Professional Documents
Culture Documents
Oxytocin
Oxytocin
Uploaded by
Nurkholis Amin0 ratings0% found this document useful (0 votes)
50 views2 pagesOxytocin is a hormone used to induce labor and control postpartum bleeding. It works by stimulating uterine contractions. When given intravenously, it must be administered slowly and the patient monitored closely for signs of water intoxication and changes in fetal heart rate or contractions. Nurses assess contraction strength and frequency, uterine tone, and fetal heart rate during administration and watch for signs of water retention like hyponatremia. Oxytocin requires dilution and is given via infusion pump or intramuscular injection to control dosage.
Original Description:
oxytocin
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentOxytocin is a hormone used to induce labor and control postpartum bleeding. It works by stimulating uterine contractions. When given intravenously, it must be administered slowly and the patient monitored closely for signs of water intoxication and changes in fetal heart rate or contractions. Nurses assess contraction strength and frequency, uterine tone, and fetal heart rate during administration and watch for signs of water retention like hyponatremia. Oxytocin requires dilution and is given via infusion pump or intramuscular injection to control dosage.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
0 ratings0% found this document useful (0 votes)
50 views2 pagesOxytocin
Oxytocin
Uploaded by
Nurkholis AminOxytocin is a hormone used to induce labor and control postpartum bleeding. It works by stimulating uterine contractions. When given intravenously, it must be administered slowly and the patient monitored closely for signs of water intoxication and changes in fetal heart rate or contractions. Nurses assess contraction strength and frequency, uterine tone, and fetal heart rate during administration and watch for signs of water retention like hyponatremia. Oxytocin requires dilution and is given via infusion pump or intramuscular injection to control dosage.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
You are on page 1of 2
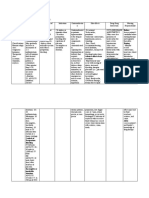
Name /bks_53161_deglins_md_disk/oxytocin 03/14/2014 07:53AM Plate # 0-Composite pg 1 # 1
1 High Alert ternal— hypotension; fetal, arrhythmias. F and E: maternal— hypochloremia,
hyponatremia, water intoxication. Misc: maternal—q uterine motility, painful
PDF Page #1
oxytocin (ox-i-toe-sin) contractions, abruptio placentae,puterine blood flow, hypersensitivity.
Pitocin Interactions
Classification Drug-Drug: Severe hypertension may occur if oxytocin follows administration of
Therapeutic: hormones vasopressors.
Pharmacologic: oxytocics
Pregnancy Category X Route/Dosage
Induction/Stimulation of Labor
Indications IV (Adults): 0.5– 1 milliunits/min;qby 1– 2 milliunits/min q 30– 60 min until de-
IV: Induction of labor at term. IV: Facilitation of threatened abortion. IV, IM: Post- sired contraction pattern established; dose may bepafter desired frequency of con-
partum control of bleeding after expulsion of the placenta. tractions is reached and labor has progressed to 5-6 cm dilation.
Action Postpartum Hemorrhage
Stimulates uterine smooth muscle, producing uterine contractions similar to those in IV (Adults): 10 units infused at 20– 40 milliunits/min.
spontaneous labor. Has vasopressor and antidiuretic effects. Therapeutic Ef- IM (Adults): 10 units after delivery of placenta.
fects: Induction of labor. Control of postpartum bleeding.
Pharmacokinetics Incomplete/Inevitable Abortion
Absorption: IV administration results in 100% bioavailability. IV (Adults): 10 units at a rate of 20– 40 milliunits/min.
Distribution: Widely distributed in extracellular fluid. Small amounts reach fetal NURSING IMPLICATIONS
circulation.
Metabolism and Excretion: Rapidly metabolized by liver and kidneys. Assessment
● Fetal maturity, presentation, and pelvic adequacy should be assessed prior to ad-
Half-life: 3– 9 min.
ministration of oxytocin for induction of labor.
