Professional Documents
Culture Documents
Epilepticus: Morbidity and Mortality
Epilepticus: Morbidity and Mortality
Uploaded by
Indah Maharani NasutionOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Epilepticus: Morbidity and Mortality
Epilepticus: Morbidity and Mortality
Uploaded by
Indah Maharani NasutionCopyright:
Available Formats
EPILEPTICUS
Abstract
Status epilepticus (SE) is divided into convulsive and non-convulsive types; both are
associated with significant morbidity and mortality. Although convulsive SE is easily
recognized, non-convulsive SE remains an elusive diagnosis as physical signs are varied and
subtle. Successful management depends on a comprehensive approach that involves
diagnostic testing and pharmacological interventions while ensuring cerebral oxygenation
and perfusion at all times. There are a limited number of well-designed studies to support the
development of evidence-based recommendations for the management of SE, especially for
the management of non-convulsive status. Benzodiazepines, specifically lorazepam, continue
to be the most commonly recommended first-line therapy; best treatment for refractory status
cases depends on resources available and must be tailored to the individual institution. In
order to facilitate care, it is recommended that each institution develop a management
protocol for these patients.
Introduction and definitions
Status epilepticus (SE) is a potentially life-threatening condition. A seizure, as defined
by the International League Against Epilepsy and the International Bureau of Epilepsy is a
transient occurrence of signs and/or symptoms due to abnormal excessive or synchronous
neuronal activity in the brain. Most seizures last less than 12 min : Seizures that last more
than 510 min are less likely to stop without intervention. The International League Against
Epilepsy originally defined SE in 1964 as a situation in which a seizure persists for a
sufficient length of time or is repeated frequently enough to produce a fixed and enduring
epileptic condition.This definition lacked a specific duration, and 30 min became a popular
time frame based on neuronal injury patterns seen in animal models. Recent research supports
a modified working definition of SE as an event lasting 5 min or more.
Epidemiology
- Generalized convulsive status epilepticus
GCSE has an annual incidence of 6.841 cases per 100 000 people, or about 50 000
150 000 cases in the USA. Incidence is bimodal, with the first peak at less than 4 years of age
and a second peak between 60 and 75 years. Acute mortality is between 110%, with total
deaths in the USA numbering 55 000 per year. For patients with pre-existing epilepsy, up to
16% will have one episode of SE during their lifetime.
- Non-convulsive status epilepticus
Population-based incidence of NCSE is difficult to ascertain for several reasons. The
variety of definitions and classifications of NCSE make it difficult to compare incidence and
frequency across studies. Also, many studies investigating NCSE suffer from selection bias as
they are based at tertiary care centres. The reported incidence of NCSE ranges from 4% to
50% of all cases of SE.
In one prospective study of 164 patients with convulsive SE who were subjected to
continuous EEG monitoring for at least 24 h after seemingly successful treatment, 14% were
found to have NCSE and 48% had some persistent electrographic seizure activity. In another
study of 384 patients, Treiman et al. used EEG early during the course of treatment and found
that up to 25% of patients treated for GCSE had ongoing seizure activity in the form of subtle
convulsive SE or NCSE.
Refractory SE
Refractory SE occurs in up to 45% of all adults and children with SE. In a
retrospective study of 107 patients at two tertiary care hospitals, Rossetti et al. reported that
first-time seizures have a slightly higher rate of evolving into refractory SE (4050%)
compared with recurrent seizures. In up to 20% of patients with refractory SE, seizures might
last weeks or even months. In a retrospective cohort of 74 patients with SE,
Mayer et al. found that patients with NCSE have a higher rate of progression to refractory SE
than those with GCSE. A retrospective study of 134 children in SE reported an association
between delay in provision of first- and second-line anti-epileptic drugs (AED) and the
development of refractory SE. In addition to delay in treatment, other factors that have been
associated with the development of refractory SE include CNS infections, metabolic
abnormalities and hypoxic-ischaemic injury.
