Professional Documents
Culture Documents
Jurnal 2 Ebcr
Jurnal 2 Ebcr
Uploaded by
hermanfirdausOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Jurnal 2 Ebcr
Jurnal 2 Ebcr
Uploaded by
hermanfirdausCopyright:
Available Formats
ORIGINAL PAPER
The combination of amlodipinevalsartan 5160 mg
produces less peripheral oedema than amlodipine 10 mg
in hypertensive patients not adequately controlled with
amlodipine 5 mg
J. Schrader,1 A. Salvetti,2 C. Calvo,3 E. Akpinar,4 L. Keeling,5 M. Weisskopf,5 P. Brunel5
1
St. Josef-Hospital,
SUMMARY
Whats known Cloppenburg, Germany
2
Aims: To demonstrate the benefit of the combination amlodipine valsartan Amlodipine, a widely used antihypertensive agent, Department of Internal
Medicine, University of Pisa,
5 160 mg over amlodipine 10 mg, in producing a lower incidence of peripheral causes peripheral oedema, an adverse event that is
Pisa, Italy
oedema for a comparable mean sitting systolic blood pressure (MSSBP) reduction. established to be dose-dependent, owing primarily 3
Hospital Clinico Universitario
to preferential arteriolar dilation. At the capillary
Methods: After a 4-week amlodipine 5 mg run-in phase, inadequately controlled Santiago De Compostela,
level, venodilation should compensate for the C Choupana, s n, Spain
hypertension patients (aged 55 years, MSSBP 130 and 160 mmHg) were
arteriolar dilation and thus minimise amlodipine- 4
Cukurova University Medical
randomised to receive amlodipine valsartan 5 160 mg or amlodipine 10 mg for induced peripheral oedema. The combination of Faculty, Department of Family
8 weeks, followed by amlodipine valsartan 5 160 mg for 4 weeks for all patients. valsartan and amlodipine is associated with better Medicine, Adana, Turkey
5
Primary variables were MSSBP change from baseline to week 8 and incidence of efficacy and tolerability than amlodipine alone. Clinical Development &
peripheral oedema reported as an AE. Resolution of peripheral oedema was Medical Affairs, Novartis
Whats new Pharma AG, Basel, Switzerland
assessed 4 weeks after switching patients from amlodipine 10 mg to amlodipine
This study shows that adding valsartan to the
valsartan 5 160 mg. Results: At week 8, MSSBP showed greater reduction with common starting dose of amlodipine provides Correspondence to:
amlodipine valsartan 5 160 mg than amlodipine 10 mg (least square mean: similar BP reduction with a better tolerability profile Patrick Brunel,
)8.01 vs. )5.95 mmHg, p < 0.001 for non-inferiority and p = 0.002 for superior- (leading to fewer discontinuations) when compared
Clinical Development & Medical
Affairs, Novartis Pharma AG,
ity). Systolic control, overall BP control and systolic response rate at week 8 were with the up-titration of amlodipine. This further
Basel, Switzerland
significantly higher with combination than amlodipine 10 mg (34 vs. 26%; 57 vs. enhances the clinical evidence for the early use of Tel.: + 41 61 32 40245
50%; 36.57 vs. 27.77%, respectively). Incidence of peripheral oedema was signifi- combination therapy, supported by effective BP Fax: + 41 61 3242078
cantly lower with the combination than amlodipine 10 mg (6.6 vs. 31.1%, reduction, improved tolerability and increased Email:
persistence on antihypertensive treatment. patrick.brunel@novartis.com
p < 0.001). Peripheral oedema resolved in 56% patients who switched from am-
lodipine 10 mg to the combination, without the loss of effect on BP reduction. Disclosures
Conclusion: In non-responders to amlodipine 5 mg, treatment with amlodi- This study was supported and
pine valsartan 5 160 mg induced significantly less peripheral oedema than amlod- funded by Novartis Pharma AG,
Basel, Switzerland. Patrick
ipine 10 mg for similar BP reduction. Peripheral oedema resolved in > 50% Brunel, Marianne Weisskopf
patients switching from amlodipine 10 mg to the combination. and Lucy Keeling are employees
of Novartis Pharma AG.
ClinicalTrials.gov
with only 338% of patients worldwide (3) and 31
Introduction Identifier NCT00437645
63% in developed countries attaining target BP of
Hypertension is a well-known major risk factor for < 140 90 mmHg (4). Among various factors contrib- Re-use of this article is
permitted in accordance with
target organ damage and cardiovascular (CV) clinical uting to inadequate BP control, efficacy and tolera- the Creative Commons Deed,
events (1), representing the number one underlying bility of drug treatment seem to play a prominent Attribution 2.5, which does not
cause of death worldwide (2). Although available role (1,3). permit commercial exploitation.
data from controlled clinical studies indicate that Monotherapy is a rational therapeutic approach in
blood pressure (BP) reduction to target levels (BP patients with mild BP elevation and low-to-moderate
< 140 90 mmHg in all hypertensive patients and CV risk, with targeted BP < 140 90 mmHg (1).
< 130 80 mmHg in diabetic patients and high or However, the ability of any agent used alone to achieve
very high-risk patients) is associated with a signifi- target BP values is limited to not more than 2030%
cant decrease in CV mortality and morbidity, such of hypertensive patients except in those with grade 1
target BP values are difficult to achieve (1). Thus, hypertension (1). In responders to monotherapy, but
available data indicate that a major challenge in the with uncontrolled BP, the increase in dosage for drugs
treatment of hypertension is inadequate BP control, with dose-dependent efficacy constitutes a further
2009 The Authors
Journal compilation 2009 Blackwell Publishing Ltd Int J Clin Pract, February 2009, 63, 2, 217225
doi: 10.1111/j.1742-1241.2008.01977.x 217
218 Reduced peripheral oedema with amlodipine valsartan vs. amlodipine monotherapy
rational therapeutic approach. But several antihyper-
tensive drugs, including calcium antagonists, also have
Methods
a dose-dependent tolerability profile. Therefore, Study design
increasing the dose could result in an increased This was a multi-centre, randomised, double-blind,
incidence of adverse events (AEs), thus reducing double-dummy, placebo-controlled, parallel-group
patient compliance with therapy. In these patients, study evaluating the benefit of the amlodipine val-
low-dose combination therapy is a better therapeutic sartan 5 160 mg combination in reducing peripheral
alternative, provided that the combination includes oedema, for the same BP lowering, compared with
drugs with different and complementary mechanisms amlodipine 10 mg alone in patients with essential
of action, which could additionally potentiate the hypertension. The study was performed in 148 cen-
antihypertensive effect and improve tolerability while tres in 12 countries (Argentina, Chile, Ecuador, Fin-
minimising individual side effects (1,5). Moreover, a land, France, Germany, Italy, Norway, Spain,
fixed-dose combination of two drugs fulfilling the Sweden, Switzerland, Turkey) between January and
above mentioned criteria can simplify the treatment November 2007 and was conducted in accordance
schedule and improve patient compliance (1,6). with International Conference on Harmonization
Amlodipine, a dihydropyridine calcium channel Good Clinical Practice (ICH-GCP), Declaration of
blocker, is one of the most widely used agents in the Helsinki and applicable local regulations. The study
treatment of hypertension (7) and is considered by received approval from Institutional Review Board or
many to be the most efficacious. However, a major Ethical Review Committee, and all patients provided
hurdle with the use of amlodipine is the occurrence written informed consent.
