Professional Documents
Culture Documents
1042 Full PDF
1042 Full PDF
Uploaded by
Ramy ElmasryCopyright:
Available Formats
You might also like
- Dai 2001Document5 pagesDai 2001Sri MahadhanaNo ratings yet
- Schick2006 Treatment PDFDocument7 pagesSchick2006 Treatment PDFRifqi FNo ratings yet
- OTA Highlight Paper Predicting Future Displacement of Nonoperatively Managed Lateral Compression Sacral Fractures - Can It Be DoneDocument6 pagesOTA Highlight Paper Predicting Future Displacement of Nonoperatively Managed Lateral Compression Sacral Fractures - Can It Be Doneakb601No ratings yet
- Spinal Epidural Cavernous Hemangiomas in The 2024 International Journal of SDocument3 pagesSpinal Epidural Cavernous Hemangiomas in The 2024 International Journal of SRonald QuezadaNo ratings yet
- Dickman Classification (1996)Document7 pagesDickman Classification (1996)João Pedro ZenattoNo ratings yet
- Fractures of The Scapular Neck: Diagnosis, Classifications and TreatmentDocument11 pagesFractures of The Scapular Neck: Diagnosis, Classifications and Treatmentsoheil ostovanNo ratings yet
- Posterior Lumbar Interbody Fusion (PLIF) With Cages and Local Bone Graft in The Treatment of Spinal StenosisDocument7 pagesPosterior Lumbar Interbody Fusion (PLIF) With Cages and Local Bone Graft in The Treatment of Spinal StenosisMd.Shafiul EzazNo ratings yet
- The Use of A Transolecranon Pin in The Treatment of Flexion-Type SCFsDocument6 pagesThe Use of A Transolecranon Pin in The Treatment of Flexion-Type SCFsBariša KiršnerNo ratings yet
- Fuchs 2005Document5 pagesFuchs 2005BudhiNo ratings yet
- 264 2014 Article 2282Document4 pages264 2014 Article 2282fm123165464No ratings yet
- J Neurol Sci (Turk)Document9 pagesJ Neurol Sci (Turk)nulaeli Siti ANo ratings yet
- Endoscopic Resection of Symptomatic Osteochondroma of The Distal FemurDocument4 pagesEndoscopic Resection of Symptomatic Osteochondroma of The Distal FemurAlex CirlanNo ratings yet
- Foramen Huschke PatologicoDocument7 pagesForamen Huschke PatologicoLM AdrianneNo ratings yet
- Tur CicaDocument8 pagesTur CicazubayetarkoNo ratings yet
- Intramedullary K-Wire Fixation of Metacarpal Fractures: Georg Kelsch Christoph UlrichDocument4 pagesIntramedullary K-Wire Fixation of Metacarpal Fractures: Georg Kelsch Christoph UlrichVolcNo ratings yet
- Spinous Process Fractures in Osteoporotic Thoracolumbar Vertebral FracturesDocument4 pagesSpinous Process Fractures in Osteoporotic Thoracolumbar Vertebral FracturesAditya Arya PutraNo ratings yet
- Percutaneous Endoscopic Decompression Via Transforaminal Approach For Lumbar Lateral Recess Stenosis in Geriatric PatientsDocument7 pagesPercutaneous Endoscopic Decompression Via Transforaminal Approach For Lumbar Lateral Recess Stenosis in Geriatric PatientsAmina GoharyNo ratings yet
- Hip Arthroplasty in Failed Intertrochanteric Fract 103652Document6 pagesHip Arthroplasty in Failed Intertrochanteric Fract 103652seatrrtleNo ratings yet
- 5-Level Spondylectomy For en Bloc Resection of Thoracic Chordoma: Case ReportDocument9 pages5-Level Spondylectomy For en Bloc Resection of Thoracic Chordoma: Case Reportholt linNo ratings yet
- Free Hand Pedicle Screw Placement in The Thoracic KIM LENKE 2004 Spine PDFDocument10 pagesFree Hand Pedicle Screw Placement in The Thoracic KIM LENKE 2004 Spine PDFOlgerAlarconCasanovaNo ratings yet
- PCL Avulsion Fracture 2Document2 pagesPCL Avulsion Fracture 2harpreet singhNo ratings yet
- Variability in Olecranon Ao Fracture Fixation: A Radiological StudyDocument6 pagesVariability in Olecranon Ao Fracture Fixation: A Radiological StudyFhietry Idrus ScaftweeNo ratings yet
- Ganesh 2011Document5 pagesGanesh 2011Giang Nguyễn NgânNo ratings yet
- Paper 38Document6 pagesPaper 38Dr Vineet KumarNo ratings yet
- Phillips 2013Document6 pagesPhillips 2013thanawatsimaNo ratings yet
- Songcharoen 1995Document5 pagesSongcharoen 1995Le Manh ThuongNo ratings yet
- Nakamichi 1997Document10 pagesNakamichi 1997miguelNo ratings yet
- Art3a10 10072fs00256-014-1842-5Document9 pagesArt3a10 10072fs00256-014-1842-5api-253958760No ratings yet
- Süleyman Alp Çölbe Mert Çiftdemir Fethi Emre Ustabaşıoğlu Cihan ÖzgürDocument10 pagesSüleyman Alp Çölbe Mert Çiftdemir Fethi Emre Ustabaşıoğlu Cihan Özgüraymanelhoudali6911No ratings yet
- Short Versus Long Outcome RadiologisDocument7 pagesShort Versus Long Outcome Radiologisandy ardiansyahNo ratings yet
- Fluoroscopic Analysis of The Kinematics of Deep Exion in Total Knee ArthroplastyDocument4 pagesFluoroscopic Analysis of The Kinematics of Deep Exion in Total Knee Arthroplastyjmhinos4833No ratings yet
- 3 Column AnkleDocument8 pages3 Column AnkleJosé Eduardo Fernandez RodriguezNo ratings yet
- Ueki 2007Document7 pagesUeki 2007abhishekjha0082No ratings yet
- Pedicle Screw Fixation in Fracture of Thoraco-Lumbar SpineDocument21 pagesPedicle Screw Fixation in Fracture of Thoraco-Lumbar SpineNiyati SharmaNo ratings yet
- Haglund's Syndrome Schneider2000Document5 pagesHaglund's Syndrome Schneider2000emrahaltuntasNo ratings yet
- iCVTPFDocument5 pagesiCVTPFErwin Chiquete, MD, PhDNo ratings yet
- 1413 7852 Aob 24 03 00159Document5 pages1413 7852 Aob 24 03 00159Rakesh KumarNo ratings yet
- Effects On Inadvertent Endplate Fracture Following Lateral Cage Placement On Range of Motion and Indirect Spine Decompression in Lumbar Spine Fusion Constructs: A Cadaveric StudyDocument8 pagesEffects On Inadvertent Endplate Fracture Following Lateral Cage Placement On Range of Motion and Indirect Spine Decompression in Lumbar Spine Fusion Constructs: A Cadaveric Studysiti hanifahNo ratings yet
- Zygomatic Fractures: Classification and Complications: TveterasDocument7 pagesZygomatic Fractures: Classification and Complications: TveterasBriando Stevano LinelejanNo ratings yet
- Rodilla Inervación Tran2018 PDFDocument8 pagesRodilla Inervación Tran2018 PDFLore BarreraNo ratings yet
- Discrimination of Metastatic From Acute Osteoporotic Compression Spinal Fractures With MRIDocument9 pagesDiscrimination of Metastatic From Acute Osteoporotic Compression Spinal Fractures With MRIChow Tat SingNo ratings yet
- Using The Endoscopic Transconjunctival and Transcaruncular Approach To Repair Combined Orbital Floor and Medial Wall Blowout FracturesDocument4 pagesUsing The Endoscopic Transconjunctival and Transcaruncular Approach To Repair Combined Orbital Floor and Medial Wall Blowout Fracturesstoia_sebiNo ratings yet
