Professional Documents
Culture Documents
Long-Term Efficacy of House Dust Mite Immunotherapy in Bronchial Asthma: A 15-Year Follow-Up Study
Long-Term Efficacy of House Dust Mite Immunotherapy in Bronchial Asthma: A 15-Year Follow-Up Study
Uploaded by
Nicole SierraCopyright:
Available Formats
You might also like
- Adenotonsillitis NewDocument100 pagesAdenotonsillitis NewDrravikumar Bhandari100% (1)
- Catgutpuntura Rinitis AlérgicaDocument11 pagesCatgutpuntura Rinitis AlérgicaDubichelNo ratings yet
- Evaluation of Antibiotic Sensitivity Pattern in Acute TonsillitisDocument5 pagesEvaluation of Antibiotic Sensitivity Pattern in Acute TonsillitisyoanaNo ratings yet
- Sublingual Immunotherapy To House Dust Mite in Pediatric Patients With Allergic Rhinitis and Asthma: A Retrospective Analysis of Clinical Course Over A 3-Year Follow-Up PeriodDocument4 pagesSublingual Immunotherapy To House Dust Mite in Pediatric Patients With Allergic Rhinitis and Asthma: A Retrospective Analysis of Clinical Course Over A 3-Year Follow-Up PeriodPeter SalimNo ratings yet
- 12erny (Full Permission)Document15 pages12erny (Full Permission)Peter SalimNo ratings yet
- 895 902 1 PB PDFDocument5 pages895 902 1 PB PDFBadai Ardyana PutriNo ratings yet
- A Randomised Dose-Ranging Study of Tiotropium Respimat® in Children With Symptomatic Asthma Despite Inhaled CorticosteroidsDocument10 pagesA Randomised Dose-Ranging Study of Tiotropium Respimat® in Children With Symptomatic Asthma Despite Inhaled CorticosteroidsabdmaliknasNo ratings yet
- Atopic Dermatitis and Vegan DietDocument9 pagesAtopic Dermatitis and Vegan DietIuliu Ciupe-VaidaNo ratings yet
- Typhoid Fever Vaccines: A Meta-Analysis of Studies On Efficacy and ToxicityDocument7 pagesTyphoid Fever Vaccines: A Meta-Analysis of Studies On Efficacy and ToxicityYudha AkihiroNo ratings yet
- Clinical Presentation and Laboratory Features in Pediatric Typhoid Fever Patient Susceptibility To First-Line Antibiotic TherapyDocument10 pagesClinical Presentation and Laboratory Features in Pediatric Typhoid Fever Patient Susceptibility To First-Line Antibiotic TherapySuci ZahraniNo ratings yet
- Nutrients 10 01678Document11 pagesNutrients 10 01678zulfa nadiaNo ratings yet
- Evidence Based Medicine - CONSORT & AppraisalDocument52 pagesEvidence Based Medicine - CONSORT & AppraisalNurul Aulia AbdullahNo ratings yet
- Ayu Ijpsr14-05-01-001Document9 pagesAyu Ijpsr14-05-01-001Listiani AyuNo ratings yet
- Prevalence of Allergic Rhinitis Symptoms and Positive Skin Prick Test Results in Children With Recurrent EpistaxisDocument6 pagesPrevalence of Allergic Rhinitis Symptoms and Positive Skin Prick Test Results in Children With Recurrent EpistaxisKevinFeraldyNo ratings yet
- Universitas Indonesia: U. Weber, M. Krammel, S. Linke, T. Hamp, T. Stimpfl, B. Reiter, W. PlӧchlDocument8 pagesUniversitas Indonesia: U. Weber, M. Krammel, S. Linke, T. Hamp, T. Stimpfl, B. Reiter, W. PlӧchlgoldenNo ratings yet
- High-Dose Versus Standard-Dose Amoxicillin/ Clavulanate For Clinically-Diagnosed Acute Bacterial Sinusitis: A Randomized Clinical TrialDocument15 pagesHigh-Dose Versus Standard-Dose Amoxicillin/ Clavulanate For Clinically-Diagnosed Acute Bacterial Sinusitis: A Randomized Clinical TrialHendra EfendiNo ratings yet
- Typhoid JournalDocument7 pagesTyphoid JournalRegina AyediaNo ratings yet
- Prosiding Seminar Nasional Dan Workshop "Perkembangan Terkini Sains Farmasi Dan Klinik IV" Tahun 2014Document7 pagesProsiding Seminar Nasional Dan Workshop "Perkembangan Terkini Sains Farmasi Dan Klinik IV" Tahun 2014IdafabdullahNo ratings yet
- Effectiveness of Low Dose Immunotherapy in The Treatment of Canine Atopic Dermatitis - A Prospective, Double-Blinded, Clinical Study (Document9 pagesEffectiveness of Low Dose Immunotherapy in The Treatment of Canine Atopic Dermatitis - A Prospective, Double-Blinded, Clinical Study (jenNo ratings yet
- Radioiodine TherapyDocument5 pagesRadioiodine Therapyaccime24No ratings yet
- Ebm SeptemberDocument29 pagesEbm SeptemberJulius OentarioNo ratings yet
- Dog Allergen Immunotherapy: Past, Present, and Future: Derek M. Smith, MD and Christopher A. Coop, MDDocument6 pagesDog Allergen Immunotherapy: Past, Present, and Future: Derek M. Smith, MD and Christopher A. Coop, MDbrakim23No ratings yet
- Gabapentin For Refractory Chronic Cough: A Randomised, Double-Blind, Placebo-Controlled TrialDocument8 pagesGabapentin For Refractory Chronic Cough: A Randomised, Double-Blind, Placebo-Controlled TrialIAmILoNo ratings yet
- SII, FODMAPS e Hormonios EndócrinosDocument7 pagesSII, FODMAPS e Hormonios Endócrinosmari bNo ratings yet
- Prof Iwin - Asit Course Final Method and Its Eval Exp 30' JKT Feb 08Document79 pagesProf Iwin - Asit Course Final Method and Its Eval Exp 30' JKT Feb 08nick_mdNo ratings yet
- Jurnal Reading OtomikosisDocument4 pagesJurnal Reading OtomikosisTria JuwitaNo ratings yet
- Journal of EthnopharmacologyDocument5 pagesJournal of EthnopharmacologypipisoseticaNo ratings yet
- Perbedaan Imunoterapi Alergen Spesifik (ITS) Dengan Vaksinasi BCG Dalam Meningkatkan Kualitas Hidup Penderita Rinitis AlergiDocument12 pagesPerbedaan Imunoterapi Alergen Spesifik (ITS) Dengan Vaksinasi BCG Dalam Meningkatkan Kualitas Hidup Penderita Rinitis AlergiThya Alif KahfNo ratings yet
- A Placebo-Controlled Trial of Antimicrobial Treatment For Acute Otitis MediaDocument6 pagesA Placebo-Controlled Trial of Antimicrobial Treatment For Acute Otitis MediaegieprajaNo ratings yet
- Allergen Immunotherapy Expert ExchangeDocument4 pagesAllergen Immunotherapy Expert ExchangeAnna LiachenkoNo ratings yet
- Indacaterol Provides 24-Hour Bronchodilation in COPD: A Placebo-Controlled Blinded Comparison With TiotropiumDocument8 pagesIndacaterol Provides 24-Hour Bronchodilation in COPD: A Placebo-Controlled Blinded Comparison With TiotropiumCalca NeusNo ratings yet
- A Nationwide Survey of Inhalant Allergens Sensitization and Levels of Indoor Major Allergens in KoreaDocument6 pagesA Nationwide Survey of Inhalant Allergens Sensitization and Levels of Indoor Major Allergens in KoreaRatna WindyaningrumNo ratings yet
- Veterinary Dermatology - 2021 - MuellerDocument20 pagesVeterinary Dermatology - 2021 - MuellerMandycat75No ratings yet
- Jurnal Sidang RespiDocument4 pagesJurnal Sidang RespiAnis Eka SukmadadariNo ratings yet
- 14 2011-14-Ajmr Isn 2011Document5 pages14 2011-14-Ajmr Isn 2011Dr. Taha NazirNo ratings yet