Pathophysiology
Ordinarily, seizures self-terminate via gamma-aminobutyric acid (GABA)-mediated
inhibitory pathways. In SE, GABA receptors appear to be internalized and destroyed by
lysosomes, thus inactivating the inhibitory mechanism, and persistent seizures appear to
change the GABA receptor's conformation, making them less responsive to
benzodiazepines. Both of these findings help explain why benzodiazepines appear to be less
effective as seizure duration increases. When seizures last more than 30 min, the body's
homeostatic regulating mechanisms begin to deteriorate, as autonomic control is lost.
Hypotension ensues along with a decrease in oxygen saturation and a decrease in pH,
especially if the patient's respiratory status is compromised. Hyperthermia, hypoglycaemia
and lactic acidosis occur as a result of excess neuromuscular activity. Animal models suggest
that even if systemic factors, such as acidosis and hypoxia, are controlled, prolonged SE
results in neuronal damage secondary to the release of neurotoxic excitatory amino acids and
influx of calcium into cells. Ultimately, all of the above can contribute to adverse outcomes
through the development of cardiac dysrhythmias, hypoxia , hypotension, Hyperthermia,
rhabdomyolysis, acidosis (respiratory and metabolic) and pulmonary oedema .
Aetiology
SE can present in individuals with known epilepsy or de novo. The key for ED
management is identifying reversible causes. SE can be the result of an acute or remote event:
the acute causes include metabolic abnormalities, infections, toxicities, structural lesions and
vascular events. Remote events are usually related to past CNS injuries (e.g. head trauma,
anoxia or stroke). In patients with existing epilepsy, the most common aetiology of SE is
AED non-compliance or sub-therapeutic AED levels.
NCSE has been associated with benzodiazepine or other medication withdrawal,
excessive use of psychotropic drugs, infections, trauma, metabolic derangements, stroke and
alcohol use. Several drugs, including ceftazidime, ifosfamide, chloroquine, digoxin and
penicillin, have been associated with NCSE. Carbamazepine, a commonly use anti-epileptic
medication, has also been found to have the potential to precipitate NCSE.
Toxicological causes
Toxicological causes account for a small number of cases of SE each year. In a
retrospective review, Thundiyil et al. found that 386 cases of seizures related to poisoning or
drug intoxication were reported to California Poison Control in 2003, of which 14 (3.6%)
featured SE. Drugs involved included benzonatate, cocaine, bupropion, ethylene glycol,
isoniazid, citalopram, amitriptyline, methamphetamine and tiagabine. In 1993,
Lowenstein et al. found that drug toxicity accounted for 9% of all cases of SE presenting to
an urban ED over 10 years. Although recreational drugs, such as cocaine, amphetamine,
heroin and phencyclidine, appear to induce seizures, the rate of SE among these patients
appears to be low (4%).
Outcomes and complications
As mentioned above, SE might have grave consequences as the body's homeostatic
mechanisms are disrupted. Subsequent complications might affect any organ system and will
eventually lead to death. Several articles have attempted to determine the mortality of SE.
The best available estimates suggest a range between 10% and 40%. Recently, one article
estimated the case-fatality rate using the National Inpatient Sample based on ICD-9 codes
and found an overall mortality of 3.43%. The study was large (n= 11 580), subtle SE (which
features high mortality rates) was excluded and this might explain why these findings were
very different from prior results. Estimates in children appear to be lower, with case-fatality
rates between 2.7% and 5.2% for younger populations, and up to 13% for adolescents. 103 The
most common cause of GCSE in children is febrile convulsive SE, which has a negligible
morbidity and mortality.
