Professional Documents
Culture Documents
The Diagnosis and Management Of: Tinea Capitis
The Diagnosis and Management Of: Tinea Capitis
Uploaded by
Quraisy jamal sahilOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
The Diagnosis and Management Of: Tinea Capitis
The Diagnosis and Management Of: Tinea Capitis
Uploaded by
Quraisy jamal sahilCopyright:
Available Formats
CLINICAL
Tinea capitis (scalp ringworm) is a common paediatric infection usually affecting school-aged children. The
commonest causative organisms are dermatophytes from the genera Trichophyton or Microsporum.
Dermatophytes are keratinophilic and invade the stratum corneum, hair and nails.
The diagnosis and
management of
TINEA CAPITIS
Prof HF Jordaan, Department of Dermatology, University of Stellenbosch
Summary capitis occurs occasionally in other age groups.
The fungistatic properties of post-pubertal sebum
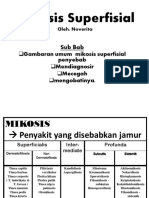
Dermatophytosis encompasses several distinct may repel dermatophytes.
clinical entities, namely tinea capitis (scalp
ringworm), tinea corporis (ringworm of glabrous The following morphological presentations
skin), tinea cruris (ringworm of the groin), tinea have been described: black dot type, sebor-
unguium or onychomycosis (ringworm of the rhoeic dermatitis type, gray patch type, yellow
nail), tinea pedis (ringworm of the feet), tinea patch type, pustular type, annular type, kerion,
barbae (ringworm of the beard), and tinea favus and dermatophytic mycetoma (Figures 1-
manuum (ringworm of the hand). 6). Combinations of these lesions are not
uncommon. The common denominator of all
Dermatophyte fungi causing tinea capitis can types is the presence of hair loss. Pruritus is
be divided into anthropophilic and zoophilic usually minimal. Infected hairs are brittle, and
organisms. Anthropophilic fungi grow preferen- by the third week, broken hairs are evident.
tially on humans, and the most common type Hair loss is subtle in the seborrhoeic type.
forms large conidia of approximately 3-4 mm in Secondary impetigo may complicate any form
diameter within the hair shaft (endothrix). of tinea capitis. Regional occipital lympha-
Common causes of endothrix infection include denopathy is not uncommon. Impetigo of the
Trichophyton tonsurans , T schoenleinii and T scalp should always arouse suspicion of under-
violaceum. Zoophilic fungi are acquired lying tinea capitis. Other causes of scalp
through direct contact with infected animals impetigo in this age group include pediculosis
(e.g. puppy, kitten). Smaller conidia of capitis, scabies, atopic dermatitis and primary
approximately 1-3 mm in diameter extend impetigo.
around the exterior of the hair shaft (ectothrix).
Ectothrix infection is caused by T verrucosum, T Dermatophyte infection of the scalp can usually
Note:
Contact INFOMED at the mentagrophytes, and all Microsporum be diagnosed clinically. Additional diagnostic
Tygerberg Campus species. methods include a potassium hydroxide (KOH)
Library at preparation and microscopy, culture on
mailto:infomed@sun.ac.za
to request one of Tinea capitis is seen most commonly in Sabouraud dextrose agar (SDA), Wood’s lamp
the references children younger than 10 years of age Peak examination and skin biopsy.
© Stellmed
Updates,Faculty of Health age range is in patients aged 3-7 years.
Sciences,Stellenbosch Gender distribution is approximately equal. Infection may resolve spontaneously at puberty.
University. Tinea capitis is the most common paediatric Treatment using X-ray epilation was reported in
All Articles are Peer
Reviewed. dermatophyte infection worldwide. Tinea 1904. Griseofulvin became available in the
8 SA Pharmaceutical Journal – October 2006
CLINICAL
1950s and is the treatment of choice at templating pregnancy. Adverse effects leaving the infected dark stubs visible
a dosage of 10-25 mg/kg/day for 6-8 are reported occasionally, including in the follicular orifices. Closely shaven
weeks. Drug absorption is enhanced headache, nausea, fatigue, abdominal hair may simulate black dot tinea
when fatty food is taken simultaneously discomfort, or transient rash; less capitis (personal observation). Black
(e.g. glass of milk). There are three common adverse reactions include urti- dot tinea capitis is caused by T
reasons for treatment failure with caria, diarrhoea, and photosensitivity; tonsurans and T schoenleinii.