- Unstable Burst Fractures of The Thoraco-Lumbar Junction TreatmentDocument8 pagesUnstable Burst Fractures of The Thoraco-Lumbar Junction TreatmentRafael Jardim de MouraNo ratings yet
- Yulisa 2Document7 pagesYulisa 2Ardi WidiatmikaNo ratings yet
- A Long Term Follow Up Study of Total Meniscectomy.30Document5 pagesA Long Term Follow Up Study of Total Meniscectomy.30Anshal GuptaNo ratings yet
- (10920684 - Neurosurgical Focus) Surgical Treatment of Primary Sacral Tumors - Complications Associated With SacrectomyDocument8 pages(10920684 - Neurosurgical Focus) Surgical Treatment of Primary Sacral Tumors - Complications Associated With Sacrectomyfloroiu.ioana.valeriaNo ratings yet
- Anterior Decompression Techniques For Thoracic and Lumbar FracturesDocument10 pagesAnterior Decompression Techniques For Thoracic and Lumbar Fracturesmetasoniko81No ratings yet
- Operative Treatment of Peritrochanteric Osteoporotic Fractures With Proximal Femur Locking Compression Plate A Consecutive StudyDocument6 pagesOperative Treatment of Peritrochanteric Osteoporotic Fractures With Proximal Femur Locking Compression Plate A Consecutive StudyAthenaeum Scientific PublishersNo ratings yet
- Relación Flujo y Fractura ClinicaDocument5 pagesRelación Flujo y Fractura ClinicaPedro TorresNo ratings yet
- Nasional 3 NIC:KOE Penetrating Cervial Spine Injury ENDocument6 pagesNasional 3 NIC:KOE Penetrating Cervial Spine Injury ENHeru Sutanto KNo ratings yet
- Syndesmotic Screw Removed Verusus Retained: A Comparative Functional AnalysisDocument4 pagesSyndesmotic Screw Removed Verusus Retained: A Comparative Functional AnalysisSarath KumarNo ratings yet
- Core Decompression With Bone Grafting For Osteonecrosis of The Femoral HeadDocument8 pagesCore Decompression With Bone Grafting For Osteonecrosis of The Femoral Headmuhammad0umar-4No ratings yet
- Clinical Outcome of A Precontoured Symphysis Pubis Plate With Tension Band Wiring For Traumatic Symphysis Pubis Rupture in Pelvic FracturesDocument6 pagesClinical Outcome of A Precontoured Symphysis Pubis Plate With Tension Band Wiring For Traumatic Symphysis Pubis Rupture in Pelvic FracturesodyNo ratings yet
- Surgical Management of Sacral Chordomas - Illustrative Cases and Current Management ParadigmsDocument7 pagesSurgical Management of Sacral Chordomas - Illustrative Cases and Current Management ParadigmsHugo JBNo ratings yet
- Treatment of Distal Humerus FracturedDocument10 pagesTreatment of Distal Humerus Fracturedauliya ningsihNo ratings yet
- Ojo 2013112116194629 PDFDocument5 pagesOjo 2013112116194629 PDFYash SharmaNo ratings yet
- "A To P" Screw Versus Posterolateral Plate For PosteriorDocument6 pages"A To P" Screw Versus Posterolateral Plate For PosteriorErlin EsauNo ratings yet
- (10920684 - Neurosurgical Focus) Percutaneous Pedicle Screw Fixation of The Lumbar SpineDocument9 pages(10920684 - Neurosurgical Focus) Percutaneous Pedicle Screw Fixation of The Lumbar Spineefancoolhand09No ratings yet
- Giacalone 2015Document7 pagesGiacalone 2015Joseval FilhoNo ratings yet
- Surgery of the Cranio-Vertebral JunctionFrom EverandSurgery of the Cranio-Vertebral JunctionEnrico TessitoreNo ratings yet
- 586 2009 Article 1037Document7 pages586 2009 Article 1037Ramy ElmasryNo ratings yet
- Versus Overall Sagittal AlignmentDocument7 pagesVersus Overall Sagittal AlignmentRamy ElmasryNo ratings yet
- Spontaneous Height Restoration of Vertebral Compression FractureDocument4 pagesSpontaneous Height Restoration of Vertebral Compression FractureRamy ElmasryNo ratings yet
- Pediatrics With Answers and ExplanationsDocument77 pagesPediatrics With Answers and ExplanationsRamy Elmasry100% (6)
- Significance of Dynamic Mobility in Restoring Vertebral Body Height in VertebroplastyDocument4 pagesSignificance of Dynamic Mobility in Restoring Vertebral Body Height in VertebroplastyRamy ElmasryNo ratings yet
- 16-Zhou Et AlDocument6 pages16-Zhou Et AlRamy ElmasryNo ratings yet
- 86 D 8Document7 pages86 D 8Ramy ElmasryNo ratings yet
- Leakage of Cement in Percutaneous Transpedicular Vertebroplasty For Painful Osteoporotic Compression FracturesDocument7 pagesLeakage of Cement in Percutaneous Transpedicular Vertebroplasty For Painful Osteoporotic Compression FracturesRamy ElmasryNo ratings yet
- MainDocument8 pagesMainRamy ElmasryNo ratings yet
- Acute Osteoporotic Vertebral Collapse: Open Study On Percutaneous Injection of Acrylic Surgical Cement in 20 PatientsDocument6 pagesAcute Osteoporotic Vertebral Collapse: Open Study On Percutaneous Injection of Acrylic Surgical Cement in 20 PatientsRamy ElmasryNo ratings yet
- Percutaneous Vertebroplasty and Balloon Kyphoplasty For The Treatment of Osteoporotic Vertebral Compression Fractures and Osteolytic TumoursDocument10 pagesPercutaneous Vertebroplasty and Balloon Kyphoplasty For The Treatment of Osteoporotic Vertebral Compression Fractures and Osteolytic TumoursRamy ElmasryNo ratings yet
- Morning Endorsements: MAY 15-16, 2019 Coc: Dr. Arriola Rod: Dr. Oyas Iod: Co & DickinaDocument11 pagesMorning Endorsements: MAY 15-16, 2019 Coc: Dr. Arriola Rod: Dr. Oyas Iod: Co & DickinaNeil Victor Ongco PajugotNo ratings yet
- Surgical Management in LeprosyDocument33 pagesSurgical Management in Leprosynsv.epicNo ratings yet
- Brochure of ICE SHAPING IV PRODocument15 pagesBrochure of ICE SHAPING IV PROUniforrmes ArcoirisNo ratings yet
- Perioperative Care For CABG PatientsDocument32 pagesPerioperative Care For CABG PatientsAya EyadNo ratings yet
- HIATAL HERNIA PPT Final PDFDocument49 pagesHIATAL HERNIA PPT Final PDFregysujit60% (5)
- Instruments of Throat: Sparsh Goel 77Document19 pagesInstruments of Throat: Sparsh Goel 77Sparsh GoelNo ratings yet
- Hernia QuestionsDocument6 pagesHernia QuestionsNica Lopez Fernandez100% (1)
- LAPORAN TUTORIAL SKENARIO 5 B.3-DikompresiDocument30 pagesLAPORAN TUTORIAL SKENARIO 5 B.3-DikompresiKrishna Dava Putra SNo ratings yet
- Frozen Shoulder - Adhesive CapsulitisDocument8 pagesFrozen Shoulder - Adhesive CapsulitisfriskaNo ratings yet
- Product Catalog Bauerfeind Usa 0312Document88 pagesProduct Catalog Bauerfeind Usa 0312Guillermo Carpio FloriaNo ratings yet
- Atls Pre Test 1 PDFDocument72 pagesAtls Pre Test 1 PDFmary011danielNo ratings yet
