Professional Documents
Culture Documents
Myasthenia Gravis
Myasthenia Gravis
Uploaded by
dmnd_cdCopyright:
Available Formats
You might also like
- Neonatal and Pediatric Respiratory CareDocument552 pagesNeonatal and Pediatric Respiratory CareFayena JoseNo ratings yet
- Seqs Uhs Past Shahroze (n66) All SubjectsDocument128 pagesSeqs Uhs Past Shahroze (n66) All SubjectsAli AhmadNo ratings yet
- Week 7 Practical Organ Bath SimulationDocument5 pagesWeek 7 Practical Organ Bath SimulationCésar Vallejo0% (1)
- Biology Project-Drugs and Alcohol AbuseDocument23 pagesBiology Project-Drugs and Alcohol AbuseDeepika81% (21)
- Physical Pharmacy Laboratory Experiment No PDFDocument8 pagesPhysical Pharmacy Laboratory Experiment No PDFAria DomingoNo ratings yet
- Myasthenia Gravis: An Autoimmune Neurologic DisorderDocument16 pagesMyasthenia Gravis: An Autoimmune Neurologic DisorderHibba NasserNo ratings yet
- Adrenergic AgonistsDocument18 pagesAdrenergic AgonistsJod Bell100% (1)
- Vasodilators: A B C D XDocument1 pageVasodilators: A B C D XPatricia Marie BuenafeNo ratings yet
- Pharmacology Assignment No.02: Submitted By: Submitted To: Nandraj Ma'am Areeba Shafiq Roll No. 1817007Document23 pagesPharmacology Assignment No.02: Submitted By: Submitted To: Nandraj Ma'am Areeba Shafiq Roll No. 1817007Nandraj123100% (1)
- Tissue TransplantDocument20 pagesTissue TransplantEva Boje-JugadorNo ratings yet
- Assessing Neurologic SystemDocument7 pagesAssessing Neurologic Systemjanikkakristal100% (1)
- Early and Late Signs of Increased Intracranial PressureDocument8 pagesEarly and Late Signs of Increased Intracranial PressureRhae Raynog100% (2)
- Assessment On RSDocument13 pagesAssessment On RSavinash dhameriyaNo ratings yet
- BMT ReportDocument26 pagesBMT ReportCaroline AgbayNo ratings yet
- Osteomyelitis 130708212636 Phpapp01Document107 pagesOsteomyelitis 130708212636 Phpapp01merikasorNo ratings yet
- AnaemiaDocument40 pagesAnaemiaNaveen Kumar100% (1)
- Drugs Used in TuberculosisDocument27 pagesDrugs Used in Tuberculosisapi-3705123No ratings yet
- Asthma (Reactive Airway Disease)Document33 pagesAsthma (Reactive Airway Disease)anwar jabariNo ratings yet
- Degenerative Disease of CNSDocument50 pagesDegenerative Disease of CNSRadhikaNo ratings yet
- Addisonian Crisis: Manish K Medical Officer IgmhDocument47 pagesAddisonian Crisis: Manish K Medical Officer IgmhNaaz Delhiwale100% (1)
- Acute Decompensated Heart FailureDocument31 pagesAcute Decompensated Heart Failure568563No ratings yet
- Nursing Process PlanningDocument18 pagesNursing Process PlanningRiezkya SiiKeke 'TaliaRegazze'No ratings yet
- CH 14 Test BankDocument21 pagesCH 14 Test BankKrestine Molle100% (1)
- Applications of AerosolesDocument7 pagesApplications of AerosolesAbhijeet GuptaNo ratings yet
- 20 Questions On AtherosclerosisDocument5 pages20 Questions On AtherosclerosisPaul WestonNo ratings yet
- Acute Biologic Crisis 1Document45 pagesAcute Biologic Crisis 1Nina OaipNo ratings yet
- ECG Rhythm InterpretationDocument16 pagesECG Rhythm InterpretationJanettNo ratings yet
- Diabetes Management ATIDocument15 pagesDiabetes Management ATIJessica ChirinoNo ratings yet
- Chapter 40: Drugs Used in Obstetrics Test Bank: Multiple ChoiceDocument10 pagesChapter 40: Drugs Used in Obstetrics Test Bank: Multiple ChoiceNurse UtopiaNo ratings yet
- Suctioning TracheaDocument24 pagesSuctioning Trachealuis_chubee100% (1)
