Card, 22 U.C. DAVIS L. REV. 499, 501-03, 522-23, 525 (1989) (providing
KINNEY FINAL (DO NOT DELETE)
2012
Potential of Captives and Damage Caps
3/31/2012 11:29 AM
491
companies to lower premiums and exercise greater control over the
management of malpractice claims.7 These companies did not do well.8
More recently, as this article describes, hospitals and physicians have
increasingly chosen to self-insure through a variety of vehicles including
creating captive insurance companies. The insurance market for healthcare
institutions and professionals is posed to transform still with the
implementation of the new health reform legislation enacted in 2010.9
This Article suggests that two existing strategies already in place in
many state, and among many providers can be intentionally designed and
coordinated to facilitate the fair and expeditious resolution of medical
malpractice claims. Specifically, captive insurance companies operating in
states with caps on damages can work more effectively with healthcare
providers to resolve identified malpractice claims and also to identify and
compensate medical injury where claims are not pressed. This
phenomenon is because the damage cap informs insurers and providers of
the full extent of their liability. This knowledge establishes space for
providers and the captive insurers to settle claims expeditiously and fairly.
The space also enables providers and the captive insurers to go further and
express apologies to patients who have been injured in the care process.
This Article explores how this phenomenon can be implemented and
realized. This Article also explores how captives can be structured and
barriers addressed to mitigate the problems for physicians and to improve
the management of medical error for all stakeholders.
I.
Background
This section reviews past efforts of malpractice reform as well as the
rise and evolution of the patient-safety movement. These developments are
important precursors to the reforms suggested in this article.
A. Medical Liability
There is much debate over the existence, nature and scope of the
malpractice problem, with little consensus about the problem or its
examples of reforms aimed at reducing the number of lawsuits and the potential recovery size
as a legislative reaction to the steep increase in insurance premiums).
7 See Nicole Williams Koviak, An Insurance Perspective on the Medical Malpractice Crisis:
Introduction, 13 ANNALS HEALTH L. 607, 610-11 (2004); Transcribed Speech of Mr. Robert
Mulcahey, 13 ANNALS HEALTH L. 617, 621 (2004) [hereinafter Mulcahey].
8
Koviak, supra note 7, at 610-11; Mulcahey, supra note 7, at 621.
See generally Patient Protection and Affordable Care Act, Pub. L. No. 111-148, 124 Stat. 119
(2010), amended by Healthcare and Education Reconciliation Act of 2010, Pub. L. No. 111-152,
124 Stat. 1029 (2010) [hereinafter ACA].
9
KINNEY FINAL (DO NOT DELETE)
492
3/31/2012 11:29 AM
New England Law Review
v. 46 | 489
resolution.10 Most importantly, there is not a one-to-one ratio in the
incidence of medical malpractice and lawsuits. The Harvard Malpractice
Study found that 45% of claims present no malpractice,11 and the older
California Malpractice Study reported 57% false positives,12 with the more
recent Utah-Colorado Study having similar rates. 13 Also, there is some
evidence that some groupsfor example, recipients of Medicare and
Medicaidsustain medical injury that is less likely to result in malpractice
claims.14 In addition, the poor and the elderly are less likely to sue than
younger, more affluent individuals.15 These data suggest that the current
tort system does not address all medical injuries. From a social and
jurisprudential perspective, this inconsistency is problematic and unjust.
Another important phenomenon with medical injury is that providers
often fail to disclose and/or apologize for medical errors. This phenomenon
influences claiming behavior. Studies have shown that patients find
themselves in an adversarial position when seeking accountability from
providers in the event of a poor outcome and would have responded
positively to an explanation or an apology. One study showed that twentyfour percent of the surveyed patients sued because physicians had failed
to be completely honest with them about what happened, allowed them to
believe things that were not true, or intentionally misled them.16 Empirical
10 William M. Sage, The Forgotten Third: Liability Insurance and the Medical Malpractice Crisis,
23 HEALTH AFF. 10, 13-16 (2004) (arguing that the insurance component of the medical
malpractice system has not kept pace with other factors in the system).
11 Patient Safety and Medical Liability Reform Demonstration Projects, DEPT OF HEALTH &
HUMAN SERVS., http://grants.nih.gov/grants/guide/pa-files/PAR-11-025.html (last visited Mar.
30, 2012); see PAUL C. WEILER ET AL., A MEASURE OF MALPRACTICE: MEDICAL INJURY,
MALPRACTICE LITIGATION, AND PATIENT COMPENSATION 71 (1993); A. Russell Localio et al.,
Relation Between Malpractice Claims and Adverse Events Due to Negligence: Results of the Harvard
Medical Practice Study III, 325 NEW ENG. J. MED. 245, 250 (1991).
12 See Don Harper Mills, Medical Insurance Feasibility Study, 128 WEST J. MED. 360, 364
(1978).
13 See David M. Studdert et al., Negligent Care and Malpractice Claiming Behavior in Utah and
Colorado, 38 MED. CARE 250, 253 (2000).
14 See U.S. GENERAL ACCOUNTING OFFICE, GAO/HRD-93-126, MEDICAL MALPRACTICE:
MEDICARE/MEDICAID BENEFICIARIES ACCOUNT FOR A RELATIVELY SMALL PERCENTAGE OF
MALPRACTICES LOSSES (1993) (finding Medicaid patients file claims at a lower rate than other
groups, based on population).
15 Helen R. Burstin et al., Do the Poor Sue More? A Case-Control Study of Malpractice Claims
and Socioeconomic Status, 270 JAMA 1697, 1700 (1993); see also Mark Sager et al., Do the Elderly
Sue Physicians?, 150 ARCHIVE INTERNAL MED. 1091, 1091 (1990) (reviewing Wisconsin
malpractice cases to determine the frequency of elderly patients lawsuits).
16
Gerald B. Hickson et al., Factors that Prompted Families to File Medical Malpractice Claims
Following Perinatal Injuries, 267 JAMA 1359, 1361 (1992); see also Carol B. Liebman & Chris
Stern Hyman, A Mediation Skills Model to Manage Disclosure of Errors and Adverse Events to
KINNEY FINAL (DO NOT DELETE)
2012
Potential of Captives and Damage Caps
3/31/2012 11:29 AM
493
evidence developed by Gerald B. Hickson and colleagues suggests that
patient complaints have a predictive qualitythe more dissatisfied the
patient, the more likely a malpractice claim will result.17 Additionally,
James W. Pichert, studying feedback from patients, identified individual
units within an institution that could be considered high risk.18
B. Damage Caps
Historically and predominantly, medical liability reform has consisted
of state legislation to reduce the frequency and severity of recovery for
malpractice claims.19 Damage caps are the major strategy to reduce severity
and bring predictability to the medical liability insurance market. Damage
caps and reduced statutes of limitations have been shown to reduce
severity and frequency, respectively.20 Damage caps in medical malpractice
cases have been effective in controlling the cost of malpractice insurance. 21
Damage caps have also been criticized as hurting malpractice claimants to
the benefit of providers and liability insurers.22
C. The Patient Safety Movement
The Patient Safety Movement, inspired by the Institute of Medicines
(IoM) report, To Err Is Human, has precipitated a sea change in the way
healthcare providers and policy makers perceive the problem of medical
injury.23 This IoM report made several important findings and observations
that have contributed to this sea change: (1) an estimated 44,000 to 98,000
people die each year in hospitals from medical injury; and (2) systems
failures, rather than poor performance by individual practitioners, cause at
Patients, 23 HEALTH AFF. 22, 24 (2004) (listing factors that lead to the decision to sue, including
physician dishonesty).
