Professional Documents
Culture Documents
0 ratings0% found this document useful (0 votes)
13 viewsUnit 3 Physiology Leff Control of Growth and Body Mass-1
Unit 3 Physiology Leff Control of Growth and Body Mass-1
Uploaded by
Abhineeth BhatGrowth Hormone
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5823)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (852)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (898)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (541)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (349)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (823)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (403)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Book Good Calories Bad Calories by Gary TaubesDocument3 pagesBook Good Calories Bad Calories by Gary TaubesMelissa0% (2)
- Urinary Concentration and DilutionDocument10 pagesUrinary Concentration and DilutionAbhineeth BhatNo ratings yet
- STEP1 ResourcesDocument2 pagesSTEP1 ResourcesAbhineeth BhatNo ratings yet
- Guide To BoardsDocument3 pagesGuide To BoardsAbhineeth BhatNo ratings yet
- Approved: HFHS Nov-June Only HFH Has No PrerequisitesDocument1 pageApproved: HFHS Nov-June Only HFH Has No PrerequisitesAbhineeth BhatNo ratings yet
- Pharm - Endocrine - Anti-DiabeticsDocument1 pagePharm - Endocrine - Anti-DiabeticsAbhineeth BhatNo ratings yet
- Pathophys - Endocrine - LipoproteinsDocument4 pagesPathophys - Endocrine - LipoproteinsAbhineeth BhatNo ratings yet
- Question PhilosophyDocument3 pagesQuestion PhilosophyAbhineeth BhatNo ratings yet
- Gi HyDocument2 pagesGi HyAbhineeth BhatNo ratings yet
- Aging and MenopauseDocument3 pagesAging and MenopauseAbhineeth BhatNo ratings yet
- CLA SuplementoDocument40 pagesCLA SuplementoÓscar HurtadoNo ratings yet
- Green Coffee Bean Extract As A Weight Loss Supplement 2161 0509 1000180 PDFDocument3 pagesGreen Coffee Bean Extract As A Weight Loss Supplement 2161 0509 1000180 PDFdorathiNo ratings yet
- Equine Metabolic SyndromeDocument7 pagesEquine Metabolic SyndromeSebastianSierraNo ratings yet
- Spesial Untuk Member Baru: Body Fat CalculatorDocument1 pageSpesial Untuk Member Baru: Body Fat CalculatorSiska Syadiatul ZanahNo ratings yet
- Compensatory Growth in The Broiler Chicken: Review: A.K. Zubair S. LeesonDocument13 pagesCompensatory Growth in The Broiler Chicken: Review: A.K. Zubair S. LeesonHassan AL-HillaliNo ratings yet
- Insulin, Glucagon, and Diabetes MellitusDocument22 pagesInsulin, Glucagon, and Diabetes Mellitusghadeer1No ratings yet
- Geriatric NutritionDocument45 pagesGeriatric Nutritionveena viswanathan100% (2)
- How It Works Book of The Human Body 6th EditionDocument180 pagesHow It Works Book of The Human Body 6th Editionthoma71% (7)
- Obesity AND The Metabolic Syndrome: BY DR Anyamele IbuchimDocument49 pagesObesity AND The Metabolic Syndrome: BY DR Anyamele IbuchimPrincewill SmithNo ratings yet
- Feed Your Brain, Lose Your Belly A Brain Surgeon Reveals The Weight-Loss Secrets of The Brain-Belly Conne PDFDocument147 pagesFeed Your Brain, Lose Your Belly A Brain Surgeon Reveals The Weight-Loss Secrets of The Brain-Belly Conne PDFBineke100% (2)
- Acute Response of Serum Leptin To Short Single Bout Exercise in Patients With Moderate AsthmaDocument8 pagesAcute Response of Serum Leptin To Short Single Bout Exercise in Patients With Moderate AsthmaOpenaccess Research paperNo ratings yet
- Important Information About Low Carb, Cortisol and GlucoseDocument12 pagesImportant Information About Low Carb, Cortisol and GlucoseCarlos RodriguezNo ratings yet
- The Anatomy and Physiology of The HorseDocument383 pagesThe Anatomy and Physiology of The HorseserjutoNo ratings yet