As expected, mortality appears to be related to the underlying cause and to the level of
secondary brain injury from that cause. CNS anoxia and infection carry higher mortality. Any
identifiable cause usually portends a higher mortality as well. Recently,
Rossetti et al.developed a Status Epilepticus Scoring System (STESS) to predict survival
from SE. Their system used four factors (age, history of seizure, type of seizure and
impairment of consciousness). A STESS score was calculated for 154 patients with SE in
three centres before assessment of outcomes. STESS predicted survival with a high negative
predictive value for mortality (0.97). This scoring system still requires prospective validation,
as their study was only an observational cohort.
In terms of morbidity, neurological impairment after SE is usually the greatest
concern. Although data on adults are sparse, studies in children have found that neurological
disability follows in up to 15% of patients. Reduction of IQ has been studied in children, and
some studies, but not all, document a measurable decline. Rates of epilepsy following index
event are also higher. Even with a prolonged febrile convulsion, the rate of subsequent
epilepsy is 10 times higher than for the general population. Animal studies have found that
SE causes hippocampal damage, including oedema and injury, predisposing to recurrent
seizures.
Innovative therapies for refractory SE
In addition, several agents and techniques have been tried in small case series as
innovative therapies for refractory SE. None of the following may be considered for routine
use, but are mentioned here as future directions for treatment. Ketamine has been explored as
a unique agent to control seizures because it targets N-methyl-D-aspartate receptors and
therefore represents a way to activate separate inhibitory mechanisms. One small case series
of five patients with NCSE found that all were controlled, but concerns about its effect on
intracranial pressure linger. Intravenous levetiracetam features a wide therapeutic index and
one small case series of 18 patients with refractory SE similarly showed some promise, with
control achieved in all patients. Of the inhalational anaesthetics, isoflurane in particular has
been studied in a small case series of nine patients and seizure activity ceased in all
patients. Unfortunately, seizures quickly returned in 73% once the gas is discontinued,
limiting its use. Surgery,electroconvulsive therapy and hypothermia have all been tried in
small case series with some success, but further trials are required before these may be
considered for general use.
Conclusions
- Generalized convulsive status epilepticus
SE is a condition that requires early and aggressive therapy for better outcomes.
GCSE in particular features a high mortality, especially in older adults. To prevent seizure
activity from becoming entrenched, the emergency physician must act quickly with the use of
a benzodiazepine, preferably lorazepam, followed by a second- or third-line agent, such as
phenytoin, barbiturate, valproate or benzodiazepine infusion. Although clinical trials are
lacking to recommend a specific protocol, smaller studies suggest that any of these agents
might be of benefit. Admission to an intensive care unit is recommended for patients
continuing to seize, and EEG must be considered in cases where definitive diagnosis cannot
be established.
- Non-convulsive status epilepticus
In NCSE, seizure activity is manifested primarily through behavioural alteration or
obtundation. Confusion and altered mental status, which are commonly encountered in ED,
have very large differential diagnoses. Clearly, the majority of patients presenting to the ED
with altered mental status will not have NCSE asthe cause. Making the diagnosis can be
challenging, although certain scenarios, such as patients who have had a change in their anti-
epileptic medication or those who are having a prolonged post-ictal state after a generalized
convulsion, might indicate the presence of NCSE. The key is for the emergency physician to
have a high index of suspicion and be alert to the possibility of this treatable cause of altered
mental status.
