Professional Documents
Culture Documents
Laparoscopic Versus Open Appendicectomy: A Comparative Study
Laparoscopic Versus Open Appendicectomy: A Comparative Study
Uploaded by
ChristianWicaksonoOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Laparoscopic Versus Open Appendicectomy: A Comparative Study
Laparoscopic Versus Open Appendicectomy: A Comparative Study
Uploaded by
ChristianWicaksonoCopyright:
Available Formats
International Surgery Journal
Karatparambil A et al. Int Surg J. 2016 Feb;3(1):128-134
http://www.ijsurgery.com pISSN 2349-3305 | eISSN 2349-2902
DOI: http://dx.doi.org/10.18203/2349-2902.isj20160213
Research Article
Laparoscopic versus open appendicectomy: a comparative study
Abidali Karatparambil*, Sidhic Abbas Kummankandath, Ranjith Mannarakkal,
Mujeeb Rahman Nalakath, Deepu Babu
MES Medical College, Perinthalmanna, Kerala, India
Received: 02 October 2015
Revised: 18 November 2015
Accepted: 16 December 2015
*Correspondence:
Dr. Abidali karatparambil,
E-mail: dr_abid1@yahoo.com
Copyright: © the author(s), publisher and licensee Medip Academy. This is an open-access article distributed under
the terms of the Creative Commons Attribution Non-Commercial License, which permits unrestricted non-commercial
use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
Background: Acute appendicitis is one of the common emergency surgical problems that usually we encounters.
Since its introduction by McBurney in 1894, appendicectomy has been the treatment of choice for acute appendicitis.
Since its initial description by Semm in 19834, Laparoscopic appendicectomy (LA) has struggled to prove its
superiority over the open technique. The advantages of LA over open appendicectomy (OA) are thought to be less
postoperative pain, shorter hospital stay and early return to usual activity. While the incidence of postoperative wound
infection is thought to be lower after the laparoscopic technique. There is however notions showing only minimal
benefit from laparoscopic appendicectomy, with higher cost of this method. Though multiple prospective randomized
trials, meta-analyses, and systematic reviews have been conducted to assess the value of LA over OA, the
heterogeneity of the measured variables and other weaknesses in methodology have not allowed drawing definitive
conclusions and generalizations.
Methods: It is a prospective study comparing the advantage of laparoscopic over open appendicectomy.
Results: The mean duration of hospital stay in both the study groups (OA and LA) 3.5 and 3.4 respectively. There
was no significant return of bowel sounds, return to normal activity and surgical site infection. But cost for to be high
with laparoscopic appendicectomy.
Conclusions: There was no advantage of laparoscopic appendicectomy over open appendicectomy in terms of return
of bowel sounds, return to normal activity and surgical site infection. But cost for to be high with lap appendectomy.
To conclude, LA has no definite advantages over OA as per results of my study.
Keywords: Acute appendicitis, Laparoscopic appendicectomy, Open appendicectomy, Pelvic abscess, Quality of life
INTRODUCTION surgical intervention, with a lifetime risk of 6%.1,2 Since
its introduction by McBurney in 1894, appendicectomy
In the last decade laparoscopy has significantly affected has been the treatment of choice for acute appendicitis3.
general surgical procedures for a variety of pathological Since its initial description by Semm in 19834,
indications. With accumulation of experience and Laparoscopic appendicectomy (LA) has struggled to
progress in armamentarium technology the number and prove its superiority over the open technique. This is in
types of procedures routinely performed with minimally contrast to laparoscopic cholecystectomy, which has
invasive technique has grown. Laparoscopy is more often promptly become the gold standard for gallstone disease.3
applied not only in elective surgery, but also in Open appendicectomy (OA) has withstood the test of
emergency surgeries. Suspected appendicitis is time for more than a century. The procedure is
undoubtedly the most common indication for emergency standardized among surgeons and unlike
International Surgery Journal | January-March 2016 | Vol 3 | Issue 1 Page 128
Karatparambil A et al. Int Surg J. 2016 Feb;3(1):128-134
cholecystectomy, OA is typically completed using a All cases of LA converted to OA were excluded
small right lower quadrant incision and postoperative from comparison with OA.
recovery is usually uneventful.
RESULTS
The advantages of LA over OA are thought to be less
postoperative pain, shorter hospital stay and early return A total of 187 patients were included in the study during
to usual activity.4,5 While the incidence of postoperative this period, according to the inclusion criteria. Of this 100
wound infection is thought to be lower after the patients underwent an open appendicectomy, 87
laparoscopic technique, the incidence of postoperative underwent a laparoscopic appendicectomy, and 13
intra-abdominal sepsis may be higher in patients operated patients were converted from an LA to OA. These 13
on for gangrenous or perforated appendicitis.4,5 There are patients were excluded from analyzing the primary
however notions showing only minimal benefit from outcome measures. post operative pain, post operative
laparoscopic appendicectomy, with higher cost of this recovery, duration of hospital stay, wound infection
method. (surgical site infection) , cost analysis and time to return
to usual activities. Out of the total 187 patients, there
However conversion to open surgery is inevitable in were 88 males and 99 females. The mean age of the study
some cases. The conversion causes prolongation of population was 24.1 years (Range: 5-55 years).
