Professional Documents
Culture Documents
IT 3 - Spinal Cord Injury
IT 3 - Spinal Cord Injury
Uploaded by
Anonymous aH8gCZ7zj0 ratings0% found this document useful (0 votes)
31 views38 pagesThe document discusses spinal cord injury, including anatomy, causes, classifications, clinical manifestations, and management. It describes the ascending and descending tracts, differences between upper and lower motor neuron injuries, and classifications of spinal cord injuries as complete or incomplete. Clinical manifestations vary depending on the level and degree of injury. Initial management focuses on immobilization, preventing hypotension, and maintaining oxygenation.
Original Description:
IT
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThe document discusses spinal cord injury, including anatomy, causes, classifications, clinical manifestations, and management. It describes the ascending and descending tracts, differences between upper and lower motor neuron injuries, and classifications of spinal cord injuries as complete or incomplete. Clinical manifestations vary depending on the level and degree of injury. Initial management focuses on immobilization, preventing hypotension, and maintaining oxygenation.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
0 ratings0% found this document useful (0 votes)
31 views38 pagesIT 3 - Spinal Cord Injury
IT 3 - Spinal Cord Injury
Uploaded by
Anonymous aH8gCZ7zjThe document discusses spinal cord injury, including anatomy, causes, classifications, clinical manifestations, and management. It describes the ascending and descending tracts, differences between upper and lower motor neuron injuries, and classifications of spinal cord injuries as complete or incomplete. Clinical manifestations vary depending on the level and degree of injury. Initial management focuses on immobilization, preventing hypotension, and maintaining oxygenation.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
You are on page 1of 38
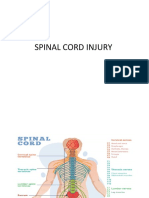
Spinal Cord Injury
Anugrah onie w, dr, Neurosurgeon
Basic Anatomy and Physiology
What is the anatomy of the spinal cord on
cross section?
What is the anatomy of the spinal cord on
cross section?
What are the clinically important ascending tracts and where do they
cross over?
What are the clinically important descending tracts and where do they
cross over?
At what level does the spinal cord end and
why is it important?
What are the differences between UMN and LMN? (e.g., cauda equina
vs. myelopathy)
Spinal Cord Injuries
Whos at risk?
ADULT MEN BETWEEN 15 AND 30 YEARS
Anyone in a risk-taking occupation or lifestyle
SCI in older clients increasing largely due to MVAs
Spinal Cord Injuries
Causes (in order of frequency)
MVA
Gunshot wounds/acts of violence
Falls
Sports injuries
Spinal and Neurogenic Shock
Below site of injury:
Total lack of function
Decreased or absent reflexes and flaccid paralysis
Lasts from a week to several months after onset.
End of spinal shock signaled by muscular spasticity, reflex
bladder emptying, hyperreflexia
What is the difference between spinal shock
and neurogenic shock?
Spinal shock is mainly a loss of reflexes (flaccid paralysis)
Neurogenic shock is mainly hypotension and bradycardia due
to loss of sympathetic tone
Neurogenic shock
Seen in cervical injuries
Due to interruption of the sympathetic input from
hypothalamus to the cardiovascular centers
Hallmark: hypotension (due to vasodilation, due to loss of
sympathetic tonic input) is associated with bradycardia (not
tachycardia, the usual response), due to inability to convey
the information to the vasomotor centers in the spinal cord
Classification of SCI
Mechanism of injury
Flexion (bending forward)
Hyperextension (backward)
Rotation (either flexion- or extension-rotation)
Compression (downward motion)
Pathophysiology
of SCI
Classification of SCI
Level or Injury
Cervical (C-1 through ??)
Thoracic (T-1through ??)
Lumbar (L-1through ??)
Degree of Injury
Complete
Total paralysis and loss of sensory and motor function
although arms or rarely completely paralyzed
Incomplete or partial
Motor: how do you test each segment?
Motor: how do you grade the strength?
Sensory: how do you determine the level?
What are the important vegetative functions
and when are they affected?
Reflexes
Deep Tendon Reflexes
Arm
Bicipital: C5
Styloradial: C6
Tricipital: C7
Leg
Patellar: L3, some L4
Achilles: S1
Pathological reflexes
Babinski (UMN lesion)
Hoffman (UMN lesion at or above cervical spinal cord)
Clonus (plantar or patellar) (long standing UMN lesion)
What is and how do you determine the level
of injury?