- Aids ComprehensiveDocument2 pagesAids ComprehensiveErororoNo ratings yet
- IV FluidsDocument17 pagesIV FluidsTiffany NicolèNo ratings yet
- Acute Biologic CrisisDocument385 pagesAcute Biologic CrisisSheryl Ann Barit PedinesNo ratings yet
- Physiology Review: Neurophysiology: (Based On Guyton's and Personal Extras)Document5 pagesPhysiology Review: Neurophysiology: (Based On Guyton's and Personal Extras)djxela89No ratings yet
- Respiration 16 Respiratory FailureDocument31 pagesRespiration 16 Respiratory Failureapi-19641337No ratings yet
- Diabetes InsipidusDocument17 pagesDiabetes InsipidusSan Siddz100% (2)
- Lesson 5 - Oxygen TherapyDocument16 pagesLesson 5 - Oxygen TherapyDewi PrasetiaNo ratings yet
- Chapter 14Document15 pagesChapter 14missy23papNo ratings yet
- 10 EncephalopathyDocument18 pages10 EncephalopathyAbdullah ShiddiqNo ratings yet
- Fecal ImpactionDocument5 pagesFecal Impactioncharie2No ratings yet
- AerosolsDocument9 pagesAerosolsTubaNo ratings yet
- 10 AsthmaDocument39 pages10 AsthmaAkash MishraNo ratings yet
- Aerosoltherapy Nebu 120503115712 Phpapp01Document65 pagesAerosoltherapy Nebu 120503115712 Phpapp01Aan Ika SugathotNo ratings yet
- NCM100 Cystoclysis CareDocument2 pagesNCM100 Cystoclysis CarecchiechieNo ratings yet
- Oxygen Delivery Devices: Dr. HimanshuDocument40 pagesOxygen Delivery Devices: Dr. HimanshusnezaimNo ratings yet
- Ch. 1, Lesson 1: What Is The Next Gen NCLEXDocument4 pagesCh. 1, Lesson 1: What Is The Next Gen NCLEXChantel100% (1)
- Upper Respiratory DiseasesDocument3 pagesUpper Respiratory DiseasesanreilegardeNo ratings yet
- Seminar Hydrocephalus Surgery Yr 4 Rotation 3Document81 pagesSeminar Hydrocephalus Surgery Yr 4 Rotation 3BorhanNo ratings yet
- Tuberculosis Power PointDocument20 pagesTuberculosis Power PointLeena LapenaNo ratings yet
- Seminar Asthma PDFDocument39 pagesSeminar Asthma PDFAriff Mahdzub0% (1)
- Woman With PneumoniaDocument9 pagesWoman With PneumoniaNohaira SADANGNo ratings yet
- NUR 104 Nursing Process MY NOTESDocument77 pagesNUR 104 Nursing Process MY NOTESmeanne073100% (1)
- Myocardial InfarctionDocument18 pagesMyocardial InfarctionYanna Habib-MangotaraNo ratings yet
- Adverse Drug EffectsDocument66 pagesAdverse Drug EffectsSuba Ranjana BalaNo ratings yet
- Nebulization SHODocument10 pagesNebulization SHOkotekingNo ratings yet
- Drugs Affecting The Respiratory SystemDocument151 pagesDrugs Affecting The Respiratory SystemMajestic RavenNo ratings yet
- NUR100 Sherpath Skin Overview + Skin IntegrityDocument15 pagesNUR100 Sherpath Skin Overview + Skin Integritycaloy2345caloy100% (1)
- Chapter 29 Practice TestDocument8 pagesChapter 29 Practice Testnursingstudentd100% (1)
- Pericarditis NCLEX Review: Serous Fluid Is Between The Parietal and Visceral LayerDocument2 pagesPericarditis NCLEX Review: Serous Fluid Is Between The Parietal and Visceral LayerlhenNo ratings yet
- Pneumonia and BronchiolitisDocument48 pagesPneumonia and Bronchiolitisshashank panwarNo ratings yet
- A. Cardiac Failure: Biologic CrisisDocument11 pagesA. Cardiac Failure: Biologic CrisisJillian CaumbanNo ratings yet
- SnakebiteDocument4 pagesSnakebiteallenininiNo ratings yet
- Ebstein Anomaly, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandEbstein Anomaly, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- The politics of hunger: Protest, poverty and policy in England, <i>c.</i> 1750–<i>c.</i> 1840From EverandThe politics of hunger: Protest, poverty and policy in England, <i>c.</i> 1750–<i>c.</i> 1840No ratings yet