hospital stay, increased total cost and dissatisfaction of
the patients. The most valuable aspect of laparoscopy in Duration of hospital stay
the management of suspected appendicitis is as a
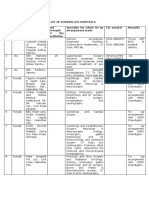
diagnostic tool, particularly in women of child-bearing The mean duration of hospital stay in both the study
age8. Though multiple prospective randomized trials, groups (OA and LA) 3.5 and 3.4 respectively. There was
meta-analyses6-9 and systematic reviews10-13 have been no significant difference in number of patients who
conducted to assess the value of LA over OA, the stayed for 3 or 4 days in hospital between OA and LA,
heterogeneity of the measured variables and other but among the group of patients who satyed for more than
weaknesses in methodology have not allowed to draw 5 days 69% belong to open appendicectomy group (Table
definitive conclusions and generalizations.12-13 Hence, the 1 & 2; Figure 1).
„gold standard‟ modality of treatment for clinically
confirmed appendicitis is still not established. Table 1: Distribution according to hospital stay.
Unfortunately, there are not many authoritative studies
comparing the results of LA with OA in our locality. Open LAP
Hence the need for this study. appendicectomy appendicectomy
Mean 3.5 3.4
Objectives Std Deviation 0.8 0.7
Median 3.0 3.0
To compare laparoscopic appendicectomy versus open Minimum 3.0 3.0
appendicectomy in terms of hospital stay, post operative
Maximum 6.0 6.0
analgesia, post operative recovery, return to work.
METHODS
All cases of appendicitis operated from January 2013 to
January 2014 in the Department of Surgery in our
hospital „Clinically confirmed‟ case of appendicitis
means an Alvarado score of 7 or more or an equivocal
score (5-6) with sonological evidence. Both emergency
and elective cases were included in the study
Inclusion criteria
The new patients of both sexes belonging to age
group 5-50 years presenting with acute appendicitis.
Emergency as well as elective cases were included. Figure 1: Comparison of hospital stay based on type
of procedure.
Exclusion criteria
Post operative analgesia in the study groups
Patients with delayed presentation leading to
appendicular mass. There was no significant difference in the post operative
Patient not willing to participate in the study. analgesia requirement between the 2 groups (p – 0.7).
The mean analgesic requirement was 6.5 ± 0.8 doses in
International Surgery Journal | January-March 2016 | Vol 3 | Issue 1 Page 129
Karatparambil A et al. Int Surg J. 2016 Feb;3(1):128-134
the OA group and 6.5 ± 0.6 in the LA group (Table 3 & Table 4: Comparison of type of procedure based on
Figure 2). return bowel sounds.
Table 2: Comparison of hospital stay based on type of Return Open LAP
P
procedure. bowel appendicec appendicecto
χ2
sounds tomy my
Hospital Open LAP Count Percent Count Percent
stay appendicectomy appendicectomy First post
Count Percent Count Percent operative 70 70.0 67 77.0
3 67 67.0 60 69.0 day
4 24 24.0 23 26.4 Second 1.17 0.280
5-6 9 9.0 4 4.6 post
30 30.0 20 23.0
Mean ± SD 3.5 ± 0.8 3.4 ± 0.7 operative
day
Table 3: Comparison of post op analgesia based on
type of procedure.
Open LAP
Analgesia
appendicectomy appendicectomy
Post OP Count Percent Count Percent
5 5-6 57 57.0 46 52.9
7 7-8 41 41.0 41 47.1
9 9-10 2 2.0 0 0.0
Mean ± SD 6.5 ± 0.8 6.5 ± 0.6
t= 0.28; p= 0.781
Figure 3: Comparison of type of procedure based on
return bowel sounds.
Table 5: Comparison of type of procedure based on
return to normal activity.
Return
Open LAP
bowel P
appendice appendice χ2
normal
ctomy ctomy
activity
Count Percent Count Percent
6 7 7.0 10 11.5
Figure 2: Comparison of post operative based on type 7 54 54.0 49 56.3
of procedure. 2.23 0.526
8 34 34.0 26 29.9
9 5 5.0 2 2.3
Return of bowel sounds
70% of the patients in OA group and 77 % in LA group
had return of bowel sounds in first postoperative day (at
24 hours) and remaining 30 and 23% in 2nd post
operative day (at 48 hours) No statistical significance in
return of bowel sounds was noticed in the 2 study groups
(Table 4 & Figure 3).
Return to normal activity
Majority of the patients in OA and LA group had return
to normal activity by 7th post operative day ( 54% and
56.3%) . there was no statistical significance in return to
normal activity between the 2 study groups (Table 5 &
Figure 4). Figure 4: Comparison of type of procedure based on
return to normal activity.
International Surgery Journal | January-March 2016 | Vol 3 | Issue 1 Page 130
Karatparambil A et al. Int Surg J. 2016 Feb;3(1):128-134
Surgical site infection around 11%.18 Given the large number of procedures
done annually, the validation of a minimally invasive
When surgical site infection was compared between the 2 technique that would improve outcomes may have a
study groups there was 6 cases of surgical site infection direct impact on patient management and possibly an
in OA group and 2 cases in LA group,no statistical indirect effect on the economics of health care.17
significance in surgical site infection between the 2 study
groups (Table 6 & Figure 5). In an article published in Ann Surg 2005, Katkhouda et al
performed an extensive search of literature comparing LA
Table 6: Comparison of type of procedure based on to OA in adults using the review of Cochrane Central
surgical site infection. Registry of controlled trials, MEDLINE, and Sci Search.