of peripheral oedema (8,9), when the dose is
increased (10,11). Therefore, a rational therapeutic The study comprised a 4-week, single-blind,
approach for preventing the peripheral oedema asso- amlodipine 5 mg run-in period and a 12-week,
ciated with amlodipine, would be to add a potent double-blind, active-treatment period. At the end of
and highly selective blocker of the reninangiotensin the single-blind, run-in period, patients whose mean
system (1), such as valsartan to compensate for the sitting systolic BP (MSSBP) was not adequately
arteriolar dilation produced by amlodipine (12) by controlled (MSSBP 130 and 160 mmHg) were
also dilating the venules (13), limiting fluid leakage randomised (1 : 1) to receive amlodipine valsartan
into tissues. Thus, two key mechanisms are targeted 5 160 mg combination or amlodipine 10 mg alone
to achieve rapid and optimal BP control (14) and for 8 weeks. At week 8, patients who were on am-
indeed the combination of amlodipine and valsartan lodipine valsartan 5 160 mg combination continued
is associated with a significantly better BP-lowering the same treatment, whereas those who were on
effect and greater response rate compared with amlodipine 10 mg alone switched to the amlodi-
amlodipine alone (15). pine valsartan combination for an additional
In this study, we evaluated the non-inferiority of 4 weeks (Figure 1).
the combination amlodipine valsartan 5 160 mg Patients were instructed to take the study medica-
compared with amlodipine 10 mg with respect to tion orally with water once daily in the morning,
antihypertensive efficacy, along with the incidence of regardless of meals, except on days of visit, when the
peripheral oedema, in patients not adequately con- medication was taken under the supervision of the
trolled with amlodipine 5 mg alone. We also assessed investigator after BP assessment. On the first day of
the incidence of peripheral oedema resolution when the double-blind phase, BP was measured in both
patients who developed peripheral oedema during arms using an Omron automated BP monitor, and
8 weeks of treatment were switched from amlodipine the arm with higher diastolic BP reading was used at
10 mg to the combination of amlodipine valsartan all subsequent visits. The MSSBP and mean sitting
5 160 mg. diastolic BP (MSDBP) were measured at trough three
Week -4 Aml/Val 5/160 mg
Visit 1 Aml 5 mg
single-
blind run- Aml/Val
Aml 10 mg
in phase 5/160 mg
Randomization Week 4 Week 8 Week 12
Visit 2, Day 1 Visit 3 Visit 4 Visit 5
Figure 1 Schematic representation of the study design. Aml, amlodipine; Aml Val, amlodipine valsartan
2009 The Authors
Journal compilation 2009 Blackwell Publishing Ltd Int J Clin Pract, February 2009, 63, 2, 217225
Reduced peripheral oedema with amlodipine valsartan vs. amlodipine monotherapy 219
times (at 2-min intervals between measurements) at for analyses. If a patient experienced more than one
each visit, and the average of three readings was occurrence of peripheral oedema between start of the
recorded for analysis. double-blind phase and week 8, it was only counted
once in the analysis. In the case of patients who
Study population discontinued before week 8, the information available
Male and female patients (aged 55 years) with up to that point was used for analysis.
essential systolic hypertension (MSSBP 140 and The absolute number and proportion of patients
160 mmHg, if not previously treated and MSSBP with peripheral oedema resolution at week 12 (after
160 mmHg, if pretreated on monotherapy) were switching from amlodipine 10 mg to the amlodi-
enrolled into the run-in phase at week-4. pine valsartan 5 160 mg combination at week 8 or
The inclusion criteria for randomisation were continuing on amlodipine valsartan 5 160 mg for
patients with MSSBP 130 and 160 mmHg and 12 weeks) were also recorded.
no peripheral oedema. Exclusion criteria were
patients with MSSBP > 180 mmHg or MSDBP Further safety assessments
> 110 mmHg at any time during the single-blind Other safety assessments included regular monitoring
run-in phase; patients on more than one antihyper- and recording of all AEs, vital signs and physical
tensive agent on the day of randomisation; secondary examination, laboratory investigations and ECG as
hypertension; suspected contraindications; significant per the visit schedules. Each AE was described by its
CV and cerebrovascular, renal, hepatic or pancreatic duration, severity and relationship to the study drug.
diseases; type 1 diabetes mellitus and inadequately
controlled type 2 diabetes mellitus; any surgical or Statistical analysis
medical condition, which could affect drug disposi- All statistical analyses were performed using non-
tion or place the patient at higher risk; and women inferiority tests at the one-sided significance level of
of child-bearing potential. 0.025. A sample size of 916 patients (458 patients per
group) was required (90% power) to show non-infe-
Efficacy riority (change in MSSBP and MSDBP) between the
One of the co-primary variables was change in treatment groups. The intent-to-treat population was
MSSBP from baseline (day of randomisation) up to used for the efficacy analyses. The safety population
week 8 [last observation carried forward (LOCF)]. (defined as patients who received at least one dose of
The secondary efficacy variables were the (i) change double-blind study drug) was used for the analysis of
in MSSBP and MSDBP, (ii) systolic control rate data on peripheral oedema and AEs.