- AO 2009 0025 Essential Newborn CareDocument15 pagesAO 2009 0025 Essential Newborn Carejulesubayubay542895% (21)
- Action Verbs For ObjectivesDocument4 pagesAction Verbs For ObjectivesAnn Michelle TarrobagoNo ratings yet
- January 2010: Monday Tuesday Wednesday Thursday Friday Saturday SundayDocument12 pagesJanuary 2010: Monday Tuesday Wednesday Thursday Friday Saturday Sundaydmnd_cdNo ratings yet
- Components of CompetencyDocument4 pagesComponents of Competencydmnd_cd67% (3)
- Acute Complicated Urinary Tract Infection (Including Pyelonephritis) in Adults - UpToDateDocument39 pagesAcute Complicated Urinary Tract Infection (Including Pyelonephritis) in Adults - UpToDateLaís FialhoNo ratings yet
- 20 Travel Medicine Supplemental ChapterDocument57 pages20 Travel Medicine Supplemental ChapterDr. BriefsNo ratings yet
- Management of The Patient With A Burn InjuryDocument43 pagesManagement of The Patient With A Burn InjuryAshraf HusseinNo ratings yet
- New Therapies in Heart Failure Management: Nagendra S ChouhanDocument87 pagesNew Therapies in Heart Failure Management: Nagendra S ChouhanNagendra ChouhanNo ratings yet
- Protokol RcheopDocument3 pagesProtokol RcheopYudha RozyNo ratings yet
- Doctor of PhilosophyDocument3 pagesDoctor of PhilosophylichenresearchNo ratings yet
- Daftar Obat High Alert: 1.obat Risiko Tinggi A.NarkotikaDocument5 pagesDaftar Obat High Alert: 1.obat Risiko Tinggi A.NarkotikayuliNo ratings yet
- Pharmacognosy AlkaloidsDocument14 pagesPharmacognosy Alkaloidsdr amjadNo ratings yet
- Electives Module Pharmacology - 36Document2 pagesElectives Module Pharmacology - 36prasan bhandariNo ratings yet
- The Allergic Response: Kathleen Nicole B. Bidua First Year ResidentDocument44 pagesThe Allergic Response: Kathleen Nicole B. Bidua First Year ResidentNicole BiduaNo ratings yet
- Androgenic Supplementation in Men - Effects of Age Herbal ExtractDocument154 pagesAndrogenic Supplementation in Men - Effects of Age Herbal ExtractMaria PopaNo ratings yet
- Dermatologic Agents Integumentary System FunctionsDocument3 pagesDermatologic Agents Integumentary System FunctionsMay Chelle ErazoNo ratings yet
- NCM 103 Final Requirement - Nursing Care PlanDocument6 pagesNCM 103 Final Requirement - Nursing Care PlanCyrille Aira AndresaNo ratings yet
- AC After StrokeDocument6 pagesAC After StrokeDileepa chathurangaNo ratings yet
- MichauxDocument14 pagesMichauxSchwab RealHumanNo ratings yet
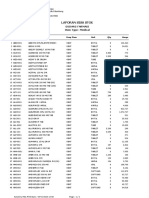
- Item Balance Per Unit RPTDocument58 pagesItem Balance Per Unit RPTYogie 1290No ratings yet
- SPAM Study Pack QLD HospitalsDocument15 pagesSPAM Study Pack QLD Hospitalskaira musahariNo ratings yet
- Anesthetic PDFDocument1 pageAnesthetic PDFsai calderNo ratings yet
- Kasus Acute Alcohol Poisoning ForensikDocument8 pagesKasus Acute Alcohol Poisoning ForensikSheila Sesary JNo ratings yet
- Hasler1997 OkDocument10 pagesHasler1997 OkRamiro Manzano NúñezNo ratings yet
- Heart Failure NCLEX QuestionsDocument5 pagesHeart Failure NCLEX QuestionsMelodia Turqueza GandezaNo ratings yet
- 22PG MATH-plus-Rationale-Journal-of-Intensive-Care-Medicine-Dec2020Document22 pages22PG MATH-plus-Rationale-Journal-of-Intensive-Care-Medicine-Dec2020Barbara RoweNo ratings yet
- Research Paper On Tuberculosis in IndiaDocument8 pagesResearch Paper On Tuberculosis in Indiakcjzgcsif100% (1)