griseofulvin: dosage too low, treatment may precipitate acute intermittent
duration too short, and, failure to take porphyria and systemic lupus ery- A kerion is an abscess-like lesion
the drug with a meal. The drug accu- thematosus in predisposed individuals. studded with pustules. Lesions heal with
mulates in keratin of the horny layer, scarring and permanent alopecia. Kerion
hair, and nails, rendering them resis- Alternative treatment methods include is commonly caused by T tonsurans.
tant to invasion by the fungus. Treat- itraconazole (Sporanox®), terbinafine
ment must continue long enough for (Lamisil®) and fluconazole (Diflucan ®). Favus is caused most commonly by T
infected keratin to be replaced by Although oral ketoconazole (Nizoral®) schoenleinii and occasionally by T
resistant keratin, usually 4-6 weeks. is an acceptable alternative, the risk of violaceum or Microsporum gypsum.
Resistant strains of dermatophytes are hepatotoxicity is significant. Topical Yellow, saucer-shaped crusts termed
rare. treatment is usually ineffective. Oral scutulae surround infected hair follicles.
steroids may help reduce the risk for Favus heals with scarring.
Contraindications include documented and extent of permanent alopecia in
hypersensitivity, porphyria and hepato- the treatment of kerion. Topical cortico- Dermatophytic mycetoma is uncommon
cellular failure. Griseofulvin may steroids should be avoided. Povidone- and is characterised by the presence of
decrease the hypoprothrombinoemic iodine (Betadine ® ) or selenium sul- one or more reddish nodules on the
activity of warfarin (adjust dose); phide shampoo may diminish the scalp. Histology shows granules com-
coadministration decreases contra- spread of spores. The shampoo is posed of masses of dermatophytes,
ceptive effects, resulting in break- applied twice weekly for 15 minutes for usually T rubrum, in a background of
through bleeding, amenorrhea, or un- 4 consecutive weeks. inflammation.
intended pregnancy; may reduce effects
of cyclosporine and salicylates; Clinical presentation, diagnosis Yellow patch tinea capitis is charac-
barbiturates may decrease griseofulvin and treatment terised by one, a few or several patches
effects. The oral form is embryotoxic and of hair loss covered fully or partially by
teratogenic to pregnant rats; there- fore, Black dot tinea capitis refers to an yellowish scale-crust.
do not prescribe for women con- infection with fractures of the hair
Figures 1 & 2: Child with one large, irregularly shaped area of scaling and several smaller Figure 3: Child with a large elevated plaque
scaly areas on the scalp. Note hair loss and crusting. devoid of hair. Extensive pustulation and
crusting are evident.
Figure 4: Gray patch tinea capitis above the Figure 5: Gray patch tinea capitis of the Figure 6: A kerion-like lesion. Note
ear involving the parietal area of the scalp. postauricular area. Note hair loss caused nodularity of the lesion.
by tight braiding
SA Pharmaceutical Journal – October 2006 9
CLINICAL
Secondary infection (= impetigo) by some cases the disease can cause the diagnosis of tinea capitis. Hair loss,
Staphylococcus aureus or beta severe emotional impairment in vul- not responding to treatment, may be an
haemolytic streptococci causes this nerable children and can destabilise indication for skin biopsy. Dermato-
appearance. Regional lymphadeno- family relationships. phytes may be visualised on routine
pathy is common. staining, but a PAS&D stain facilitates
Four diagnostic methods are identification of fungi. In endothrix
Gray patch tinea capitis is an ectothrix utilised in the diagnosis of tinea infection, spheric-to-box-like spores are
infection and by far the commonest capitis found within the hair shaft. In ectothrix
presentation seen at the Dermatology infection, organisms form a sheath
Clinic at Tygerberg Hospital. This form Potassium hydroxide and micro- around the hair shaft. The cuticle is
is characterised by one, a few or scopy destroyed. Fungal elements may also be
several patches of hair loss, of variable The belly of a number 15 blade is present in the epidermis and dermis.
shape and size with lack of applied to the surface of a scaly patch.