- Intestinal Ostomy: Classification, Indications, Ostomy Care and Complication ManagementDocument8 pagesIntestinal Ostomy: Classification, Indications, Ostomy Care and Complication ManagementEriekafebriayana RNo ratings yet
- BD-11097 UltraCor BrochureDocument3 pagesBD-11097 UltraCor Brochurepo leongNo ratings yet
- 6.6) Diagnostic and Therapeutic Abdominal Paracentesis - UpToDateDocument18 pages6.6) Diagnostic and Therapeutic Abdominal Paracentesis - UpToDatefedericoNo ratings yet
- Arn Report List 20200505Document305 pagesArn Report List 20200505zoheir salmaniNo ratings yet
- PTBD 2Document4 pagesPTBD 2Alcntara AllenNo ratings yet
- ORDocument4 pagesORJoana Marie A. LaoNo ratings yet
- Spiritual Needs of A Patient With Acute IllnessDocument3 pagesSpiritual Needs of A Patient With Acute IllnessMarimiel PagulayanNo ratings yet
- V3 WEREWOLF Tech Bro Flo 0720Document6 pagesV3 WEREWOLF Tech Bro Flo 0720hongyuan xuNo ratings yet
- Laparoscopic Cholecystectomy Perioperative Management: An UpdateDocument5 pagesLaparoscopic Cholecystectomy Perioperative Management: An UpdateNurlailah AliNo ratings yet
- Pearls Nov Dec 2010Document3 pagesPearls Nov Dec 2010Nhật LongNo ratings yet
- Laser Technolas 217 - Excimer Laser SystemDocument34 pagesLaser Technolas 217 - Excimer Laser Systemrubens.nascimento213No ratings yet
- Cone-Beam Computed Tomography and Its Applications in DentistryDocument4 pagesCone-Beam Computed Tomography and Its Applications in DentistryMeris JugadorNo ratings yet
- Karnatka 2023Document3 pagesKarnatka 2023bvkarthik.99No ratings yet
- Appleby OperationDocument9 pagesAppleby OperationPeter Paul PascualNo ratings yet
- Helland L Nursing ChecklistDocument6 pagesHelland L Nursing Checklistapi-703155063No ratings yet
- Complications of The Arteriovenous Fistula: A Systematic ReviewDocument45 pagesComplications of The Arteriovenous Fistula: A Systematic ReviewAnonymous ATdLPZNo ratings yet
- Hernia 1Document28 pagesHernia 1Aminatulhuda SulaimanNo ratings yet
- យល់ដឹងអំពីតួនាទីរបស់ខ្នែងពោះវៀនDocument4 pagesយល់ដឹងអំពីតួនាទីរបស់ខ្នែងពោះវៀនReal Madrid FCNo ratings yet
- Intra Operative Allowable Blood Loss: Estimation Made Easy: Original Research ArticleDocument5 pagesIntra Operative Allowable Blood Loss: Estimation Made Easy: Original Research ArticlesafwanNo ratings yet
1042 Full PDF
1042 Full PDF
Uploaded by
Ramy ElmasryOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
1042 Full PDF
1042 Full PDF
Uploaded by
Ramy ElmasryCopyright:
Available Formats
New Symptomatic Compression Fracture after
ORIGINAL
Percutaneous Vertebroplasty at the
RESEARCH Thoracolumbar Junction
C.C. Lin BACKGROUND AND PURPOSE: The purpose of this study was to investigate the risk factors for new
I.H. Chen symptomatic vertebral compression fractures after vertebroplasty at the thoracolumbar junction.
T.C. Yu MATERIALS AND METHODS: We conducted a retrospective analysis of 53 patients treated with per-
A. Chen cutaneous vertebroplasty at the thoracolumbar junction (T12, L1). The follow-up period was 1527
months. The occurrence of new symptomatic vertebral compression fractures was recorded after
P.S. Yen
vertebroplasty. We evaluated patient age and sex, amount of injected cement, vacuum clefts in the
collapsed bodies, initial wedge angle of the compression fracture, change of the wedge angle after
vertebroplasty, intradiskal cement leak, and percentage of height restoration of the vertebral body. In
this report, we surveyed the possible risk factors for new symptomatic vertebral compression
fractures.
RESULTS: Thirty-nine (74%) of the 53 patients had fluid and/or air in the compression fracture at the
thoracolumbar junction (T12, L1). Eight (20.5%) of the 39 patients with vacuum clefts had new
symptomatic compression fracture after vertebroplasty between 1 month and 4 days after surgery to
23 months and 4 days after surgery. The patients with new symptomatic compression fracture had
higher initial wedge angle and wedge angle change (more than 7) after vertebroplasty than those
without fractures; these data were considered statistically significant.
CONCLUSIONS: The incidence of vacuum clefts in the compression fracture at the thoracolumbar
junction is high (74%). The severity of initial wedge angle and wedge angle change affects the
incidence of new symptomatic compression fracture.
F lexion and extension of the spine is most dynamic at the
thoracolumbar junction.1 Vertebral insufficiency fractures
at these levels would be less likely to undergo complete healing
screw fixation, a history of steroid use, and multiple myeloma or
pathologic fracture.
Only 53 patients (42 female, 11 male; mean age, 76.1 years) with 61
than the other vertebral levels, which are comparatively im- vertebral body fractures (T12 or L1, 53; 8 at other levels) were eligible
mobile. One study reported that elderly patients with a se- for the study. The preoperative spine MR imaging and conventional
verely collapsed or deformed fracture at the thoracolumbar radiographs were taken about 17 days before the procedure. The
junction were at high risk of developing a nonunion of the image protocol included sagittal T1-weighted (TR, 600 650 ms; TE
fracture.2 This unhealed fracture appeared as an air-filled cleft 9 11 ms) and T2-weighted (TR, 3500 3750 ms; TE, 100 116 ms)
on conventional radiograph or as fluid-filled cavities on MR spin-echo images, short inversion recovery (STIR) images (TR, 3800
imaging. Although some long-term follow-up studies3,4 have ms; TE, 38 ms; TI, 150 ms) with 4-mm section thickness. The first
discussed the association between new compression fracture radiograph was taken about 13 days after the vertebroplasty. The
and vertebroplasty, the risk factors associated with new symp- final follow-up images were obtained and reviewed 1527 months
tomatic compression fracture and vertebroplasty are still un- after the procedure. Only patients with new symptomatic fracture
der investigation. In this study, we evaluated possible risk fac- after vertebroplasty had follow-up MR imaging. The indication for
tors of developing new symptomatic compression fracture vertebroplasty was painful compression fracture with hyperintensity
after vertebroplasty at the thoracolumbar junction. on sagittal STIR images with or without a vacuum cleft. Patients with
chronic compression fractures without abnormal signal intensity
Materials and Methods change on spine MR imaging were excluded.