TIME/ACTION PROFILE (reduction in uterine contractions) ● Assess character, frequency, and duration of uterine contractions; resting uterine
ROUTE ONSET PEAK DURATION tone; and fetal heart rate frequently throughout administration. If contractions oc-
IV immediate unknown 1 hr cur ⬍2 min apart and are ⬎50– 65 mm Hg on monitor, if they last 60– 90 sec or
IM 3–5 min unknown 30–60 min longer, or if a significant change in fetal heart rate develops, stop infusion and turn
patient on her left side to prevent fetal anoxia. Notify health care professional im-
Contraindications/Precautions mediately.
Contraindicated in: Hypersensitivity; Anticipated nonvaginal delivery. ● Monitor maternal BP and pulse frequently and fetal heart rate continuously
Use Cautiously in: OB: First and second stages of labor; slow infusion over 24 hr throughout administration.
has caused water intoxication with seizure and coma or maternal death due to oxy- ● This drug occasionally causes water intoxication. Monitor patient for signs and
tocin’s antidiuretic effect. symptoms (drowsiness, listlessness, confusion, headache, anuria) and notify phy-
Adverse Reactions/Side Effects sician or other health care professional if they occur.
Maternal adverse reactions are noted for IV use only CNS: maternal— COMA, SEI- ● Lab Test Considerations: Monitor maternal electrolytes. Water retention may
ZURES; fetal, INTRACRANIAL HEMORRHAGE. Resp: fetal— ASPHYXIA, hypoxia. CV: ma- result in hypochloremia or hyponatremia.
⫽ Canadian drug name. ⫽ Genetic Implication. CAPITALS indicate life-threatening, underlines indicate most frequent. Strikethrough ⫽ Discontinued.
Name /bks_53161_deglins_md_disk/oxytocin 03/14/2014 07:53AM Plate # 0-Composite pg 2 # 2
2 setron, heparin, hydrocortisone sodium succinate, hydromorphone, imipenem/
cilastatin, isoproterenol, ketamine, ketorolac, labetalol, leucovorin calcium, lev-
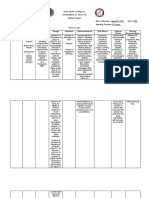
Potential Nursing Diagnoses ofloxacin, lidocaine, linezolid, lorazepam, magnesium sulfate, mannitol, meperi- PDF Page #2
Deficient knowledge, related to medication regimen (Patient/Family Teaching) dine, meropenem, metaraminol, methyldopate, methylprednisolone, metoclopra-
mide, metoprolol, metronidazole, midazolam, milrinone, morphine,
Implementation moxifloxacin, multivitamins, mycophenolate, nafcillin, nalbuphine, naloxone, ne-
● Do not administer oxytocin simultaneously by more than one route.
siritide, nicardipine, nitroglycerin, nitroprusside, norepinephrine, ondansetron,
IV Administration oxacillin, palonosetron, pamidronate, papaverine, penicillin G , pentamdine, pen-
● Continuous Infusion: Rotate infusion container to ensure thorough mixing. tazocine, pentobarbital, phenobarbital, phentolamine, phenylephrine, phytona-
Store solution in refrigerator, but do not freeze. dione, piperacillin/tazobactam, potassium acetate, potassium chloride, potassium
● Infuse via infusion pump for accurate dose. Oxytocin should be connected via Y- phosphates, procainamide, prochlorperazine, promethazine, propranolol, prot-
site injection to an IV of 0.9% NaCl for use during adverse reactions. amine, pyridoxime, quinupristin/dalfopristin, ranitidine, sodium acetate, sodium
● Magnesium sulfate should be available if needed for relaxation of myometrium. bicarbonate, sodium phosphates, streptokinase, succinylcholine, sufentanil, tac-
● Induction of Labor: Diluent: Dilute 1 mL (10 units) in 1 L of compatible in- rolimus, theophylline, thiamine, ticarcillin/clavulanate, tigecycline, tirofiban, to-
fusion fluid (0.9% NaCl, D5W, or LR). Concentration: 10 milliunits/mL. Rate: bramycin, tolazoline, vancomycin, vasopressin, verapamil, vitamin B complex
Begin infusion at 0.5– 2 milliunits/min (0.05– 0.2 mL); increase in increments of with C, voriconazole, warfarin, zidovudine, zoledronic acid.