(defined as MSSBP < 130 mmHg), (iii) overall con- For the primary efficacy variable, the last postbase-
trol rate (defined as BP < 140 90 mmHg for non- line MSSBP measurement collected (LOCF) was used
diabetic patients and < 130 80 mmHg for diabetic for the analysis in case of patients who discontinued
patients), and systolic response rate (defined as prior to week 8. The change from baseline (day 1) in
MSSBP < 130 mmHg or at least 20 mmHg reduction MSSBP and MSDBP at weeks 4, 8 and 12 was analy-
from baseline in MSSBP) at weeks 4, 8 and 12 in sed using analysis of covariance (ANCOVA) with
each treatment group. baseline as covariate and a non-inferiority margin of
3 mmHg for MSSBP and 2 mmHg for MSDBP. A
Safety and tolerability logistic regression model was used for the analysis of
the number of patients with systolic BP control and
Peripheral oedema systolic response rate (with baseline MSSBP as covar-
The second co-primary variable was the presence of iate) and overall BP control (with baseline MSSBP
peripheral oedema, which was evaluated at every visit. and MSDBP as covariates). The proportion of
The evaluation was based on spontaneously reported patients who developed peripheral oedema in each
oedema by the patients and on the presence of signs treatment group up to and including week 8 was
of oedema on physical examination of the patient by analysed using logistic regression, with treatment,
the investigator. Patients were counted as having region and diabetic status as fixed factors.
peripheral oedema if it occurred at any time postdose,
up to and including week 8. The absolute number
Results
and proportion of patients with peripheral oedema at
any time postdose and up to and including week 8 Patient demographics
were summarised by severity (none, mild, moderate Of 1644 patients who were screened, 1521 were
and severe) and treatment group. If the severity enrolled into the single-blind amlodipine 5 mg, run-
changed over time, the maximum severity was used in phase (week-4). Overall, 1183 patients were
2009 The Authors
Journal compilation 2009 Blackwell Publishing Ltd Int J Clin Pract, February 2009, 63, 2, 217225
220 Reduced peripheral oedema with amlodipine valsartan vs. amlodipine monotherapy
randomised (1 : 1) to receive amlodipine valsartan )0.79); p < 0.001 for non-inferiority and p = 0.002
5 160 mg (n = 592) or amlodipine 10 mg (n = 591) for superiority].
(Figure 2). Of these, 1033 patients completed the Non-inferiority was also observed with LSM
study, and the rate of completion was higher in the reductions from baseline at week 4 ()8.29 vs. )6.29;
amlodipine valsartan group (94.1%) than in the p < 0.001) and week 8 ()8.23 vs. )6.13; p < 0.001)
amlodipine 10 mg group (80.5%). The frequency of in MSSBP, at week 4 ()5.02 vs. )4.23; p < 0.001)
discontinuation caused by AEs was higher in the and week 8 ()4.70 vs. )4.06; p < 0.001) in MSDBP
amlodipine group (14.2%) when compared with the and at week 12 after the switch from amlodipine
amlodipine valsartan group (2.5%). 10 mg to amlodipine valsartan 5 160 mg ()9.13 vs.
Males and females were equally represented with )8.16; p < 0.001 for MSSBP and )5.52 vs. )4.90;
an overall mean age of 65.5 years, and in both treat- p < 0.001 for MSDBP) between the amlodipine val-
ment groups most of the patients were Caucasian sartan and amlodipine treatment strategy groups
(95%). At baseline, after 4 weeks of treatment with (Figure 3).
amlodipine 5 mg, the overall MSSBP and MSDBP The systolic control produced by the combination
were 143.9 and 83.8 mmHg, respectively. The treat- of amlodipine valsartan was better than amlodipine
ment groups were well-matched with respect to age, alone, at week 4 [34.98 vs. 24.83%; 95% CI (1.22,
gender, race, body mass index, MSSBP, MSDBP, dia- 2.14); p < 0.001] and week 8 [34.28 vs. 26.21%; 95%
betes status and a history of prior antihypertensive CI (1.06, 1.88); p = 0.019], and similar after the
medication (Table 1). switch from amlodipine 10 mg to amlodipine valsar-
tan 5 160 mg at week 12 [38.04 vs. 31.81%; 95% CI
Efficacy (0.92, 1.62); p = 0.162].
For change in MSSBP from baseline at week 8 Overall BP control was attained in a significantly
(LOCF), the least square mean (LSM) reduction with higher proportion of patients when treated with the
the amlodipine valsartan group was shown to be amlodipine valsartan combination therapy than
statistically non-inferior when compared with the with amlodipine monotherapy at weeks 4 and 8
amlodipine group [)8.01 vs. )5.95; 95% CI ()3.34, (Figure 4).
Screened
(n = 1644)
Enrolled (Visit 1)
Received amlodipine 5 mg
(n = 1521)
Randomized (Visit 2)
(n = 1183)
Received amlodipine/valsartan Received amlodipine
5/160 mg (n = 592) 10 mg (n = 591)
Discontinued (n = 35) Discontinued (n = 115)
Adverse events: n = 15 Adverse events: n = 84
Withdrawal of consent: n = 10 Withdrawal of consent: n = 22
Protocol deviation: n = 3 Protocol deviation: n = 3
Lost to follow-up: n = 2 Lost to follow-up: n = 3
Administrative problems: n = 2 Administrative problems: n = 1
Unsatisfactory therapeutic effect: n = 2 Unsatisfactory therapeutic effect: n = 1
Drug no longer required: n = 1 Drug no longer required: n = 1
Completed and analyzed Completed and analyzed
(n = 557) (n = 476)
Figure 2 Overall patient disposition during the treatment period
2009 The Authors
Journal compilation 2009 Blackwell Publishing Ltd Int J Clin Pract, February 2009, 63, 2, 217225
Reduced peripheral oedema with amlodipine valsartan vs. amlodipine monotherapy 221
Table 1 Demographic and baseline characteristics of the patient population at randomisation
Amlodipine valsartan 5 160 mg Amlodipine 10 mg Total
n = 592 n = 591 n = 1183
Age (years) [Mean (SD)] 65.6 (7.56) 65.4 (7.16) 65.5 (7.36)
Gender n (%)
Male 307 (51.9%) 307 (51.9%) 614 (51.9%)
Female 285 (48.1%) 284 (48.1%) 569 (48.1%)
Race n (%)
Caucasian 559 (94.4%) 560 (94.8%) 1119 (94.6%)
Other 33 (5.6%) 28 (4.7%) 61 (5.2%)
Asian 0 2 (0.3%) 2 (0.2%)
Pacific islander 0 1 (0.2%) 1 (0.1%)
BMI kg m2 28.9 (4.59) 28.7 (4.41) 28.8 (4.50)
MSSBP (mmHg) 143.4 (7.99) 144.4 (8.16) 143.9 (8.09)
MSDBP (mmHg) 83.3 (8.74) 84.2 (8.44) 83.8 (8.60)
Diabetes status n (%)
No 486 (82.1%) 493 (83.4%) 979 (82.8%)
Yes 106 (17.9%) 98 (16.6%) 204 (17.2%)
Prior antihypertensive medication n (%)
No 146 (24.7%) 120 (20.3%) 266 (22.5%)
Yes 446 (75.3%) 471 (79.7%) 917 (77.5%)
MSSBP, mean sitting systolic blood pressure; MSDBP, mean sitting diastolic blood pressure; BMI, body mass index.