45 prospective randomized studies, 4 meta analyses, 4
surgical Open LAP systematic reviews (including 1 cochrane database) and 4
P
site appendice appendice χ2 large non randomized comparative trials were included in
infection ctomy ctomy the review.17
Count Percent Count Percent
No 94 94.0 85 97.7 1.56 0.212 As suggested by all meta- analyses and systematic
reviews, the methodological quality of most studies was
“poor to moderate”. Only 7 PRS had a sample size of 200
patients or more. The majority of non randomized studies
favored laparoscopy. These should be analysed with
caution because of their inherent bias.
In 1993, Tate et al from Hong Kong published data
collected on the initial 55patients 6 months after the
introduction of LA in their hospital, that were compared
to 100 OA42. They found significant benefits in favour of
LA. These same authors in a follow up PRS conducted in
the same institution concluded that their study could “no
longer support the widespread adoption of a laparoscopic
alternative to a traditional operation based on initial
Figure 5: Comparison of type of procedure based on uncontrolled studies”.14
surgical site infection.
Two studies from Sweden and Denmark that included
Cost 500 and 583 patients, respectively followed sound
scientific principles,19-20 but the lack of appropriate
When cost between the 2 studies groups were compared blinding and inclusion of multiple centres weakened the
mean in OA group was 9160.8 and LA was 13676.3. Lap results.
appendicectomy costs more than open appendicectomy
(Table 7). Review of outcomes
Table 7: Distribution according to cost. The overall reported mortality of appendectomy is very
low and was estimated in a review of large administrative
Open LAP database at 0.05% for LA and 0.3% for OA,18 reinforcing
appendicectomy Appendicectomy the fact that appendicectomy in the absence of peritonitis
Mean 9106.8 13676.3 is a safe procedure, regardless of the technique.
Std Deviation 1875.6 1259.1
Median 8600.0 13600.0 Overall complication rates were similar in both groups in
most of the studies. The most serious early complication
Minimum 7100.0 12100.0
in the LA group, that required a reoperation is injury of
Maximum 10000.0 17880.0 the epigastric vessels due to an inadequate trocar
placement, and is avoidable with the placement of trocars
DISCUSSION under direct vision lateral to the epigastric arteries.17 The
removal of all cannulas should also be done under direct
Results of previous studies vision prior to releasing of the pneumoperitoneum to
detect any subtle bleeding from the abdominal wall.
Numerous prospective randomized trials,14-16 meta- Infectious complications like wound infection and intra
analyses,6-9 and systematic critical reviews10-13 have been abdominal abscesses are two variables by which the
conducted to assess the value of LA over OA, but there is techniques have been traditionally compared. However
some variability in the results of these studies.17 The most studies demonstrated reduced wound infection rate
overall mortality of OA is around 0.3%; and morbidity for LA. On the other hand, Klingler et al21 and Katkhouda
International Surgery Journal | January-March 2016 | Vol 3 | Issue 1 Page 131
Karatparambil A et al. Int Surg J. 2016 Feb;3(1):128-134
et al17 found that infectious complications were similar in was selected because the mandatory documentation
both groups. The incidence of intra abdominal abscess required for convalescence in the military, made for
formation was slightly higher in the laparoscopic accurate assessment of lost days. In this study there was
group.11-13 It is possible to reduce this if the sigmoid no difference in pain on days 1 and 7 postoperatively or
colon is retracted, the patient is placed in trendelenburg, in the time to return to work.23
and the pelvis is completely irrigated and aspirated under
direct vision.22 It has been previously reported that the presence of
appendiceal perforation or abscess is associated with
The operating room time, in most of the previous studies poorer outcome.26 Most studies, however, didn‟t stratify
was longer for the LA group, despite the subjective the findings by the presence of abscess or perforation. In
perception that it can be an easier operation.10-12 This may a large retrospective study, stratified analyses were
be due to the inclusion of additional steps for set up, performed for patients with or without perforation.26 The
insufflation, trocar entry under direct vision, and average length of hospital stay was significantly shorter
diagnostic laparoscopy. for LA patients with or without perforation. Similar
results were reported by Hebebrand et al31 from
Pain assessment can be done in two ways: Subjectively Germany. In an administrative database conducted by
by the visual analogue scale and objectively by the Ulrich and associates, median length of hospital stay was
tabulation of pain medications. The literature is divided shorter regardless of whether abscess or perforation was
on this subject. Some studies show less pain in the first present but, in- hospital infections were significantly
two days after LA.6-9 All but one of these studies were lower in the subset of LA patients without abscess or
non-blinded, thus reducing the validityof the results.16,23 perforation.