inflammation. Fine, grayish scales Scales are gently scraped off onto a In the differential diagnosis of tinea
cover the surface of these lesions. clean glass slide. A drop of 20% KOH capitis one should consider alopecia
Hairs in the involved area are dull, is placed next to the material and there- areata , primary impetigo, lupus
grayish, discoloured and broken off. after thoroughly mixed. The preparation erythematosus, psoriasis, seborrhoeic
is left for 15-20 minutes. Gentle heat dermatitis, secondary syphilis and
Seborrhoeic dermatitis-like tinea capitis may be applied. A coverslip is placed trichotillomania.
shows more or less diffuse scaling of on the glass slide and viewed with a
the scalp. Hair loss is often subtle. microscope (x 40 magnification). Alopecia areata is characterised by
Seborrhoeic dermatitis is extremely Rubbings (with a moist gauze pad or patches of complete hair loss, of
uncommon in this age group. toothbrush), pluckings or clippings from variable number, shape and size.
lesions may be prepared similarly. The Inflammatory changes are absent. The
The pustular type of tinea capitis refers presence of fungal hyphae and spores exclamation mark hairs seen in
to the presence of one or more areas of within (endothrix) or around (ectothrix) alopecia areata, in which broken hairs
hair loss, of variable shape and size, hair shafts is diagnostic. taper from the fractured end towards
peppered with pustules, scaling and the skin surface, are pathognomonic.
scale-crust. Culture on Sabouraud’s dextrose agar Alopecia areata is an autoimmune
Material is collected as for microscopy. disease. Regrowing hairs are usually
The annular type is characterised by Scales, crusts and/or hair are placed thin and non-pigmented.
papules or pustules forming a ring that between two glass sides, taped at the
may coalesce with other infected areas. ends and despatched to the laboratory. Primary impetigo is caused by S
Combinations of these morphological This material is incubated on SDA + aureus or group A beta haemolytic
presentations are not uncommon. cycloheximide (suppresses the growth of streptococci. Lesions show pustulation
environmental contaminant fungi) and and honey-coloured crusts. Hairs tend
Ide reactions are manifestations of the SDA + chloramphenicol (to prevent to be firmly seated in impetigo.
immune response to dermatophytes. bacterial overgrowth). Most dermato- Regional lymphadenopathy is
These reactions occur at a distant site phytes can be identified within 2 weeks. common. Skin lesions of lupus erythe-
and are devoid of organisms. Ide Identification depends on gross colony matosus show atrophy, scaling and
reactions may be triggered by anti- and microscopic morphology. follicular plugging. Hair loss is
fungal treatment. These patients have a permanent.
strong delayed-type hypersensitivity Wood’s lamp examination
reaction to intradermal dermatophyte Wood’s lamp is a source of long wave Psoriasis shows patches of erythema
antigens. These eruptions may be (365 nm) ultraviolet light. Hairs infected with silvery scaling. Hair loss is un-
vesicular, especially of the hands and by M canis, M audouinii and M ferru- common. Hairs are not broken. Lesions
feet, dermatitis-like, annular (e.g. gineum fluoresce a bright green to may be present elsewhere, such as the
erythema annulare centrifugum) or yellow-green color. Hairs infected by T elbows, knees and lower back.
nodular (e.g. erythema nodosum). schoenleinii may show a dull green or
blue-white color. T verrucosum exhibits Seborrhoeic dermatitis, characterised by
The causative fungal organisms of tinea a green fluorescence in cow hairs, but greasy scaling and variable hair loss, is
capitis destroy hair and pilo- sebaceous infested human hairs do not fluoresce. T uncommon in childhood. Seborrhoeic
structures, resulting in severe hair loss violaceum, the causative fungus of dermatitis may also involve the ears,
and scarring alopecia. The disease is grey patch tinea capitis, is Wood’s light eyebrows, paranasal area, chin, anterior
detrimental, both physically and negative. Wood’s light is not used in chest, back and intertriginous areas. In
mentally, to children who are affected. the Department of Dermatology. seborrhoeic dermatitis hairs are not
Young patients with itchy scalp and broken.
patchy or total hair loss frequently are Scalp biopsy
ridiculed, isolated and bullied by This procedure is seldom employed in Patchy hair loss occurs in secondary
classmates or playmates. In
10 SA Pharmaceutical Journal – October 2006
CLINICAL
syphilis (motheaten alopecia). When occur with coadministration of HMG- creases in cyclosporine concentrations
secondary syphilis is suspected, one CoA reductase inhibitors (lovastatin or may occur when administered con-
should look for generalised lympha- simvastatin); coadministration with currently. Safety for use during
denopathy, symmetrical skin eruptions cisapride can cause cardiac rhythm pregnancy has not been established.
with palmoplantar involvement, snail- abnormalities and death; may increase
track ulcers of the oral mucosae and digoxin levels; coadministration may Patients should be followed up
condylomata lata. Serological tests for increase plasma levels of midazolam clinically, by KOH-preparation and
syphilis are positive. or triazolam; phenytoin and rifampin microscopy, by Wood’s light examina-
may reduce itraconazole levels. Safety tion, and myocologically (= culture).