- Key Answers On The ExamDocument81 pagesKey Answers On The ExamKarl Kiw-is100% (1)
- Fibromyalgia: PathophysiologyDocument4 pagesFibromyalgia: PathophysiologyMohamed Al-zichrawyNo ratings yet
- MEPRODocument4 pagesMEPROichaNo ratings yet
Myasthenia Gravis
Myasthenia Gravis
Uploaded by
dmnd_cdOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Myasthenia Gravis
Myasthenia Gravis
Uploaded by
dmnd_cdCopyright:
Available Formats
MYASTHENIA GRAVIS
>Is a neuromuscular disorder characterized by failure of transmission of nerve impulses at the
myoneural junction.
>MG may be caused by decreased functioning of acetylcholine receptor sites.
>Failure of transmission to skeletal muscles and voluntary muscles in the body
>Associated with autoimmunity and thymus gland anomalies (thymoma – tumor in the thymus gland)
Risk Factors:
> 20-30 years old for women
> 60-70 years old for men
> Heredity
Assessment:
Vision disturbances: Diplopia and Ptosis from ocular weakness
Masklike facial expression form involvement of facial muscles
Dysarthia and dysphagia from weakness of laryngeal muscles and pharyngeal muscles
Extreme muscular weakness and easy fatigability with repetitive activity and speech
Possible respiratory difficulty.
Diagnostic Evaluation:
Serum test for Ach receptor antibodies, which is positive in 90% of patients
Tensilon test (Endrophonium) : short acting cholinergic;
Positive Results: Definitive conclusion for MG. Muscle strength is improve, but muscle
weakness returns within 3 -5 minutes.
Electrophysiologic Test: shows decremental response to repetitive nerve stimulation
CT scan: reveals hyperplasia of the thymus, which is thought to initiate the autoimmune
response.
Medical Management:
Pharmacological:
> Acetylcholinesterase inhibitors/Cholinesterase Inhibitor
-Prostigmin (Neostigmine)
-Mestinon (Pyridostigmine)
-Mytelase (Ambenomium)
- These medications transmit neuromuscular impulses by preventing the destruction of Ach.
Therefore, there is increased muscle strength.
Nursing Interventions for Achterase Inhibitor
1. Monitor improvement of muscle strength and respirations.
2. Observe the client for signs and symptoms of cholinergic crisis caused by overdosing of the drug –
muscle weakness, increased salivation, sweating, tearing and miosis
3. Have readily available on antidote for cholinergic crisis (Atropine SO4)
4. Encourage the client to wear Medic Alert bracelet that indicates the health problem and the drug
taken
5. Instruct the client to take the medication before meals and in the morning for best drug absorption
6. Observe and report possible side effects and adverse reactions:
- N & V, diarrhea, abdominal cramps
-Increased salivation
-Tearing
-Miosis
-Possible hypertension
7. Administer drugs on time. To prevent myasthenic crisis
> Glucocorticoids. For anti-inflammatory and immunosuppressive effects
>Antacids. To prevent GI upset due to Glucocorticoids
Surgical Approach:
-Thymectomy (surgical removal of the thymus gland). 25% of people with MG have been found to
have thymoma. This surgery achieves remission for 5 to 10 years.
Other Approach:
Plasmapherisis: separation of Ach receptor antibodies from plasma.
Nursing Responsibilities:
>Monitor the patient’s RR, use of accessory muscles and O2 sat. to watch for possible respiratory
failure related to myasthenic or cholinergic crisis.