Between September 2002 and October 2004, our medical center per-
Two experienced neuroradiologists (P.S.Y., C.C.L.) performed
formed percutaneous vertebroplasty procedures on 174 patients with
the procedure using a modified form of the method used by Jensen et
201 levels of vertebral bodies. Of these 174 patients, we excluded those
al.5 The patient was in the prone position under local anesthesia. An
who did not have a compression fracture at the thoracolumbar junc-
11- or 13-gauge bone marrow biopsy needle was used to puncture the
tion (T12, L1) and who did not have preoperative or postoperative
collapsed vertebral body through one of the pedicles, and the needle
radiographs. We also excluded patients who had laminectomy and
was advanced to the anterior third of the vertebral body or into the
vacuum cleft, under fluoroscopic guidance. One 20-mL syringe kept
Received August 2, 2006; accepted after revision October 4. under negative pressure was connected to the biopsy needle to suck
From the Departments of Medical Imaging (P.S.Y., C.C.L., A.C.), Orthopedics (I.H.C., T.C.Y.), out the fluid or bone marrow. The bone cement (Surgical Simplex P;
and Anesthesiology (A.C.), Buddhist Tzu Chi General Hospital, Tzu Chi University, Hualien, Stryker Howmedica Osteonics, Limerick, Ireland) was prepared by
Taiwan.
mixing the copolymer powder with sterile barium sulfate and mono-
Address correspondence to Dr. Pao-Sheng Yen, Department of Radiology, Buddhist
Tzu Chi General Hospital, Tzu Chi University, 707, Section 3, Chung Yang Road, mer liquid for polymerization. The bone cement was injected manu-
Hualien, Taiwan; e-mail:cc@tma.tw ally under fluoroscopic guidance. The injection was stopped if the
DOI 10.3174/ajnr.A0520 bone cement 1) filled the vacuum cleft, 2) reached the posterior
1042 Lin AJNR 28 Jun-Jul 2007 www.ajnr.org
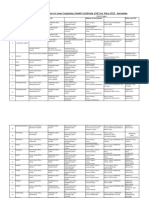
Table 1: Patients undergoing vertebroplasty at thoracolumbar junction with and without vacuum clefts
Initial Wedge Improved
No of Age Sex Cement Intradiskal Leak Wedge Angle Percentage
Group Patients (yrs) (F/M, no.) (mL) (u disk*:l disk) Angle () Change of Height
I 14 71.6 11/3 3.8 3:1 15.3 1.2 9.0
II 39 77.7 31/8 5.3 6:2 14.5 6.3 48.3
P value .01 .006 .42 .001 .001
Note:F indicates female; M, male; u, upper; l, lower.
* Cement leakage into the upper disk.
Cement leakage into the lower disk.
Wedge angle of the collapsed body before vertebroplasty.
(Wedge angle change) before (wedge angle) after vertebroplasty.
(H/HN) post (H/HN)pre/(H/HN) pre.
Fig 1. Measurement of the collapsed vertebral body before
(A ) and after (B ) vertebroplasty. (H indicates the height of
the collapsed body at the center; NH, the height of the
posterior border of an adjacent normal vertebral body; , the
wedge angle as described by Teng et al.7)
the follow-up MR imaging, which showed
new compression fracture.
We used the single-tail Student t test to
evaluate the difference between groups I and
II. To analyze the risk factors in group II, lo-
gistic regression with SPSS software (SPSS,
Chicago, Ill) was applied. We set value equal
to 0.05 as statistically significant.
Results
The intraclass correlation coefficients
for the height of the vertebral body and
the wedge angle were 0.94 and 0.92
SPINE
fourth of the vertebral body, or 3) was leaking into the perivertebral (C.C.L.) and 0.97 and 0.96 (P.S.Y.). The interobserver repro-
veins or significantly leaking into the disk space. ducibility between the 2 authors was 0.92 and 0.88 for the
The preoperative spine MR imaging and plain film were reviewed vertebral body height and wedge angle, respectively.
to identify a vacuum cleft. The vacuum clefts of the vertebral bodies Of the 53 patients, vacuum clefts were found in 39 (74%)
ORIGINAL RESEARCH
are depicted as fluid- or air-filled clefts inside the vertebral body. treated vertebral bodies at the thoracolumbar junction. Eight
Fluid-filled clefts were defined as well-demarcated, linear, or ellipsoid (15.1%) of the 53 patients developed a new compression frac-
areas of T2 prolongation, which were isointense relative to CSF on ture after vertebroplasty. The mean age and sex distributions
T2-weighted images acquired in the sagittal plane.6 All the images were not significantly different between groups I and II,
were blindly reviewed by the 2 neuroradiologists (P.S.Y., C.C.L.). If though the mean age was a little higher in group II. The
they disagreed on interpretation of the images, they reviewed the data amount of injected cement, wedge angle change, and percent-
together to establish a consensus. The patients were divided into 2 age of height restoration were significantly higher in group II
groups: group I consisted of patients with no vacuum clefts in the than in group I.
collapsed vertebral body, and group II consisted of those with vacuum We further analyzed group II with logistic regression to
clefts (Table 1). The digital files of each patients radiographs before evaluate the correlation of these factors: age, sex, initial wedge
and after the vertebroplasty were used to measure the following: 1) angle, intradiskal leakage, wedge angle change, and percentage
wedge angle of the compressed vertebral body, 2) height at the center of change of height. Initial wedge angle, change in wedge an-
of the collapsed vertebral body, and 3) height of the posterior border gle, and percentage of height restoration had significantly in-
of an adjacent normal vertebral body. We used the method described creased odds ratio (Table 2). As a result of the correlation
by Teng et al7 to measure the wedge angle and the height of the col- between wedge angle change and percentage change of height,
lapsed vertebral body. The height improvement at the center of the putting these 2 factors in 1 model would cause a colinear prob-
vertebral body was also calculated as follows: [(H/HN)post (H/ lem. To avoid the colinear problem, we performed the logistic
HN)pre]/[(H/HN)pre] (Fig 1). The 2 neuroradiologists (P.S.Y., regression of wedge angle change with adjustment of the age
C.C.L.) measured the collapsed levels at T12 or L1 in the 53 patients. and sex factors. The odds ratio was 1.46. (Table 3). The odds
The intraobserver and interobserver reproducibility of the measure- ratio of the initial wedge angle to sustaining a new compres-
ments was evaluated by intraclass correlation coefficients. We ignored sion fracture was 1.59 after correlation of the age and sex fac-
the bony spur and focal protrusion of the bone cement to avoid pos- tors (Table 4).
sible biases in taking the measurements before and after the proce- The details of the 8 patients are summarized in Table 5.
dure. The measurements were discussed between the authors to es- There were 11 total new compression fractures in the 8 pa-
tablish consensus. The intervals of new compression fracture were tients. Eight (72.7%) of the 11 new compression fracture levels
recorded according to the time between the initial vertebroplasty and were adjacent to the previously treated vertebral body. In Ta-
AJNR Am J Neuroradiol 28:1042 45 Jun-Jul 2007 www.ajnr.org 1043
Table 2: Risk factor analysis in group II with logistic regression
at the thoracolumbar junction. Almost three fourths of the
patients with fracture at the thoracolumbar junction were
Odds 95.0% CI P found to have vacuum clefts.