- Dry Needling in Lateral Epicondylitis A Prospective EBP PDFDocument5 pagesDry Needling in Lateral Epicondylitis A Prospective EBP PDFDanielle Denice LacabaNo ratings yet
- 2011 Article 437Document6 pages2011 Article 437AlexandraParedesPuertaNo ratings yet
- Insulin Allergy Can Be Successfully Managed by A Systematic ApproachDocument6 pagesInsulin Allergy Can Be Successfully Managed by A Systematic Approachjames antonyNo ratings yet
- Jurnal AsmaDocument12 pagesJurnal AsmaaulNo ratings yet
- Sublingual ImmunotherapyDocument4 pagesSublingual ImmunotherapyAnonymous eZqDZbObRiNo ratings yet
- Cea 13169 PDFDocument15 pagesCea 13169 PDFrisanataliasiburianNo ratings yet
- Super 1st Draft 1Document10 pagesSuper 1st Draft 1iNeimoNo ratings yet
- 276 Jaipal Singh VishwakarmaDocument8 pages276 Jaipal Singh Vishwakarmashubh1511No ratings yet
- Jurnal 2Document9 pagesJurnal 2dewi trisnawatiNo ratings yet
- Lo Han Guo FruitDocument9 pagesLo Han Guo FruitInten KusumaNo ratings yet
- Use of Superoxide Dismutase in Accelerating Symptom PDFDocument7 pagesUse of Superoxide Dismutase in Accelerating Symptom PDFWilliam JavierNo ratings yet
- Efikasi AzitromisinDocument4 pagesEfikasi AzitromisinNadia DesiNo ratings yet
- General Practice: Are Antibiotics Indicated As Initial Treatment For Children With Acute Otitis Media? A Meta-AnalysisDocument5 pagesGeneral Practice: Are Antibiotics Indicated As Initial Treatment For Children With Acute Otitis Media? A Meta-AnalysisJuan Carlos Aguayo RomeroNo ratings yet
- The Clinical Effect of Erdosteine On Acute Respiratory Tract Diseases in ChildrenDocument17 pagesThe Clinical Effect of Erdosteine On Acute Respiratory Tract Diseases in ChildrenResha Adriana PuttyNo ratings yet
- Aom PDFDocument13 pagesAom PDFiyan rNo ratings yet
- Jurnal AsthmaDocument11 pagesJurnal AsthmaNadira Juanti PratiwiNo ratings yet
- REITHINGERCID2055Document8 pagesREITHINGERCID2055Wulan YuwitaNo ratings yet
- Moxifloxaxin For CAPDocument9 pagesMoxifloxaxin For CAPmateri posNo ratings yet
- A Comparison of Oral Procaterol and Albuterol in Reversible Airflow ObstructionDocument6 pagesA Comparison of Oral Procaterol and Albuterol in Reversible Airflow Obstructionparris shanyNo ratings yet
- Pengobatan Pyomentra Dengan AglepristoneDocument7 pagesPengobatan Pyomentra Dengan AglepristoneraldyNo ratings yet
- All Questions To Be Answered. Each Question To Be Answered in A Separate Book (Or Books If More Than One Is Required For The One Answer)Document3 pagesAll Questions To Be Answered. Each Question To Be Answered in A Separate Book (Or Books If More Than One Is Required For The One Answer)matentenNo ratings yet
- IJP - Volume 8 - Issue 9 - Pages 11939-11944Document6 pagesIJP - Volume 8 - Issue 9 - Pages 11939-11944A'la Nur RoyanNo ratings yet
- Garlic (Allium sativum): Monograph on a herb reputed to be medicinalFrom EverandGarlic (Allium sativum): Monograph on a herb reputed to be medicinalNo ratings yet
- Complementary and Alternative Medical Lab Testing Part 5: GastrointestinalFrom EverandComplementary and Alternative Medical Lab Testing Part 5: GastrointestinalNo ratings yet
- Complementary and Alternative Medical Lab Testing Part 2: RespiratoryFrom EverandComplementary and Alternative Medical Lab Testing Part 2: RespiratoryNo ratings yet
- 22 Varicella Pink BookDocument24 pages22 Varicella Pink BookMohamad Syaikhul IslamNo ratings yet
- Eucast Discussion Document E.Dis 5.1 March 2003 Determination of Minimum Inhibitory Concentrations (Mics) of Antibacterial Agents by Broth DilutionDocument7 pagesEucast Discussion Document E.Dis 5.1 March 2003 Determination of Minimum Inhibitory Concentrations (Mics) of Antibacterial Agents by Broth DilutionPankajNo ratings yet
- Swine FluDocument4 pagesSwine FluDarwotoNo ratings yet
- Donor Selections..Document17 pagesDonor Selections..OmamaNo ratings yet
- Basic Manual For Free Range Colored Broilers Production PDFDocument12 pagesBasic Manual For Free Range Colored Broilers Production PDFAndy LimNo ratings yet
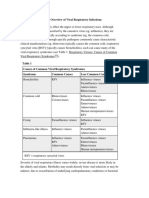
- 1 - Overview of Viral Respiratory InfectionsDocument3 pages1 - Overview of Viral Respiratory Infectionssapik zirafNo ratings yet
- Complete Abstract Book ASTMH - Atlanta 2012-USADocument3 pagesComplete Abstract Book ASTMH - Atlanta 2012-USAPercy Lezama VigoNo ratings yet
- Contractor UPM Weekly HSE Submittal Rev 01 - OMPPD 2024 WEEK-3Document10 pagesContractor UPM Weekly HSE Submittal Rev 01 - OMPPD 2024 WEEK-3Rolando MarceloNo ratings yet
- Commercial Chicken Vaccination Part 3 Injectable AdministrationDocument6 pagesCommercial Chicken Vaccination Part 3 Injectable AdministrationAnjum IslamNo ratings yet
- Rubella: Lilian B - Rosario, MD, FPPSDocument19 pagesRubella: Lilian B - Rosario, MD, FPPSRiya KayarkarNo ratings yet
- 05 Introduction To Plant PathologyDocument20 pages05 Introduction To Plant PathologyirwanpaluNo ratings yet
- Sci Chapter 2 8thDocument18 pagesSci Chapter 2 8thAakash ChatakeNo ratings yet
- Care of The Older or Disabled AdultDocument63 pagesCare of The Older or Disabled Adultfairwoods100% (1)
- Health Programme Manager's Manual PDFDocument140 pagesHealth Programme Manager's Manual PDFLakshmi SethNo ratings yet
- OJAP Summary Major EventsDocument6 pagesOJAP Summary Major EventsReid KirbyNo ratings yet
- Disinfectant Efficacy StudyDocument63 pagesDisinfectant Efficacy Studydeepanshsharma100% (2)
- K. Kapita Selekta-Farmakologi (DR - Astrianda)Document13 pagesK. Kapita Selekta-Farmakologi (DR - Astrianda)Nela LutfianaNo ratings yet
- Bat in Watertown Reported To Have RabiesDocument1 pageBat in Watertown Reported To Have RabiesNewzjunkyNo ratings yet
- RMS Case Study (Leptospirosis) GRP 1 BSTM 1-B FinalDocument12 pagesRMS Case Study (Leptospirosis) GRP 1 BSTM 1-B FinalLauren Abas Dela CruzNo ratings yet
- Course 9 - VC225ILR - UsageDocument7 pagesCourse 9 - VC225ILR - UsageDulasNo ratings yet
- Analytic Guide For Assessing Vaccination Coverage Using An IISDocument42 pagesAnalytic Guide For Assessing Vaccination Coverage Using An IISBenjamin LarsonNo ratings yet
- Group 2 Lesson Plan HandwashingDocument8 pagesGroup 2 Lesson Plan HandwashingKaloy KamaoNo ratings yet
- Kitten ContractDocument4 pagesKitten Contractapi-318766222No ratings yet
- ABO Forward and Reverse Tube MethodDocument4 pagesABO Forward and Reverse Tube Method''Rochelle Mylene ﭢ Ygoña100% (1)