Motor level = the last level with at least 3/5
(against gravity) function
NB: this is the most important for clinical purposes
Sensory level = the last level with preserved
sensation
Radiographic level = the level of fracture on plain
XRays / CT scan / MRI
NB: spine level does not correspond to spinal cord
level below the cervical region
Degree of Injury
Complete transection
Total paralysis and loss of sensory and motor function
although arms or rarely completely paralyzed
Incomplete (partial transection)
Mixed loss of voluntary motor activity and sensation
Four patterns or syndromes
Incomplete cord patterns
Insert picture of cord here
Central cord syndrome More common in older
clients
Frequently from hyperextension of spine
Weakness in upper and lower ext, but greater in upper.
Anterior cord syndrome
Posterior cord syndrome
Brown-Sequard syndrome
Anterior cord syndrome
Compression of the ant. Cord, usually a flexion injury
Sudden, complete motor paralysis at lesion and below;
decreased sensation (including pain) and loss of
temperature sensation below site.
Touch, position, vibration and motion remain intact.
Posterior cord syndrome
Assoc with cervical hyperextension injuries
Dorsal area of cord is damaged resulting in loss of
proprioception
Pain, temperature sensation and motor function remain
intact.
Brown-Sequard syndrome
Damage to one half of the cord on either side.
Caused by penetrating trauma or ruptured disk.
ischemia (obstruction of a blood vessel), or infectious
or inflammatory diseases such as tuberculosis, or
multiple sclerosisBSS may be caused by a spinal cord
tumor, trauma (such as a puncture wound to the neck
or back),.
a rare SCI syndrome which results in
weakness or paralysis (hemiparaplegia) on one side of the
body and
a loss of sensation (hemianesthesia) on the opposite side.
Clinical manifestations of SCI
Depend on the LEVEL and DEGREE of the injury!
Quadriplegia occurs with C-1 through
C-8 injuries.
Paraplegia occurs with T-1 thru L-4.
SEE TABLE 57-3 ON PAGE 1725!
Clinical Manifestations of SCI
Respiratory
C1 C3: Absence of ability to breathe independently.
C4 poor cough, diaphragmatic breathing,
hypoventilation
C5 T6: decreased respiratory reserve
T6 or T7 L4: functional respiratory system with adequate
reserve.
Initial Management
Immobilization
Rigid collar
Sandbags and straps
Spine board
Log-roll to turn
Prevent hypotension
Pressors: Dopamine, not Neosynephrine
Fluids to replace losses; do not overhydrate
Maintain oxygenation
O2 per nasal canula
If intubation is needed, do NOT move the neck
Management in the hospital
NGT to suction
Prevents aspiration
Decompresses the abdomen (paralytic ileus is
common in the first days)
Foley
Urinary retention is common
Methylprednisolone (Solu-Medrol)
Only if started within 8 hours of injury
Exclusion criteria
Cauda equina syndrome
GSW
Pregnancy
Age <13 years
Patient on maintenance steroids
You might also like
- Harga Perkiraan Sendiri Pengadaan Obat JKN 2023Document1 pageHarga Perkiraan Sendiri Pengadaan Obat JKN 2023Farah BestanisaNo ratings yet
- Safety Data Sheet: Magiclean For Professional (Antibacterial) : Product NameDocument6 pagesSafety Data Sheet: Magiclean For Professional (Antibacterial) : Product NameFerryTimothyNo ratings yet
- Spine and Spinal Cord InjuryDocument39 pagesSpine and Spinal Cord InjuryblackcatNo ratings yet
- Polytrauma, ABC of Trauma & Its ManagementDocument33 pagesPolytrauma, ABC of Trauma & Its ManagementMongolian MutuNo ratings yet