Factors Ratio Lower Upper Value Several studies6,8,9 have demonstrated that vertebroplasty
Age 1.05 0.92 1.20 .44 can effectively improve vertebral body height and wedge angle.
Sex 2.04 0.21 19.53 .54 However, the long-term outcome associated with restoration
Cement 1.06 0.70 1.62 .79
Intradiskal leak 2.55 0.27 24.06 .42
of the height and correction of wedge angle was not reported.
Initial wedge angle 1.42 1.11 1.81 .005 In our study, when we put the wedge angle change and per-
Wedge angle change 1.02 1.00 1.03 .02 centage of height restoration into a single logistic regression
Improved percentage of height 1.02 1.00 1.03 .03 model, there was correlation between these 2 factors. The
Note:CI indicates confidence interval. wedge angle change was more remarkable than the percentage
of height restoration. This might be attributed to the following
Table 3: Risk predictor-wedge angle change of new-onset factors: 1) the increased height and wedge angle was propor-
compression fracture after adjusting for age and sex in group II tional and 2) the bone cement was deposited mainly in the
95.0% CI anterior three fourths of the vertebral body. The 8 patients in
Odds P
Factors Ratio Lower Upper Value group II who sustained new symptomatic compression frac-
Wedge angle change 1.46 1.11 1.91 .006
ture after vertebroplasty showed greater initial wedge angle
Age 1.07 0.90 1.28 .44 and wedge angle change (21.4 and 12.6) than the group II
Sex 0.17 0.002 18.84 .46 patients without new fractures (12.7 and 4.7) and the pa-
Note:CI indicates confidence interval. tients in group I (15.3 and 1.2). In those 8 patients, the wedge
angle change ranged from 7 to 20. In previously published
Table 4: Risk predictor-initial wedge angle of new-onset studies,6,8,9 the mean reduction of the wedge angle ranged
compression fracture after adjusting for age and sex in group II from 3.5 to 7.4. The odds ratio of wedge angle change to
95.0% CI sustaining new symptomatic compression fracture was 1.46.
Odds P
Factors Ratio Lower Upper Value
This means that if the wedge angle change increased 1 degree,
then the risk of the new-onset fracture has increased 0.46
Initial wedge angle 1.59 1.17 2.17 .003
Age 1.31 1.01 1.70 .04 times. In addition, 8 (42%) of 19 patients (Table 5) who had a
Sex 8.95 0.08 1027.5 .37 wedge angle change of more than 7 sustained new symptom-
Note:CI indicates confidence interval. atic compression fractures. The incidence was higher than the
incidence reported and also higher than our average.
ble 6, the group II patients were divided into 3 subgroups The initial wedge angle is another factor shown to increase
according to the initial wedge angle. Eight of the 39 patients the risk of new symptomatic compression fracture. When we
had initial wedge angles of more than 20, and 6 (75%) of these put the initial wedge angle and wedge angle change into 1
8 patients developed new symptomatic compression fracture logistic model with age and sex adjustment, the initial wedge
after vertebroplasty. In Table 7, the group II patients were angle was more remarkable than the wedge angle change. This
subdivided into 2 subgroups according to the wedge angle may indicate that wedge angle changes are affected by the ini-
change. Nineteen of the 39 patients had wedge angle reduction tial severity of the wedge deformity. Furthermore, the odds
of more than 7. Eight (42%) of 19 patients sustained new ratio of initial wedge angle to sustaining new symptomatic
symptomatic compression fracture after vertebroplasty. compression fracture is 1.59, which means that the risk of new
compression fracture increased 0.59 times if the initial wedge
Discussion angle increased 1 degree. However, this was a retrospective
The association between percutaneous vertebroplasty and study with nonrandomized data. To definitively demonstrate
newly sustained symptomatic compression fracture is still un- the risks of these 2 possible factors (wedge angle change and
der investigation. New symptomatic compression fracture af- initial wedge angle) to cause new symptomatic compression
ter vertebroplasty has been reported in some studies.3,4 In fracture will require well-designed, randomized, controlled
those studies, the incidence of new vertebral body fracture trials comparing vertebroplasty with conservative therapy.
after percutaneous vertebroplasty was reported to be 12.4%3 Currently, maximum or sufficient filling during vertebro-
and 21.7%.4 In our study, the incidence was 15.1%. This inci- plasty is still controversial.10 The average injected amount of
dence was not higher than in other studies, though we limited cement was 3.8 mL in the patients without vacuum clefts and
the treated vertebral level to the thoracolumbar junction. 5.3 mL in the patients with vacuum clefts. Vacuum clefts re-
Group I (patients without vacuum clefts), showed no new quired more cement to fill the space, but the average injected
symptomatic compression fracture after vertebroplasty. Vac- amount of cement in group II demonstrated no difference in
uum clefts of vertebral bodies can represent unhealed fracture the development of new compression fracture. Thus, the
and can appear as fluid-filled cavities on MR imaging or as amount of cement injection did not influence the develop-
gas-filled cavities on conventional radiographs.6 Two stud- ment of an adjacent new compression fracture in our study.
ies2,7 have reported high frequency of these clefts at the thora- One study11 reported that cement leakage into the disk
columbar junction. The flexion and extension dynamic mo- during vertebroplasty increases the risk of a new fracture of
bility of the spine was thought to be responsible for insufficient adjacent vertebral bodies. In our study, 4 patients in group I
fracture at the thoracolumbar junction. In our study, 39 (74%) and 8 patients in group II experienced cement leakage into the
of the 53 patients had compression fracture with vacuum clefts upper or lower disk. However, only 1 patient from group II
1044 Lin AJNR 28 Jun-Jul 2007 www.ajnr.org
Table 5: Patients who sustained new compression fractures after undergoing vertebroplasty
Ad Fx po Initial Wedge Restoration
Pt PVP PVP Level of Cement Wedge Angle Percentage of Disk
No. Age Sex Level Fluid/Air* (mo/d) Ad Fx (mL) Angle () Change Height (%) Rupture
1 87 M T12 F 23/4 T11, L1 8 24 20 176.6 Lower
2 82 F L1 F/A 2/22 T12 8 21 18 62.0 Upper
3 72 F T12 A 1/4 T9, T11 4 26 9 163.4 Upper
4 73 F T12 F 1/24 L1 5 24 16 170.9 Nil
5 82 F T12 A 15/7 T9, T11 3 22 8 36.0 Upper
6 71 F T12 A 5/16 T11 5 27 13 20.4 Upper
7 78 F L1 F 12 L2 4 17 7 25.4 Nil
8 88 F L1 F 3/15 L5 3.5 10 10 30.2 Nil
Note:PVP level indicates treated level of percutaneous vertebroplasty; Fx, fracture; Ad, adjacent.
* Vacuum cleft with fluid or air in the PVP level.
Interval from the date of PVP to the follow-up MRI in which new symptomatic compression fracture was depicted.
Disk rupture with migration toward the new adjacent compression level in the follow-up MRI.