The question of whether LA decreases the length of The assessment of quality of life using the SF-36, by
hospitalization has been a matter of debate over the past Katkhouda et al17 showed improved scores in the LA
decade.18-24 The literature provides contradictory results. group for 3 of the 8 parameters, namely physical
Although some recent retrospective cohort studies or functioning, general health, physical health, and in the
chart reviews found LA associated with significantly general score.
shorter hospital stay,25-28 other retrospective
investigations reported non-significant differences.29-30 Gynaecological diseases are common causes of acute
Similarly some RCT associated LA with decreased abdominal symptoms, in childbearing women.
hospital stay; however others report no significant Laparoscopy makes definite determination of intra
differences. Even meta-analyses report controversial abdominal pathology possible and allows for avoidance
findings. Sauerland and associates summarized the results of unnecessary laparotomy and risk of adhesions, which
of 28 RCT and almost 3000 patients and reported a can be a cause of intestinal obstruction or infertility in
significant decrease in length of hospital stay in LA long term observation. But diagnostic laparoscopy was
group.9 Similar results were found by Golub and not included in our study.
colleagues,10 whereas another meta-analysis failed to
show a statistically significant difference.7 The current Results of present study
literature describes that the difference may be affected by
hospital factors or social habits. Moreover further In our study conducted at our hospital during a period
discrepancies may arise from diverse health care policies from January 2013 to January 2014, 200 patients
and insurance systems in different countries. underwent appendicectomy, of which 100 patients chose
for laparoscopic surgery. As 13 out of this had to be
The return to normal activity following appendicectomy converted to open surgery, finally 87cases of LA were
is also a subject of debate. A minimally invasive compared with 100 cases of OA. There was no mortality
operation by definition should allow for a quicker in either group.
recovery, shorter convalescence at home, and quicker
return to work. Several studies found LA to be associated The mean age of the patient population was 24.1 years.
with significantly earlier return to normal activities Majority of females chose an LA (70.1%), while majority
compared to OA. The results of a prospective RCT by of males (62 %) chose for an OA. Certain medical
Katkhouda and colleagues, based on the use of an conditions like bronchial asthma, COPD, and cardiac
objective instrument to measure the activity showed no diseases where general anaesthesia is considered risky,
difference in scores post operatively and at 2 weeks.17 also influenced the decision making. The direct cost
Others found improved postoperative activity in the LA involved in an LA was definitely higher than that in OA,
group. But the comparison among the studies is difficult and hence some economically backward class of patients
because of the variable definitions of activity. Results in could not afford an LA.
4 meta-analyses were statistically “highly
heterogenous”.6-9 In contrast, Ignacio et al23 carried out a There was no significant difference in incidence of
blinded prospective study in a tertiary care military based wound infection between the two groups. The incidence
hospital on healthy active-duty men. This specific cohort of intra-abdominal abscess which is thought to be more in
International Surgery Journal | January-March 2016 | Vol 3 | Issue 1 Page 132
Karatparambil A et al. Int Surg J. 2016 Feb;3(1):128-134
the LA group as per some previous studies was not 4. Michael JZ, Stanley WA, Douglas SS, David IS.
analysed in my study. Appendix and appendectomy. Maingot‟s abdominal
operations. 11th edition. 2007;21:589-608.
Duration of hospital stay was similar in both the study 5. Frazee RC, Roberts JW, Symmonds RE. A
groups and there are contradictory reports in different prospective randomized trial comparing open versus
studies, with similar as well as opposite results. laparoscopic appendectomy. Ann Surg.
1994;219:725-8.
The duration of return of bowel sounds and return to 6. Chung RS, Rowland DY, Li P. A meta-analysis of
normal activities were compared between the two groups randomized controlled trials of laparoscopic versus
.But there was no statistically significant difference in conventional appendectomy. Am J Surg.
either of these parameters. 1999;177:250-6.
7. Garbutt JM, Soper NJ, Shannon WD. Meta-analysis
CONCLUSION of randomized controlled trials comparing
laparoscopic and open appendectomy. Surg
Appendicectomy in uncomplicated acute appendicitis is a Laparosc Endosc. 1999;9:17-26.
safe procedure, regardless of the technique performed. 8. Golub R, Siddiqui F, Pohl D. Laparoscopic versus
open appendectomy: a meta-analysis. J Am Coll
OA is a time-tested procedure, with a small incision Surg. 1998;186:545-3.
and minimal morbidity. 9. Sauerland S, Lefering R, Holthausen U.
Epidemiologically there was no significant Laparoscopic vs conventional appendectomy: a
difference in selection of procedure between meta-analysis of randomized controlled trials. Arch
different age, but there was a definite preference for Surg. 1998;383:289-95.
laparoscopic appendicectomy among the female 10. Fingerhut A, Millat B, Borrie F. Laparoscopic
population. versus open appendectomy: time to decide. World J
Laparoscopic appendicectomy has no definite Surg. 1999;23:835-45.
advantages over its open counterpart, in terms of 11. McCall JL, Sharples K, Jadallah F. Systematic
postoperative analgesic requirement, duration of review of randomized controlled trials comparing
hospital stay, time to return of bowel sounds, time to laparoscopic with open appendicectomy. Br J Surg.
return to normal activities. 1997;84:1045-50.
There is no significant difference in wound infection 12. Sauerland S, Lefering R, Neugebauer EA.
between the two groups. Laparoscopic versus open surgery for suspected
Cost was definitely higher for the laparoscopic appendicitis. Cochrane Database Syst Rev.
procedure over the open procedure in my study 2002;(1):CD001546.
setting which was a factor against choosing LA. 13. Slim K, Pezet D, Chipponi J. Laparoscopic or open
To conclude, LA has no definite advantages over appendectomy ? critical review of randomized,
OA as per results of my study. controlled trials. Dis Colon Rectum. 1998;41:398-
403.