- G02-Assessment, Management and Decision Making in The Treatment of Polytrauma Patients With Head InjuriesDocument42 pagesG02-Assessment, Management and Decision Making in The Treatment of Polytrauma Patients With Head InjuriesAbdirizak SheikdonNo ratings yet
- CME Spinal Cord InjuryDocument49 pagesCME Spinal Cord InjuryEllappa GhanthanNo ratings yet
- Spinal Cord Injuries: Gabriel C. Tender, MDDocument49 pagesSpinal Cord Injuries: Gabriel C. Tender, MDCathyCarltonNo ratings yet
- Spinal Cord Injuries: Gabriel C. Tender, MDDocument49 pagesSpinal Cord Injuries: Gabriel C. Tender, MDGatotNo ratings yet
- Spinal Cord InjuriesDocument49 pagesSpinal Cord Injuriesjustin_saneNo ratings yet
- Spinal Cord InjuryDocument49 pagesSpinal Cord InjuryIis Rica MustikaNo ratings yet
- Spinal Cord InjuryDocument37 pagesSpinal Cord InjuryCanz PamateNo ratings yet
- 1 Materi Kuliah Spine, Dr. AzharuddinDocument59 pages1 Materi Kuliah Spine, Dr. AzharuddinfazliahNo ratings yet
- Spinal Injury1Document37 pagesSpinal Injury1Selam Tesfaye ShebaNo ratings yet
- Spinal Cord InjuryDocument47 pagesSpinal Cord InjuryShitaljit IromNo ratings yet
- Spinal Cord Injuries Anatomy & Pathophysiology: JckingDocument51 pagesSpinal Cord Injuries Anatomy & Pathophysiology: JckingSatyaRandyNo ratings yet
- Spinal Cord InjuryDocument90 pagesSpinal Cord Injurymuthuu0% (1)
- SCI (Spinal Cord Injury)Document51 pagesSCI (Spinal Cord Injury)Awal AlfitriNo ratings yet
- Spinal Cord InjuriesDocument51 pagesSpinal Cord Injurieswanglee2000No ratings yet
- Spinal Cord Injury: by Muhammad SulimanDocument40 pagesSpinal Cord Injury: by Muhammad SulimanYou TuberNo ratings yet
- Spinal Cord InjuryDocument17 pagesSpinal Cord InjuryPrincess Gutierrez RositaNo ratings yet
- Traumatic Spinal Cord InjuriesDocument28 pagesTraumatic Spinal Cord Injuriesbibi bennyNo ratings yet
- Trauma To Cervical Spine & Thoracolumbar SpineDocument52 pagesTrauma To Cervical Spine & Thoracolumbar SpineVel AnandhanNo ratings yet
- Nice Cap SciDocument46 pagesNice Cap SciDyah SafitriNo ratings yet
- Spinal Cord InjuriesDocument31 pagesSpinal Cord Injuriesmariam bassemNo ratings yet
- Trauma Spinal: DR Bambang Priyanto, SpbsDocument64 pagesTrauma Spinal: DR Bambang Priyanto, Spbsbaiq niningNo ratings yet
- Clinical Anatomy, Trauma of The Upper ExDocument103 pagesClinical Anatomy, Trauma of The Upper ExNeil Vincent De AsisNo ratings yet
- Spinal Cord Injury, DisordersDocument54 pagesSpinal Cord Injury, DisordersChananNo ratings yet
- Spinal TraumaDocument45 pagesSpinal TraumaSaminu JabirNo ratings yet
- Trauma and Brain InjuryDocument48 pagesTrauma and Brain Injurya20-0353-958No ratings yet
- Ahn PresentationDocument23 pagesAhn Presentationsceince with EZNo ratings yet
- Kuliah Spine TraumaDocument91 pagesKuliah Spine Traumatutor tujuhNo ratings yet
- Lecture 6 Spinal Cord InjuriesDocument26 pagesLecture 6 Spinal Cord InjuriesMahroosh KhanNo ratings yet
- Spinal Traumas: Fisseha G (MD)Document63 pagesSpinal Traumas: Fisseha G (MD)mubarek nesiroNo ratings yet
- Spinal Trauma: Oleh: Winda Arista HaeriyokoDocument33 pagesSpinal Trauma: Oleh: Winda Arista HaeriyokoWinda HaeriyokoNo ratings yet
- 9 Orthopaedic EmergenciesDocument68 pages9 Orthopaedic EmergenciesAndrew WdsmithNo ratings yet
- 1-Acute Spinal Cord Trauma-1Document49 pages1-Acute Spinal Cord Trauma-1fathanrasyidNo ratings yet
- Trauma Spinal Wates Dr. WRDocument68 pagesTrauma Spinal Wates Dr. WRLanlan LesmanaNo ratings yet
- Trauma Lecture 7Document61 pagesTrauma Lecture 7The bella GirlNo ratings yet
- 5 7 06spinalinjDocument32 pages5 7 06spinalinjJon Wafa AzwarNo ratings yet