>Be alert for signs of an impending crisis:
-Sudden respiratory distress
-Signs of dysphagia, dysarthia, Ptosis and Diplopia
-Tachycardia. Anxiety
-Rapidly increasing weakness of extremities and trunk
-Monitor the patient’s responses to drug therapy
-Assess gag reflex and ability to swallow before giving anything PO
-Give cold water before starting feeding. To promote contractions
-Administer drugs on time
-Prevent infections
-Promote rest and comfort
Supportive Care
> Administer medications so their peak effect coincides with meals or essential activities
>Help the patient develop throughout the day to minimize fatigue
>Allow for rest periods throughout the day to minimize fatigue
> Provide assistive devices to help patient perform ADLs despite weakness
>For Diplopia, provide an eye patch to use n alternate eye to minimize risk of tripping and falling.
>To avoid aspiration
- Teach the patient to position the head in a slight ly flexed position to protect the airway during
eating
- Have a suction available that the patient can operate
- If the patient in crisis or has impaired swallowing, administer IV fluids and foods through NGT
-Elevate head after feeding
-If patient is on a mechanical ventilator, provide frequent suction, assess breath sounds and check
chest radiograph reports
> Show the patient how to cup chin in hands to support lower jaw to assist with speech
>If speech is severely affected, encourage the patient to use an alternate communication method,
such as flash cards or a letter board.
Education and Health Maintenance
>Instruct the patient and family about the symptoms of Myasthenic Crisis
>Teach the patient ways to prevent crisis and aggravation of symptoms
-Avoid exposure to colds and other infections
-Avoid excessive heat and cold
-Tell patient the patient to inform the dentist of condition because use of procaine (Novocaine) is not
well tolerated and may provoke crisis.
-Avoid emotional upset
>Teach the patient and family about the use of home suction
>Review the peak times of medications and how to schedule activity for best results
>Stress the importance of scheduled rest periods to avoid fatigue
>Encourage the patient to wear a medical alert bracelet
>Refer the patient and family to a support group such as www.myasthenia.org
Myasthenic Crisis
- is caused by undermedication or delayed medication
-clinical manifestations of Myasthenic Crisis is caused by undermedication or delayed medication
>Sudden rise in BP due to hypoxia
>Increase HR
>Severe respiratory distress and cyanosis
>Absent of cough and swallowing reflex
>Increased secretions, increased diaphoresis and increase lacrimation
>Restlessness and dysarthria
>Bowel and bladder incontinence
Interventions for MC are as follows:
-Increased doses of Cholinergics as long as the client responds positively to Tensilon
-Possible mechanical ventilation of respiratory muscle paralysis is acute.
Cholinergic Crisis
> Weakness with difficulty swallowing , chewing, speaking and breathing
>Apprehension, N & V
>Abdominal cramps and diarrhea
>Increased salivation
>Diaphoresis, lacrimation, fasciculations and blurred vision
Interventions for CC are as follows
-Discontinue cholinergic drugs until cholinergic effects decrease
-Provide adequate ventilation support
-Give Atropine SO4 as ordered
The followingshould be avoided:
-Muscle relaxants
-Barbiturates
-Morphine SO4
-Tranquilizers
- Neomycin
These drugs potentiate muscle weakness due to effect on neuromuscular junction.