- TESTOFEN Published Australian StudyDocument7 pagesTESTOFEN Published Australian StudyWilliam E. Saucer IINo ratings yet
- Serum Interleukin-1beta and Lipid Profile Responses To Aerobic Training in Obese MenDocument7 pagesSerum Interleukin-1beta and Lipid Profile Responses To Aerobic Training in Obese MenOpenaccess Research paperNo ratings yet
- The Bidirectional Relationship Between Obstructive Sleep Apnea and Metabolic DiseaseDocument14 pagesThe Bidirectional Relationship Between Obstructive Sleep Apnea and Metabolic DiseaseVenny SarumpaetNo ratings yet
- Updated Pe 104 Course Design 2ND Sem 2022-2023-1Document53 pagesUpdated Pe 104 Course Design 2ND Sem 2022-2023-1Gadez JeanpelNo ratings yet
- 6 Essential NutrientsDocument133 pages6 Essential NutrientsLouisa Marie MirandaNo ratings yet
- JPM 13 00098Document15 pagesJPM 13 00098Maria Júlia ProtiNo ratings yet
- User ManualDocument31 pagesUser ManualDiane MNo ratings yet
- Final Third Quarter Exam in Pe 12-1Document5 pagesFinal Third Quarter Exam in Pe 12-1deomalyn.canalNo ratings yet
- Obesity: Term Paper OnDocument13 pagesObesity: Term Paper OnNur AthirahNo ratings yet
- Featuring Christian Thibaudeau, Lonnie Lowery, PHD, David Barr, and Dr. John BerardiDocument17 pagesFeaturing Christian Thibaudeau, Lonnie Lowery, PHD, David Barr, and Dr. John Berardiogre600100% (1)
- Obesity Inflammation and Endothelial DysDocument8 pagesObesity Inflammation and Endothelial DysgoldNo ratings yet
- Pharmacology of The Endocrine SystemDocument74 pagesPharmacology of The Endocrine SystemarpanabiswassshetyeNo ratings yet
- Effects of Guanidinoacetic Acid Supplementation in Broiler Chicken Diet On Carcass CharacteristicsDocument8 pagesEffects of Guanidinoacetic Acid Supplementation in Broiler Chicken Diet On Carcass CharacteristicsIJAR JOURNALNo ratings yet
- Arthritis of The Knee 2017 MASUDDocument139 pagesArthritis of The Knee 2017 MASUDMario IličićNo ratings yet
- Body FatDocument5 pagesBody FatPaulo CameloNo ratings yet
- Textbook Obesity and Lipotoxicity 1St Edition Ayse Basak Engin Ebook All Chapter PDFDocument53 pagesTextbook Obesity and Lipotoxicity 1St Edition Ayse Basak Engin Ebook All Chapter PDFkenneth.whittaker355100% (5)
Unit 3 Physiology Leff Control of Growth and Body Mass-1
Unit 3 Physiology Leff Control of Growth and Body Mass-1
Uploaded by
Abhineeth Bhat0 ratings0% found this document useful (0 votes)
13 views4 pagesGrowth Hormone
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentGrowth Hormone
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Download as docx, pdf, or txt
0 ratings0% found this document useful (0 votes)
13 views4 pagesUnit 3 Physiology Leff Control of Growth and Body Mass-1
Unit 3 Physiology Leff Control of Growth and Body Mass-1
Uploaded by
Abhineeth BhatGrowth Hormone
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Download as docx, pdf, or txt
You are on page 1of 4
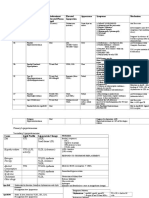
Unit 3 Physiology: Control of Growth and Body Mass (Leff)
HUMAN GROWTH HORMONE:
Structure:
- 2 forms of GH that result from differential splicing
o 20 kDa (176 AA) GH and 22 KDa (191 AA) GH
o Difference is 14 amino acids
o Not clear what the difference is between the 2
Gene Expression:
- GH is part of a gene cluster of closely related genes on cs17
- Gene encodes:
o Human GH (191 AA)
o pvGH (191 AA, 93% homologous with hGH)
Thought to be a major regulator of fetal growth (GH itself does NOT control
fetal growth; GH levels are actually low during fetal development)
Has same affinity for GH receptor as GH itself