17 See Gerald B. Hickson et al., Patient Complaints and Malpractice Risk, 287 JAMA 2951, 2955
(2002).
18 See James W. Pichert et al., Identifying Medical Center Units with Disproportionate Shares of
Patient Complaints, 25 JOINT COMMN J. QUALITY IMPROVEMENT 288, 292, 298 (1999).
19
Kinney, supra note 5, at 101.
Patricia M. Danzon, The Frequency and Severity of Medical Malpractice Claims: New
Evidence, 49 LAW & CONTEMP. PROBS. 57, 71, 73-74 (1986); Frank A. Sloan et al., Effects of Tort
Reforms on the Value of Closed Medical Malpractice Claims: A Microanalysis, 14 J. HEALTH POL.
POLY & L. 663, 665, 678 (1989).
20
21 Leonard J. Nelson, III et al., Damage Caps in Medical Malpractice Cases, 85 MILBANK Q. 259,
269 (2007).
22
Eleanor D. Kinney, An Empirical and Critical Look at the Current Medical Liability Crisis,
FRONTIERS HEALTH SERVS. MGMT., Fall 2003, at 31, 34.
23 Ross D. Silverman, Patient Safety and Patients Rights, VIRTUAL MENTOR (June 2004)
http://virtualmentor.ama-assn.org/2004/06/pfor2-0406.html.
KINNEY FINAL (DO NOT DELETE)
494
3/31/2012 11:29 AM
v. 46 | 489
New England Law Review
least half of patient injuries.24 The IoM report concluded that eliminating
or minimizing unintended risks and hazards associated with the structure
and process of care, improvements in patient safety could decrease medical
liability claims.25 The IoM recommended that providers create a culture of
safety in institutions by: (1) focusing on reducing errors in systems
providing care; (2) borrowing from quality science in the engineering
industries; and (3) moving away from emphasizing placement of blame on
individual physicians and other providers.26
Additionally, the Patient Safety and Quality Improvement Act of 2005
authorized creation of Patient Safety Organizations (PSOs) at the state
level to improve quality and safety through the collection and analysis of
data on patient events.27 PSOs offer a secure environment where clinicians
and healthcare organizations can collect, aggregate, and analyze data,
thereby improving quality by identifying and reducing the risks and
hazards associated with patient care.28
An important development in the Patient Safety Movement has been
the identification of so-called never events, which are incidents that,
according to some authorities, should never occur in the provision of good
quality medical care.29 In 2002, the National Quality Forum (NQF)
published its report, Serious Reportable Events in Healthcare, which identified
twenty-seven adverse events occurring in hospitals that are serious,
largely preventable, and of concern to both the public and healthcare
providers.30 According to NQF, the reports objective is to establish
consensus among consumers, providers, purchasers, researchers, and
other healthcare stakeholders about those preventable adverse events that
should never occur and to define them in a way that, should they occur, it
would be clear what had to be reported.31
24 INST. OF MED., TO ERR IS HUMAN: BUILDING A SAFER HEALTH SYSTEM 26, 30 (Linda T.
Kohn et al. eds., 2000).
25 Patient Safety and Medical Liability Reform Demonstration Projects, supra note 11.
26 See INST. OF MED., supra note 24, at 49, 71; see also Lucian L. Leape, Error in Medicine, 272
JAMA 1851, 1852 (1994).
27
See Patient Safety and Quality Improvement Act of 2005, Pub. L. No. 109-41, 119 Stat. 424
(codified as amended at 42 U.S.C. 299(b)-21 to 299(b)-26 (2006)).
28 Patient Safety Organizations, AGENCY FOR HEALTHCARE RES. & QUALITY, http://pso.ahrq.
gov/psos/overview.htm (last visited Mar. 30, 2012).
29 Nancy Berlinger, Medical Error, in FROM BIRTH TO DEATH AND BENCH TO CLINIC: THE
HASTINGS CENTER BIOETHICS BRIEFING BOOK FOR JOURNALISTS, POLICYMAKERS, AND
CAMPAIGNS 97, 97 (Mary Crowley ed., 2008) (describing never events as a major
development in patient care).
30 Kenneth W. Kizer, Foreword to THE NATL QUALITY F., SERIOUS REPORTABLE EVENTS IN
HEALTHCARE: A CONSENSUS REPORT (2002), available at www.ahrq.gov/qual/nqfpract.pdf.
31
Patient
Safety:
Serious
Reportable
Events
in
Healthcare,
NATL
QUALITY
F.,
KINNEY FINAL (DO NOT DELETE)
2012
3/31/2012 11:29 AM
Potential of Captives and Damage Caps
495
The Centers for Medicare and Medicaid Services (CMS) have also
taken steps to limit payment for so-called never events including
hospital-acquired conditions. Specifically, section 5001(c) of the Deficit
Reduction Act of 2005 requires the Secretary to identify conditions that: (a)
are high cost or high volume, or both . . . .; (b) results in the assignment
of a case to a diagnosis-related group that has a higher payment when . . .
present as a secondary diagnosis; and (c) could reasonably have been
prevented through the application of evidence-based guidelines.32 In
August 2007, CMS adopted a final rule identifying eight never events for
which, beginning October 1, 2008, Medicare would not provide additional
payment to hospitals unless the events were present on admission. 33 The
ACA expanded reimbursement restrictions for never events to the
Medicaid program.34 In June 2011, CMS promulgated a final rule to
implement this ACA provision.35
D. Captive Insurance Companies
In recent years, both institutional and professional healthcare
providers have moved away from commercial insurance carriers toward
alternative insurance vehicles to provide malpractice liability coverage.36
Captive insurance is a self-funded insurance mechanism that is primarily
controlled by its owners and whose owners are typically the principal
insureds.37 The Captive Insurance Companies Association defines captive
insurers as follows:
http://www.qualityforum.org/projects/hacs_and_sres.aspx (last visited Mar. 30, 2012).
32
Deficit Reduction Act of 2005, Pub. L. No. 109-171, 5001(c)(1)(iv)(I)-(III), 120 Stat. 30
(codified as amended at 42 U.S.C. 1395ww(d)(4)(A)(iv)(I)-(III) (2006)); accord CTRS. FOR
MEDICARE & MEDICAID SERVS., DEPT OF HEALTH & HUMAN SERVS., HOSPITAL-ACQUIRED
CONDITIONS (HAC) IN ACUTE INPATIENT PROSPECTIVE PAYMENT SYSTEM (IPPS) HOSPITALS (Oct.
2011), available at https://www.cms.gov/HospitalAcqCond/downloads/HACFactsheet.pdf.