Griseofulvin is the treatment of choice for for use during pregnancy has not been Children receiving treatment may
tinea capitis. established. attend school. Haircuts, shaving of the
head, and wearing a cap during
Alternative treatments for tinea capitis Terbinafine is given in a dosage of 62.5 treatment are not necessary.
include itraconazole, fluconazole and mg/day (<20 kg), 125 mg/day (20-40 kg)
terbinafine. and 250 mg/day (>40 kg). Treat- ment Deterrence/prevention
should be given for 2-6 weeks (usual
Itraconazole should be administered at range, 2-4 weeks). Documented Asymptomatic carriers should be
a dosage of 3-5 mg/kg for 2-6 weeks hypersensitivity is the main contra- detected and treated, since they are the
(usual range, 2-4 weeks). The oral indication. May decrease cyclosporine continuous source of infection. Sib-
solution contains cyclodextrin, which effects; toxicity of terbinafine may lings and playmates of patients should
may cause diarrhoea in children. increase with rifampin and cimetidine. avoid close physical contact and
Contraindications include documented The drug is safe in pregnancy but sharing of toys or other personal
hypersensitivity; concomitant adminis- benefits must outweigh the risks. objects, such as combs and hair-
tration with HMG-CoA reductase brushes, since organisms can spread
inhibitors (e.g. lovastatin, simvastatin), The dosage of fluconazole is 6 mg/kg from one person to another and infec-
astemizole (recalled from US Market), for 20 days. Documented hyper- tious agents can be transported to
cisapride, midazolam, triazolam, or sensitivity is the main contraindication. different classrooms within the same or
terfenadine (recalled from the US Levels may increase with hydro- different schools. Shared facilities and
market) are contraindicated. Antacids chlorothiazides; fluconazole levels may objects also may promote spread of
may reduce absorption of itraconazole; decrease with chronic coadministration disease, both within the home and
oedema may occur with coadministra- of rifampin; coadministration of flucona- classroom.❒
tion of calcium channel blockers (e.g. zole may decrease phenytoin
amlodipine, nifedipine); hypoglycaemia clearance; may increase concen- REFERENCES
may occur with sulphonylureas; may trations of theophylline, tolbutamide, 1. Koa GF. Tinea capitis. eMedicine Journal
2002;3(1):1-17.
increase tacrolimus and cyclosporine glyburide, and glipizide; effects of www.emedicine.com/derm/topic420.htm
plasma concentrations when high anticoagulants may increase with 2. Frieden IJ and Howard R. Tinea Capitis:
epidemiology, diagnosis, treatment and control. J
doses are used; rhabdomyolysis may fluconazole coadministration; in- Am Acad Dermatol 1994;31:542-546.