14. Tate JJ, Dawson JW, Chung SC. Laparoscopic
ACKNOWLEDGEMENT
versus open appendicectomy: prospective
randomised trial. Lancet. 1993;342:633-7.
I am expressing my thanks to my colleagues in the
15. Ortega AE, Hunter JG, Peters JH. A prospective,
department and the departmental secretary for collecting
randomized comparison of laparoscopic
and tabulating the data.
appendectomy with open appendectomy. Am J
Funding: No funding sources Surg. 1995;169:208-12.
Conflict of interest: None declared 16. Minne L, Varner D, Burnell A. Laparoscopic vs.
Ethical approval: The study was approved by the open appendectomy: prospective randomized study
institutional ethics committee of outcomes. Arch Surg. 1997;132:708-11.
17. Katkhouda N, Rodney JM, Shirin T. Laparoscopic
versus open appendectomy: A prospective
REFERENCES
randomized double-blind study. Ann Surg.
1. Samelson SL, Reyes HM. Management of 2005;242:439-50.
perforated appendicitis in children-revisited. Arch 18. Guller U, Hervey S, Purves H. Laparoscopic versus
Surg. 1987;122:691-6. open appendectomy: outcomes comparison based on
2. Editorial. A sound approach to the diagnosis of a large administrative database. Ann Surg.
acute appendicitis. Lancet. 1987;198-200. 2004;239(1):43-52.
3. Majeed AW, Troy G, Nicholl JP. Randomized, 19. Heikkinen TJ, Haukipuro K, Hulkko A. Cost-
prospective, single-blind comparison of effective appendectomy. Open or laparoscopic? A
laparoscopic versus small-incision cholecystectomy. prospective randomized study. Surg Endosc.
Lancet. 1996;347:989-94. 1998;12(10):1204-8.
International Surgery Journal | January-March 2016 | Vol 3 | Issue 1 Page 133
Karatparambil A et al. Int Surg J. 2016 Feb;3(1):128-134
20. Pedersen AG, Petersen OB, Wara P. Randomized appendectomy in 720 patients. Surg Laparosc
clinical trial of laparoscopic versus open Endosc. 1996;6:205-9.
appendicectomy. Br J Surg. 2001;88:200-5. 27. Heinzelmann M, Simmen HP, Cummins AS. Is
21. Klingler A, Henle KP, Beller S. Laparoscopic laparoscopic appendectomy the new „gold
appendectomy does not change the incidence of standard‟? Arch Surg. 1995;130:782-5.
postoperative infectious complications. Am J Surg. 28. Kurtz RJ, Heimann TM. Comparison of open and
1998;175:232-5. laparoscopic treatment of acute appendicitis. Am J
22. Katkhouda N, Friedlander MH, Grant SW. Surg. 2001;182:211-4.
Intraabdominal abscess rate after laparoscopic 29. Moberg AC, Montgomery A. Appendicitis:
appendectomy. Am J Surg. 2000;180:456-9. laparoscopic versus conventional operation: a study
23. Ignacio RC, Burke R, Spencer D. Laparoscopic and review of literature. Surg Laparosc Endosc.
versus open appendectomy: what is the real 1997;7:459-63.
difference? results of a prospective randomized 30. Fallahzadeh H. Should a laparoscopic
double-blinded trial. SurgEndosc. 2004;18(2):334-7. appendectomy be done? Am Surg. 1998;64:231-3.
24. Temple LK, Litwin DE, McLeod RS. A meta- 31. Hebebrand D, Troidl H, Spangenberger W.
analysis of laparoscopic versus open appendectomy Laparoscopic or classical appendectomy? A
in patients suspected of having acute appendicitis. prospective randomized study. Chirurg.
Can J Surg. 1999;42:377-83. 1994;65:112-20.
25. Vallina VL, Velasco JM, McCulloch CS.
Laparoscopic versus conventional appendectomy. Cite this article as: Karatparambil A,
Ann Surg. 1993;218:685-92. Kummankandath SA, Mannarakkal R, Nalakath MR,
26. Richards KF, Fisher KS, Flores JH. Laparoscopic Babu D. Laparoscopic versus open appandicectomy: a
appendectomy: comparison with open comparative study. Int Surg J 2016;3:128-34.