1– 2 milliunits/min at 15– 30-min intervals until contractions simulate normal la- ● Y-Site Incompatibility: dantrolene, diazepam, diazoxide, indomethacin,
bor. methohexital, phenytoin, remifentanil, trimethoprim/sulfamethoxazole.
● Postpartum Bleeding: Diluent: For control of postpartum bleeding, dilute 1– ● Solution Compatibility: dextrose/Ringer’s or lactated Ringer’s combinations,
4 mL (10– 40 units) in 1 L of compatible infusion fluid. Concentration: 10– dextrose/saline combinations, Ringer’s or lactated Ringer’s injection, D5W,
40 milliunits/mL. Rate: Begin infusion at a rate of 20– 40 milliunits/min to con- D10W, 0.45% NaCl, 0.9% NaCl.
trol uterine atony. Adjust rate as indicated.
● Incomplete or Inevitable Abortion: Diluent: For incomplete or inevitable Patient/Family Teaching
abortion, dilute 1 mL (10 units) in 500 mL of 0.9% NaCl or D5W. Concentra- ● Advise patient to expect contractions similar to menstrual cramps after adminis-
tion: 20 milliunits/mL. Rate: Infuse at a rate of 20– 40 milliunits/min. tration has started.
● Y-Site Compatibility: acyclovir, alfentanil, allopurinol, amikacin, aminocaproic
acid, aminophylline, amphotericin B liposome, anidulafungin, argatroban, ascor- Evaluation/Desired Outcomes
bic acid, atropine, azathioprine, azithromycin, aztreonam, benztropine, bivaliru- ● Onset of effective contractions.
din, bumetanide, buprenorphine, butorphanol, calcium chloride, calcium glu- ● Increase in uterine tone.
conate, capreomycin, caspofungin, cefazolin, cefepime, cefoperazone, ● Reduction in postpartum bleeding.
cefotaxime, cefotetan, cefoxitin, ceftazidime, ceftriaxone, cefuroxime, chloram-
phenicol, ciprofloxacin, cisatracurium, clindamycin, cyanocobalamin, cyclospor-
Why was this drug prescribed for your patient?
ine, daptomycin, dexamethasone, dexmedetomidine, digoxin, digoxin, diphen-
hydramine, dobutamine, dolasetron, dopamine, doxycycline, droperidol,
enalaprilat, ephedrine, epinephrine, epoetin alfa, eptifibatide, ertapenem, eryth-
romycin, esmolol, famotidine, fenoldopam, fentanyl, fluconazole, folic acid, fos-
carnet, fosphenytoin, furosemide, ganciclovir, gentamicin, glycopyrrolate, grani-
䉷 2015 F.A. Davis Company
You might also like
- Chat GPTDocument13 pagesChat GPTsuly maniyahNo ratings yet
- Nurse Practitioner Board ReviewFrom EverandNurse Practitioner Board ReviewRating: 5 out of 5 stars5/5 (1)
- London Cancer Mesna Guideline v1Document8 pagesLondon Cancer Mesna Guideline v1Nurkholis AminNo ratings yet
- NitinolDocument20 pagesNitinolTamara PricilaNo ratings yet
- Drugs Study and Discharge Plan Arnold and SelwynDocument17 pagesDrugs Study and Discharge Plan Arnold and SelwynArnold ZamoroNo ratings yet
- Drug Study On Labor and DeliveryDocument4 pagesDrug Study On Labor and DeliveryJune Dumdumaya67% (3)
- ACLS Drugs (2010)Document16 pagesACLS Drugs (2010)RN333100% (2)
- Drug Study-ncp-Abruptio Placentae (Oxytocin) - PeregrinoDocument3 pagesDrug Study-ncp-Abruptio Placentae (Oxytocin) - PeregrinoJOYCE ANN PEREGRINONo ratings yet
- Oxytocin Induction or Stimulation of Labor BeforeDocument4 pagesOxytocin Induction or Stimulation of Labor BeforeIrene Grace BalcuevaNo ratings yet
- Drug AnalysisDocument27 pagesDrug AnalysisCzarina Mae Quinones TadeoNo ratings yet