33 Changes to the Hospital Inpatient Prospective Payment Systems and Fiscal Year 2008
Rates, 72 Fed. Reg. 47,130, 47,217 (Aug. 22, 2007) (codified at 42 C.F.R. 411-13, 489); see also
MEDICARE NATIONAL COVERAGE DETERMINATIONS MANUAL, Ch. 1, Part 2, 140.6-140.8,
https://www.cms.gov/manuals/downloads/ncd103c1_Part2.pdf (last visited Mar. 21, 2012).
34 Patient Protection and Affordable Care Act, Pub. L. No. 111-148, 2702, 124 Stat. 319
(2010) (codified as amended at 42 U.S.C. 136b-1).
35
Payment Adjustment for Provider-Preventable Conditions Including HealthcareAcquired Conditions, 76 Fed. Reg. 32, 816 (June 6, 2011) (to be codified at 42 C.F.R. Pts. 434,
438, & 447).
36 See generally JAY D. ADKISSON, ADKISSONS CAPTIVE INSURANCE COMPANIES (2006); R.
WESLEY SIERK, III, TAKEN CAPTIVE (2008..
37
TOWERS WATSON, CAPTIVES 101: MANAGING COST AND RISK 2, available at
http://www.towerswatson.com/assets/pdf/2435/TW_Captives_101.pdf; see also ROBERT H.
JERRY, II, NEW APPLEMAN ON INSURANCE LAW LIBRARY EDITION 1.09 (2011); Arthur G.
Koritzinsky, The Captive Concept, in INSURANCE COVERAGE 2009, at 698, 691 (2009).
KINNEY FINAL (DO NOT DELETE)
496
3/31/2012 11:29 AM
New England Law Review
v. 46 | 489
Captive Insurance Company - A risk-financing method or form
of self-insurance involving the establishment of a subsidiary
corporation or association organized to write insurance. Captive
insurance companies are formed to serve the insurance needs of
the parent organization and to escape uncertainties of
commercial insurance availability and cost. The insureds have a
direct involvement and influence over the companys major
operations, including underwriting, claims, management policy,
and investments.38
Captive insurers, as they are known today, originated in the 1960s and
were primarily domiciled in Bermuda with its loose insurance regulation. 39
The laws in Bermuda facilitated easy incorporation of captive insurance
companies and light regulation and continue to do so today. In the 1950s,
only about 100 captive companies, domiciled in Bermuda, existed; by 1982,
over 1000 captives existed with the majority incorporated in Bermuda. 40
The global consulting firm Towers Watson estimates that there are now
some 5400 captive insurance companies worldwide with 885 incorporated
in Bermuda.41 However, more and more state insurance regulatory
schemes recognize captives and license them accordingly. Figure 1 lists the
U.S. jurisdictions that currently license captive insurers:
38 Captives Glossary, CAPTIVE INS. COS. ASSN, http://www.cicaworld.com/Resources/
CaptivesGlossary.aspx (last visited Mar. 30, 2012).
39 TOWERS WATSON, supra note 37, at 2.
40 Id.
41 Id.
KINNEY FINAL (DO NOT DELETE)
2012
Potential of Captives and Damage Caps
3/31/2012 11:29 AM
497
Figure 142
U.S. Jurisdictions Authorizing Captive Insurers
Alabama
Montana
Arizona
Nevada
Arkansas
New York
Colorado
Puerto Rico
Delaware
Rhode Island
District of Columbia
South Carolina
Florida
South Dakota
Georgia
Tennessee
Hawaii
U.S. Virgin Islands
Illinois
Utah
Kansas
Vermont
Kentucky
Virginia
Maine
West Virginia
There are two primary forms of captives: single-parent captives and
group captives.43 In a single-parent captive, also known as a pure captive, a
parent company forms an insurance company to insure its own risks. 44 In a
group captive, multiple, non-related organizations form or participate in an
insurance company to insure risks common to the group.45 Other
classifications of captives include an association captive, a rent-a-captive,
a sponsored or protected cell captive, and a risk retention group
(RRG).46
Captives are of interest to all industries because they allow corporate
control over the captive; reduce premiums that do not reflect profits for
commercial insurers or expenses related to any other non-associated risk;
and, for for-profit corporations, permit tax deductions for premiums paid
to the captive. Initially, industries use of captives generally was inhibited
by the tax treatment of premiums paid to the captive. In 1978, the U.S. Tax
Court ruled that a taxpayer corporations agreement with an insurance
company, to the extent it reinsured the taxpayers wholly owned
subsidiary, was not insurance for tax purposes and that payments made
42 Complete Listing of All U.S. and Offshore Captive Insurance Domiciles: Best Domiciles for
Captive Insurance Companies, WEALTH MGMT. SOLUTIONS, LLC, http://www.wmsolutionsnow.
com/captive_insurance_domiciles.htm (last visited Mar. 30, 2012).
43 See TOWERS WATSON, supra note 37, at 2.
44 Michael R. Mead, Captive Structures, IRMI.COM (Apr. 2002), http://www.irmi.com/expert
/articles/2002/mead04.aspx.
45
46
Id.
TOWERS WATSON, supra note 37, at 2.
KINNEY FINAL (DO NOT DELETE)
498
3/31/2012 11:29 AM
New England Law Review
v. 46 | 489
were not deductible as business expenses. 47 The Court of Appeals for the
Ninth Circuit affirmed.48
In 1986, to clarify tax policy, Congress enacted the Liability Risk
Retention Act of 1986 to recognize captives and other arrangements as
RRGs for tax purposes.49 An RRG must be domiciled in a U.S. state that
regulates it as a captive insurance company. 50 The RRG may then operate
nationwide, provided it registers with each state in which it is to operate.51
Of note, the U.S. Government Accountability Office has raised concerns
about the effectiveness of state regulation of captives. 52
In recent years, healthcare providers have increasingly used captive
insurance companies for their medical liability coverage.53 Over the past
several years, an increasing number of individual hospitals and consortia
of hospitals and physicians have begun to self-insure in a variety of ways.
In 2003, the American Hospital Association estimated that forty percent of
its member hospitals were self-insured.54 A more recent industry survey
conducted by AON Risk Solutions and the American Society for
Healthcare Risk Management found that 73 percent of systems surveyed
will self-insure the combined hospital-physician malpractice risk.55
47
Carnation Co. v. Commr, 71 T.C. 400, 415 (1978), affd, 640 F.2d 1010 (9th Cir. 1981).
Carnation Co. v. Commr of Internal Revenue, 640 F.2d 1010, 1013 (9th Cir. 1981); see 3
COUCH ON INSURANCE 39:2 (3d ed. 2011).
48
49
Pub. L. No. 99-563, 100 Stat. 3170 (codified as amended at 15 U.S.C. 3901(4) (2006)).
Id. 3901(4)(c).
51 Id. 3902(a).
52 See U.S. GOVT ACCOUNTABILITY OFFICE, GAO-05-536, RISK RETENTION GROUPS:
COMMON REGULATORY STANDARDS AND GREATER MEMBER PROTECTIONS ARE NEEDED 65-66
(2005), available at http://www.gao.gov/new.items/d05536.pdf.
