Professional Documents
Culture Documents
Antibiotic Woman Final 2013
Antibiotic Woman Final 2013
Uploaded by
Fitri RachmadaniCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Antibiotic Woman Final 2013
Antibiotic Woman Final 2013
Uploaded by
Fitri RachmadaniCopyright:
Available Formats
Pregnancy and Post Natal Empirical Treatment of Infection Guidance
THINK SEPSIS IN ALL WOMEN RECENTLY DELIVERED WHO FEEL UNWELL OR HAVE PYREXIA OR HYPOTHERMIA
FULL GUIDANCE IS AVAILABLE IN TAYSIDE AREA FORMULARY SECTION 5 (www.nhstaysideadtc.scot.nhs.uk) or LINK ON STAFFNET HOME PAGE)
TO REDUCE EMERGENCE OF RESISTANCE AND CLOSTRIDIUM DIFFICILE INFECTION USE NARROW SPECTRUM ANTIBIOTICS WHEREVER POSSIBLE LIMIT PRESCRIBING
OVER THE TELEPHONE TO EXCEPTIONAL CIRCUMSTANCES
NORMAL HEPATIC AND RENAL FUNCTION IS ASSUMED AND DELIVERY OF A HEALTHY, FULL TERM INFANT WHERE RELEVANT SEEK ADVICE IF NECESSARY
IF THE PATIENT IS PREGNANT YOU MUST STATE THIS ON ANY MICROBIOLOGY REQUESTS
SURGICAL PROPHYLAXIS Refer to full guidelines on TAF website for obstetric, gynaecological and general surgery procedures
General USE OF MEDICINES IN PREGNANCY AND BREASTFEEDING:
If in doubt always check BNF, contact your ward or locality pharmacist, or Medicines Information, for clarification before
Points prescribing.
*Co-trimoxazole - If breastfeeding monitor baby for hyperbilirubinaemia and kernicerterus. If baby premature or already
jaundiced, avoid and seek advice on alternative.
MATERNAL SEPSIS Refer to hospital immediately. Refer to full policy and complete sepsis bundle within 1 hour.
GROUP B STREP Refer to policy
Pregnancy UTI OR ASYMPTOMATIC 1st or 2nd trimester nitrofurantoin MR 100mg bd or 50mg qds. 3rd trimester trimethoprim
BACTERIURIA 200mg bd (unlicensed). 2nd line (any trimester) cefalexin 500mg tds or as per sensitivities.
Vaginal discharge Treat for 7 days and sample for test of cure.
is heavier in
pregnancy swabs
RECURRENT UTI If 2 or more positive MSUs then test 3-4 weekly and treat each positive sample as above
are only indicated
if there is associated
discomfort PYELONEPHRITIS Co-amoxiclav 625mg tds for 14 days or co-amoxiclav IV 1.2g tds
or foul odour (if penicillin allergy PO cefalexin 1g tds or IV ceftriaxone 2g od seek advice in severe allergy)
CHLAMYDIA COMPLETE PARTNER NOTIFICATION CONSENT BOX ON ICE REQUEST PRIOR TO TESTING.
Azithromycin 1g stat (unlicensed) or erythromycin 500mg qds (7 days)
plus test of cure after 6 weeks. Rescreen in 3rd trimester.
THRUSH Clotrimazole 500mg pessary stat + clotrimazole 1% cream 2-3 times daily.
BACTERIAL VAGINOSIS Metronidazole 400mg bd for 5-7 days or clindamycin 2% vaginal cream 5g at night for 7 nights
TRICHOMONIASIS Metronidazole 400mg bd for 5-7 days. Refer to Sexual Health Clinic.
PELVIC INFLAMMATORY DISEASE Requires inpatient IV therapy refer to policy
GENITAL HERPES Aciclovir 200mg 5 times daily for 5 days
If new infection or multiple recurrences refer to Sexual Health Clinic and inform Obstetrician.
SEPSIS SHOULD BE CONSIDERED IN ALL RECENTLY DELIVERED WOMEN WHO FEEL UNWELL OR HAVE PYREXIA
OR HYPOTHERMIA. PATIENTS IN COMMUNITY SHOULD BE URGENTLY REFERRED TO HOSPITAL.
Post- MATERNAL SEPSIS Refer to full policy and complete sepsis bundle within 1 hour
Natal ENDOMETRITIS Co-amoxiclav 625mg tds + metronidazole 400mg tds for 7 days
(If penicillin allergy *co-trimoxazole 960mg bd + metronidazole 400mg tds)
If uterine tenderness or signs of sepsis refer to hospital urgently.