You might also like
- Neonatal and Pediatric Respiratory CareDocument552 pagesNeonatal and Pediatric Respiratory CareFayena JoseNo ratings yet
- Seqs Uhs Past Shahroze (n66) All SubjectsDocument128 pagesSeqs Uhs Past Shahroze (n66) All SubjectsAli AhmadNo ratings yet
- Week 7 Practical Organ Bath SimulationDocument5 pagesWeek 7 Practical Organ Bath SimulationCésar Vallejo0% (1)
- Biology Project-Drugs and Alcohol AbuseDocument23 pagesBiology Project-Drugs and Alcohol AbuseDeepika81% (21)
- Physical Pharmacy Laboratory Experiment No PDFDocument8 pagesPhysical Pharmacy Laboratory Experiment No PDFAria DomingoNo ratings yet
- Myasthenia Gravis: An Autoimmune Neurologic DisorderDocument16 pagesMyasthenia Gravis: An Autoimmune Neurologic DisorderHibba NasserNo ratings yet
- Adrenergic AgonistsDocument18 pagesAdrenergic AgonistsJod Bell100% (1)
- Vasodilators: A B C D XDocument1 pageVasodilators: A B C D XPatricia Marie BuenafeNo ratings yet
- Pharmacology Assignment No.02: Submitted By: Submitted To: Nandraj Ma'am Areeba Shafiq Roll No. 1817007Document23 pagesPharmacology Assignment No.02: Submitted By: Submitted To: Nandraj Ma'am Areeba Shafiq Roll No. 1817007Nandraj123100% (1)
- Tissue TransplantDocument20 pagesTissue TransplantEva Boje-JugadorNo ratings yet
- Assessing Neurologic SystemDocument7 pagesAssessing Neurologic Systemjanikkakristal100% (1)
- Early and Late Signs of Increased Intracranial PressureDocument8 pagesEarly and Late Signs of Increased Intracranial PressureRhae Raynog100% (2)
- Assessment On RSDocument13 pagesAssessment On RSavinash dhameriyaNo ratings yet
- BMT ReportDocument26 pagesBMT ReportCaroline AgbayNo ratings yet
- Osteomyelitis 130708212636 Phpapp01Document107 pagesOsteomyelitis 130708212636 Phpapp01merikasorNo ratings yet
- AnaemiaDocument40 pagesAnaemiaNaveen Kumar100% (1)
- Drugs Used in TuberculosisDocument27 pagesDrugs Used in Tuberculosisapi-3705123No ratings yet
- Asthma (Reactive Airway Disease)Document33 pagesAsthma (Reactive Airway Disease)anwar jabariNo ratings yet
- Degenerative Disease of CNSDocument50 pagesDegenerative Disease of CNSRadhikaNo ratings yet
- Addisonian Crisis: Manish K Medical Officer IgmhDocument47 pagesAddisonian Crisis: Manish K Medical Officer IgmhNaaz Delhiwale100% (1)
- Acute Decompensated Heart FailureDocument31 pagesAcute Decompensated Heart Failure568563No ratings yet
- Nursing Process PlanningDocument18 pagesNursing Process PlanningRiezkya SiiKeke 'TaliaRegazze'No ratings yet
- CH 14 Test BankDocument21 pagesCH 14 Test BankKrestine Molle100% (1)
- Applications of AerosolesDocument7 pagesApplications of AerosolesAbhijeet GuptaNo ratings yet
- 20 Questions On AtherosclerosisDocument5 pages20 Questions On AtherosclerosisPaul WestonNo ratings yet
- Acute Biologic Crisis 1Document45 pagesAcute Biologic Crisis 1Nina OaipNo ratings yet
- ECG Rhythm InterpretationDocument16 pagesECG Rhythm InterpretationJanettNo ratings yet
- Diabetes Management ATIDocument15 pagesDiabetes Management ATIJessica ChirinoNo ratings yet
- Chapter 40: Drugs Used in Obstetrics Test Bank: Multiple ChoiceDocument10 pagesChapter 40: Drugs Used in Obstetrics Test Bank: Multiple ChoiceNurse UtopiaNo ratings yet
- Suctioning TracheaDocument24 pagesSuctioning Trachealuis_chubee100% (1)
- Aids ComprehensiveDocument2 pagesAids ComprehensiveErororoNo ratings yet
- IV FluidsDocument17 pagesIV FluidsTiffany NicolèNo ratings yet