- Great Dane Limited ContractDocument9 pagesGreat Dane Limited Contractapi-391051712No ratings yet
- Yellow Fever Instructions (Final)Document6 pagesYellow Fever Instructions (Final)AbhishekNo ratings yet
- Handout 13 Biotechnology in Promoting Law and Order PDFDocument36 pagesHandout 13 Biotechnology in Promoting Law and Order PDFMiccah Angela Parreño FraynaNo ratings yet
- CHECKLIST PROCEDURES (Immunization)Document2 pagesCHECKLIST PROCEDURES (Immunization)Elaine Frances IlloNo ratings yet
- Animal Bite GuildlinesDocument7 pagesAnimal Bite GuildlinesHari Pawan Kishore GarimellaNo ratings yet
Long-Term Efficacy of House Dust Mite Immunotherapy in Bronchial Asthma: A 15-Year Follow-Up Study
Long-Term Efficacy of House Dust Mite Immunotherapy in Bronchial Asthma: A 15-Year Follow-Up Study
Uploaded by
Nicole SierraOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Long-Term Efficacy of House Dust Mite Immunotherapy in Bronchial Asthma: A 15-Year Follow-Up Study
Long-Term Efficacy of House Dust Mite Immunotherapy in Bronchial Asthma: A 15-Year Follow-Up Study
Uploaded by
Nicole SierraCopyright:
Available Formats
Allergology International.
2005;54:443-449
ORIGINAL ARTICLE
Long-term Efficacy of House Dust Mite
Immunotherapy in Bronchial Asthma:
A 15-year Follow-up Study
Wiqar A Shaikh1
ABSTRACT
Background: Specific immunotherapy for bronchial asthma has been documented to be efficacious in several
studies ; however, it is not known whether this efficacy is sustained for several years after cessation of immu-
notherapy. The aim of this study is to determine the efficacy of house dust mite immunotherapy over a 15-year
period.
Methods: This study is an open, parallel, comparative trial in which 31 patients were administered immuno-
therapy for 5 years and then followed-up for a further 10 years. Their global symptom scores and FEV1 values
were compared with another group of 38 patients who refused immunotherapy.
Results: The use of immunotherapy resulted in a statistically significant improvement in both global symptom
scores and FEV1 in patients receiving immunotherapy when compared with those in the control group who did
not receive immunotherapy. This improvement was sustained for at least 10 years after cessation of immuno-
therapy.
Conclusions: The benefits of house dust mite immunotherapy are significant and sustained, a decade after
its discontinuation.
KEY WORDS
allergy, benefits, bronchial asthma, house dust mite, immunotherapy
INTRODUCTION METHODS
Specific immunotherapy (SIT) has been used in the INVESTIGATIONS
management of allergic diseases since 1911. 1 Several 85 selected patients with BA (of more than 512 newly
studies have clearly documented the clinical efficacy detected BA cases who attended the clinic during the
of SIT in house dust mite allergy , yet this mode of year 1986) were subjected to a detailed history and
therapy remains controversial , 2 especially in bron- physical examination. Each patient underwent the fol-
chial asthma ( BA ) despite the fact that 3 meta- lowing investigations
analyses have proven the beneficial effects in this ( 1 ) Estimation of serum IgE levels ( radio-
condition.3-5 immunoassay)
A very important question to be answered is (2) Skin prick tests (SPT) with a battery of com-
whether the effects of SIT are long lasting, particu- mon Indian allergens (ALCIT India Pvt. Ltd., Delhi,
larly after it has been discontinued. If the answer is India)6
yes, it would make SIT an attractive, disease modify- (3) Specific IgE levels (RAST) to the house dust
ing, treatment modality for allergic diseases such as mite D. farinae.
asthma and! or rhinitis. (4) Spirometry
This study is a prospective , open , parallel , com- (5) Peak nasal inspiratory flow rates (PNFIR) using
parative trial of SIT versus a control group of patients a Youltens nasal flow meter (Clement Clark Interna-
who did not receive SIT. tional, London, UK)
1Allergy Clinic, Bombay Hospital Institute of Medical Sciences, Email: drwiqar@vsnl.com
Bombay, India. Received 8 November 2004. Accepted for publication 19 January
Correspondence: Dr . Wiqar A Shaikh, Allergy & Asthma Clinic, 2005.
Shakti Sadan, Ground Floor, B Block, Opp Navjeevan Society , !2005 Japanese Society of Allergology
Lamington Road, Bombay, - 400 007 India.
Allergology International Vol 54, No3, 2005 www.js-allergol.gr.jp! 443
Shaikh WA
tients (4 men and 6 women) dropped out for a final
CRITERIA tally of 38 patients (20 men and 18 women) who com-
The criteria for selecting patients for this study pleted the study. The age range in this group was 11
were : years to 35 years (mean age 22.61 years)
(1) Symptoms of perennial BA alone, with no evi- None of the 85 patients finally selected were pre-
dence of rhinitis or skin allergies. Patients with sea- scribed or administered ICS during the entire study
sonal BA were excluded from this study so as to period. Since this was a prospective, long-term study,
avoid intermittent variations in parameters studied . allocation to either the SIT or the placebo group
Patients with rhinitis (which in India co-exists with could not be randomized. No attempt was made to
asthma in 55% of cases)6 were excluded, since vari- stratify the patients during selection or allotment of
ation in symptoms of rhinitis could have falsely al- patients. Informed consent was obtained from every
tered the patients perception of asthma symptom patient (or their parents in case of minors) before in-
scores. duction into the study
(2) Elevated total serum IgE levels (normal value 0
to 50 IU! ml) STUDY PLAN
(3) Reduced FEV1 (obstructive airway disease on Avoidance Measures
spirometry).7 Each patient was given instructions regarding appro-
( 4 ) Normal PNIFR ( normal value 100 to 300 priate avoidance measures, depending on their SPT
L! min) results. Avoidance measures for house dust included
(5) Positive SPT results (2+ or more) to D. farinae. removal of carpets , frequent vacuuming , changing
(6) Positive RAST to D. farinae (>class III) bedding to synthetic material such as foam and re-
Although an attempt was made to do so, social ob- moval of soft toys . All measures suggested were
jections precluded any house dust mite measure- strictly scrutinized and audited at each clinic visit, so
ments from patients homes. Patients who had been that they would, as far as possible, result in uniform
previously treated with SIT or those in whom there benefits.