You might also like
- Mari Fitness Home Guide PDFDocument30 pagesMari Fitness Home Guide PDFviva100% (1)
- Diagnosis and Management of Common Tinea InfectionsDocument23 pagesDiagnosis and Management of Common Tinea InfectionsGiovanni AnggastaNo ratings yet
- Critical Care NephrologyDocument209 pagesCritical Care NephrologyJohn Karol Ramirez100% (5)
- The Diagnosis and Management of Tinea CapitisDocument4 pagesThe Diagnosis and Management of Tinea CapitisKeyla Kehara PutriNo ratings yet
- DERMATOMYCOSISDocument114 pagesDERMATOMYCOSISQonita Qurrota AyunNo ratings yet
- Ringworm (Tinea Capitis)Document15 pagesRingworm (Tinea Capitis)farmasi_hmNo ratings yet
- Fungal Skin Infections ملزمةDocument6 pagesFungal Skin Infections ملزمةعبدالرحمن طارق عبدالله صالحNo ratings yet
- Tinea Capitis Inggris CKDocument3 pagesTinea Capitis Inggris CKBhagawanta AptakayanaNo ratings yet
- Derma To Phyto SesDocument5 pagesDerma To Phyto SesNia Sari Nastiti LubisNo ratings yet
- Fungal InfectionsDocument9 pagesFungal InfectionsCoral Srinivasa RamaluNo ratings yet
- Tinea Capitis EmedicineDocument16 pagesTinea Capitis EmedicineIkram IkramNo ratings yet
- Tinea CapitisDocument9 pagesTinea CapitisadityakafiberkahsmgNo ratings yet
- Tinea CapitisDocument7 pagesTinea Capitismufidah nurfajNo ratings yet
- BAHAN Tinea CapitisDocument28 pagesBAHAN Tinea CapitisYorika HafelaniNo ratings yet
- Tinea Corporis Pedia-1Document11 pagesTinea Corporis Pedia-1Denso Antonius LimNo ratings yet
- E Tra: Diagnosis and Management of Cutaneous Tinea InfectionsDocument8 pagesE Tra: Diagnosis and Management of Cutaneous Tinea InfectionsFuad hadyanNo ratings yet
- Tinea CapitisDocument7 pagesTinea CapitisNadya LiemNo ratings yet
- Superficial Fungal Infections of The Skin VoiceoverDocument67 pagesSuperficial Fungal Infections of The Skin VoiceoverMedo JT100% (1)
- Superficial Fungal InfectionsDocument40 pagesSuperficial Fungal InfectionsMarimuthu PrabhakaranNo ratings yet
- Medical MycologyDocument14 pagesMedical Mycologyhawkar omerNo ratings yet
- Tinea BarbaeDocument4 pagesTinea BarbaeKevin EdroNo ratings yet
- Super Ficial Fungal Infections: Key PointsDocument4 pagesSuper Ficial Fungal Infections: Key PointsBagus Putra KurniawanNo ratings yet
- Mycology: Clinical FindingsDocument5 pagesMycology: Clinical FindingsLuqman Al-Bashir FauziNo ratings yet
- Tinea Capitis Q & ADocument2 pagesTinea Capitis Q & Aandre yuindartantoNo ratings yet
- Tinea Corporis BologniaDocument4 pagesTinea Corporis BologniaHardiyanti HermanNo ratings yet
- Topical Treatment of Common Superficial Tinea InfectionsDocument8 pagesTopical Treatment of Common Superficial Tinea InfectionsColate LocoNo ratings yet
- The Kerion An Angry Tinea Capitis PBDocument7 pagesThe Kerion An Angry Tinea Capitis PBprajnamitaNo ratings yet
- Tinea FasialisDocument8 pagesTinea FasialisFelix Tortora SekaiNo ratings yet
- Palmoplantar PustulosisDocument6 pagesPalmoplantar PustulosisputraimanullahNo ratings yet
- Superficial MycosisDocument8 pagesSuperficial MycosisLuqman Al-Bashir FauziNo ratings yet
- Chapter 4Document103 pagesChapter 4tenaw100% (1)
- Superficial Mycoses 3Document8 pagesSuperficial Mycoses 3Mohammad KaifNo ratings yet
- DermatophytosisDocument5 pagesDermatophytosisRadovan Miki RadovanovicNo ratings yet
- L3 - DermatophytesDocument40 pagesL3 - Dermatophytesdvph2fck6qNo ratings yet
- Tinea Capitis: Audouinii), Which Give A Typical Green Fluorescence. T. Rubrum, The Commonest Cause of TineaDocument10 pagesTinea Capitis: Audouinii), Which Give A Typical Green Fluorescence. T. Rubrum, The Commonest Cause of TineaSyamsul ArifinNo ratings yet