You might also like
- The Miracle Morning PDFDocument6 pagesThe Miracle Morning PDFAnonymous SdgCs6mY81% (32)
- Generalized Convulsive Status Epilepticus in Adults and Children Treatment Guidelines and ProtocolsReviewDocument14 pagesGeneralized Convulsive Status Epilepticus in Adults and Children Treatment Guidelines and ProtocolsReviewAribeth PeñalozaNo ratings yet
- Hanhan 2001Document12 pagesHanhan 2001ATIKAH NUR HAFIZHAHNo ratings yet
- Epidemiology and Outcomes of Status Epilepticus - PMC PDFDocument18 pagesEpidemiology and Outcomes of Status Epilepticus - PMC PDFCi CiNo ratings yet
- Referat Status OkDocument34 pagesReferat Status OkmarfirarizkiNo ratings yet
- Manejo Estatus 2020Document14 pagesManejo Estatus 2020Juanda MedinaNo ratings yet
- Status Epilepticus: Current Understanding: D P, M A M C, D GR M C, G, M PDocument17 pagesStatus Epilepticus: Current Understanding: D P, M A M C, D GR M C, G, M PDMishraNo ratings yet
- Systemic and Neurologic Autoimmune Disorders Associated With Seizures or EpilepsyDocument6 pagesSystemic and Neurologic Autoimmune Disorders Associated With Seizures or EpilepsyarindacalvinesNo ratings yet
- Status Epilepticus in AdultsDocument10 pagesStatus Epilepticus in AdultssiscaNo ratings yet
- Pats 200709-155mgDocument8 pagesPats 200709-155mgDea MaulidiaNo ratings yet
- Evaluation and Management of Seizures and Status EpilepticusDocument32 pagesEvaluation and Management of Seizures and Status Epilepticusmorena19932308No ratings yet
- A "Malignant" Variant of Status EpilepticusDocument8 pagesA "Malignant" Variant of Status Epilepticushijaugreen55No ratings yet
- Clinical Manifestation and Diagnosis of Epilepsy in ElderlyDocument2 pagesClinical Manifestation and Diagnosis of Epilepsy in ElderlyKartika Nurul FahmiNo ratings yet
- Epilepsy: Bassel F. Shneker, MD, and Nathan B. Fountain, MDDocument53 pagesEpilepsy: Bassel F. Shneker, MD, and Nathan B. Fountain, MDDiane Mx100% (1)
- Status Epileptic in Pediatric PDFDocument12 pagesStatus Epileptic in Pediatric PDFHanna SimbolonNo ratings yet
- J Neurol Neurosurg Psychiatry 2016 Dlouhy 402 13Document13 pagesJ Neurol Neurosurg Psychiatry 2016 Dlouhy 402 13pebinscribdNo ratings yet
- Status Epilepticus Work-Up and Management in AdultsDocument9 pagesStatus Epilepticus Work-Up and Management in AdultsAnonymous QLadTClydkNo ratings yet
- Febrile SeizureDocument6 pagesFebrile SeizurepipimseptianaNo ratings yet
- A Cohort Study To Assess The New WHO Japanese Encephalitis Surveillance StandardsDocument9 pagesA Cohort Study To Assess The New WHO Japanese Encephalitis Surveillance StandardsarmankoassracunNo ratings yet
- The NORSE (New-Onset Refractory Status Epileptic Us) SyndromeDocument4 pagesThe NORSE (New-Onset Refractory Status Epileptic Us) Syndromebenghooi75No ratings yet
- Education and Self-Assessment: The Epidemiology of Epilepsy: The Size of The ProblemDocument11 pagesEducation and Self-Assessment: The Epidemiology of Epilepsy: The Size of The ProblemKhalvia KhairinNo ratings yet
- Causes of Status Epilepticus: Seizures in Special and Severe SituationsDocument12 pagesCauses of Status Epilepticus: Seizures in Special and Severe SituationsAlex GasnasNo ratings yet