- OxytocinDocument1 pageOxytocinIvanne Hisoler100% (7)
- DfneruigrDocument3 pagesDfneruigrKapy KapsNo ratings yet
- DRUG STUDY-NCP-ABRUPTIO PLACENTAE (Oxytocin) - PeregrinoDocument3 pagesDRUG STUDY-NCP-ABRUPTIO PLACENTAE (Oxytocin) - PeregrinoJOYCE ANN PEREGRINONo ratings yet
- Methylergonovine Maleate (Methergine) Indication Contraindication Adverse Effect Action Nursing Consideration RationaleDocument5 pagesMethylergonovine Maleate (Methergine) Indication Contraindication Adverse Effect Action Nursing Consideration RationalekeenoxkyNo ratings yet
- OXYTOCINDocument3 pagesOXYTOCINJaye Aprile Adrianne KuizonNo ratings yet
- Drug Study Format 1Document3 pagesDrug Study Format 1Janeenne Fe Nicole SilvanoNo ratings yet
- Drug Study: (Oxytocin)Document10 pagesDrug Study: (Oxytocin)Shara Lailanie A. AzisNo ratings yet
- Drug Study For OxytocinDocument2 pagesDrug Study For OxytocinAngelica CorpuzNo ratings yet
- Drug Study OxytocinDocument2 pagesDrug Study Oxytocinrica sebabillonesNo ratings yet
- OxytocinDocument3 pagesOxytocinjints poterNo ratings yet
- OxytocinDocument3 pagesOxytocinjints poterNo ratings yet
- Generic NameDocument3 pagesGeneric NameSittie Nashieva A. UsmanNo ratings yet
- Drug StudyDocument12 pagesDrug StudyDaniel Andre S. SomorayNo ratings yet
- Task IncomingDocument14 pagesTask Incomingmonica mittiamNo ratings yet
- St. Paul University Dumaguete St. Paul University System College of Nursing ISO 9001Document16 pagesSt. Paul University Dumaguete St. Paul University System College of Nursing ISO 9001Dinarkram Rabreca EculNo ratings yet
- OxytocinDocument2 pagesOxytocinshefawNo ratings yet
- Generic/ Brand Name Classification Mechanism of Action Indication Side Effects Nursing ImplicationsDocument14 pagesGeneric/ Brand Name Classification Mechanism of Action Indication Side Effects Nursing ImplicationsbokanegNo ratings yet
- EtoposideDocument3 pagesEtoposideNoamiNo ratings yet
- QUE - Sandara Section 7 OXYTOCIN - DrugStudyDocument4 pagesQUE - Sandara Section 7 OXYTOCIN - DrugStudyquesandara16No ratings yet
- CefotaximeDocument3 pagesCefotaximeMargotNo ratings yet
- JINGCO - BSN 2-D - Module-6-Drug-StudyDocument16 pagesJINGCO - BSN 2-D - Module-6-Drug-StudyJashtine JingcoNo ratings yet
- 11 Drug StudyDocument13 pages11 Drug Studykwon nanaNo ratings yet
- Drug Name Mechanism of Action Indication Contraindication Side Effects/ Adverse Effects Nursing Considerations Generic Name Oxytocin Side EffectsDocument15 pagesDrug Name Mechanism of Action Indication Contraindication Side Effects/ Adverse Effects Nursing Considerations Generic Name Oxytocin Side EffectsRomwella May AlgoNo ratings yet
- Nursing Pharmacology HandoutsDocument10 pagesNursing Pharmacology HandoutsMICHAELA TIMBOLNo ratings yet
- OxytocinDocument2 pagesOxytocinwishnieizelwyn.daguioNo ratings yet
- Trimester or As Prescribed by The PhysicianDocument4 pagesTrimester or As Prescribed by The PhysicianDonna Mae BoolNo ratings yet
- OXYTOCINDocument2 pagesOXYTOCINPang ProjectNo ratings yet
- Cancer Cell-Specific AgentsDocument5 pagesCancer Cell-Specific AgentsRomwella May AlgoNo ratings yet
- Drug StudyDocument10 pagesDrug StudyFrancis BelotindosNo ratings yet
- MCN Lect Hypertensive Disorders in PregnancyDocument4 pagesMCN Lect Hypertensive Disorders in PregnancyAmethystNo ratings yet