were any known contraindications for administering
SIT were excluded from this study. Every patient was Rescue Medication
found to have taken some form of therapy for BA Patients in both groups were trained in the use of a
prior to this study, including oral and inhaled corti- salbutamol metered dose inhaler ( MDI ) through a
costeroids and beta2-agonists ; hence, a washout pe- large volume spacer device (750 ml ). Each patient
riod of 3 months preceded the beginning of the trial was instructed to use salbutamol as a rescue medica-
during which only inhaled salbutamol was permitted tion only
A double blind, placebo controlled trial was con-
templated, but was not possible in view of the long- SIT Vaccines
term nature of this study Patients in the SIT group were given a course of sub-
cutaneous desensitizing vaccines , which contained
RANDOMIZATION the dust mite D. farinae alone (Alcit India Pvt. Ltd.,
A core group of 197 patients were randomly selected Delhi, India). D. farinae is a more common allergen
using a random allocation table from the 512 new in India than D . pteronyssinus . 6 Vaccines were
asthmatics that attended the clinic in 1986. Each pa- started simultaneously in all 31 patients in the SIT
tient was offered SIT and inhaled corticosteroids group on January 1, 1987. These were administered
( ICS ) . Beclomethasone dipropionate was the only in increasing strength, beginning with 1 : 25,000 w! v
ICS available in India in the form of MDI when the conc. to a maximum of 1 : 50 w! v conc., in increas-
study was initiated. Patients who accepted SIT but re- ing doses (0.1 1.0 ml ) and decreasing frequency,
fused ICS were placed in Group 1 (SIT group) and beginning with twice a week, then once a week and
those who refused both SIT and ICS were placed in later once in two weeks. The maximal dose of 1.0 ml.,
Group 2 (control group). There were 46 men and 39 1 : 50 w! v conc., was reached at the end of 30 weeks
women among the 85 patients who were finally se- followed by administration of a once in 2 weeks main-
lected in both groups tenance dose (1.0 ml, 1 : 50 w! v conc.). Vaccines in
Group 1 : The specific immunotherapy group (SIT the SIT group were administered from January 1,
group) had 37 patients (22 men and 15 women), of 1987 to December 31, 1991, and then discontinued.
which 6 patients (4 men and 2 women) dropped out Subsequently both groups were asked to continue
from the study . Thus 31 patients ( 18 men and 13 with avoidance measures and rescue salbutamol until
women) completed the study with ages ranging from the end of the study on December 31, 2001. During
8 years to 28 years (mean age 19.77 years) the five-year vaccination period (1987 to 2001), vac-
Group 2 : The control group consisted of patients cines in India were still quantified as w!v. However,
who refused SIT as well as ICS ; it initially consisted as a part of a later study, 8 it was determined that the
of 48 patients (24 men and 24 women) of which 10 pa- strength of the vaccines administered was approxi-
444 Allergology International Vol 54, No3, 2005 www.js-allergol.gr.jp!
Long-term Benefits of Immunotherapy in Asthma
16 SIT
Control
14
12
10
Mean % Change in FEV1
-2
-4
-6 Mar 87 Mar 88 Mar 89 Mar 90 Mar 91 Mar 92 Mar 93 Mar 94 Mar 95 Mar 96 Mar 97 Mar 98 Mar 99 Mar 00 Mar 01
Time (Mar 1987 Dec 2001)
Fi
g.1Per cent
agechangeandvar
iat
ioni
nFEV1 i
nthecont
rol(
C)andspeci
fi
cimmunot
her
apy(
SIT)
gr
oupsoveraperiodof15year
s
mately 40 bioequivalent allergy units (BAU !ml ) to the beginning of the study, compare it with the status
start with 9 a maximum of 8000 BAU !ml during the on evaluation day and then decide on the current
maintenance phase , which would be designated as symptom score.
high dose All the instructions provided by the
manufacturer (Alcit India Pvt. Ltd.) were carefully fol- Spirometry
lowed. Side effects of SIT (local and systemic) if any, FEV 1 values obtained through spirometry were
were observed and carefully recorded at each consul- noted and the percentage change in FEV1 (PCFEV1)
tation. Between January 1, 1987 and December 31, was calculated at each visit, taking the FEV1 at the
2001, while the study was ongoing, symptom scores beginning of the study as the baseline value . Al-
and FEV1 of each patient were recorded once every 3 though this was an open trial, in order to eliminate
months on the first day of March, June, September bias, the clinic secretaries recorded symptom scores
and December and the clinic physician conducted spirometry. Clinic
secretaries were strictly instructed not to discuss
Symptom Scores with patients their mode of treatment. Also, patients
Symptom scores were assessed on a visual analogue from both groups were assigned to different days for
scale (VAS) from 0 to 10, where0indicated wors- clinic visits (even dates for the SIT group and odd
ening or no improvement and 10 indicated maximal dates for the control group) so as to ensure that no
improvement. While assessing symptom scores, pa- patients from one group would meet patients from
tients were instructed to make a global evaluation, in- the other group during the course of this study
cluding frequency and severity of symptoms , pres-
ence of other complaints such as cough and phlegm Rescue Medication Records
and improvement in quality of life Each patient was instructed to keep a careful record
Since symptom scores were evaluated for a lengthy of the number of doses of rescue salbutamol used.
15 year period, the possibility of patients forgetting Patients were asked to report back to the clinic if they
their initial global symptom severity and intensity was had any uncontrolled symptoms or clarifications. Pa-
kept in mind . Consequently during the symptom tients not responding to salbutamol MDI were asked
score evaluation period every attempt was made to to report to the clinic immediately and were pre-
jog the patients memory, re-live symptom severity at scribed a short course of oral prednisolone , begin-
Allergology International Vol 54, No3, 2005 www.js-allergol.gr.jp! 445
Shaikh WA
10 STI
Control
9
7
Changes in symptom scores
-1
Mar 87 Mar 88 Mar 89 Mar 90 Mar 91 Mar 92 Mar 93 Mar 94 Mar 95 Mar 96 Mar 97 Mar 98 Mar 99 Mar 00 Mar 01
Time (Mar 1987 Dec 2001)
Fig.2Per
cent
agechangeandvari
ati
onins
ympt
om scor
esi
nthec
ont
rol(
C)andspeci
fi
cimmunot
her
-
apy(SI
T)gr
oupsoveraper
iodof15years
10 Pearson s Corr = 0.87
9 P < 0.01
8
Mean Symptom Scores
0
-3 -2 -1 0 1 2 3 4 5 6 7 8 9 10 11 12 13
Mean % Change in FEV1
Fi
g.3Cor r
elat
i
onbet
weenmean% changei
nFEV1andmeansy
mpt
om s
cor
es
i
nthespeci
f
icimmunot
her
apy(
SIT)gr
oup
446 Allergology International Vol 54, No3, 2005 www.js-allergol.gr.jp!
Long-term Benefits of Immunotherapy in Asthma
7
Pearsons Corr = 0.58
P < 0.01
6
Mean Symptom Scores
5
0
-3 -2 -1 0 1 2 3 4 5 6 7 8 9 10 11 12 13 14
Mean % Change in FEV1
Fi
g.4Cor r
elati
onbet
weenmean% c
hangei
nFEV1 andmeans
ympt
om scor
es
i
nthecont
rolgroup
ning with 30 mg per day and tapered off within 3 asthma Control group patients had FEV1.0 ranging
weeks. from 68% to 76% of predicted normal values (mean-
71%) while those in the SIT group had FEV1.0 rang-
Skin Prick Tests ing from 66% to 70% (mean-70%)
SPT with D. farinae was repeated in all 85 patients be- The baseline data in this study revealed that the
fore the beginning of the study (December 1986), on SIT and Control groups were well matched with re-
discontinuation of SIT (January 1992) and on comple- gard to age, sex, disease period, total serum IgE lev-
tion of the study (January 2002) els and FEV1.0 (p< 0.05). This close match occurred
despite proper randomization and without any at-
Statistical Analysis tempt at stratification
Analysis of the correlation coefficient was calculated The results obtained from this study are shown in
using Pearsons test. The Mann Whitney test and Wil- Figures 14.