53 Mark E. Battersby, Create a Strategy to Protect Your Practice, 88 MED. ECON. 65, 66 (2011);
Koviak, supra note 7, at 609; David B. Mandell & Maureen Verduyn, Captive Insurance
Companies: Why You Should Consider Them Now More than Ever, 26 DERMATOLOGY TIMES 82, 82
(2005); Mulcahey, supra note 7, at 622; see Michael J. Moody, 25 Years of Stability in Medical
Malpractice, ROUGH NOTES, Feb. 2008, at 68, 68, available at http://www.captive.com/
captives/FuturoArticle/Rough%20Notes%20Article%202-08.pdf; Steve Taravella, Frustrated
Healthcare Systems Seek Alternatives to Traditional Insurance, MOD. HEALTHCARE, May 13, 1988,
at 30, 31-32.
50
54 U.S. GEN. ACCOUNTING OFFICE, GAO-03-702, MEDICAL MALPRACTICE INSURANCE:
MULTIPLE FACTORS HAVE CONTRIBUTED TO INCREASED PREMIUM RATES 39 (2003), available at
http://www.gao.gov/new.items/d03702.pdf.
55 Healthcare Industry Faces Unprecedented Change in Hospital Landscape, AON (Oct. 18, 2011),
http://aon.mediaroom.com/index.php?s=43&item=2414.
KINNEY FINAL (DO NOT DELETE)
2012
Potential of Captives and Damage Caps
3/31/2012 11:29 AM
499
E. The Potential Contribution of Health Reform
The Affordable Care Act, enacted in 2010, has multiple provisions that
encourage providers to integrate their quality improvement, patient safety,
and care delivery activities, and thus could greatly benefit by the flexibility
accorded by captive insurance companies managing liability.56 One of the
most important provisions in this regard is the Shared Savings Program for
Medicare fee-for-service providers.57 Under this program, a group of
providers and suppliers of services (e.g., hospitals, physicians, and others
involved in patient care) collaborate to care for Medicare beneficiaries who
are not enrolled in Medicare Advantage plans in organizations called
accountable care organizations (ACOs).58 ACOs must adhere to certain
requirements and practices aimed at providing seamless, high quality care.
In November 2011, CMS promulgated a final rule to implement the Shared
Savings program and ACOs.59
II. Captive Insurance Coverage and Damage Caps
The patient safety movement has fundamentally changed the
perspective through which providers view the management of error and
injury. Rather than taking a completely defensive posture of blame and
subsequent concealment in many instances, providers are looking at errors
and injuries as system problems that need better internal management to
ameliorate wrongs and improve future practice.60 Thus, the infrastructure
is in place that allows providers to move toward remediating medical
injury and deflecting malpractice claims in a more proactive, effective, and
just manner.
56 See DAVID M. LINER & KATHLEEN E. ELY, HEALTHCARE REFORM: POTENTIAL
OPPORTUNITIES FOR CAPTIVES (2011), available at http://publications.milliman.com/publications/
healthreform/pdfs/potential-opportunities-for-captives.pdf; EDWARD M. WROBEL AND JEFFREY
LEVIN-SCHERZ, US HEALTHCARE REFORM (Dec. 2010), http://www.towerswatson.com/
assets/pdf/mailings/Towers-Watson-Captive-Review-Article.pdf.
57
See 42 U.S.C. 1395jjj (2010).
See Accountable Care Organizations: Improving Care Coordination for People with Medicare,
HEALTHCARE.GOV,
http://www.healthcare.gov/news/factsheets/2011/03/accountablecare03
312011a.html (last updated Nov. 16, 2011); Ctrs. for Medicare & Medicaid Servs., Overview:
Accountable Care Organizations, CMS.GOV, https://www.cms.gov/aco/ (last modified Feb. 7,
2012, 11:25 AM).
58
59
Medicare Program; Medicare Shared Savings Program: Accountable Care Organizations
Final Rule, 76 Fed. Reg. 67, 802 (Nov. 2, 2011) (to be codified at 42 C.F.R. pt. 25).
60 See NATL PATIENT SAFETY FOUND., RESEARCH PROGRAM: SUMMARY OF PROGRESS 2
(2010),
available
at
http://www.npsf.org/wp-content/uploads/2011/10/2010_Research_Summary_of_Progress.pdf.
KINNEY FINAL (DO NOT DELETE)
500
3/31/2012 11:29 AM
New England Law Review
v. 46 | 489
A. The Potential of Captives and Caps
While preferential to providers, damage caps provide an extraordinary
opportunity for real medical liability reform that benefits patients first and
foremost while mitigating the trauma of medical malpractice for physicians
and providers. Specifically, captive malpractice insurers and state damage
caps, working in conjunction, show great promise in closing the chasms in
medical error identification, risk management, and medical injury
compensation.
Specifically, captives can work better with providers to resolve
identified malpractice claims. Moreover, they can better identify and
compensate medical injury where claims are not pressed. The cap accords
the captive and provider knowledge of the full extent of their liability and
thereby establishes space for providers and the captive insurers to settle
claims expeditiously and fairly. The space also enables providers and the
captive insurers to go further and express apologies to patients who have
been injured in the care process.61 Consequently, providers have more
flexibility to manage medical injuries and/or claims more justly and make
disclosures of errors, frank apologies, and remediation without fear of
large jury verdicts that might include punitive damages.
Captives can assume this function because of the fact that the owners
of the captives, insured providers, can essentially direct the decisions
relating to underwriting, claims, and investments of the captive. Thus,
captives can take steps to limit medical liability claims and protect the
provider, as the provider is the only insured entity. Because they are acting
in the providers interest without another incentive, such as serving
shareholders or other insureds, they have greater flexibility to compensate
patients for medical injury as part of a providers patient safety program.62
In this regard, captives can act in ways that conventional commercial
liability insurers cannot. Conventional medical liability insurers are
incentivized to contest medical liability claims in pursuit of profits or
revenue. In their effort to control their liability, conventional liability
insurers have little incentive to work with provider patient safety
programs in compensating patients for medical injury.
61 See Richard C. Boothman et al., A Better Approach to Medical Malpractice Claims? The
University of Michigan Experience, 2 J. HEALTH & LIFE SCI. L. 125, 142, 144-45 (2009).
62 See Mary Chmielowiec & Brad Granger, Cost of Risk: Show Me the Money, US CAPTIVE,
Apr. 2011, at 26, 27-29, available at www.uscaptivemagazine.com/archive.asp (accessed by
following 2011 Issue hyperlink) (explaining that using data and data analytics can predict
risks, allow captives to be proactive by monitoring their exposure, and create financially
sound captives).