- Neonatalseizures:An Updateonmechanisms Andmanagement: Frances E. JensenDocument20 pagesNeonatalseizures:An Updateonmechanisms Andmanagement: Frances E. JensenJuan Martín Velasco CárdenasNo ratings yet
- Status Epilepticus in AdultsDocument3 pagesStatus Epilepticus in AdultsampalNo ratings yet
- Lennox Gastaut SyndromeDocument12 pagesLennox Gastaut SyndromedulcejuvennyNo ratings yet
- Peculiarities of The Effect of Epilepsy On The Hypothalamic-Pituitary SystemDocument3 pagesPeculiarities of The Effect of Epilepsy On The Hypothalamic-Pituitary SystemCentral Asian StudiesNo ratings yet
- Fneur 08 00507Document8 pagesFneur 08 00507bozasnachoNo ratings yet
- Epilepsia Adulto Mayor Tto y Comorbilidades 2018 CoreaDocument9 pagesEpilepsia Adulto Mayor Tto y Comorbilidades 2018 Coreafelipe10054910No ratings yet
- Status Epilepticus in Critically Ill PatientsDocument11 pagesStatus Epilepticus in Critically Ill PatientsAkbal Nur KarimNo ratings yet
- Sleep Hypoventilation in Neuromuscular and Chest Wall DisordersDocument15 pagesSleep Hypoventilation in Neuromuscular and Chest Wall Disorderssavvy_as_98-1No ratings yet
- Kejang HiperglikemiaDocument10 pagesKejang HiperglikemiaAbigail PheiliaNo ratings yet
- Sloan Szse Acep 2005 PedsDocument8 pagesSloan Szse Acep 2005 Pedsstrawberry pieNo ratings yet
- EEG Endpoints IV Treatment For RSE and SRSE 2020Document12 pagesEEG Endpoints IV Treatment For RSE and SRSE 2020luigi.pietro.carlo.undaNo ratings yet
- Evaluating An Apparent Unprovoked - NeurologyDocument15 pagesEvaluating An Apparent Unprovoked - NeurologyCARZ 42No ratings yet
- Bravo 2021Document22 pagesBravo 2021Ivan MihailovicNo ratings yet
- Jurnal ReadingDocument27 pagesJurnal ReadingPatresya LantanNo ratings yet
- Status Epilepticus in Adults: A Study From Nigeria: SciencedirectDocument6 pagesStatus Epilepticus in Adults: A Study From Nigeria: SciencedirectLuther ThengNo ratings yet
- Epilepsy: EssentialsDocument3 pagesEpilepsy: Essentialshannah_pharmNo ratings yet
- Key Concepts: Susan J. Rogers and Jose E. CavazosDocument24 pagesKey Concepts: Susan J. Rogers and Jose E. CavazosLia Ruby FariztaNo ratings yet
- Epilepsy: New Advances: Journal ReadingDocument29 pagesEpilepsy: New Advances: Journal Readingastra yudhaTagamawanNo ratings yet
- 29fc 2 PDFDocument6 pages29fc 2 PDFgunawanNo ratings yet
- SNM America PsikiatriDocument7 pagesSNM America PsikiatriMuhammad Abdul RahmanNo ratings yet
- 4 Hashimoto's Encephalopathy: Myth or Reality? An Endocrinologist's PerspectiveDocument14 pages4 Hashimoto's Encephalopathy: Myth or Reality? An Endocrinologist's PerspectiveAleksandar KopitovićNo ratings yet
- Prevention, Treatment, and Monitoring of Seizures in The Intensive Care UnitDocument17 pagesPrevention, Treatment, and Monitoring of Seizures in The Intensive Care Unitanggi abNo ratings yet
- Neurolupus 1Document13 pagesNeurolupus 1Josue LayedraNo ratings yet
- Current Treatment For Generalized Convulsive Status Epilepticus in AdultsDocument15 pagesCurrent Treatment For Generalized Convulsive Status Epilepticus in AdultsKrisna DwiantamaNo ratings yet
- Causes of Status EpilepticusDocument12 pagesCauses of Status EpilepticusSergio MouraNo ratings yet