- Acute Biologic CrisisDocument385 pagesAcute Biologic CrisisSheryl Ann Barit PedinesNo ratings yet
- Physiology Review: Neurophysiology: (Based On Guyton's and Personal Extras)Document5 pagesPhysiology Review: Neurophysiology: (Based On Guyton's and Personal Extras)djxela89No ratings yet
- Respiration 16 Respiratory FailureDocument31 pagesRespiration 16 Respiratory Failureapi-19641337No ratings yet
- Diabetes InsipidusDocument17 pagesDiabetes InsipidusSan Siddz100% (2)
- Lesson 5 - Oxygen TherapyDocument16 pagesLesson 5 - Oxygen TherapyDewi PrasetiaNo ratings yet
- Chapter 14Document15 pagesChapter 14missy23papNo ratings yet
- 10 EncephalopathyDocument18 pages10 EncephalopathyAbdullah ShiddiqNo ratings yet
- Fecal ImpactionDocument5 pagesFecal Impactioncharie2No ratings yet
- AerosolsDocument9 pagesAerosolsTubaNo ratings yet
- 10 AsthmaDocument39 pages10 AsthmaAkash MishraNo ratings yet
- Aerosoltherapy Nebu 120503115712 Phpapp01Document65 pagesAerosoltherapy Nebu 120503115712 Phpapp01Aan Ika SugathotNo ratings yet
- NCM100 Cystoclysis CareDocument2 pagesNCM100 Cystoclysis CarecchiechieNo ratings yet
- Oxygen Delivery Devices: Dr. HimanshuDocument40 pagesOxygen Delivery Devices: Dr. HimanshusnezaimNo ratings yet
- Ch. 1, Lesson 1: What Is The Next Gen NCLEXDocument4 pagesCh. 1, Lesson 1: What Is The Next Gen NCLEXChantel100% (1)
- Upper Respiratory DiseasesDocument3 pagesUpper Respiratory DiseasesanreilegardeNo ratings yet
- Seminar Hydrocephalus Surgery Yr 4 Rotation 3Document81 pagesSeminar Hydrocephalus Surgery Yr 4 Rotation 3BorhanNo ratings yet
- Tuberculosis Power PointDocument20 pagesTuberculosis Power PointLeena LapenaNo ratings yet
- Seminar Asthma PDFDocument39 pagesSeminar Asthma PDFAriff Mahdzub0% (1)
- Woman With PneumoniaDocument9 pagesWoman With PneumoniaNohaira SADANGNo ratings yet
- NUR 104 Nursing Process MY NOTESDocument77 pagesNUR 104 Nursing Process MY NOTESmeanne073100% (1)
- Myocardial InfarctionDocument18 pagesMyocardial InfarctionYanna Habib-MangotaraNo ratings yet
- Adverse Drug EffectsDocument66 pagesAdverse Drug EffectsSuba Ranjana BalaNo ratings yet
- Nebulization SHODocument10 pagesNebulization SHOkotekingNo ratings yet
- Drugs Affecting The Respiratory SystemDocument151 pagesDrugs Affecting The Respiratory SystemMajestic RavenNo ratings yet
- NUR100 Sherpath Skin Overview + Skin IntegrityDocument15 pagesNUR100 Sherpath Skin Overview + Skin Integritycaloy2345caloy100% (1)
- Chapter 29 Practice TestDocument8 pagesChapter 29 Practice Testnursingstudentd100% (1)
- Pericarditis NCLEX Review: Serous Fluid Is Between The Parietal and Visceral LayerDocument2 pagesPericarditis NCLEX Review: Serous Fluid Is Between The Parietal and Visceral LayerlhenNo ratings yet
- Pneumonia and BronchiolitisDocument48 pagesPneumonia and Bronchiolitisshashank panwarNo ratings yet
- A. Cardiac Failure: Biologic CrisisDocument11 pagesA. Cardiac Failure: Biologic CrisisJillian CaumbanNo ratings yet
- SnakebiteDocument4 pagesSnakebiteallenininiNo ratings yet
- Ebstein Anomaly, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandEbstein Anomaly, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- The politics of hunger: Protest, poverty and policy in England, <i>c.</i> 1750–<i>c.</i> 1840From EverandThe politics of hunger: Protest, poverty and policy in England, <i>c.</i> 1750–<i>c.</i> 1840No ratings yet
- AO 2009 0025 Essential Newborn CareDocument15 pagesAO 2009 0025 Essential Newborn Carejulesubayubay542895% (21)