KINNEY FINAL (DO NOT DELETE)
2012
3/31/2012 11:29 AM
Potential of Captives and Damage Caps
501
B. Linking Quality Assurance, Safety Programs, and Risk Management
with Medical Injury Remediation
Patient safety initiatives are very useful in addressing medical
malpractice. With these initiatives, the circumstances are in place to link
quality assurance, patient safety, and risk management with the complete
remediation of medical injury. Of note, some important policymakers have
called for linking patient safety and liability reform. 63
The envisioned role of captive providers in the resolution of claims and
injuries is a major factor in enabling this linkage. By crossing the historical
chasm between risk management and remediation, many of the problems
now caused by adjudicating medical injury claims in the tort system would
be mitigated. Specifically, genuine medical injuries could be identified
early and resolved expeditiously. Also, grievances that do not involve
medical injury, but have caused concerns for patients, can be identified and
resolved, thus lessening the likelihood that the patient will seek satisfaction
through the tort system. In sum, early remediation can resolve incidents
and claims more promptly, privately, and informally, thus reducing the
high financial and emotional costs that attend traditional tort litigation.
C. Some Minor Caveats
There are some important considerations to take into account in
structuring captive insurance companies for hospitals and other healthcare
providers. As indicated above, the tax treatment of captives and premiums
paid by a hospital or other healthcare organizations is complicated.64
Also, complex Medicare reimbursement issues are implicated in
hospital ownership of captives. CMS, which administers the Medicare
program, issued Section 2162.2.A.4 of The Provider Reimbursement Manual
regarding the treatment of the cost of premiums paid to captive insurance
companies for Medicare cost reimbursement. 65 Specifically, Section
2162.2.A.4 limits cost reimbursement if the captives investments in
63 See, e.g., JOINT COMMN ON ACCREDITATION OF HEALTHCARE ORGS., HEALTHCARE AT THE
CROSSROADS: STRATEGIES FOR IMPROVING THE MEDICAL LIABILITY SYSTEM AND PREVENTING
PATIENT INJURY 6, 10 (2005), available at http://www.jointcommission.org/assets/1/18/
Medical_Liability.pdf [hereinafter HEALTHCARE AT THE CROSSROADS]; Hillary Rodham Clinton
& Barack Obama, Making Patient Safety the Centerpiece of Medical Liability Reform, 354 NEW ENG.
J. MED. 2205, 2205 (2006), available at http://www.nejm.org/doi/pdf/10.1056/NEJMp068100.
64 See supra notes 43-47 and accompanying text; see also James A. Christopherson, The
Captive Medical Malpractice Insurance Company Alternative, 5 ANNALS HEALTH L. 121, 122, 12526 (1996); Karen Gantt, Federal Tax Treatment of Medical Malpractice Insurance Alternatives for
Nonprofits, 52 DRAKE L. REV. 495, 501, 503 (2004).
65
See Catholic Health Initiatives v. Sebelius, 617 F.3d 490, 491-92 (D.C. Cir. 2010).
KINNEY FINAL (DO NOT DELETE)
502
3/31/2012 11:29 AM
New England Law Review
v. 46 | 489
equities exceed what state insurance regulators ordinarily require. 66 The
Circuit Court for the District of Columbia invalidated this rule in 2010,
creating some uncertainty regarding this policy.67
There is also question about the degree to which Medicare fraud and
abuse rules will permit institutional healthcare providers to assist affiliated
physicians with the cost of medical malpractice insurance through
captives. In 2004, the American Health Lawyers Association wrote a letter
to officials with the Internal Revenue Service and the U.S. Department of
Health and Human Services (DHHS) requesting details of the
permissible assistance that hospitals and other acute and long-term care
providers may provide to physicians and other health professionals to
lessen the effects of rising malpractice insurance premiums.68 DHHS
declined to offer a response to the letter given the restrictions of the
Medicare fraud and abuse authorities.69
D. A Major Barrier
There is one important barrier that threatens the possibility of the
integrative reforms suggested in this Article. A captive that insures a
corporate entity may also be covering providing coverage for physicians
and other professionals on a theory of vicarious liability.70 The captive as
the physicians insurer will have specific obligations to defend the
employee physicians. These obligations may be inconsistent with the
captives desire to resolve claims expeditiously.71
Specifically, medical malpractice claims have serious consequences for
individual physicians. One of the most serious consequences of a settled
66
See id.at 491-92.
See id. at 494, 496 (invalidating the rule on grounds that it had been improperly
promulgated); see also D.C. Circuit Reverses, Remands Judgment on Payment for Offshore Insurer
Coverage, 19 HEALTH L. REP. 1176, 1176 (2010).
68 Letter from Gerald M. Griffith, on Behalf of the Am. Health Lawyers Assn, to the U.S.
Dept of Health & Human Servs. and the Internal Revenue Serv. (Apr. 22, 2004), available at
http://www.healthlawyers.org/SiteCollectionDocuments/Content/ContentGroups/Press_Relea
ses/pi_MalpracticeLtr.pdf; see Attorneys Ask Agencies to Clarify Limits on Assisting with Coverage,
13 HEALTH L. REP. 677, 677 (2004).
67
69
With Little Help from Feds, Hospitals Explore Ways to Fix Staff Physicians Insurance Woes, 13
HEALTH L. REP. 1363, 1363 (2004).
70 See Leona Egeland Siadek, Vicarious Liability Spreads with Ostensible Partnerships, THE
DOCTORS CO.: THE DOCTORS ADVOC. (2007), http://www.thedoctors.com/KnowledgeCenter/
Publications/TheDoctorsAdvocate/CON_ID_000351 (discussing that doctors are often named
in lawsuits due to vicarious liability).
71
See HEALTHCARE AT THE CROSSROADS, supra note 63, at 5 (noting that a medical
malpractice lawsuit is lengthy and reduces the opportunity for quick resolution of unsafe
practices).
KINNEY FINAL (DO NOT DELETE)
2012
3/31/2012 11:29 AM
Potential of Captives and Damage Caps
503
malpractice claim against a physician is the obligation under the Health
Care Quality Improvement Act of 198672 to report settled claims to the
National Practitioner Data Bank (NPDB) that the U.S. Department of
Health and Human Services maintains. 73 Such reports to the NPDB follow
physicians throughout their careers and can limit employment and
advancement opportunities.
Indeed, the NPDB stands in the way of the reforms proposed in this
Article, as well as other forward-looking reforms, such as enterprise
liability for healthcare organizations. Further, the NPDB is not consistent
with the patient safety movements philosophy to focus less on blaming
individuals and more on addressing systemic problems that contribute to
medical injury. In closing, this Article calls for a reassessment of the
NPDBs value in todays era of access to information on the Internet and
the increased quality assurance and improvement methods of hospitals,
physicians, and all other healthcare providers.
CONCLUSION
Patient safety initiatives provide much promise in addressing medical
malpractice. Indeed, policymakers have called for linkages between patient
safety promotion strategies and the resolution of medical liability claims
and injuries. It makes great sense to link provider quality, patient safety,
and risk management efforts with remediation of medical injuries,
grievances, and medical malpractice claims. As providers become more
integrated under healthcare reform, captives can facilitate and support
integration initiatives. Captives and caps, working in the context of health
reform, provide an opportunity to resolve medical injury claims and events
internally and expeditiously. But such linkages should only be
implemented if physicians can be adequately protected from settlement
decisions that unfairly compromise their reputation. Reforming the
National Practitioner Data Bank would be a good first step in this regard.