- Tinea Capitis Favus-Like Appearance: Problem of Diagnosis: Dwi Ratna Adisty, Linda AstariDocument7 pagesTinea Capitis Favus-Like Appearance: Problem of Diagnosis: Dwi Ratna Adisty, Linda AstarihaningpradyNo ratings yet
- Lecture 2 MycologyDocument22 pagesLecture 2 MycologyDragon Gie30No ratings yet
- (JURNAL) Update Terapy MycosesDocument51 pages(JURNAL) Update Terapy MycosesHabibah Nurla LumiereNo ratings yet
- Systemic MycologyDocument95 pagesSystemic Mycologytejasbhukal567No ratings yet
- M13 - Dermatology - Chapter 5Document11 pagesM13 - Dermatology - Chapter 5Idham BaharudinNo ratings yet
- TineaDocument4 pagesTineaFenni OktoberryNo ratings yet
- Week 3. DermatophytesDocument48 pagesWeek 3. DermatophytesAsdfghjklNo ratings yet
- Fungal Skin Infections-1Document27 pagesFungal Skin Infections-1Fabb Nelson100% (1)
- Dermatophytosis: LectureDocument35 pagesDermatophytosis: LectureGideon MukalaziNo ratings yet
- Fungal InfectionDocument5 pagesFungal InfectionFiras HamidehNo ratings yet
- Mikosis SuperfisialDocument46 pagesMikosis SuperfisialAdipuraAtmadjaEgokNo ratings yet
- Dermatomycosis 18th July 2021Document120 pagesDermatomycosis 18th July 2021Sekar OktaviaNo ratings yet
- Superficial MycosisDocument61 pagesSuperficial MycosisBrightKinglySweetDomsonNo ratings yet
- Fungal Pathogens GroupingsDocument25 pagesFungal Pathogens GroupingsJhade Rio GadinganNo ratings yet
- Itrafungol PrezentareDocument20 pagesItrafungol PrezentaredCpoPPNo ratings yet
- Derm Quick ReviewDocument124 pagesDerm Quick ReviewRohit NalamasuNo ratings yet
- Dermatophytosis: EtiologyDocument6 pagesDermatophytosis: EtiologyTheresia FalentinaNo ratings yet
- Tinea - The DermatophytesDocument67 pagesTinea - The Dermatophytesmansoor aliNo ratings yet
- Tinea Barbae Is A Rare Dermatophytic Infection That Is Limited To The Bearded Areas of The FaceDocument3 pagesTinea Barbae Is A Rare Dermatophytic Infection That Is Limited To The Bearded Areas of The FaceMardiah Nurul HasanahNo ratings yet
- Fungal Diseases (Mycoses)Document48 pagesFungal Diseases (Mycoses)Claire GonoNo ratings yet
- IT-11 DERMATOMIKOSIS SUPERFISIALIS Edit 8 OktDocument69 pagesIT-11 DERMATOMIKOSIS SUPERFISIALIS Edit 8 Oktputri.SpANo ratings yet
- Tinea Corporis, Tinea Cruris, Tinea Nigra, and Piedra: Dermatologic Clinics August 2003Document7 pagesTinea Corporis, Tinea Cruris, Tinea Nigra, and Piedra: Dermatologic Clinics August 2003Dicky KurniawanNo ratings yet
- Superficial & Cutaneous MycosesDocument42 pagesSuperficial & Cutaneous Mycosesdawam986142No ratings yet
- MycologyDocument55 pagesMycologyAlpana Laisom100% (2)
- Superficial MycosesDocument26 pagesSuperficial Mycosesdhainey100% (3)
- CHN Fungal InfectionDocument14 pagesCHN Fungal InfectionChrysteline FabrezNo ratings yet
- Dermatology Notes for Medical StudentsFrom EverandDermatology Notes for Medical StudentsRating: 4 out of 5 stars4/5 (5)
- Right Here Waiting: by - Richard MarxDocument1 pageRight Here Waiting: by - Richard MarxQuraisy jamal sahilNo ratings yet
- Laporan Penjualan Perangkat Komputer PD - KomputindoDocument3 pagesLaporan Penjualan Perangkat Komputer PD - KomputindoQuraisy jamal sahilNo ratings yet
- J. Biol. Chem.-2008-Musiek-19927-35Document18 pagesJ. Biol. Chem.-2008-Musiek-19927-35Quraisy jamal sahilNo ratings yet
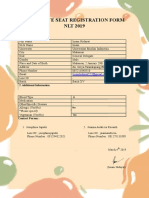
- Late Seat Registration Form NLT 2019: 1. General InformationDocument1 pageLate Seat Registration Form NLT 2019: 1. General InformationQuraisy jamal sahilNo ratings yet