Week 4 Week 8 Week 12 Week 4 Week 8 Week 12
LSM change from baseline (mm Hg)
0
1
2
3
4
423 406
5
470 490
502
6 552
629 613
7
8 * *
829 823 816 *
9
913
10
* * *
MSSBP MSDBP
Amlodipine/valsartan 5/160 mg
Amlodipine 10 mg
Amlodipine 10 mg switched to amlodipine/valsartan 5/160 mg
Figure 3 Change from baseline in MSSBP and MSDBP. *p < 0.001 for non-inferiority, between treatment groups. LSM,
least square mean; MSSBP, mean sitting systolic blood pressure; MSDBP, mean sitting diastolic blood pressure
The systolic BP response rate was higher with Safety and tolerability
amlodipine valsartan 5 160 mg than with amlodi-
pine 10 mg at week 4 [37.20 vs. 26.72, 95% CI (1.23, Peripheral oedema
2.08); p < 0.001] and week 8 [36.57 vs. 27.77%, 95% The most frequently reported AE during the study
CI (1.10, 1.90); p = 0.009], and similar after the was peripheral oedema, which was considerably
switch from amlodipine 10 mg to amlodipine valsar- higher in the amlodipine 10 mg group (31.5%) than
tan 5 160 mg at week 12 [40.36 vs. 35.76%; 95% CI in the amlodipine valsartan 5 160 mg group (7.3%).
(0.87, 1.48); p = 0.347]. The severity of peripheral oedema was also higher in
2009 The Authors
Journal compilation 2009 Blackwell Publishing Ltd Int J Clin Pract, February 2009, 63, 2, 217225
222 Reduced peripheral oedema with amlodipine valsartan vs. amlodipine monotherapy
Amlodipine/valsartan 5/160 mg
Amlodipine 10 mg
Amlodipine 10 mg switched to amlodipine/valsartan 5/160 mg
*
70 **
6125
60 5785 5724
5530
Proportion of patients (%)
4879 4971
50
40
30
20
10
0
Week 4 Week 8 Week 12
Figure 4 Effect of the treatment regimen on overall blood pressure (BP) control. *p < 0.001 between the treatment groups
at week 4. **p = 0.019 between the treatment groups at week 8. Overall BP control is defined as BP < 140 90 mmHg for
non-diabetic and < 130 80 mmHg for diabetic patients
the amlodipine 10 mg group compared with the group (55.7%) than the amlodipine valsartan group
amlodipine valsartan 5 160 mg group (mild: 17.6 vs. (43.9%). After peripheral oedema, the second most
5.9%; moderate: 10.3 vs. 1.2%; severe: 3.6 vs. 0.2%, frequently reported AE related to the drug was
respectively). headache, which also occurred at a higher frequency
The combination of amlodipine valsartan in the amlodipine group (3.2%) than in the amlo-
5 160 mg induced significantly less peripheral oedema dipine valsartan group (2.2%). The frequencies of
than amlodipine 10 mg [6.6 vs. 31.1%; 96% CI (0.11, other AEs were comparable in both the groups.
0.22); p < 0.001] up to and including week 8 (Table 2). The main reason for discontinuation was AEs
The incidence of peripheral oedema decreased in both (2.5% with amlodipine valsartan vs. 14.2% in am-
treatment groups from week 8 to 12. This decrease, lodipine) and the most frequently reported AE lead-
however, was more pronounced in the group that was ing to discontinuation was peripheral oedema (1%
switched over from amlodipine 10 mg to amlodi- with amlodipine valsartan vs. 11.5% with amlodi-
pine valsartan 5 160 mg combination (31.1% at week pine), followed by headache (0.2% with amlodi-
8 and 14.2% at week 12) than in the group that pine valsartan vs. 0.5% with amlodipine).
continued on amlodipine valsartan up to week 12 There were no deaths in this study, and serious
(6.6% at week 8 and 4.9% at week 12) (Figure 5). adverse experiences (SAEs) were rare. Eleven patients
Resolution of peripheral oedema was observed in (1.9%) in the amlodipine valsartan group and eight
more than half of the patients (44 out of 79, exclud- patients (1.4%) in the amlodipine group experienced
ing five new cases after week 8) after they were SAEs, which included two cases of serious cholecystitis
switched over from amlodipine 10 mg to the amlodi- in the amlodipine valsartan group and one case each
pine valsartan 5 160 mg combination (Table 2). of gastrointestinal necrosis, gastrointestinal haemo-
Resolution of peripheral oedema at week 12 was rrhage and inguinal hernia in the amlodipine group.
higher in the patients who had switched from None of these SAEs was suspected to be study drug
amlodipine 10 mg to amlodipine valsartan 5 160 mg related. There were no clinically notable laboratory
(55.6%) than in patients who were on the amlodi- findings in this study.
pine valsartan combination (41.7%).
Discussion
Further safety results
Both treatment regimens were well tolerated. The over- Amlodipine has a well-documented BP-lowering
all incidence of AEs was higher in the amlodipine efficacy; however, in non-responders to amlodipine
2009 The Authors
Journal compilation 2009 Blackwell Publishing Ltd Int J Clin Pract, February 2009, 63, 2, 217225
Reduced peripheral oedema with amlodipine valsartan vs. amlodipine monotherapy 223
Table 2 Incidence and resolution of peripheral oedema
Amlodipine Amlodipine Amlodipine switched to
valsartan 5 160 mg 10 mg amlodipine valsartan
n (%) n (%) at week 8 n (%)
No. of patients randomised 592 591
No. of patients with peripheral 39 (6.6) 184 (31.1)*
oedema during the first 8 weeks
Peripheral oedema suspected to 36 (6.1) 171 (28.9)
be drug-related by physician
No. of patients treated after week 8 (switch**) 562 484
No. of patients with peripheral 24 (4.3) 79 (16.3)
oedema entering switch phase
No. of patients with peripheral oedema 10 (1.8) 44 (9.1)
resolution during switch phase
No. of patients with unresolved 14 (2.5) 35 (7.2)
peripheral oedema during the switch phase
New cases of peripheral oedema 5 (0.9) 5 (1.0)
during the switch phase
*p < 0.001, between the two groups. **At week 8, amlodipine 10 mg patients were switched to amlodipine valsartan 5 160 mg;
patients on amlodipine valsartan 5 160 mg were continued on the same treatment regimen.