72 Healthcare Quality Improvement Act of 1986, Pub. L. No. 99-660, 100 Stat. 3784 (codified
as amended at 42 U.S.C. 11101-11152 (2006)).
73
Id. 11131-11137.
You might also like
- Bisb - Bank StatementDocument23 pagesBisb - Bank Statementazstartup.bhNo ratings yet
- The Profit Motive and Patient CareDocument448 pagesThe Profit Motive and Patient CareTCFdotorgNo ratings yet
- PESTLE Analysis For Rolls RoyceDocument2 pagesPESTLE Analysis For Rolls Roycephi podcastNo ratings yet
- Berman: ForewordDocument7 pagesBerman: ForewordNew England Law ReviewNo ratings yet
- Medical MalpracticeDocument469 pagesMedical MalpracticeMuhammad Ali100% (1)
- 8sfnf Medical MalpracticeDocument469 pages8sfnf Medical MalpracticeSana Khairi100% (2)
- Responsibility Verses ControlDocument25 pagesResponsibility Verses ControlrangababNo ratings yet
- Of Swords and Shields - The Role of Clinical Pratice Guidelines inDocument66 pagesOf Swords and Shields - The Role of Clinical Pratice Guidelines inAastha SinghNo ratings yet
- Heading Towards A Single Government Payer SystemDocument4 pagesHeading Towards A Single Government Payer SystemNeelkumar SoniNo ratings yet
- Health Care Policy and Delivery Systems SyllabusDocument6 pagesHealth Care Policy and Delivery Systems SyllabusDeekay100% (1)
- Izakt Bibliography-Rws1301Document5 pagesIzakt Bibliography-Rws1301api-325497433No ratings yet
- Policy Brief 3 ThelenDocument16 pagesPolicy Brief 3 ThelenCarol ThelenNo ratings yet
- Willard and Spackman's Occupational Therapy 11th Edition Chapter 74 PDF FreeDocument25 pagesWillard and Spackman's Occupational Therapy 11th Edition Chapter 74 PDF FreeTracy NguyenNo ratings yet
- Surgeons and Medical Liability PrimerDocument36 pagesSurgeons and Medical Liability PrimerJack BenaventeNo ratings yet
- Afforable Care Act FinalDocument64 pagesAfforable Care Act FinalArafat MazharNo ratings yet
- Health Care Reform DissertationDocument6 pagesHealth Care Reform DissertationDoMyPaperForMeEverett100% (1)
- Healthcare Is Not A Part of Your Bill of RightsDocument10 pagesHealthcare Is Not A Part of Your Bill of Rightsapi-643881078No ratings yet
- Lang - Diskusija ObameDocument7 pagesLang - Diskusija ObameanlaucNo ratings yet
- Annotated Bibliography Eng 112Document6 pagesAnnotated Bibliography Eng 112api-511289341No ratings yet
- Does The Doctor Need A Boss?, Cato Briefing Paper No. 111Document12 pagesDoes The Doctor Need A Boss?, Cato Briefing Paper No. 111Cato InstituteNo ratings yet
- Medical Malpractice ReformsDocument18 pagesMedical Malpractice ReformsUsman Naroo100% (1)
- Health Care Delivery Models and Nursing Practice 2Document6 pagesHealth Care Delivery Models and Nursing Practice 2DennisNo ratings yet
- Infertility Treatment Markets The Effects of CompeDocument44 pagesInfertility Treatment Markets The Effects of CompeMohamed SalahNo ratings yet
- 2011-Evaluating The Medical Malpractice System and Options ForDocument16 pages2011-Evaluating The Medical Malpractice System and Options ForHening Tirta KusumawardaniNo ratings yet
- Medical Savings Accounts: Answering The Critics, Cato Policy AnalysisDocument12 pagesMedical Savings Accounts: Answering The Critics, Cato Policy AnalysisCato InstituteNo ratings yet
- Research Paper in Health EconomicsDocument6 pagesResearch Paper in Health Economicscaqllprhf100% (1)
- Identifying and Resolving Disputes in New Accountable Care SettingsDocument10 pagesIdentifying and Resolving Disputes in New Accountable Care SettingsRothHealthLawNo ratings yet
- Ethical Case Analysis PaperDocument14 pagesEthical Case Analysis Paperapi-282129457100% (1)
- Health and Medicine LawDocument9 pagesHealth and Medicine Lawshikhar shuklaNo ratings yet
- Systemic Negligence and NHS Hospitals AnUnderutilised ArgumentDocument30 pagesSystemic Negligence and NHS Hospitals AnUnderutilised ArgumentanharjutsuNo ratings yet
- Retail Business Laws: A Critical Analysis of Health Care SectorDocument5 pagesRetail Business Laws: A Critical Analysis of Health Care SectorAKHILA GOPAKUMAR-RM 21RM905No ratings yet
- Negligence Liability in Medical Examination and Treatment in Vietnam in Comparision ReviewDocument22 pagesNegligence Liability in Medical Examination and Treatment in Vietnam in Comparision ReviewsimonpeternekesaNo ratings yet
- Five Myths About Medical NegligenceDocument12 pagesFive Myths About Medical NegligenceLateNightRomeNo ratings yet
- National Health Insurance FailureDocument4 pagesNational Health Insurance FailureGaddafi PhelixNo ratings yet
- Policy Action Plan - Physician ShortageDocument11 pagesPolicy Action Plan - Physician Shortageapi-349372265No ratings yet
- Medical MalpracticeDocument29 pagesMedical MalpracticeBuruiana Andrei Richard0% (1)
- Furrow: Adverse Events and Patient InjuryDocument37 pagesFurrow: Adverse Events and Patient InjuryNew England Law Review100% (1)
- Module Two 1Document3 pagesModule Two 1api-612975585No ratings yet
- Mining for Gold In a Barren Land: Pioneer Accountable Care Organization Potential to Redesign the Healthcare Business Model in a Post-Acute SettingFrom EverandMining for Gold In a Barren Land: Pioneer Accountable Care Organization Potential to Redesign the Healthcare Business Model in a Post-Acute SettingNo ratings yet
- Hospital As FactoryDocument4 pagesHospital As FactoryecartetescuissesNo ratings yet
- Jurnal HBMDocument10 pagesJurnal HBMSeindz OstenNo ratings yet
- Hme 2301 Topic 3Document6 pagesHme 2301 Topic 3Mofy AllyNo ratings yet
- Coursematerial 214Document16 pagesCoursematerial 214Francisco Reyes IslaNo ratings yet
- Anatomy of Health InsuranceDocument124 pagesAnatomy of Health InsurancesimerjeetNo ratings yet
- Deadly Ties and The Rise of Multi-Drug Resistant Infections: A Case For A New Health Care Practitioner Hygienic Dress CodeDocument20 pagesDeadly Ties and The Rise of Multi-Drug Resistant Infections: A Case For A New Health Care Practitioner Hygienic Dress CodeRich AzzopardiNo ratings yet
- Physicians Us Versus HospitalsDocument4 pagesPhysicians Us Versus Hospitalssavvy_as_98-1No ratings yet
- Mckeon: New York's Innovative Approach To Medical MalpracticeDocument13 pagesMckeon: New York's Innovative Approach To Medical MalpracticeNew England Law ReviewNo ratings yet