Table 6: Association of initial wedge angle and new compression
that increased initial wedge angle and change in wedge angle
fracture in group II patients increased the incidence of new symptomatic compression
Initial wedge angle 10 1120 20
fracture. To definitively demonstrate the relationship between
No. of patients 7 24 8
these 2 possible causative factors (wedge angle change and
New fracture* 1 1 6 initial wedge angle) and the incidence of new-onset vertebral
Percentage (%) 14 4 75 fracture will require well-designed, randomized, controlled
* Patient sustained new symptomatic compression fracture after undergoing vertebro- trials comparing vertebroplasty with conservative therapy.
plasty.
Table 7: Association of wedge angle change and new compression
fracture in group II patients References
1. Lindh M. Biomechanics of the lumbar spine. In: Frankel H, Nordin M, eds.
Wedge Angle Change* 7 7 Basic Biomechanics of the Skeletal System. Philadelphia: Lea and Febiger;
No. of patients 20 19 1981:25590
New fracture 0 8 2. Mirovsky Y, Anekstein Y, Shalmon E, et al. Vacuum clefts of the vertebral
Percentage (%) 0 42 bodies. AJNR Am J Neuroradiol 2005;26:1634 40
3. Uppin AA, Hirsch JA, Centenera LV, et al. Occurrence of new vertebral body
* (Wedge angle) before vertebroplasty (wedge angle) after vertebroplasty. fracture after percutaneous vertebroplasty in patients with osteoporosis. Ra-
Patient developed new symptomatic compression fracture after undergoing vertebro-
plasty. diology 2003;226:119 24
4. Syed MI, Patel NA, Jan S, et al. New symptomatic vertebral compression frac-
sustained a new, nonadjacent compression fracture 3 months tures within a year following vertebroplasty in osteoporotic women. AJNR
Am J Neuroradiol 2005;26:1601 04
after the vertebroplasty. Therefore, we did not find a connec- 5. Jensen ME, Evans AJ, Mathis JM, et al. Percutaneous polymethylmethacrylate
tion between disk leakage and new adjacent compression vertebroplasty in the treatment of osteoporotic vertebral body compression
fracture. fractures: technical aspects. AJNR Am J Neuroradiol 1997;18:1897904
6. Lane JI, Maus TP, Wald JT, et al. Intravertebral clefts opacified during
There were several limitations in this study. We did not vertebroplasty: pathogenesis, technical implications, and prognostic signifi-
have data to survey the severity of osteoporosis in different cance. AJNR Am J Neuroradiol 2002;23:1642 46
groups, which was thought to be a significant factor for pro- 7. Teng MM, Wei CJ, Wei LC, et al. Kyphosis correction and height restoration
gression of compression fracture. Furthermore, the number of effects of percutaneous vertebroplasty. AJNR Am J Neuroradiol 2003;24:1893900
8. Dublin AB, Hartman J, Latchaw RE, et al. The vertebral body fracture in
patients in our study was small. Another limitation is that only osteoporosis: restoration of height using percutaneous vertebroplasty. AJNR
patients who had symptomatic new compression fracture re- Am J Neuroradiol 2005;26:489 92
ceived MR imaging in the follow-up period. Asymptomatic 9. Carlier RY, Gordji H, Mompoint DM, et al. Osteoporotic vertebral collapse:
percutaneous vertebroplasty and local kyphosis correction. Radiology
new compression fracture with only MR imaging signal inten- 2004;233:89198
sity change may have been missed. 10. Baroud G, Heini P, Nemes J, et al. Biomechanical explanation of adjacent
fractures following vertebroplasty. Radiology 2003;229:606 07; author reply
607 08
Conclusions
11. Lin EP, Ekholm S, Hiwatashi A, et al. Vertebroplasty: cement leakage into the
The incidence of vacuum clefts in the compression fracture at disc increases the risk of new fracture of adjacent vertebral body. AJNR Am J
the thoracolumbar junction is high (74%). This study showed Neuroradiol 2004;25:175 80
AJNR Am J Neuroradiol 28:1042 45 Jun-Jul 2007 www.ajnr.org 1045
You might also like
- Dai 2001Document5 pagesDai 2001Sri MahadhanaNo ratings yet
- Schick2006 Treatment PDFDocument7 pagesSchick2006 Treatment PDFRifqi FNo ratings yet
- OTA Highlight Paper Predicting Future Displacement of Nonoperatively Managed Lateral Compression Sacral Fractures - Can It Be DoneDocument6 pagesOTA Highlight Paper Predicting Future Displacement of Nonoperatively Managed Lateral Compression Sacral Fractures - Can It Be Doneakb601No ratings yet
- Spinal Epidural Cavernous Hemangiomas in The 2024 International Journal of SDocument3 pagesSpinal Epidural Cavernous Hemangiomas in The 2024 International Journal of SRonald QuezadaNo ratings yet
- Dickman Classification (1996)Document7 pagesDickman Classification (1996)João Pedro ZenattoNo ratings yet
- Fractures of The Scapular Neck: Diagnosis, Classifications and TreatmentDocument11 pagesFractures of The Scapular Neck: Diagnosis, Classifications and Treatmentsoheil ostovanNo ratings yet
- Posterior Lumbar Interbody Fusion (PLIF) With Cages and Local Bone Graft in The Treatment of Spinal StenosisDocument7 pagesPosterior Lumbar Interbody Fusion (PLIF) With Cages and Local Bone Graft in The Treatment of Spinal StenosisMd.Shafiul EzazNo ratings yet
- The Use of A Transolecranon Pin in The Treatment of Flexion-Type SCFsDocument6 pagesThe Use of A Transolecranon Pin in The Treatment of Flexion-Type SCFsBariša KiršnerNo ratings yet
- Fuchs 2005Document5 pagesFuchs 2005BudhiNo ratings yet
- 264 2014 Article 2282Document4 pages264 2014 Article 2282fm123165464No ratings yet
- J Neurol Sci (Turk)Document9 pagesJ Neurol Sci (Turk)nulaeli Siti ANo ratings yet
- Endoscopic Resection of Symptomatic Osteochondroma of The Distal FemurDocument4 pagesEndoscopic Resection of Symptomatic Osteochondroma of The Distal FemurAlex CirlanNo ratings yet
- Foramen Huschke PatologicoDocument7 pagesForamen Huschke PatologicoLM AdrianneNo ratings yet
- Tur CicaDocument8 pagesTur CicazubayetarkoNo ratings yet
- Intramedullary K-Wire Fixation of Metacarpal Fractures: Georg Kelsch Christoph UlrichDocument4 pagesIntramedullary K-Wire Fixation of Metacarpal Fractures: Georg Kelsch Christoph UlrichVolcNo ratings yet
- Spinous Process Fractures in Osteoporotic Thoracolumbar Vertebral FracturesDocument4 pagesSpinous Process Fractures in Osteoporotic Thoracolumbar Vertebral FracturesAditya Arya PutraNo ratings yet