200
184 Amlodipine/valsartan 5/160 mg
180 Amlodipine 10 mg
160 Amlodipine 10 mg switched to
amlodipine/valsartan 5/160 mg
140
No. of patients
120
100
79
80
60
39 35
40
24
20 14
0
Upto and including Week 8 At the 'switch' at Week 8 At the end of the study
(week 12)
Resolution of oedema at Week 12
Amlodipine/valsartan 5/160 mg: 41.7%
Amlodipine 10 mg switched to amlodipine/valsartan 5/160 mg: 55.6%
Figure 5 Incidence of peripheral oedema at week 8 and 12
monotherapy, up-titration is limited by dose-depen- Adding an ARB, such as valsartan, presents a feasible
dent adverse effects such as peripheral oedema (11). and safe therapeutic alternative to dose escalation in
This study evaluated the antihypertensive effect and such patients. (17).
tolerability of the combination of amlodipine valsar- While efficacy is the prerequisite for optimal BP
tan 5 160 mg compared with amlodipine 10 mg, in control, tolerability is an important determinant of
non-responders to amlodipine 5 mg. Among those adherence to therapy and attainment of long-term
non-responders, a higher proportion achieved BP BP goals. The high incidence of peripheral oedema
control with low-dose combination therapy com- with amlodipine is because of potent arteriolar or
pared with high-dose amlodipine monotherapy (16). precapillary dilation (without dilation in the venules
2009 The Authors
Journal compilation 2009 Blackwell Publishing Ltd Int J Clin Pract, February 2009, 63, 2, 217225
224 Reduced peripheral oedema with amlodipine valsartan vs. amlodipine monotherapy
or postcapillary circulation). The resultant extravasa- patients experiencing oedema in the high-dose am-
tion of fluid into the surrounding tissue manifests as lodipine monotherapy arm, more than half resolved
peripheral oedema (8). Addition of valsartan in the after switching to amlodipine valsartan 5 160 mg.
combination dilates venous capacitance vessels with Thus, an effective alternative to amlodipine dose
consequent intracapillary pressure normalisation, escalation in patients would be a combination of
thereby minimising exudation of fluid from the low-dose amlodipine and valsartan, which has a bet-
inter-capillary space, and counteracting oedema ter antihypertensive effect than high-dose amlodipine
caused by amlodipine (14). In previous studies and a better tolerability profile.
(15,18), the combination of amlodipine and valsartan
demonstrated a lower incidence of oedema in
Acknowledgements
patients randomised to the combination. However,
in this study, much of the reduction in the incidence The authors are grateful to all participating investi-
of oedema seen with the combination is likely gators and study co-ordinators at the study centres
because of the different doses of amlodipine in the and all patients for their commitment to the study.
two arms. The authors acknowledge the assistance provided
In those patients from the high-dose amlodipine by Rosemary Jose, Ashish Agarwal and Sunita Nair
group experiencing oedema, resolution occurred in (all Novartis), in the preparation of this manu-
more than half of the cases after switching to the script.
combination. However, these data must be consid-
ered in light of the fact that significantly more
patients discontinued from the amlodipine mono- References
therapy arm during the first 8 weeks of the study,
1 Mancia G, De Backer G, Dominiczak A et al. Guidelines for the
primarily caused by peripheral oedema. This may management of arterial hypertension: the task force for the man-
have introduced a selection bias where only those agement of arterial hypertension of the European Society of
patients whose oedema was less severe continued Hypertension (ESH) and of the European Society of Cardiology
(ESC). J Hypertens 2007; 25: 110587.
into the second phase of the study and were switched
2 Ezzati M, Lopez AD, Rodgers A, Vander Hoorn S, Murray CJ.
to the combination. Thus, one might surmise that Selected major risk factors and global and regional burden of dis-
the effect would have been different and had more ease. Lancet 2002; 360: 134760.
patients experiencing oedema in the amlodipine 3 Salvetti A, Versari D. Control of blood pressure in the community:
an unsolved problem. Curr Pharm Des 2003; 9: 237584.
10 mg arm completed the study.
4 Wang YR, Alexander GC, Stafford RS. Outpatient hypertension
Aside from the lower incidence and resolution of treatment, treatment intensification, and control in Western
peripheral oedema, the overall incidence of AEs Europe and the United States. Arch Intern Med 2007; 167: 1417.
(oedema being the most frequent AE) was also lower 5 Giles TD. Rationale for combination therapy as initial treatment
for hypertension. J Clin Hypertens 2003; 5: 411.
with the amlodipine valsartan 5 160 mg combina-
6 Scholze J, Bida M, Hansen A et al. Initiation of hypertension treat-
tion than with amlodipine 10 mg. This led to many ment with a fixed-dose combination or its monocomponents
more discontinuations because of AEs with amlodi- does it really matter? Int J Clin Pract 2006; 60: 26574.
pine monotherapy than with the combination. In 7 Basile J. The role of existing and newer calcium channel blockers
in the treatment of hypertension. J Clin Hypertens (Greenwich)
addition to the added advantage of a better tolerabil- 2004; 6: 6219. quiz 30-1.
ity profile for a comparable efficacy, the administra- 8 Pedrinelli R, DellOmo G, Mariani M. Calcium channel blockers,
tion of fixed-dose combination regimen in postural vasoconstriction and dependent oedema in essential
hypertension is associated with fewer discontinua- hypertension. J Hum Hypertens 2001; 15: 45561.
9 Weir MR. Incidence of pedal edema formation with dihydropyri-
tions and better compliance than administration of dine calcium channel blockers: issues and practical significance.
two agents separately (19). Lack of discontinuation J Clin hypertens 2003; 5: 33035.
or persistence to the treatment regimen is essential 10 Corea L, Cardoni O, Fogari R et al. Valsartan, a new angiotensin
II antagonist for the treatment of essential hypertension: a compar-
for hypertension control and best clinical outcome
ative study of the efficacy and safety against amlodipine. Clin Phar-
(20). macol Ther 1996; 60: 3416.