- The Fine Line of Defensive Medicine PDFDocument3 pagesThe Fine Line of Defensive Medicine PDFEMMA LAURA MORALES GONZALEZNo ratings yet
- HADM 4326 Assignment 1Document4 pagesHADM 4326 Assignment 1saraNo ratings yet
- Affordable Care Act ThesisDocument5 pagesAffordable Care Act Thesisgbtrjrap100% (1)
- DDJHPPL 23 4 661Document26 pagesDDJHPPL 23 4 661AlexNo ratings yet
- Eff Ects of The Medical Liability System in Australia, The UKDocument7 pagesEff Ects of The Medical Liability System in Australia, The UKesther kwanNo ratings yet
- Dr. Ram Manohar Lohiya National Law University, Lucknow: Academic Session: 2018 - 19Document12 pagesDr. Ram Manohar Lohiya National Law University, Lucknow: Academic Session: 2018 - 19Aditi VatsaNo ratings yet
- Themedicalliability System:Essential Informationforthe HospitalistDocument12 pagesThemedicalliability System:Essential Informationforthe Hospitalistjoaquín_chavollaNo ratings yet
- How To Write A Research Paper On Health Care ReformDocument7 pagesHow To Write A Research Paper On Health Care Reformlyn0l1gamop2No ratings yet
- Thesis Statement Against The Affordable Care ActDocument6 pagesThesis Statement Against The Affordable Care Actjanetrobinsonjackson100% (2)
- American Medicine: The Quest for CompetenceFrom EverandAmerican Medicine: The Quest for CompetenceRating: 3 out of 5 stars3/5 (1)
- BibliographyDocument3 pagesBibliographyapi-253028254No ratings yet
- EpisodeBasedPayment PerspectivesforConsiderationDocument24 pagesEpisodeBasedPayment PerspectivesforConsiderationHazelnutNo ratings yet
- The New Hospital-Physician Enterprise: Meeting the Challenges of Value-Based CareFrom EverandThe New Hospital-Physician Enterprise: Meeting the Challenges of Value-Based CareNo ratings yet
- Solution Manual For Health Care Management and The Law Principles and Applications 1st EditionDocument37 pagesSolution Manual For Health Care Management and The Law Principles and Applications 1st Editioneozoicjaggern2ni4100% (19)
- Why State Constitutions MatterDocument12 pagesWhy State Constitutions MatterNew England Law ReviewNo ratings yet
- Reforming The NYPD and Its Enablers Who Thwart ReformDocument44 pagesReforming The NYPD and Its Enablers Who Thwart ReformNew England Law ReviewNo ratings yet
- 101 99% Human and 1%animal? Patentable Subject Matter and Creating Organs Via Interspecies Blastocyst Complementation by Jerry I-H HsiaoDocument23 pages101 99% Human and 1%animal? Patentable Subject Matter and Creating Organs Via Interspecies Blastocyst Complementation by Jerry I-H HsiaoNew England Law ReviewNo ratings yet
- "Swear Not at All": Time To Abandon The Testimonial OathDocument52 pages"Swear Not at All": Time To Abandon The Testimonial OathNew England Law ReviewNo ratings yet
- Reformation of The Supreme Court: Keeping Politics OutDocument22 pagesReformation of The Supreme Court: Keeping Politics OutNew England Law ReviewNo ratings yet
- The Massachusetts Sexually Dangerous Persons Statute: A Critique of The Unanimous Jury Verdict Requirement by Widmaier CharlesDocument17 pagesThe Massachusetts Sexually Dangerous Persons Statute: A Critique of The Unanimous Jury Verdict Requirement by Widmaier CharlesNew England Law ReviewNo ratings yet
- Employment Discrimination: Pretext, Implicit Bias, and The Beast of BurdensDocument27 pagesEmployment Discrimination: Pretext, Implicit Bias, and The Beast of BurdensNew England Law Review100% (1)
- The Fight Against Online Sex Trafficking: Why The Federal Government Should View The Internet As A Tool and Not A WeaponDocument16 pagesThe Fight Against Online Sex Trafficking: Why The Federal Government Should View The Internet As A Tool and Not A WeaponNew England Law ReviewNo ratings yet
- Section 43 (A) in A Vacuum: Cleaning Up False Advertising in An Unfair Competition MessDocument14 pagesSection 43 (A) in A Vacuum: Cleaning Up False Advertising in An Unfair Competition MessNew England Law ReviewNo ratings yet
- Combating The Opioid Crisis: The Department of Health and Human Services Must Update EMTALADocument21 pagesCombating The Opioid Crisis: The Department of Health and Human Services Must Update EMTALANew England Law ReviewNo ratings yet
- Harvesting Hope: Regulating and Incentivizing Organ DonationDocument31 pagesHarvesting Hope: Regulating and Incentivizing Organ DonationNew England Law ReviewNo ratings yet
- Cuz I'm Young & I'm Black & My Hat's Real Low: Constitutional Rights To The Political Franchise For Parolees Under Equal Protection by Shaylen Roberts, Esq.Document33 pagesCuz I'm Young & I'm Black & My Hat's Real Low: Constitutional Rights To The Political Franchise For Parolees Under Equal Protection by Shaylen Roberts, Esq.New England Law ReviewNo ratings yet
- The Shadowy Law of Modern Surveillance by Gina AbbadessaDocument3 pagesThe Shadowy Law of Modern Surveillance by Gina AbbadessaNew England Law ReviewNo ratings yet
- An "Obvious Truth": How Underfunded Public Defender Systems Violate Indigent Defendants' Right To CounselDocument30 pagesAn "Obvious Truth": How Underfunded Public Defender Systems Violate Indigent Defendants' Right To CounselNew England Law ReviewNo ratings yet
- Trademarks and Twitter: The Costs and Benefits of Social Media On Trademark Strength, and What This Means For Internet-Savvy CelebsDocument25 pagesTrademarks and Twitter: The Costs and Benefits of Social Media On Trademark Strength, and What This Means For Internet-Savvy CelebsNew England Law ReviewNo ratings yet
- Revealing A Necessary Evil: The United States Must Continue To Use Some Form of Domesticated Counter-Terrorism Program by Daniel R. GodefroiDocument17 pagesRevealing A Necessary Evil: The United States Must Continue To Use Some Form of Domesticated Counter-Terrorism Program by Daniel R. GodefroiNew England Law ReviewNo ratings yet
- Outer Space and International Geography Article II and The Shape of Global OrderDocument29 pagesOuter Space and International Geography Article II and The Shape of Global OrderNew England Law ReviewNo ratings yet