coxon Rank Sum test were used to compare the Both the PCFEV1 and the symptom scores were
symptom scores. PCFEV1 and SPT wheal sizes in the evaluated for each time point over a period of 15
two groups with p values < 0.05 were considered sta- years for both SIT and control group. Data were ex-
tistically significant. Area under the curve (AUC) was pressed as means + !- standard deviation (SD). Pa-
used to compare the overall effect of SIT with the tients receiving SIT showed less variability in SD
control group over the entire duration of the 15 year whereas patients in the control group showed a large
period. The SPSS statistical package was used to pre- variation over the 15-year period (Fig. 2).
dict the maximum possible period of benefit obtained Patients in the control group showed wide devia-
with SIT tions in mean symptom scores (range 2.60 to 6.21 )
and in PCFEV1 (varying up to 7%) during the study
RESULTS period. However, the SIT group showed a marked im-
Data obtained from this study showed that patients in provement through December 1987, a steady in-
the control group suffered from their disease for 1 to crease until December 1993, followed by a gradual
6 years (mean duration-2 years 7 months) whereas decline until December 2001 (Fig. 2)
those in the SIT group suffered for 1 to 7 years (mean Pearson correlations between mean PCFEV1 and
duration-3 years 5 months) mean symptom scores (Figs. 3, 4) showeda highly
Total serum IgE levels were in the range of 426 to significant correlationin the SIT group ( r = 0.87, p
978 IU!ml. (mean-581 IU!ml.) in the control group < 0.01) anda significant correlationin the control
and 488 to 1007 IU! ml (mean - 602 IU! ml.) in the SIT group ( r = 0.58, p < 0.01)
group The Mann-Whitney Test was performed for symp-
Based on the International Consensus Report, 7 all tom scores. The null hypotheses of no difference be-
69 cases were classified as moderately severe tween patients receiving SIT and control group was
Allergology International Vol 54, No3, 2005 www.js-allergol.gr.jp! 447
Shaikh WA
Tabl
e 1 AREAUNDERTHE CURVE(
AUC)
Par
amet
er Group 1987t o1991 1992t o2001 1987t o2001 pval
ues
SIT 159.72 409.38 569.10
% changei
nFEV1.
0(PCFEV1) p<0.
05
Cont
rol 122.78 155.33 278.11
SIT 139.85 277.73 417.58
Sy
mpt
om Scor
es p<0.
05
Cont
rol 101.43 145.78 247.21
rejected . There was a statistically significant differ- tained for the rest of the study due to inaccurate re-
ence between the two groups ( p < 0.01) with statisti- cording of MDI usage by patients in both groups
cally significant higher symptom scores in the SIT None of the 31 patients in the SIT group needed
group prednisolone during the 15-year study period. How-
Area under the curve ( AUC ) was estimated by ever, there were a total of 347 occasions when predni-
means of linear interpolation using the trapezoidal solone was administered to patients from the control
rule (EquivTest, version 2.0, Solutions Ltd., Republic group ; thus on an average each control group pa-
of Ireland). AUC was calculated for both PCFEV1 and tient required prednisolone 9 times during the study
symptom scores in both groups for the entire 15-year
period (1987 to 2001) and also separately for the pe- DISCUSSION
riod during which SIT was administered ( 1987 to The end points used in this study, viz. PCFEV1 and
1991 ) and the follow-up period ( 1992 to 2001 )(Ta- symptom scores are accepted as two of the most con-
ble 1).For all 3 periods, the AUC analysis concluded venient methods of monitoring the clinical efficacy of
that the AUC is significantly higher for the SIT group SIT. Bronchial hyper reactivity (BHR) was not con-
for both PCFEV1 and symptom scores ( p < 0.05) sidered as a parameter in this study since it has
The two sample Wilcoxon Rank Sum Test and con- yielded conflicting results in patients undergoing SIT.
fidence intervals ( CI ) for symptom scores and Of the eight studies measuring BHR before and after
PCFEV1 for March 1987 when compared with De- SIT, only one showed a decrease in BHR, but the re-
cember 2001 for the SIT group showed a statistically maining seven showed no change.9
significant difference ( p < 0.05 ) and significantly In addition there have been conflicting results with
higher scores for December 2001 regard to changes in skin reactivity following SIT. In
The data obtained from this study was applied to 13 out of 30 beneficial studies with SIT, four showed
the SPSS version 11.0 statistical package in an at- no change and nine demonstrated decreased skin
tempt to determine the maximum period of benefit test reactivity. 10 Furthermore, the present study con-
following cessation of SIT. Thecurve fit method firms that test reactivity is not a reliable end point for
predicted that symptom scores and PCFEV1 would studying the efficacy of SIT.
drop to zero in December 2014, which is after a dura- A number of studies have studied the efficacy of
tion of 28 years following initiation of the study (in SIT in asthma and !or rhinitis over periods varying
January 1987) from 1 to 6 years using house dust mite , tree and
The two-sample Wilcoxon Rank Sum Test was ap- grass pollen, fungi (Alternaria) and animal danders
plied to the skin prick test data which revealed no sig- (cat and! or dog).11-21 Only one study observed the ef-
nificant differences in wheal sizes when the 3 read- fects of SIT over a period of 14 years.22 However, that
ings (1986, 1992 and 2002) were compared to each study did not use any of the usual end points viz ,
other in both the SIT and control groups symptom scores, PCFEV1, SPT wheal size or bron-
Although side effects were not included in the chial hyperresponsiveness. Indeed, this same study
study plan, it is pertinent to note here that there were did not discuss the details of statistical analysis.
no systemic reactions in the SIT group. There were The present study has shown a statistically signifi-
however, 20 episodes of small local reactions (<4 cm cant improvement in end points in the SIT group ,
in diameter) at the site of injection, none of which re- which persisted for a decade after cessation of SIT
quired therapeutic intervention and using statistical projection would be expected to
The records maintained by patients revealed that last for approximately 13 years after completion of the
the control group inhaled a total of 61,400 puffs of sal- study (or for a total of 23 years following discontinu-
butamol (approximately 307 MDIs) during the first ation of SIT). This study concludes that contrary to all
year of this study as rescue medication. During the current skepticism , SIT indeed has a long lasting
same period the SIT group inhaled 8,600 puffs (or ap- beneficial role in BA. In sum, SIT could therefore be
proximately 43 MDIs). The difference therefore, be- considered a truly disease modifying drug (DMD)
tween the two groups with regards to rescue medica-
tion, is stark. However, no reliable data could be ob-
448 Allergology International Vol 54, No3, 2005 www.js-allergol.gr.jp!
Long-term Benefits of Immunotherapy in Asthma
9. Turkeltaub PC. Allergen vaccine unitage based on bio-
ACKNOWLEDGEMENTS logical standardization : Clinical significance. In: Bukantz
The author wishes to acknowledge the assistance of SC, Lockey RF (eds). Allergens and Allergen Immunother-
apy, 2nd edn. New York: Marcel Dekker Inc, 1999;321-340.
the following clinic secretaries in completing this
10. Ledford DK. Efficacy of immunotherapy. In: Bukantz SC,
study : Sampada Haldankar, Sheela Sawant, Kishore Lockey RF (eds). Allergens and Allergen Immunotherapy,
Dhuri , Gurudatt Dhuri , Charusheela Patwardhan , 2nd edn. New York: Marcel Dekker Inc., 1999;359-379.