- British Association of Dermatologists' Guidelines For The Management of Tinea Capitis 2014Document11 pagesBritish Association of Dermatologists' Guidelines For The Management of Tinea Capitis 2014Quraisy jamal sahilNo ratings yet
- After Class - AVTC4 - Unit 7 - Pie-ChartsDocument3 pagesAfter Class - AVTC4 - Unit 7 - Pie-Chartslequynhnhi1306No ratings yet
- JCM 11 07406Document10 pagesJCM 11 07406juajimenez55No ratings yet
- Respiratory System Word Search - WordMintDocument1 pageRespiratory System Word Search - WordMintJulio Cesar Pineda BetancourtNo ratings yet
- Building Coordinator HandbookDocument37 pagesBuilding Coordinator HandbookHélcio Vieira de Souza Jr.No ratings yet
- The Arc of North Carolina Compares N.C. House and Senate BudgetsDocument3 pagesThe Arc of North Carolina Compares N.C. House and Senate BudgetsNC Policy WatchNo ratings yet
- KGVK Business ModelDocument30 pagesKGVK Business ModelSomnath KejriwalNo ratings yet
- Excellence of Parry Spirulina-1Document2 pagesExcellence of Parry Spirulina-1Ashwyn1No ratings yet
- Velammal VidyalayaDocument19 pagesVelammal VidyalayaRammesh Kumar RNo ratings yet
- CEP Compro Juni 2023Document67 pagesCEP Compro Juni 2023didi sudiNo ratings yet
- Abstract Infusion Pumps Dedicated Sets Report 2018 PDFDocument2 pagesAbstract Infusion Pumps Dedicated Sets Report 2018 PDFmochkurniawanNo ratings yet
- Medical Officers Combatisation Course: "Annexure-A"Document7 pagesMedical Officers Combatisation Course: "Annexure-A"Murali KumarNo ratings yet
- Med AdmissionDocument3 pagesMed Admissionrujean romy p guisandoNo ratings yet
- Annotated BibliographyDocument7 pagesAnnotated BibliographyGENEVIEVE LANE POLONo ratings yet
- Cosmetology CBCDocument115 pagesCosmetology CBCMphilipT100% (1)
- Philip NitschkeDocument30 pagesPhilip NitschkeSean DalyNo ratings yet
- EMERGENCY AND DISASTER MANAGEMENT Unit 3Document12 pagesEMERGENCY AND DISASTER MANAGEMENT Unit 3Aparna KinginiNo ratings yet
- Chapter 46: Neurologic Disorders Garzon Maaks: Burns' Pediatric Primary Care, 7th EditionDocument5 pagesChapter 46: Neurologic Disorders Garzon Maaks: Burns' Pediatric Primary Care, 7th EditionHelen UgochukwuNo ratings yet
- Seminar On Rehabiliatation 11 TH AugDocument51 pagesSeminar On Rehabiliatation 11 TH AugValathati Beena MadhuriNo ratings yet
- Right To Health National and InternationalDocument17 pagesRight To Health National and Internationalsoukumar8305No ratings yet
- A Practical Handbook of Pancha Karma ProceduresDocument92 pagesA Practical Handbook of Pancha Karma ProceduresHari100% (1)
- Rogers and AggressionDocument11 pagesRogers and AggressionAnonymous ztqMxx75INo ratings yet
- Quick and Owren PDFDocument5 pagesQuick and Owren PDFpieterinpretoria391No ratings yet
- Khalanga Darchula New Vol 1 20200425 PDFDocument80 pagesKhalanga Darchula New Vol 1 20200425 PDFAmul ShresthaNo ratings yet
- Dr. Yoshimizu's Infrared Therapy Research With The Amethyst BiomatDocument2 pagesDr. Yoshimizu's Infrared Therapy Research With The Amethyst BiomatKusk29KuskNo ratings yet
- Serous Fluid: FormationDocument4 pagesSerous Fluid: FormationemmanuelNo ratings yet
- Dr. Sri Gautham Bodduluri MBBS, MS, Figo DOB: 26/10/1988 Languages: Telugu, English, Hindi, TamilDocument3 pagesDr. Sri Gautham Bodduluri MBBS, MS, Figo DOB: 26/10/1988 Languages: Telugu, English, Hindi, TamilvenugopalNo ratings yet
- Bipp Bismuth Iodine Paraffine Paste Pack RevisitedDocument2 pagesBipp Bismuth Iodine Paraffine Paste Pack RevisitedAyisha NazNo ratings yet
- Bulimia NervosaDocument4 pagesBulimia NervosaLillabinNo ratings yet