o Human CS1 and CS2 (191 AA each, 84% homologous)
Human chorionic somatomammotropin
Relevant only in embryonic development
Produced by the placenta
o Human PRL (199 AA, 16% homologous)
Synthesis:
- Gene is differentially spliced, resulting in the pre-22 kDa or pre-20 kDa growth hormone
mRNA (in the nucleus)
- Enters RER where it is transcribed to the pre-pro-hormone, and is then transported to the
Golgi where it is converted to the pro-hormone
- Eventually stored in secretory granules in the somatotrophic cells of the anterior
pituitary, awaiting signal to be released
Episodic Production:
- Higher GH levels exist at night during non-REM stages of sleep
o Earlier in the night
o Slow wave/deep sleep
- This is used in treatment as therapeutic GH is administered at night when endogenous GH
is normally produced
Factors Affecting GH Production:
- Increase GH Production:
o Fasting (hypoglycemia, low circulating free FAs)
o High protein diet (elevated circulating AA)
o Exercise (obviously not mediating growth here, but serves a function)
o Deep sleep (non-REM sleep)
- Decrease GH Production:
o Stress/Anxiety (causes release of glucocorticoids which suppresses downstream GH
effects; does not affect GH production)
Direct (Acute) Effects of GH:
- These effects are mainly diabetogenic (ant-insulin effects); do not commonly play a role in
normal individuals
- Short-term effects (minutes to hours)
- Effects:
o Increases glucose uptake in muscle
o Increases lipolysis in fat
o Increases gluconeogenesis in liver
o Causes insulin resistance muscle, fat and liver
- GH itself does NOT have growth promoting activity
Indirect Effects of GH Mediated by IGF-1:
- The primary mediatory of growth-promoting effects of GH is IGF-1 (produced in the liver
when stimulated by GH)
- Causes chronic effects of GH, which are all related to growth:
o Increased DNA, RNA and protein synthesis
o Increase in cell size and number
o Increase in organ size
o Increase in organ function
o Increase in linear growth (has a direct effect on osteoblasts, causing bone building
process to be favored)
Cell Signaling Pathway:
- Growth hormone receptor is a JAK/STAT receptor
- Growth hormone binds to a pair of receptors, causes dimerization and autophoshorylation
of the receptor occurs
- This autophosphorylation leads to phosphorylation of janus kinases associated with the
receptor
- STATs bind to the phsophorylated receptor, and become phosphorylated by the janus
kinases
- Phosphorylated STATs move to the nucleus to act as transcription factors and modulate
gene expression
o Increase expression of IGF-1 and IGFBPs
IGF-1 (SOMATOMEDIN):
Structure:
- Highly homologous with insulin
o In lower animals, only have one hormone that carries out activities of IGF-1 and
insulin
o C peptide in IGF-1 is shorter and is NOT cleaved out of the IGF-1 gene product
- There also exists an IGF-2 molecule
o Function is not totally clear
o May be limited to specific periods of growth
IGF-1 Receptor:
- Very similar structure to the insulin receptor (also a tyrosine kinase)
- Has similar signaling to the insulin pathway
o At very high concentrations of insulin (ie. in severe hyperinsulinemia associated
with type II diabetes), insulin can bind IGF-1 receptor causing undesirable effects
- IGF-2 receptor has also been characterized
o Mannose-6-phosphate receptor
o Does not induce cell signaling inside the cell
o IGF-2 can also bind the IGF-1 receptor in some circumstances
IGF-1 and Growth:
- Most rapid growth occurs in early childhood, but is not mediated by IGF-1 (what does
mediate this growth is unclear; might be IGF-2, placental lactogens etc.)