- Drug Classificati On Indications Action Route/Dos e Side Effects Patient Teaching Nursing ImplicationsDocument7 pagesDrug Classificati On Indications Action Route/Dos e Side Effects Patient Teaching Nursing ImplicationsJenny NguyenNo ratings yet
- Suxamethonium Dosage, Side Effect MIMS - Com PhilippinesDocument2 pagesSuxamethonium Dosage, Side Effect MIMS - Com PhilippinesWay LyanNo ratings yet
- Pharmacotherapeutics in ObstetricsDocument14 pagesPharmacotherapeutics in ObstetricsmercyNo ratings yet
- ErythromycinDocument2 pagesErythromycinBtob meloNo ratings yet
- Family and Drug MOA Physiologic Effect Indications Side EffectsDocument11 pagesFamily and Drug MOA Physiologic Effect Indications Side EffectsraquelNo ratings yet
- Roxipan (Oxytocin) - Drug StudyDocument4 pagesRoxipan (Oxytocin) - Drug StudyIzza DeloriaNo ratings yet
- DRUG STUDY and CASE ANALYSISDocument6 pagesDRUG STUDY and CASE ANALYSISMa. Kaile Shyla LlacarNo ratings yet
- Oxytocin Drug StudyDocument2 pagesOxytocin Drug StudyRem remNo ratings yet
- Bondoc Drug StudyDocument3 pagesBondoc Drug StudyJan Dale BondocNo ratings yet
- DrugDocument11 pagesDrugrihamNo ratings yet
- 15 DrugsDocument10 pages15 Drugscharles babasaNo ratings yet
- PHINMA Education Network College of Health SciencesDocument2 pagesPHINMA Education Network College of Health SciencesJozarine ChelseaNo ratings yet
- Ceftriaxone PDFDocument3 pagesCeftriaxone PDFLauren JalandoniNo ratings yet
- Mannitol PDFDocument2 pagesMannitol PDFM MukulNo ratings yet
- Obat Ayu (Anestesi)Document11 pagesObat Ayu (Anestesi)Ayu PratiwiNo ratings yet
- Ampicillin PDFDocument3 pagesAmpicillin PDFandriNo ratings yet
- DR Drug Study: 401 2nd SemDocument2 pagesDR Drug Study: 401 2nd SemHazel Grace AhitoNo ratings yet
- RAMOS-BN Drug Study Delivery RoomDocument2 pagesRAMOS-BN Drug Study Delivery RoomLouwella RamosNo ratings yet
- Obstetric Medication ProfileDocument7 pagesObstetric Medication Profilejulie.wilkNo ratings yet
- L&D DrugsDocument3 pagesL&D DrugsJessica 'Baker' IsaacsNo ratings yet
- Pedia Drug StudyDocument11 pagesPedia Drug StudyPeetah PanNo ratings yet
- Drug Study OxytocinDocument3 pagesDrug Study OxytocinSheena Marie M. TarleNo ratings yet
- Isoxsuprine HydrochlorideDocument3 pagesIsoxsuprine HydrochloridePatricia Mae MirandaNo ratings yet
- My Mifespristone and Misoprostol Story: How I used mifepristone and misoprostol for a successful medical abortion and all you must know about these abortion pillsFrom EverandMy Mifespristone and Misoprostol Story: How I used mifepristone and misoprostol for a successful medical abortion and all you must know about these abortion pillsNo ratings yet
- 1111 09 PDFDocument7 pages1111 09 PDFNurkholis AminNo ratings yet
- Treatment and Prophylaxis of Ifosfamide-Induced Encephalopathy With Intravenous Methylene BlueDocument2 pagesTreatment and Prophylaxis of Ifosfamide-Induced Encephalopathy With Intravenous Methylene BlueNurkholis Amin0% (1)
- 15 NG - PPH Algorithm-Aug08Document8 pages15 NG - PPH Algorithm-Aug08Nurkholis AminNo ratings yet
- Ifosfamide: InjectionDocument2 pagesIfosfamide: InjectionNurkholis AminNo ratings yet
- Soluvit NinfDocument4 pagesSoluvit NinfNurkholis AminNo ratings yet