- Lec6 - Spinal Cord InjuryDocument18 pagesLec6 - Spinal Cord Injuryمحمد قاسمNo ratings yet
- Spine Fractures and Spinal Cord InjuryDocument54 pagesSpine Fractures and Spinal Cord InjuryAloy PudeNo ratings yet
- Spinal Cord DisordersDocument50 pagesSpinal Cord DisordersIsaac Mwangi100% (1)
- Diseases of Spine andDocument37 pagesDiseases of Spine andgunawan djayaNo ratings yet
- Lecture 5 Shoulder and Elbow Orthopedics-1Document52 pagesLecture 5 Shoulder and Elbow Orthopedics-1mukhtar abddi100% (1)
- Kuliah Spine TraumaDocument91 pagesKuliah Spine TraumaEvi MaisyariNo ratings yet
- Rehabilitation of Spinal Cord InjuryDocument23 pagesRehabilitation of Spinal Cord InjuryConcepcion R. AquinoNo ratings yet
- Cervical Spine InjuriesDocument50 pagesCervical Spine InjuriesgamalramadiNo ratings yet
- NeckDocument67 pagesNeckdr_asaleh100% (1)
- Spinal Cord: Austin Penman Stephen Newell Logan Su Marissa SmallwoodDocument25 pagesSpinal Cord: Austin Penman Stephen Newell Logan Su Marissa SmallwoodEyzan Rashid NorieyNo ratings yet
- Sports Medicine (Elbow and Spinal Injuries) InjuriesDocument73 pagesSports Medicine (Elbow and Spinal Injuries) InjuriesnhfbyqvgwhNo ratings yet
- Head and Neck Trauma Board ReviewDocument65 pagesHead and Neck Trauma Board Reviewrigo montejoNo ratings yet
- Peripheral Nerve DisordersDocument75 pagesPeripheral Nerve DisordersAllahbesertkitaNo ratings yet
- Spinal Cord Injury: Barrios, Kevin George BDocument52 pagesSpinal Cord Injury: Barrios, Kevin George B乔治凯文No ratings yet
- Spine Emergencies: Spinal Cord Injury (SCI) - The BasicsDocument67 pagesSpine Emergencies: Spinal Cord Injury (SCI) - The Basicsditya_madridistasNo ratings yet
- 23 Emergency in SportmedicineDocument46 pages23 Emergency in SportmedicineDhia UlfajriNo ratings yet
- Management of Back Pain in AdultsDocument41 pagesManagement of Back Pain in AdultsMadhusree GhoshNo ratings yet
- Whiplash Injury Spondylosis, Spondolysis and SpondylolisthesisDocument58 pagesWhiplash Injury Spondylosis, Spondolysis and SpondylolisthesistoobaNo ratings yet
- StrokeDocument58 pagesStrokeMarah AbdulrahimNo ratings yet
- Spinal Deformities NewDocument79 pagesSpinal Deformities Newapi-26159412100% (3)
- Syndromes of Spinal Cord: Dr.A.Meenakshi Prof.S.Tito'S Unit M6Document32 pagesSyndromes of Spinal Cord: Dr.A.Meenakshi Prof.S.Tito'S Unit M6NinaNo ratings yet
- Orthopedic Examination - a Step by Step Guide: Black and White PrintFrom EverandOrthopedic Examination - a Step by Step Guide: Black and White PrintNo ratings yet
- Daftar Obat Puskes MerdekaDocument2 pagesDaftar Obat Puskes MerdekaAnonymous aH8gCZ7zjNo ratings yet
- 3 Shift: Pola 3 Hari Masuk 1 Hari Libur + Max. 40 Jam/mingguDocument4 pages3 Shift: Pola 3 Hari Masuk 1 Hari Libur + Max. 40 Jam/mingguAnonymous aH8gCZ7zjNo ratings yet
- Research Article: Characterization of Pediatric Acute Lymphoblastic Leukemia Survival Patterns by Age at DiagnosisDocument10 pagesResearch Article: Characterization of Pediatric Acute Lymphoblastic Leukemia Survival Patterns by Age at DiagnosisAnonymous aH8gCZ7zjNo ratings yet
- Case HemoroidDocument19 pagesCase HemoroidAnonymous aH8gCZ7zjNo ratings yet
- ID Hubungan Faktor Resiko Dengan Terjadinya Nyeri Punggung Bawah Low Back Pain Pada PDFDocument10 pagesID Hubungan Faktor Resiko Dengan Terjadinya Nyeri Punggung Bawah Low Back Pain Pada PDFAnonymous aH8gCZ7zjNo ratings yet
- Excercise 2 - Frequency MeasureDocument6 pagesExcercise 2 - Frequency MeasureAnonymous aH8gCZ7zj75% (4)
- Thorax and Lungs Physical Assessment Includes InspectionDocument9 pagesThorax and Lungs Physical Assessment Includes InspectionwiwinNo ratings yet