International Surgery Journal | January-March 2016 | Vol 3 | Issue 1 Page 134
You might also like
- Orthopedic LogbookDocument152 pagesOrthopedic LogbookIslam Amin100% (1)
- DNB Questions Year WiseDocument104 pagesDNB Questions Year WiseSirisha Ckv100% (4)
- Improved Outcomes in Colon and Rectal SurgeryDocument432 pagesImproved Outcomes in Colon and Rectal SurgeryMiguel Angel AguirreNo ratings yet
- Laparoscopic Versus Open Resection For TDocument8 pagesLaparoscopic Versus Open Resection For TElena CaterevNo ratings yet
- Apendisitis MRM 3Document8 pagesApendisitis MRM 3siti solikhaNo ratings yet
- Versus: Laparoscopic Open Appendectomy: Which Way To Go?Document6 pagesVersus: Laparoscopic Open Appendectomy: Which Way To Go?Claudiu Ungureanu ClauNo ratings yet
- Emergency Inguinal Hernia Repair Under Local Anesthesia: A 5-Year Experience in A Teaching HospitalDocument5 pagesEmergency Inguinal Hernia Repair Under Local Anesthesia: A 5-Year Experience in A Teaching HospitalleonardoNo ratings yet
- Journal Homepage: - : Manuscript HistoryDocument9 pagesJournal Homepage: - : Manuscript HistoryIJAR JOURNALNo ratings yet
- Acute Appendicitis: Position Paper, WSES, 2013: Review Open AccessDocument4 pagesAcute Appendicitis: Position Paper, WSES, 2013: Review Open AccessgamhaelNo ratings yet
- Ebm AppendectomyDocument20 pagesEbm AppendectomyMichael ChenNo ratings yet
- Laparoscopic Peptic Ulcer Perforation Closure: The Preferred ChoiceDocument5 pagesLaparoscopic Peptic Ulcer Perforation Closure: The Preferred ChoiceHanny FadhilaNo ratings yet
- A Prospective Comparativestudy of Open Versus Laparoscopic Appendectomy: A Single Unit StudyDocument8 pagesA Prospective Comparativestudy of Open Versus Laparoscopic Appendectomy: A Single Unit StudyIJAR JOURNALNo ratings yet
- Xiao 2014Document10 pagesXiao 2014AndikaNo ratings yet
- Laparoscopic Appendectomy PostoperativeDocument6 pagesLaparoscopic Appendectomy PostoperativeDamal An NasherNo ratings yet
- 014 - Primary-Colorectal-Cancer - 2023 - Surgical-Oncology-Clinics-of-North-AmericaDocument16 pages014 - Primary-Colorectal-Cancer - 2023 - Surgical-Oncology-Clinics-of-North-AmericaDr-Mohammad Ali-Fayiz Al TamimiNo ratings yet
- Original ArticlesDocument18 pagesOriginal ArticlesvNo ratings yet
- 1 s2.0 S1743919116308421 MainDocument10 pages1 s2.0 S1743919116308421 MainRony RonyNo ratings yet
- Laparoscopic Appendectomy PDFDocument4 pagesLaparoscopic Appendectomy PDFdydydyNo ratings yet
- Gastrectomía LaparoscópicaDocument7 pagesGastrectomía LaparoscópicaGreyza VelazcoNo ratings yet
- An Updated Meta Analysis of Laparoscopic Versus Open Repair For Perforated Peptic UlcerDocument13 pagesAn Updated Meta Analysis of Laparoscopic Versus Open Repair For Perforated Peptic UlcerSANDRA MILENA GUTIERREZ CAÑASNo ratings yet
- Appendicitis NaddlerDocument6 pagesAppendicitis NaddlerMedardo ApoloNo ratings yet
- Laparaskopi PeritonitisDocument5 pagesLaparaskopi PeritonitisPutri RiszaNo ratings yet
- Tiwari 2011Document6 pagesTiwari 2011syeda rabikaNo ratings yet
- Apendicitis - LaparosDocument3 pagesApendicitis - LaparosLaura CampañaNo ratings yet
- Perbedaan Penanganan Antara Laparoskopi Vs Open Repair Pada Perforasi GasterDocument7 pagesPerbedaan Penanganan Antara Laparoskopi Vs Open Repair Pada Perforasi GasterAfiani JannahNo ratings yet
- A Prospective Treatment Protocol For Outpatient Laparoscopic Appendectomy For Acute AppendicitisDocument5 pagesA Prospective Treatment Protocol For Outpatient Laparoscopic Appendectomy For Acute AppendicitisBenjamin PaulinNo ratings yet
- Acute Appendicitis in AdultsDocument19 pagesAcute Appendicitis in Adultsdimi firmatoNo ratings yet
- Corto y Largo PlazoDocument6 pagesCorto y Largo PlazoElard Paredes MacedoNo ratings yet
- 268 2011 Article 1088 PDFDocument6 pages268 2011 Article 1088 PDFIoel Tovar TrovaNo ratings yet
- Laparoscopia Versus Laparotomía para El Manejo Del Traumatismo Abdominal - Revisión Sistemática y MetanálisisDocument13 pagesLaparoscopia Versus Laparotomía para El Manejo Del Traumatismo Abdominal - Revisión Sistemática y MetanálisisLuis Miguel Díaz VegaNo ratings yet
- Laparoscopic Appendectomy For Complicated Appendicitis - An Evaluation of Postoperative Factors.Document5 pagesLaparoscopic Appendectomy For Complicated Appendicitis - An Evaluation of Postoperative Factors.Juan Carlos SantamariaNo ratings yet