POST CS WOUND INFECTION Flucloxacillin 1g qds + metronidazole 400mg tds OR clindamycin 450mg tds
Adjust according to swab results if necessary
3RD OR 4TH DEGREE Refer to Obs/Gynae surgical prophylaxis guideline for pre-procedure one off IV antibiotics
PERINEAL TEAR followed by co-amoxiclav 625mg tds for 7 days
(In penicillin allergy: *co-trimoxazole 960mg bd + metronidazole 400mg tds)
MASTITIS Ensure complete drainage of breast at each feed by baby +/- expressing. Symptom relief with NSAIDs
and warm compresses can help. Consider antibiotics if symptoms do not improve or are worsening after
12-24 hours. Flucloxacillin 1g qds (or clindamycin 450mg tds if penicillin allergy) for 7-10 days.
Breast BREAST ABSCESS Send pus for culture. Flucloxacillin 1g qds (or clindamycin 450mg tds if penicillin allergy) for 7-10 days.
Feeding Adjust treatment according to culture sensitivity if indicated.
THRUSH Ensure good attachment of baby to the breast, and treat mother and baby simultaneously. For further
management information see NES Medicines and Mothers or The Breastfeeding Network
FOR MOTHER: Miconazole 2% cream (do not use oral gel on mother) applied to nipple and areola after
each feed for 7 days. Gently wipe away any residue before the next feed. If pain is severe or deep within
Developed by: the breasts after feeds systemic treatment may be needed with fluconazole 300mg on day one followed by
Obstetrics/
SHC/AMG
150mg daily for at least 10 days (unlicensed treatment). Review diagnosis if no improvement after 10
days and refer for further breastfeeding assessment.
Approved by FOR INFANT: Over 4 months, miconazole oral gel, 2.5ml applied gently to oral mucosa (to avoid choking) 4
AMG: times a day after feeds (unlicensed dose). Under 4 months, nystatin oral suspension 1ml 4 times a day
Dec 2012
after feeds (unlicensed in neonates)
Review:
Dec 2014 NIPPLE FISSURE Only treat if signs of infection e.g. yellow discharge or crusts around fissures. If isolated use topical fusidic
acid applied sparingly 3 or 4 times daily after feeds, if widespread use antibiotics as for mastitis.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5822)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (852)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (898)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (349)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (823)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (403)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- B777-Engines and APUDocument66 pagesB777-Engines and APUcubare100% (5)
- Servicing Deutsch HD and DT Style Connectors (1408) : Tool Operating ManualDocument16 pagesServicing Deutsch HD and DT Style Connectors (1408) : Tool Operating ManualRajan MullappillyNo ratings yet
- Pitfalls in Haemodynamic Monitoring in The Postoperative and Critical Care SettingDocument6 pagesPitfalls in Haemodynamic Monitoring in The Postoperative and Critical Care SettingFitri RachmadaniNo ratings yet
- The Role of Abdominal X-Rays in The Investigation of Suspected Acute AppendicitisDocument5 pagesThe Role of Abdominal X-Rays in The Investigation of Suspected Acute AppendicitisFitri RachmadaniNo ratings yet
- MaggotsDocument4 pagesMaggotsFitri RachmadaniNo ratings yet
- Kuliah AFDocument44 pagesKuliah AFFitri RachmadaniNo ratings yet
- CNS: Ent:: Review Antibiotic Therapy Daily - Can You: Stop? Switch? Simplify? or State Duration?Document1 pageCNS: Ent:: Review Antibiotic Therapy Daily - Can You: Stop? Switch? Simplify? or State Duration?Fitri RachmadaniNo ratings yet
- CNS: Ent:: Review Antibiotic Therapy Daily - Can You: Stop? Switch? Simplify? or State Duration?Document1 pageCNS: Ent:: Review Antibiotic Therapy Daily - Can You: Stop? Switch? Simplify? or State Duration?Fitri RachmadaniNo ratings yet
- JEduHealthPromot516-2877995 075939Document6 pagesJEduHealthPromot516-2877995 075939Fitri RachmadaniNo ratings yet