11 Sica DA. Pharmacotherapy review: calcium channel blockers. J Clin
Hypertens (Greenwich) 2006; 8: 536.
Conclusion 12 Sica DA. Calcium channel blocker-related periperal edema: can it
be resolved? J Clin Hypertens (Greenwich) 2003; 5: 2914.
In those hypertensive patients not adequately 13 Messerli FH. Vasodilatory edema: a common side effect of antihy-
responding to amlodipine 5 mg monotherapy, the pertensive therapy. Am J Hypertens 2001; 14: 9789.
combination of amlodipine valsartan 5 160 mg 14 Kjeldsen SE, Asknes TA, de la Sierra A et al. Amlodipine and
valsartan; calcium channel blockers angiotensin II receptor block-
induces significantly lesser peripheral oedema for
ers combination for hypertension. Therapy 2007; 4: 3140.
similar BP reductions, and a better safety and tolera- 15 Philipp T, Smith TR, Glazer R et al. Two multicenter, 8-week, ran-
bility profile than amlodipine 10 mg. In addition, in domized, double-blind, placebo-controlled, parallel-group studies
2009 The Authors
Journal compilation 2009 Blackwell Publishing Ltd Int J Clin Pract, February 2009, 63, 2, 217225
Reduced peripheral oedema with amlodipine valsartan vs. amlodipine monotherapy 225
evaluating the efficacy and tolerability of amlodipine and valsartan monotherapy in patients with stage 2 hypertension: a randomized,
in combination and as monotherapy in adult patients with mild to double-blind, multicenter study: the EX-EFFeCTS study. J Am Soc
moderate essential hypertension. Clin Ther 2007; 29: 56380. Hypertens 2008; 2: 294302.
16 Andreadis EA, Tsourous GI, Marakomichelakis GE et al. High-dose 19 Wanovich R. Compliance patterns of patients treated with 2
monotherapy vs low-dose combination therapy of calcium channel separate antihypertensive agents versus fixed-dose combination
blockers and angiotensin receptor blockers in mild to moderate therapy. Am J Hypertens 2004; 17: 223A. (poster).
hypertension. J Hum Hypertens 2005; 19: 4916. 20 Halpern MT, Khan ZM, Schmier JK et al. Recommendations for
17 Bakris GL. Combined therapy with a calcium channel blocker and evaluating compliance and persistence with hypertension therapy
an angiotensin II type 1 receptor blocker. J Clin Hypertens using retrospective data. Hypertension 2006; 47: 103948.
(Greenwich) 2008; 10: 2732.
18 Destro M, Luckow A, Samson M, Kandra A, Brunel P. Efficacy
and safety of amlodipine valsartan compared with amlodipine Paper received October 2008, accepted November 2008
2009 The Authors
Journal compilation 2009 Blackwell Publishing Ltd Int J Clin Pract, February 2009, 63, 2, 217225
You might also like
- Family Satisfaction Scale (FSS) : David H. Olson, Ph.D. I. Overview of Family SatisfactionDocument9 pagesFamily Satisfaction Scale (FSS) : David H. Olson, Ph.D. I. Overview of Family SatisfactionElena BuduroiNo ratings yet
- What Is Narrative TherapyDocument10 pagesWhat Is Narrative Therapymakinwhoopie100% (3)
- Acetaminophen Drug StudyDocument2 pagesAcetaminophen Drug StudyMelissa Marie Custodio100% (3)
- Report On THE CONCEPT OF THERAPEUTIC EMPLOTMENT' 1Document33 pagesReport On THE CONCEPT OF THERAPEUTIC EMPLOTMENT' 1Jeorge M. Dela Cruz100% (1)
- Why Humanistic Psychology Lost Its Power and Influence in American PsychologyDocument25 pagesWhy Humanistic Psychology Lost Its Power and Influence in American PsychologyInan Muñoz100% (1)
- AmlodipineDocument4 pagesAmlodipineGermin CesaNo ratings yet
- Amdocal Final PDFDocument5 pagesAmdocal Final PDFSaifur Rahman SuzonNo ratings yet
- Medication 2Document181 pagesMedication 2Marin AndreiNo ratings yet
- AmlodipinaDocument2 pagesAmlodipinaCorina-Felicia BabosNo ratings yet
- Nifedipine Memo FinalDocument3 pagesNifedipine Memo FinalMike ThrowawayNo ratings yet
- PV 23 06 558Document3 pagesPV 23 06 558Komal PatelNo ratings yet
- Amlodipine-10mg TabletDocument7 pagesAmlodipine-10mg TabletMd. Abdur RahmanNo ratings yet
- LofralDocument10 pagesLofralAh BoonNo ratings yet
- Olivier Hanon MD - Laure Caillard MD - Edouard Chaussade MD - Intza Hernandorena MD - Clemence Boully MDDocument8 pagesOlivier Hanon MD - Laure Caillard MD - Edouard Chaussade MD - Intza Hernandorena MD - Clemence Boully MDVinh Quy VoNo ratings yet
- Amlodipine Uses, Side Effects & DosageDocument7 pagesAmlodipine Uses, Side Effects & DosagepatgarettNo ratings yet
- Enalapril MaleateDocument4 pagesEnalapril Maleatetaner_soysurenNo ratings yet
- Calcium Channel Blocker Formulary Review 24 June 14Document6 pagesCalcium Channel Blocker Formulary Review 24 June 14icen00bNo ratings yet
- 038 AnaphylaxisDocument5 pages038 AnaphylaxisabbuahmedibbuNo ratings yet
- Assignment, Done by Fadhl&Hadi&Hamza&Awad&AliDocument10 pagesAssignment, Done by Fadhl&Hadi&Hamza&Awad&AliFadhlNo ratings yet
- Amlodipine BesylateDocument2 pagesAmlodipine BesylateGLen CaniedoNo ratings yet
- Norvasc 5 & 10mg TabletsDocument10 pagesNorvasc 5 & 10mg TabletsasdwasdNo ratings yet
- Effect of Amlodipine Versus Felodipine Extended Release On 24-Hour Ambulatory Blood Pressure in HypertensionDocument7 pagesEffect of Amlodipine Versus Felodipine Extended Release On 24-Hour Ambulatory Blood Pressure in HypertensionKhor Chin PooNo ratings yet