Eknath Gawde , Ahmed Shaikh, Gopichand Kamble 11. Nagaya H. Long term effects of immunotherapy in south-
and Asif Mohimtule. ern California. Ann. Allergy 1980;44:193-199.
Thanks are also due to Dr. S. C. Talwalkar of Hor- 12. Cantani A, Businco E, Maglio A. Alternaria allergy : a
mone Labs, Bombay for IgE levels and Mr. Nirankar three-year controlled study in children treated with immu-
notherapy. Allergol. Immunopathol. 1988;16:1-4.
Sharma, Technical Director, ALCIT (India) Pvt. Ltd.,
13. Hedlin G, Heilborn H, Lilja G et al. Long term follow-up of
Delhi, for regular supply of SPT allergens and SIT
patients treated with a course of cat or dog immunother-
vaccines apy. J. Allergy Clin. Immunol. 1995;96:879-885.
The author is grateful to Ms . Priya Deshpande 14. Jacobsen L, Nuchel PB, Wihl JA et al. Immunotherapy
( statistician) , Ms. Trupti Bal ( statistician ) and Dr . with partially purified and standardized tree pollen ex-
Sundeep Salvi of the Chest Research Foundation , tracts. IV. Results from long-term (6-year) follow up. Al-
Pune, and Dr. J.A. Gogtay, Medical Director, Cipla lergy 1997;52:914-920.
Ltd., Bombay, for their help in statistical analysis of 15. Olaguibel JM, Tabar AI, Garcia BE et al. Long-term im-
munotherapy with an optimal maintenance dose of a stan-
data obtained from this study
dardized Dermatophagoides pteronyssinus extract in
Finally thanks are due to my daughter Shifa, medi- asthmatic patients. J. Investig . Allergol . Clin . Immunol .
cal student at Topiwala National Medical College , 1999;9:110-116.
Bombay, for her help in compiling the data and statis- 16. Ariano R, Kroom AM, Augeri G et al. Long-term treat-
tics and for the word processing. ment with allergoid immunotherapy with Parietaria. Clini-
cal and immunologic effects in a randomized controlled
trial. Allergy 1999;54:313-319.
REFERENCES
17. Durham SR, Walker SM, Varga EM et al. Long-term clini-
1. Noon L. Prophylactic inoculation against hay fever. Lan-
cally efficacy of grass-pollen immunotherapy. N. Engl. J.
cet 1911;i:1572-1573.
Med. 1999;341:468-475.
2. Committee on safety of medicinesCSM update : desensi-
18. Cools M, Van Bever HP, Weyler JJ et al. Long-term ef-
tizing vaccines. Br. Med. J. 1986;293:948.
fects of specific immunotherapy , administered during
3. Abramson MJ, Puy RM, Weiner JM. Immunotherapy in
childhood in asthmatic patients allergic to either house-
asthma : an updated systemic review. Allergy 1999;54:
dust mite or to both house-dust mite and grass pollen. Al-
1022-1041.
lergy 2000;55:69-73.
4. Abramson MJ, Puy RM, Weiner JM. Is allergen immuno-
19. Pichler CE, Helbling A, Pichler WJ. Three years of spe-
therapy effective in asthma? A meta-analysis of random-
cific immunotherapy with house-dust-mite extracts in pa-
ized controlled trials. Am. J. Respir. Crit. Care Med. 1995;
tients with rhinitis and asthma : significant improvement
151:969-974.
of allergen-specific parameters and of non-specific bron-
5. Abramson MJ, Puy RM, Weiner JM. Allergen immuno-
chial hyper reactivity. Allergy 2001;56:301-306.
therapy for asthma (Cochrane Review). The Cochrane Li-
20. Nagata M, Tanaka K. An evaluation of the long-term ef-
brary, 2003.
fects of clustered immunotherapy in house-dust-mite sen-
6. Shaikh WA. Allergies in India : An analysis of 1916 pa-
sitive adult bronchial asthma. Arerugi 2001;50:453-439.
tients attending an allergy clinic in Bombay , India. Int .
21. Eng PA, Reinhold M, Gnehm HP. Long-term efficacy of
Rev. Allergol. Clin. Immunol. 1997;3:101-104.
preseasonal grass pollen immunotherapy in children. Al-
7. National Institute of Health , National Heart Lung and
lergy 2002;57:306-312.
blood Institute. International consensus report on diagnosis
22. Johnstone DE, Dutton A. The value of hyposensitization
and treatment of asthma. Publication no . 92-3091. Be-
therapy for bronchial asthma in children- a 14-year study.
thesda: National Institute of Health, 1992.
Paediatrics 1968;42:793-802.
8. Shaikh WA. Immunotherapy v !s inhaled budesonide in
bronchial asthma : an open parallel, comparative trial .
Clin. Exp. Allergy 1997;27:1279-1284.