- IGF-1 primarily mediates pubertal body growth
o IGF-1 levels increase during childhood and peak at puberty
REGULATION OF GH SECRETION AND FEEDBACK:
Secretion:
- Cells in the arcuate nucleus secrete GHRH (stimulate GH release)
o Causes fusion and release of GH by somatotrophs
GHRH binds GHRH receptor (Gs coupled receptor) which activates
adenylate cyclase, increasing cAMP and PKA, causing Ca++ influx
o Circadian rhythm plays a role in GHRH production (increasing GH secretion during
the night)
- Cells in periventricular region release somatostatin (inhibit GH release)
o Somatostatin binds somatostatin receptor (Gi coupled receptor) which inactivates
adenylate cyclase , decreasing cAMP and PKA (prevent Ca++ influx into cell,
therefore preventing docking and fusion of GH vesicles)
Feedback:
- GH Feedback:
o Feeds back to inhibit somatotrophs in anterior pituitary, therefore inhibiting GH
release
o GH is removed rapidly from circulation
- IGF-1 Feedback:
o Feeds back to inhibit somatotrophs in anterior pituitary, therefore inhibiting GH
release
o Feeds back to inhibit GHRH secretion fro arcuate nucleus
o Feeds back to stimulate somatostatin release (inhibit GH release)
o IGF-1 has a longer half life in circulation than GH
OTHER HORMONES THAT AFFECT BODY GROWTH:
- Thyroid hormone
- Sex steroids
- Glucocorticoids
- Insulin
- Tissue and cell-specific growth factors promote growth (have hormone like effects):
o Nerve growth factor (NGF)
o Fibroblast growth factor (FGF)
o Angiogenesis factor
o Vascular endothelial growth factor (VEGF; repairs vascular endothelium)
o Epidermal growth factor (EGF)
o Hepatocyte growth factor (HGF)
ABNORMALITIES IN GROWTH HORMONE:
GH Excess: caused by tumor of somatotrophs in anterior pituitary (usually treatable)
- Causes:
o Hyperglycemia
o Insulin resistance
o Reduced body fat/increased lean body mass
o Acromegaly in adults (epiphyseal plates have been fused)
o Gigantism in kids (followed by acromegaly later in life)
GH Deficiency:
- Causes:
o Short stature
o Hypoglycemia
o Increased body fat
o Reduced lean body mass (muscle mass)
- Laron Dwarfism: mutation in the receptor for GH (cannot induce production of IGF-1)
LEPTIN AND THE CONTROL OF BODY MASS:
Discovery:
- 2 genes, the when defective, cause obesity: Ob gene and Db gene
- Experiments performed in mice:
o Ob defective mouse attached to normal mouse
Ob mouse became slender, normal mouse remained normal
Therefore, Ob mouse must have a defective hormone that normally
reduces body weight (because it became slender after being able to
receive the normal mouses hormone)
o Db defective mouse attached to normal mouse
Db mouse remained fat, normal mouse became anorexic
Therefore, Db mouse must have a defective receptor for the normal
hormone that reduces body weight (because it remained fat even after
receiving hormone from the normal mouse)
It also must have normal functioning hormone since the normal mouse
became anorexic (received extra weight reducing hormone from the Db
mouse)
Physiological Effects of Leptin:
- Leptin affects appetite (reduces appetite)
- Does NOT affect metabolic processes (receptors for leptin are in the CNS)
- Giving leptin to Ob mouse (with defective hormone) decreased food intake dramatically
- Giving leptin to the Db mouse (with the defective receptor) had no effect on food intake