- Me Sna Dose GuidelinesDocument1 pageMe Sna Dose GuidelinesNurkholis AminNo ratings yet
- 15 NG - PPH Algorithm-Aug08Document1 page15 NG - PPH Algorithm-Aug08Nurkholis AminNo ratings yet
- IfosfamideDocument4 pagesIfosfamideNurkholis AminNo ratings yet
- Guidelines - In-Hospital ResuscitationDocument18 pagesGuidelines - In-Hospital ResuscitationparuNo ratings yet
- How A GPU Works: Kayvon Fatahalian 15-462 (Fall 2011)Document87 pagesHow A GPU Works: Kayvon Fatahalian 15-462 (Fall 2011)Michaele ErmiasNo ratings yet
- Decision Utah LighthouseDocument28 pagesDecision Utah LighthousemschwimmerNo ratings yet
- A Hybrid Intrution Detection Approach Based On Deep LearningDocument16 pagesA Hybrid Intrution Detection Approach Based On Deep LearningVictor KingbuilderNo ratings yet
- Buyer Decision ProcessDocument3 pagesBuyer Decision ProcesswahirumaisaNo ratings yet
- Code On Wages 2019, 2Document9 pagesCode On Wages 2019, 2Saxena M.No ratings yet
- EPDDocument34 pagesEPDRobin AbrahamNo ratings yet
- Fusion Apps Integration Patterns WPDocument36 pagesFusion Apps Integration Patterns WPPraveen KsNo ratings yet
- Display CAT PDFDocument2 pagesDisplay CAT PDFAndres130No ratings yet
- Powercrete R95Document2 pagesPowercrete R95arturomaravillaNo ratings yet
- Chapter 1 Computer SecurityDocument22 pagesChapter 1 Computer SecurityAjay GuptaNo ratings yet
- Group 8 Design Main Report + Appendix (1) 1 400Document400 pagesGroup 8 Design Main Report + Appendix (1) 1 400Manishaa Varatha RajuNo ratings yet
- Trad Ic Mock ExamDocument15 pagesTrad Ic Mock ExamArvin AltamiaNo ratings yet
- Doe School PlanDocument16 pagesDoe School PlanHNNNo ratings yet
- ETM-OT - Electronic Temperature Monitor: DescriptionDocument3 pagesETM-OT - Electronic Temperature Monitor: DescriptionMKNo ratings yet
- 3l/epublit of Tbe Bilippine9': Supreme !courtDocument15 pages3l/epublit of Tbe Bilippine9': Supreme !courtCesar ValeraNo ratings yet
- AdvertisingDocument16 pagesAdvertisingSun KambojNo ratings yet
- Cdi 3Document39 pagesCdi 3Argencel MaddelaNo ratings yet
- Connorm Edid6507-Assign 2Document27 pagesConnorm Edid6507-Assign 2api-399872156No ratings yet
- Gender Informality and PovertyDocument15 pagesGender Informality and Povertygauravparmar1No ratings yet
- Berea College B Ed FP Teaching SubmissionDocument520 pagesBerea College B Ed FP Teaching SubmissionGbengaNo ratings yet
- Criteria For Master Teacher: (With Additional Proposed Documents and The Specific Points As Support To Other Criteria)Document19 pagesCriteria For Master Teacher: (With Additional Proposed Documents and The Specific Points As Support To Other Criteria)Dennis ReyesNo ratings yet
- Minerals Potential - Minerals Law of Lao PDRDocument44 pagesMinerals Potential - Minerals Law of Lao PDRkhamsone pengmanivongNo ratings yet
- Turbine Blade Shop-Block 3 BhelDocument40 pagesTurbine Blade Shop-Block 3 Bheldeepak GuptaNo ratings yet
- Assignment 2-Groundwater MovementDocument2 pagesAssignment 2-Groundwater MovementPhước LêNo ratings yet
- Sheik Md. Maadul Hoque (ID 150201010035)Document49 pagesSheik Md. Maadul Hoque (ID 150201010035)Mizanur RahmanNo ratings yet
- Water Insulation - ENDocument9 pagesWater Insulation - ENNoorul Mufas MnNo ratings yet
- IMS JRDocument4 pagesIMS JRRyoNo ratings yet