- Epilepsia - 2005 - Fountain - Status Epilepticus Risk Factors and ComplicationsDocument8 pagesEpilepsia - 2005 - Fountain - Status Epilepticus Risk Factors and ComplicationssyavinaNo ratings yet
- Epilepsy 2Document6 pagesEpilepsy 2fikaNo ratings yet
- Kejang Hiperglikemi PDFDocument10 pagesKejang Hiperglikemi PDFNishfullaili Nurun NisaNo ratings yet
- SeizureDocument2 pagesSeizureS SNo ratings yet
- AkutDocument5 pagesAkutFanel PutraNo ratings yet
- Lennox-Gastaut Syndrome: A Comprehensive ReviewDocument12 pagesLennox-Gastaut Syndrome: A Comprehensive ReviewLuís Felipe AmorimNo ratings yet
- Explaining The Unexplained Expecting The Unexpected: Where Are We With Sudden Unexpected Death in Epilepsy?Document5 pagesExplaining The Unexplained Expecting The Unexpected: Where Are We With Sudden Unexpected Death in Epilepsy?Dian Permana BurlandNo ratings yet
- Status Epilepticus in A ChildDocument37 pagesStatus Epilepticus in A ChildVibin K vNo ratings yet
- Review: Hartmut Meierkord, Martin HoltkampDocument11 pagesReview: Hartmut Meierkord, Martin HoltkampMelissa Peña LópezNo ratings yet
- Estatus Epileptico EmergencyDocument13 pagesEstatus Epileptico EmergencytorresjairrNo ratings yet
- Cerebrospinal Fluid and Blood Biomarkers of Status Epilepticus - 2020Document40 pagesCerebrospinal Fluid and Blood Biomarkers of Status Epilepticus - 2020Reny Wane Vieira dos SantosNo ratings yet
- Problemas Clínicos y Apnea Del SueñoDocument12 pagesProblemas Clínicos y Apnea Del SueñoVALENTIN MARTINEZ-OTERO PEREZNo ratings yet
- Handbook of Medical Neuropsychology: Applications of Cognitive NeuroscienceFrom EverandHandbook of Medical Neuropsychology: Applications of Cognitive NeuroscienceNo ratings yet
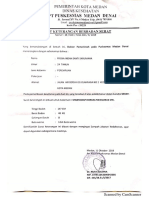
- Surat SehatDocument1 pageSurat SehatIndah Maharani NasutionNo ratings yet
- Paraphrasing Skill: By. Ulfa Rahmi, S. Si, M. EdDocument19 pagesParaphrasing Skill: By. Ulfa Rahmi, S. Si, M. EdIndah Maharani Nasution100% (2)
- Hormone in Pituitary GlandDocument15 pagesHormone in Pituitary GlandIndah Maharani NasutionNo ratings yet
- Hormone in Pituitary GlandDocument15 pagesHormone in Pituitary GlandIndah Maharani NasutionNo ratings yet
- Elliptical: By: Nur AzizahDocument9 pagesElliptical: By: Nur AzizahIndah Maharani NasutionNo ratings yet
- Name: Indah Maharani Nasution: Class: 3B/PsikDocument5 pagesName: Indah Maharani Nasution: Class: 3B/PsikIndah Maharani NasutionNo ratings yet
- 25 Stories in EnglishDocument39 pages25 Stories in EnglishIndah Maharani NasutionNo ratings yet
- Pharmacology For Nursing Care 6e Test BankDocument5 pagesPharmacology For Nursing Care 6e Test BankSharon Spence100% (36)
- Ist Year Assignment July 2019 PDFDocument16 pagesIst Year Assignment July 2019 PDFAsha SurelaNo ratings yet
- HOPE Model - Ideas Tackling 2020 Pandemic by Gandhi Medical College, Hyderabad StudentsDocument11 pagesHOPE Model - Ideas Tackling 2020 Pandemic by Gandhi Medical College, Hyderabad StudentsdrswetharanisavalaNo ratings yet
- Society: America's "Young" Weight ProblemDocument9 pagesSociety: America's "Young" Weight ProblemFabiano HenriqueNo ratings yet
- Venue Letter Email - Life Skills - Islamabad - November - 2023Document1 pageVenue Letter Email - Life Skills - Islamabad - November - 2023janshabana9166No ratings yet