Hormonal Regulation of Appetite:
- Leptin is secreted at all times from all adipose tissue in the body
o Amount of leptin produced is proportional to the amount of body fat a person has
- Leptin is only secreted by adipose tissue
o Gene for leptin is expressed only in adipose tissue
- Receptors for leptin are located in the arcuate nucleus of the hypothalamus on 2
populations of neurons
o Anorexogenic neurons (POMC/CART, decrease appetite)
o Orexigenic neurons (AGRP/NPY, increase appetite)
- Leptin stimulates anorexigenic neurons and inhibits orexigenic neurons
- Other Hormones Playing a Role: Ghrelin and CCK (released from the gut)
- Clinical Use of Leptin:
o Leptin is only effective at decreasing appetite and body weight in people that have
a defect in the leptin gene (very rare)
o Obese individuals actually have more leptin than normal sized individuals
Thought is that hyperleptinemia leads to leptin resistance in a similar
fashion to hyperinsulinemia causing insulin resistance in diabetes
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5823)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (852)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (898)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (541)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (349)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (823)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (403)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Book Good Calories Bad Calories by Gary TaubesDocument3 pagesBook Good Calories Bad Calories by Gary TaubesMelissa0% (2)
- Urinary Concentration and DilutionDocument10 pagesUrinary Concentration and DilutionAbhineeth BhatNo ratings yet
- STEP1 ResourcesDocument2 pagesSTEP1 ResourcesAbhineeth BhatNo ratings yet
- Guide To BoardsDocument3 pagesGuide To BoardsAbhineeth BhatNo ratings yet
- Approved: HFHS Nov-June Only HFH Has No PrerequisitesDocument1 pageApproved: HFHS Nov-June Only HFH Has No PrerequisitesAbhineeth BhatNo ratings yet
- Pharm - Endocrine - Anti-DiabeticsDocument1 pagePharm - Endocrine - Anti-DiabeticsAbhineeth BhatNo ratings yet
- Pathophys - Endocrine - LipoproteinsDocument4 pagesPathophys - Endocrine - LipoproteinsAbhineeth BhatNo ratings yet
- Question PhilosophyDocument3 pagesQuestion PhilosophyAbhineeth BhatNo ratings yet
- Gi HyDocument2 pagesGi HyAbhineeth BhatNo ratings yet
- Aging and MenopauseDocument3 pagesAging and MenopauseAbhineeth BhatNo ratings yet
- CLA SuplementoDocument40 pagesCLA SuplementoÓscar HurtadoNo ratings yet
- Green Coffee Bean Extract As A Weight Loss Supplement 2161 0509 1000180 PDFDocument3 pagesGreen Coffee Bean Extract As A Weight Loss Supplement 2161 0509 1000180 PDFdorathiNo ratings yet
- Equine Metabolic SyndromeDocument7 pagesEquine Metabolic SyndromeSebastianSierraNo ratings yet
- Spesial Untuk Member Baru: Body Fat CalculatorDocument1 pageSpesial Untuk Member Baru: Body Fat CalculatorSiska Syadiatul ZanahNo ratings yet
- Compensatory Growth in The Broiler Chicken: Review: A.K. Zubair S. LeesonDocument13 pagesCompensatory Growth in The Broiler Chicken: Review: A.K. Zubair S. LeesonHassan AL-HillaliNo ratings yet
- Insulin, Glucagon, and Diabetes MellitusDocument22 pagesInsulin, Glucagon, and Diabetes Mellitusghadeer1No ratings yet