- Consumption of Sugar-Sweetened Beverages in Mississippi: Is There A Disparity? Behavioral Risk Factor Surveillance System, 2012Document9 pagesConsumption of Sugar-Sweetened Beverages in Mississippi: Is There A Disparity? Behavioral Risk Factor Surveillance System, 2012Fitri RachmadaniNo ratings yet
- A Comparison Between Premortem and Postmortem Diagnosis in Trauma CasesDocument6 pagesA Comparison Between Premortem and Postmortem Diagnosis in Trauma CasesFitri RachmadaniNo ratings yet
- Kra-4.hiv Sti AidsDocument2 pagesKra-4.hiv Sti AidsGio BitoyNo ratings yet
- Sandvik Cs550 Cone Crusher: Technical SpecificationDocument8 pagesSandvik Cs550 Cone Crusher: Technical SpecificationLmf DanielNo ratings yet
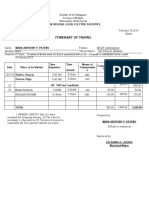
- Iterenary Travel FormDocument3 pagesIterenary Travel Formsplef lguNo ratings yet
- List of Family ValuesDocument9 pagesList of Family ValuesTrisha Anne TorresNo ratings yet
- Lose Weight and Get Fit With No Diet - No Gym - Be Healthier, Stronger, and Live LongerDocument122 pagesLose Weight and Get Fit With No Diet - No Gym - Be Healthier, Stronger, and Live LongerShoaib MohammadNo ratings yet
- Behavioral Studies of Bats in Captivity: Methodology, Training, and Experimental DesignDocument20 pagesBehavioral Studies of Bats in Captivity: Methodology, Training, and Experimental DesignIslam Ausraf RajibNo ratings yet
- Agrobiodiversity in Southeast Europe - Assessment and Policy Recommendations. Country Report SerbiaDocument92 pagesAgrobiodiversity in Southeast Europe - Assessment and Policy Recommendations. Country Report SerbiaSuzanaĐorđević-MiloševićNo ratings yet
- 10.method Statement Piling WorkDocument6 pages10.method Statement Piling Workشاز إياسNo ratings yet
- Avh-Z9280tv - Manual de ServicoDocument248 pagesAvh-Z9280tv - Manual de ServicoFernando Aparecido BaldáviaNo ratings yet
- PMR v26 I4 158 166 PDFDocument9 pagesPMR v26 I4 158 166 PDFemzzNo ratings yet
- Draft For Lifting of Persons in Work Platforms Suspended From CranesDocument25 pagesDraft For Lifting of Persons in Work Platforms Suspended From CranesSharulNo ratings yet
- First DraftDocument83 pagesFirst DraftNicole Cliano0% (1)
- Dsh220 Marenga Counseling Individual AssignmentDocument8 pagesDsh220 Marenga Counseling Individual AssignmentBeauty Indrah MarengaNo ratings yet
- Pilates For Beginners Class 1 Guide Booklet PDFDocument12 pagesPilates For Beginners Class 1 Guide Booklet PDFnakisgio5568No ratings yet
- ProcedureDocument2 pagesProcedureNeni SuryaniNo ratings yet
- 2015 VN Single InverterDocument29 pages2015 VN Single InverterMinhvan LeNo ratings yet
- Container Type Linear Dimensions (Base Width / Overall Width × Depth × Height) RemarksDocument2 pagesContainer Type Linear Dimensions (Base Width / Overall Width × Depth × Height) RemarksBablu JiNo ratings yet
- Visual Inspection SCRATA: Comparators For The Definition of Surface Quality of CastingsDocument2 pagesVisual Inspection SCRATA: Comparators For The Definition of Surface Quality of CastingsMARIO SANDOVAL PAIPAYNo ratings yet
- World Sight Day-Activity Report - 2022-PICO PakistanDocument5 pagesWorld Sight Day-Activity Report - 2022-PICO Pakistanjibran khanNo ratings yet
- List of CseDocument13 pagesList of CseAyni ReyesNo ratings yet
- Julie AncisDocument27 pagesJulie AncisJulie R. AncisNo ratings yet
- For Protein !: Say C HeeseDocument4 pagesFor Protein !: Say C HeeseJuan Sebastian CeleitaNo ratings yet
- Bakery's Open Hiring' Offers Anyone A Chance - New York TimesDocument2 pagesBakery's Open Hiring' Offers Anyone A Chance - New York TimesNavniNo ratings yet
- 13 - Photosynthesis AQA BookletDocument28 pages13 - Photosynthesis AQA BookletSevilay CaferogluNo ratings yet
- ITDI Hand Sanitizer Production 07172020Document27 pagesITDI Hand Sanitizer Production 07172020Marilyn LaquindanumNo ratings yet
- Dal Fry RecipeDocument2 pagesDal Fry RecipejunkyardNo ratings yet
- Bod Procedure 1Document26 pagesBod Procedure 1kuthappadyNo ratings yet
- OPGWDocument64 pagesOPGWfNo ratings yet