- Hydroseeding WorkDocument26 pagesHydroseeding WorkSamsiah TolaNo ratings yet
- EP1400 Operation Guide 2 Button KeypadDocument24 pagesEP1400 Operation Guide 2 Button KeypadMambaul UlumNo ratings yet
- Importance of Traditional Indian Dairy ProductsDocument20 pagesImportance of Traditional Indian Dairy ProductsTapas KarNo ratings yet
- DR HaifaDocument28 pagesDR HaifaAlex SamNo ratings yet
- Andariki AyurvedamDocument6 pagesAndariki AyurvedammurugangdNo ratings yet
- Endocrine, Reproductive Block ObjectivesDocument22 pagesEndocrine, Reproductive Block Objectiveshur-azmi-1154No ratings yet
- Ati Fundamentals Proctored Exam 2019 2022 2023 Retake Guide Complete Study Guide Questions PDFDocument67 pagesAti Fundamentals Proctored Exam 2019 2022 2023 Retake Guide Complete Study Guide Questions PDFndirangucollins9No ratings yet
- 8223-Article Text-34619-3-10-20230704Document6 pages8223-Article Text-34619-3-10-20230704Dea NopiantiNo ratings yet
- Individual and Family Application Checklist (Uae) : How To ApplyDocument9 pagesIndividual and Family Application Checklist (Uae) : How To ApplyJacob PriyadharshanNo ratings yet
- Ugrc ExamDocument3 pagesUgrc Examgameda nicoNo ratings yet
- Biodeterioration of Cosmetic ProductsDocument21 pagesBiodeterioration of Cosmetic ProductsSundaralingam RajNo ratings yet
- Anemia: Clinical Approach and Management: Dairion Gatot, Savita Handayani, Heny Syahrini, Andri MardiaDocument22 pagesAnemia: Clinical Approach and Management: Dairion Gatot, Savita Handayani, Heny Syahrini, Andri MardiarubyniNo ratings yet
- Resisted Ex'sDocument109 pagesResisted Ex'svenkata ramakrishnaiahNo ratings yet
- Statistical Diabetic ReportDocument10 pagesStatistical Diabetic ReportSunila AkramNo ratings yet
- QR HypertensionDocument8 pagesQR Hypertensionwaniaqilah workNo ratings yet
- M-Mode Echocardiography in DogsDocument10 pagesM-Mode Echocardiography in DogsTactvisNo ratings yet
- Female Natural Bodybuilding Competition Preparation - A 6-Week Cas PDFDocument64 pagesFemale Natural Bodybuilding Competition Preparation - A 6-Week Cas PDFtamNo ratings yet
- Osh 6301Document4 pagesOsh 6301Hassan ShahzadNo ratings yet
- Understanding Rape Shield Laws - Michelle J AndersonDocument10 pagesUnderstanding Rape Shield Laws - Michelle J Andersonmary engNo ratings yet
- 1 Vias de Desarrollo en Los Trastornos Afectivos en La Vida Adulta Existe Un Rol de Las Alteraciones Del SueñoDocument12 pages1 Vias de Desarrollo en Los Trastornos Afectivos en La Vida Adulta Existe Un Rol de Las Alteraciones Del SueñoCamila Quispe aquipuchoNo ratings yet
- NCM 117a Module #3 (B2)Document25 pagesNCM 117a Module #3 (B2)Jan Lianne BernalesNo ratings yet
- Toward A Healthy and Harmonious Life in China: Stemming The Rising Tide of Non-Communicable DiseasesDocument48 pagesToward A Healthy and Harmonious Life in China: Stemming The Rising Tide of Non-Communicable DiseasesADB Health Sector GroupNo ratings yet
- Robinson2019 Article MeasuringAttitudesTowardsMentaDocument8 pagesRobinson2019 Article MeasuringAttitudesTowardsMentaVan LopezNo ratings yet
- Brunner and Suddarth's Textbook of Medical-Surgical Nursing 12th Ed. (Dragged) 4Document1 pageBrunner and Suddarth's Textbook of Medical-Surgical Nursing 12th Ed. (Dragged) 4jamie carpioNo ratings yet