- Geriatric NutritionDocument45 pagesGeriatric Nutritionveena viswanathan100% (2)
- How It Works Book of The Human Body 6th EditionDocument180 pagesHow It Works Book of The Human Body 6th Editionthoma71% (7)
- Obesity AND The Metabolic Syndrome: BY DR Anyamele IbuchimDocument49 pagesObesity AND The Metabolic Syndrome: BY DR Anyamele IbuchimPrincewill SmithNo ratings yet
- Feed Your Brain, Lose Your Belly A Brain Surgeon Reveals The Weight-Loss Secrets of The Brain-Belly Conne PDFDocument147 pagesFeed Your Brain, Lose Your Belly A Brain Surgeon Reveals The Weight-Loss Secrets of The Brain-Belly Conne PDFBineke100% (2)
- Acute Response of Serum Leptin To Short Single Bout Exercise in Patients With Moderate AsthmaDocument8 pagesAcute Response of Serum Leptin To Short Single Bout Exercise in Patients With Moderate AsthmaOpenaccess Research paperNo ratings yet
- Important Information About Low Carb, Cortisol and GlucoseDocument12 pagesImportant Information About Low Carb, Cortisol and GlucoseCarlos RodriguezNo ratings yet
- The Anatomy and Physiology of The HorseDocument383 pagesThe Anatomy and Physiology of The HorseserjutoNo ratings yet
- TESTOFEN Published Australian StudyDocument7 pagesTESTOFEN Published Australian StudyWilliam E. Saucer IINo ratings yet
- Serum Interleukin-1beta and Lipid Profile Responses To Aerobic Training in Obese MenDocument7 pagesSerum Interleukin-1beta and Lipid Profile Responses To Aerobic Training in Obese MenOpenaccess Research paperNo ratings yet
- The Bidirectional Relationship Between Obstructive Sleep Apnea and Metabolic DiseaseDocument14 pagesThe Bidirectional Relationship Between Obstructive Sleep Apnea and Metabolic DiseaseVenny SarumpaetNo ratings yet
- Updated Pe 104 Course Design 2ND Sem 2022-2023-1Document53 pagesUpdated Pe 104 Course Design 2ND Sem 2022-2023-1Gadez JeanpelNo ratings yet
- 6 Essential NutrientsDocument133 pages6 Essential NutrientsLouisa Marie MirandaNo ratings yet
- JPM 13 00098Document15 pagesJPM 13 00098Maria Júlia ProtiNo ratings yet
- User ManualDocument31 pagesUser ManualDiane MNo ratings yet
- Final Third Quarter Exam in Pe 12-1Document5 pagesFinal Third Quarter Exam in Pe 12-1deomalyn.canalNo ratings yet
- Obesity: Term Paper OnDocument13 pagesObesity: Term Paper OnNur AthirahNo ratings yet
- Featuring Christian Thibaudeau, Lonnie Lowery, PHD, David Barr, and Dr. John BerardiDocument17 pagesFeaturing Christian Thibaudeau, Lonnie Lowery, PHD, David Barr, and Dr. John Berardiogre600100% (1)
- Obesity Inflammation and Endothelial DysDocument8 pagesObesity Inflammation and Endothelial DysgoldNo ratings yet
- Pharmacology of The Endocrine SystemDocument74 pagesPharmacology of The Endocrine SystemarpanabiswassshetyeNo ratings yet
- Effects of Guanidinoacetic Acid Supplementation in Broiler Chicken Diet On Carcass CharacteristicsDocument8 pagesEffects of Guanidinoacetic Acid Supplementation in Broiler Chicken Diet On Carcass CharacteristicsIJAR JOURNALNo ratings yet
- Arthritis of The Knee 2017 MASUDDocument139 pagesArthritis of The Knee 2017 MASUDMario IličićNo ratings yet
- Body FatDocument5 pagesBody FatPaulo CameloNo ratings yet
- Textbook Obesity and Lipotoxicity 1St Edition Ayse Basak Engin Ebook All Chapter PDFDocument53 pagesTextbook Obesity and Lipotoxicity 1St Edition Ayse Basak Engin Ebook All Chapter PDFkenneth.whittaker355100% (5)