- 2015 Laparoscopic Surgery in Abdominal Trauma A Single Center Review of A 7-Year ExperienceDocument7 pages2015 Laparoscopic Surgery in Abdominal Trauma A Single Center Review of A 7-Year ExperiencejohnnhekoNo ratings yet
- Laparoscopic Vs Open Appendectomy: Which Way To Go?Document22 pagesLaparoscopic Vs Open Appendectomy: Which Way To Go?fahryzal_noteNo ratings yet
- Reoperative Antireflux Surgery For Failed Fundoplication: An Analysis of Outcomes in 275 PatientsDocument8 pagesReoperative Antireflux Surgery For Failed Fundoplication: An Analysis of Outcomes in 275 PatientsDiego Andres VasquezNo ratings yet
- 1 s2.0 S0002961013004558 Main PDFDocument11 pages1 s2.0 S0002961013004558 Main PDFCarlos AlbertoNo ratings yet
- A Randomized Trial of Laparoscopic Versus Open Surgery For Rectal CancerDocument9 pagesA Randomized Trial of Laparoscopic Versus Open Surgery For Rectal CancerFarizka Dwinda HNo ratings yet
- Isj-5899 oDocument5 pagesIsj-5899 oAbhiram MundleNo ratings yet
- World Journal of Emergency Surgery: Emergency Laparoscopy - Current Best PracticeDocument9 pagesWorld Journal of Emergency Surgery: Emergency Laparoscopy - Current Best PracticeHendra JojoNo ratings yet
- Jurnal Keperawatan Medikal BedahDocument10 pagesJurnal Keperawatan Medikal Bedahtotoles100% (2)
- Fonc 09 00597Document13 pagesFonc 09 00597Giann PersonaNo ratings yet
- Conventional Versus Laparoscopic Surgery For Acute AppendicitisDocument4 pagesConventional Versus Laparoscopic Surgery For Acute AppendicitisAna Luiza MatosNo ratings yet
- @medicinejournal European Journal of Pediatric Surgery January 2020Document126 pages@medicinejournal European Journal of Pediatric Surgery January 2020Ricardo Uzcategui ArreguiNo ratings yet
- The Incidence and Risk of Early Postoperative Small Bowel Obstruction After Laparoscopic Resection For Colorectal Cancer 2014Document7 pagesThe Incidence and Risk of Early Postoperative Small Bowel Obstruction After Laparoscopic Resection For Colorectal Cancer 2014alemago90No ratings yet
- 1 Bjs 10662Document8 pages1 Bjs 10662Vu Duy KienNo ratings yet
- Is 9Document9 pagesIs 9intan juitaNo ratings yet
- Laparoscopic Ventral Hernia Repair With Tacker Only Mesh Fixation: Single Centre ExperienceDocument5 pagesLaparoscopic Ventral Hernia Repair With Tacker Only Mesh Fixation: Single Centre ExperienceMudassar SattarNo ratings yet
- Could Laparoscopic Colon and Rectal Surgery Become The Standard of Care? A Review and Experience With 750 ProceduresDocument9 pagesCould Laparoscopic Colon and Rectal Surgery Become The Standard of Care? A Review and Experience With 750 ProcedurespingusNo ratings yet
- Complicated AppendicitisDocument4 pagesComplicated AppendicitisMedardo ApoloNo ratings yet
- El Beheiry2019Document4 pagesEl Beheiry2019achmadaNo ratings yet
- qt5kh1c39r NosplashDocument12 pagesqt5kh1c39r NosplashSusieNo ratings yet
- Laparoscopic Versus Conventional Appendectomy - A Meta-Analysis of Randomized Controlled TrialsDocument8 pagesLaparoscopic Versus Conventional Appendectomy - A Meta-Analysis of Randomized Controlled TrialsAdrian HaningNo ratings yet
- f194 DikonversiDocument5 pagesf194 DikonversiFarizka Dwinda HNo ratings yet
- Management of Perforated Peptic Ulcer in A District General HospitalDocument5 pagesManagement of Perforated Peptic Ulcer in A District General HospitalNurul Fitrawati RidwanNo ratings yet
- Bun V34N3p223Document6 pagesBun V34N3p223pingusNo ratings yet
- Single Incision Laparoscopic Appendicectomy Versus Conventional Laparoscopic Appendicectomy-A Prospective StudyDocument6 pagesSingle Incision Laparoscopic Appendicectomy Versus Conventional Laparoscopic Appendicectomy-A Prospective StudySabreen SaniaNo ratings yet
- Journal AppDocument3 pagesJournal AppliqqamuqitaNo ratings yet
- Jurnal 3 AppDocument4 pagesJurnal 3 AppmaulidaangrainiNo ratings yet
- Laparoscopic Correction of Perforated Peptic Ulcer First Choice A Review of LiteratureDocument9 pagesLaparoscopic Correction of Perforated Peptic Ulcer First Choice A Review of LiteratureLe Hu ThaNo ratings yet
- Moberg 2007Document5 pagesMoberg 2007Julio Adan Campos BadilloNo ratings yet
- MOC IV 2014 Laparoscopy and Elective Colon Resection June 2012Document18 pagesMOC IV 2014 Laparoscopy and Elective Colon Resection June 2012pingusNo ratings yet
- IMU Learning Outcome: Psychomotor SkillsDocument11 pagesIMU Learning Outcome: Psychomotor SkillsRameshNo ratings yet