- Percutaneous Endoscopic Decompression Via Transforaminal Approach For Lumbar Lateral Recess Stenosis in Geriatric PatientsDocument7 pagesPercutaneous Endoscopic Decompression Via Transforaminal Approach For Lumbar Lateral Recess Stenosis in Geriatric PatientsAmina GoharyNo ratings yet
- Hip Arthroplasty in Failed Intertrochanteric Fract 103652Document6 pagesHip Arthroplasty in Failed Intertrochanteric Fract 103652seatrrtleNo ratings yet
- 5-Level Spondylectomy For en Bloc Resection of Thoracic Chordoma: Case ReportDocument9 pages5-Level Spondylectomy For en Bloc Resection of Thoracic Chordoma: Case Reportholt linNo ratings yet
- Free Hand Pedicle Screw Placement in The Thoracic KIM LENKE 2004 Spine PDFDocument10 pagesFree Hand Pedicle Screw Placement in The Thoracic KIM LENKE 2004 Spine PDFOlgerAlarconCasanovaNo ratings yet
- PCL Avulsion Fracture 2Document2 pagesPCL Avulsion Fracture 2harpreet singhNo ratings yet
- Variability in Olecranon Ao Fracture Fixation: A Radiological StudyDocument6 pagesVariability in Olecranon Ao Fracture Fixation: A Radiological StudyFhietry Idrus ScaftweeNo ratings yet
- Ganesh 2011Document5 pagesGanesh 2011Giang Nguyễn NgânNo ratings yet
- Paper 38Document6 pagesPaper 38Dr Vineet KumarNo ratings yet
- Phillips 2013Document6 pagesPhillips 2013thanawatsimaNo ratings yet
- Songcharoen 1995Document5 pagesSongcharoen 1995Le Manh ThuongNo ratings yet
- Nakamichi 1997Document10 pagesNakamichi 1997miguelNo ratings yet
- Art3a10 10072fs00256-014-1842-5Document9 pagesArt3a10 10072fs00256-014-1842-5api-253958760No ratings yet
- Süleyman Alp Çölbe Mert Çiftdemir Fethi Emre Ustabaşıoğlu Cihan ÖzgürDocument10 pagesSüleyman Alp Çölbe Mert Çiftdemir Fethi Emre Ustabaşıoğlu Cihan Özgüraymanelhoudali6911No ratings yet
- Short Versus Long Outcome RadiologisDocument7 pagesShort Versus Long Outcome Radiologisandy ardiansyahNo ratings yet
- Fluoroscopic Analysis of The Kinematics of Deep Exion in Total Knee ArthroplastyDocument4 pagesFluoroscopic Analysis of The Kinematics of Deep Exion in Total Knee Arthroplastyjmhinos4833No ratings yet
- 3 Column AnkleDocument8 pages3 Column AnkleJosé Eduardo Fernandez RodriguezNo ratings yet
- Ueki 2007Document7 pagesUeki 2007abhishekjha0082No ratings yet
- Pedicle Screw Fixation in Fracture of Thoraco-Lumbar SpineDocument21 pagesPedicle Screw Fixation in Fracture of Thoraco-Lumbar SpineNiyati SharmaNo ratings yet
- Haglund's Syndrome Schneider2000Document5 pagesHaglund's Syndrome Schneider2000emrahaltuntasNo ratings yet
- iCVTPFDocument5 pagesiCVTPFErwin Chiquete, MD, PhDNo ratings yet
- 1413 7852 Aob 24 03 00159Document5 pages1413 7852 Aob 24 03 00159Rakesh KumarNo ratings yet
- Effects On Inadvertent Endplate Fracture Following Lateral Cage Placement On Range of Motion and Indirect Spine Decompression in Lumbar Spine Fusion Constructs: A Cadaveric StudyDocument8 pagesEffects On Inadvertent Endplate Fracture Following Lateral Cage Placement On Range of Motion and Indirect Spine Decompression in Lumbar Spine Fusion Constructs: A Cadaveric Studysiti hanifahNo ratings yet
- Zygomatic Fractures: Classification and Complications: TveterasDocument7 pagesZygomatic Fractures: Classification and Complications: TveterasBriando Stevano LinelejanNo ratings yet
- Rodilla Inervación Tran2018 PDFDocument8 pagesRodilla Inervación Tran2018 PDFLore BarreraNo ratings yet
- Discrimination of Metastatic From Acute Osteoporotic Compression Spinal Fractures With MRIDocument9 pagesDiscrimination of Metastatic From Acute Osteoporotic Compression Spinal Fractures With MRIChow Tat SingNo ratings yet
- Using The Endoscopic Transconjunctival and Transcaruncular Approach To Repair Combined Orbital Floor and Medial Wall Blowout FracturesDocument4 pagesUsing The Endoscopic Transconjunctival and Transcaruncular Approach To Repair Combined Orbital Floor and Medial Wall Blowout Fracturesstoia_sebiNo ratings yet
- Unstable Burst Fractures of The Thoraco-Lumbar Junction TreatmentDocument8 pagesUnstable Burst Fractures of The Thoraco-Lumbar Junction TreatmentRafael Jardim de MouraNo ratings yet
- Yulisa 2Document7 pagesYulisa 2Ardi WidiatmikaNo ratings yet
- A Long Term Follow Up Study of Total Meniscectomy.30Document5 pagesA Long Term Follow Up Study of Total Meniscectomy.30Anshal GuptaNo ratings yet
- (10920684 - Neurosurgical Focus) Surgical Treatment of Primary Sacral Tumors - Complications Associated With SacrectomyDocument8 pages(10920684 - Neurosurgical Focus) Surgical Treatment of Primary Sacral Tumors - Complications Associated With Sacrectomyfloroiu.ioana.valeriaNo ratings yet
- Anterior Decompression Techniques For Thoracic and Lumbar FracturesDocument10 pagesAnterior Decompression Techniques For Thoracic and Lumbar Fracturesmetasoniko81No ratings yet
- Operative Treatment of Peritrochanteric Osteoporotic Fractures With Proximal Femur Locking Compression Plate A Consecutive StudyDocument6 pagesOperative Treatment of Peritrochanteric Osteoporotic Fractures With Proximal Femur Locking Compression Plate A Consecutive StudyAthenaeum Scientific PublishersNo ratings yet
- Relación Flujo y Fractura ClinicaDocument5 pagesRelación Flujo y Fractura ClinicaPedro TorresNo ratings yet
- Nasional 3 NIC:KOE Penetrating Cervial Spine Injury ENDocument6 pagesNasional 3 NIC:KOE Penetrating Cervial Spine Injury ENHeru Sutanto KNo ratings yet
- Syndesmotic Screw Removed Verusus Retained: A Comparative Functional AnalysisDocument4 pagesSyndesmotic Screw Removed Verusus Retained: A Comparative Functional AnalysisSarath KumarNo ratings yet
- Core Decompression With Bone Grafting For Osteonecrosis of The Femoral HeadDocument8 pagesCore Decompression With Bone Grafting For Osteonecrosis of The Femoral Headmuhammad0umar-4No ratings yet
- Clinical Outcome of A Precontoured Symphysis Pubis Plate With Tension Band Wiring For Traumatic Symphysis Pubis Rupture in Pelvic FracturesDocument6 pagesClinical Outcome of A Precontoured Symphysis Pubis Plate With Tension Band Wiring For Traumatic Symphysis Pubis Rupture in Pelvic FracturesodyNo ratings yet
- Surgical Management of Sacral Chordomas - Illustrative Cases and Current Management ParadigmsDocument7 pagesSurgical Management of Sacral Chordomas - Illustrative Cases and Current Management ParadigmsHugo JBNo ratings yet