- QA Amlodipine Felodipine Jan2018 FinalDocument11 pagesQA Amlodipine Felodipine Jan2018 FinalCzarina CidNo ratings yet
- Combination Therapy With Amlodipine and Captopril For Resistant Systemic HypertensionDocument4 pagesCombination Therapy With Amlodipine and Captopril For Resistant Systemic HypertensionAgus SetiawanNo ratings yet
- Randomized Evaluation of A Novel, Fixed-Dose Combination of Perindopril 3.5 Mg/amlodipine 2.5 MG As A First-Step Treatment in HypertensionDocument10 pagesRandomized Evaluation of A Novel, Fixed-Dose Combination of Perindopril 3.5 Mg/amlodipine 2.5 MG As A First-Step Treatment in HypertensionVu ChuNo ratings yet
- NCM 118B Emergency MedicationsDocument110 pagesNCM 118B Emergency MedicationsJan Crizza Dale R. Franco100% (1)
- LBL DoneDocument6 pagesLBL DoneShoaib KhatikNo ratings yet
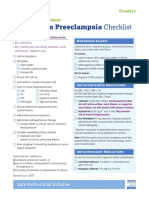
- Postpartum Preeclampsia Checklist: SafemotherhoodinitiativeDocument1 pagePostpartum Preeclampsia Checklist: SafemotherhoodinitiativeazimaNo ratings yet
- Poulter2019 Article EfficacyAndSafetyOfIncremental (1225)Document11 pagesPoulter2019 Article EfficacyAndSafetyOfIncremental (1225)Vinh Quy VoNo ratings yet
- Isoprenaline Infusion 2016Document3 pagesIsoprenaline Infusion 2016Glory Claudia KarundengNo ratings yet
- Universiti Teknologi Mara (Uitm) Puncak Alam Campus Faculty of Health SciencesDocument7 pagesUniversiti Teknologi Mara (Uitm) Puncak Alam Campus Faculty of Health SciencesMOHD MU'IZZ BIN MOHD SHUKRINo ratings yet
- O Carter Snead - 2007Document4 pagesO Carter Snead - 2007Kossay ZaouiNo ratings yet
- Group 3 5acl CML Core Prime FarmDocument29 pagesGroup 3 5acl CML Core Prime FarmAubey TanNo ratings yet
- Postpartum Preeclampsia Checklist: Emergency Department ExampleDocument1 pagePostpartum Preeclampsia Checklist: Emergency Department ExamplewijeNo ratings yet
- Text A: Transfusion ReactionDocument2 pagesText A: Transfusion ReactionSheeja JaisonNo ratings yet
- Eplerenone As A Treatment For Resistant Hypertension in PregnancyDocument4 pagesEplerenone As A Treatment For Resistant Hypertension in PregnancyLabontu IustinaNo ratings yet
- Amisulprid in SK 2Document13 pagesAmisulprid in SK 2Robert MovileanuNo ratings yet
- IvabradineDocument4 pagesIvabradineLamy SNo ratings yet
- 21 9 1034Document6 pages21 9 1034Marcela MurafaNo ratings yet
- Drug Study Analgesics AcetaminophenDocument2 pagesDrug Study Analgesics AcetaminophenGwyneth SantiagoNo ratings yet
- Drug Presentation On AminophyllineDocument10 pagesDrug Presentation On Aminophyllineelisha immanuelNo ratings yet
- Amlodipine by HamidDocument21 pagesAmlodipine by HamidShaheen UiiahNo ratings yet
- Epinephrine 1mg-ml (Adrenaline S.A.L.F. Solution For Injection I.V. S.C. I.M.)Document2 pagesEpinephrine 1mg-ml (Adrenaline S.A.L.F. Solution For Injection I.V. S.C. I.M.)asdwasdNo ratings yet
- Artigo Enviado Por Tamile - bfm.2020.0198Document3 pagesArtigo Enviado Por Tamile - bfm.2020.0198Fran MerigoNo ratings yet
- MRX Clinical Alert-April 2019Document5 pagesMRX Clinical Alert-April 2019Nattawat TeerawattanapongNo ratings yet
- A Case Report On Faropenem Induced Focal SeizuresDocument3 pagesA Case Report On Faropenem Induced Focal SeizuresInternational Journal of Innovative Science and Research Technology100% (1)
- Canine Glaucoma - Medical and Surgical Traetment OptionsDocument6 pagesCanine Glaucoma - Medical and Surgical Traetment OptionsRochiWinchesterNo ratings yet
- Flolan Drug Monograph - Munoz-3Document3 pagesFlolan Drug Monograph - Munoz-3Muhammad Muneeb KhawarNo ratings yet
- Compounded Pimobendan: FeatureDocument8 pagesCompounded Pimobendan: FeatureMadelineNo ratings yet
- Amlodipine: An Effective Once-Daily Antihypertensive Agent.: Author InformationDocument3 pagesAmlodipine: An Effective Once-Daily Antihypertensive Agent.: Author InformationIsharianto IsNo ratings yet
- Po512 Mid Fall 19 ModelDocument3 pagesPo512 Mid Fall 19 ModelDr.PharmacistNo ratings yet
- Case Presentation StrokeDocument17 pagesCase Presentation StrokeGURUPRAKASH RNo ratings yet
- Glossary and Guidelines For Use: PreparationsDocument36 pagesGlossary and Guidelines For Use: PreparationsMuhammad ThaufiqurrakhmanNo ratings yet
- Amlodipine Drug StudyDocument8 pagesAmlodipine Drug StudyChamCham Aquino75% (4)
- A Case Presentation On GLAUCOMA.Document37 pagesA Case Presentation On GLAUCOMA.Nirbhay KatiyarNo ratings yet
- Art 2Document8 pagesArt 2Brandon morenoNo ratings yet
- Vademecum MedicationsDocument19 pagesVademecum MedicationsScribdTranslationsNo ratings yet
- Reduced Versus Conventional Dose Insulin For Hyperkalemia TreatmentDocument5 pagesReduced Versus Conventional Dose Insulin For Hyperkalemia TreatmentvictorNo ratings yet
- Paracetamol - Fresenius 10mg - MLDocument3 pagesParacetamol - Fresenius 10mg - MLainia taufiqaNo ratings yet
- Efficacy and Safety of Amlodipine Versus Captopril and Their Combination Inhypertensive Urgency A Randomized Controlled Trial 2329 9126 1000274 PDFDocument7 pagesEfficacy and Safety of Amlodipine Versus Captopril and Their Combination Inhypertensive Urgency A Randomized Controlled Trial 2329 9126 1000274 PDFMaya sariNo ratings yet