- Outcome of Total Laparoscopic HysterectomyDocument4 pagesOutcome of Total Laparoscopic HysterectomyDanica SavićNo ratings yet
- Top Trials in Gastroenterology & HepatologyFrom EverandTop Trials in Gastroenterology & HepatologyRating: 4.5 out of 5 stars4.5/5 (7)
- Iranjradiol 10 14Document7 pagesIranjradiol 10 14ChristianWicaksonoNo ratings yet
- 117 1445002005 PDFDocument7 pages117 1445002005 PDFChristianWicaksonoNo ratings yet
- Nej Mo A 1601747Document11 pagesNej Mo A 1601747ChristianWicaksonoNo ratings yet
- Dermatology 1993 186 1 23-31Document12 pagesDermatology 1993 186 1 23-31ChristianWicaksonoNo ratings yet
- Thali - Virtopsy, A New Imaging Horizon in Forensic Pathology, Virtual Autopsy by Postmortem MSCT and MRI, A Feasibility Study - 2003 - J Forensic Sci PDFDocument18 pagesThali - Virtopsy, A New Imaging Horizon in Forensic Pathology, Virtual Autopsy by Postmortem MSCT and MRI, A Feasibility Study - 2003 - J Forensic Sci PDFChristianWicaksonoNo ratings yet
- The Power of ColorDocument2 pagesThe Power of ColorChristianWicaksonoNo ratings yet
- Jurnal 1Document6 pagesJurnal 1ChristianWicaksonoNo ratings yet
- Bixin DryingDocument7 pagesBixin DryingChristianWicaksonoNo ratings yet
- Ijmm 32 3 539 PDFDocument5 pagesIjmm 32 3 539 PDFChristianWicaksonoNo ratings yet
- Anesthesia ConsentDocument2 pagesAnesthesia ConsentRAMAPATI SANYALNo ratings yet
- UntitledDocument38 pagesUntitledChandan ChatterjeeNo ratings yet
- **醫生診金收費 (2021) - 中環鍾經略醫生【皮膚科碩士 X 美容醫學碩士】(課程案例研究)Document7 pages**醫生診金收費 (2021) - 中環鍾經略醫生【皮膚科碩士 X 美容醫學碩士】(課程案例研究)Hemkerovner Keresztszegh von Kolowrat-KrakowskyNo ratings yet
- Keloids Which Types Can Be Excised Without Risk.17Document9 pagesKeloids Which Types Can Be Excised Without Risk.17ban huỳnhNo ratings yet
- Surgical Management For Cryptorchidism With Nursing ManagementsDocument4 pagesSurgical Management For Cryptorchidism With Nursing ManagementsAprille Claire MoralesNo ratings yet
- Roadmap To Choosing A Medical Specialty PDFDocument4 pagesRoadmap To Choosing A Medical Specialty PDFd-fbuser-20491778No ratings yet
- Horizon - Clip - Size - CardretDocument12 pagesHorizon - Clip - Size - CardretDerkis MarcanoNo ratings yet
- Osteotomies Jarthrodesis JDocument41 pagesOsteotomies Jarthrodesis Jdesire kbpNo ratings yet
- Scientific Events Distribution PDFDocument9 pagesScientific Events Distribution PDFCodrin FodorNo ratings yet
- FAST-FIX™ 360 Meniscal Repair SystemDocument12 pagesFAST-FIX™ 360 Meniscal Repair Systemehabede6445No ratings yet
- Practice PerfectDocument10 pagesPractice PerfectzranNo ratings yet
- Export ReportDocument24 pagesExport Reportpranit.gumgaonkarNo ratings yet
- PGDIM2015Document12 pagesPGDIM2015haneefmdfNo ratings yet
- Service Standard 09B Clinical Services - Surgical Related ServicesDocument30 pagesService Standard 09B Clinical Services - Surgical Related ServicesSuhaimeNo ratings yet
- Sis Tablas Dra. OdpDocument11 pagesSis Tablas Dra. OdpmargariamarisolfloresNo ratings yet
- Nasal Septal PerforationDocument12 pagesNasal Septal PerforationRini RahmawulandariNo ratings yet
- Dental Accreditation StandardsDocument66 pagesDental Accreditation Standardsdhir.ankurNo ratings yet
- Nylon LoopDocument4 pagesNylon LooporlandgpicadoNo ratings yet
- Kim Kunzman ResumeDocument3 pagesKim Kunzman Resumeapi-280455698No ratings yet
- Massry - Management of Postblepharoplasty Lower Eyelid RetractionDocument10 pagesMassry - Management of Postblepharoplasty Lower Eyelid RetractionLuiggi Fayad100% (1)
- Enhanced Recovery After Surgery JournalDocument9 pagesEnhanced Recovery After Surgery JournalDea DickytaNo ratings yet
- Instrument OrtopediDocument2 pagesInstrument Ortopediinstalasi bedah sentralNo ratings yet
- Pi Is 0161642015004194Document8 pagesPi Is 0161642015004194debbyNo ratings yet
- Medical Department OpthomticDocument2 pagesMedical Department OpthomticdkhatriNo ratings yet
- Revision Total Knee Arthroplasty: Principles of Management: Israel Orthopaedic Association December, 2012Document35 pagesRevision Total Knee Arthroplasty: Principles of Management: Israel Orthopaedic Association December, 2012TEJA B.M.K.PNo ratings yet
- Full Pdfpage31Document153 pagesFull Pdfpage31Keneuoe MokoenaNo ratings yet
- VIVO-Operation Theatre Technician (OTT) : ObjectivesDocument1 pageVIVO-Operation Theatre Technician (OTT) : ObjectivesFredy PaulNo ratings yet