Allergology International Vol 54, No3, 2005 www.js-allergol.gr.jp! 449
You might also like
- Adenotonsillitis NewDocument100 pagesAdenotonsillitis NewDrravikumar Bhandari100% (1)
- Catgutpuntura Rinitis AlérgicaDocument11 pagesCatgutpuntura Rinitis AlérgicaDubichelNo ratings yet
- Evaluation of Antibiotic Sensitivity Pattern in Acute TonsillitisDocument5 pagesEvaluation of Antibiotic Sensitivity Pattern in Acute TonsillitisyoanaNo ratings yet
- Sublingual Immunotherapy To House Dust Mite in Pediatric Patients With Allergic Rhinitis and Asthma: A Retrospective Analysis of Clinical Course Over A 3-Year Follow-Up PeriodDocument4 pagesSublingual Immunotherapy To House Dust Mite in Pediatric Patients With Allergic Rhinitis and Asthma: A Retrospective Analysis of Clinical Course Over A 3-Year Follow-Up PeriodPeter SalimNo ratings yet
- 12erny (Full Permission)Document15 pages12erny (Full Permission)Peter SalimNo ratings yet
- 895 902 1 PB PDFDocument5 pages895 902 1 PB PDFBadai Ardyana PutriNo ratings yet
- A Randomised Dose-Ranging Study of Tiotropium Respimat® in Children With Symptomatic Asthma Despite Inhaled CorticosteroidsDocument10 pagesA Randomised Dose-Ranging Study of Tiotropium Respimat® in Children With Symptomatic Asthma Despite Inhaled CorticosteroidsabdmaliknasNo ratings yet
- Atopic Dermatitis and Vegan DietDocument9 pagesAtopic Dermatitis and Vegan DietIuliu Ciupe-VaidaNo ratings yet
- Typhoid Fever Vaccines: A Meta-Analysis of Studies On Efficacy and ToxicityDocument7 pagesTyphoid Fever Vaccines: A Meta-Analysis of Studies On Efficacy and ToxicityYudha AkihiroNo ratings yet
- Clinical Presentation and Laboratory Features in Pediatric Typhoid Fever Patient Susceptibility To First-Line Antibiotic TherapyDocument10 pagesClinical Presentation and Laboratory Features in Pediatric Typhoid Fever Patient Susceptibility To First-Line Antibiotic TherapySuci ZahraniNo ratings yet
- Nutrients 10 01678Document11 pagesNutrients 10 01678zulfa nadiaNo ratings yet
- Evidence Based Medicine - CONSORT & AppraisalDocument52 pagesEvidence Based Medicine - CONSORT & AppraisalNurul Aulia AbdullahNo ratings yet
- Ayu Ijpsr14-05-01-001Document9 pagesAyu Ijpsr14-05-01-001Listiani AyuNo ratings yet
- Prevalence of Allergic Rhinitis Symptoms and Positive Skin Prick Test Results in Children With Recurrent EpistaxisDocument6 pagesPrevalence of Allergic Rhinitis Symptoms and Positive Skin Prick Test Results in Children With Recurrent EpistaxisKevinFeraldyNo ratings yet
- Universitas Indonesia: U. Weber, M. Krammel, S. Linke, T. Hamp, T. Stimpfl, B. Reiter, W. PlӧchlDocument8 pagesUniversitas Indonesia: U. Weber, M. Krammel, S. Linke, T. Hamp, T. Stimpfl, B. Reiter, W. PlӧchlgoldenNo ratings yet
- High-Dose Versus Standard-Dose Amoxicillin/ Clavulanate For Clinically-Diagnosed Acute Bacterial Sinusitis: A Randomized Clinical TrialDocument15 pagesHigh-Dose Versus Standard-Dose Amoxicillin/ Clavulanate For Clinically-Diagnosed Acute Bacterial Sinusitis: A Randomized Clinical TrialHendra EfendiNo ratings yet
- Typhoid JournalDocument7 pagesTyphoid JournalRegina AyediaNo ratings yet
- Prosiding Seminar Nasional Dan Workshop "Perkembangan Terkini Sains Farmasi Dan Klinik IV" Tahun 2014Document7 pagesProsiding Seminar Nasional Dan Workshop "Perkembangan Terkini Sains Farmasi Dan Klinik IV" Tahun 2014IdafabdullahNo ratings yet
- Effectiveness of Low Dose Immunotherapy in The Treatment of Canine Atopic Dermatitis - A Prospective, Double-Blinded, Clinical Study (Document9 pagesEffectiveness of Low Dose Immunotherapy in The Treatment of Canine Atopic Dermatitis - A Prospective, Double-Blinded, Clinical Study (jenNo ratings yet
- Radioiodine TherapyDocument5 pagesRadioiodine Therapyaccime24No ratings yet
- Ebm SeptemberDocument29 pagesEbm SeptemberJulius OentarioNo ratings yet
- Dog Allergen Immunotherapy: Past, Present, and Future: Derek M. Smith, MD and Christopher A. Coop, MDDocument6 pagesDog Allergen Immunotherapy: Past, Present, and Future: Derek M. Smith, MD and Christopher A. Coop, MDbrakim23No ratings yet
- Gabapentin For Refractory Chronic Cough: A Randomised, Double-Blind, Placebo-Controlled TrialDocument8 pagesGabapentin For Refractory Chronic Cough: A Randomised, Double-Blind, Placebo-Controlled TrialIAmILoNo ratings yet
- SII, FODMAPS e Hormonios EndócrinosDocument7 pagesSII, FODMAPS e Hormonios Endócrinosmari bNo ratings yet
- Prof Iwin - Asit Course Final Method and Its Eval Exp 30' JKT Feb 08Document79 pagesProf Iwin - Asit Course Final Method and Its Eval Exp 30' JKT Feb 08nick_mdNo ratings yet
- Jurnal Reading OtomikosisDocument4 pagesJurnal Reading OtomikosisTria JuwitaNo ratings yet
- Journal of EthnopharmacologyDocument5 pagesJournal of EthnopharmacologypipisoseticaNo ratings yet
- Perbedaan Imunoterapi Alergen Spesifik (ITS) Dengan Vaksinasi BCG Dalam Meningkatkan Kualitas Hidup Penderita Rinitis AlergiDocument12 pagesPerbedaan Imunoterapi Alergen Spesifik (ITS) Dengan Vaksinasi BCG Dalam Meningkatkan Kualitas Hidup Penderita Rinitis AlergiThya Alif KahfNo ratings yet
- A Placebo-Controlled Trial of Antimicrobial Treatment For Acute Otitis MediaDocument6 pagesA Placebo-Controlled Trial of Antimicrobial Treatment For Acute Otitis MediaegieprajaNo ratings yet
- Allergen Immunotherapy Expert ExchangeDocument4 pagesAllergen Immunotherapy Expert ExchangeAnna LiachenkoNo ratings yet
- Indacaterol Provides 24-Hour Bronchodilation in COPD: A Placebo-Controlled Blinded Comparison With TiotropiumDocument8 pagesIndacaterol Provides 24-Hour Bronchodilation in COPD: A Placebo-Controlled Blinded Comparison With TiotropiumCalca NeusNo ratings yet
- A Nationwide Survey of Inhalant Allergens Sensitization and Levels of Indoor Major Allergens in KoreaDocument6 pagesA Nationwide Survey of Inhalant Allergens Sensitization and Levels of Indoor Major Allergens in KoreaRatna WindyaningrumNo ratings yet
- Veterinary Dermatology - 2021 - MuellerDocument20 pagesVeterinary Dermatology - 2021 - MuellerMandycat75No ratings yet
- Jurnal Sidang RespiDocument4 pagesJurnal Sidang RespiAnis Eka SukmadadariNo ratings yet
- 14 2011-14-Ajmr Isn 2011Document5 pages14 2011-14-Ajmr Isn 2011Dr. Taha NazirNo ratings yet
- Dry Needling in Lateral Epicondylitis A Prospective EBP PDFDocument5 pagesDry Needling in Lateral Epicondylitis A Prospective EBP PDFDanielle Denice LacabaNo ratings yet
- 2011 Article 437Document6 pages2011 Article 437AlexandraParedesPuertaNo ratings yet
- Insulin Allergy Can Be Successfully Managed by A Systematic ApproachDocument6 pagesInsulin Allergy Can Be Successfully Managed by A Systematic Approachjames antonyNo ratings yet