- Drug Study MedicalDocument4 pagesDrug Study MedicalJoan Marie BelegaNo ratings yet
- Drug Study FinalDocument11 pagesDrug Study FinalKadymars JaboneroNo ratings yet
- Pharmacodynamic and Pharmacokinetic Modelling of Amlodipine in Feline Hypertensive PatientsDocument2 pagesPharmacodynamic and Pharmacokinetic Modelling of Amlodipine in Feline Hypertensive PatientsMartin WiniarskiNo ratings yet
- Drugs Used in Hypersensitivity Reactions: Dewi Selvina RosdianaDocument24 pagesDrugs Used in Hypersensitivity Reactions: Dewi Selvina RosdianahermanfirdausNo ratings yet
- Wing Et Al-2010-Academic Emergency MedicineDocument8 pagesWing Et Al-2010-Academic Emergency MedicinehermanfirdausNo ratings yet
- bjpg55 218Document4 pagesbjpg55 218hermanfirdausNo ratings yet
- Aspirin PpiDocument10 pagesAspirin PpihermanfirdausNo ratings yet
- Sirs and Sepsis Pasca TraumaDocument61 pagesSirs and Sepsis Pasca TraumahermanfirdausNo ratings yet
- Recognizing Clinical Reasoning ErrorsDocument20 pagesRecognizing Clinical Reasoning ErrorshermanfirdausNo ratings yet
- Long-Acting Risperidone and Oral Antipsychotics in Unstable SchizophreniaDocument29 pagesLong-Acting Risperidone and Oral Antipsychotics in Unstable SchizophreniahermanfirdausNo ratings yet
- Hecting SituasiDocument5 pagesHecting Situasihermanfirdaus100% (1)
- Mega UreterDocument27 pagesMega UreterDafne Aguilera FraustoNo ratings yet
- Chromo (Color) Therapy For Healing ChakraDocument26 pagesChromo (Color) Therapy For Healing ChakraManjari Sakhi100% (3)
- Testicular CancerDocument48 pagesTesticular Cancerluckyswiss7776848No ratings yet
- Blood Glucose MonitoringDocument19 pagesBlood Glucose MonitoringSaleha QuadsiaNo ratings yet
- Test Bank: Chapter 14: Human Immunodeficiency Virus InfectionDocument6 pagesTest Bank: Chapter 14: Human Immunodeficiency Virus InfectionJerry Varghese Thomas100% (2)
- Master Diploma in Acupressure Therapy (M.D.Acu.) Attempt Any Ten Questions All Questions Carry Equal Marks Maximum Marks - 100Document1 pageMaster Diploma in Acupressure Therapy (M.D.Acu.) Attempt Any Ten Questions All Questions Carry Equal Marks Maximum Marks - 100shabanaNo ratings yet
- Introduction and Need Results and Discussion: Harini Sowmya Narayanan, Priyanka S, Heramba GanapathyDocument1 pageIntroduction and Need Results and Discussion: Harini Sowmya Narayanan, Priyanka S, Heramba GanapathyPriyankaNo ratings yet
- Indikasi KolesistektomiDocument3 pagesIndikasi KolesistektomiwadejackNo ratings yet
- 11 94Document118 pages11 94titis dwi tantiNo ratings yet
- I Hi Trigger Tool For Measuring Adverse Drug EventsDocument16 pagesI Hi Trigger Tool For Measuring Adverse Drug EventsGaby ValenzuelaNo ratings yet
- Treatment of Erythematotelangiectatic Rosacea, Facial Erythema, and Facial Telangiectasia With A 577-nm Pro-Yellow Laser: A Case SeriesDocument6 pagesTreatment of Erythematotelangiectatic Rosacea, Facial Erythema, and Facial Telangiectasia With A 577-nm Pro-Yellow Laser: A Case Seriesdr. Amelia Budhianto AnjaniNo ratings yet
- The Use of Calcium Hydroxide, Antibiotics and Biocides As Antimicrobial Medicaments in EndodonticsDocument19 pagesThe Use of Calcium Hydroxide, Antibiotics and Biocides As Antimicrobial Medicaments in EndodonticsSudhakar NaiduNo ratings yet
- The Review of Medicines Used For Treating Diabetes: A SummaryDocument8 pagesThe Review of Medicines Used For Treating Diabetes: A SummaryAliNo ratings yet
- Prediction of Difficulty in Impacted Lower Third Molars Extraction Review LiteratureDocument10 pagesPrediction of Difficulty in Impacted Lower Third Molars Extraction Review LiteratureCiutac ŞtefanNo ratings yet
- Specimen Management in Diagnostic MicrobiologyDocument25 pagesSpecimen Management in Diagnostic Microbiologytummalapalli venkateswara raoNo ratings yet
- US Cancer Generics Market Outlook 2022Document5 pagesUS Cancer Generics Market Outlook 2022Neeraj ChawlaNo ratings yet
- nuRSING rEVIEWER PART 2Document9 pagesnuRSING rEVIEWER PART 2Johny VillanuevaNo ratings yet
- Ethical Issues in Pediatric AnesDocument16 pagesEthical Issues in Pediatric AnesrejNo ratings yet
- Guia Parala Elecci OnDocument2 pagesGuia Parala Elecci OnPaola Elizabeth CardenasNo ratings yet
- Acute Kidney InjuryDocument9 pagesAcute Kidney InjuryRobertNo ratings yet
- Meconium Aspiration SyndromeDocument41 pagesMeconium Aspiration SyndromeClara Verlina100% (2)
- Jospt 2019 8825 PDFDocument12 pagesJospt 2019 8825 PDFLuis Sepulveda PincheiraNo ratings yet
- Assessme NT Diagnosis Inference Objectives Intervention / Implementatio N Rationale EvaluationDocument1 pageAssessme NT Diagnosis Inference Objectives Intervention / Implementatio N Rationale EvaluationAlakdan TorresNo ratings yet
- PHC Citizen Charter BookDocument169 pagesPHC Citizen Charter BookParisGeronimoNo ratings yet
- Asthma OSCE Jamie TanDocument5 pagesAsthma OSCE Jamie TanAini Afifah HuzaimyNo ratings yet
- Topic Wise DNB Question BankDocument30 pagesTopic Wise DNB Question Bankritesh100% (1)