- Jurnal RespiDocument5 pagesJurnal RespiNurul Huda KowitaNo ratings yet
- Edukasi Corona Virus Desease 19 (Covid-19) Melalui Penyebaran Poster Kepada Masyarakat Kecamatan Slawi Kabupaten TegalDocument10 pagesEdukasi Corona Virus Desease 19 (Covid-19) Melalui Penyebaran Poster Kepada Masyarakat Kecamatan Slawi Kabupaten TegalJariyah AmiliaNo ratings yet
- Society For Obesity and Bariatric Anaesthesia: OS-MRS Calculator Tools - Farmacologiaclinica.infoDocument1 pageSociety For Obesity and Bariatric Anaesthesia: OS-MRS Calculator Tools - Farmacologiaclinica.infoHizami Norddin100% (2)
- Pre & Post Operative TracheostomyDocument2 pagesPre & Post Operative TracheostomyHantu Kak Limah100% (2)
- Material Safety Data Sheet: 1. Chemical Product / Company InformationDocument5 pagesMaterial Safety Data Sheet: 1. Chemical Product / Company InformationM.FAIZAN ARSHADNo ratings yet
- RefranceDocument13 pagesRefranceNoor Hasan WaheedNo ratings yet
- Activity 1.1 Science 9Document2 pagesActivity 1.1 Science 9Crzy TiffNo ratings yet
- ACM608BDocument1 pageACM608BSoporte VitalNo ratings yet
- Aeon7200: Anaesthesia MachineDocument2 pagesAeon7200: Anaesthesia Machineok centralNo ratings yet
- Noccarc V310+ BiFold Brochure V9.0 1Document4 pagesNoccarc V310+ BiFold Brochure V9.0 1Tushar AgarwalNo ratings yet
- Luisa: VentilatorsDocument42 pagesLuisa: VentilatorsSalman SaeedNo ratings yet
- InnAccel - VapCare - NH Covid StudyDocument15 pagesInnAccel - VapCare - NH Covid Studyemailtrinaya30No ratings yet
- Cough ConversationDocument2 pagesCough ConversationWindy Viiantari100% (1)
- Abg Practice QuizDocument13 pagesAbg Practice QuizPatty Romero0% (1)
- Jose P. Laurel Sr. High School: Department of Education Schools Division Office-Quezon CityDocument7 pagesJose P. Laurel Sr. High School: Department of Education Schools Division Office-Quezon CityEricha SolomonNo ratings yet
- El Ganzouri 2Document7 pagesEl Ganzouri 2Tamin SamudaNo ratings yet
- Learners Material Module 1 Respiratory ADocument27 pagesLearners Material Module 1 Respiratory AJelly FloresNo ratings yet
- SikaQuick 2500 Patch IdDocument3 pagesSikaQuick 2500 Patch IdRialno TambunanNo ratings yet
- The Autopsy of Jane DoeDocument23 pagesThe Autopsy of Jane Doejb.ortizrodriguesNo ratings yet
- Seven Ps For RSI BOARDDocument2 pagesSeven Ps For RSI BOARDJames BrownNo ratings yet
- Week 8 Respiratory System Weekly Workbook 2022Document22 pagesWeek 8 Respiratory System Weekly Workbook 2022rishabhvasisht03No ratings yet
- Brazilian Recommendations of Mechanical Ventilation: Recomendações Brasileiras de Ventilação Mecânica 2013. Parte 2Document25 pagesBrazilian Recommendations of Mechanical Ventilation: Recomendações Brasileiras de Ventilação Mecânica 2013. Parte 2Renata Araújo Borges XavierNo ratings yet
- Aerosol in The Oral Health Care Setting: A Misty Topic: Fridus Van Der WeijdenDocument10 pagesAerosol in The Oral Health Care Setting: A Misty Topic: Fridus Van Der WeijdenkhamilatusyNo ratings yet
- Bls Class CPR Power PointDocument45 pagesBls Class CPR Power Point2020 MSc bhuvaneswari 05100% (1)
- WBC-1622-01 SL XLC N Black No 9 Ikea Dof CRBDocument4 pagesWBC-1622-01 SL XLC N Black No 9 Ikea Dof CRBFindora InternusaNo ratings yet
- Health and Illness British English Student PDFDocument3 pagesHealth and Illness British English Student PDFNuria ReyesNo ratings yet
- Sulfur Hexafluoride sf6 Safety Data Sheet Sds p4657Document9 pagesSulfur Hexafluoride sf6 Safety Data Sheet Sds p4657Terkel GinaNo ratings yet