- Treatment of Distal Humerus FracturedDocument10 pagesTreatment of Distal Humerus Fracturedauliya ningsihNo ratings yet
- Ojo 2013112116194629 PDFDocument5 pagesOjo 2013112116194629 PDFYash SharmaNo ratings yet
- "A To P" Screw Versus Posterolateral Plate For PosteriorDocument6 pages"A To P" Screw Versus Posterolateral Plate For PosteriorErlin EsauNo ratings yet
- (10920684 - Neurosurgical Focus) Percutaneous Pedicle Screw Fixation of The Lumbar SpineDocument9 pages(10920684 - Neurosurgical Focus) Percutaneous Pedicle Screw Fixation of The Lumbar Spineefancoolhand09No ratings yet
- Giacalone 2015Document7 pagesGiacalone 2015Joseval FilhoNo ratings yet
- Surgery of the Cranio-Vertebral JunctionFrom EverandSurgery of the Cranio-Vertebral JunctionEnrico TessitoreNo ratings yet
- 586 2009 Article 1037Document7 pages586 2009 Article 1037Ramy ElmasryNo ratings yet
- Versus Overall Sagittal AlignmentDocument7 pagesVersus Overall Sagittal AlignmentRamy ElmasryNo ratings yet
- Spontaneous Height Restoration of Vertebral Compression FractureDocument4 pagesSpontaneous Height Restoration of Vertebral Compression FractureRamy ElmasryNo ratings yet
- Pediatrics With Answers and ExplanationsDocument77 pagesPediatrics With Answers and ExplanationsRamy Elmasry100% (6)
- Significance of Dynamic Mobility in Restoring Vertebral Body Height in VertebroplastyDocument4 pagesSignificance of Dynamic Mobility in Restoring Vertebral Body Height in VertebroplastyRamy ElmasryNo ratings yet
- 16-Zhou Et AlDocument6 pages16-Zhou Et AlRamy ElmasryNo ratings yet
- 86 D 8Document7 pages86 D 8Ramy ElmasryNo ratings yet
- Leakage of Cement in Percutaneous Transpedicular Vertebroplasty For Painful Osteoporotic Compression FracturesDocument7 pagesLeakage of Cement in Percutaneous Transpedicular Vertebroplasty For Painful Osteoporotic Compression FracturesRamy ElmasryNo ratings yet
- MainDocument8 pagesMainRamy ElmasryNo ratings yet
- Acute Osteoporotic Vertebral Collapse: Open Study On Percutaneous Injection of Acrylic Surgical Cement in 20 PatientsDocument6 pagesAcute Osteoporotic Vertebral Collapse: Open Study On Percutaneous Injection of Acrylic Surgical Cement in 20 PatientsRamy ElmasryNo ratings yet
- Percutaneous Vertebroplasty and Balloon Kyphoplasty For The Treatment of Osteoporotic Vertebral Compression Fractures and Osteolytic TumoursDocument10 pagesPercutaneous Vertebroplasty and Balloon Kyphoplasty For The Treatment of Osteoporotic Vertebral Compression Fractures and Osteolytic TumoursRamy ElmasryNo ratings yet
- Morning Endorsements: MAY 15-16, 2019 Coc: Dr. Arriola Rod: Dr. Oyas Iod: Co & DickinaDocument11 pagesMorning Endorsements: MAY 15-16, 2019 Coc: Dr. Arriola Rod: Dr. Oyas Iod: Co & DickinaNeil Victor Ongco PajugotNo ratings yet
- Surgical Management in LeprosyDocument33 pagesSurgical Management in Leprosynsv.epicNo ratings yet
- Brochure of ICE SHAPING IV PRODocument15 pagesBrochure of ICE SHAPING IV PROUniforrmes ArcoirisNo ratings yet
- Perioperative Care For CABG PatientsDocument32 pagesPerioperative Care For CABG PatientsAya EyadNo ratings yet
- HIATAL HERNIA PPT Final PDFDocument49 pagesHIATAL HERNIA PPT Final PDFregysujit60% (5)
- Instruments of Throat: Sparsh Goel 77Document19 pagesInstruments of Throat: Sparsh Goel 77Sparsh GoelNo ratings yet
- Hernia QuestionsDocument6 pagesHernia QuestionsNica Lopez Fernandez100% (1)
- LAPORAN TUTORIAL SKENARIO 5 B.3-DikompresiDocument30 pagesLAPORAN TUTORIAL SKENARIO 5 B.3-DikompresiKrishna Dava Putra SNo ratings yet
- Frozen Shoulder - Adhesive CapsulitisDocument8 pagesFrozen Shoulder - Adhesive CapsulitisfriskaNo ratings yet
- Product Catalog Bauerfeind Usa 0312Document88 pagesProduct Catalog Bauerfeind Usa 0312Guillermo Carpio FloriaNo ratings yet
- Atls Pre Test 1 PDFDocument72 pagesAtls Pre Test 1 PDFmary011danielNo ratings yet
- Intestinal Ostomy: Classification, Indications, Ostomy Care and Complication ManagementDocument8 pagesIntestinal Ostomy: Classification, Indications, Ostomy Care and Complication ManagementEriekafebriayana RNo ratings yet
- BD-11097 UltraCor BrochureDocument3 pagesBD-11097 UltraCor Brochurepo leongNo ratings yet
- 6.6) Diagnostic and Therapeutic Abdominal Paracentesis - UpToDateDocument18 pages6.6) Diagnostic and Therapeutic Abdominal Paracentesis - UpToDatefedericoNo ratings yet
- Arn Report List 20200505Document305 pagesArn Report List 20200505zoheir salmaniNo ratings yet
- PTBD 2Document4 pagesPTBD 2Alcntara AllenNo ratings yet
- ORDocument4 pagesORJoana Marie A. LaoNo ratings yet
- Spiritual Needs of A Patient With Acute IllnessDocument3 pagesSpiritual Needs of A Patient With Acute IllnessMarimiel PagulayanNo ratings yet
- V3 WEREWOLF Tech Bro Flo 0720Document6 pagesV3 WEREWOLF Tech Bro Flo 0720hongyuan xuNo ratings yet
- Laparoscopic Cholecystectomy Perioperative Management: An UpdateDocument5 pagesLaparoscopic Cholecystectomy Perioperative Management: An UpdateNurlailah AliNo ratings yet
- Pearls Nov Dec 2010Document3 pagesPearls Nov Dec 2010Nhật LongNo ratings yet
- Laser Technolas 217 - Excimer Laser SystemDocument34 pagesLaser Technolas 217 - Excimer Laser Systemrubens.nascimento213No ratings yet
- Cone-Beam Computed Tomography and Its Applications in DentistryDocument4 pagesCone-Beam Computed Tomography and Its Applications in DentistryMeris JugadorNo ratings yet
- Karnatka 2023Document3 pagesKarnatka 2023bvkarthik.99No ratings yet
- Appleby OperationDocument9 pagesAppleby OperationPeter Paul PascualNo ratings yet
- Helland L Nursing ChecklistDocument6 pagesHelland L Nursing Checklistapi-703155063No ratings yet
- Complications of The Arteriovenous Fistula: A Systematic ReviewDocument45 pagesComplications of The Arteriovenous Fistula: A Systematic ReviewAnonymous ATdLPZNo ratings yet
- Hernia 1Document28 pagesHernia 1Aminatulhuda SulaimanNo ratings yet
- យល់ដឹងអំពីតួនាទីរបស់ខ្នែងពោះវៀនDocument4 pagesយល់ដឹងអំពីតួនាទីរបស់ខ្នែងពោះវៀនReal Madrid FCNo ratings yet
- Intra Operative Allowable Blood Loss: Estimation Made Easy: Original Research ArticleDocument5 pagesIntra Operative Allowable Blood Loss: Estimation Made Easy: Original Research ArticlesafwanNo ratings yet