- Augustine and Estabrook: Defying The Third-Party Doctrine by Michael LockeDocument13 pagesAugustine and Estabrook: Defying The Third-Party Doctrine by Michael LockeNew England Law ReviewNo ratings yet
- “The Legalization of Recreational Marijuana in Massachusetts and the Limits of Social Justice for Minorities and Communities Disproportionately Impacted by Prior Marijuana Laws and Drug Enforcement Policies”Document13 pages“The Legalization of Recreational Marijuana in Massachusetts and the Limits of Social Justice for Minorities and Communities Disproportionately Impacted by Prior Marijuana Laws and Drug Enforcement Policies”New England Law ReviewNo ratings yet
- Death by 1000 Lawsuits: The Public Litigation in Response To The Opioid Crisis Will Mirror The Global Tobacco Settlement of The 1990s by Paul L. KeenanDocument26 pagesDeath by 1000 Lawsuits: The Public Litigation in Response To The Opioid Crisis Will Mirror The Global Tobacco Settlement of The 1990s by Paul L. KeenanNew England Law ReviewNo ratings yet
- Ojukwu Final 3Document26 pagesOjukwu Final 3New England Law ReviewNo ratings yet
- Ignorance Is Bliss: Why The Human Mind Prevents Defense Attorneys From Providing Zealous Representation While Knowing A Client Is GuiltyDocument25 pagesIgnorance Is Bliss: Why The Human Mind Prevents Defense Attorneys From Providing Zealous Representation While Knowing A Client Is GuiltyNew England Law ReviewNo ratings yet
- Secret Law and The Snowden Revelations: A Response To The Future of Foreign Intelligence: Privacy and Surveillance in A Digital Age, by Laura K. Donohue by HEIDI KITROSSERDocument10 pagesSecret Law and The Snowden Revelations: A Response To The Future of Foreign Intelligence: Privacy and Surveillance in A Digital Age, by Laura K. Donohue by HEIDI KITROSSERNew England Law ReviewNo ratings yet
- A Citizens Commission For The 28 Amendment: Massachusetts Advances Constitutional Reform of Our Broken Political SystemDocument8 pagesA Citizens Commission For The 28 Amendment: Massachusetts Advances Constitutional Reform of Our Broken Political SystemNew England Law ReviewNo ratings yet
- Remnants of Information Privacy in The Modern Surveillance State by Lawrence FriedmanDocument15 pagesRemnants of Information Privacy in The Modern Surveillance State by Lawrence FriedmanNew England Law ReviewNo ratings yet
- Unconstitutional Constitutional Change by Courts: NtroductionDocument23 pagesUnconstitutional Constitutional Change by Courts: NtroductionNew England Law ReviewNo ratings yet
- New Light On State Constitutional ChangeDocument4 pagesNew Light On State Constitutional ChangeNew England Law ReviewNo ratings yet
- Mechanisms of Accountability Fundamental To An Independent JudiciaryDocument6 pagesMechanisms of Accountability Fundamental To An Independent JudiciaryNew England Law ReviewNo ratings yet
- Collins Final 3Document20 pagesCollins Final 3New England Law ReviewNo ratings yet
- V.51-3 TOC FinalDocument2 pagesV.51-3 TOC FinalNew England Law ReviewNo ratings yet
- 1LOC005 - How Do I Allocate Legs To A Drivers Run SheetDocument2 pages1LOC005 - How Do I Allocate Legs To A Drivers Run Sheetguolidong2017No ratings yet
- Slug LowDocument13 pagesSlug LowDr Mohammed AzharNo ratings yet
- The Elusive Chemical Potential PDFDocument12 pagesThe Elusive Chemical Potential PDFbonesisaliveNo ratings yet
- (TV) Present TenseDocument8 pages(TV) Present TenseDe Aparicio DenisseNo ratings yet
- The Company Name Has Evolved Over Its 100 Years in BusinessDocument6 pagesThe Company Name Has Evolved Over Its 100 Years in BusinessFrancisco UrizarNo ratings yet
- Biography of Jamgön Ju MiphamDocument6 pagesBiography of Jamgön Ju MiphamBLhundrupNo ratings yet
- Result Phase III - A, B - Lot (23!03!2024)Document15 pagesResult Phase III - A, B - Lot (23!03!2024)xxxlordimpalerxxxNo ratings yet
- Vine-Vpdc Report As of Feb. 3, 2022Document9 pagesVine-Vpdc Report As of Feb. 3, 2022Elbert Ryan OcampoNo ratings yet
- Assembly BuildingDocument1 pageAssembly BuildingHarshit RajNo ratings yet
- Wvsu NCM 106 Sample Lesson PlanDocument10 pagesWvsu NCM 106 Sample Lesson Plangreen_archerNo ratings yet
- Online Marketing EssentialsDocument508 pagesOnline Marketing EssentialsElena BotezatuNo ratings yet
- Gravoca 1C 본문 170705 인쇄용Document192 pagesGravoca 1C 본문 170705 인쇄용GreysenNo ratings yet
- Class - 12th Annual ReportDocument4 pagesClass - 12th Annual ReportPreksha SharmaNo ratings yet
- MDR11 InstructionsDocument4 pagesMDR11 Instructionsjuan tellezNo ratings yet
- Ceramics II Project Ideas Spring 2019Document2 pagesCeramics II Project Ideas Spring 2019api-170572422No ratings yet
- Surface Preparation Standards JotunDocument2 pagesSurface Preparation Standards JotunbacabacabacaNo ratings yet
- Konsep Pendidikan Religius RasionalDocument14 pagesKonsep Pendidikan Religius RasionalSri ParwatiNo ratings yet
- How Deep Is Your LoveDocument1 pageHow Deep Is Your LoveJanina JaworskiNo ratings yet
- 1430-Article Text-4196-2-10-20220929Document21 pages1430-Article Text-4196-2-10-20220929Annisa SophiaNo ratings yet
- Samsung Brittle Fracture Evaluation - Additional Scope P23-0105-R3Document5 pagesSamsung Brittle Fracture Evaluation - Additional Scope P23-0105-R3Vipin NairNo ratings yet
- Anyone Who Had A Heart - A Case Study in PhysiologyDocument9 pagesAnyone Who Had A Heart - A Case Study in PhysiologyJohnSnow0% (1)
- NXF Perforated Cable Tray en 2017Document65 pagesNXF Perforated Cable Tray en 2017LANKAPALLISURINo ratings yet
- Birth QnaDocument8 pagesBirth QnaaliazgarNo ratings yet
- PDF - Marine Bio Semester One Review SheetDocument2 pagesPDF - Marine Bio Semester One Review Sheetapi-205313794No ratings yet
- Unit 1 Prog Logic DevelopmentDocument8 pagesUnit 1 Prog Logic DevelopmentAtharv KhadatareNo ratings yet
- Test Report Quadplexer 4in1outDocument8 pagesTest Report Quadplexer 4in1outHagniAryaGunadiNo ratings yet
- Safety Instrumented Systems: GlobalDocument410 pagesSafety Instrumented Systems: Globalmohammed el erianNo ratings yet
- Model Name: GA-B75M-D2V: Gigabyte TechnologyDocument26 pagesModel Name: GA-B75M-D2V: Gigabyte TechnologyMaaf GarenaNo ratings yet