- Action Verbs For ObjectivesDocument4 pagesAction Verbs For ObjectivesAnn Michelle TarrobagoNo ratings yet
- January 2010: Monday Tuesday Wednesday Thursday Friday Saturday SundayDocument12 pagesJanuary 2010: Monday Tuesday Wednesday Thursday Friday Saturday Sundaydmnd_cdNo ratings yet
- Components of CompetencyDocument4 pagesComponents of Competencydmnd_cd67% (3)
- Acute Complicated Urinary Tract Infection (Including Pyelonephritis) in Adults - UpToDateDocument39 pagesAcute Complicated Urinary Tract Infection (Including Pyelonephritis) in Adults - UpToDateLaís FialhoNo ratings yet
- 20 Travel Medicine Supplemental ChapterDocument57 pages20 Travel Medicine Supplemental ChapterDr. BriefsNo ratings yet
- Management of The Patient With A Burn InjuryDocument43 pagesManagement of The Patient With A Burn InjuryAshraf HusseinNo ratings yet
- New Therapies in Heart Failure Management: Nagendra S ChouhanDocument87 pagesNew Therapies in Heart Failure Management: Nagendra S ChouhanNagendra ChouhanNo ratings yet
- Protokol RcheopDocument3 pagesProtokol RcheopYudha RozyNo ratings yet
- Doctor of PhilosophyDocument3 pagesDoctor of PhilosophylichenresearchNo ratings yet
- Daftar Obat High Alert: 1.obat Risiko Tinggi A.NarkotikaDocument5 pagesDaftar Obat High Alert: 1.obat Risiko Tinggi A.NarkotikayuliNo ratings yet
- Pharmacognosy AlkaloidsDocument14 pagesPharmacognosy Alkaloidsdr amjadNo ratings yet
- Electives Module Pharmacology - 36Document2 pagesElectives Module Pharmacology - 36prasan bhandariNo ratings yet
- The Allergic Response: Kathleen Nicole B. Bidua First Year ResidentDocument44 pagesThe Allergic Response: Kathleen Nicole B. Bidua First Year ResidentNicole BiduaNo ratings yet
- Androgenic Supplementation in Men - Effects of Age Herbal ExtractDocument154 pagesAndrogenic Supplementation in Men - Effects of Age Herbal ExtractMaria PopaNo ratings yet
- Dermatologic Agents Integumentary System FunctionsDocument3 pagesDermatologic Agents Integumentary System FunctionsMay Chelle ErazoNo ratings yet
- NCM 103 Final Requirement - Nursing Care PlanDocument6 pagesNCM 103 Final Requirement - Nursing Care PlanCyrille Aira AndresaNo ratings yet
- AC After StrokeDocument6 pagesAC After StrokeDileepa chathurangaNo ratings yet
- MichauxDocument14 pagesMichauxSchwab RealHumanNo ratings yet
- Item Balance Per Unit RPTDocument58 pagesItem Balance Per Unit RPTYogie 1290No ratings yet
- SPAM Study Pack QLD HospitalsDocument15 pagesSPAM Study Pack QLD Hospitalskaira musahariNo ratings yet
- Anesthetic PDFDocument1 pageAnesthetic PDFsai calderNo ratings yet
- Kasus Acute Alcohol Poisoning ForensikDocument8 pagesKasus Acute Alcohol Poisoning ForensikSheila Sesary JNo ratings yet
- Hasler1997 OkDocument10 pagesHasler1997 OkRamiro Manzano NúñezNo ratings yet
- Heart Failure NCLEX QuestionsDocument5 pagesHeart Failure NCLEX QuestionsMelodia Turqueza GandezaNo ratings yet
- 22PG MATH-plus-Rationale-Journal-of-Intensive-Care-Medicine-Dec2020Document22 pages22PG MATH-plus-Rationale-Journal-of-Intensive-Care-Medicine-Dec2020Barbara RoweNo ratings yet
- Research Paper On Tuberculosis in IndiaDocument8 pagesResearch Paper On Tuberculosis in Indiakcjzgcsif100% (1)
- Key Answers On The ExamDocument81 pagesKey Answers On The ExamKarl Kiw-is100% (1)
- Fibromyalgia: PathophysiologyDocument4 pagesFibromyalgia: PathophysiologyMohamed Al-zichrawyNo ratings yet
- MEPRODocument4 pagesMEPROichaNo ratings yet