- Jurnal AsmaDocument12 pagesJurnal AsmaaulNo ratings yet
- Sublingual ImmunotherapyDocument4 pagesSublingual ImmunotherapyAnonymous eZqDZbObRiNo ratings yet
- Cea 13169 PDFDocument15 pagesCea 13169 PDFrisanataliasiburianNo ratings yet
- Super 1st Draft 1Document10 pagesSuper 1st Draft 1iNeimoNo ratings yet
- 276 Jaipal Singh VishwakarmaDocument8 pages276 Jaipal Singh Vishwakarmashubh1511No ratings yet
- Jurnal 2Document9 pagesJurnal 2dewi trisnawatiNo ratings yet
- Lo Han Guo FruitDocument9 pagesLo Han Guo FruitInten KusumaNo ratings yet
- Use of Superoxide Dismutase in Accelerating Symptom PDFDocument7 pagesUse of Superoxide Dismutase in Accelerating Symptom PDFWilliam JavierNo ratings yet
- Efikasi AzitromisinDocument4 pagesEfikasi AzitromisinNadia DesiNo ratings yet
- General Practice: Are Antibiotics Indicated As Initial Treatment For Children With Acute Otitis Media? A Meta-AnalysisDocument5 pagesGeneral Practice: Are Antibiotics Indicated As Initial Treatment For Children With Acute Otitis Media? A Meta-AnalysisJuan Carlos Aguayo RomeroNo ratings yet
- The Clinical Effect of Erdosteine On Acute Respiratory Tract Diseases in ChildrenDocument17 pagesThe Clinical Effect of Erdosteine On Acute Respiratory Tract Diseases in ChildrenResha Adriana PuttyNo ratings yet
- Aom PDFDocument13 pagesAom PDFiyan rNo ratings yet
- Jurnal AsthmaDocument11 pagesJurnal AsthmaNadira Juanti PratiwiNo ratings yet
- REITHINGERCID2055Document8 pagesREITHINGERCID2055Wulan YuwitaNo ratings yet
- Moxifloxaxin For CAPDocument9 pagesMoxifloxaxin For CAPmateri posNo ratings yet
- A Comparison of Oral Procaterol and Albuterol in Reversible Airflow ObstructionDocument6 pagesA Comparison of Oral Procaterol and Albuterol in Reversible Airflow Obstructionparris shanyNo ratings yet
- Pengobatan Pyomentra Dengan AglepristoneDocument7 pagesPengobatan Pyomentra Dengan AglepristoneraldyNo ratings yet
- All Questions To Be Answered. Each Question To Be Answered in A Separate Book (Or Books If More Than One Is Required For The One Answer)Document3 pagesAll Questions To Be Answered. Each Question To Be Answered in A Separate Book (Or Books If More Than One Is Required For The One Answer)matentenNo ratings yet
- IJP - Volume 8 - Issue 9 - Pages 11939-11944Document6 pagesIJP - Volume 8 - Issue 9 - Pages 11939-11944A'la Nur RoyanNo ratings yet
- Garlic (Allium sativum): Monograph on a herb reputed to be medicinalFrom EverandGarlic (Allium sativum): Monograph on a herb reputed to be medicinalNo ratings yet
- Complementary and Alternative Medical Lab Testing Part 5: GastrointestinalFrom EverandComplementary and Alternative Medical Lab Testing Part 5: GastrointestinalNo ratings yet
- Complementary and Alternative Medical Lab Testing Part 2: RespiratoryFrom EverandComplementary and Alternative Medical Lab Testing Part 2: RespiratoryNo ratings yet
- 22 Varicella Pink BookDocument24 pages22 Varicella Pink BookMohamad Syaikhul IslamNo ratings yet
- Eucast Discussion Document E.Dis 5.1 March 2003 Determination of Minimum Inhibitory Concentrations (Mics) of Antibacterial Agents by Broth DilutionDocument7 pagesEucast Discussion Document E.Dis 5.1 March 2003 Determination of Minimum Inhibitory Concentrations (Mics) of Antibacterial Agents by Broth DilutionPankajNo ratings yet
- Swine FluDocument4 pagesSwine FluDarwotoNo ratings yet
- Donor Selections..Document17 pagesDonor Selections..OmamaNo ratings yet
- Basic Manual For Free Range Colored Broilers Production PDFDocument12 pagesBasic Manual For Free Range Colored Broilers Production PDFAndy LimNo ratings yet
- 1 - Overview of Viral Respiratory InfectionsDocument3 pages1 - Overview of Viral Respiratory Infectionssapik zirafNo ratings yet
- Complete Abstract Book ASTMH - Atlanta 2012-USADocument3 pagesComplete Abstract Book ASTMH - Atlanta 2012-USAPercy Lezama VigoNo ratings yet
- Contractor UPM Weekly HSE Submittal Rev 01 - OMPPD 2024 WEEK-3Document10 pagesContractor UPM Weekly HSE Submittal Rev 01 - OMPPD 2024 WEEK-3Rolando MarceloNo ratings yet
- Commercial Chicken Vaccination Part 3 Injectable AdministrationDocument6 pagesCommercial Chicken Vaccination Part 3 Injectable AdministrationAnjum IslamNo ratings yet
- Rubella: Lilian B - Rosario, MD, FPPSDocument19 pagesRubella: Lilian B - Rosario, MD, FPPSRiya KayarkarNo ratings yet
- 05 Introduction To Plant PathologyDocument20 pages05 Introduction To Plant PathologyirwanpaluNo ratings yet
- Sci Chapter 2 8thDocument18 pagesSci Chapter 2 8thAakash ChatakeNo ratings yet
- Care of The Older or Disabled AdultDocument63 pagesCare of The Older or Disabled Adultfairwoods100% (1)
- Health Programme Manager's Manual PDFDocument140 pagesHealth Programme Manager's Manual PDFLakshmi SethNo ratings yet
- OJAP Summary Major EventsDocument6 pagesOJAP Summary Major EventsReid KirbyNo ratings yet
- Disinfectant Efficacy StudyDocument63 pagesDisinfectant Efficacy Studydeepanshsharma100% (2)
- K. Kapita Selekta-Farmakologi (DR - Astrianda)Document13 pagesK. Kapita Selekta-Farmakologi (DR - Astrianda)Nela LutfianaNo ratings yet
- Bat in Watertown Reported To Have RabiesDocument1 pageBat in Watertown Reported To Have RabiesNewzjunkyNo ratings yet
- RMS Case Study (Leptospirosis) GRP 1 BSTM 1-B FinalDocument12 pagesRMS Case Study (Leptospirosis) GRP 1 BSTM 1-B FinalLauren Abas Dela CruzNo ratings yet
- Course 9 - VC225ILR - UsageDocument7 pagesCourse 9 - VC225ILR - UsageDulasNo ratings yet
- Analytic Guide For Assessing Vaccination Coverage Using An IISDocument42 pagesAnalytic Guide For Assessing Vaccination Coverage Using An IISBenjamin LarsonNo ratings yet
- Group 2 Lesson Plan HandwashingDocument8 pagesGroup 2 Lesson Plan HandwashingKaloy KamaoNo ratings yet
- Kitten ContractDocument4 pagesKitten Contractapi-318766222No ratings yet
- ABO Forward and Reverse Tube MethodDocument4 pagesABO Forward and Reverse Tube Method''Rochelle Mylene ﭢ Ygoña100% (1)
- Great Dane Limited ContractDocument9 pagesGreat Dane Limited Contractapi-391051712No ratings yet
- Yellow Fever Instructions (Final)Document6 pagesYellow Fever Instructions (Final)AbhishekNo ratings yet
- Handout 13 Biotechnology in Promoting Law and Order PDFDocument36 pagesHandout 13 Biotechnology in Promoting Law and Order PDFMiccah Angela Parreño FraynaNo ratings yet
- CHECKLIST PROCEDURES (Immunization)Document2 pagesCHECKLIST PROCEDURES (Immunization)Elaine Frances IlloNo ratings yet
- Animal Bite GuildlinesDocument7 pagesAnimal Bite GuildlinesHari Pawan Kishore GarimellaNo ratings yet